Key Points
Question
What is the long-term quality of life (QOL) and patient satisfaction after antibiotic treatment or appendectomy for uncomplicated acute appendicitis?
Findings
In this secondary analysis of a randomized clinical trial with 7-year observational follow-up of 423 patients, there was no difference in QOL between the treatments. Patients who underwent appendectomy were more satisfied in their treatment than patients taking antibiotics based on the antibiotic group patients undergoing appendectomy; patient satisfaction after successful antibiotic treatment and appendectomy was similar.
Meaning
The long-term QOL of patients with uncomplicated acute appendicitis is similar after appendectomy and antibiotics, but the lower satisfaction of patients who underwent an operation and took antibiotics calls for identifying predictive parameters for appendicitis recurrence.
Abstract
Importance
Long-term results support antibiotics for uncomplicated acute appendicitis as an alternative to appendectomy. To our knowledge, treatment-related long-term patient satisfaction and quality of life (QOL) are not known.
Objective
To determine patient satisfaction and QOL after antibiotic therapy and appendectomy for treating uncomplicated acute appendicitis.
Interventions
Open appendectomy vs antibiotics with intravenous ertapenem, 1 g once daily, for 3 days followed by 7 days of oral levofloxacin, 500 mg once daily, and metronidazole, 500 mg 3 times per day.
Design, Setting, and Participants
This observational follow-up of the Appendicitis Acuta (APPAC) multicenter randomized clinical trial comparing appendectomy with antibiotics included 530 patients age 18 to 60 years with computed tomography–confirmed uncomplicated acute appendicitis who were randomized to undergo appendectomy (273 [52%]) or receive antibiotics (257 [49%]). The trial was conducted from November 2009 to June 2012; the last follow-up was May 9, 2018. The data were analyzed in February 2019.
Main Outcomes and Measures
In this analysis, post hoc secondary end points of postintervention QOL (EQ-5D-5L) and patient satisfaction and treatment preference were evaluated.
Results
Of the 530 patients enrolled in the trial (appendectomy group: 273 [174 men (64%)] with a median age of 35 years; (antibiotic group: 257 [155 men (60%)] with a median age of 33 years), 423 patients (80%) were available for phone interview at a median follow-up of 7 years; 206 patients (80%) took antibiotics and 217 (79%) underwent appendectomy. Of the 206 patients taking antibiotics, 81 (39%) had undergone appendectomy. The QOL between appendectomy and antibiotic group patients was similar (median health index value, 1.0 in both groups; 95% CI, 0.86-1.0; P = .96). Patients who underwent appendectomy were more satisfied in the treatment than patients taking antibiotics (68% very satisfied, 21% satisfied, 6% indifferent, 4% unsatisfied, and 1% very unsatisfied in the appendectomy group and 53% very satisfied, 21% satisfied, 13% indifferent, 7% unsatisfied, and 6% very unsatisfied in the antibiotic group; P < .001) and in a subgroup analysis this difference was based on the antibiotic group patients undergoing appendectomy. There was no difference in patient satisfaction after successful antibiotic treatment compared with appendectomy (cumulative odds ratio [COR], 7.8; 95% CI, 0.5-1.3; P < .36). Patients with appendectomy or with successful antibiotic therapy were more satisfied than antibiotic group patients who later underwent appendectomy (COR, 7.7; 95% CI, 4.6-12.9; P < .001; COR, 9.7; 95% CI, 5.4-15.3; P < .001, respectively). Of the 81 patients taking antibiotics who underwent appendectomy, 27 (33%) would again choose antibiotics as their primary treatment.
Conclusions and Relevance
In this analysis, long-term QOL was similar after appendectomy and antibiotic therapy for the treatment of uncomplicated acute appendicitis. Patients taking antibiotics who later underwent appendectomy were less satisfied than patients with successful antibiotics or appendectomy.
Trial Registration
Clinicaltrials.gov Identifier: NCT01022567
This secondary analysis of a randomized clinical trial compares the long-term quality of life and patient satisfaction among Finnish patients after appendectomy and antibiotic therapy for the treatment of uncomplicated acute appendicitis.
