Abstract
Background
The WHO estimates a global shortage of 2.8 million physicians, with severe deficiencies especially in low and middle-income countries (LMIC). The unequitable distribution of physicians worldwide is further exacerbated by the migration of physicians from LMICs to high-income countries (HIC). This large-scale migration has numerous economic consequences which include increased mortality associated with inadequate physician supply in LMICs.
Methods
We estimate the economic cost for LMICs due to excess mortality associated with physician migration. To do so, we use the concept of a value of statistical life and marginal mortality benefit provided by physicians. Uncertainty of our estimates is evaluated with Monte Carlo analysis.
Results
We estimate that LMICs lose US$15.86 billion (95% CI $3.4 to $38.2) annually due to physician migration to HICs. The greatest total costs are incurred by India, Nigeria, Pakistan and South Africa. When these costs are considered as a per cent of gross national income, the cost is greatest in the WHO African region and in low-income countries.
Conclusion
The movement of physicians from lower to higher income settings has substantial economic consequences. These are not simply the result of the movement of human capital, but also due to excess mortality associated with loss of physicians. Valuing these costs can inform international and domestic policy discussions that are meant to address this issue.
Keywords: health economics, epidemiology, health policies and all other topics, medical demography
Key questions.
What is already known?
Previous studies attempting to estimate the economic value lost when physicians emigrate from low and middle-income countries were specific to the African continent, and only calculate cost of emigration by quantifying the cost of educating a physician.
What are the new findings?
We expand the concept of economic losses due to physician migration by also incorporating mortality benefits that would have been realised had the physicians stayed in their country of origin.
We expand the scope of the estimates to include nearly all low and middle-income countries.
What do the new findings imply?
The large-scale migration of physicians from poor to rich countries results in a US$16 billion annual cost associated with excess mortality in low and middle-income countries.
These data may inform low and middle-income country policies on expenditure for physician retention, high-income country policies on physician recruitment and foreign aid, and international trade negotiations.
Introduction
In 2012, the New York Times magazine published a provocatively titled piece: ‘America is stealing the world’s doctors’.1 The article featured the story of a Zambian doctor who left his country in pursuit of a career in the USA. The story described how physician brain drain—the migration of physicians out of low and middle-income countries (LMIC)—is driven by many factors, including poor working conditions, burnout and better opportunities abroad. The author wrote that with the migration of the Zambian doctor, ‘the world’s richest country will have gained a bright young doctor. The loss to Zambia will be much greater.’ With this, the story conveys that while the motivation for any individual to migrate is deeply personal, the totality of this brain drain has profound public health and economic consequences.
It is estimated that there is a shortage of 2.8 million physicians worldwide,2 with LMICs suffering the brunt of this burden.3 This physician shortage is exacerbated by physician brain drain, with some high-income countries (HIC) drawing as much as one-fifth of their physician workforce from LMICs.4 The cost of brain drain to LMICs has been quantified in economic terms by calculating the cost of educating LMIC physicians prior to their emigration.5–7 However, physician emigration represents a unique loss of resources for LMICs that includes the loss of direct financial investment and the loss of lives that emigrating physicians could have saved had they stayed in their country of origin—that is, a cost of excess mortality. This public health aspect on the cost of brain drain has not yet been calculated. In this study, we aim to provide a valuation of the cost sustained by LMICs due to physician emigration to HICs as it pertains to the mortality benefits provided by physicians.
Methods
Model development
Conceptual model
We conceptualised the excess mortality cost of physician brain drain as the economic value of the lives that physicians could have saved had they stayed in their country of origin. This model required quantifying the economic value of a life, the lives that a physician saves and the number of physicians migrating from LMICs to HICs. To do this, we used the value of statistical life (VSL), an economic concept that places a monetary value on reductions in risk of mortality. To calculate the lives a physician saves we estimated the effect of physician density on two key parameters of public health: maternal mortality and under-five mortality. While this is not a comprehensive assessment of the mortality benefit provided by physicians, it provides a conservative value. Finally, we used existing data on physician migration in which a physician émigré is defined as those who received their initial medical qualification in an LMIC and are currently registered to practise in an HIC. Some island nations, such as Grenada, with American-based medical schools were eliminated from this model as source countries. The conceptual basis of our model can be described as:
where LS is the number of lives saved per physician in a year, and PA is the number of emigrated physicians currently abroad.
