This cohort study assesses whether copy number variations are associated with specific phenotypes in patients with germline PTEN mutations.
Key Points
Question
Are copy number variations associated with specific clinical outcomes in patients with germline PTEN mutations?
Findings
In this cohort study of 481 patients with germline PTEN mutations, pathogenic and/or likely pathogenic copy number variations associated with neurodevelopmental disorders were found in 10.0% of patients with autism spectrum disorder and/or developmental delay. Pathogenic and/or likely pathogenic copy number variations were found in 2.6% of patients without autism spectrum disorder and/or developmental delay and 1.7% of patients with cancer.
Meaning
These findings suggest that copy number variations are associated with the autism spectrum disorder and/or developmental delay phenotype in patients with germline PTEN mutations.
Abstract
Importance
PTEN is among the most common autism spectrum disorder (ASD)–predisposition genes. Germline PTEN mutation carriers can develop malignant neoplasms and/or neurodevelopmental disorders such as ASD and developmental delay. Why a single gene contributes to disparate clinical outcomes, even in patients with identical PTEN mutations, remains unclear.
Objective
To investigate the association of copy number variations (CNVs), altered numbers of copies of DNA sequences within the genome, with specific phenotypes in patients with germline PTEN mutations.
Design, Setting, and Participants
This prospective cohort study examined genome-wide microarrays performed on blood-derived DNA to detect germline CNVs from September 1, 2005, through January 3, 2018. Multicenter accrual occurred from community and academic medical centers throughout North America, South America, Europe, Australia, and Asia. Participants included patients with PTEN hamartoma tumor syndrome (PHTS) (n = 481), molecularly defined as carrying germline pathogenic PTEN mutations. Data were analyzed from November 14, 2018, to August 1, 2019.
Exposures
Detection of CNVs from patient-derived germline DNA.
Main Outcomes and Measures
Prevalence of pathogenic and/or likely pathogenic CNVs in patients with PHTS and association with ASD/developmental delay and/or cancer, ascertained through medical records and pathology reports.
Results
The study included 481 patients with PHTS (mean [SD] age, 33.2 [21.6] years; 268 female [55.7%]). The analytic series consisted of 309 patients with PHTS and genetically determined European ancestry. Patients were divided into 3 phenotypic groups, excluding family members within each group. These include 110 patients with ASD/developmental delay, 194 without ASD/developmental delay, and 121 with cancer (of whom 116 were in the no ASD/developmental delay group). Genome-wide evaluation of autosomal CNVs indicated an increased CNV burden, particularly duplications in genic regions, in patients with ASD/developmental delay compared with those without ASD/developmental delay (odds ratio [OR], 1.9; 95% CI, 1.1-3.4; P = .03) and those with cancer (OR, 2.5; 95% CI, 1.3-4.6; P = .003). Eleven of the 110 patients (10.0%) with ASD/developmental delay carried pathogenic and/or likely pathogenic CNVs associated with neurodevelopmental disorders, compared with 5 of 194 (2.6%) without ASD/developmental delay (OR, 4.2; 95% CI, 1.4-13.7; P = .008) and 2 of 121 (1.7%) with cancer (OR, 6.6; 95% CI, 1.6-44.5; P = .007). Evidence of an association between pathogenic and/or likely pathogenic CNVs and PHTS with ASD/developmental delay was further supported in a validation series of 69 patients with PHTS of genetically determined non-European ancestry.
Conclusions and Relevance
These findings suggest that copy number variations are associated with the ASD/developmental delay clinical phenotype in PHTS, providing proof of principle for similarly heterogeneous disorders lacking outcome-specific associations.
Introduction
The triumph of using genetics in precision medicine is the ability to stratify individuals at very high risk of disease and thereby enact specific gene-informed medical management.1,2 In the case of heritable disease, genetics also allow testing of family members to determine with 100% accuracy whether they are at risk of disease. However, for any single individual carrying a mutation, we can estimate risk by probabilities but not with certainty. For example, a germline mutation in gene X may give an 80% lifetime risk of disease Y, but for the single patient with that germline mutation, the risk of developing disease Y will be 100% or 0%. Searching for genomic modifiers of heritable disease risk at the individual level in humans has proven challenging.1,3 This makes estimation of clinical outcomes difficult, especially for phenotypically variable disorders. As such, why a mutation in 1 particular gene predisposes to disparate clinical outcomes, including in patients with identical mutations, remains poorly understood.
PTEN germline mutations are among the most common causes of autism spectrum disorder (ASD), accounting for approximately 2% to 5% of cases,4,5 yet originally identified in a subset of relatively rare syndromes predisposing to breast, thyroid, and other cancers.6 The PTEN-related ASD-cancer phenotypic dichotomy and inability to preemptively estimate disease outcomes pose a challenge for more timely and precise clinical management. The concept of PTEN hamartoma tumor syndrome (PHTS [OMIM 158350]) was proposed to encompass any clinical disorder with germline PTEN mutation on molecular genetic testing, regardless of phenotype.7,8 Based on this broad clinical spectrum and unified genetic etiology, PHTS serves as a useful disease model to identify modifiers of variable heritable disease risk at the individual level.
Copy number variation (CNV), a common type of structural variation in the human genome, is considered an important contributor to nonsyndromic idiopathic ASD and sporadic cancer.9,10,11 Copy number variations have also been associated with complex disorders, particularly those involving developmental delay, intellectual disabilities, and/or congenital anomalies.12,13,14 As such, the purpose of this study was to address the hypothesis that specific CNV associations in patients carrying germline PTEN mutations are associated with development of specific clinical phenotypes at an individual level. Thus, we performed a genome-wide investigation of whether pathogenic and/or likely pathogenic CNVs may be associated with particular clinical outcomes in patients with germline PTEN mutations.
Methods
Patients
A total of 6782 patients were prospectively accrued from September 1, 2005, through January 3, 2018, and provided informed written consent to participate. This prospective cohort study was approved by the Cleveland Clinic institutional review board. This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline for cohort studies.
Inclusion criteria for enrollment included meeting at least the relaxed International Cowden Consortium operational diagnostic criteria, meaning full diagnostic criteria minus 1 feature, termed Cowdenlike syndrome15; having macrocephaly plus neurodevelopmental disorders (eg, ASD, developmental delay [DD], mental retardation) and/or penile freckling; or the presence of a known pathogenic germline PTEN mutation (patients referred to the PTEN Multidisciplinary Clinic at the Cleveland Clinic).16,17 These patients were broadly recruited from community and academic medical centers throughout North America, South America, Europe, Australia, and Asia, as noted by Tan et al.16,17 After informed consent was obtained, checklists to document the presence or absence of specific features were completed by specialist genetic counselors or physicians concurrently with withdrawal of blood specimen (team led by C.E., medical director, PTEN/Cowden Multidisciplinary Clinic, Center for Personalized Genetic Healthcare, Genomic Medicine Institute, Cleveland Clinic, Cleveland, Ohio). Specialist genetics staff reviewed all checklists and corresponded with the enrolling center if necessary to obtain further primary documentation of medical records and, for cancer, pathology reports, for phenotype confirmation with patient consent.16 For each consenting patient, we reviewed medical records, including pedigrees, clinical genetic testing reports, and clinical notes associated with genetics evaluations, ASD Diagnostic and Statistical Manual of Mental Disorders (Fourth Edition, Text Revision) criteria, and/or genetic counseling visits, where applicable. We followed up this cohort prospectively for development of phenotypic features.
