Abstract
Introduction
Lower urinary tract symptoms (LUTS) affect ≥60% of adult men and are associated with erectile dysfunction (ED) and sexual dissatisfaction.
Aim
The aim of this study was to evaluate the relationship among male LUTS, ED, and sexual satisfaction.
Methods
This was a secondary analysis of the Brazil LUTS study, a cross-sectional, epidemiological survey conducted by telephone interview in 5 cities in Brazil. This analysis included men aged ≥40 years.
Main Outcome Measure
LUTS were identified using International Continence Society definitions. LUTS severity was assessed using the International Prostate Symptom Score questionnaire. Erectile function was assessed using the International Index of Erectile Function-5 (IIEF-5) questionnaire and sexual satisfaction was rated on a 5-point scale.
Results
2,433 men participated in the study. Of 2,183 men reporting data on LUTS, 873 (40%) had LUTS “about half the time” or more. The prevalence of ED and sexual dissatisfaction was 14.4% and 7.8%, respectively. The proportion of men reporting ED and sexual dissatisfaction was higher among men with LUTS (24.6% and 13.8%, respectively) than men without LUTS (8.7% and 4.5%, respectively; P < .001). LUTS severity was negatively correlated with IIEF-5 scores (r = –0.199; P < .001); we estimated a 0.431-point decrease in IIEF-5 score per 3-point increase in International Prostate Symptom Score. Increased age and the presence of LUTS were associated with a greater chance of ED and sexual dissatisfaction; depression/anxiety and diabetes were associated with a greater chance of sexual dissatisfaction only. Among men with LUTS, urgency with fear of leaking, urgency urinary incontinence, and nocturnal enuresis were associated with a greater chance of ED, whereas slow stream and urgency urinary incontinence were associated with a greater chance of sexual dissatisfaction.
Conclusion
These results demonstrate that the presence of LUTS is associated with an increased chance of ED and sexual dissatisfaction in Brazilian men and reinforce the importance of a comprehensive assessment of these conditions.
Gomes CM, Averbeck MA, Koyama M, et al. Association Among Lower Urinary Tract Symptoms, Erectile Function, and Sexual Satisfaction: Results from the Brazil LUTS Study. Sex Med 2019;8:45–56.
Key Words: Erectile Dysfunction, Lower Urinary Tract Symptoms, Men, Prevalence, Sexual Satisfaction
Introduction
According to the definition provided by the International Continence Society, lower urinary tract symptoms (LUTS) is a general term that describes storage, voiding, and post-micturition symptoms.1 The prevalence of LUTS in men exceeds 60% and increases with age.2
Erectile dysfunction (ED)3 is also very prevalent in men aged ≥40 years and, similar to LUTS, is age dependent. The Kinsey survey is a comprehensive study on male sexual behavior conducted in the United States that reported that the prevalence of ED in a sample of 5,460 white and 177 black male subjects was 42% and increased with age.4 In Brazil, ED impacts up to 45% of men, and its prevalence and severity both increase with age.5 Epidemiological studies have shown that LUTS and ED share common risk factors, including obesity, smoking, depression, hypertension, diabetes, and dyslipidemia.6 Furthermore, several common biological mechanisms between ED and LUTS have been proposed,6 although a causal relationship has not been established. An association between LUTS and ED has been widely demonstrated among men in Asia,7 Europe,8,9 and the United States.8,10 In line with these findings, an analysis of Brazilian men aged ≥45 years who participated in a prostate cancer screening program reported a prevalence of ED among men with LUTS of 58% and demonstrated that men with LUTS are more likely to develop ED than those without LUTS.11 However, given that the patient population consisted of men seeking urologic care, these results may not be representative of the general Brazilian population.
Both ED and LUTS can negatively impact quality of life and sexual health. Men with ED report negative effects on self-esteem, work, and social relationships, and ED has been shown to be associated with reduced sexual satisfaction.12, 13, 14 However, despite the availability of effective medications, the rate of treatment-seeking behavior for ED remains low, ranging among 7.7% in Brazil,13 17−43% across Asia,15 and 21−56% in the United States and Europe.16 Commonly reported reasons for low treatment-seeking behavior include the belief that ED is part of the aging process, expecting that ED will resolve spontaneously, reluctance/embarrassment of talking openly about ED with a physician,16 and, in some Asian countries, low availability of Western medicine.15 Although the relationship between LUTS and ED has been well established,17 data on the inter-relationship among LUTS, sexual dysfunction, and sexual satisfaction are limited, particularly in the Brazilian male population and awareness of the importance of sexual satisfaction in general health and quality of life is increasing. More recent studies have shown that overall sexual health was rated as highly important in regard to quality of life, particularly among those who considered themselves to be in good health,18 and that the presence of comorbidities (ie, hypertension, dyslipidemia, diabetes, and depression) that are known to be associated with sexual dysfunction increases the likelihood of sexual dissatisfaction.19 As such, the assessment of sexual satisfaction as part of routine clinical practice is gaining attention.
The Brazil LUTS study was a large cross-sectional study evaluating the prevalence of LUTS among men and women aged ≥40 years in 5 major cities in Brazil.20 When frequency of LUTS was defined as “less than half the time” or more, the prevalence of LUTS was 75% overall and 69% in men; when defined as “half the time” or more, the prevalence was 49% overall and 40% in men. The objectives of this secondary analysis of the Brazil LUTS study were to investigate the association among male LUTS, erectile function, and sexual satisfaction, and to identify factors associated with ED and sexual dissatisfaction among men with LUTS.
Materials and Methods
Study Design, Patients, and Setting
Brazil LUTS was a cross-sectional, epidemiologic survey conducted by telephone interview between September 1, 2015, and December 31, 2015. Study participants were men aged ≥40 years who had access to residential telephone lines, residing in 5 Brazilian cities (São Paulo, Porto Alegre, Recife, Belém, and Goiânia). To avoid any potential confounding of urinary symptoms, subjects with a history of urinary tract infection at the time of the interview were excluded. The study was approved by a local ethics committee (Ethics Committee of the University of São Paulo School of Medicine) and was performed in compliance with Good Clinical Practice and in accordance with the Declaration of Helsinki. Verbal informed consent was provided by all participants by acknowledging the following script by the interviewer “Verbal consent to participate in this telephone survey will be obtained documenting the participant’s willingness to continue with the telephone survey.” The full methodology of the Brazil LUTS study has been published previously.20 This report is a secondary analysis that focused on the male subpopulation and the inter-relationship among LUTS, erectile function, and sexual satisfaction.
