Abstract
Background
There is mixed evidence and lack of consensus on the impact of economic development on stunting, and likewise there is a dearth of empirical studies on this relationship in the case of sub-Saharan Africa. Thus, this paper examines whether economic growth is associated with childhood stunting in low-income and middle-income sub-Saharan African countries.
Methods
We analysed data from 89 Demographic and Health Surveys conducted between 1987 and 2016 available as of October 2018 using multivariable multilevel logistic regression models to show the association between gross domestic product (GDP) per capita and stunting. We adjusted the models for child’s age, survey year, child’s sex, birth order and country random effect, and presented adjusted and unadjusted ORs.
Results
We included data from 490 526 children. We found that the prevalence of stunting decreased with increasing GDP per capita (correlation coefficient=−0.606, p<0.0001). In the unadjusted model for full sample, for every US$1000 increase in GDP per capita, the odds of stunting decreased by 23% (OR=0.77, 95% CI 0.76 to 0.78). The magnitude of the association between GDP per capita and stunting was stronger among children in the richest quintile. After adjustment was made, the association was not significant among children from the poorest quintile. However, the magnitude of the association was more pronounced among children from low-income countries, such that, in the model adjusted for child’s age, survey year, child’s sex, birth order and country random effect, the association between GDP per capita and stunting remained statistically significant; for every US$1000 increase in GDP per capita, the odds of stunting decreased by 12% (OR=0.88, 95% CI 0.87 to 0.90).
Conclusion
There was no significant association between economic growth and child nutritional status. The prevalence of stunting decreased with increasing GDP per capita. This was more pronounced among children from the richest quintile. The magnitude of the association was higher among children from low-income countries, suggesting that households in the poorest quintile were typically the least likely to benefit from economic gains. The findings could serve as a building block needed to modify current policy as per child nutrition-related programmes in Africa.
Keywords: health policy, public health, stunting, cross-sectional survey
Key questions.
What is already known?
Child health goals remain far from being met in most parts of sub-Saharan Africa.
Policymakers expect economic growth to influence child well-being positively.
What are the new findings?
The prevalence of stunting decreases with increasing gross domestic product (GDP) per capita.
There is no significant association between GDP growth per capita and child stunting across sub-Saharan Africa.
Improved economic growth may positively affect the lives of children in wealthy households, but not of those from poor households.
What do the new findings imply?
Improving child well-being requires clear policies that will ensure the most affected children have access to the resources needed.
Background
High rates of child mortality and undernutrition remain a persistent barrier to economic and human development goals in sub-Saharan African countries.1–8 Chronic undernutrition is a key predictor of child mortality and morbidity, both of which exert long-term consequences on cognitive development, as well as educational and professional outcomes, and lower the opportunities for upward mobility.9–12 As such, addressing child stunting is a critical aspect of Africa’s human development efforts in the post-millennium development goals (MDGs) era.13 14
Researchers have shown that in many countries child mortality MDGs remain far from being met in sub-Saharan Africa, and risk factors such as inadequate healthcare infrastructure, lack of skilled human resources for healthcare and low use of reproductive and child health services are still widespread.5 15–19 Signs of great achievements are reported in the areas of fighting subsistence poverty, and improving access to better water and sanitation facilities, electricity, high school enrolment, and national and household food security, which are important preconditions for better child nutrition outcomes.15 20–23 Notwithstanding these achievements, sub-Saharan Africa and South Asian countries continue to account for most of the undernourished children worldwide, which in turn is contributing to the poor economic and human development outcomes.8 22
During the last two decades, the relationship between economic growth and child nutrition has attracted noteworthy research and donor attention.24–30 Using a data set of 74 developing countries observed between 1984 and 2014, many concluded that economic growth is not a sufficient condition for child undernutrition reductions,31 while others suggested that factors that contributed the most to the decrease in child stunting are full immunisation, iron supplements and deworming medication.32 Economic growth can lead to widening inequalities in a variety of ways, such as access to education, health and technology, and growth represents an important means to reduce poverty only if income distribution remains constant over time.29 A most recent review of evidence on the association between stunting and undernutrition in childhood and economic outcomes in adulthood indicated that economic growth is effective at reducing stunting when ‘increases in national income are directed at improving the diets of children, addressing gender inequalities and strengthening the status of women, improving sanitation and reducing poverty and inequities’.33
In the context of some developing countries, political reforms, influx of foreign aid and foreign direct investments are bringing unprecedented opportunities for growth, employment, education and improvement in public health indices.34–38 At the same time, significant challenges remain in an effort to sustain the growth trajectories, reduce the prevalence of extreme poverty, and cut child stunting and mortality rates. For sustaining the economic growth, challenges arise most notably from ineffective governance, endemic corruption, internal conflicts, high debt levels and poor resource management, which altogether downsize the impact of inadequate investment and intervention efforts to fight low child survival and anthropometric outcomes.39–42
The challenges for improving child health are more pronounced in the resource-limited countries with chronic fiscal deficits, high dependence on foreign donors and low-performing agriculture sector. Poor agricultural resources with chronic water and energy crisis generally result in higher dependency on imported food and inflation in consumer prices, with diminishing food security among the poor households.13 43–47 The burden of stunting gets further compounded by the fast-changing demography, labour market and sociocultural environment. An increasing number of people are leaving the agricultural sector as they struggle for a better life and migrate to urban areas for better job and livelihood prospects.48–51 This increasing trend of rural-to-urban migration is causing serious imbalances in the labour force, increasing urban poverty and mounting pressure on the fragile healthcare infrastructure, exacerbating the situation of health and nutritional status of the urban population.52–55
African age structure is predominantly young, meaning that each year an increasing number of people are enrolling in higher education and entering the job market without enough employment opportunities being created. Poor access to credit, market and technology also hinders the transition to high productivity jobs, and consequently a larger proportion of the youth remains stuck in low-productivity jobs.56–58 Low-income families face competing challenges between meeting basic needs such as food and housing and less immediate needs such as education and healthcare. This perpetuating cycle of poverty and stunting has been a key barrier to meeting most of the MDGs, and is most likely to remain so for the sustainable development goals as well, unless effective interventions (increased coverage of iron supplementation, immunisation, water, sanitation and hygiene, and social safety nets) are formulated and implemented.