Value of statistical life
VSL provides a monetary measure of welfare for assessing and comparing public health interventions. This number has been used to calculate the economic burden attributed to health problems and the cost-benefit ratios of addressing them.8 The VSL for each country was calculated using previously proposed models for adjusting VSL between countries with different income levels,9
where VSLi is the VSL of country i, VSLBase is the value to be adjusted based on the gross national income (GNI) per capita purchasing power parity (PPP), and IE VSL is the income elasticity of the VSL. For our main analysis, we have followed the recommendations by Robinson et al,10 and used a base VSL value of $9.4 million with a base GNI per capita PPP value of $57 900, and an IE of 1.5. Where the income-level adjustment leads the estimated VSL to be below 20 times the GNI per capita, we have used 20 times GNI per capita as the VSL value for that country.10 As an example, a country with a GNI per capita of half that of the base country would have an estimated VSL of times the base VSL.
An IE of 1.0 implies that individuals are willing to spend the same proportion of their income on mortality risk reductions regardless of income, while an IE >1 implies that this proportion is lower in lower income settings—that is, that in low-income settings people are willing to spend a smaller portion of their income on mortality risk reduction. There is uncertainty as to what IE should be used when transferring VSL estimates. A recent study using panel data suggests an IE of 1.44.11 For international transfers of VSL, Viscusi and Masterman12 suggest using an IE between 1 and 1.2 based on revealed preference studies; evidence from stated preference studies suggests an elasticity of 0.55 for higher income countries and 1.0 for lower income countries.13 Given the lack of consensus, we used an IE of 1.5 which has been used in a similar healthcare-based economic analysis14 and is supported by Robinson et al.10 This results in a lower VSL in lower income countries.
Lives saved by physicians
To estimate the effect of physician density on mortality, we performed a cross-country multivariable regression using the latest available data, controlling for previously accepted confounders that have independently been shown to affect population health.15 We performed separate regressions using maternal mortality ratio (MMR) and under-five mortality ratio (U5MR) as dependent variables, with physician density, GNI per capita PPP, female literacy rate, nurse density and proportion of the population living in absolute poverty as independent variables. We examined the pair-wise correlation between the independent variables in order to assess collinearity.
To account for the fact that a single physician in a country with very few physicians provides a different benefit than a physician in a country with an abundance of physicians, we estimated the marginal effect (ie, elasticity) of physician density on mortality. This was done with linear regression on logarithmically transformed data. Logarithmical transformation of the data also results in better model fit than using non-transformed data. We then calculated the proportional decrease in mortality that would be brought about by an increase in the number of physicians:
where y is the mortality measure, ∂ is the elasticity, PA is the number of physicians abroad and P is the number of physicians in a country. Finally, we obtained an estimate of the number of lives saved by multiplying the proportional decrease with current absolute mortality rates.
Final model
Our final model for estimating cost of physician brain drain from LMICs was:
where AM is the absolute number of maternal and under-five deaths.
Statistical analysis
Monte Carlo estimation
Because of the uncertainty involved in measuring several of the input parameters of our model, we ran a Monte Carlo simulation with 10 000 runs. For the mortality measures, we constructed beta distributions using the uncertainty intervals reported by the WHO. For the physician densities, we used a normal distribution with µ=¼*σ. For the mortality elasticities, we used t-distributions derived from the regression.
Sensitivity analysis
In addition to the Monte Carlo simulation, we also ran one-way sensitivity analyses on VSL values as proposed by Robinson et al.10 In one sensitivity analysis, IE was set to 1.0, and in a second, the VSL base values were set to match those used in an Organisation for Economic Co-operation and Development (OECD) meta-analysis.
