Abstract
Objective
Osteoradionecrosis (ORN) of the sphenoid is a rare but potentially lethal complication that can occur after irradiation of nasopharyngeal and clival malignancies. The objective of this study was to describe a multimodal treatment strategy tailored to the clinical signs and to the radiological extent of the disease, and to report on its preliminary results.
Methods
Retrospective monocentric study at a tertiary skull base center. Patients treated for a sphenoid ORN from January 2014 to August 2018 were identified and charts were retrospectively reviewed for demographics, histologic tumor type, previous treatments of the tumor, clinical signs at presentation, radiological data, treatment, and outcomes. Sphenoid ORN was treated by a combination of medical therapy, endovascular treatment, and/or surgery. The use of each of these therapeutic modalities was based on the extent of ORN and on the presenting signs.
Results
Seven patients were included: four patients underwent endovascular treatment with occlusion of the internal carotid artery, five patients underwent surgical debridement, and covering of the exposed bone by a local flap, seven patients received antibiotics (in combination with pentoxyphilline, tocopherol, and clodronate in one case). Three patients died after progression of the ORN. The global survival rate was 57% (4/7) with a mean follow‐up of 24 months. In one case, ORN was treated successfully by medical treatment only, with a combination of antibiotics, pentoxyphilline, tocopherol, and clodronate.
Conclusion
This retrospective study describes the results of a management strategy adapted to the extent of the disease in sphenoid ORN and based on medical therapy only, or on a combination of medical therapy, interventional radiology, and/or surgery.
Level of evidence
4
Keywords: chordoma, Clivus, endoscopic surgery, nasopharyngeal carcinoma, olfactory neuroblastoma, osteoradionecrosis, pentoxifylline‐tocopherol‐clodronate, radiotherapy, skull base, sphenoid
This study reports on 7 cases with sphenoid ORN and their management by a combination of medical therapy, endovascular treatment and/or surgery. The global survival rate was 57% (4/7) with a mean follow‐up of 24 months. One patient was successfully treated by medical treatment only, with a combination of antibiotics, pentoxyphilline, tocopherol and clodronate.
1. INTRODUCTION
Radiotherapy is a cornerstone of treatment for the management of nasopharyngeal and skull base malignancies. It is used either alone or in combination with surgery. Osteoradionecrosis (ORN) is a severe complication following radiation therapy. There are relatively few studies on sphenoid ORN but it appears to be a life‐threatening condition, with reported survival rates as low as 33%.1 Several treatment regimen have been described, including conservative management with antibiotherapy or hyperbaric oxygen and more aggressive approaches such as surgical debridement of the necrotic tissues followed by protection of the exposed bone by local or free flaps.2, 3 However, the extent of ORN may be very variable, and it seems difficult to use a single approach for the management of the various stages of the disease.
The aim of this study was to report on a series of seven patients treated by a combination of medical therapy, endovascular treatment, and/or surgery, with a strategy discussed on a case by case basis and tailored to the symptoms and to the extent of the ORN.
2. MATERIALS AND METHODS
2.1. Ethical considerations
In accordance with French laws, the study was approved by the CNIL (Commission Nationale Informatique et Libertés—authorization number 2213218), and all patients gave their informed consent.
2.2. Study design and patients selection
This was a retrospective monocentric study performed in a tertiary skull base center. Patients treated for a skull base ORN from January 2014 to August 2018 were identified from a local database and charts were retrospectively reviewed for the following data: demographics, histologic tumor type, previous treatments of the tumor, clinical signs at presentation, radiological data, treatment, and outcomes. The diagnosis of sphenoid ORN was based on the presence of a bone lysis on Computed Tomography (CT) within the field of irradiation, with a biopsy ruling out tumor recurrence. In all cases, the patients underwent both CT and Magnetic Resonance Imaging (MRI).