PTEN Mutation and Deletion Analysis
All eligible patients underwent germline PTEN (NM_000314.8) mutation and deletion analysis. Genomic DNA was extracted from peripheral blood samples using standard protocols. Mutation analysis was standardly performed, with a combination of denaturing gradient gel electrophoresis, high-resolution melting curve analysis (Idaho Technology), and direct Sanger sequencing (ABI 3730xl; Applied Biosystems, Life Technologies).18 Deletion analysis using the multiplex ligation-dependent probe amplification assay was performed with the multiplex ligation-dependent probe amplification kit (P158; MRC-Holland) according to manufacturer protocol.18 All patients underwent polymerase chain reaction–based Sanger sequencing of the PTEN promoter region as previously described.18 Only cases with pathogenic or likely pathogenic germline PTEN mutations were included in the analytic sample. To be conservative, individuals with PTEN promoter variants were considered mutation positive only if the underlying variants had been previously associated with PHTS or known to affect PTEN function.16,17,19,20 Pathogenicity predictions were ascertained by reports from orthogonal testing in a Clinical Laboratory Improvement Amendments of 1988–certified facility, ClinVar database classifications, and/or the ClinGen gene-specific criteria for PTEN variant curation.21 The resultant data set represents, to our knowledge, the largest deeply phenotyped worldwide series of patients with PHTS from the International Cowden Consortium.15
Genotyping, CNV Calling, and Quality Control
We evaluated DNA quality (A260/A280) using spectrophotometry (NanoDrop 1000; Thermo Fisher Scientific) and quantity using a double-stranded DNA high-sensitivity assay kit (Qubit; Thermo Fisher Scientific). DNA samples were all genotyped on a commercially available genotyping array (Infinium Global Screening Array-24, version 1.0; Illumina) at the Broad Institute Genomic Services, Cambridge, Massachusetts. We used a total of 642 824 markers for quality control. To correct for population stratification, single-nucleotide polymorphism (SNP) genotype quality control was performed. We excluded samples with a call rate of less than 0.91 or with discordant sex. We focused on autosomal CNVs owing to higher fidelity of CNV calling compared with sex chromosomes.22 To perform principal component analysis to assess population stratification, we filtered autosomal SNPs with low genotyping rates (>0.98) and deviation from Hardy-Weinberg equilibrium (P ≤ .001) before pruning SNPs for linkage disequilibrium using default parameters in PLINK, version 1.927 (--indep-pairwise 200 100 0.2).23 We used the PennCNV algorithm24 to generate GC DNA nucleotide wave-adjusted log R ratio intensity files and to call CNVs in all samples. A custom population B-allele frequency file was generated before CNV calling. We merged adjacent CNV calls if the number of intervening markers was less than 20% of the total number than when both segments were combined. Next, we performed intensity-based quality control to exclude samples with low quality based on waviness factor, log R ratio SD, and B-allele frequency drift. These thresholds were calculated by taking the median plus 3 SD to identify outliers.25 After intensity-based quality control, all samples had a log R ratio SD of less than 0.25, an absolute waviness factor of less than 0.04, and a B-allele frequency drift of less than 0.007. We excluded samples with an excessively high CNV load (>100) as determined empirically by visual inspection of CNV distribution across a combined set of samples. None of the PHTS samples had a CNV load above this threshold (with a maximum of 16 CNVs detected in 1 patient). Finally, we excluded CNVs spanning less than 20 markers, CNVs of less than 20 Kb in length, CNVs with SNP density (number of markers/CNV length) of less than 0.0001, and/or CNVs with greater than 50% of total length overlapping artifactual regions in SNP-based CNV calling.26,27 The final data set consisted of 309 patients of genotype-determined European ancestry with at least 1 CNV call (eFigure 1 in the Supplement).
Genome-wide CNV Burden Analysis
We measured CNV burden among patients with PHTS and ASD and/or developmental delay (ASD/DD group), those without ASD or developmental delay (no ASD/DD group), and those with cancer. Genome-wide burden was also analyzed for only rare CNVs (excluding CNVs overlapping >80% of regions known to be recurrent in the general population28). Duplications and deletions were analyzed in combination as well as separately. Moreover, within each category (duplications and deletions), genic and nongenic CNVs were analyzed in combination as well as separately. For all comparisons, we counted the number of unrelated probands with such genomic events within each phenotype group.
CNV Annotation and Identification of Clinically Relevant CNVs
A CNV was considered as genic if it overlapped more than 80% of a gene29; otherwise it was annotated as nongenic. Cancer-relevant loci included 46 genes associated with Cowden syndrome component cancers,17 of which 24 are clinically actionable cancer-related genes according to the American College of Medical Genetics and Genomics guidelines.30,31 Genes associated with ASD were curated from the Simons Foundation Autism Research Initiative Gene module.32 Only syndromic (category S), high-confidence (category 1), and strong candidate (category 2) genes were retained. We also interrogated regions associated with genomic disorders, congenital malformations, and neurodevelopmental phenotypes, including 48 loci from DECIPHER (Database of Chromosomal Imbalance and Phenotype Using Ensembl Resources), 298 genes from the Developmental Disorders Genotype-Phenotype Database, and 92 loci of pathogenic CNVs from the UK Biobank.33,34,35,36,37 Pathogenicity and likely pathogenicity of previously unreported CNVs were estimated based on size and gene content according to the American College of Medical Genetics and Genomics guidelines.34 We used Human Phenotype Ontology terms for standard annotation of CNVs with associated phenotypic abnormalities.38
Statistical Analysis
Data were analyzed from November 14, 2018, to August 1, 2019. Patient demographic characteristics were reported by age, sex, and clinical phenotypes. OpenEpi software was used to calculate odds ratios (ORs) for burden and enrichment analyses. For analyses among different patient phenotype groups, 2 × 2 tables were used to calculate ORs. The 95% CIs and corresponding P values were calculated using the mid-P exact test. The nonparametric Mann-Whitney test was used to analyze CNV burden per individual among the different patient phenotype groups. All P values were 2-sided and considered to be significant at P < .05. We used Prism 8, version 8.1.1 (GraphPad) to generate box-and-whisker and forest plots.