Data sources
Data on the number of emigrated physicians were obtained from the OECD (stats.oecd.org). For some HICs not covered in the OECD database, we used data from Bhargava et al.16 Data on the number of physicians and nurses by country, U5MR and MMR were obtained from the WHO (www.who.int/gho). Data for the independent variables in the regression were obtained from the World Bank World Development Indicators database (databank.worldbank.org). In each case, the most recent available data as of May 2017 were selected.
Absent or missing data
LMICs that were not in the OECD data set on physician migration were assumed to have no physician emigration. LMICs that did not have data on total number of physicians, GNI, U5MR or MMR were dropped from the analysis.
To handle missing data in the cross-country multivariable regression, we used multiple imputation by chained equation.17 The plausibility of imputations was assessed using diagnostic plots and by comparing the pooled regression results on multiply imputed data against those using ordinary listwise deletion.
Role of the funding source
No funding source had any part in study design, collection, analysis, and interpretation of data, writing the report, or the decision to submit the paper.
Data sharing
All data and codes used to produce the results in this study are available on request from the authors.
Patient and public involvement
Patients were not involved in this study.
Results
Characteristics of the included countries
One hundred and twenty-five LMICs were included in the study, covering a population of 6.3 million physicians, 260 000 of whom have immigrated to the 23 included HICs. Overall, 3.9% of the world’s physicians trained in LMICs are currently practising in HICs, but there is considerable regional variability, ranging from 0.9% of physicians trained in the Western Pacific region to 11.3% in the African region (table 1).
Table 1.
Characteristics of studied low and middle-income countries, by WHO region and World Bank income group
| n | GNI per capita PPP | Population | Physicians | Physicians abroad (percentage of physicians trained in region) | |
| WHO region | |||||
| Africa | 45 | 3803 | 976 754 579 | 189 157 | 24 166 (11.3) |
| Americas | 23 | 13 869 | 605 000 488 | 1 110 361 | 39 421 (3.4) |
| Eastern Mediterranean | 12 | 8095 | 560 768 323 | 552 434 | 49 484 (8.2) |
| Europe | 20 | 16 888 | 409 541 087 | 1 161 351 | 45 596 (3.8) |
| Southeast Asia | 10 | 6357 | 1 903 375 205 | 1 064 199 | 80 437 (7.0) |
| Western Pacific | 15 | 12 737 | 1 629 169 248 | 2 267 501 | 20 350 (0.9) |
| World Bank income group | |||||
| Low income | 28 | 1509 | 589 565 832 | 41 799 | 5204 (11.07) |
| Lower middle income | 48 | 5984 | 2 901 804 530 | 2 054 239 | 137 976 (6.29) |
| Upper middle income | 49 | 14 714 | 2 593 238 568 | 4 248 965 | 116 274 (2.66) |
| Total | 125 | 9271 | 6 084 608 930 | 6 345 003 | 259 454 (3.93) |
GNI, gross national income; PPP, purchasing power parity.
Inputs to the model
The VSL and details of the physician density-mortality regression broken down by WHO region are demonstrated in online supplementary appendix tables 1 and 2. The mean predicted number of lives saved per physician per year is demonstrated in online supplementary appendix table 3.
