Abstract
Introduction
Women's sexual health is a vital and important part of life at any age. In particular, pregnancy and childbirth bring biological, psychological, and social changes which may influence sexual health. It has been shown that sexual function declines during pregnancy and does not return to its baseline levels during the postpartum period. Despite the complexity and significance of this subject, health providers often neglect sexual aspects during pregnancy and postpartum.
Aim
We believe that clarifying the risk factors will help open conversations and improvements in sexual function.
Methods
In this review, we focus on how postpartum sexual function is affected by mode of delivery, perineal trauma during delivery, episiotomy, and lactation.
Concclusions
We conclude that the mode of delivery has no significant effect on short- and long-term postpartum sexual function. On the other hand, 3rd and 4th degree tears are strongly associated with postpartum sexual dysfunction. We found that episiotomy does not adversely affect sexual function, and lactation has a slightly negative effect. We believe that shedding light on this topic will lead to a better understanding for pregnant and postpartum women and the obstetrician. Further studies may elucidate more useful treatment approaches.
Ola Gutzeit, Gali Levy, Lior Lowenstein. Postpartum Female Sexual Function: Risk Factors for Postpartum Sexual Dysfunction. Sex Med 2019;8:8–13.
Key Words: Postpartum, Mode of delivery, Perineal trauma, Episiotomy, Breastfeeding
Introduction
Women's sexual health is a vital and important part of life at any age and is influenced by many factors.1 In particular, pregnancy and childbirth bring biological, psychological, and social changes which may alter sexual health.2,3 There is evidence that sexual function declines during pregnancy and does not return to its baseline levels during the postpartum period. This is in part attributed to changes in body image, lack of sleep, tension, and urinary stress and urge complaints.4, 5, 6, 7 Despite the significant impact on life, women's sexual function after delivery is often neglected by health-care professionals.5 There is a significant worsening in all sexual domains postpartum, such as dyspareunia, lack of vaginal lubrication, difficulty to reach orgasm, vaginal bleeding or irritation after sex, and loss of sexual desire.6,7 Studies have shown that 89% of women resume sexual activity within 6 months of giving birth. Sexual dysfunction prevalence rates vary from 41% to 83% at 2–3 months postpartum7,8 to 64% at 6 months postpartum,5 not reaching prepregnancy levels of 38%.7 Some studies indicate that at a span of >18 months after birth, women have markedly lower levels of sexual pleasure and emotional satisfaction.9 The high prevalence of sexual disorders postpartum significantly impact quality of life.10 Impaired postpartum sexual function is extremely common, and its negative impact on quality of life emphasizes the need to understand the parameters that cause this impairment. This review will explore the effects of delivery and postpartum factors on sexual function after childbirth.
Mode of Delivery
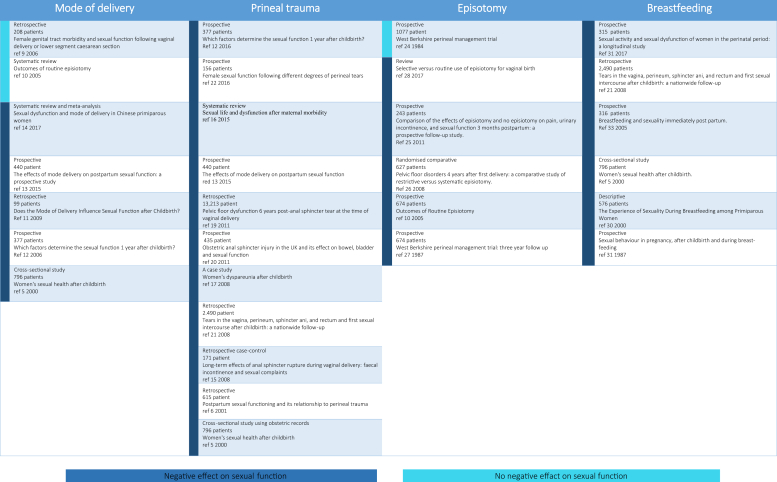