Results
Patient Characteristics and PTEN Mutation Spectrum
At baseline, we prospectively accrued 481 patients with PHTS (mean [SD] age at consent, 33.2 [21.6] years; 268 female [55.7%] and 213 male [44.3%]) (eTable 1 in the Supplement). The Cleveland Clinic score, a quantitative surrogate of age-related PHTS disease burden,16 ranged from 0 to 69 (mean [SD], 20 [13]), corroborating the broad phenotypic spectrum, including participants with unexpectedly mild disease manifestations (eg, absence of early-onset component cancers and neurotypical development) despite their underlying pathogenic germline PTEN mutations. Patients with PHTS were stratified into 3 phenotypically ascertained groups, including the ASD/DD group, no ASD/DD group, and cancer group (a subset of the no ASD/DD group). We did not include a no cancer group owing to the inability to ascertain cancer diagnoses, particularly in pediatric, adolescent, and young adult patients. Importantly, the PTEN mutation spectra were similar across the 3 PHTS phenotype groups (eFigure 2 in the Supplement).
Genome-wide CNV Burden in Patients With PHTS
The analytic sample consisted of 309 patients with PHTS (Table 1) of genetically determined European ancestry (mean [SD] age at consent, 32.0 [21.0] years; 167 female [54.0%] and 142 male [46.0%]). Phenotypically ascertained groups consisted of 110 unrelated patients in the ASD/DD phenotype group, 194 unrelated patients in the no ASD/DD phenotype group, and a subset of 121 unrelated patients, including 116 in the no ASD/DD group, with cancer. To determine the genome-wide CNV burden, we quantified the total number of CNVs in each participant within the 3 PHTS phenotype groups (Figure 1A). Patients in the ASD/DD group had an overall increased CNV burden per individual (median, 3.5; range, 0-15) compared with those in the no ASD/DD group (median, 3.0; range, 0-13; Mann-Whitney 2-sided test comparing ranks, P = .04) and the subset with cancer (median, 2.0; range, 0-12; Mann-Whitney 2-sided test, P = .002). Similarly, patients in the ASD/DD group had an overall increased burden of rare CNVs per individual (median, 3.0; range, 0-14) compared with those in the no ASD/DD group (median, 2.0; range, 0-12; Mann-Whitney 2-sided test comparing ranks, P = .01) and the subset with cancer (median, 2.0; range, 0-10; Mann-Whitney 2-sided test, P < .001). No difference was observed in CNV burden among patients in the no ASD/DD group (median, 3.0; range, 0-13) compared with the subset with cancer (median, 2.0; range, 0-12; Mann-Whitney 2-sided test, P = .15). Similarly, no difference was observed in rare CNV burden among patients in the no ASD/DD group (median, 2.0; range, 0-12) compared with the subset with cancer (median, 2.0; range, 0-10; Mann-Whitney 2-sided test, P = .19). Stratified analyses according to CNV type and genomic locus revealed that patients in the ASD/DD group had a significant enrichment of duplications in genic regions (Figure 1B), compared with patients in the no ASD/DD group (OR, 1.9; 95% CI, 1.1-3.4; P = .03) and the subset with cancer (OR, 2.5; 95% CI, 1.3-4.6; P = .003).
Table 1. Clinical Characteristics of the Analytic Series of 309 Patients With PHTS and European Ancestry.
| Clinical Phenotypic Characteristics | Data |
|---|---|
| Sex, No. (%) | |
| Female | 167 (54.0) |
| Male | 142 (46.0) |
| Age at consent, mean (SD) [range], y | 32 (21) [1-85] |
| No. of germline PTEN mutations | |
| Promoter | 8 |
| Missense | 99 |
| Nonsense | 86 |
| Splice site | 28 |
| Frameshift truncating | 63 |
| Insertions and deletions | 25 |
| Neurodevelopmental features, No. (%) | 110 (35.6) |
| Autism spectrum disorder | 45 (14.6) |
| Global developmental delay | 56 (18.1) |
| Variable delay | 25 (8.1) |
| Mental retardation | 9 (2.9) |
| Learning disabilities | 9 (2.9) |
| Cancer, No. (%)a | 130 (42.1) |
| PHTS component malignant neoplasms, No. (%) | |
| Breast cancer | 58 (18.8) |
| Thyroid cancer | 36 (11.7) |
| Renal cell cancer | 25 (8.1) |
| Endometrial cancer | 27 (8.7) |
| Colon cancer | 10 (3.2) |
| Melanoma | 10 (3.2) |
| Nonmalignant features, No. (%)b | 78 (25.2) |
| Macrocephaly | 70 (22.7) |
| Dermatologic featuresc | 42 (13.6) |
| Arteriovenous malformations | 10 (3.2) |
| Hemangiomas | 13 (4.2) |
| Polyposis | 38 (12.3) |
| Benign breast featuresd | 21 (6.8) |
| Benign thyroid featurese | 49 (15.9) |
| Lhermitte-Duclos disease | 9 (2.9) |
Abbreviation: PHTS, PTEN hamartoma tumor syndrome.
Includes 9 patients with neurodevelopmental disorders who have also been diagnosed with cancer.
Includes patients without a personal history of neurodevelopmental disorders or cancer at the time of the last clinical visit and/or follow-up.
Includes trichilemmoma, acral keratosis, papillomatous papules, and genital lentiginosis (penile freckling in males).
Includes breast fibroadenoma, fibrocystic breast disease, breast papilloma, breast hamartoma, atypical ductal hyperplasia, and typical ductal hyperplasia.
Includes thyroid nodules, goiter, and Hashimoto thyroiditis.
Figure 1. Genome-wide Copy Number Variation (CNV) Landscape Showing Phenotype-Specific Associations in PTEN Hamartoma Tumor Syndrome (PHTS).
A, Genome-wide CNV burden representing the total number of CNVs in each patient within the 3 PHTS phenotype groups. The line in the middle of each box is plotted at the median. Each box extends from the 25th to 75th percentiles (interquartile range [IQR]). Whiskers and outliers (circles) are plotted according to the Tukey method. The upper whiskers extend to the largest value no further than 1.5 times the IQR. The lower whiskers extend to the smallest value no further than 1.5 times the IQR. B, Stratified analyses showing CNV burden (duplications and deletions) in genic and nongenic genomic regions, accounted for by the number of unrelated patients carrying such CNVs within each clinical phenotype group. The size of each box is proportional to the respective odds ratio (OR) depicted in the adjacent table. ASD indicates autism spectrum disorder; DD, developmental delay.
Clinically Relevant CNVs in Patients With PHTS
We identified 3 of 309 patients with PHTS (1.07%) and pathogenic and/or likely pathogenic CNVs affecting genes associated with PTEN-related cancers17 or other inherited cancer syndromes according to the American College of Medical Genetics and Genomics guidelines.30,31 These included 2 BMPR1A (OMIM 601299) deletions and 1 BRCA1 (OMIM 113705) deletion. We could not ascertain cancer diagnoses because all 3 CNV carriers were children or young adults (aged 3, 6, and 21 years) without a personal history of cancer at the time of consent (eTable 2 in the Supplement). The 2 patients with PHTS and BMPR1A deletions upstream of their individual PTEN deletion had juvenile polyposis, as is often observed in chromosome 10q23 microdeletions involving both genes (OMIM 612242). Notably, no pathogenic and/or likely pathogenic CNVs involving known cancer-associated genes were identified among patients in the subset with cancer.