2.3. Treatment strategy
The treatment strategy was discussed on a case by case basis by a multidisciplinary team. Medical therapy was used in combination with other treatments, or alone in very limited cases of ORN, well tolerated and with low risk of carotid rupture. It consisted either of a targeted antibiotherapy prescribed for at least 3 months or of a regimen based on pentoxifylline, α‐tocopherol, and clodronate used in combination with antibiotics, antifungal therapy, and steroids, as described previously by Delanian et al (PENTOCLO).4 Endovascular treatment was advocated in patients presenting with active bleeding or when the internal carotid artery (ICA) was considered at‐risk for rupture (irregular shape of the lumen of the artery, the presence of a pseudo‐aneurism, ICA no longer covered by bone, and exposed to necrotic soft tissues); in these patients, angiography was performed under general anesthesia, and a balloon test occlusion (BTO) of the ICA was performed. If the test was well tolerated, the ICA was occluded using coils. If the ICA occlusion could not be performed (negative BTO or previous occlusion of the contralateral ICA), a covered stent was used to protect the ICA. Surgery was advocated in symptomatic cases with major bone exposure on endoscopy. In such cases, endoscopic surgical treatment was performed under general anesthesia (after ICA occlusion if necessary) with a maximum drilling of the exposed bone, and covering of the surgical area by a local flap. In this situation, the pedicled temporoparietal fascia flap (TPFF) was the first option.5 Clinical follow‐up was then scheduled at least every 3 months for the first 2 years, and imaging by CT‐scan and/or MRI was performed at least every 6 months for the first 2 years.
3. RESULTS
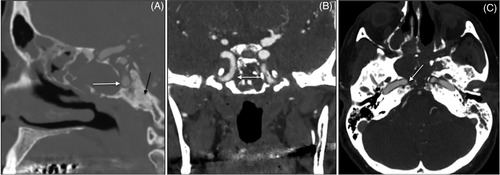
Seven patients were included in this study. Clinical and radiological data, treatments, and outcomes are summarized in Table 1. Mean age at diagnosis was 54 and the sex ratio was 1.3. The patients had been previously treated for nasopharyngeal carcinoma (n = 4, 57%), chordoma (n = 2, 29%), and olfactory neuroblastoma (n = 1, 14%). They had received 1, 2, or 3 courses of radiotherapy (n = 4, n = 2, and n = 1, respectively). The mean delay between the last course of radiotherapy and the diagnosis of ORN was 7 years (range 1‐25). Clinical signs at presentation included acute symptoms such as epistaxis (including 1 carotid blow‐out), CSF rhinorrhea, and cranial nerve palsy in five cases (71%), and/or chronic aspecific signs such as asthenia and headache in six cases (86%). Endoscopic examinations revealed a typical aspect of exposed bone surrounded by necrotic tissues in the nasopharynx in all cases (Figure 1). Of note, the area of exposed bone was very limited in one asymptomatic patient, but the sphenoid ORN was further confirmed by CT‐scan.
Table 1.
Clinical characteristics, imaging findings, treatments, and outcomes
| Case # | Gender/age | Tumor type | Previous treatment | Clinical signs | Radiological extent of the ORN | Medical treatment | Endovascular treatment | Surgerya | Outcome | Follow‐up (months) |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | F/62 | NPC | CT + RT (202 Gy) | Headache, cranial nerve palsy (XII) | Sphenoid + temporal bone | ABT | + | + | DOD (sepsis) | |
| 2 | M/74 | NPC | CT + RT (70 Gy) | Asthenia | Sphenoid | ABT | + | + | NED | 35 |
| 3 | M/42 | Chordoma | Surgery + RT (70 Gy) | Headache, cranial nerve palsy (VI), epistaxis | Sphenoid | ABT | + | Patient refusal | DOD (in stent thrombosis) | 42 |
| 4 | F/65 | ONB | Surgery + RT (70 Gy) | Headache, cranial nerve palsy (VI) | Sphenoid | ABT | + | NED | ||
| 5 | M/31 | NPC | CT + RT (130 Gy) | Headache, epistaxis | Sphenoid | ABT | + | + | DOD (ICA rupture) | 7 |
| 6 | M/45 | NPC | CT + RT (70 Gy) | − | Sphenoid + C1 | PENTOCLO | NED | 19 | ||
| 7 | F/57 | Chordoma | Surgery + RT (144 Gy) | Headache, CSF rhinorrhea | Sphenoid + temporal bone | ABT | + | NED | 17 |
Abbreviations: ABT, antibiotics; CSF, cerebrospinal fluid; CT, chemotherapy; DOD, dead of disease (ORN); NED, no evidence of disease; NPC, nasopharyngeal carcinoma; ONB, olfactory neuroblastoma; ORN, osteoradionecrosis; PENTOCLO, pentoxifylline, α‐tocopherol, and clodronate; RT, radiotherapy.