Spontaneous delivery and assisted vaginal delivery are both associated with short-term damage to the perineum and long-term changes to the pelvic floor. Many studies have attempted to answer the following question: Do these changes influence sexual function? The findings are quite controversial. A scant number of underpowered studies have shown an association between vaginal delivery and sexual dysfunction.11,12 In one of the larger studies, Griffiths et al11 assessed 208 women at 2 years after delivery, recording the prevalence of dyspareunia, subjective depression, sexual satisfaction, urinary incontinence, fecal incontinence, and incontinence of flatus. These statistics were correlated with the mode of delivery. With the help of original questionnaires relating to urinary incontinence, fecal incontinence, incontinence of flatus, dyspareunia, subjective depression, and sexual satisfaction, Griffiths et al11 demonstrated a significant decrease in sexual satisfaction scores in women who underwent vaginal delivery in comparison with those who underwent elective cesarean section at 2-year follow-up. There was also a significant increase in the prevalence of urinary incontinence, incontinence of flatus, dyspareunia, and subjective depression in women who underwent vaginal delivery in comparison with those who underwent caesarean delivery.11 Another study examined 55 primiparae who delivered vaginally and 44 who underwent elective cesarean section, assessing sexual function by a validated self-reported questionnaire, the Female Sexual Function Index (FSFI). This assessment was carried out 12 months after birth and compared between groups. The total score of the FSFI was not significantly different between the groups. The rate of patients' dyspareunia at 3 months after childbirth was higher in those who underwent vaginal delivery (45.3% vs 11.9%; P < .001).13 Barrett et al7 carried out a cross-sectional study published in 2000 that analyzed 484 women, comparing their status during the 3rd trimester just before delivery using obstetric records and their status 6 months after delivery using a postal survey. Compared with the pregnancy period, the problems of pain, lack of vaginal lubrication, and loss of sexual desire all increased significantly in the 1st 3 months after delivery; these problems declined by 6 months but not to prepregnancy levels.5 The study concluded that dyspareunia in the 1st 3 months of the postnatal period was significantly associated with assisted vaginal deliveries; however, at 6 months, there was no significant difference.7,14 A limitation of this study was that the questionnaires received only a 61% response rate, and therefore, a selection bias could not be ruled out. The authors attributed this relatively low compliance rate to the low socioeconomic status population. Another possible limitation of the study by Barrett et al7 is that it was found to have recall bias; women were asked to recall information from before their pregnancy and the early months of the postnatal period.7 van Brummen et al15 conducted a prospective study in 2006 with 377 primiparous women which illustrated that satisfaction with their sexual functioning 1 year after delivery was not related to the mode of delivery. This prospective study used the Maudsley Marital Questionnaire to assess sexual function. Dissatisfaction with a sexual relationship 1 year after childbirth was associated with not having been sexually active at 12 weeks of gestation and with older maternal age at delivery.15 Another prospective study published in 2015 included 440 women and showed decreased desire, arousal and orgasm, and increased pain at 6 months postpartum. These parameters returned to prebirth levels by 12 months.16 Finally, a meta-analysis in 2017 of Chinese primiparous women indicated that the mode of delivery did not affect short- and long-term postpartum sexual satisfaction.17 Most prospective data (Figure 1) have concluded that the mode of delivery has no significant effect on short- and long-term postpartum sexual function. Based on the accumulated data, it is possible that assisted vaginal deliveries are associated with a negative effect on sexual function; however, larger prospective studies are needed to definitively answer this question.
Figure 1.
Risk factors for female postpartum sexual dysfunction.