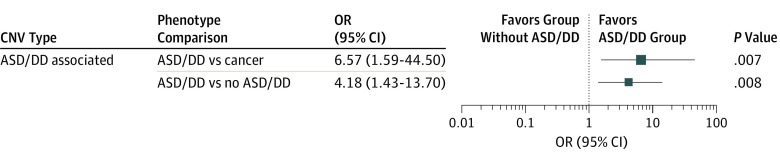
We then investigated pathogenic and/or likely pathogenic CNVs involving genes implicated in the etiology of idiopathic nonsyndromic and syndromic ASD/developmental delay and/or neurodevelopmental disorders as well as known pathogenic CNVs associated with ASD, developmental delay, and neurodevelopmental disorders. We found 11 of 110 patients in the ASD/DD group (10.0%) harbored such pathogenic and/or likely pathogenic CNVs, compared with 5 of 194 patients in the no ASD/DD group (2.6%) (OR, 4.2; 95% CI, 1.4-13.7; P = .008) and 2 of 121 (1.7%) patients in the subset with cancer (OR, 6.6; 95% CI, 1.6-44.5; P = .007) (Figure 2). The CNV carriers included 10 male and 6 female patients with PHTS (mean [SD] age at consent, 22 [22.1] years). The CNVs included genomic loci associated with other genomic syndromes with overlapping clinical features, such as chromosome 8p23.1 duplication syndrome and chromosome 1q21.1 thrombocytopenia-absent radius syndrome (Table 2 and Table 3).
Figure 2. Enrichment of Clinically Relevant Copy Number Variations (CNVs) in Patients With PTEN Hamartoma Tumor Syndrome (PHTS) and Autism Spectrum Disorder/Developmental Delay (ASD/DD).
Pathogenic and/or likely pathogenic CNVs associated with neurodevelopmental disorders were found in 11 of 110 patients in the ASD/DD group (10.0%), 5 of 194 patients in the no ASD/DD group (2.6%), and 2 of 121 patients in the subgroup with cancer (1.7%). The size of each box is proportional to the respective odds ratio (OR) depicted in the adjacent table.
Table 2. Pathogenic and Likely Pathogenic CNVs Associated With Neurodevelopmental Disorders.
| Patient Identification | Phenotype Group | CNV (Size) | Genomic Coordinates (hg19) | Associated Genes | SFARI Gene Score | Associated Source or Genomic Syndromes | Related Human Phenotype Ontology |
|---|---|---|---|---|---|---|---|
| CCF00105 | ASD/DD | 4p16.1 dup (3.3 Mb) | chr4:5064533-8381168 | JAKMIP1 | NA | Smith-Magenis syndrome-like (OMIM 611195; ClinVar VCV000254206.1) | HP:0001249, intellectual disability; HP:0001263, global DD |
| CCF00301 | ASD/DD | 22q11.21 del (133 Kb) | chr22:18875445-19008424 | PRODH | Strong candidate, syndromic | PMID: 29895855 | HP:0001249, intellectual disability; HP:0000729, autistic behavior; HP:0001263, global DD |
| CCF00547 | ASD/DD | 10q23.2 del (4.8 Mb) | chr10:85624500-90412968 | GRID1 | Strong candidate | 10q23.2 Deletion syndrome | HP:0000256, macrocephaly; HP:0000717, autism; HP:0001263, global DD; HP:0001249, intellectual disability; HP:0200008, intestinal polyposis |
| 6p12.1 dup (354 Kb) | chr6:56566691-56920804 | KIAA1586 | Strong candidate | NA | NA | ||
| CCF03028 | ASD/DD | 10q23.2 del (3.3 Mb) | chr10:87976544-91250370 | GRID1 | Strong candidate | 10q23.2-q23.31 Deletion syndrome | HP:0000256, macrocephaly; HP:0000717, autism; HP:0001263, global DD; HP:0001249, intellectual disability; HP:0200008, intestinal polyposis |
| CCF05681 | ASD/DD | 15q13.3 dup (490 Kb) | chr15:32025034-32515100 | CHRNA7 | Strong candidate | 15q13.3 Duplication syndrome | HP:0003829, incomplete penetrance; HP:0000256, macrocephaly; HP:0000717, autism; HP:0001263, global DD |
| CCF06601 | ASD/DD | 15q11.2 dup (154 Kb) | chr15:22839023-22993121 | CYFIP1 | Strong candidate | NA | NA |
| CCF08207 | ASD/DD | 15q11.2 del (916 Kb) | chr15:22310511-23226254 | CYFIP1 | Strong candidate | 15q11.2 Deletion syndrome (OMIM 615656) | HP:0001249, intellectual disability; HP:0000729, autistic behavior; HP:0001263, global DD |
| CCF11952 | ASD/DD | 15q11.1-q11.2 dup (3 Mb) | chr15:20263192-23242837 | CYFIP1 | Strong candidate | NA | NA |
| CCF07685 | ASD/DD | 2q13 del (130 Kb) | chr2:110852875-110983320 | NPHP1 | NA | PMID: 29895855 | HP:0001249, intellectual disability |
| CCF08084 | ASD/DD | 2p12 dup (355 Kb) | chr2:80673046-81027675 | CTNNA2 | Syndromic | NA | HP:0001263, global DD; HP:0001321, cerebellar hypoplasia; HP:0001302, pachygyria |
| CCF10918 | ASD/DD | 8p23.1 dup (3.8 Mb) | chr8:8092788-11895164 | PINX1 | NA | 8p23.1 Duplication syndrome (DECIPHER) | HP:0001263, global DD; HP:0001249, intellectual disability; HP:0000846, adrenal insufficiency |
| CCF05270 | No ASD/DD | 2q13 del (130 Kb) | chr2:110852875-110983320 | NPHP1 | NA | PMID: 29895855 | HP:0001249, intellectual disability |
| CCF13078 | No ASD/DD | 15q13.3 dup (450 Kb) | chr15:32065095-32515100 | CHRNA7 | Strong candidate | 15q13.3 Duplication syndrome | HP:0003829, incomplete penetrance; HP:0000256, macrocephaly; HP:0000717, autism; HP:0001263, global DD |
| CCF13466 | No ASD/DD | 1q21.1 del (356 Kb) | chr1:145383239-145738979 | TAR region | NA | 1q21.1 TAR deletion syndrome (OMIM 274000, DECIPHER) | HP:0006101, finger syndactyly; HP:0001263, global DD; HP:0001249, intellectual disability; HP:0007413, nevus flammeus localized in the skin of the forehead |
| CCF01879 | No ASD/DD (cancer) | 2q13 del (130 Kb) | chr2:110852875-110983320 | NPHP1 | NA | PMID: 29895855 | HP:0001249, intellectual disability |
| 11p15.4 del (47.5 Kb) | chr11:4530773-4578227 | OR52M1 | Strong candidate | NA | NA | ||
| CCF04392 | No ASD/DD (cancer) | 3p21.1 del (997 Kb) | chr3:53414424-54411844 | CACNA2D3, CACNA1D | Strong candidate | NA | HP:0001263, global DD; HP:0010864, intellectual disability, severe |
Abbreviations: ASD, autism spectrum disorder; CNV, copy number variation; DD, developmental delay; DECIPHER, Database of Chromosomal Imbalance and Phenotype Using Ensembl Resources; del, deletion; dup, duplication; NA, not applicable; OMIM, Online Mendelian Inheritance in Man; PMID, PubMed identification number; TAR, thrombocytopenia-absent radius.