bmjgh-2019-001535supp001.pdf (94.3KB, pdf)
The cost of physician migration
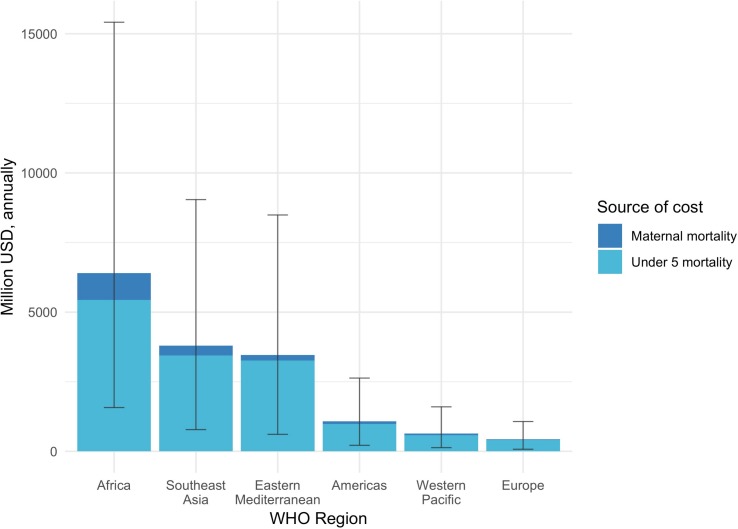
Our model suggests the cost of excess mortality due to physician emigration from LMICs is $15.86 billion annually (95% CI $3.38 to $38.25), or the equivalent of 0.057% (95% CI 0.012% to 0.138%) of total LMIC GNI. The per cent of GNI lost is greatest in the African region (0.370%; 95% CI 0.091% to 0.888%) and in low-income countries (table 2). The majority (89%) of the cost is due to VSL lost from under-five mortality, while VSL lost from maternal mortality contributes 11% (figure 1).
Table 2.
Annual cost of physician emigration, by WHO region and World Bank income group
| Total annual cost (million US$) | % of gross national income | Cost per physician per year (thousand US$) | |
| WHO regions | |||
| Africa | 6425 (1572 to 15 414) | 0.370% (0.091% to 0.888%) | 293 (71 to 740) |
| Americas | 1079 (216 to 2631) | 0.020% (0.004% to 0.050%) | 30 (6 to 78) |
| Eastern Mediterranean | 3468 (610 to 8490) | 0.205% (0.036% to 0.503%) | 76 (13 to 194) |
| Europe | 434 (75 to 1070) | 0.013% (0.002% to 0.031%) | 10 (2 to 26) |
| Southeast Asia | 3804 (780 to 9042) | 0.102% (0.021% to 0.243%) | 49 (10 to 121) |
| Western Pacific | 645 (132 to 1598) | 0.005% (0.001% to 0.014%) | 34 (7 to 86) |
| WB income groups | |||
| Low income | 936 (233 to 2213) | 0.258% (0.064% to 0.609%) | 208 (51 to 530) |
| Lower middle income | 10 582 (2352 to 25 350) | 0.181% (0.040% to 0.434%) | 82 (18 to 205) |
| Upper middle income | 4337 (798 to 10 682) | 0.020% (0.004% to 0.050%) | 41 (7 to 105) |
| Total | 15 855 (3384 to 38 245) | 0.057% (0.012% to 0.138%) | 66 (14 to 166) |
Median (95% CI).
WB, World Bank.
Figure 1.
Annual cost of physician emigration by WHO region and source of cost. Whiskers represent 95% CI. USD, US dollar.
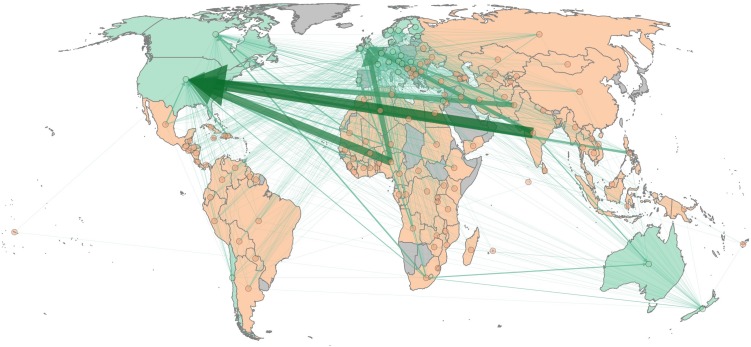
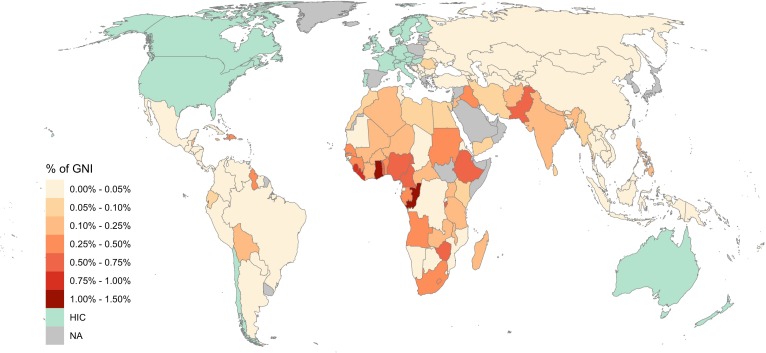
India, Nigeria, Pakistan and South Africa sustain the greatest total costs (figure 2, online supplementary appendix table 4). When measured as a proportion of GNI, the greatest costs are incurred by the Congo, Ghana, Liberia and Sierra Leone (figure 3, online supplementary appendix table 4). As an income group, lower middle-income countries have the greatest cost (67% of total cost), whereas low-income countries sustain the greatest proportion of GNI lost (0.26%, 95 CI 0.06% to 0.61%) (table 2).
