Abstract
Anemia is a significant public health problem during pregnancy and its prevalence varies in different cohorts. Correct identification of this problem in a given population is important for implementation of various health schemes. This study was carried out at a tertiary care hospital in Haryana. The prevalence of anemia in females at the time pregnancy diagnosis during first trimester was studied. The study period was January 2018 to June 2019. Severity of anemia was categorized as mild (hemoglobin 10–10.9 gm/dl), moderate (hemoglobin 7–9.9 gm/dl) and severe (hemoglobin < 7 gm/dl) as per the WHO definition. Relevant review of literature on prevalence of anemia in pregnancy in different Indian states was done. The median age of 388 females with diagnosis of pregnancy during first trimester was 27 years. Mean hemoglobin concentration was 10.47 gm/dl. 264 (68%) females had anemia. Out of these 191 (72.3%) had mild anemia, 65 (24.6%) had moderate anemia and eight had severe anemia. Out of the total study population, 270 (69.58%) were from rural and 118 (30.41%) were from urban background. Among the anemic pregnant females, 179 (67.8%) belonged to rural areas and 85 (32.20%) belonged to urban areas. Out of 264 patients with anemia, 87 (32.95%) patients were primigravida and 177 (67.04%) were multiparous females. The results of literature review showed a high prevalence of anemia in the other Indian states also. There is high prevalence of anemia in females at the time of diagnosis of pregnancy. Rates of anemia are higher in females with higher parity.
Keywords: Anemia, Pregnancy, Haryana, First trimester
Introduction
Anemia is a significant public health problem all around the globe [1]. The prevalence of anemia in pregnancy varies in different series from various parts of the world. According to WHO estimates, 35–75% (average 56%) pregnant females in developing countries suffer from anemia [2]. The worldwide prevalence of anemia during pregnancy was estimated to be 38% in the Nutrition Impact Model Study’s 2011 estimates [3]. There is increased risk of maternal and perinatal mortality with anemia during pregnancy [4, 5]. Anemia during pregnancy is also associated with higher risk of low birth weight and small for date babies [6, 7]. There is decreased mental and physical potential of children born to mothers with anemia [8, 9]. The most common cause of anemia in pregnancy is iron deficiency with other causes being less frequent [3]. This is the reason that hemoglobin concentration is used as a surrogate marker of iron deficiency due to its low cost and ease of determination [10]. This health problem is widely prevalent in India [9]. There are many government public health programs like National Rural Health mission (NRHM) and Integrated Child Development Scheme (ICDS) trying to tackle anemia during pregnancy [11]. Iron and folic acid supplementation during pregnancy is an effective way of tackling a large part of this problem. All pregnant females are mandated to take iron folic acid tablets made up of 0.5 mg folic acid and 100 mg elemental iron by government of India, and females receive 100 such tablets under this program [11]. However, the true success of these programs would depend upon identification of the burden of this problem in different regions of India. With this background, the present study was planned to assess the prevalence of anemia at the time of diagnosis of pregnancy during first trimester in a rural hospital in Haryana.
Materials and Methods
Setting
Tertiary care teaching Hospital in Haryana.
Study Duration
January 2018 to June 2019.
Methodology
This was a retrospective study of all females diagnosed to have pregnancy during first trimester. The list of such patients was obtained from the electronic medical records of the hospital. The clinical details were noted from the antenatal register of the department and were entered in a predesigned proforma.
The age at diagnosis of pregnancy, parity, education status, rural or urban background and the value of hemoglobin (gram/deciliter) were noted. For the purpose of this study, the anemia was defined as any hemoglobin (Hb) value less than 11 g/deciliter (gm/dl). Anemia was further subclassified as mild (Hb = 10–10.9 gm/dl), Moderate (Hb = 7–9.9 gm/dl) and severe (Hb ≤ 7 gm/dl). This is according to the WHO classification of severity of anemia [1]. The parity was noted either as primigravida or multiparous. The literary status was based upon the ability to read and write. The estimation of hemoglobin at our hospital is done by cyanmethhemoglobin method by photoelectric colorimeter.
A detailed review of anemia in pregnancy was done. A PubMed search was carried out with the keywords ‘anemia’ and ‘pregnancy’ and ‘India’ and ‘prevalence’ and ‘first trimester’. This search did not yield any studies with relevant details, and then the scope of search was widened by excluding the keyword ‘first trimester’. All the original research articles having details of prevalence of anemia during pregnancy were studied. To make the search complete, a hand-picked google search was done from all the studies which had been cited in the PubMed studies but were not available on PubMed. One study with highest subject numbers from each state was taken for final comparison.