Table 3. Clinical Features of Patients With PHTS and Pathogenic and Likely-Pathogenic CNVs.
| Patient Identification | Germline PTEN Mutationa | Phenotype Group | Sex | Neurodevelopmental and Cognitive Features | Other Clinical Features |
|---|---|---|---|---|---|
| CCF00105 | p.Lys164Argfs*3 | ASD/DD | Male | Intellectual disability | Thyroid cancer (7 y of age), renal cell cancer (21 y of age), benign skin neoplasm, acral keratoses, trichilemmoma, lipoma, arteriovenous malformation, thyroid nodule |
| CCF00301 | p.Met239Thr | ASD/DD | Male | Intellectual disability | Macrocephaly |
| CCF00547 | Whole gene deletion | ASD/DD | Male | Global DD | Macrocephaly, dysmorphic features, epilepsy, juvenile polyps, tan macules on glans penis and penile shaft, cryptorchidism, mild chordee |
| CCF03028 | Whole gene deletion | ASD/DD | Male | Mental retardation | Macrocephaly, dysmorphic features, juvenile polyposis syndrome, GI polyps, arteriovenous malformation, oral mucosa papilloma, tan macules on glans penis and penile shaft |
| CCF05681 | p.Leu139Phe | ASD/DD | Male | ASD, global DD | Macrocephaly, dysmorphic features, café-au-lait spots |
| CCF06601 | p.Ala39Thr | ASD/DD | Male | ASD, global DD | Macrocephaly, isolated hemihyperplasia, skin tag |
| CCF08207 | p.Cys136Arg | ASD/DD | Female | Variable delay | Macrocephaly, oral mucosa papilloma, lobular breast carcinoma in situ (44 y of age), benign breast disease, goiter, ovarian cysts, skin tag |
| CCF11952 | p.Arg130* | ASD/DD | Male | Global DD | Macrocephaly, hemangioma, lipoma |
| CCF07685 | p.Asn12Thr | ASD/DD | Male | Global DD | Macrocephaly, dysmorphic features |
| CCF08084 | p.Tyr68Cys | ASD/DD | Female | Global DD, anxiety disorder | Macrocephaly and dolicocephaly, café-au-lait spots, ventriculomegaly, Rathke cleft cyst, skin thickening |
| CCF10918 | p.Thr319Asnfs*6 | ASD/DD | Female | Mental retardation, global DD | Macrocephaly, dysmorphic features, hirsutism |
| CCF05270 | p.Gly129Glu | No ASD/DD | Female | NA | Macrocephaly, GI polyps, arteriovenous malformation, benign breast disease, colon lipoma, glycogenic acanthosis, goiter, skin tag |
| CCF13078 | p.Thr319* | No ASD/DD | Female | NA | Macrocephaly, GI polyps, benign neurologic neoplasms, benign breast disease, lipoma, neoplasms in vascular tissue, skin papilloma, thyroid nodule |
| CCF13466 | p.Arg335* | No ASD/DD | Male | NA | Macrocephaly and dolicocephaly, Chiari malformation type I, syndactyly (toes 2 and 3), papillomatous papules, multiple melanocytic nevi, nevus flammeus of face, epidermal nevus |
| CCF01879 | p.Arg335* | No ASD/DD (cancer) | Male | NA | Macrocephaly, thyroid cancer (69 y of age), GI polyps, angiolipoma, lipoma, basal cell carcinoma, benign neoplasm of skin, goiter, oral mucosa papilloma, skin papilloma, trichilemmoma |
| CCF04392 | p.Arg233* | No ASD/DD (cancer) | Female | NA | Macrocephaly, thyroid cancer (42 y of age), breast cancer (44 y of age), lobular carcinoma in situ of breast, benign breast disease, benign neoplasm of skin, benign neurologic neoplasms, dermal fibroma, Hashimoto thyroiditis, lipoma |
Abbreviations: ASD, autism spectrum disorder; CNV, copy number variation; DD, developmental delay; GI, gastrointestinal; NA, not applicable; PHTS, PTEN hamartoma tumor syndrome.
All mutations have been reported in ClinVar as pathogenic except for 2 unreported mutations (p.Met239Thr and p.Ala39Thr).
Discussion
The present study evaluated the association of CNVs with clinical outcomes, specifically cancer vs ASD/DD, in individuals with germline pathogenic PTEN mutations. We found that patients with PHTS and ASD/DD have an overall increased genome-wide CNV burden per individual and an enrichment of clinically relevant CNVs when compared with the subset of patients with cancer and those without ASD/DD. These data appear to provide proof of principle that CNVs may act as genomic modifiers of disease risk in phenotypically heterogeneous hereditary disorders such as PHTS.
As many as 23% of patients with PHTS develop ASD/DD.16 Conversely, 2% to 5% of unselected patients with ASD/DD and as many as 50% of children with ASD and macrocephaly have been found to carry germline PTEN mutations.39 As such, PTEN itself is a syndromic autism gene with well-established roles in nervous system development and neuronal function.40 However, why more than 75% of PTEN mutation carriers do not develop ASD/DD remains a clinical conundrum. Our findings suggest pathogenic and likely pathogenic CNVs are associated with ASD/DD risk regardless of the particular coexisting germline PTEN mutation. Autism spectrum disorder is believed to be a highly heritable disorder, with complex genetic and biological bases.41,42,43 Pathogenic CNVs have been identified in 8% to 21% of individuals with idiopathic ASD, with higher frequencies reported in more severe cases, including causing syndromic ASD.9,44,45 Notably, particular pathogenic CNVs have also been identified in neurotypical control individuals, including unaffected family members, albeit with significantly lower frequencies.46 First, this observation corroborates the incomplete penetrance and extreme variability in expression of the associated CNVs, meaning that not all carriers will manifest the associated clinical features. Second, this observation supports the burgeoning hypothesis that ASD etiology and severity are modulated through additive effects of multiple genomic aberrations, the so-called 2-hit (or multiple-hit) model.47,48,49 These characteristics are highly relevant in the context of modifiers within an inherently predisposed genetic background. In the case of PHTS, we found evidence for the association of pathogenic CNVs with the coexisting germline PTEN mutations to favor ASD/DD clinical outcomes.