Perineal Trauma
Perineal tears are classified in 4 degrees: the 1st degree involves the fourchette, perineal skin, and vaginal mucous membrane. 2nd-degree tears involve the perineal muscles and skin. 3rd-degree tears extend from the vaginal wall and perineum to the anal sphincter and 4th-degree tears extend to the anus or rectum. Severe perineal trauma is defined as a 3rd-degree or 4th-degree tear. The reported rate of severe perineal trauma among vaginal deliveries is 1–3% in European countries and 2.2–19% in USA.18 A prospective study in 2006 with 377 primiparous women found that women were 5 times less likely to be sexually active after a 3rd/4th-degree anal sphincter tear compared with women with an intact perineum. A systematic review of 14 studies performed in 2015 compared women with 3rd- or 4th-degree laceration with women without major injuries.19 4 of the 14 studies found that women with 3rd- or 4th-degree laceration suffered from dyspareunia significantly, more frequently, and for longer duration. The frequency of dyspareunia with severe perineal trauma compared to 1st- and 2nd-degree tears at 3 months postpartum was 32–55% vs 51–64%, respectively. The frequency of dyspareunia with severe perineal trauma compared to 1st- and 2nd-degree tears at 6 months postpartum was 18–26% vs 26–33%,7,8,18,20 respectively. The average time to resume sexual activity when childbirth resulted in no major injuries compared with severe perineal trauma was 7.1 weeks ±3.3 vs 9.3 weeks ±3.5 (P < .001).8 No differences were seen in total FSFI mean scores postpartum at 3 days and 6 weeks, after 6 and 12 months,16,21 or after 6 years.22 The prevalence of renewal of sexual activity in women with 3rd- and/or 4th-degree tear was low at 3 months,23 6 months,16,24 and 1 year postpartum.15 A more recent prospective cohort study in 2016 assessed women with 3rd- or 4th-degree perineal tears compared with women who underwent episiotomy or had minor lacerations. This study showed that 3rd- or 4th- degree perineal tears negatively affected sexual function at 6 months and 1 year after delivery.25 Severe perineal trauma during labor is associated with diminished sexual function postpartum, with higher incidence of dyspareunia and longer time to renewal of sexual activity (Figure 1). On the other hand, 1st- and 2nd-degree tears have no significant effect on perineal pain or dyspareunia during the postpartum period.26
Episiotomy
Episiotomy is a controlled vaginal and perineal surgical cut. The American College of Obstetricians and Gynecologists states that episiotomy should be performed for maternal or fetal indications such as avoiding severe maternal lacerations or facilitating or expediting difficult deliveries.27,28 Episiotomy is one of the most commonly performed procedures worldwide. Rates of episiotomies vary from 9.7% in Sweden to as high as 100% in Taiwan.29 Hartmann et al,12 in a 2005 systematic review, concluded that routine episiotomy did not reduce sexual dysfunction.12 A trial involving selective/restrictive vs routine episiotomy reported intention-to-treat analyses of sexual outcomes: 37% of the restrictive-use group and 27% of the routine-use group had resumed sexual intercourse by 1 month after delivery (P <.01).30 A review by Hartmann et al12 determined that the proportion of women who resumed intercourse by 3 months and/or ceased to experience dyspareunia at 3 months, did not differ by group. This review concluded that no evidence suggests that sexual function is improved by episiotomy.12 A more recent prospective follow-up study in 2010 with 243 women compared vaginal delivery with or without episiotomy. This study portrayed no difference between groups in sexual function at weeks 1, 2, and 6 postpartum.31 A limited number of studies that compared routine and restrictive episiotomy outcomes reported that the frequency of dyspareunia 3 and 4 years postpartum did not differ between the groups.32,33 Fritel et al32 compared 2 French university hospitals with contrasting policies for episiotomy: one used a strictive protocol and the other, a routine protocol. The study found that 4 years after the 1st delivery, the groups did not differ in the prevalence of urinary incontinence (26% vs 32%), perineal pain (6 vs 8%), or pain during intercourse (18 vs 21%). The pitfall in this study was that the populations differed demographically between hospitals. For example, the women who gave birth in the hospital that routinely preformed episiotomies were significantly older and had a higher educational level, along with more epidurals and more instrumental and cesarean deliveries.32 In 2017, Cochrane Library published an extensive review and concluded that there is no difference in the presence or lack of episiotomy in women reporting painful sexual intercourse 6 months or longer after delivery.34 This large database review included 12 studies (6,177 women) from different populations; for example, 8 of the 12 trials included primiparous women only, and 4 trials were in both primiparous and multiparous women. The review's conclusions had only low-to-moderate certainty evidence and suggested that the trials should use better, standardized outcome assessment methods.34 In summary, studies have, to date, not defined episiotomy as a risk factor for decreased sexual function (Figure 1). However, the level of evidence is still unsatisfactory and more studies need to be carried out to confirm this finding.