This study was carried out in accordance with the ethical standards of the institutional and/national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Results
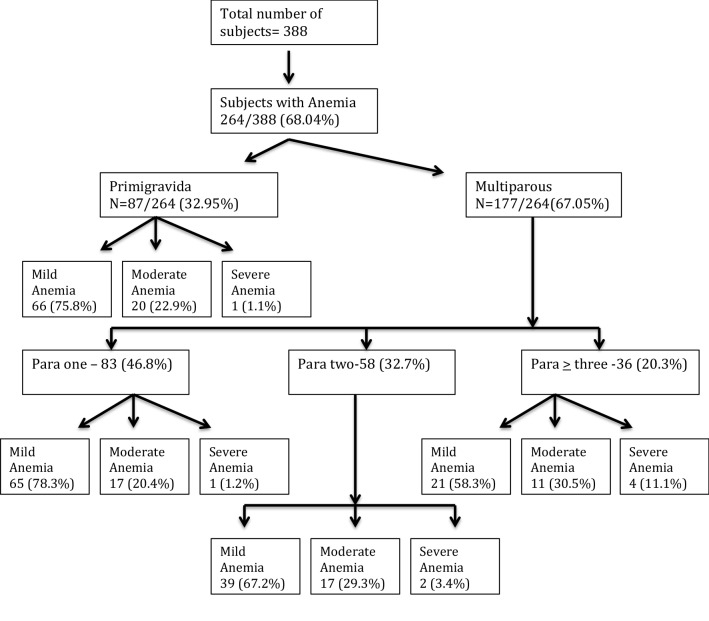
388 females with diagnosis of pregnancy during first trimester were identified during the study period. The median age of the study group was 27 years. Mean hemoglobin concentration was 10.47 gm/dl. 264 (68%) patients were detected to have anemia as per WHO definition of anemia. Out of these 191 (72.3%) had mild anemia, 65 (24.6%) had moderate anemia and eight had severe anemia. The demographic details of the patients are given in Table 1. The distribution of anemia in different age groups is shown in Table 2. Out of the total study population, 270 (69.58%) were from rural and 118 (30.41%) were from urban background. 334 (87.1%) pregnant females were literate and 54 (13.9%) were illiterate. 222 (66.46%) literate patients had anemia out of which 173 (77.93%) had mild, 48 (21.6%) had moderate and one (0.45%) had severe anemia. Amongst 54 illiterate pregnant females, anemia was detected in 42, out of which 18 (33.3%) had mild, 17 (31.48%) had moderate and seven (12.96%) had severe anemia. Among the anemic pregnant females, 179 (67.8%) belonged to rural areas and 85 (32.20%) belonged to urban areas. Total 264 pregnant females were detected to have anemia out of which 87 (32.95%) were primigravida and 177 (67.04%) multiparous. The association of anemia with parity is shown in Fig. 1. Out of 177 multiparous females, higher prevalence of anemia was observed with increasing parity. Among multiparous females, 94 (53.10%) cases were para 2 or more. Mild anemia was found in 66 primigravida females and 125 multigravida females. 20 primigravida had moderate anemia and 45 multipara had moderate anemia. Out of eight cases of severe anemia, four patients had parity of three or more. The results of literature review on the prevalence of anemia during pregnancy as per the search strategy are given in Table 3.
Table 1.
Sociodemographic details of the females at the time of pregnancy diagnosis
| Number of pregnant females | Percentage (%) | |
|---|---|---|
| Age (years) | ||
| < 20 | 1 | 0.26 |
| 20–24 | 108 | 27.83 |
| 25–29 | 191 | 49.23 |
| ≥ 30 | 88 | 22.68 |
| Median age (years) | 27 | |
| Parity | ||
| 0 | 160 | 41.23 |
| 1 | 110 | 28.35 |
| 2 | 70 | 18.04 |
| ≥ 3 | 48 | 12.38 |
| Literacy status | ||
| Literate | 334 | 86.08 |
| Illiterate | 54 | 13.92 |
| Occupation | ||
| Home maker | 236 | 60.82 |
| Labourer | 97 | 25 |
| Service/job | 39 | 13.54 |
| Others | 16 | 4.12 |
| Rural/urban | ||
| Rural | 270 | 69.58 |
| Urban | 118 | 30.41 |
| Dietary habits | ||
| Vegetarian | 240 | 61.85 |
| Non vegetarian | 148 | 31.14 |
Table 2.