Outcome Measures
The assessment of LUTS was based on the International Continence Society definitions.1 The frequency of individual LUTS (voiding, storage, or post-micturition symptoms) was reported on a Likert scale (0 = not at all; 1 = <1 in 5 times; 2 = less than half the time; 3 = about half the time; 4 = more than half the time; and 5 = almost always) and was used to determine the presence of LUTS in accordance with previous studies8; the occurrence of any individual LUTS was defined as a score of 3–5 (ie, frequency of “about half the time” or more). LUTS severity was assessed using the International Prostate Symptom Score (IPSS) questionnaire,21 comprising 7 questions on urinary symptoms and a score ranging between 0 and 35 points (0 = none; 1–7 = mild; 8–19 = moderate; and 20–35 = severe). Bother associated with LUTS was assessed using a Likert scale for each symptom (0 = not at all; 5 = a very great deal). Assessments of erectile function were conducted on subjects who were sexually active in the past 6 months and were based on the International Index of Erectile Function-5 (IIEF-5) questionnaire,22 with a total score ranging between 1 and 25 (1–7 = severe; 8–11 = moderate; 12–16 = mild-moderate; 17–21 = mild; and 22–25 = no ED). For the purposes of this study, the presence of ED was defined as a score of <17 on the IIEF-5 questionnaire.23 Sexual satisfaction among sexually active subjects was rated on a 5-point scale (1 = very satisfied; 2 = satisfied; 3 = unsure; 4 = dissatisfied; and 5 = very dissatisfied); sexual dissatisfaction was defined as a score of ≥3.
Statistical Analyses
Because this is a secondary analysis, no formal sample size calculations were performed on these analyses. The sample size calculation was performed on the primary objective and was determined to be 1,000 interviews in each of the 5 cities.20 Descriptive statistics were used to summarize continuous data. Categorical data were summarized as the number and proportion of the total population. A chi-squared test and 1-way anova were used for categorical and continuous variables, respectively, with an alpha level of significance of 0.05. Logistic and ordered logit regression models were used to assess the association between dependent variables (ie, erectile function and sexual satisfaction [logistic regression for sexual satisfaction in dichotomic form {all men} and ordered logit for sexual satisfaction in 5 levels {men with LUTS}], respectively) and predictor variables (ie, age, educational status, working situation, marital status, body mass index, smoking status, physical activity, comorbidities [depression/anxiety, diabetes, hypertension, heart disease, constipation, and dyslipidemia], and LUTS). The relationship between IPSS and IIEF was evaluated using Pearson’s correlation coefficient and linear regression. Statistical analyses were performed with SPSS (version 20 for Windows).
Results
Of 17,600 subjects contacted, a total of 5,184 men and women completed the interview, and 2,433 men met the eligibility criteria. Among them, 2,183, 1,871, and 2,034 men provided data on LUTS, erectile function, and sexual satisfaction, respectively. Of the 2,183 men who reported data on LUTS, 873 (40%) had LUTS “about half the time” or more. The overall prevalence of ED and sexual dissatisfaction was 14.4% (269/1,871) and 7.8% (159/2,034), respectively, and the prevalence of LUTS among men with ED was 61.0% (164/269). Among men with LUTS, 666 respondents provided evaluable data on erectile function and 723 provided evaluable data on sexual satisfaction (Table 1). The demographic characteristics of the subjects with and without LUTS who also provided evaluable data on erectile function and sexual satisfaction are reported in Tables 2 and 3.
Table 1.
Prevalence of sexual satisfaction and erectile function by the occurrence of LUTS
| LUTS |
No LUTS |
Total |
P value | ||||
|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | ||
| Sexual satisfaction | 723 | 100 | 1,311 | 100 | 2,034 | 100 | < .001 |
| Yes | 623 | 86.2 | 1,252 | 95.5 | 1,875 | 92.2 | |
| No | 100 | 13.8 | 59 | 4.5 | 159 | 7.8 | |
| Erectile function | 666 | 100 | 1,206 | 100 | 1,871 | 100 | < .001 |
| Normal function | 502 | 75.4 | 1,100 | 91.2 | 1,602 | 85.6 | |
| Dysfunction | 164 | 24.6 | 106 | 8.8 | 269 | 14.4 | |
All data values are weighted (sample weight); subgroups may not equal the total number in all instances due to rounding and/or weighted values.
LUTS = lower urinary tract symptoms.
Table 2.
Demographics of men with (N = 873) and without (N = 1,310) LUTS
| LUTS (N = 873) |
No LUTS (N = 1,310) |
Total (N = 2,183) |
P value | |
|---|---|---|---|---|
| Age | <.001 | |||
| Mean (SE) | 57.6 (0.6) | 53.8 (0.4) | 55.3 (0.4) | |
| Median | 56.0 | 52.0 | 54.0 | |
| Range | 40.0-91.0 | 40.0-86.0 | 40.0-91.0 | |
| Age category, n (%) | 873 (100) | 1,310 (100) | 2,183 (100) | <.001 |
| 40–49 | 224 (25.7) | 500 (38.2) | 724 (33.2) | |
| 50–59 | 303 (34.7) | 479 (36.6) | 782 (35.8) | |
| 60–69 | 209 (23.9) | 227 (17.3) | 436 (20.0) | |
| ≥70 | 137 (15.7) | 104 (7.9) | 241 (11.0) | |
| Education status, n (%) | 873 (100) | 1,310 (100) | 2,183 (100) | <.001 |
| Illiterate | 39 (4.5) | 33 (2.5) | 72 (3.3) | |
| Incomplete elementary education | 271 (31.0) | 232 (17.7) | 503 (23.0) | |
| Complete elementary | 155 (24.9) | 221 (16.9) | 375 (17.2) | |