Introduction
Appendectomy has been the standard treatment for acute appendicitis for more than a century1 and one of the most common surgical procedures performed annually.2 Large epidemiological studies have shown that there are 2 forms of acute appendicitis: uncomplicated and complicated, suggesting a differing pathophysiology for the 2 forms.3 In recent years, there has been increasing evidence from randomized clinical trials4,5,6,7,8 and meta-analyses9,10,11 indicating that patients with uncomplicated acute appendicitis can be treated safely and efficiently with antibiotics. Our recent 5-year results further support the notion that antibiotic treatment is a safe alternative to appendectomy for uncomplicated acute appendicitis also at long-term follow-up.12 In addition, antibiotic therapy for uncomplicated acute appendicitis is associated with substantial cost savings.13 Nonoperative management of uncomplicated acute appendicitis is under intense research and the important aspects of patient preference and satisfaction, quality of life (QOL), and joint decision-making have only recently been recognized.9,14 However, providing patients with unbiased information of all treatment options for uncomplicated acute appendicitis is challenging, as the manner of presenting and framing the information has a substantial influence on the answers; in survey trials, this is further complicated by an imaginary situation. To our knowledge, the assessment of postintervention QOL, patient satisfaction, and preference at long-term follow-up has not yet been conducted in randomized clinical trials in an adult patient population comparing antibiotics with appendectomy for uncomplicated acute appendicitis. The aim of this study was to compare the post hoc long-term QOL and patient satisfaction after antibiotic therapy and appendectomy for treating uncomplicated acute appendicitis for all the patients enrolled in the original Appendicitis Acuta (APPAC) trial.
Methods
The study design, rationale, and methods for the initial APPAC trial have been previously reported (Supplement 1).4,15 Briefly, the initial APPAC trial is a multicenter, open-label, noninferiority randomized clinical trial conducted from November 2009 to June 2012 at 6 Finnish hospitals (Turku, Oulu, and Tampere university hospitals and Jyväskylä, Mikkeli, and Seinäjoki central hospitals). The trial protocol was approved by the ethics committees of all participating hospitals and all patients gave written informed consent to participate in the study. The ethics committee granted a waiver for this study. The trial involved 530 patients age 18 to 60 years with computed tomography (CT)–confirmed uncomplicated acute appendicitis. Patients were randomized to either undergo open appendectomy or receive antibiotic treatment with intravenous ertapenem (1 g, once daily) for 3 days followed by 7 days of oral levofloxacin (500 mg, once daily) and metronidazole (500 mg, 3 times per day).
The CT criteria for acute appendicitis included an appendiceal diameter exceeding 6 mm with wall thickening accompanied with at least 1 of the following features: abnormal contrast enhancement of the appendiceal wall, inflammatory edema, or fluid collections around the appendix. The exclusion criteria included complicated acute appendicitis (defined as the presence of an appendicolith, perforation, abscess, or suspicion of a tumor on the CT scan), age younger than 18 years or older than 60 years, contraindications for CT, peritonitis, an inability to adhere with treatment and provide informed consent, and the presence of serious systemic illness. Patients in the antibiotic group were followed up by surgeons who could use their clinical judgement to pursue appendectomy if considered necessary. Most of the treating surgeons were not part of the core study team and provided care according to their normal clinical practice. All antibiotic group patients with a clinical suspicion of recurrent appendicitis underwent appendectomy. The last follow-up date for the current report at a median follow-up of 7 years (range, 5.7-8.2 years) was May 6, 2018. The objective for the long-term follow-up study was to compare the post hoc secondary end point of QOL with patient satisfaction and treatment preference between antibiotic therapy and appendectomy for the treatment of uncomplicated acute appendicitis.