There is mixed evidence and lack of consensus on the impact of economic development on nutrition improvement, and there is a dearth of empirical studies on this relationship in the case of sub-Saharan Africa. In the present study, we used data from 89 Demographic and Health Surveys (DHS) in sub-Saharan Africa to assess the relationship between child nutritional status and economic development. The main rationale was to contribute to the current evidence base and assist in policymaking for child nutrition-related programmes in Africa.
Methods
Study design
We used cross-sectional data from the DHS, which are nationally representative household surveys conducted in sub-Saharan Africa. This study used data from 89 DHS surveys conducted between 1987 and 2016 available as of October 2018. The DHS uses a multistage, stratified sampling design with households as the sampling unit.59 Eligible women and men living in households were interviewed. The survey data were comparable across countries as all survey instruments and procedures were implemented similarly.
Outcome variable
Childhood stunting and chronic childhood malnutrition were assessed using height-for-age according to WHO recommendations. We defined stunting as less than −2 SD for height-for-age z score (haz) according to the WHO international reference. The outliers were removed in line with the exclusion ranges recommended by WHO.60 Hence, haz <−6.0 and >+6 are excluded from the analysis.
Main explanatory variable
We used national aggregate data for gross domestic product (GDP) per capita from World Bank’s World Development Indicators (WDI). WDI provided data for GDP per capita, adjusted for purchasing power parity exchange rates. This adjustment makes the GDP per capita comparable across countries. Data from each respondent were merged with GDP per capita by country and survey year.
Covariates
The following covariates were included in the study: survey year, child’s age (0–11 months, 12–23 months, 24–48 months), child’s sex (male vs female), child’s birth order, household wealth index (poorest vs richest quintile),61 62 maternal educational attainment (no formal education vs secondary or higher education) and country income category (low-income vs lower-middle-income).
Statistical analyses
We used multivariable multilevel logistic regression models to analyse the association between stunting and GDP per capita. We specified a three-level model for binary response (stunted child or not), for a child (level 1), in a neighbourhood (level 2) living in a country (level 3). Two models were developed. First, the unadjusted model was with only GDP per capita as the only explanatory variable. The second model was adjusted for child’s age, survey year, child’s sex, birth order and country random effect.
In addition to the analyses of the full sample, we also developed regression models for various subsamples: the poorest and richest wealth quintiles; children aged 0–11, 12–23 and 24–48 months; no formal education and secondary or higher education; and low-income and lower-middle-income. We reported the measures of association and ORs with their 95% CIs. Finally, Pearson correlation analysis was performed to examine the association of (1) a country’s prevalence of stunting and GDP per capita and (2) the average annual change in the prevalence of stunting and the average annual change in GDP per capita. For correlation analysis, a country’s GDP per capita was log-transformed. Multilevel analysis was performed with the MLwiN V.3.02 software63 using Stata’s ‘runmlwin’.64 For all analyses, associations with a p value of less than 0.05 were considered significant.
Patient and public involvement
Patients and the public were not involved in the design and conduct of this research.
Results
Characteristics of the included surveys
We included data from 89 surveys conducted between 1987 and 2016 in 20 sub-Saharan African countries with anthropometric data for 490 526 children. The characteristics of the included surveys are summarised in table 1. The total sample size ranged from 8065 in Cote D’Ivoire to 54 880 in Kenya. In recent surveys, the prevalence of stunting ranged from 19.2% in Ghana to 48.4% in Madagascar, and recent GDP per capita ranged from US$300 in Malawi to US$2997 in Nigeria. Of the 20 countries, 14 experienced decline in the average annual change in the prevalence of stunting, from as much as −12.1% in Ethiopia to as little as −0.3% in Cote D’Ivoire. Meanwhile, the remaining six countries experienced an increase in the average annual change in the prevalence of stunting, ranging from as much as 10.2% in Mali to as little as 0.1% in Burkina Faso. Nigeria and Ethiopia experienced the strongest economic growth with an average annual growth rate of GDP per capita of 87.6% and 83.6%, respectively, while Zimbabwe and Uganda experienced the weakest economic growth with an average annual growth rate of GDP per capita of 10.3% and 13.8%, respectively.