Removal of necrotic tissus and TPFF.
Figure 1.
Endoscopic aspect of ORN after radiotherapy for nasopharyngeal carcinoma, with an area of exposed bone in the nasopharynx
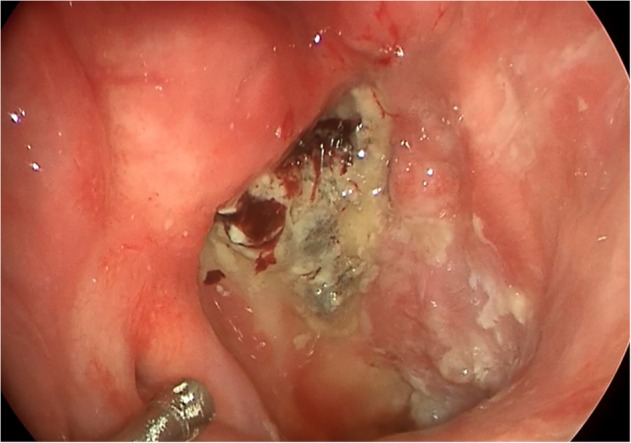
CT‐scan and MRI were performed in all cases to assess the extent of ORN. A bony lysis of the lower part of the sphenoid bone was present in all cases. The ORN extended to the temporal bone in two cases, and to C1, with a bony sequestration within the anterior arch of C1, in one case (patient #6). The ICA was no longer covered by bone in six cases, and it was directly exposed to necrotic tissues in four cases. An example of ORN of the sphenoid bone with exposure of the ICA is displayed in Figure 2.
Figure 2.
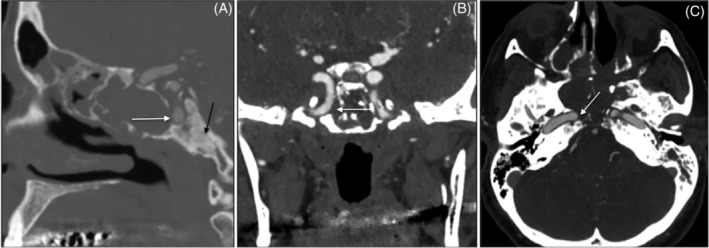
Contrast‐enhanced CT‐scan of a patient with sphenoid ORN in a sagital (A), coronal (B), and axial (C) plane. Note the dehiscence of the paraclival segment of the ICA (white arrow), and the bony sclerosis in the clivus area (black arrow)
The treatment strategy was decided based on the extent of the ORN and on the clinical symptoms, as described in section 2. Endovascular treatment was advocated in four cases: two patients presented with epistaxis, and the remaining two had no bleeding but the radiological aspect suggested that there was a significant risk of ICA rupture. In all cases, the BTO was positive, and occlusion of the ICA was performed with coils. In one patient, the procedure resulted in a transient hemiparesis, which resolved after curative anticoagulant therapy. Five patients underwent surgical debridement through an endoscopic transnasal approach, with removal of the necrotic tissues and drilling of the exposed bone. In all five cases, the surgical field was covered at the end of the procedure by a pedicled TPFF (Figure 3). A 3‐month course of antibiotics was prescribed post‐operatively in these five patients. Two patients had no surgical treatment. Patient #3 presented with massive epistaxis and was treated by ICA occlusion. Surgical treatment was then advocated, but the patient refused surgery and was treated only by antibiotics. After 8 months, he experienced a carotid blowout on the contralateral side, and though the bleeding was controlled after placement of a covered stent, the patient died 1 month later because of in‐stent thrombosis. Patient #6 was diagnosed with a minimal ORN, with very limited bone exposure and visualization on CT‐scan of a bony sequestration detached from the anterior branch of C1. A medical treatment based on PENTOCLO regimen was prescribed for 12 months. Endoscopic and radiological follow‐up showed a progressive healing of the mucosa and an ossification of the affected bone.