Assessment of QOL and Patient Satisfaction
Quality of life was assessed using the validated EQ-5D-5L questionnaire (version April 18, 2017; EuroQOL).16,17,18 The assessment was conducted by unmasked, structured phone interviews between January and May 2018 by 3 researchers (S.S., J.H., and L.V.) who had not been involved in patient treatment. The descriptive questions cover 5 dimensions of everyday life: mobility, self-care, usual activities, pain/discomfort, and anxiety/depression. The answers are categorized in 5 levels ranging from no problems to extreme problems with numerical scoring from 1 to 5, respectively. These numerical scores for the 5 dimensions can be combined into a 5-digit number describing the respondent’s health state. These health state scores may then be converted into a single index value19 ranging between 0 (death) and 1 (full health) for each patient, illustrating the total QOL of the patient by country-specific validation tools. The validation specific for Finland for the EQ-5L-5D is not available. In this situation, according to the recommendations by the EuroQOL group to use a population closely resembling ours, we used the validation for Denmark. Additionally, the questionnaire reflects the patient’s self-rated health on a vertical visual analog scale (VAS) between 0 (worst health imaginable) and 100 (best health imaginable). Based on the study aim and patient population, we slightly modified the questionnaire by asking about abdominal pain and/or discomfort instead of general pain and discomfort.
Patient satisfaction with a received treatment was assessed by asking patients to score their satisfaction on a 5-point scale: very satisfied, satisfied, indifferent, unsatisfied, and very unsatisfied. The patients were also asked whether they would again choose the same treatment knowing the course and outcomes of the treatment.
In addition to the intention-to-treat analysis comparing the appendectomy and antibiotic treatment groups, we also performed a subgroup analysis by categorizing patients into 3 groups: appendectomy group, successful antibiotic treatment group (ie, no appendectomy), and antibiotic treatment group undergoing appendectomy. The primary end point of the original APPAC study was treatment success predefined to be assessed at 1-year follow-up.4,15 Success for the appendectomy group was defined as a patient successfully undergoing an appendectomy. In the antibiotic group, treatment efficacy was defined as the resolution of acute appendicitis resulting in discharge from the hospital without the need for surgical intervention and no recurrent appendicitis during a minimum follow-up of 1 year. The need for later appendectomy after primary antibiotic treatment for this study was evaluated at the time of QOL and satisfaction assessment. In this post hoc outcome analysis of QOL and patient satisfaction, this subgroup analysis is of clinical interest as the main drawback of antibiotic treatment of uncomplicated acute appendicitis is the possibility of appendicitis recurrence.