For example, we identified CNVs involving CYFIP1 (OMIM 606322) in 3 unrelated patients with PHTS in the ASD/DD group. CYFIP1 encodes cytoplasmic FMR1-interacting protein 1, a protein originally found to interact with fragile X mental retardation protein.50 Increased CYFIP1 dosage has been shown to cause aberrant neuronal cellular and dendritic morphologic features and to be associated with ASD in humans and murine model organisms.51,52 Importantly, CYFIP1 expression was inversely correlated with PTEN expression levels, with concomitant dysregulation of mammalian target of rapamycin (mTOR) signaling,51 suggesting that such CNVs may represent a second hit for patients with PHTS already harboring deleterious PTEN mutations that upregulate AKT-mTOR signaling. In cases of CYFIP1 duplications, decreased PTEN protein levels could also affect wild-type PTEN. In the context of CYFIP1 deletion, as was observed for 1 of the 3 patients with PHTS and CNVs involving CYFIP1 in this study, increased levels of a mutant PTEN protein may result in dominant negative effects,53 inhibiting wild-type PTEN and hence exacerbating the condition.
Notwithstanding the association of CNVs with multiple neurodevelopmental disorders, CNVs have also been implicated in the etiology of neuropsychiatric diseases such as epilepsy, schizophrenia, and bipolar disorder.11,29,54,55 A broad spectrum of neuropsychiatric phenotypes has been observed in patients with PHTS ranging from normal development and intelligence to severely debilitating neurocognitive and motor aberrations, including generalized anxiety, adult-onset movement disorders, obsessive-compulsive disorder, and psychosis.56,57 Whether particular CNVs affect the spectrum or severity of such motor and/or neurocognitive disease manifestations in PHTS warrants further scrutiny in larger independent prospective series.
Limitations
One limitation of this study is the relatively small sample size of patients within each phenotype group, owing to the rarity of PHTS, despite our cohort being the largest globally to our knowledge. Cowden syndrome, the most common component disorder in PHTS, is estimated to have a prevalence of 1 per 200 000 individuals.58 This precludes us from performing in-depth analyses, such as the association of particular CNVs with specific phenotypes or severity of manifestations within the ASD/DD group. Another limitation is the absence of a large independent replication sample to ascertain our findings. We therefore attempted a minivalidation by analyzing 69 genetically determined non-European patients with PHTS excluded from the above presented data to control for population stratification (eTable 3 in the Supplement). We similarly found that 3 of 28 patients in the ASD/DD group (10.7%) carried pathogenic and/or likely pathogenic CNVs compared with 1 of 41 patients in the no ASD/DD group (2.4%) (eTable 4 in the Supplement). The clinical relevance of increased duplications in genic regions in the ASD/DD group compared with the no ASD/DD group remains unanswered. Other loci may be implicated in the etiology of ASD/developmental delay in PHTS, and therefore the extent of CNVs in our study is likely an underestimate through the conservative inclusion of only pathogenic and/or likely pathogenic CNVs in this study.
Conclusions
The identification of testable clinically relevant genomic modifiers in PHTS is important for risk stratification and serves as proof of principle for other phenotypically variable disorders. Patients with PHTS and ASD/DD have an increased burden of pathogenic and/or likely pathogenic CNVs associated with neurodevelopmental disorders. Although CNV analysis is indicated as a first-tier clinical diagnostic test for patients with unexplained ASD/DD,13 it is not standard to test for such genomic alterations in the setting of an established diagnosis with a syndromic high-penetrance mendelian gene such as PTEN. Copy number variation analysis on immediate identification of germline PTEN mutation in infants and children may be beneficial. The presence of pathogenic and/or likely pathogenic CNVs in PHTS would suggest high likelihood of ASD/neurodevelopmental delay, leading to timely referral to formal evaluation and, if the results are positive, subsequent therapy. The earlier such interventions are instituted, the better the outcomes.
eFigure 1. Workflow for CNV Discovery, Quality Control, and Downstream Analyses
eFigure 2. PTEN Mutation Spectra Across the 3 PHTS Clinical Phenotype Groups
eTable 1. Demographic and Clinical Characteristics of 481 PHTS Patients
eTable 2. Patients With PHTS and Germline Pathogenic and Likely Pathogenic CNVs in Cancer-Predisposing Genes
eTable 3. Demographic and Clinical Characteristics of 69 Patients With PHTS of Non-European Ancestry
eTable 4. Pathogenic and Likely Pathogenic CNVs Identified in Patients With PHTS of Non-European Ancestry
References
- 1.Topol EJ. Individualized medicine from prewomb to tomb. Cell. 2014;157(1):-. doi: 10.1016/j.cell.2014.02.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Eichler EE. Genetic variation, comparative genomics, and the diagnosis of disease. N Engl J Med. 2019;381(1):64-74. doi: 10.1056/NEJMra1809315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Riordan JD, Nadeau JH. From peas to disease: modifier genes, network resilience, and the genetics of health. Am J Hum Genet. 2017;101(2):177-191. doi: 10.1016/j.ajhg.2017.06.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Butler MG, Dasouki MJ, Zhou XP, et al. . Subset of individuals with autism spectrum disorders and extreme macrocephaly associated with germline PTEN tumour suppressor gene mutations. J Med Genet. 2005;42(4):318-321. doi: 10.1136/jmg.2004.024646 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fernandez BA, Scherer SW. Syndromic autism spectrum disorders: moving from a clinically defined to a molecularly defined approach. Dialogues Clin Neurosci. 2017;19(4):353-371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Liaw D, Marsh DJ, Li J, et al. . Germline mutations of the PTEN gene in Cowden disease, an inherited breast and thyroid cancer syndrome. Nat Genet. 1997;16(1):64-67. doi: 10.1038/ng0597-64 [DOI] [PubMed] [Google Scholar]
- 7.Marsh DJ, Kum JB, Lunetta KL, et al. . PTEN mutation spectrum and genotype-phenotype correlations in Bannayan-Riley-Ruvalcaba syndrome suggest a single entity with Cowden syndrome. Hum Mol Genet. 1999;8(8):1461-1472. doi: 10.1093/hmg/8.8.1461 [DOI] [PubMed] [Google Scholar]
- 8.Eng C. PTEN hamartoma tumor syndrome GeneReviews. https://www.ncbi.nlm.nih.gov/books/NBK1488/. Updated June 2, 2016. Accessed August 6, 2019.