Table 1.
Summary characteristics of the surveys
| Country | Surveys | Recent survey | Average annual change | ||||
| n | Years | Sample | % stunting | GDP per capita | Stunting | Economic growth | |
| Benin | 4 | 1996, 2001, 2006, 2011 | 26 084 | 44 | 825.9 | 10.1 | 31.7 |
| Burkina Faso | 4 | 1993, 1998, 2003, 2010 | 22 319 | 34.2 | 575.4 | 0.1 | 36 |
| Cameroon | 4 | 1991, 1998, 2004, 2011 | 12 343 | 31.6 | 1429.6 | 5.4 | 16.9 |
| Congo Democratic Republic | 2 | 2007, 2013 | 11 324 | 44.1 | 458.1 | −2 | 59.9 |
| Cote d’Ivoire | 3 | 1994, 1998, 2011 | 8065 | 29.8 | 1214.7 | −0.3 | 43.7 |
| Ethiopia | 4 | 2000, 2005, 2011, 2016 | 30 890 | 36.4 | 712.9 | −12.1 | 83.6 |
| Ghana | 6 | 1988, 1993, 1998, 2003, 2008, 2014 | 14 476 | 19.2 | 1449.7 | −9.3 | 49.4 |
| Guinea | 3 | 1999, 2005, 2012 | 8645 | 30.8 | 665.2 | 3.7 | 47.6 |
| Kenya | 5 | 1993, 1998, 2003, 2008, 2014 | 54 880 | 27.1 | 1335.1 | −8.4 | 65 |
| Madagascar | 4 | 1992, 1997, 2003, 2008 | 16 181 | 48.4 | 470.7 | −6.3 | 25.8 |
| Malawi | 5 | 1992, 2000, 2004, 2010, 2016 | 30 188 | 35.2 | 300.3 | −8.7 | 23.6 |
| Mali | 5 | 1987, 1995, 2001, 2006, 2012 | 30 082 | 37.7 | 777.3 | 10.2 | 34.2 |
| Mozambique | 3 | 1997, 2003, 2011 | 20 468 | 39.3 | 526.5 | −4.4 | 48.8 |
| Niger | 4 | 1992, 1998, 2006, 2012 | 16 459 | 41.9 | 391.5 | 1.6 | 18.2 |
| Nigeria | 5 | 1990, 1999, 2003, 2008, 2013 | 54 730 | 36.1 | 2997 | −5.3 | 87.5 |
| Rwanda | 5 | 1992, 2000, 2005, 2010, 2014 | 21 587 | 37.4 | 706.6 | −8.9 | 31.5 |
| Tanzania | 6 | 1991, 1996, 1999, 2004, 2010, 2015 | 36 853 | 33.6 | 872.3 | −7.8 | 38.6 |
| Uganda | 6 | 1988, 1995, 2001, 2006, 2011, 2016 | 22 207 | 28.4 | 580.4 | −9.1 | 13.8 |
| Zambia | 5 | 1992, 1996, 2001, 2007, 2013 | 32 389 | 39.6 | 1850.8 | −3.9 | 65 |
| Zimbabwe | 6 | 1988, 1994, 1999, 2005, 2010, 2015 | 20 356 | 25.6 | 1033.4 | −3.3 | 10.3 |
GDP, gross domestic product.
Association between economic growth and chronic childhood stunting
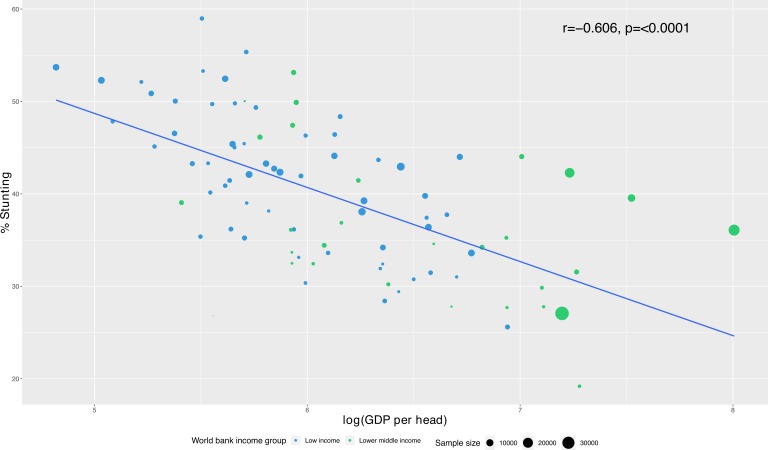
The ecological association between GDP per capita and the prevalence of stunting is shown in figure 1. There was a strong statistically significantly negative correlation between GDP per capita and stunting rate, such that the prevalence of stunting decreased with increasing GDP per capita (correlation coefficient=−0.606, p<0.0001) (figure 1). There was a negative correlation between the average annual economic growth and the average annual change in the prevalence of stunting, although not statistically significant (correlation coefficient=−0.291, p=0.214) (figure 2).