Statistical Analysis
Continuous variables were characterized using means or medians and the range of values or 95% confidence intervals of medians for nonnormally distributed variables; in the case of categorical variables, frequencies and percentages were used. The differences between groups in QOL scores and VAS values were tested using the Mann-Whitney U test. The satisfaction of care was analyzed using a multivariable cumulative logistic regression analysis to adjust the results for sex and age. The treatment preference in hindsight was analyzed using a multivariable multinomial logistic regression analysis to adjust the results for sex and age. The results of the logistic regression analyses were quantified using cumulative odds ratios (CORs) or odds ratios (ORs) with 95% confidence intervals. Two-sided tests were used and P < .05 was considered statistically significant. Statistical analyses were conducted using the SAS system for Windows, version 9.4 (SAS Institute).
Results
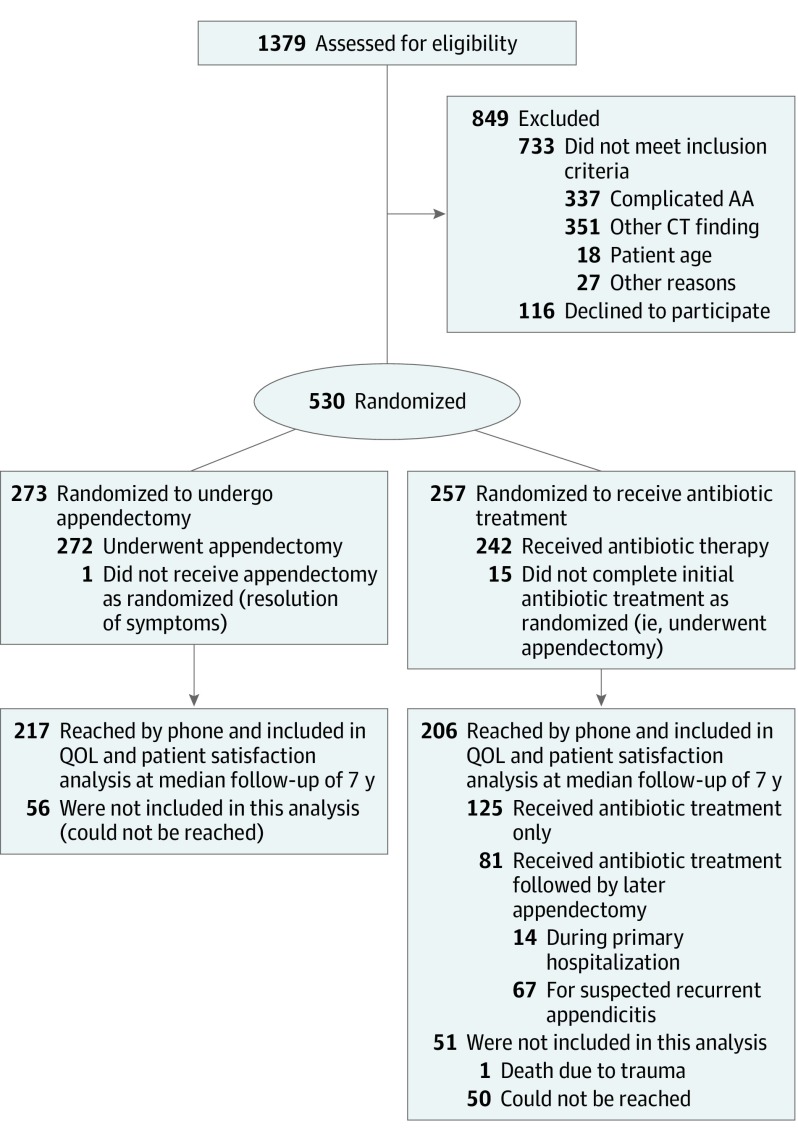
Figure 1 shows the trial profile. Patient baseline demographic characteristics were similar between the study groups at baseline4 and in this QOL analysis. Of the 530 patients (201 women [38%]) enrolled in the APPAC trial, 423 (80%) were available for a phone interview at a median follow-up of 7 years (range, 5.7-8.2 years). All of the patients reached by the researchers participated in the study. Of the 423 patients available for phone interview, 206 (47%) were originally randomized to receive antibiotic treatment (84 women [41%]; mean [SD] age, 43 [12.4] years; follow-up rate, 80%) and 217 (51%) to undergo appendectomy (76 women [35%]; mean [SD] age, 45 [12.0] years; follow-up rate, 79%). Of the 206 antibiotic group patients, 81 (39%) had undergone appendectomy (36 women [44.4%]; mean [SD] age, 44 [11.4] years), 14 (17.3%) during primary hospitalization and 67 (83%) for suspected recurrent appendicitis. There were no differences in response rates by group (217 of 272 [80%]) in the appendectomy group, 80% (206 of 257) in the antibiotic group, with 125 receiving antibiotics alone and 81 antibiotics with later appendectomy (response rates 80% and 81%, respectively). Of the 81 patients who underwent appendectomy after initial antibiotic treatment, 70 patients (86%) had surgery before the 1-year follow-up, 30 patients (37%) between years 1 and 5, and 1 patient (1%) between year 5 and QOL follow-up.
Figure 1. Study Flowchart.
AA indicates acute appendicitis; CT, computed tomography; QOL, quality of life.
QOL (EQ-5D-5L)
The QOL between appendectomy and antibiotic group patients was similar (median health index value, 1.0; 95% CI, 0.86-1.0 in both groups; P = .96). The patient self-rated health VAS values did not differ between the groups (P = .65), with patients who underwent appendectomy reporting a median health of 79.7 (95% CI, 77.7-81.7) and patients taking antibiotics a median health of 79.5 (95% CI, 77.5-81.4).