Agewise distribution of degree of anemia
| Age (years) | Normal Hb (No./%) | Mild anemia (No./%) | Moderate anemia (No./%) | Severe anemia (No./%) | Total |
|---|---|---|---|---|---|
| < 20 | 0 | 0 | 1 | 0 | 1 (0.26%) |
| 20–24 | 40 (32.26%) | 49 (25.65%) | 19 (29.23%) | 0 | 108 (27.83%) |
| 25–29 | 68 (54.84%) | 104 (54.45%) | 16 (24.62) | 3 (37.5%) | 191 (49.23%) |
| > 30 | 16 (12.9%) | 38 (19.89%) | 29 (44.62%) | 5 (62.5%) | 88 (22.68%) |
| Total | 124 | 191 | 65 | 8 | 388 |
Hb Hemoglobin
Fig. 1.
Distribution of anemia with parity
Table 3.
Prevalence of anaemia during pregnancy at different periods of gestation
| Study | State | Number of subjects | Prevalence (%) | Period of gestation | |
|---|---|---|---|---|---|
| 1. | Patel et al. [12] | Maharashtra | 72,750 | 91 | NA |
| 2. | Suryanarayana et al. [13] | Karnataka | 427 | 58.6 | < 20 weeks |
| 58.89 | > 20 weeks | ||||
| 3. | Mehrotra et al. [14] | Andaman and Nicobar Islands | 786 | 50.9 | NA |
| 4. | Nair et al. [15] | Assam | 1007 | 64.64 | > 20 weeks |
| 5. | Rajaratnam et al. [16] | Tamil Nadu | 895 | 69.3 | |
| 6. | Mangla et al. [17] | Haryana | 850 | 98 | NA |
| 7. | Bisoi et al. [18] | West Bengal | 193 | 59.5 | First trimester |
| 67.9 | Second trimester | ||||
| 77.4 | Third trimester | ||||
| 8. | Singh et al. [19] | Uttaranchal | 200 | 65.5 | NA |
| 9. | Mahashabde et al. [20] | Madhya Pradesh | 300 | 63 | NA |
| 10. | Singh et al. [21] | Uttar Pradesh | 300 | 58.3 | NA |
| 11. | Vemulapalli et al. [22] | Andhra Pradesh | 986 | 99.96 | First trimester |
| 99.99 | Second trimester | ||||
| 99.99 | Third trimester |
NA Not available
Discussion
Anemia or low hemoglobin concentration is widely prevalent during pregnancy [3]. Anemia during pregnancy not only affects the health of the mother but also impacts the health of the fetus. The association of anemia during pregnancy with adverse maternal and fetal outcomes is well established [6–10]. The results of the present study are largely in line with the other reports of anemia during pregnancy. The overall prevalence of anemia during pregnancy in our study was 68.04%, which is similar to that reported from other parts of India and other developing countries. The results of prevalence reported from various states have been shown in Table 3. Our study was done at a teaching hospital in Haryana. In another study from Gohana, Haryana, a very high prevalence of anemia in 98% pregnant females was reported with 41.7% having mild anemia, 37.05% having moderate anemia and 15.8% having severe anemia [17]. In the National Family Health Survey 2005–2006 (NFHS- 3), the prevalence of anemia in Haryana was second amongst the various Indian states, though the prevalence reported in NHFS-2 was 55%. In another multicentric study done in seven states, the prevalence of anemia was found to be highest in Orissa (97%), followed by Madhya Pradesh (96.8%), Assam (93.9%), Haryana (91%), followed by Himachal Pradesh (68%) and Kerala (57.8%) [23]. In an ICMR study of 4181 pregnant women from 11 states in rural India done in 1989, the prevalence of anemia was 87.6% [24]. The differences across various states and even in the same state may not only be due to economical, ethnic and resource differences but also due to sampling bias and method of hemoglobin detection.
The high prevalence of anemia in pregnancy seems to be due to multitude of factors like low socioeconomic status, poverty, poor access to health in rural areas, limited availability of adequate food and nutrition, lack of education and gender discrimination may be playing a role in our patriarchal society. Education is an important key factor for health related issues. Prevalence of anemia is higher in women who are not educated [25]. 86% females in our study were literate. But we have to understand that literate only meant those who could read or write and the details of formal education were not noted. It is also well recognized that in developing countries problem of anemia during pregnancy is compounded by early onset of childbearing and high number of births [26]. We also observed that the prevalence was higher in females with higher parity.