Breastfeeding
Breastfeeding is strongly encouraged by pediatric and obstetric organizations.35 Its positive effect on maternal health is undebatable, but the evidence of breastfeeding's influence on maternal sexual function is limited. In addition to its psychological aspects, lactation is associated with low estrogen, progesterone, and androgen levels and high levels of prolactin. This hormonal balance may indirectly affect sexual interest by decreasing vaginal lubrication, causing vaginal atrophy, increased breast sensitivity, and decreased sexual desire.7 A descriptive, longitudinal, prospective study of 635 women concluded that there is a slightly negative correlation between physiologic aspects of breastfeeding and sexuality. Nevertheless, breastfeeding did not affect most women's sexual relationship with their partners. The women in the study demonstrated that their partner's perception attitudes toward breastfeeding and sexuality were slightly positive. On the other hand, breastfeeding mothers do not usually worry that sexual activity will harm their milk supply or their ability to nurse. This study was limited to primiparous, predominantly Caucasian women recruited in 1 hospital. Owing to these limitations, the ability to generalize findings of breastfeeding women is restricted. Despite the large sample size, the descriptive design of this study limits the significant value of these findings.36 In a longitudinal cohort study of 315 women evaluated by standardized FSFI questionnaires, it was revealed that breastfeeding as a risk factor for sexual dysfunction decreased arousal and sexual satisfaction.37 Several studies concluded that breastfeeding delayed resumption of vaginal intercourse after childbirth.24,38,39 Interestingly, a study that evaluated breastfeeding's social chemosignal concluded that natural compounds collected from lactating women and their breastfed infants increased the sexual motivation of other women, those with a partner experienced enhanced sexual desire and those without one had more sexual fantasies.40 The accumulating evidence suggests that breastfeeding has a negative effect on sexual function postpartum and delays resumption of sexual activity after birth (Figure 1).
Discussion
Sexual health is a universal part of life quality at all ages. Childbirth brings many changes that may affect the quality of life and sexual function. Sexual function declines significantly after delivery because of factors such as complications during pregnancy, different characteristics of delivery, postpartum physiological and psychological changes, postpartum depression, and many others. Culture can be a significant factor in sexual behavior postpartum: different cultures in the developing world forbid sexual intercourse for a period of time after childbirth. While modern health care provides postnatal care in most of the Western world, the absence of postnatal care in Africa, Asia, the Middle East, and Latin America allow rites and observances based on belief systems to thrive.41,42
In addition, parity has an effect on sexual function; primiparous women experience more dyspareunia than multiparous women. This may be explained by higher rates of severe perineal trauma and instrumental delivery in primiparae. Furthermore, primiparae usually feel less secure about postpartum sexual life because of their lack of experience.10 In addition, women who are not sexually active at 12 weeks of gestation and women who are older at the time of delivery have a higher rate of dissatisfaction with sexual relationship 1 year after childbirth.15
Despite the complexity and significance of this subject, health providers often neglect sexual aspects during pregnancy and postpartum. We believe that a better understanding of the risk factors will lead to more open conversation and improvement in sexual function. In this review, we focused on the effect on postpartum sexual function by mode of delivery, perineal trauma during delivery, episiotomy, and lactation.
We conclude that the mode of delivery has no significant effect on short- and long-term postpartum sexual function. It is possible that assisted vaginal deliveries are associated with a negative effect on sexual function; however, more large prospective studies are needed to answer this question. In addition, women should be more cautious to choose cesarean section to preserve sexual function.