Figure 1.
Association between gross domestic product (GDP) per capita and prevalence of stunting.
Figure 2.
Association between average annual change in gross domestic product (GDP) per capita and prevalence of stunting.
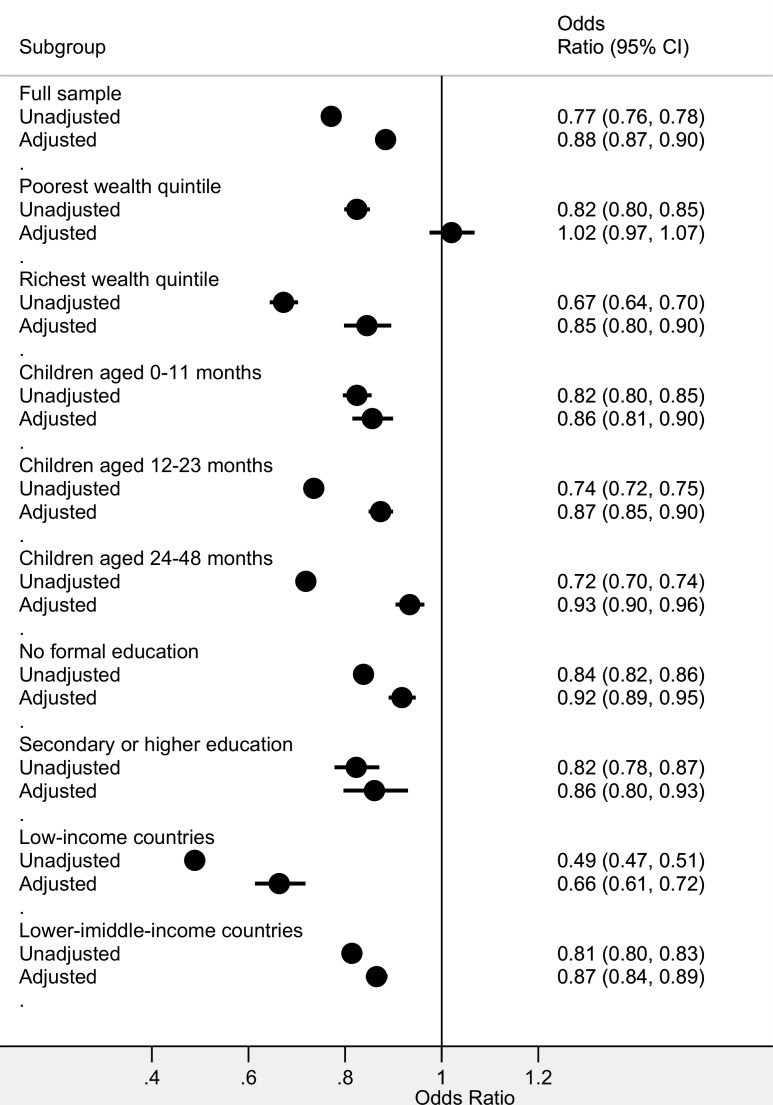
Figure 3 shows the adjusted and unadjusted associations (ORs) between GDP per capita and stunting for the full sample and the different subsamples. In the unadjusted model for full sample, for every US$1000 increase in GDP per capita, the odds of stunting decreased by 23% (OR=0.77, 95% CI 0.76 to 0.78). In the model adjusted for child’s age, survey year, child’s sex, birth order and country random effect, the association between GDP per capita and stunting remained statistically significant; for every US$1000 increase in GDP per capita, the odds of stunting decreased by 12% (OR=0.88, 95% CI 0.87 to 0.90).
Figure 3.
Unadjusted and adjusted associations between gross domestic product per capita and stunting.
The magnitude of the association between GDP per capital and stunting was stronger among children in the richest quintile. After an adjustment was made, the association was not significant among children from the poorest quintile. The pattern of the associations across different age groups of children was similar to the full sample, and similarly for the different maternal educational groups. However, the magnitude of the association was more pronounced among children from low-income countries, such that, in the model adjusted for child’s age, survey year, child’s sex, birth order and country random effect, the association between GDP per capita and stunting remained statistically significant; for every US$1000 increase in GDP per capita, the odds of stunting decreased by 12% (OR=0.88, 95% CI 0.87 to 0.90).