The identification of magnitude of problem in a given population will not only be helpful in implementation of various public health intervention programs but also measuring their outcomes over a period of time. Government of India under various national programmes aims to reduce prevalence of anemia. One of the goals of the 12th five year plan (2012–2017) was to reduce anemia in girls and women of reproductive age group by 50%. Recently launched program in 2018 I-NIPI (Intensified national iron plus initiative) of anemia mukt bharat campaign under POSHAN(PM’s overarching scheme for holistic nourishment) and Iron plus intiative started by Government of India in 2013 recommends prophylaxis of iron and folic acid among adolescents, pregnant female and females of reproductive age group. Hemoglobin estimates in most of the studies has been done by cyanmethaemoglobin method, whereas the NFHS-2 data using hemocue system reported lower prevalence of 49.7% in pregnant women [27, 28]. There is enormous burden of anemia in Indian population including pregnant women and this study reiterates the same [29]. The management of anemia as per various recommendations will only be successful if we address these issues [30]. The limitations of the study were retrospective study design, recruitment bias from a single tertiary care center, estimation of hemoglobin by cyanmethaemoblobin method and inability to study the attributable causes of anemia due to the study design.
The present study highlights high prevalence of anaemia in females at the time of diagnosis of pregnancy during first trimester. There is thus a huge unmet need to make the various government programs reach the end users at the grassroot level. Increased active participation and empowerment of ASHA workers, anganwadi workers, various continuous education programs along with education of the masses might help in reducing these startling numbers of this seemingly easily manageable yet challenging public health problem. This will not only affect the present but also the future of not only the region but also the nation. This is not only a matter of touching one but two lives.
Conclusion
There was high prevalence of anemia in females at the time of diagnosis of pregnancy at first trimester. This was more frequent in multiparous females and illiterate population had more moderate to severe anemia.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.World Health Organization (2011) Hemoglobin concentration for the diagnosis of anemia and assessment of severity. https://www.who.int/vmnis/indicators/haemoglobin.pdf
- 2.World Health Organization . The prevalence of anaemia in women: a tabulation of available information. 2. Geneva: World Health Organization; 1992. [Google Scholar]
- 3.Stevens G, Finucane M, De-Regil L, Paciorek C, Flaxman S, Branca F, et al. Global, regional, and national trends in total and severe anaemia prevalence in children and pregnant and non-pregnant women. Lancet Global Health. 2013;1:e16–e25. doi: 10.1016/S2214-109X(13)70001-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stoltzfus RJ, Mullany L, Black RE. Iron deficiency anaemia. In: Ezzati M, Lopez AD, Rodgers A, Murray CJL, editors. Comparative quantification of health risks: global and regional burden of disease attributable to selected major risk factors. Geneva: World Health Organization; 2004. pp. 163–210. [Google Scholar]
- 5.Zhang Q, Ananth CV, Rhoads GG, Li Z. The impact of maternal anemia on perinatal mortality: a population-based, prospective cohort study in China. Ann Epidemiol. 2009;19:793–799. doi: 10.1016/j.annepidem.2009.06.002. [DOI] [PubMed] [Google Scholar]
- 6.Kozuki N, Lee AC, Katz J. Moderate to severe, but not mild, maternal anemia is associated with increased risk of small-for-gestational-age outcomes. J Nutr. 2012;142:358–362. doi: 10.3945/jn.111.149237. [DOI] [PubMed] [Google Scholar]
- 7.Steer PJ. Maternal hemoglobin concentration and birth weight. Am J Clin Nutr. 2000;71:1285S–1287S. doi: 10.1093/ajcn/71.5.1285s. [DOI] [PubMed] [Google Scholar]
- 8.Roy K, Baruah J, Kumar S, Malhotra N, Deorari AK, Sharma JB. Maternal antenatal profile and immediate neonatal outcome in VLBW and ELBW babies. Indian J Pediatr. 2006;73:669–673. doi: 10.1007/BF02898441. [DOI] [PubMed] [Google Scholar]
- 9.Singla P, Tyagi M, Kumar A, Dash D, Shankar R. Fetal growth in maternal anaemia. J Trop Pediatr. 1997;43:89–92. doi: 10.1093/tropej/43.2.89. [DOI] [PubMed] [Google Scholar]