Figure 2.
Physician migration patterns with arrows demonstrating direction of migration and arrow thickness proportional to cost of associated migration to source country.
Figure 3.
Annual cost of physician emigration, expressed as a percentage of gross national income (GNI). HIC, high-income country; NA, not applicable.
Sensitivity analysis
Changing the VSL estimates for LMICs increased our estimates. When IE was set to 1.0, the estimated cost was $49.5 billion. When IE was set to 1.0 and the base VSL value was 3.0 million as estimated by the OECD, the estimated cost was $30.5 billion.
Discussion
We estimate that LMICs lose nearly US$16 billion annually (95% CI $3.4 to $38.2) due to the cost of excess mortality that results from physician migration to HICs. The majority of this cost in our model is attributed to under-five mortality associated with lower physician density. When considering the excess mortality cost of brain drain as a percentage of GNI, the cost is greatest among low-income countries and in the African region. However, when total cost was assessed, it is greatest in lower middle-income countries and in the Southeast Asia and Eastern Mediterranean regions
Previous research evaluating the cost to LMICs of physician migration focused primarily on the cost of education. These studies, which were exclusive to the African continent, found the cost of educating a physician ranged from $29 898 to $65 997.5 6 These figures reflect a different conceptual cost of brain drain that is focused on the cost that LMICs incur based on what they have put in to training physicians. Our model moves beyond the interpretation of physicians as human capital and considers their productive function instead. Thus, we present cost as it pertains to what LMICs fail to receive out of the physicians they train. Our figures are several times higher than those of previous models on the cost of brain drain. Specifically, while Mills et al 5 estimated the total overall ‘lost investment’ for sub-Saharan Africa was $2.17 billion, we estimate the African region bears a cost of $6.4 billion yearly due to excess mortality owed to physician migration.
Further, our numbers reflect the cost of physician brain drain to LMICs each year that the current emigrated workforce remains out of the country. This incorporates the fact that brain drain does not result in a one-time capital loss but rather continues to affect LMIC each year that their physicians are out of the country. By focusing on mortality benefits that physicians bring to a given society and not just the cost of training them, we believe our models provide an important additional element in estimating the implications of physician migration.
Additionally, our analysis on a per-country basis and as a percentage of a country’s GNI can provide policymakers a data point for understanding one of the ways in which physician migration may affect a country’s economy. As an example, a policymaker in Nigeria would observe that our model suggests the excess mortality cost for Nigerian physicians who emigrate to HIC totals $3.1 billion annually (95% CI $0.8 to $7.5). This number is specific to Nigeria in a few critical ways: it accounts for the mortality benefit of physicians at Nigeria’s current physician density and the VSL based on Nigeria’s current domestic economic situation. While it cannot be interpreted as a comprehensive cost of physician migration, these annualised data may in part inform how much the country is willing to spend to improve physician retention. While individual motivations for migration are myriad, they include pursuit of higher salaries, improved work environment and quality of life18—factors that may be influenced by domestic initiatives.19 Our data may provide some empirical basis for increasing domestic health spending targeted towards ensuring adequate posts for physicians and adequate remuneration.