- 9.Jeste SS, Geschwind DH. Disentangling the heterogeneity of autism spectrum disorder through genetic findings. Nat Rev Neurol. 2014;10(2):74-81. doi: 10.1038/nrneurol.2013.278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Huang KL, Mashl RJ, Wu Y, et al. ; Cancer Genome Atlas Research Network . Pathogenic germline variants in 10,389 adult cancers. Cell. 2018;173(2):355-370.e14. doi: 10.1016/j.cell.2018.03.039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Takumi T, Tamada K. CNV biology in neurodevelopmental disorders. Curr Opin Neurobiol. 2018;48:183-192. doi: 10.1016/j.conb.2017.12.004 [DOI] [PubMed] [Google Scholar]
- 12.Lupski JR. Genomic disorders: structural features of the genome can lead to DNA rearrangements and human disease traits. Trends Genet. 1998;14(10):417-422. doi: 10.1016/S0168-9525(98)01555-8 [DOI] [PubMed] [Google Scholar]
- 13.Miller DT, Adam MP, Aradhya S, et al. . Consensus statement: chromosomal microarray is a first-tier clinical diagnostic test for individuals with developmental disabilities or congenital anomalies. Am J Hum Genet. 2010;86(5):749-764. doi: 10.1016/j.ajhg.2010.04.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cooper GM, Coe BP, Girirajan S, et al. . A copy number variation morbidity map of developmental delay. Nat Genet. 2011;43(9):838-846. doi: 10.1038/ng.909 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Eng C. Will the real Cowden syndrome please stand up: revised diagnostic criteria. J Med Genet. 2000;37(11):828-830. doi: 10.1136/jmg.37.11.828 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tan MH, Mester J, Peterson C, et al. . A clinical scoring system for selection of patients for PTEN mutation testing is proposed on the basis of a prospective study of 3042 probands. Am J Hum Genet. 2011;88(1):42-56. doi: 10.1016/j.ajhg.2010.11.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tan MH, Mester JL, Ngeow J, Rybicki LA, Orloff MS, Eng C. Lifetime cancer risks in individuals with germline PTEN mutations. Clin Cancer Res. 2012;18(2):400-407. doi: 10.1158/1078-0432.CCR-11-2283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ngeow J, Stanuch K, Mester JL, Barnholtz-Sloan JS, Eng C. Second malignant neoplasms in patients with Cowden syndrome with underlying germline PTEN mutations. J Clin Oncol. 2014;32(17):1818-1824. doi: 10.1200/JCO.2013.53.6656 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Teresi RE, Zbuk KM, Pezzolesi MG, Waite KA, Eng C. Cowden syndrome-affected patients with PTEN promoter mutations demonstrate abnormal protein translation. Am J Hum Genet. 2007;81(4):756-767. doi: 10.1086/521051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wang Y, Romigh T, He X, et al. . Differential regulation of PTEN expression by androgen receptor in prostate and breast cancers. Oncogene. 2011;30(42):4327-4338. doi: 10.1038/onc.2011.144 [DOI] [PubMed] [Google Scholar]
- 21.Mester JL, Ghosh R, Pesaran T, et al. . Gene-specific criteria for PTEN variant curation: recommendations from the ClinGen PTEN Expert Panel. Hum Mutat. 2018;39(11):1581-1592. doi: 10.1002/humu.23636 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pinto D, Darvishi K, Shi X, et al. . Comprehensive assessment of array-based platforms and calling algorithms for detection of copy number variants. Nat Biotechnol. 2011;29(6):512-520. doi: 10.1038/nbt.1852 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chang CC, Chow CC, Tellier LC, Vattikuti S, Purcell SM, Lee JJ. Second-generation PLINK: rising to the challenge of larger and richer datasets. Gigascience. 2015;4:7. doi: 10.1186/s13742-015-0047-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wang K, Li M, Hadley D, et al. . PennCNV: an integrated hidden Markov model designed for high-resolution copy number variation detection in whole-genome SNP genotyping data. Genome Res. 2007;17(11):1665-1674. doi: 10.1101/gr.6861907 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Huang AY, Yu D, Davis LK, et al. ; Tourette Syndrome Association International Consortium for Genetics (TSAICG); Gilles de la Tourette Syndrome GWAS Replication Initiative (GGRI) . Rare copy number variants in NRXN1 and CNTN6 increase risk for Tourette syndrome. Neuron. 2017;94(6):1101-1111.e7. doi: 10.1016/j.neuron.2017.06.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Marshall CR, Howrigan DP, Merico D, et al. ; Psychosis Endophenotypes International Consortium; CNV and Schizophrenia Working Groups of the Psychiatric Genomics Consortium . Contribution of copy number variants to schizophrenia from a genome-wide study of 41,321 subjects. Nat Genet. 2017;49(1):27-35. doi: 10.1038/ng.3725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Niestroj L-M, Howrigan DP, Perez-Palma E, et al. . Evaluation of copy number burden in specific epilepsy types from a genome-wide study of 18,564 subjects [published online May 27, 2019]. bioRxiv. doi: 10.1101/651299 [DOI] [Google Scholar]
- 28.The Centre for Applied Genomics. Database of genomic variants. http://dgv.tcag.ca/dgv/app/home. Accessed January 9, 2020.
- 29.Coppola A, Cellini E, Stamberger H, et al. ; EuroEPINOMICS-RES Consortium; EpiCNV Consortium . Diagnostic implications of genetic copy number variation in epilepsy plus. Epilepsia. 2019;60(4):689-706. doi: 10.1111/epi.14683 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Green RC, Berg JS, Grody WW, et al. ; American College of Medical Genetics and Genomics . ACMG recommendations for reporting of incidental findings in clinical exome and genome sequencing. Genet Med. 2013;15(7):565-574. doi: 10.1038/gim.2013.73 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yehia L, Ni Y, Sesock K, et al. . Unexpected cancer-predisposition gene variants in Cowden syndrome and Bannayan-Riley-Ruvalcaba syndrome patients without underlying germline PTEN mutations. PLoS Genet. 2018;14(4):e1007352. doi: 10.1371/journal.pgen.1007352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.SFARI Gene. https://gene.sfari.org. Updated June 20, 2019. Accessed November 26, 2019.
- 33.Firth HV, Richards SM, Bevan AP, et al. . DECIPHER: Database of Chromosomal Imbalance and Phenotype in Humans Using Ensembl Resources. Am J Hum Genet. 2009;84(4):524-533. doi: 10.1016/j.ajhg.2009.03.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kearney HM, Thorland EC, Brown KK, Quintero-Rivera F, South ST; Working Group of the American College of Medical Genetics Laboratory Quality Assurance Committee . American College of Medical Genetics standards and guidelines for interpretation and reporting of postnatal constitutional copy number variants. Genet Med. 2011;13(7):680-685. doi: 10.1097/GIM.0b013e3182217a3a [DOI] [PubMed] [Google Scholar]
- 35.Carvill GL, Mefford HC. Microdeletion syndromes. Curr Opin Genet Dev. 2013;23(3):232-239. doi: 10.1016/j.gde.2013.03.004 [DOI] [PubMed] [Google Scholar]
- 36.Deciphering Developmental Disorders Study Prevalence and architecture of de novo mutations in developmental disorders. Nature. 2017;542(7642):433-438. doi: 10.1038/nature21062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Crawford K, Bracher-Smith M, Owen D, et al. . Medical consequences of pathogenic CNVs in adults: analysis of the UK Biobank. J Med Genet. 2019;56(3):131-138. doi: 10.1136/jmedgenet-2018-105477 [DOI] [PubMed] [Google Scholar]
- 38.The Human Phenotype Ontology. https://hpo.jax.org/app/. Updated November 8, 2019. Accessed August 9, 2019.