Discussion
The study explored the association between economic growth and childhood stunting in 20 sub-Saharan African countries. Secondary data from DHS conducted between 1987 and 2016 were considered and used. The study involved 490 526 children who had anthropometric data. This multicountry analysis provided evidence for the complex association between economic growth and childhood stunting,65–67 and suggested that economic growth does not necessarily translate or lead to higher nutritional status of children in Africa. To make sense of this observation, we considered the argument that economic gains in many parts of Africa accrue disproportionately to the richest quintile.68 69 For this subpopulation, economic growth may have the desired effect of improving the welfare of children and other household members. Households in the poorest quintile are typically the least likely to benefit from economic gains, and are thus the least affected. In a sense, the study aligns with explanations from a few earlier studies.65–67 70–72
For policy implementation and evaluation, a major implication is that macro-level economic growth indicators offer very little information about childhood stunting and general well-being, especially among the poorest, who also happen to be the most affected by negative health outcomes.73–75 Interventions designed with the assumption that economic growth translates to improved child well-being also run a high risk of being ineffective. Achieving the sustainable development goals depends on getting governments to address the gap between the rich and the poor, which is still at its highest level in decades.76
The findings of this study will serve as a building block needed to modify current policy as per child nutrition-related programmes in Africa. Perhaps, the economic gains achieved accrue disproportionately to the rich, who are less affected by the problems of poor child well-being and health outcomes. Improving child well-being requires clear policies that will ensure the most affected children have access to the resources needed. At present, those benefiting from the economic gains are those with higher order needs. We recommend that low-income and middle-income countries of the world are encouraged to commit more to equitable distribution through social investment programmes that alleviate the poorest of the poor so that the poor–rich gap in childhood stunting can be bridged.
Strengths and limitations
The study involved a large sample from 89 surveys conducted in 20 countries to measure the association between economic growth and child nutritional status. The data were nationally representative; therefore, the findings were generalisable in the study area. There are various ways of assessing the nutritional status of children aged under 5 years, such as using clinical signs, biochemical indicators or anthropometry.77 The anthropometric approach is the most commonly used method/approach78 and is more advantageous when compared with the other two because it has the benefit of ease of interpretation, rapidity and objectivity. Stunting is regarded as an indicator of long-standing dietary inadequacy and can also be due to chronic infections. The height-for-age measure is less sensitive to temporary food shortages and thus is the most reliable indicator of long-standing malnutrition in childhood.79 Furthermore, the WHO recommended stunting as a reliable measure of overall social deprivation.78 However, DHS data have limitations. The surveys were cross-sectional and therefore associations but no causalities could be established. In addition, the surveys were conducted in different years. Therefore, results from different surveys should be compared with caution.
Conclusions
Economic growth does not necessarily improve the well-being of children in Africa. Perhaps, the economic gains achieved accrue disproportionately to the rich, who are less affected by problems of poor child well-being and health outcomes. Improving child well-being requires clear policies that will ensure the most affected children have access to the resources needed. At present, those benefiting from the economic gains are those with higher order needs.
Acknowledgments
The authors thank the MEASURE DHS project for their support and for free access to the original data.
Footnotes
Handling editor: Seye Abimbola
Contributors: SY and OAU contributed to study design and conceptualisation. MK, NK, JOA, RMK and VA reviewed the literature. SY, OAU, OA and GB performed the analysis. All authors provided technical support and critically reviewed the manuscript for intellectual content. SY had the final responsibility to submit the manuscript for publication. All authors read and amended the drafts of the paper and approved the final version.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: SY is Associate editor of this journal.
Patient consent for publication: Not required.
Ethics approval: Ethics approval was not required for this study since it used secondary data, which are available in the public domain. More details regarding DHS data and ethical standards are available at http://goo.gl/ny8T6X.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data are available in a public, open access repository. Data for this study were sourced from Demographic and Health Surveys (DHS) and available at http://dhsprogram.com/data/available-datasets.cfm.
References
- 1. Accorsi S, Fabiani M, Nattabi B, et al. The disease profile of poverty: morbidity and mortality in northern Uganda in the context of war, population displacement and HIV/AIDS. Trans R Soc Trop Med Hyg 2005;99:226–33. 10.1016/j.trstmh.2004.09.008 [DOI] [PubMed] [Google Scholar]
- 2. Adjiwanou V, LeGrand T. Gender inequality and the use of maternal healthcare services in rural sub-Saharan Africa. Health Place 2014;29:67–78. 10.1016/j.healthplace.2014.06.001 [DOI] [PubMed] [Google Scholar]
- 3. Anele Nigeria Has the Third Highest Infant Mortality Rate In The World – WHO [Internet]. Listwand, 2017. Available: http://listwand.com/2017/10/nigeria-has-the-third-highest-infant-mortality-rate-in-the-world-who/ [Accessed 24 Jan 2018].