The results of this study are also pertinent to HIC policymakers. Many HICs mitigate their own physician shortfalls by drawing on LMIC physicians.4 In the UK, more than one-quarter of the country’s physicians are international medical graduates and more than three-fourths of these originate from LMICs.4 This demand for foreign healthcare workers in HICs is driven in part by domestic HIC policies such as training numbers, pay and employment conditions,20 with some HICs having adopted specific policies to promote physician immigration to compensate for domestic physician undertraining.21 Moreover, in some cases, health workers from LMICs are actively recruited by professional recruitment agencies and corporations.21 22 The Commonwealth,23 the International Council of Nursing24 and the WHO25 have defined ethical principles for the international recruitment of health personnel which may be additionally informed by these data. Further, while these ethical statements are non-enforceable, some authors have raised idea of using World Trade Organization General Agreement on Trade Services to enforce fair recruitment practices.26 Our analysis may provide important values for such trade negotiations.
While we provide a policy-relevant analysis of the cost of excess mortality in LMICs owed to physician migration to HIC, our findings must be interpreted with care. First, our model assumes a causal relationship between physician density and mortality, whereas the underlying data can only show association. While mortality may be related to physician density, there are numerous other confounders that my influence this correlation. Moreover, our study uses mortality as an outcome variable—parameter that not all types of physicians are likely to affect as many physician interventions target morbidity or quality of life. Thus, our data are not meant to be interpreted at the level of an individual physician, but rather at the aggregate level of physician density. Our estimated effects of physician density on mortality are consistent with those of previous cross-sectional studies.15 27 Additionally, longitudinal panel data regressions28 and data from natural experiments in Japan,29 Germany30 and Indonesia31 seem to suggest a larger effect than our model implies, which would suggest our overall estimates are conservative. Additionally, the model predicts a rather limited effect on mortality, ranging from an average of 1.72 lives saved per physician per year in the WHO African region, to 0.01 in the WHO Europe region.
Additionally, we only consider under-five mortality and maternal mortality. It is likely that increased physician density is also associated with decreased non-maternal adult mortality, which is not incorporated into our model. Moreover, our model does not adjust for selection bias in the specialty of these physicians or the quality of physicians who emigrate. Recent work has demonstrated that foreign graduates in the USA perform at or above the level of their American counterparts, suggesting that emigrating physicians might represent ‘some of the best physicians in their country of origin’,32 again rendering our estimate conservative.
A third limitation is our use of extrapolated data for VSL. While it would be ideal to use VSLs that were determined individually for each country, such data are not available.9 Our sensitivity analysis allows us to demonstrate what the total costs of physician migration would be if different VSLs are used. In our main results, we present the smallest of these estimates.
A large degree of uncertainty exists around several of our input parameters, including the current number of maternal and under-five deaths and the number of remaining and emigrated physicians. As a direct consequence of this, CIs produced by the model are wide. We have accounted for the uncertainty of key inputs by using the Monte Carlo method.
Finally, our model is not exhaustive in calculating the cost of physician migration and reflects only one dimension of economic valuation. Undoubtedly, there are costs and benefits incurred from physician migration beyond our estimates. Just a few examples include the economic benefit to the countries that receive the migrants, the benefit from exchange of ideas, the effects on physician productivity and effects on physician salary. Notably, we do not account for remittances to LMICs from physicians. While it has been suggested that remittances offset the cost of brain drain to LMICs, the true amount of such remittances is unknown and recent studies have suggested that remittance rates among healthcare workers are lower than expected.19 33 We believe the economic consequences of physician migration are determined by an innumerable set of factors and no single model can fully value the total cost. Our model aims to provide a simple and easily understood value that policymakers can use as one data point for valuing the cost of physician migration. Our model should not be interpreted as a comprehensive valuation.
