Abstract
This study characterizes the costs of recommended initial HIV antiretroviral therapy regimens in the United States from 2012 to 2018 and the magnitude of cost changes over time.
The United States has the highest antiretroviral treatment (ART) prices yet the lowest rate of HIV viral suppression (54%) compared with all other well-resourced countries, including Britain, Australia, and Canada.1 High ART costs are among many structural barriers that lead to poor treatment access and adherence, contributing to suboptimal HIV outcomes in the United States.2 We sought to characterize costs of recommended initial ART regimens in the United States from 2012 to 2018 and the magnitude of cost changes over time.
Methods
This research was covered by a protocol approved by the institutional review board for Massachusetts General Hospital, the Partners Human Research Committee. Informed consent was not needed because this analysis is a synthesis of published data, and no individual-level data was used. The US Department of Health and Human Services updates the Guidelines for the Use of Antiretroviral Agents in Adults and Adolescents annually; since 2012, these Guidelines include the average wholesale price (AWP) of available regimen components.3 Recommended initial ART regimens for “most people with HIV (PWH)”3 demonstrate durable virologic efficacy, favorable tolerability/toxicity, and ease of use. Alternative initial ART regimens are recommended in “certain clinical situations,” such as presence of comorbidities. We used data from the Guidelines to determine the annual per person cost of each of the recommended initial regimens from 2012 to 2018. We calculated the trend in mean regimen costs annually and the percentage change over time for all regimens recommended for most PWH, as well as in certain clinical situations. Then, for each regimen that was recommended for most PWH and subsequently recommended only in certain clinical situations, we compared the changes in costs over time as those recommendations evolved. All cost trends were compared with the consumer price index (US city average; all urban consumers). We used the urban consumer price index rather than the medical care component of the consumer price index because of its standard use in discounting and rebating formulas for Federal and Medicaid Ceiling Pricing.4
Results
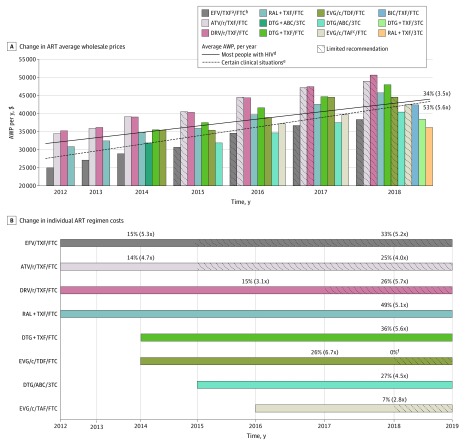
In 2012, the annual AWP of initial ART regimens recommended for most PWH ranged from $24 970 to $35 160 and increased to $36 080 to $48 000 in 2018. The average annual cost of ART recommended for most PWH has increased 34% since 2012, 3.5 times faster than inflation (Figure, A). The mean annual cost of initial ART regimens recommended for PWH in certain clinical situations was lower ($25 930-$39 670) from 2012 to 2018 but has increased 53%, 5.6 times faster than inflation. Regimens recommended for most PWH increased 2.8 to 6.7 times faster than inflation during their recommended horizon (Figure, B; solid bars); after falling out of recommendation for most PWH and limited to certain clinical situations, the AWP of these regimens still increased 4.0 to 5.7 times faster than inflation (Figure, B; hatched bars).
Figure. Average Wholesale Price (AWP) of Initial Antiretroviral Treatment (ART), 2012-2018.
A, Solid bars: regimens for most people with HIV (PWH). Hatched bars: regimens removed for most PWH and recommended only in certain clinical situations. Solid line: mean AWP of initial ART recommended for most PWH, 2012-2018. Dotted line: mean AWP of initial ART recommended in certain clinical situations, 2012-2018, including some regimens not depicted in the Figure. For example, because darunavir/cobicistat-based and doravirine-based regimens were never recommended for most PWH, they are not shown as bars, but their costs are calculated into the mean cost of initial ART for PWH in certain clinical situations (dotted line). The percentage change (2012-2018) in initial ART costs is shown; in parentheses, the change compared with inflation. B. Solid bars: regimens for most PWH greater than 1 year. Hatched bars: regimens removed for most PWH and recommended only in certain clinical situations. The percentage change in initial ART costs is shown; in parentheses, the change compared with inflation. ABC indicates abacavir; ATV, atazanavir; BIC, bictegravir; DRV, darunavir; DTG, dolutegravir; EFV, efavirenz; FTC, emtricitabine; /r, boosting with ritonavir; RAL, raltegravir; 3TC, lamivudine.