- 4. Bishai DM, Cohen R, Alfonso YN, et al. Factors contributing to maternal and child mortality reductions in 146 low- and middle-income countries between 1990 and 2010. PLoS One 2016;11:e0144908 10.1371/journal.pone.0144908 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Cha S. The impact of the worldwide Millennium Development Goals campaign on maternal and under-five child mortality reduction: ‘Where did the worldwide campaign work most effectively?’. Glob Health Action 2017;10:1267961 10.1080/16549716.2017.1267961 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Ezeh O, Agho K, Dibley M, et al. The impact of water and sanitation on childhood mortality in Nigeria: evidence from demographic and health surveys, 2003–2013. Int J Environ Res Public Health 2014;11:9256–72. 10.3390/ijerph110909256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Koblinsky M, Anwar I, Mridha MK, et al. Reducing maternal mortality and improving maternal health: Bangladesh and mdg 5. J Health Popul Nutr 2008;26:280–94. 10.3329/jhpn.v26i3.1896 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Singh A. Why are economic growth and reductions in child undernutrition so weakly correlated--and what can public policy do? Lancet Glob Health 2014;2:e185–6. 10.1016/S2214-109X(14)70200-1 [DOI] [PubMed] [Google Scholar]
- 9. Cusick SE, Georgieff MK. The Role of Nutrition in Brain Development: The Golden Opportunity of the "First 1000 Days". J Pediatr 2016;175:16–21. 10.1016/j.jpeds.2016.05.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Fulhan J, Collier S, Duggan C. Update on pediatric nutrition: breastfeeding, infant nutrition, and growth. Curr Opin Pediatr 2003;15:323–32. 10.1097/00008480-200306000-00017 [DOI] [PubMed] [Google Scholar]
- 11. Kar BR, Rao SL, Chandramouli BA. Cognitive development in children with chronic protein energy malnutrition. Behav Brain Funct 2008;4:31 10.1186/1744-9081-4-31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Martins VJB, Toledo Florêncio TMM, Grillo LP, et al. Long-Lasting effects of undernutrition. Int J Environ Res Public Health 2011;8:1817–46. 10.3390/ijerph8061817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Bain LE, Awah PK, Geraldine N, et al. Malnutrition in sub-Saharan Africa: burden, causes and prospects. Pan Afr Med J 2013;15:120 10.11604/pamj.2013.15.120.2535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Davies JI, Macnab AJ, Byass P, et al. Developmental origins of health and disease in Africa-influencing early life. Lancet Glob Health 2018;6:e244–5. 10.1016/S2214-109X(18)30036-6 [DOI] [PubMed] [Google Scholar]
- 15. Assefa Y, Damme WV, Williams OD, et al. Successes and challenges of the millennium development goals in Ethiopia: lessons for the sustainable development goals. BMJ Glob Health 2017;2:e000318 10.1136/bmjgh-2017-000318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Cohen RL, Alfonso YN, Adam T, et al. Country progress towards the millennium development goals: adjusting for socioeconomic factors reveals greater progress and new challenges. Global Health 2014;10 10.1186/s12992-014-0067-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. English M, English R, English A. Millennium development goals progress: a perspective from sub-Saharan Africa. Arch Dis Child 2015;100:S57–8. 10.1136/archdischild-2013-305747 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Lomazzi M, Borisch B, Laaser U. The millennium development goals: experiences, achievements and what's next. Glob Health Action 2014;7:23695 10.3402/gha.v7.23695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Ssewanyana S, Younger SD. Infant mortality in Uganda: determinants, trends and the millennium development goals. J Afr Econ 2008;17:34–61. 10.1093/jae/ejm004 [DOI] [Google Scholar]
- 20. Cha S, Mankadi PM, Elhag MS, et al. Trends of improved water and sanitation coverage around the globe between 1990 and 2010: inequality among countries and performance of official development assistance. Glob Health Action 2017;10:1327170 10.1080/16549716.2017.1327170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Institute of Medicine (US) Roundtable on Environmental Health Sciences Achieving water and sanitation services for health in developing countries. National Academies Press (US), 2009. [Google Scholar]
- 22. Khan ZR, Midega CAO, Pittchar JO, et al. Achieving food security for one million sub-Saharan African poor through push-pull innovation by 2020. Philos Trans R Soc Lond B Biol Sci 2014;369:20120284 10.1098/rstb.2012.0284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Masipa TS. The impact of climate change on food security in South Africa: current realities and challenges ahead. Jàmbá 2017;9 10.4102/jamba.v9i1.411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Ali SS, Goudar S. The impact of nutrition on child development at 3 years in a rural community of India. Int J Prev Med 2014;5:494–9. [PMC free article] [PubMed] [Google Scholar]
- 25. Bershteyn A, Lyons HM, Sivam D, et al. Association between economic growth and early childhood nutrition. Lancet Glob Health 2015;3:e79–80. [DOI] [PubMed] [Google Scholar]
- 26. Biadgilign S, Shumetie A, Yesigat H. Does economic growth reduce childhood undernutrition in Ethiopia? PLoS One 2016;11:e0160050 10.1371/journal.pone.0160050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Hurley KM, Yousafzai AK, Lopez-Boo F, et al. Early child development and nutrition: a review of the benefits and challenges of implementing integrated interventions. Adv Nutr 2016;7:357–63. 10.3945/an.115.010363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Martorell R. The role of nutrition in economic development. Nutr Rev 1996;54:S66–71. 10.1111/j.1753-4887.1996.tb03900.x [DOI] [PubMed] [Google Scholar]
- 29. McGovern ME, Krishna A, Aguayo VM, et al. A review of the evidence linking child stunting to economic outcomes. Int J Epidemiol 2017;46:1171–91. 10.1093/ije/dyx017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Vollmer S, Harttgen K, Subramanyam MA, et al. Association between economic growth and early childhood nutrition-Authors’ reply. Lancet Glob Health 2014;2:e501–2. [DOI] [PubMed] [Google Scholar]
- 31. Mary S. How much does economic growth contribute to child stunting reductions? Economies 2018;6:55 10.3390/economies6040055 [DOI] [Google Scholar]
- 32. Buisman LR, Van de Poel E, O'Donnell O, et al. What explains the fall in child stunting in sub-Saharan Africa? SSM Popul Health 2019;8:100384 10.1016/j.ssmph.2019.100384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Beker V. Growth, Inequality and Poverty: What Do We Know?Available: https://ssrn.com/abstract=2727231 [Accessed 14 Nov 2019].