| Complete high school | 217 (24.9) | 400 (30.5) | 617 (28.3) | |
| College | 191 (21.9) | 425 (32.4) | 616 (28.2) | |
| Work status, n (%) | 860 (100) | 1,276 (100) | 2,136 (100) | <.001 |
| Active | 449 (52.2) | 840 (65.8) | 1,289 (60.3) | |
| Unemployed | 67 (7.8) | 101 (7.9) | 168 (7.9) | |
| Retired or pensioner | 315 (36.6) | 256 (20.1) | 571 (26.7) | |
| Other | 29 (3.4) | 80 (6.3) | 109 (5.1) | |
| Marital status, n (%) | 867 (100) | 1,300 (100) | 2,167 (100) | .055 |
| Single | 79 (9.1) | 130 (10.0) | 209 (9.6) | |
| Married or living with partner | 667 (76.9) | 1,068 (82.2) | 1,734 (80.0) | |
| Separated or divorced | 68 (7.8) | 69 (5.3) | 137 (6.3) | |
| Widower | 53 (6.1) | 33 (2.5) | 86 (4.0) | |
| Nutritional status, n (%) | 866 (100) | 1,290 (100) | 2,156 (100) | .832 |
| Underweight (BMI <18.5) | 7 (0.8) | 6 (0.5) | 13 (0.6) | |
| Eutrophic (18.5 ≤BMI <25) | 292 (33.7) | 418 (32.4) | 710 (32.9) | |
| Overweight (25 ≤BMI <30) | 384 (44.3) | 569 (44.1) | 953 (44.2) | |
| Obese (BMI ≥30) | 183 (21.1) | 297 (23.0) | 480 (22.3) | |
| Smoking, n (%) | 873 (100) | 1,310 (100) | 2,183 (100) | .094 |
| Never | 379 (43.4) | 680 (51.9) | 1,059 (48.5) | |
| Ex-smoker | 337 (38.6) | 431 (32.9) | 768 (35.2) | |
| Smoker | 157 (18.0) | 199 (15.2) | 356 (16.3) | |
| Physical activity∗, n (%) | 873 (100) | 1,310 (100) | 2,183 (100) | |
| Sedentary | 488 (55.9) | 590 (45.0) | 1,078 (49.4) | .018 |
| Moderate | 143 (16.4) | 264 (20.2) | 407 (18.6) | |
| High | 242 (27.7) | 456 (34.8) | 698 (32.0) | |
| Depression/anxiety, n (%) | 868 (100) | 1,310 (100) | 2,178 (100) | <.001 |
| No | 747 (86.1) | 1,231 (94.0) | 1,977 (90.8) | |
| Yes | 121 (13.9) | 80 (6.1) | 201 (9.2) | |
| Diabetes, n (%) | 873 (100) | 1,310 (100) | 2,183 (100) | <.001 |
| No | 727 (83.3) | 1,208 (92.2) | 1,935 (90.8) | |
| Yes | 146 (16.7) | 102 (7.8) | 248 (11.4) | |
| Hypertension, n (%) | 873 (100) | 1,310 (100) | 2,183 (100) | .001 |
| No | 543 (62.2) | 967 (73.8) | 1,510 (69.2) | |
| Yes | 330 (37.8) | 343 (26.2) | 673 (30.8) | |
| Cardiac diseases, n (%) | 872 (100) | 1,310 (100) | 2,183 (100) | <.001 |
| No | 769 (92.5) | 1249 (95.3) | 2,018 (92.4) | |
| Yes | 103 (11.8) | 62 (4.7) | 165 (7.6) | |
| Constipation, n (%) | 872 (100) | 1,310 (100) | 2,182 (100) | .119 |
| No | 807 (92.5) | 1,250 (95.4) | 2,057 (94.3) | |
| Yes | 65 (7.5) | 60 (4.6) | 125 (5.7) | |
| Dyslipidemia, n (%) | 871 (100) | 1,301 (100) | 2,172 (100) | .126 |
| No | 656 (75.3) | 1,043 (80.2) | 1,698 (78.2) | |
| Yes | 215 (24.7) | 258 (19.8) | 474 (21.8) |
All data values are weighted (sample weight); subgroups may not equal the total number in all instances due to rounding and/or weighted values.
BMI = body mass index; LUTS = lower urinary tract symptoms.
Sedentary, no physical activity; moderate = 1–2 times per week or 3–4 times per week for at least 30 minutes; high = 3–4 times per week for >30 minutes or 5–7 times per week for at least 30 minutes or 5–7 times per week for >30 minutes.
Table 3.
Demographics of men with LUTS by erectile function (N = 666) and sexual satisfaction (N = 723)
| Erectile function |
Sexual satisfaction |
|||||||
|---|---|---|---|---|---|---|---|---|
| Normal function | Dysfunction∗ | Total | P value | Satisfied | Dissatisfied† | Total | P value | |
| Age | .016 | .172 | ||||||
| Mean (SE) | 54.5 (0.7) | 58.1 (1.3) | 55.4 (0.6) | 55.3 (0.6) | 57.9 (1.8) | 55.7 (0.6) | ||
| Median | 53.0 | 58.0 | 55.0 | 55.0 | 56.0 | 55.0 | ||
| Range | 40.0-85.0 | 40.0-82.0 | 40.0-85.0 | 40.0-86.0 | 40.0-85.0 | 40.0-86.0 | ||
| Age category, n (%) | 502 (100) | 164 (100) | 666 (100) | .019 | 623 (100) | 100 (100) | 723 (100) | .426 |
| 40–49 | 168 (33.5) | 33 (20.1) | 201 (30.2) | 181 (29.1) | 27 (27.0) | 208 (28.8) | ||
| 50–59 | 200 (39.8) | 51 (31.1) | 251 (37.7) | 247 (39.6) | 32 (32.0) | 279 (38.6) | ||
| 60–69 | 101 (20.1) | 59 (36.0) | 160 (24.0) | 148 (23.8) | 25 (25.0) | 173 (23.9) | ||
| ≥70 | 33 (6.6) | 21 (12.8) | 54 (8.1) | 47 (7.5) | 16 (16.0) | 63 (8.7) | ||
| Education status, n (%) | 502 (100) | 164 (100) | 666 (100) | .108 | 623 (100) | 100 (100) | 723 (100) | .394 |
| Illiterate | 9 (1.8) | 4 (2.4) | 13 (2.0) | 20 (3.2) | 4 (4.0) | 24 (3.3) | ||
| Incomplete elementary education | 110 (21.9) | 61 (37.2) | 171 (25.7) | 167 (26.8) | 32 (32.0) | 199 (27.5) | ||
| Complete elementary | 94 (18.7) | 34 (20.7) | 128 (19.2) | 102 (16.4) | 31 (31.0) | 133 (18.4) | ||
| Complete high school | 158 (31.5) | 31 (18.9) | 189 (28.4) | 182 (29.2) | 16 (16.0) | 198 (27.4) | ||
| College | 132 (26.3) | 34 (20.7) | 166 (24.9) | 152 (24.4) | 17 (17.0) | 169 (23.4) | ||
| Work status | 496 (100) | 164 (100) | 660 (100) | .022 | 613 (100) | 98 (100) | 711 (100) | .285 |
| Active | 312 (71.6) | 72 (43.9) | 384 (58.2) | 366 (59.7) | 51 (52.0) | 417 (58.6) | ||
| Unemployed | 50 (11.5) | 14 (8.5) | 64 (9.7) | 51 (8.3) | 13 (13.3) | 64 (9.0) | ||
| Retired or pensioner | 115 (26.4) | 71 (43.3) | 186 (28.2) | 170 (27.7) | 34 (34.7) | 204 (28.7) | ||
| Other | 18 (4.1) | 7 (4.3) | 25 (3.8) | 25 (4.1) | 1 (1.0) | 26 (3.7) | ||
| Marital status | 502 (100) | 164 (100) | 666 (100) | .993 | 618 (100) | 100 (100) | 718 (100) | .028 |
| Single | 40 (8.0) | 15 (9.1) | 55 (8.3) | 50 (8.1) | 10 (10.0) | 60 (8.4) | ||
| Married or living with partner | 403 (80.3) | 132 (80.5) | 535 (80.3) | 503 (81.4) | 77 (77.0) | 580 (80.8) | ||