- 10.Haider BA, Olofin I, Wang M, Spiegelman D, Ezzati M, Fawzi WW, Nutrition Impact Model Study Group (anaemia) Anaemia, prenatal iron use, and risk of adverse pregnancy outcomes: systematic review and meta-analysis. BMJ. 2013;346:f3443. doi: 10.1136/bmj.f3443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ministry of Health and Family Welfare (2013) Weekly iron and folic acid supplementation programme. http://www.mohfw.nic.in/NRHM/AH/WIFS.htm. Accessed January 10, 2013
- 12.Patel A, Prakash AA, Das PK, Gupta S, Pusdekar YV, Hibberd PL. Maternal anemia and underweight as determinants of pregnancy outcomes: cohort study in eastern rural Maharashtra, India. BMJ Open. 2018;8(8):e021623. doi: 10.1136/bmjopen-2018-021623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Suryanarayana R, Chandrappa M, Santhuram AN, Prathima S, Sheela SR. Prospective study on prevalence of anemia of pregnant women and its outcome: a community based study. J Family Med Prim Care. 2017;6:739–743. doi: 10.4103/jfmpc.jfmpc_33_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mehrotra M, Yadav S, Deshpande A, Mehrotra H. A study of the prevalence of anemia and associated sociodemographic factors in pregnant women in Port Blair, Andaman and Nicobar Islands. J Family Med Prim Care. 2018;7:1288–1293. doi: 10.4103/jfmpc.jfmpc_139_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nair M, Choudhury MK, Choudhury SS, et al. Association between maternal anaemia and pregnancy outcomes: a cohort study in Assam, India. BMJ Glob Health. 2016;1(1):000026. doi: 10.1136/bmjgh-2015-000026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rajaratnam J, Abel R, Ganesan C, Jayaseelan SA. Maternal anaemia: a persistent problem in rural Tamil Nadu. Natl Med J India. 2000;13:242–245. [PubMed] [Google Scholar]
- 17.Mangla M, Singla D. Prevalence of anaemia among pregnant women in rural India: a longitudinal observational study. Int J Reprod Contracept Obstet Gynecol. 2016;5:3500–3505. doi: 10.18203/2320-1770.ijrcog20163431. [DOI] [Google Scholar]
- 18.Bisoi S, Haldar D, Majumdar TK, et al. Correlates of anemia among pregnant women in rural area of West Bengal. J Fam Welf. 2011;57:72–78. [Google Scholar]
- 19.Singh AB, Kandpal SD, Chandra R, Srivastava VK, Negi KS. Anemia amoght pregnant and lactating women in district Dehradun. Ind J Prev Soc Med. 2009;40:19–22. [Google Scholar]
- 20.Mahashabde P, Arora VK, Sharma S, Shahjada A, Dabhi HM. Prevalence of anaemia and its socio-demographic determinants in pregnant women: a cross-sectional study in tertiary health care setup in central India. Natl J Commun Med. 2014;5:126–130. [Google Scholar]
- 21.Singh P, Chaudhary V. Prevalence of anaemia and its socio demographic determinants among pregnant women in Bareilly district, Uttar Pradesh. Indian J Commun Health. 2014;26:348–352. [Google Scholar]
- 22.Vemulapalli B, Rao K. Prevalence of anaemia among pregnant women of rural community in Vizianagaram, North Coastal Andhra Pradesh, India. Asian J Med Sci. 2013;5:21–25. doi: 10.3126/ajms.v5i2.5295. [DOI] [Google Scholar]
- 23.Agarwal KN, Agarwal DK, Sharma A, Sharma K, Prasad K, Kalita MC, et al. Prevalence of anaemia in pregnant and lactating women in India. Indian J Med Res. 2006;124:173–184. [PubMed] [Google Scholar]
- 24.ICMR Task Force Study . CMR evaluation of the national nutritional anemia prophylaxis programme. New Delhi: Indian Council of Medical Research; 1989. [Google Scholar]
- 25.Balarajan Y, Ramakrishnan U, Ozaltin E, Shankar AH, Subramanian SV. Anemia in low-income and middle-income countries. Lancet. 2011;378:2123–2135. doi: 10.1016/S0140-6736(10)62304-5. [DOI] [PubMed] [Google Scholar]
- 26.Kalaivani K. Prevalence and consequences of anaemia in pregnancy. Indian J Med Res. 2009;130:627–633. [PubMed] [Google Scholar]
- 27.Crosby WH, Munn JG, Furth ED. Cyanmethaemoglobin method for estimation of hemoglobin. US Armed Forces Med J. 1964;5:693–697. [Google Scholar]
- 28.NFHS . India 1998-99–National Family Health Survey-2 NFHS-2–anemia among women and children. Mumbai: International Institute for Population Sciences; 2002. p. 2000. [Google Scholar]
- 29.Malhotra P, Kumari S, Kumar R, et al. Prevalence of anemia in adult rural population of North India. J Assoc Phys India. 2004;52:18–20. [PubMed] [Google Scholar]
- 30.Tandon R, Jain A, Malhotra P. Management of iron deficiency anemia in pregnancy in India. Indian J Hematol Blood Transfus. 2018;34:204–215. doi: 10.1007/s12288-018-0949-6. [DOI] [PMC free article] [PubMed] [Google Scholar]