aTenofovir disoproxil fumarate (TDF) or tenofovir alafenamide (TAF) are denoted as TXF. In 2012 through 2015, tenofovir is TDF. In 2016 through 2018, tenofovir may be TDF or TAF. Unless otherwise specified, AWPs of TDF and TAF are the same.
bFTC may be substituted with cheaper 3TC, which is available generically; we did not include 3TC substitution costs here. We included TDF/3TC in 2018.
cCost of TDF and TAF are only different in combination with elvitegravir (EVG)/c/FTC.
dUS Department of Health and Human Services guidelines distinguish recommended regimens for “most people with HIV” from those in “certain clinical situations,” who may not tolerate the most common initial ART regimens and are therefore eligible for alternative regimens.
eThis may indicate a lack of updated cost data or no change in cost from 2017 to 2018.
Discussion
Even with new generic options in 2018, initial regimens recommended for most PWH today are all priced at more than $36 000 per patient per year, with annual costs that increased 6% on average since 2012. Increases in ART costs far outpaced the overall inflation rate.
Although US HIV prevalence is low, ART is the nation’s fifth costliest therapeutic class, accounting for $22.5 billion in spending in 2018.5 The federal “Ending the HIV Epidemic” initiative aims to achieve a 90% decrease in new HIV infections by 2030. To do so, the United States needs to increase viral suppression by 33%,1 which will require a total of $35.6 billion in annual spending on ART alone.
Limitations of this study include use of AWP. We acknowledge that AWP is often used as a benchmark and not reflective of patient out-of-pocket expenses. Complex systems of discounts and rebates help insulate public and private insurers from the full brunt of high ART costs, and federally funded safety nets may minimize costs for patients. However, in response to mounting ART costs and prolonged survival among PWH, insurers are increasingly seeking to manage ART access through formulary design, utilization management, and cost-sharing.6 We provide these details so that physicians can be sensitive to drug costs when recommending initial regimens of similar efficacy because costs borne directly by patients can affect their adherence and engagement in care. Slowing the trend of rapidly increasing ART costs is essential to expand and sustain access to effective individualized care and treatment for PWH and to meet “End the HIV Epidemic” goals.
References
- 1.The Henry J. Kaiser Family Foundation. HIV viral suppression rate in US lowest among comparable high-income countries. https://www.kff.org/hivaids/slide/hiv-viral-suppression-rate-in-u-s-lowest-among-comparable-high-income-countries/. Published 2019. Accessed November 7, 2019.
- 2.Zamani-Hank Y. The Affordable Care Act and the burden of high cost sharing and utilization management restrictions on access to HIV medications for people living with HIV/AIDS. Popul Health Manag. 2016;19(4):272-278. doi: 10.1089/pop.2015.0076 [DOI] [PubMed] [Google Scholar]
- 3.U.S Department of Health and Human Services Archived adult and adolescent guidelines. AIDSinfo. https://aidsinfo.nih.gov/guidelines/archive/adult-and-adolescent-guidelines. Accessed November 7, 2019.
- 4.US Department of Labor: Bureau of Labor Statistics. CPI for All Urban Consumers (CPI-U). https://data.bls.gov/PDQWeb/cu. Accessed November 7, 2019.
- 5.The IQVIA Institute. Medicine use and spending in the US: a review of 2018 and outlook to 2023. https://www.iqvia.com/insights/the-iqvia-institute/reports/medicine-use-and-spending-in-the-us-a-review-of-2018-and-outlook-to-2023. Published 2019. Accessed November 5, 2019.
- 6.National Alliance of State and Territorial AIDS Directors . Discriminatory design: HIV treatment in the Marketplace. https://www.nastad.org/sites/default/files/Discriminatory-Design-HIV-Treatment-in-the-Marketplace.pdf. Published 2016. Accessed November 5, 2019.