| Separated or divorced | 38 (7.6) | 12 (7.3) | 50 (7.5) | 48 (7.8) | 2 (2.0) | 50 (7.0) | ||
| Widower | 20 (4.0) | 6 (3.7) | 26 (3.9) | 16 (2.6) | 10 (10.0) | 26 (3.6) | ||
| Nutritional status | 499 (100) | 162 (100) | 661 (100) | .112 | 620 (100) | 98 (100) | 718 (100) | .124 |
| Underweight (BMI <18.5) | 3 (0.6) | 2 (1.2) | 5 (0.8) | 3 (0.5) | 2 (2.0) | 5 (0.7) | ||
| Eutrophic (≤18.5 BMI <25) | 173 (34.7) | 35 (21.6) | 208 (31.5) | 210 (33.9) | 27 (27.6) | 237 (33.0) | ||
| Overweight (≤25 BMI <30) | 233 (46.7) | 79 (48.8) | 312 (47.2) | 292 (47.1) | 45 (45.9) | 337 (46.9) | ||
| Obese (BMI ≥30) | 90 (18.0) | 46 (28.4) | 136 (20.6) | 114 (18.4) | 26 (26.5) | 140 (19.5) | ||
| Smoking | 502 (100) | 164 (100) | 666 (100) | .895 | 623 (100) | 100 (100) | 723 (100) | .147 |
| Never | 232 (46.2) | 78 (47.6) | 310 (46.5) | 282 (45.3) | 45 (45.0) | 327 (45.2) | ||
| Ex-smoker | 173 (34.5) | 59 (36.0) | 232 (34.8) | 222 (35.6) | 34 (34.0) | 256 (35.4) | ||
| Smoker | 96 (19.1) | 27 (16.5) | 123 (18.5) | 118 (18.9) | 20 (20.0) | 138 (19.1) | ||
| Physical activity‡ | 502 (100) | 164 (100) | 666 (100) | .028 | 623 (100) | 100 (100) | 723 (100) | .495 |
| Sedentary | 242 (48.2) | 111 (67.7) | 353 (53.0) | 349 (56.0) | 46 (46.0) | 395 (54.6) | ||
| Moderate | 89 (17.7) | 24 (14.6) | 113 (17.0) | 90 (14.4) | 29 (29.0) | 119 (16.5) | ||
| High | 171 (34.1) | 29 (17.7) | 200 (30.0) | 184 (29.5) | 26 (26.0) | 210 (29.0) | ||
| Depression/anxiety | 498 (100) | 164 (100) | 662 (100) | .324 | 623 (100) | 95 (100) | 718 (100) | .161 |
| No | 443 (89.0) | 138 (84.1) | 581 (87.8) | 551 (88.4) | 76 (80.0) | 627 (87.3) | ||
| Yes | 55 (11.0) | 27 (16.5) | 82 (12.4) | 73 (11.7) | 20 (21.1) | 93 (13.0) | ||
| Diabetes | 502 (100) | 164 (100) | 666 (100) | .012 | 623 (100) | 100 (100) | 723 (100) | .05 |
| No | 439 (87.5) | 119 (72.6) | 558 (83.8) | 535 (85.9) | 74 (74.0) | 609 (84.2) | ||
| Yes | 64 (12.7) | 45 (27.4) | 109 (16.4) | 89 (14.3) | 26 (26.0) | 115 (15.9) | ||
| Hypertension | 502 (100) | 164 (100) | 666 (100) | .188 | 623 (100) | 100 (100) | 723 (100) | .309 |
| No | 330 (65.7) | 92 (56.1) | 422 (63.4) | 399 (64.0) | 59 (59.0) | 458 (63.3) | ||
| Yes | 172 (34.3) | 72 (43.9) | 244 (36.6) | 225 (36.1) | 41 (41.0) | 266 (36.8) | ||
| Cardiac diseases | 502 (100) | 164 (100) | 666 (100) | .416 | 622 (100) | 100 (100) | 722 (100) | .682 |
| No | 455 (90.6) | 143 (87.2) | 598 (89.8) | 561 (90.2) | 92 (92.0) | 653 (90.4) | ||
| Yes | 47 (9.4) | 21 (12.8) | 68 (10.2) | 62 (10.0) | 8 (8.0) | 70 (9.7) | ||
| Constipation | 501 (100) | 164 (100) | 665 (100) | .429 | 622 (100) | 100 (100) | 722 (100) | .117 |
| No | 474 (94.6) | 150 (91.5) | 624 (93.8) | 587 (94.4) | 88 (88.0) | 675 (93.5) | ||
| Yes | 27 (5.4) | 14 (8.5) | 41 (6.2) | 35 (5.6) | 12 (12.0) | 47 (6.5) | ||
| Dyslipidemia | 501 (100) | 164 (100) | 665 (100) | .417 | 622 (100) | 99 (100) | 721 (100) | .224 |
| No | 373 (74.5) | 113 (68.9) | 486 (73.1) | 467 (75.1) | 68 (68.7) | 535 (74.2) | ||
| Yes | 128 (25.5) | 51 (31.1) | 179 (26.9) | 155 (24.9) | 32 (32.3) | 187 (25.9) | ||
Data are presented as n (%).
All data values are weighted (sample weight); subgroups may not equal the total number in all instances due to rounding and/or weighted values.
BMI = body mass index; LUTS = lower urinary tract symptoms.
International Index of Erectile Function-5 score of <17.
Score ≥3 on 5-point scale (1 = very satisfied; 2 = satisfied; 3 = unsure; 4 = dissatisfied; and 5 = very dissatisfied).
Sedentary, no physical activity; moderate = 1−2 times per week or 3−4 times per week for at least 30 minutes; high = 3−4 times per week for >30 minutes or 5−7 times per week for at least 30 minutes or 5−7 times per week for >30 minutes.
Among men with LUTS, increasing age was associated with ED (P = .019). There was no significant association between increasing age and sexual satisfaction, but the proportion of men who reported sexual dissatisfaction seemed to be higher among men aged ≥70 years compared with younger men (Figure 1).
Figure 1.
Age distribution of men with lower urinary tract symptoms according to (A) erectile dysfunction (International Index of Erectile Function-5 <17) and (B) sexual satisfaction.
Among all respondents who provided data on LUTS and erectile function, the proportion of men reporting ED was higher among men with LUTS (164/666 [24.6%]) compared with those without LUTS (106/1,206 [8.7%]; P < .001; Table 1). Similarly, among all respondents who provided data on LUTS and sexual satisfaction, a significantly larger proportion of men with LUTS (100/723 [13.8%]) reported sexual dissatisfaction compared with men without LUTS (59/1,311 [4.5%]). Among men with LUTS, a Pearson’s correlation revealed a weak negative correlation (r = –0.199; P < .001; N = 666) between IIEF-5 and IPSS. Furthermore, we estimated a decrease of 0.431 points in the IIEF-5 score for every 3-point increase in the IPSS score. When all men were included in the analysis (ie, with and without LUTS), the correlation was r = –0.276 (P < .001; N = 1873). Among all men who reported data on erectile function and sexual satisfaction, the proportion of men who reported sexual dissatisfaction was greater among those who also reported ED (59/270 [21.9%]) than those who had normal erectile function (83/1,602 [5.2%]; P < .001). This finding was also observed among men with LUTS (P = .008) and without LUTS (P < .001; Table 4).
Table 4.