Satisfaction With Care and Treatment Preference in Hindsight
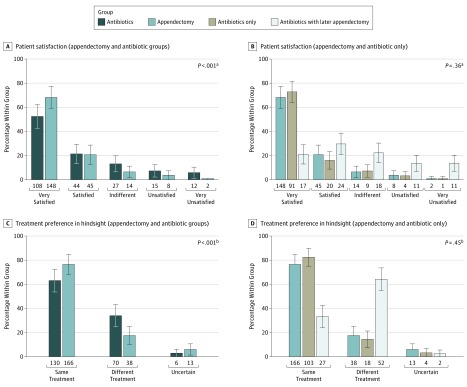
The results of patient satisfaction are shown in Figure 2A. Patients who underwent appendectomy were more satisfied in the treatment (68% very satisfied, 21% satisfied, 6% indifferent, 4% unsatisfied, and 1% very unsatisfied in the appendectomy group and 53% very satisfied, 21% satisfied, 13% indifferent, 7% unsatisfied, and 6% very unsatisfied in the antiobiotic group; P = .001) than patients taking antibiotics; in a subgroup analysis, this difference was caused by the antibiotic group patients undergoing appendectomy. There was no difference in patient satisfaction after successful antibiotic treatment (no appendectomy) compared with appendectomy (COR, 7.8; 95% CI, 0.5-1.3; P = .36). Patients with appendectomy or with successful antibiotic therapy were more satisfied than antibiotic group patients later undergoing appendectomy (COR, 7.7; 95% CI, 4.6-12.9; P < .001; COR, 9.7; 95% CI, 5.4-15.3; P < .001, respectively). The patient satisfaction results in these 3 groups are presented in Figure 2B.
Figure 2. Patient Satisfaction and Treatment Preference in Hindsight.
A, Patient satisfaction in the appendectomy and antibiotic groups. B, Patient satisfaction with a subgroup analysis in appendectomy, antibiotics only, and antibiotics with later appendectomy groups. C, Treatment preference in hindsight in the appendectomy and antibiotic groups. D, Treatment preference in hindsight with a subgroup analysis in the appendectomy, antibiotics only, and antibiotics with later appendectomy groups. The error bars represent 95% confidence intervals.
aDifference between appendectomy and antibiotic groups (A) and appendectomy and antibiotics only (B). Multivariable cumulative logistic regression analysis to adjust the results for sex and age.
bDifference between appendectomy and antibiotic groups (C) and appendectomy and antibiotics only (D). Multivariable multinomial logistic regression analysis to adjust the results for sex and age.
Treatment preference in hindsight is shown in Figure 2C and the results of the subgroup analysis in Figure 2D. There is a statistically significant difference in the reselection of treatment between the 3 groups of appendectomy, successful antibiotic therapy without the need for appendectomy, and antibiotic treatment with later appendectomy. Patients in the later appendectomy group would statistically significantly more often choose the different treatment compared with patients in the antibiotics only group (OR, 11.2; 95% CI, 5.6-22.2; P < .001) or the appendectomy group (OR, 8.8; 95% CI, 4.9-15.9; P < .001).
Discussion
In this study comparing long-term QOL and patient satisfaction after appendectomy and antibiotic therapy for the treatment of uncomplicated acute appendicitis, there was no difference in QOL between these treatment groups assessing the APPAC trial patients at a median follow-up of 7 years. Patients who underwent appendectomy were more satisfied in the treatment than patients taking antibiotics; in a subgroup analysis, this difference was based on the antibiotic group patients undergoing appendectomy. Patient satisfaction after successful antibiotic treatment (ie, no appendectomy) compared with appendectomy was similar. Patients with appendectomy or successful antibiotic therapy were more satisfied than antibiotic group patients later undergoing appendectomy. However, despite this difference, 33% of these patients taking antibiotics who later underwent appendectomy would still again choose antibiotics as their primary treatment.
To our knowledge, no other study has been conducted on the long-term QOL and patient satisfaction of adult patients randomized to receive antibiotic therapy or appendectomy for the treatment of uncomplicated acute appendicitis. A study in a pediatric population showed similar results at a very short-term follow-up of only 24 hours, with nonoperative management proving to be as an effective strategy as surgery when chosen by the family and with no difference in QOL.20 Another study in a pediatric population illustrated that the patients treated conservatively with antibiotics demonstrated higher patient QOL and health care satisfaction, and similar parental satisfaction was found in both groups.21
Quality of life is an important factor in measuring disease burden, and its additional value lies in considering the patients’ subjective perceptions of well-being and treatment.22 However, long-term QOL is difficult to measure in a comprehensive and realistic manner in cases of conditions causing more short-term burden to the patient. A QOL study in patients being treated with either open or laparoscopic appendectomy showed that although the burden of acute appendicitis should not be underestimated, the effect of appendectomy had a temporal and fully reversible effect on QOL.23 Based on this limitation of QOL after the treatment of uncomplicated acute appendicitis, we added questions about patient satisfaction and treatment preference in hindsight to gain more perspective about the patient experiences with the different treatment options and their outcomes.