Severe perineal trauma during delivery has long-term outcomes such as flatal and fecal incontinence and rectovaginal fistula. We conclude in this work that 3rd- and 4th-degree tears are strongly associated with postpartum sexual dysfunction. Pelvic floor muscle training is 1st-line treatment for all types of urinary incontinence and mild pelvic organ prolapses and can improve some aspects of a woman's sexual life. A systematic review in 2015 and in 201944 concluded that postpartum pelvic floor muscle training seems to improve sexual function postnatally.45 Conversely, a review in 2016 concluded that there is no evidence of long-term benefit of perineal rehabilitation and perineal massage on dyspareunia a year after delivery.46 More studies are needed to confirm whether muscle training has a beneficial effect.
Episiotomy is a commonly practiced surgery that is performed to prevent severe perineal trauma. There is a continuing debate in the professional literature over whether episiotomy has a protective effect from 3rd- and 4th-degree tears, despite the clear fact this is one of the most frequently performed procedures. The literature shows no harmful effect of episiotomy on sexual function.
An important aspect of women's life during the postpartum period is lactation. Several authors have suggested that women who choose to breastfeed might be more comfortable with their sexuality than those who choose to bottle feed.36 Lactation has a slightly negative effect on sexual function. The decline in sexual function may be due to the unique hormonal imbalance during lactation. Low estrogen levels can lead to decreased vaginal lubrication. 1 particular study investigated vaginal estrogen treatment postpartum and did not find a beneficial effect.43 Birth complications such as postpartum genital infections, postpartum hemorrhage, and obstructed labor may affect postpartum sexual function. However, there are no studies to our knowledge that address the effect of these complications on sexual live.
Based on the cumulative data presented in this review, severe perineal trauma, and lactation have a negative effect on sexual function during the postpartum period, while the mode of delivery and episiotomy do not have a significant effect on postpartum sexual function. Few studies have addressed the question of postpartum sexual dysfunction treatment.9,43,45,47 As for whether psychological treatment is an effective treatment for postpartum sexual dysfunction,48 we know of no studies that address the question of psychological treatment effectiveness during the postpartum period. This review highlights significant risk factors for postpartum sexual dysfunction and emphasizes the neglect of physicians to address the issue, as reflected in the lack of studies suggesting treatment approaches. We believe that raising this important topic will lead to more open conversation between pregnant and postpartum women and the obstetrician and that further studies will be able to recommend useful treatment approaches.
Statement of Authorship
Category 1
-
(a)Conception and Design
- Ola Gutzeit; Lior Lowenstein
-
(b)Acquisition of Data
- Ola Gutzeit; Gali Levy
-
(c)Analysis and Interpretation of Data
- Ola Gutzeit; Lior Lowenstein; Gali Levy
Category 2
-
(a)Drafting the Article
- Ola Gutzeit; Gali Levy
-
(b)Revising It for Intellectual Content
- Lior Lowenstein
Category 3
-
(a)Final Approval of the Completed Article
- Lior Lowenstein
Footnotes
Conflict of Interest: The authors report no conflicts of interest.
Funding: None.
References