Prevalence of erectile function by the occurrence of sexual satisfaction
| Sexual satisfaction |
P value | ||||||
|---|---|---|---|---|---|---|---|
| Yes |
No |
Total |
|||||
| N | % | N | % | N | % | ||
| Total | < .001 | ||||||
| Normal erectile function | 1,519 | 94.8 | 83 | 5.2 | 1,602 | 100 | |
| Erectile dysfunction | 211 | 78.1 | 59 | 21.9 | 270 | 100 | |
| No LUTS | < .001 | ||||||
| Normal function | 1,068 | 97.1 | 32 | 2.9 | 1,100 | 100 | |
| Dysfunction | 87 | 82.1 | 19 | 17.9 | 106 | 100 | |
| LUTS | .008 | ||||||
| Normal function | 451 | 89.8 | 51 | 10.2 | 502 | 100 | |
| Dysfunction | 124 | 75.6 | 40 | 24.4 | 164 | 100 | |
All data values are weighted (sample weight); subgroups may not equal the total number in all instances due to rounding and/or weighted values.
LUTS = lower urinary tract symptoms.
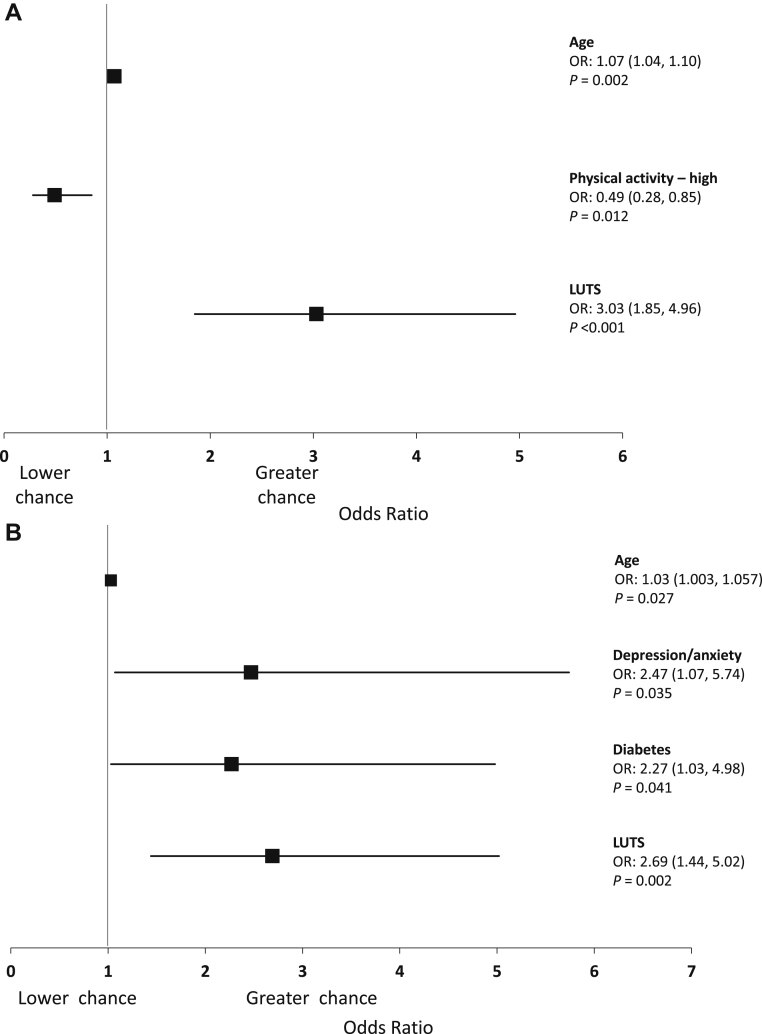
A multiple logistic regression model for erectile function and sexual satisfaction revealed that, among all respondents with available data (N = 1,871), increasing age and the presence of LUTS were associated with a greater chance of ED (age: odds ratio [OR], 1.07; 95% CI: 1.04−1.10; LUTS: OR, 3.03; 95% CI: 1.85−4.96). To the contrary, a high level of physical activity was associated with a reduced chance of ED (OR, 0.49; 95% CI: 0.28−0.85; Figure 2A). Furthermore, among all respondents with available data (N = 2,029), increasing age and the presence of depression/anxiety, diabetes, and LUTS were all associated with a greater chance of sexual dissatisfaction (age: OR, 1.03; 95% CI: 1.003−1.057; depression/anxiety: OR, 2.47; 95% CI: 1.07−5.74; diabetes: OR, 2.27; 95% CI: 1.03−4.98; LUTS: OR, 2.69; 95% CI: 1.44−5.02); Figure 2B). Data on all other predictor variables can be found in the Supporting Information.
Figure 2.
Association between (A) erectile dysfunction and (B) sexual dissatisfaction with sociodemographics, comorbidities, and lower urinary tract symptoms. OR = odds ratio.
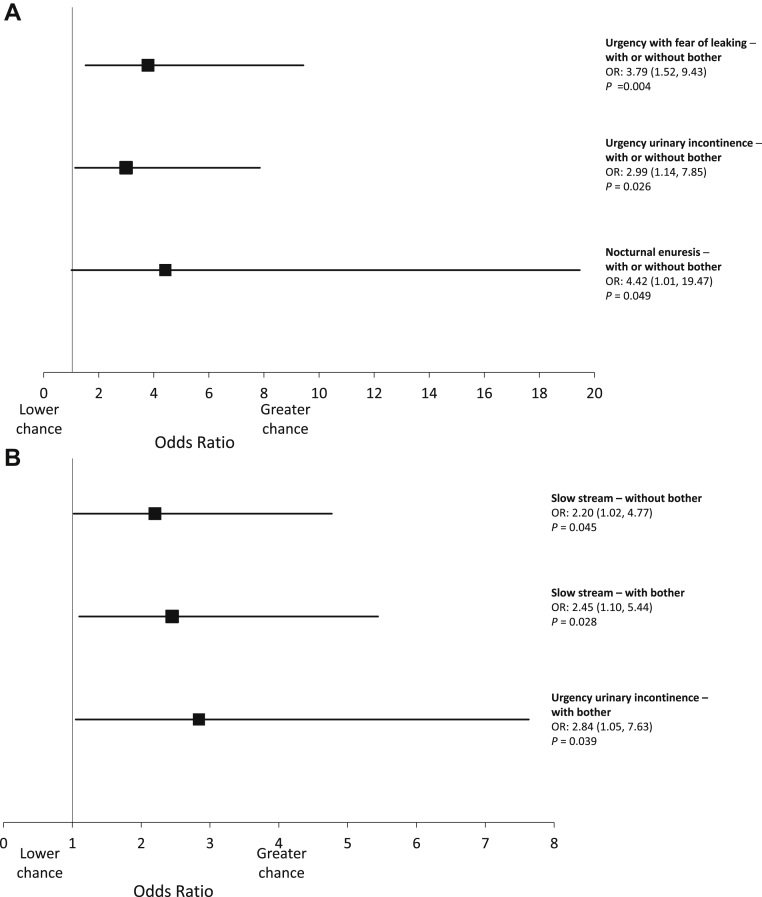
Among men with LUTS, the chance of ED was greater for those who reported urgency with fear of leaking (OR, 3.79; 95% CI: 1.52−9.43), urgency urinary incontinence (OR, 2.99; 95% CI: 1.14−7.85), and nocturnal enuresis (OR, 4.42; 95% CI: 1.01−19.47; Figure 3A) compared with subjects without symptoms, whereas the chance of more sexual dissatisfaction was significantly higher for those who reported slow stream, with (OR, 2.45; 95% CI: 1.10−5.44) or without (OR, 2.20; 95% CI: 1.02−4.77) bother, and urgency urinary incontinence with bother (OR, 2.84; 95% CI: 1.05−7.63; Figure 3B).