Conclusion
We find that the cost to LMICs of current physician migration to HIC is approximately US$16 billion each year (95% CI $3.4 to $38.2). In some countries, the value of this loss amounts to more than 0.5% of the GNI each year. In our modelling analysis, we build on previous estimates of the cost of brain drain by considering the lost mortality benefit associated with physician migration. We also expand our estimates outside of the African continent and consider all countries with available data. The modelled numbers we present can serve as benchmarks for understanding the cost of brain drain vis-à-vis health spending and are likely to prove valuable to LMIC and HIC policymakers as they seek to produce equitable health outcomes worldwide.
Acknowledgments
The Program in Global Surgery and Social Change receives funding from the GE Foundation for the SS2020 project in Ethiopia, Tanzania and Cambodia.
Footnotes
Handling editor: Sanni Yaya
SS and NR contributed equally.
Correction notice: This article has been corrected since it was published. The article type has been updated.
Contributors: SS, BBM and MGS conceived the study. SS, NR and BBM developed the methodology. NR performed the statistical analysis. SS, NR and BBM wrote the initial draft of the paper. SS, NR, BBM, JM and MGS revised the paper for critical intellectual content. JM and MGS supervised the study.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Map disclaimer: The depiction of boundaries on the map(s) in this article do not imply the expression of any opinion whatsoever on the part of BMJ (or any member of its group) concerning the legal status of any country, territory, jurisdiction or area or of its authorities. The map(s) are provided without any warranty of any kind, either express or implied.
Competing interests: None declared.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data and code used to produce the results are available upon reasonable request.
References
- 1. McAllester M. America Is Stealing the World’s Doctors. The New York Times Magazine 2012. [Google Scholar]
- 2. Global strategy on human resources for health: workforce 2030 World Health Organization; 2016. [Google Scholar]
- 3. A universal truth: no health without a workforce. Geneva: World Health Organization; 2013. [Google Scholar]
- 4. Mullan F. The metrics of the physician brain drain. N Engl J Med 2005;353:1810–8. 10.1056/NEJMsa050004 [DOI] [PubMed] [Google Scholar]
- 5. Mills EJ, Kanters S, Hagopian A, et al. . The financial cost of doctors emigrating from sub-Saharan Africa: human capital analysis. BMJ 2011;343:d7031 10.1136/bmj.d7031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kirigia JM, Gbary AR, Nyoni J, et al. . The cost of health-related brain drain to the WHO African region. Afr J Health Sci 2006;13:1–12.17348737 [Google Scholar]
- 7. Kirigia JM, Gbary AR, Muthuri LK, et al. . The cost of health professionals' brain drain in Kenya. BMC Health Serv Res 2006;6:89 10.1186/1472-6963-6-89 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Alkire B, Hughes CD, Nash K, et al. . Potential economic benefit of cleft lip and palate repair in sub-Saharan Africa. World J Surg 2011;35:1194–201. 10.1007/s00268-011-1055-1 [DOI] [PubMed] [Google Scholar]
- 9. Hammitt JK, Robinson LA. The income elasticity of the value per statistical life: transferring estimates between high and low income populations. J Benefit Cost Anal 2011;2:1–29. 10.2202/2152-2812.1009 [DOI] [Google Scholar]
- 10. Robinson LA, Hammitt JK, O’Keeffe L. Valuing mortality risk reductions in global Benefit-Cost analysis. J Benefit Cost Anal 2019;10:15–50. 10.1017/bca.2018.26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kneisner TJ, Viscusi WK. Policy relevant heterogeneity in the value of statistical life: new evidence from panel data Quantile regressions. Center for Policy Research 2009;48. [Google Scholar]
- 12. Viscusi WK, Masterman CJ. Income Elasticities and global values of a statistical life. J Benefit Cost Anal 2017;8:226–50. 10.1017/bca.2017.12 [DOI] [Google Scholar]