- 34. Alemu AM, Lee J-S. Foreign aid on economic growth in Africa: a comparison of low and middle-income countries. SAJEMS 2015;18:449–62. 10.4102/sajems.v18i4.737 [DOI] [Google Scholar]
- 35. Bendavid E, Bhattacharya J. The relationship of health aid to population health improvements. JAMA Intern Med 2014;174:881–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Riddell A, Niño-Zarazúa M. The effectiveness of foreign aid to education: what can be learned? Int J Educ Dev 2016;48:23–36. [Google Scholar]
- 37. Shajalal M, Xu J, Jing J, et al. China's engagement with development assistance for health in Africa. Glob Health Res Policy 2017;2:24 10.1186/s41256-017-0045-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Yogo TU. Assessing the effectiveness of foreign aid in the education sector in Africa: the case of primary education. Afr Dev Rev 2017;29:389–402. 10.1111/1467-8268.12276 [DOI] [Google Scholar]
- 39. Fosu AK. Implications of the external Debt-servicing constraint for public health expenditure in sub-Saharan Africa. Oxford Dev Stud 2008;36:363–77. 10.1080/13600810802455112 [DOI] [Google Scholar]
- 40. Mackey TK, Kohler JC, Savedoff WD, et al. The disease of corruption: views on how to fight corruption to advance 21st century global health goals. BMC Medicine 2016;14:149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Mostert S, Njuguna F, Olbara G, et al. Corruption in health-care systems and its effect on cancer care in Africa. Lancet Oncol 2015;16:e394–404. 10.1016/S1470-2045(15)00163-1 [DOI] [PubMed] [Google Scholar]
- 42. Rispel LC, de Jager P, Fonn S. Exploring corruption in the South African health sector. Health Policy Plan 2016;31:239–49. [DOI] [PubMed] [Google Scholar]
- 43. Akombi BJ, Agho KE, Merom D, et al. Child malnutrition in sub-Saharan Africa: a meta-analysis of demographic and health surveys (2006-2016). PLoS One 2017;12:e0177338 10.1371/journal.pone.0177338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Alemu ZA, Ahmed AA, Yalew AW, et al. Non random distribution of child undernutrition in Ethiopia: spatial analysis from the 2011 Ethiopia demographic and health survey. Int J Equity Health 2016;15:198 10.1186/s12939-016-0480-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Belfort MB, Rifas-Shiman SL, Rich-Edwards JW, et al. Maternal iron intake and iron status during pregnancy and child blood pressure at age 3 years. Int J Epidemiol 2008;37:301–8. 10.1093/ije/dyn002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Chopra M, Darnton-Hill I. Responding to the crisis in sub-Saharan Africa: the role of nutrition. Public Health Nutr 2006;9:544–50. [DOI] [PubMed] [Google Scholar]
- 47. Webb P, Stordalen GA, Singh S, et al. Hunger and malnutrition in the 21st century. BMJ 2018;361:k2238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Buchanan P. Transport, land use and economics, 2016. Available: https://www.ingentaconnect.com/content/hsp/jurr/2016/00000009/00000002/art00006 [Accessed 27 Nov 2018].
- 49. Buckley RM, Simet L. An agenda for habitat III: urban perestroika. Environ Urban 2016;28:64–76. 10.1177/0956247815622131 [DOI] [Google Scholar]
- 50. Güneralp B, Lwasa S, Masundire H, et al. Urbanization in Africa: challenges and opportunities for conservation. Environ Res Lett 2017;13:015002 10.1088/1748-9326/aa94fe [DOI] [Google Scholar]
- 51. Turok I. Getting urbanization to work in Africa: the role of the urban land-infrastructure-finance nexus. Area Development and Policy 2016;1:30–47. 10.1080/23792949.2016.1166444 [DOI] [Google Scholar]
- 52. Aliyu AA, Amadu L. Urbanization, cities, and health: the challenges to Nigeria – a review. Ann Afr Med 2017;16:149–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Keiser J, SINGER BH, SMITH TA, et al. Urbanization in sub-Saharan Africa and implication for malaria control. 71 American Society of Tropical Medicine and Hygiene, 2004: 118–27. https://www.ncbi.nlm.nih.gov/books/NBK3775/ 10.4269/ajtmh.2004.71.118 [DOI] [PubMed] [Google Scholar]