Figure 3.
Association of erectile dysfunction (A) and sexual dissatisfaction (B) with individual lower urinary tract symptoms (LUTS) and LUTS associated bother among men with LUTS. Analyses were controlled for sociodemographics and comorbidities. OR = odds ratio.
Discussion
The Brazil LUTS study20 is the largest study evaluating the prevalence of LUTS among men and women aged ≥40 years in Brazil. The results presented herein are from a secondary analysis of the Brazil LUTS study that represent the first to report on the impact of LUTS on sexual satisfaction in the Brazilian male population. In this study, the prevalence of LUTS occurring “about half the time” or more in men was 40%; the prevalence of ED and sexual dissatisfaction was 14.4% and 7.8%, respectively. The presence of LUTS was significantly associated with a greater likelihood of experiencing ED and sexual dissatisfaction. The proportion of men reporting ED or sexual dissatisfaction was significantly higher among men with LUTS (24.6% and 13.8%) compared with those without LUTS (8.7% and 4.5%). Using a Pearson’s correlation, we estimated a decrease of 0.431 points on the IIEF-5 for every 3-point increase in IPSS score (minimal clinically important difference) among men with LUTS. These results are similar to those reported in previous studies where a correlation between LUTS and sexual dysfunction was reported in Asia,7 Europe,8,9 and the United States.8,10 However, our findings are novel to Brazil and Latin America. A large multinational study conducted in Sweden, Italy, Germany, the United Kingdom, and Canada, reported that, among sexually active adults aged ≥18 years, the likelihood of having ED and sexual dissatisfaction was significantly higher among subjects with overactive bladder compared with controls.24 Similarly, multinational surveys of men aged 50 years or older conducted in the United States and Europe reported that the occurrence and severity of LUTS are risk factors for sexual dysfunction.17,25
The association between LUTS and sexual satisfaction has been less explored than that between LUTS and ED. Decreased sexual activity and sexual enjoyment were reported by men aged ≥40 years in the United Kingdom and the United States8 and a survey of Asian men aged ≥40 years reported that increasing severity and number of individual LUTS were both negatively associated with sexual desire, intercourse satisfaction, and overall satisfaction.26 Because sexual function and bother associated with LUTS may be influenced by cultural differences,27, 28, 29, 30 it is important to evaluate how LUTS and sexual satisfaction are associated in different populations. Our findings are in line with previous studies in other countries showing a correlation between LUTS severity and sexual dissatisfaction. We also report a relationship between ED and sexual dissatisfaction, in that the proportion of men who reported sexual dissatisfaction was higher among those who also reported ED. This finding is consistent with previous studies that reported a greater prevalence of sexual dissatisfaction among men with ED compared with men with normal erectile function.12,13
In this study, results from a multiple logistic regression model for erectile function and sexual satisfaction showed that, among all respondents, increasing age and the presence of LUTS increased the chance of experiencing ED, whereas a high level of physical activity was associated with a reduced chance. Moreover, LUTS, increasing age, depression/anxiety, and diabetes, were significantly associated with an increased chance of sexual dissatisfaction. An analysis of the impact of individual LUTS on erectile function demonstrated that the chance of ED increased among men reporting urgency with fear of leaking, urgency urinary incontinence, and nocturnal enuresis, and the chance of sexual dissatisfaction was higher in men who reported slow stream and urgency urinary incontinence. In line with these data, a previous study reported that older age, hypertension, diabetes, depression, and individual LUTS, including urgency with fear of leaking, weak stream, split stream, leaking during sexual activity, and dysuria, were all associated with ED.8
Interestingly, increasing age was significantly associated with ED but not with sexual satisfaction in men who reported LUTS in this study. This is consistent with recent findings where, in couples aged ≥18 years, improved sexual communication and a regular sexual routine were predictors of sexual satisfaction, whereas age was not.31 In addition, sexual satisfaction is positively correlated with IIEF-5 score, indicating greater sexual satisfaction with better erectile function,12 and increased sexual satisfaction is associated with less severe ED and with a shorter duration of ED.14 The lack of association between age and sexual satisfaction reported in this study may indicate that erectile function is a stronger predictor of sexual satisfaction than increasing age.
It is likely that ED and LUTS share common pathophysiological mechanisms, some of which are currently being investigated. These mechanisms include the nitric oxide-cyclic guanosine monophosphate pathway, Rho-kinase pathways, autonomic adrenergic hyperactivity, pelvic atherosclerosis/ischemia, inflammation, sex hormones (ie, low androgen levels), and psychological conditions (ie, depression).6 However, the mechanisms linking these 2 conditions have not been elucidated. Diabetes mellitus, metabolic syndrome, and obesity are among the risk factors common to ED and LUTS, and both conditions become more prevalent among aging men.6 An observational study of men with ED who participated in a prostate cancer screening program reported that hypertension, dyslipidemia, and a history of cardiovascular events were all significantly associated with moderate-to-severe ED.32 These differences in findings may be, in part, due to methodological variations, and represent a general limitation of observational studies. Considering the substantial impact of LUTS on ED, sexual satisfaction, and quality of life among men older than 40 years, the results of the current and previous studies support the importance of a comprehensive assessment of men with LUTS that includes not only the urinary aspect, but also sexual function and sexual satisfaction.18,19 Conversely, it would be beneficial to assess LUTS in men reporting with sexual dysfunction, as we estimated that a 3-point increase in IPSS score (minimal clinically important difference33) was associated with a decrease of 0.431 points in IIEF-5 score among men with LUTS. This approach would enable a more comprehensive evaluation of 2 highly prevalent and potentially detrimental conditions in men. It would also help in determining the most appropriate treatment strategy for each condition given the fact that medications for LUTS may affect sexual function. This has been shown with alpha-blockers, which can cause ejaculatory disorders, 5-alpha-reductase inhibitors, which may cause decreased libido, ED, and ejaculatory disorders, and phosphodiesterase type 5 inhibitors, which have demonstrated significant improvements in both LUTS and ED in men with LUTS associated with benign prostatic hyperplasia.34,35
One limitation of this study is that we used patient-reported questionnaires to assess LUTS. This system of data collection, which is the most commonly used in epidemiological studies, can provide only limited information about each symptom, and different methods of data collection used in a survey may result in varying responses. Comorbid conditions were self-reported, but not clinically verified, so all analyses, including these conditions, should be evaluated with caution. Furthermore, it has been demonstrated that self-reporting of health can be impacted by age, sex, and socioeconomic status.36 In this study, we used computer-assisted telephone interviews, which have been widely used in similar survey studies.2 A common limitation of epidemiological studies conducted via telephone interview is the reliance on patient-reported medical and medication history. As such, uses of current and previous medications were not collected in the survey. Furthermore, our data set included only those patients who reported survey responses relating to erectile function and sexual satisfaction, which may introduce a selection bias and may not be fully representative of the overall male Brazilian population. Finally, because this was a cross-sectional study, no causation between variables can be inferred.