- 1.World Health Organization . World Health Organization; Geneva, Switzerland: 2006. Defining sexual health: report of technical consultation on sexual health, 28-31 January 2002; p. 35. [Google Scholar]
- 2.Norhayati M.N., Azman Yacob M. Long-term postpartum effect of severe maternal morbidity on sexual function. Int J Psychiatry Med. 2017;52:328–344. doi: 10.1177/0091217417738933. [DOI] [PubMed] [Google Scholar]
- 3.Serati M., Salvatore S., Siesto G. Female sexual function during pregnancy and after childbirth. J Sex Med. 2010;7:2782–2790. doi: 10.1111/j.1743-6109.2010.01893.x. [DOI] [PubMed] [Google Scholar]
- 4.Pauls R.N., Occhino J.A., Dryfhout V.L. Effects of pregnancy on female sexual function and body image: A prospective study. J Sex Med. 2008;5:1915–1922. doi: 10.1111/j.1743-6109.2008.00884.x. [DOI] [PubMed] [Google Scholar]
- 5.Glazener C.M.A. Sexual function after childbirth: Women's experiences, persistent morbidity and lack of professional recognition. BJOG An Int J Obstet Gynaecol. 1997;104:330–335. doi: 10.1111/j.1471-0528.1997.tb11463.x. [DOI] [PubMed] [Google Scholar]
- 6.Rosen N.O., Pukall C. Comparing the prevalence, risk factors, and repercussions of postpartum Genito-pelvic pain and dyspareunia. Sex Med Rev. 2016;4:126–135. doi: 10.1016/j.sxmr.2015.12.003. [DOI] [PubMed] [Google Scholar]
- 7.Barrett G., Pendry E., Peacock J. Women's sexual health after childbirth. BJOG An Int J Obstet Gynaecol. 2000;107:186–195. doi: 10.1111/j.1471-0528.2000.tb11689.x. [DOI] [PubMed] [Google Scholar]
- 8.Signorello L.B., Harlow B.L., Chekos A.K. Postpartum sexual functioning and its relationship to perineal trauma: A retrospective cohort study of primiparous women. Am J Obstet Gynecol. 2001;184:881–890. doi: 10.1067/mob.2001.113855. [DOI] [PubMed] [Google Scholar]
- 9.McDonald E., Woolhouse H., Brown S.J. Sexual pleasure and emotional satisfaction in the first 18 months after childbirth. Midwifery. 2017;55:60–66. doi: 10.1016/j.midw.2017.09.002. [DOI] [PubMed] [Google Scholar]
- 10.Lagaert L., Weyers S., Van Kerrebroeck H. Postpartum dyspareunia and sexual functioning: A prospective cohort study. Eur J Contracept Reprod Heal Care. 2017;22:200–206. doi: 10.1080/13625187.2017.1315938. [DOI] [PubMed] [Google Scholar]
- 11.Griffiths A., Watermeyer S., Sidhu K. Female genital tract morbidity and sexual function following vaginal delivery or lower segment caesarean section. J Obstet Gynaecol (Lahore) 2006;26:645–649. doi: 10.1080/01443610600903701. [DOI] [PubMed] [Google Scholar]
- 12.Hartmann K., Viswanathan M., Palmieri R. Outcomes of routine episiotomy: A systematic review. J Am Med Assoc. 2005;293:2141–2148. doi: 10.1001/jama.293.17.2141. [DOI] [PubMed] [Google Scholar]
- 13.Klein K., Worda C., Leipold H. Does the mode of delivery influence sexual function after childbirth? J Women's Heal. 2009;18:1227–1231. doi: 10.1089/jwh.2008.1198. [DOI] [PubMed] [Google Scholar]
- 14.Galbally M., Watson S.J., Permezel M. Depression across pregnancy and the postpartum, antidepressant use and the association with female sexual function. Psychol Med. 2019;49:1490–1499. doi: 10.1017/S0033291718002040. [DOI] [PubMed] [Google Scholar]
- 15.Van Brummen H.J., Bruinse H.W., Van De Pol G. Which factors determine the sexual function 1 year after childbirth? BJOG An Int J Obstet Gynaecol. 2006;113:914–918. doi: 10.1111/j.1471-0528.2006.01017.x. [DOI] [PubMed] [Google Scholar]
- 16.De Souza A., Dwyer P.L., Charity M. The effects of mode delivery on postpartum sexual function: A prospective study. BJOG An Int J Obstet Gynaecol. 2015;122:1410–1418. doi: 10.1111/1471-0528.13331. [DOI] [PubMed] [Google Scholar]