- 54. Oni T, Smit W, Matzopoulos R, et al. Urban health research in Africa: themes and priority research questions. J Urban Health 2016;93:722–30. 10.1007/s11524-016-0050-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Razak F, Berkman L. Urban development in sub-Saharan Africa: bearer of goods and risks. PLoS Med 2014;11:e1001684 10.1371/journal.pmed.1001684 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Collinson MA, White MJ, Ginsburg C, et al. Youth migration, livelihood prospects and demographic dividend: a comparison of the census 2011 and Agincourt health and demographic surveillance system in the rural northeast of South Africa. Etude Popul Afr 2016;30:2629–39. 10.11564/30-2-852 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Engelbrecht M, Shaw L, van Niekerk L. A literature review on work transitioning of youth with disabilities into competitive employment. Afr J Disabil 2017;6:298 10.4102/ajod.v6i0.298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Wilkinson A, Pettifor A, Rosenberg M, et al. The employment environment for youth in rural South Africa: a mixed-methods study. Dev South Afr 2017;34:17–32. 10.1080/0376835X.2016.1259986 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Rutstein SO, Rojas G. Guide to DHS statistics: demographic and health surveys methodology. Calverton, Maryland: ORC Macro, 2006. [Google Scholar]
- 60. WHO Physical status: the use and interpretation of anthropometry. technical report series No. 854. Geneva: WHO, 1995. [PubMed] [Google Scholar]
- 61. Montgomery MR, Gragnolati M, Burke KA, et al. Measuring living standards with proxy variables. Demography 2000;37:155–74. 10.2307/2648118 [DOI] [PubMed] [Google Scholar]
- 62. Vyas S, Kumaranayake L. Constructing socio-economic status indices: how to use principal components analysis. Health Policy Plan 2006;21:459–68. 10.1093/heapol/czl029 [DOI] [PubMed] [Google Scholar]
- 63. Rasbash J, Charlton C, Browne WJ. MLwiN Version 2.31 : Centre for multilevel modelling. University of Bristol, 2014. [Google Scholar]
- 64. Leckie G, Charlton C. Runmlwin - A Program to Run the MLwiN Multilevel Modelling Software from within Stata. Journal of Statistical Software 2013;52:1–40.23761062 [Google Scholar]
- 65. Alderman H, Hoogeveen H, Rossi M. Reducing child malnutrition in Tanzania. combined effects of income growth and program interventions. Econ Hum Biol 2006;4:1–23. 10.1016/j.ehb.2005.07.001 [DOI] [PubMed] [Google Scholar]
- 66. Frijters P, Haisken-DeNew JP, Shields MA. The causal effect of income on health: evidence from German reunification. J Health Econ 2005;24:997–1017. 10.1016/j.jhealeco.2005.01.004 [DOI] [PubMed] [Google Scholar]
- 67. Heltberg R. Malnutrition, poverty, and economic growth. Health Econ 2009;18:S77–88. 10.1002/hec.1462 [DOI] [PubMed] [Google Scholar]
- 68. Kai K. Globalization, financial depth, and inequality in sub-Saharan Africa. Economics Bulletin 2009;29:2025–37. [Google Scholar]
- 69. Dreher A, Gaston N. Has globalization increased inequality? Rev Int Econ 2008;16:516–36. 10.1111/j.1467-9396.2008.00743.x [DOI] [Google Scholar]
- 70. Keeley B. Income inequality: the gap between rich and poor. Paris: OECD Insights, OECD Publishing, 2015. [Google Scholar]
- 71. Thoa NTM, Thanh NX, Chuc NTK, et al. The impact of economic growth on health care utilization: a longitudinal study in rural Vietnam. Int J Equity Health 2013;12:19 10.1186/1475-9276-12-19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. De Silva I, Sumarto S. Does economic growth really benefit the poor? income distribution dynamics and Pro-poor growth in Indonesia. Bull Indones Econ Stud 2014;50:227–42. 10.1080/00074918.2014.938405 [DOI] [Google Scholar]
- 73. Gwatkin DR. Health inequalities and the health of the poor: what do we know? what can we do? Bull World Health Organ 2000;78:3–18. [PMC free article] [PubMed] [Google Scholar]
- 74. Umuhoza SM, Ataguba JE. Inequalities in health and health risk factors in the southern African development community: evidence from World health surveys. Int J Equity Health 2018;17:52 10.1186/s12939-018-0762-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. van Doorslaer E, Wagstaff A, Bleichrodt H, et al. Income-Related inequalities in health: some international comparisons. J Health Econ 1997;16:93–112. 10.1016/S0167-6296(96)00532-2 [DOI] [PubMed] [Google Scholar]
- 76. Yaya S, Ghose B. Global inequality in maternal health care service utilization: implications for sustainable development goals. Health Equity 2019;3:145–54. 10.1089/heq.2018.0082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. de Onis M, Frongillo EA, Blössner M. Is malnutrition declining? an analysis of changes in levels of child malnutrition since 1980. Bull World Health Organ 2000;78:1222–33. [PMC free article] [PubMed] [Google Scholar]
- 78. WHO Working Group Use and interpretation of anthropometric indicators of nutritional status. who Working group. Bull World Health Organ 1986;64:929–41. [PMC free article] [PubMed] [Google Scholar]
- 79. Svedberg P. Undernutrition in sub-Saharan Africa: a critical assessment of the evidence. world Institute for development economics research, working paper No.15. Helsinki: UNU/WIDER, 1987. [Google Scholar]