Conclusions
This population-based study demonstrated that the presence of LUTS is associated with a significantly increased chance of ED and sexual dissatisfaction in Brazilian men. Specific LUTS, such as urgency with fear of leaking, urgency urinary incontinence, and nocturnal enuresis, were associated with ED. These findings support the importance of a comprehensive assessment of sexual function and satisfaction alongside the urinary aspect in men reporting with LUTS, which will complement treatment strategies for these conditions.
Statement of Authorship
Category 1
-
(a)Conception and Design
- Cristiano Mendes Gomes; Marcio Augusto Averbeck; Mitti Koyama; Roberto Soler
-
(b)Acquisition of Data
- Cristiano Mendes Gomes; Marcio Augusto Averbeck; Mitti Koyama; Roberto Soler
-
(c)Analysis and Interpretation of Data
- Cristiano Mendes Gomes; Marcio Augusto Averbeck; Mitti Koyama; Roberto Soler
Category 2
-
(a)Drafting the Article
- Cristiano Mendes Gomes; Marcio Augusto Averbeck; Mitti Koyama; Roberto Soler
-
(b)Revising It for Intellectual Content
- Cristiano Mendes Gomes; Marcio Augusto Averbeck; Mitti Koyama; Roberto Soler
Category 3
-
(a)Final Approval of the Completed Article
- Cristiano Mendes Gomes; Marcio Augusto Averbeck; Mitti Koyama; Roberto Soler
Acknowledgments
Editorial support was provided by OPEN Health Medical Communications and was funded by Astellas Pharma, Inc.
Footnotes
Conflict of Interest: Cristiano Mendes Gomes was a member of a scientific advisory board for the Brazil LUTS Study, which was funded by Astellas Pharma Brazil, and reports consulting and lecture fees from Astellas Pharma Brazil and Boston Scientifics Brazil, proctor fees from Medtronic Brazil, lecture fees from Zodiac Brazil, and a study grant from Ipsen Brazil. Marcio Augusto Averbeck reports advisory board membership fees from Coloplast Brazil, internal expert fees from GlaxoSmithKline, proctor fees from Medtronic Brazil, and principal investigator fees from Ipsen Brazil. Mitti Koyama reports statistical analysis fees from Astellas Pharma Brazil. Roberto Soler is an employee of Astellas Pharma Brazil.
Funding: This study was funded by Astellas Pharma, Inc. The funder of the study had a role in the study design, and was responsible for the collection, the analysis and interpretation of data, writing the report, and the decision to submit the paper for publication.
Supplementary Data
References
- 1.Abrams P., Cardozo L., Fall M. The standardisation of terminology of lower urinary tract function: Report from the Standardisation Sub-Committee of the International Continence Society. Neurourol Urodyn. 2002;21:167–178. doi: 10.1002/nau.10052. [DOI] [PubMed] [Google Scholar]
- 2.Irwin D.E., Milsom I., Hunskaar S. Population-based survey of urinary incontinence, overactive bladder, and other lower urinary tract symptoms in five countries: Results of the EPIC study. Eur Urol. 2006;50:1306–1314. doi: 10.1016/j.eururo.2006.09.019. [discussion: 1314−1315] [DOI] [PubMed] [Google Scholar]
- 3.Hatzimouratidis K., Amar E., Eardley I. Guidelines on male sexual dysfunction: Erectile dysfunction and premature ejaculation. Eur Urol. 2010;57:804–814. doi: 10.1016/j.eururo.2010.02.020. [DOI] [PubMed] [Google Scholar]
- 4.Hatzimouratidis K. Epidemiology of male sexual dysfunction. Am J Mens Health. 2007;1:103–125. doi: 10.1177/1557988306298006. [DOI] [PubMed] [Google Scholar]
- 5.Abdo C.H., Oliveira W.M., Jr., Scanavino Mde T. [Erectile dysfunction: Results of the Brazilian Sexual Life Study] Rev Assoc Med Bras (1992. 2006;52:424–429. doi: 10.1590/s0104-42302006000600023. [in Portuguese] [DOI] [PubMed] [Google Scholar]
- 6.De Nunzio C., Roehrborn C.G., Andersson K.E. Erectile dysfunction and lower urinary tract symptoms. Eur Urol Focus. 2017;3:352–363. doi: 10.1016/j.euf.2017.11.004. [DOI] [PubMed] [Google Scholar]
- 7.Li M.K., Garcia L.A., Rosen R. Lower urinary tract symptoms and male sexual dysfunction in Asia: A survey of ageing men from five Asian countries. BJU Int. 2005;96:1339–1354. doi: 10.1111/j.1464-410X.2005.05831.x. [DOI] [PubMed] [Google Scholar]
- 8.Wein A.J., Coyne K.S., Tubaro A. The impact of lower urinary tract symptoms on male sexual health: EpiLUTS. BJU Int. 2009;103(Suppl 3):33–41. doi: 10.1111/j.1464-410X.2009.08447.x. [DOI] [PubMed] [Google Scholar]
- 9.Hansen B.L. Lower urinary tract symptoms (LUTS) and sexual function in both sexes. Eur Urol. 2004;46:229–234. doi: 10.1016/j.eururo.2004.04.005. [DOI] [PubMed] [Google Scholar]
- 10.Chung W.S., Nehra A., Jacobson D.J. Lower urinary tract symptoms and sexual dysfunction in community-dwelling men. Mayo Clin Proc. 2004;79:745–749. doi: 10.4065/79.6.745. [DOI] [PubMed] [Google Scholar]
- 11.Reggio E., de Bessa J., Jr., Junqueira R.G. Correlation between lower urinary tract symptoms and erectile dysfunction in men presenting for prostate cancer screening. Int J Impot Res. 2007;19:492–495. doi: 10.1038/sj.ijir.3901557. [DOI] [PubMed] [Google Scholar]
- 12.Weiss P., Brody S. International Index of Erectile Function (IIEF) scores generated by men or female partners correlate equally well with own satisfaction (sexual, partnership, life, and mental health) J Sex Med. 2011;8:1404–1410. doi: 10.1111/j.1743-6109.2011.02214.x. [DOI] [PubMed] [Google Scholar]
- 13.Martins F.G., Abdo C.H.N. Erectile dysfunction and correlated factors in Brazilian men aged 18-40 years. J Sex Med. 2010;7:2166–2173. doi: 10.1111/j.1743-6109.2009.01542.x. [DOI] [PubMed] [Google Scholar]
- 14.Althof S.E., Buvat J., Gutkin S.W. Sexual satisfaction in men with erectile dysfunction: Correlates and potential predictors. J Sex Med. 2010;7(1 Pt 2):203–215. doi: 10.1111/j.1743-6109.2009.01554.x. [DOI] [PubMed] [Google Scholar]