- 17.Fan D., Li S., Wang W. Sexual dysfunction and mode of delivery in Chinese primiparous women: A systematic review and meta-analysis. BMC Pregnancy Childbirth. 2017;17:408. doi: 10.1186/s12884-017-1583-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mous M., Muller S.A., De Leeuw J.W. Long-term effects of anal sphincter rupture during vaginal delivery: Faecal incontinence and sexual complaints. BJOG An Int J Obstet Gynaecol. 2008;115:234–238. doi: 10.1111/j.1471-0528.2007.01502.x. [DOI] [PubMed] [Google Scholar]
- 19.Andreucci C.B., Bussadori J.C., Pacagnella R.C. Sexual life and dysfunction after maternal morbidity: A systematic review. BMC Pregnancy Childbirth. 2015;15:307. doi: 10.1186/s12884-015-0742-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Solana-Arellano E., Villegas-Arrizon A., Legorreta-Soberanis J. Women's dyspareunia after childbirth: a case study in a hospital in Acapulco, MexicoRev Panam Salud Publica. 2008;23:44–51. doi: 10.1590/s1020-49892008000100006. [DOI] [PubMed] [Google Scholar]
- 21.Chang S.R., Chang T.C., Chen K.H. Sexual function in women 3 days and 6 weeks after childbirth: A prospective longitudinal study using the Taiwan version of the female sexual function index. J Sex Med. 2010;7:3946–3956. doi: 10.1111/j.1743-6109.2010.01752.x. [DOI] [PubMed] [Google Scholar]
- 22.Baud D., Meyer S., Vial Y. Pelvic floor dysfunction 6 years post-anal sphincter tear at the time of vaginal delivery. Int Urogynecol J. 2011;22:1127–1134. doi: 10.1007/s00192-011-1431-2. [DOI] [PubMed] [Google Scholar]
- 23.Marsh F., Lynne R., Christine L. Obstetric anal sphincter injury in the UK and its effect on bowel, bladder and sexual function. Eur J Obstet Gynecol Reprod Biol. 2011;154:223–227. doi: 10.1016/j.ejogrb.2010.09.006. [DOI] [PubMed] [Google Scholar]
- 24.Rådestad I., Olsson A., Nissen E. Tears in the vagina, perineum, sphincter ani, and rectum and first sexual intercourse after childbirth: A nationwide follow-up. Birth. 2008;35:98–106. doi: 10.1111/j.1523-536X.2008.00222.x. [DOI] [PubMed] [Google Scholar]
- 25.Ali W., Ahmed S., Kishk E.A. Female sexual function following different degrees of perineal tears. Int Urogynecol J. 2016;28:917–921. doi: 10.1007/s00192-016-3210-6. [DOI] [PubMed] [Google Scholar]
- 26.Manresa M., Pereda A., Bataller E. Incidence of perineal pain and dyspareunia following spontaneous vaginal birth: A systematic review and meta-analysis. Int Urogynecol J. 2019;30:1–16. doi: 10.1007/s00192-019-03894-0. [DOI] [PubMed] [Google Scholar]
- 27.Sagi-Dain L., Sagi S. Indications for episiotomy performance-a cross-sectional survey and review of the literature. J Obstet Gynaecol (Lahore) 2016;36:361–365. doi: 10.3109/01443615.2015.1065233. [DOI] [PubMed] [Google Scholar]
- 28.Corrêa Junior M., Passini Júnior R. Selective episiotomy: Indications, techinique, and association with severe perineal lacerations. Rev Bras Ginecol Obstet. 2016;38:301–307. doi: 10.1055/s-0036-1584942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Graham I.D., Carroli G., Davies C. Episiotomy rates around the world: An update. Birth. 2005;32:219–223. doi: 10.1111/j.0730-7659.2005.00373.x. [DOI] [PubMed] [Google Scholar]
- 30.Sleep J., Grant A., Garcia J. West Berkshire perineal management trial. Br Med J (Clin Res Ed) 1984;289:587–590. doi: 10.1136/bmj.289.6445.587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chen K.-H., Lin H.-H., Lai Y.-H. Comparison of the effects of episiotomy and no episiotomy on pain, urinary incontinence, and sexual function 3 months postpartum: A prospective follow-up study. Int J Nurs Stud. 2010;48:409–418. doi: 10.1016/j.ijnurstu.2010.07.017. [DOI] [PubMed] [Google Scholar]