Figure 3.
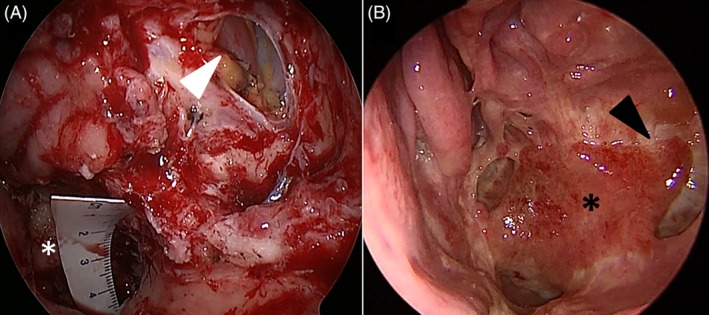
Covering of the exposed bone by a pedicled temporoparietal fascia flap (TPFF) in sphenoid ORN. (A) Intraoperative view: the exposed bone is visible in the nasopharynx (white asterisk); a left medial maxillectomy has been performed to gain a wide access to the posterior wall of the maxillary sinus, and an opening has been made in the posterior wall of the sinus (white arrowhead) to provide a direct route to the flap from the temporalis fossa to the nasopharynx. Note how the temporalis muscle is visible through this opening. (B) Post‐operative endoscopic view after 2 months: the TPFF (black asterisk) passes through the opening in the posterior wall of the left maxillary sinus (black arrowhead) and covers the area of ORN
After 24 ± 14 months [7‐42] of follow‐up, the overall survival rate was 57%. If patient #3 (who refused the surgical part of the treatment) was excluded, the overall survival rate was 67% (4/6). Four patients were considered healed, with no sign of disease. Three patients underwent progression of the ORN, and died of ICA rupture (n = 1), sepsis (n = 1), or in‐stent thrombosis of the remaining ICA (patient #3). Of note, two out of these three patients had received high doses of irradiation (202 and 130 Gy for patient #1 and #5, respectively).
4. DISCUSSION
In this study, we describe the results of a multimodal treatment strategy for the management of sphenoid ORN. By applying this strategy, the overall survival rate at 24 months was 57% (or 67% after exclusion of a patient who refused the surgical part of the treatment).
There is relatively few data on sphenoid ORN. An estimated incidence rate of 1% has been reported after radiotherapy for nasopharyngeal carcinoma.6 However, the incidence may be underestimated because the clinical signs are often not specific. Indeed, some patients present with acute signs such as massive bleeding or meningitis, but in other cases the only presenting signs are asthenia, chronic pain, or even cachexia.3, 6, 7 Such signs in a patient previously treated by radiotherapy should therefore prompt the clinician to look for ORN. These aspecific sign also explain why many patients are diagnosed at an advanced stage: four out seven patients (57%) presented with an ICA no longer covered by bone, and exposed to necrotic tissues.