- 13. Masterman CJ, Viscusi WK. The income elasticity of global values of a statistical life: stated preference evidence. J Benefit Cost Anal 2018;9:407–34. 10.1017/bca.2018.20 [DOI] [Google Scholar]
- 14. Alkire BC, Vincent JR, Burns CT, et al. . Obstructed labor and caesarean delivery: the cost and benefit of surgical intervention. PLoS One 2012;7:e34595 10.1371/journal.pone.0034595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Anand S, Bärnighausen T. Human resources and health outcomes: cross-country econometric study. The Lancet 2004;364:1603–9. 10.1016/S0140-6736(04)17313-3 [DOI] [PubMed] [Google Scholar]
- 16. Bhargava A, Docquier F, Moullan Y. Modeling the effects of physician emigration on human development. Econ Hum Biol 2011;9:172–83. 10.1016/j.ehb.2010.12.004 [DOI] [PubMed] [Google Scholar]
- 17. Buuren Svan, Groothuis-Oudshoorn K. Mice : Multivariate Imputation by Chained Equations in R. J Stat Softw 2011;45 10.18637/jss.v045.i03 [DOI] [Google Scholar]
- 18. Bezuidenhout MM, Joubert G, Hiemstra LA, et al. . Reasons for doctor migration from South Africa. South African Family Practice 2009;51:211–5. 10.1080/20786204.2009.10873850 [DOI] [Google Scholar]
- 19. Labonté R, Sanders D, Mathole T, et al. . Health worker migration from South Africa: causes, consequences and policy responses. Hum Resour Health 2015;13:92 10.1186/s12960-015-0093-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Pond B, McPake B. The health migration crisis: the role of four organisation for economic cooperation and development countries. The Lancet 2006;367:1448–55. 10.1016/S0140-6736(06)68346-3 [DOI] [PubMed] [Google Scholar]
- 21. Forcier MB, Simoens S, Giuffrida A. Impact, regulation and health policy implications of physician migration in OECD countries. Hum Resour Health 2004;2:12 10.1186/1478-4491-2-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Attaran A, Walker RB. Shoppers drug Mart or poachers drug Mart? Can Med Assoc J 2008;178:265–6. 10.1503/cmaj.071733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Migration of health workers from Commonwealth countries Experiences and recommendations for action. London: Commonwealth Secretariat; 2001. [Google Scholar]
- 24. Ethical nurse recruitment: international Council of nursing; 2001.
- 25. WHA63.16: WHO global code of practice on the International recruitment of health personnel: the world health organisation; 2010.
- 26. Martineau T, Decker K, Bundred P. "Brain drain" of health professionals: from rhetoric to responsible action. Health Policy 2004;70:1–10. 10.1016/j.healthpol.2004.01.006 [DOI] [PubMed] [Google Scholar]
- 27. Carr-Hill R, Currie E. What explains the distribution of doctors and nurses in different countries, and does it matter for health outcomes? J Adv Nurs 2013;69:n/a–37. 10.1111/jan.12138 [DOI] [PubMed] [Google Scholar]
- 28. Farahani M, Subramanian SV, Canning D. The effect of changes in health sector resources on infant mortality in the short-run and the long-run: a longitudinal econometric analysis. Soc Sci Med 2009;68:1918–25. 10.1016/j.socscimed.2009.03.023 [DOI] [PubMed] [Google Scholar]
- 29. Sakai R, Fink G, Kumamaru H, et al. . The impact of pediatrician supply on child health outcomes: longitudinal evidence from Japan. Health Serv Res 2016;51:530–49. 10.1111/1475-6773.12354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Liebert H, Mäder B. The impact of regional health care coverage on infant mortality and disease incidence 2016.
- 31. Frankenberg E. The effects of access to health care on infant mortality in Indonesia. Health Transit Rev 1995;5:143–63. [PubMed] [Google Scholar]
- 32. Tsugawa Y, Jena AB, Orav EJ, et al. . Quality of care delivered by general internists in US hospitals who graduated from foreign versus US medical schools: observational study. BMJ 2017;356 10.1136/bmj.j273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Crush J, Chikanda A, Pendleton W. The disengagement of the South African medical diaspora in Canada. J South Afr Stud 2012;38:927–49. 10.1080/03057070.2012.741811 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjgh-2019-001535supp001.pdf (94.3KB, pdf)