- 32.Fritel X., Schaal J.P., Fauconnier A. Pelvic floor disorders 4 years after first delivery: A comparative study of restrictive versus systematic episiotomy. BJOG An Int J Obstet Gynaecol. 2008;115:247–252. doi: 10.1111/j.1471-0528.2007.01540.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sleep J., Grant A. West Berkshire perineal management trial: three year follow up. Br Med J (Clin Res Ed) 1987;295:749–751. doi: 10.1136/bmj.295.6601.749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jiang H., Qian X., Carroli G. Selective versus routine use of episiotomy for vaginal birth. Cochrane Database Syst Rev. 2017;2:CD000081. doi: 10.1002/14651858.CD000081.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kramer M.S., Kakuma R. The optimal duration of exclusive breastfeeding. Cochrane Database Syst Rev. 2013;8:63–77. [Google Scholar]
- 36.Avery M.D., Duckett L., Frantzich C.R. The experience of sexuality during breastfeeding among primiparous women. J Midwifery Women's Heal. 2000;45:227–237. doi: 10.1016/s1526-9523(00)00020-9. [DOI] [PubMed] [Google Scholar]
- 37.Wallwiener S., Müller M., Doster A. Sexual activity and sexual dysfunction of women in the perinatal period: A longitudinal study. Arch Gynecol Obstet. 2017;295:873–883. doi: 10.1007/s00404-017-4305-0. [DOI] [PubMed] [Google Scholar]
- 38.Alder E.M. 7 Sexual behaviour in pregnancy, after childbirth and during breast-feeding. Baillieres Clin Obstet Gynaecol. 1989;3:805–821. doi: 10.1016/s0950-3552(89)80066-5. [DOI] [PubMed] [Google Scholar]
- 39.Rowland M., Foxcroft L., Hopman W.M. Breastfeeding and sexuality immediately post partum. Can Fam Physician. 2005;51:1366–1367. [PMC free article] [PubMed] [Google Scholar]
- 40.Spencer N.A., McClintock M.K., Sellergren S.A. Social chemosignals from breastfeeding women increase sexual motivation. Horm Behav. 2004;46:362–370. doi: 10.1016/j.yhbeh.2004.06.002. [DOI] [PubMed] [Google Scholar]
- 41.Feyisetan B.J. Postpartum sexual abstinence, breastfeeding, and childspacing, among Yoruba women in urban Nigeria. Soc Biol. 1990;37:110–127. doi: 10.1080/19485565.1990.9988751. [DOI] [PubMed] [Google Scholar]
- 42.Zulu E.M. Ethnic variations in observance and rationale for postpartum sexual Abstinence in Malawi. Demography. 2001;38:467–479. doi: 10.1353/dem.2001.0042. [DOI] [PubMed] [Google Scholar]
- 43. NCT03493126 Vaginal estrogen on postpartum atrophy, perineal pain, and sexual function. https://clinicaltrials.gov/show/nct03493126https://doi.org/10.1002/CENTRAL/CN-01567938 Available at: Accessed December 5, 2019. [DOI] [PMC free article] [PubMed]
- 44.Sobhgol S.S., Priddis H., Smith C.A. The effect of pelvic floor muscle exercise on female sexual function during pregnancy and postpartum: A systematic review. Sex Med Rev. 2019;7:13–28. doi: 10.1016/j.sxmr.2018.08.002. [DOI] [PubMed] [Google Scholar]
- 45.Ferreira C.H.J., Dwyer P.L., Davidson M. Does pelvic floor muscle training improve female sexual function? A systematic review. Int Urogynecol J. 2015;26:1735–1750. doi: 10.1007/s00192-015-2749-y. [DOI] [PubMed] [Google Scholar]
- 46.Battut A., Nizard J. Impact of pelvic floor muscle training on prevention of perineal pain and dyspareunia in postpartumProg Urol. 2016;26:237–244. doi: 10.1016/j.purol.2015.09.006. [DOI] [PubMed] [Google Scholar]
- 47.Hay-Smith J. Therapeutic ultrasound for postpartum perineal pain and dyspareunia. Cochrane Database Syst Rev. 2009;2:CD000495. doi: 10.1002/14651858.CD000495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Flanagan E., Herron K.A., O'Driscoll C. Psychological treatment for vaginal pain: Does etiology matter? A systematic review and meta-Analysis. J Sex Med. 2015;12:3–16. doi: 10.1111/jsm.12717. [DOI] [PubMed] [Google Scholar]