The best treatment protocol for sphenoid ORN still remains to be determined. An overall survival rate of 54% has been reported by Liu et al with a surgical management through an endoscopic approach.8 Other authors have reported on open approaches with free flaps.3 Huang and al. recently described their experience of 162 cases of ORN after radiotherapy for nasopharyngeal carcinoma. A conservative approach based on nasal washout and a combination of pentoxifylline and tocopherol was used first, and surgery was considered for patients with complications secondary to the ORN that failed conservative treatment. Overall, 58 patients required surgery, through an endoscopic approach in 12 cases and using a maxillary swing/mandibulotomy approach in the other cases. The authors report an overall survival of 85.2%, in operated patients, and a complete resolution of symptoms in all cases with a mean follow‐up of 36.2 months.9 In our opinion, it seems difficult to use a unique strategy for the management of sphenoid ORN, as patients may present at very variable stages of the disease. In advanced cases, surgery allows to resect the necrotic tissues. An endoscopic approach was possible in all patients in this series and the TPFF was used in all cases. Indeed, the nasoseptal flap, which is widely used in endoscopic surgery, is not always available in situations of sphenoid ORN, either because it has already been used or because the posterior part of the septum has been removed during previous surgery. Moreover, radiotherapy may alter the viability of the flap: though several authors have reported on the use of nasoseptal flap in sphenoid ORN,9 the risk of necrosis of the flap is, at least in our experience, much higher in previously irradiated patients. The TPFF has other advantages: it may be harvested on both sides, depending on the previous irradiation fields; it is easy to handle and it can cover a wide surface of exposed bone.5 It also obviates the need for a free flap, which may be more complex to use in previously irradiated patients, especially in this area.10
One patient was treated conservatively with a purely medical treatment. This patient had no symptom, but endoscopy and CT scan revealed a limited ORN of the sphenoid that extended to C1. The patient received a prolonged treatment with a pentoxifylline‐tocopherol‐clodronate combination (PENTOCLO), a protocol previously described by Delanian et al: this triple‐drug therapy has been designed to reduce radio‐induced fibrosis and bone destruction and to stimulate osteogenesis via the antioxidant pathway.4 It has proved effective in mandibular ORN. To the best of our knowledge, this is the first published case of sphenoid ORN successfully treated by PENTOCLO. This encouraging result supports the rationale for a conservative approach in limited cases of sphenoid ORN.
The high mortality rate of sphenoid ORN raises the question of the potential morbidity of radiotherapy for tumors involving the sphenoid. Most authors agree that the risk of severe complications raises significantly in patients who received more than 1 course of radiotherapy, or doses >72 Gy.6 In this study, the two patients who accepted the treatment plan but died after progression of the ORN had received 130 and 202 Gy. The indication of re‐irradiation in residual or recurrent tumor should therefore be carefully discussed. For nasopharyngeal carcinoma, it has been shown that surgery was superior to intensity‐modulated radiation therapy in selected cases of rT1‐T3 tumors.11 This new data has been incorporated into the United Kingdom National Multidisciplinary Guidelines in 2016, which state that “surgery in form of nasopharyngectomy should be considered as a first line treatment of residual or recurrent disease at the primary site.”.12
5. CONCLUSION
This retrospective study describes the results of a management strategy adapted to the extent of the disease in sphenoid ORN and based on medical therapy only, or on a combination of medical therapy, interventional radiology, and/or surgery.
CONFLICT OF INTEREST
No conflicts were reported for this work.