- 39.Hansen-Kiss E, Beinkampen S, Adler B, et al. . A retrospective chart review of the features of PTEN hamartoma tumour syndrome in children. J Med Genet. 2017;54(7):471-478. doi: 10.1136/jmedgenet-2016-104484 [DOI] [PubMed] [Google Scholar]
- 40.Tilot AK, Frazier TW II, Eng C. Balancing proliferation and connectivity in PTEN-associated autism spectrum disorder. Neurotherapeutics. 2015;12(3):609-619. doi: 10.1007/s13311-015-0356-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chen JA, Peñagarikano O, Belgard TG, Swarup V, Geschwind DH. The emerging picture of autism spectrum disorder: genetics and pathology. Annu Rev Pathol. 2015;10:111-144. doi: 10.1146/annurev-pathol-012414-040405 [DOI] [PubMed] [Google Scholar]
- 42.Tick B, Bolton P, Happé F, Rutter M, Rijsdijk F. Heritability of autism spectrum disorders: a meta-analysis of twin studies. J Child Psychol Psychiatry. 2016;57(5):585-595. doi: 10.1111/jcpp.12499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bourgeron T. Current knowledge on the genetics of autism and propositions for future research. C R Biol. 2016;339(7-8):300-307. doi: 10.1016/j.crvi.2016.05.004 [DOI] [PubMed] [Google Scholar]
- 44.Schaefer GB, Mendelsohn NJ; Professional Practice and Guidelines Committee . Clinical genetics evaluation in identifying the etiology of autism spectrum disorders: 2013 guideline revisions. Genet Med. 2013;15(5):399-407. doi: 10.1038/gim.2013.32 [DOI] [PubMed] [Google Scholar]
- 45.Napoli E, Russo S, Casula L, et al. . Array-CGH analysis in a cohort of phenotypically well-characterized individuals with “essential” autism spectrum disorders. J Autism Dev Disord. 2018;48(2):442-449. doi: 10.1007/s10803-017-3329-4 [DOI] [PubMed] [Google Scholar]
- 46.Heil KM, Schaaf CP. The genetics of autism spectrum disorders—a guide for clinicians. Curr Psychiatry Rep. 2013;15(1):334. doi: 10.1007/s11920-012-0334-3 [DOI] [PubMed] [Google Scholar]
- 47.Girirajan S, Rosenfeld JA, Cooper GM, et al. . A recurrent 16p12.1 microdeletion supports a two-hit model for severe developmental delay. Nat Genet. 2010;42(3):203-209. doi: 10.1038/ng.534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Demily C, Lesca G, Poisson A, et al. . Additive effect of variably penetrant 22q11.2 duplication and pathogenic mutations in autism spectrum disorder: to which extent does the tree hide the forest? J Autism Dev Disord. 2018;48(8):2886-2889. doi: 10.1007/s10803-018-3552-7 [DOI] [PubMed] [Google Scholar]
- 49.Pizzo L, Jensen M, Polyak A, et al. . Rare variants in the genetic background modulate cognitive and developmental phenotypes in individuals carrying disease-associated variants. Genet Med. 2019;21(4):816-825. doi: 10.1038/s41436-018-0266-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Schenck A, Bardoni B, Moro A, Bagni C, Mandel JL. A highly conserved protein family interacting with the fragile X mental retardation protein (FMRP) and displaying selective interactions with FMRP-related proteins FXR1P and FXR2P. Proc Natl Acad Sci U S A. 2001;98(15):8844-8849. doi: 10.1073/pnas.151231598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Oguro-Ando A, Rosensweig C, Herman E, et al. . Increased CYFIP1 dosage alters cellular and dendritic morphology and dysregulates mTOR. Mol Psychiatry. 2015;20(9):1069-1078. doi: 10.1038/mp.2014.124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Noroozi R, Omrani MD, Sayad A, Taheri M, Ghafouri-Fard S. Cytoplasmic FMRP interacting protein 1/2 (CYFIP1/2) expression analysis in autism. Metab Brain Dis. 2018;33(4):1353-1358. doi: 10.1007/s11011-018-0249-8 [DOI] [PubMed] [Google Scholar]
- 53.Papa A, Wan L, Bonora M, et al. . Cancer-associated PTEN mutants act in a dominant-negative manner to suppress PTEN protein function. Cell. 2014;157(3):595-610. doi: 10.1016/j.cell.2014.03.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Merikangas AK, Corvin AP, Gallagher L. Copy-number variants in neurodevelopmental disorders: promises and challenges. Trends Genet. 2009;25(12):536-544. doi: 10.1016/j.tig.2009.10.006 [DOI] [PubMed] [Google Scholar]
- 55.Kushima I, Aleksic B, Nakatochi M, et al. . Comparative analyses of copy-number variation in autism spectrum disorder and schizophrenia reveal etiological overlap and biological insights. Cell Rep. 2018;24(11):2838-2856. doi: 10.1016/j.celrep.2018.08.022 [DOI] [PubMed] [Google Scholar]
- 56.Balci TB, Davila J, Lewis D, et al. . Broad spectrum of neuropsychiatric phenotypes associated with white matter disease in PTEN hamartoma tumor syndrome. Am J Med Genet B Neuropsychiatr Genet. 2018;177(1):101-109. doi: 10.1002/ajmg.b.32610 [DOI] [PubMed] [Google Scholar]
- 57.Ciaccio C, Saletti V, D’Arrigo S, et al. . Clinical spectrum of PTEN mutation in pediatric patients: a bicenter experience. Eur J Med Genet. 2019;62(12):103596. doi: 10.1016/j.ejmg.2018.12.001 [DOI] [PubMed] [Google Scholar]
- 58.Nelen MR, Kremer H, Konings IB, et al. . Novel PTEN mutations in patients with Cowden disease: absence of clear genotype-phenotype correlations. Eur J Hum Genet. 1999;7(3):267-273. doi: 10.1038/sj.ejhg.5200289 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eFigure 1. Workflow for CNV Discovery, Quality Control, and Downstream Analyses
eFigure 2. PTEN Mutation Spectra Across the 3 PHTS Clinical Phenotype Groups
eTable 1. Demographic and Clinical Characteristics of 481 PHTS Patients
eTable 2. Patients With PHTS and Germline Pathogenic and Likely Pathogenic CNVs in Cancer-Predisposing Genes
eTable 3. Demographic and Clinical Characteristics of 69 Patients With PHTS of Non-European Ancestry
eTable 4. Pathogenic and Likely Pathogenic CNVs Identified in Patients With PHTS of Non-European Ancestry