- 15.Tan H.M., Low W.Y., Ng C.J. Prevalence and correlates of erectile dysfunction (ED) and treatment seeking for ED in Asian Men: The Asian Men's Attitudes to Life Events and Sexuality (MALES) study. J Sex Med. 2007;4:1582–1592. doi: 10.1111/j.1743-6109.2007.00602.x. [DOI] [PubMed] [Google Scholar]
- 16.Shabsigh R., Perelman M.A., Laumann E.O. Drivers and barriers to seeking treatment for erectile dysfunction: A comparison of six countries. BJU Int. 2004;94:1055–1065. doi: 10.1111/j.1464-410X.2004.05104.x. [DOI] [PubMed] [Google Scholar]
- 17.Moncada I. LUTS: A risk factor for sexual dysfunction in the BPH patient. Eur Urol Supp. 2003;2:3–8. [Google Scholar]
- 18.Flynn K.E., Lin L., Bruner D.W. Sexual satisfaction and the importance of sexual health to quality of life throughout the life course of U.S. adults. J Sex Med. 2016;13:1642–1650. doi: 10.1016/j.jsxm.2016.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.García-Gómez B., García-Cruz E., Bozzini G. Sexual satisfaction: An opportunity to explore overall health in men. Urology. 2017;107:149–154. doi: 10.1016/j.urology.2017.06.031. [DOI] [PubMed] [Google Scholar]
- 20.Soler R., Gomes C.M., Averbeck M.A. The prevalence of lower urinary tract symptoms (LUTS) in Brazil: Results from the epidemiology of LUTS (Brazil LUTS) study. Neurourol Urodyn. 2018;37:1356–1364. doi: 10.1002/nau.23446. [DOI] [PubMed] [Google Scholar]
- 21.Barry M.J., Fowler F.J., Jr., O'Leary M.P. The American Urological Association symptom index for benign prostatic hyperplasia. The Measurement Committee of the American Urological Association. J Urol. 1992;148:1549–1557. doi: 10.1016/s0022-5347(17)36966-5. [discussion: 1564] [DOI] [PubMed] [Google Scholar]
- 22.Rosen R.C., Riley A., Wagner G. The International Index of Erectile Function (IIEF): A multidimensional scale for assessment of erectile dysfunction. Urology. 1997;49:822–830. doi: 10.1016/s0090-4295(97)00238-0. [DOI] [PubMed] [Google Scholar]
- 23.Schroeck F.R., Donatucci C.F., Smathers E.C. Defining potency: A comparison of the International Index of Erectile Function short version and the Expanded Prostate Cancer Index Composite. Cancer. 2008;113:2687–2694. doi: 10.1002/cncr.23887. [DOI] [PubMed] [Google Scholar]
- 24.Irwin D.E., Milsom I., Reilly K. Overactive bladder is associated with erectile dysfunction and reduced sexual quality of life in men. J Sex Med. 2008;5:2904–2910. doi: 10.1111/j.1743-6109.2008.01000.x. [DOI] [PubMed] [Google Scholar]
- 25.Rosen R., Altwein J., Boyle P. Lower urinary tract symptoms and male sexual dysfunction: The multinational survey of the aging male (MSAM-7) Eur Urol. 2003;44:637–649. doi: 10.1016/j.eururo.2003.08.015. [DOI] [PubMed] [Google Scholar]
- 26.Liao L., Chuang Y.C., Liu S.P. Effect of lower urinary tract symptoms on the quality of life and sexual function of males in China, Taiwan, and South Korea: Subgroup analysis of a cross-sectional, population-based study. Low Urin Tract Symptoms. 2019;11:O78−O84. doi: 10.1111/luts.12220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Apostolidis A., de Nunzio C., Tubaro A. What determines whether a patient with LUTS seeks treatment? ICI-RS 2011. Neurourol Urodyn. 2012;31:365–369. doi: 10.1002/nau.22212. [DOI] [PubMed] [Google Scholar]
- 28.Namiki S., Arai Y. Sexual quality of life for localized prostate cancer: A cross-cultural study between Japanese and American men. Reprod Med Biol. 2011;10:59–68. doi: 10.1007/s12522-011-0076-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Namiki S., Litwin M.S., Kwan L. Association of lower urinary tract symptoms with sexual dysfunction: A cross-cultural study between Japanese and American men with localized prostate cancer. BJU Int. 2009;104:1071–1076. doi: 10.1111/j.1464-410X.2009.08470.x. [DOI] [PubMed] [Google Scholar]
- 30.Norton J.M., Dodson J.L., Newman D.K. Nonbiologic factors that impact management in women with urinary incontinence: review of the literature and findings from a National Institute of Diabetes and Digestive and Kidney Diseases workshop. Int Urogynecol J. 2017;28:1295–1307. doi: 10.1007/s00192-017-3400-x. [DOI] [PubMed] [Google Scholar]
- 31.Velten J., Margraf J. Satisfaction guaranteed? How individual, partner, and relationship factors impact sexual satisfaction within partnerships. PLoS One. 2017;12 doi: 10.1371/journal.pone.0172855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Barbosa J.A., Muracca E., Nakano E. Interactions between lower urinary tract symptoms and cardiovascular risk factors determine distinct patterns of erectile dysfunction: A latent class analysis. J Urol. 2013;190:2177–2182. doi: 10.1016/j.juro.2013.05.048. [DOI] [PubMed] [Google Scholar]
- 33.Barry M.J., Williford W.O., Chang Y. Benign prostatic hyperplasia specific health status measures in clinical research: How much change in the American Urological Association symptom index and the benign prostatic hyperplasia impact index is perceptible to patients? J Urol. 1995;154:1770–1774. doi: 10.1016/s0022-5347(01)66780-6. [DOI] [PubMed] [Google Scholar]
- 34.Gacci M., Ficarra V., Sebastianelli A. Impact of medical treatments for male lower urinary tract symptoms due to benign prostatic hyperplasia on ejaculatory function: A systematic review and meta-analysis. J Sex Med. 2014;11:1554–1566. doi: 10.1111/jsm.12525. [DOI] [PubMed] [Google Scholar]
- 35.Giuliano F. Impact of medical treatments for benign prostatic hyperplasia on sexual function. BJU Int. 2006;97(Suppl 2):34–38. doi: 10.1111/j.1464-410X.2006.06104.x. [discussion: 44−45] [DOI] [PubMed] [Google Scholar]
- 36.Dowd J.B., Todd M. Does self-reported health bias the measurement of health inequalities in U.S. adults? Evidence using anchoring vignettes from the Health and Retirement Study. J Gerontol B Psychol Sci Soc Sci. 2011;66:478–489. doi: 10.1093/geronb/gbr050. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.