Daoudi H, Labeyrie MA, Guillerm S, et al. Multimodal strategy for the management of sphenoid osteoradionecrosis: Preliminary results. Laryngoscope Investigative Otolaryngology. 2020;5:19–23. 10.1002/lio2.345
REFERENCES
- 1. Huang X‐M, Zheng Y‐Q, Zhang X‐M, et al. Diagnosis and management of skull base osteoradionecrosis after radiotherapy for nasopharyngeal carcinoma. Laryngoscope. 2006;116(9):1626‐1631. 10.1097/01.mlg.0000230435.71328.b9. [DOI] [PubMed] [Google Scholar]
- 2. Hachem RA, Elkhatib A, Beer‐Furlan A, Prevedello D, Carrau R. Reconstructive techniques in skull base surgery after resection of malignant lesions: a wide array of choices. Curr Opin Otolaryngol Head Neck Surg. 2016;24(2):91‐97. 10.1097/MOO.0000000000000233. [DOI] [PubMed] [Google Scholar]
- 3. Choi NY, Kim HJ, Baek CH. Surgical management of extensive osteoradionecrosis in nasopharyngeal carcinoma patients with the maxillary swing approach and free muscular flaps. Clin Otolaryngol. 2017;42(5):1100‐1104. 10.1111/coa.12866. [DOI] [PubMed] [Google Scholar]
- 4. Delanian S, Lefaix J‐L. The radiation‐induced fibroatrophic process: therapeutic perspective via the antioxidant pathway. Radiother Oncol. 2004;73:119‐131. [DOI] [PubMed] [Google Scholar]
- 5. Veyrat M, Verillaud B, Herman P, Bresson D. How I do it. The pedicled temporoparietal fascia flap for skull base reconstruction after endonasal endoscopic approaches. Acta Neurochir. 2016;158(12):2291‐2294. 10.1007/s00701-016-2969-z. [DOI] [PubMed] [Google Scholar]
- 6. Han P, Wang X, Liang F, et al. Osteoradionecrosis of the Skull Base in nasopharyngeal carcinoma: incidence and risk factors. Int J Radiat Oncol Biol Phys. 2018;102:552‐555. 10.1016/j.ijrobp.2018.06.027. [DOI] [PubMed] [Google Scholar]
- 7. Chapchay K, Weinberger J, Eliashar R, Adler N. Anterior Skull Base reconstruction following ablative surgery for osteoradionecrosis: case report and review of literature. Ann Otol Rhinol Laryngol. 2019;128:1134‐1140. 10.1177/0003489419865558. [DOI] [PubMed] [Google Scholar]
- 8. Liu J, Ning X, Sun X, Lu H, Gu Y, Wang D. Endoscopic sequestrectomy for skull base osteoradionecrosis in nasopharyngeal carcinoma patients: a 10‐year experience. Int J Clin Oncol. 2019;24(3):248‐255. 10.1007/s10147-018-1354-8. [DOI] [PubMed] [Google Scholar]
- 9. Huang WB, Wong STS, Chan JYW. Role of surgery in the treatment of osteoradionecrosis and its complications after radiotherapy for nasopharyngeal carcinoma. Head Neck. 2018;40(2):369‐376. 10.1002/hed.24973. [DOI] [PubMed] [Google Scholar]
- 10. Herle P, Shukla L, Morrison WA, Shayan R. Preoperative radiation and free flap outcomes for head and neck reconstruction: a systematic review and meta‐analysis. ANZ J Surg. 2015;85(3):121‐127. 10.1111/ans.12888. [DOI] [PubMed] [Google Scholar]
- 11. You R, Zou X, Hua Y‐J, et al. Salvage endoscopic nasopharyngectomy is superior to intensity‐modulated radiation therapy for local recurrence of selected T1‐T3 nasopharyngeal carcinoma—a case‐matched comparison. Radiother Oncol. 2015;115(3):399‐406. 10.1016/j.radonc.2015.04.024. [DOI] [PubMed] [Google Scholar]
- 12. Simo R, Robinson M, Lei M, Sibtain A, Hickey S. Nasopharyngeal carcinoma: United Kingdom National Multidisciplinary Guidelines. J Laryngol Otol. 2016;130(Suppl 2):S97‐S103. 10.1017/S0022215116000517. [DOI] [PMC free article] [PubMed] [Google Scholar]