Patient satisfaction and preference are important factors that need to be considered in the overall assessment of different efficient treatment options. In our study, it was not surprising to discover that patients in the appendectomy group were more satisfied than the antibiotic group as the latter included patients taking antibiotics who later underwent appendectomy and thus were treated twice for the same disease. When these patients taking antibiotics who later underwent appendectomy were analyzed separately as the third group, patients with appendectomy or successful antibiotic therapy were more satisfied than antibiotic group patients later undergoing appendectomy and there was no difference between the appendectomy or antibiotics alone groups. The fact that 33% of patients who later underwent appendectomy after primary antibiotic treatment would still choose primary antibiotic treatment, accepting the risk of recurrence and potential later appendectomy, illustrates that in some situations, patients accept the risk of recurrence to possibly avoid surgery. A similar notion was stated in a recent meta-analysis9 in which patients averse to the risk of recurrence would possibly choose primary immediate appendectomy, whereas patients averse to surgery may choose initial antibiotics. With increasing evidence of antibiotics for uncomplicated acute appendicitis, future studies are necessary to inform patients and clinicians about the possible benefits of each treatment approach for individual patients.24
A study regarding public perceptions about the treatment of acute appendicitis showed that the general public was knowledgeable in potential symptoms but less aware of the management options, with the belief that without surgery appendicitis would lead to perforation.25 Another study showed that after information about the risks and advantages of surgery and antibiotic treatment for uncomplicated acute appendicitis, a population of medical students were more inclined to choose surgery, also noting that the answers may have been influenced by the manner in which the summary data of each treatment arm were presented.26 A recent guideline27 states that nonoperative management of uncomplicated acute appendicitis is feasible in patients wishing to avoid surgery and accept the risk of recurrence. With an increasing amount of studies,4,5,6,7,8 meta-analyses,9,10,11 and long-term follow-up results12 indicating the feasibility of antibiotic therapy in the treatment of uncomplicated acute appendicitis, future studies should focus on a more multifactorial approach to making the treatment decision, including patient information and involvement in shared decision-making. The notion of this shared decision-making in treating uncomplicated acute appendicitis has been raised recently,28,29,30 and future studies should focus on a more patient-centered approach informing about benefits for individual patients.24 In addition, future studies need to address the biases in delivering the patient information and attempt to determine optimal ways to deliver as unbiased information as possible.
Once medical treatments become universally accepted clinical practice, they are very difficult to change, even if proven wrong or harmful.31 Appendectomy has been the criterion standard treatment of acute appendicitis for more than a decade without having to differentiate between uncomplicated and complicated acute appendicitis. This creates an understandable and inevitable bias regarding new treatment alternatives for uncomplicated acute appendicitis, especially among surgeons. In their online survey, Hanson et al14 reported that surgeons significantly more often chose surgery as their optimal treatment choice for uncomplicated acute appendicitis. Based on the presumed finding of this study that later appendectomy after antibiotic treatment decreases patient satisfaction, future studies should also be directed at reducing the failure and recurrence rates of antibiotic treatment for appendicitis14 by identifying potential predictive factors indicating the risk of recurrence of uncomplicated acute appendicitis and thus enabling an optimization of the primary treatment choice. In addition, promising results have been reported for successful symptomatic therapy of uncomplicated acute appendicitis32 and a double-blind randomized trial (APPAC III) comparing antibiotic therapy with placebo for the treatment of uncomplicated acute appendicitis is currently being conducted.33 If future studies show a similar efficacy and safety of symptomatic treatment and antibiotic therapy, the strategy of appendectomy for all patients with uncomplicated acute appendicitis will be difficult to justify and even more studies are needed to evaluate the optimization and tailoring of these treatment choices for all patients.
Strengths and Limitations
The strengths of the study include the novelty of the results as, to our knowledge, long-term QOL and patient satisfaction has not yet been reported in a randomized clinical trial on adult patients comparing appendectomy with antibiotic therapy in treating uncomplicated acute appendicitis. Another strength is the follow-up rate of 80% at a median follow-up of 7 years, which together with the multicenter characteristic of the study enhances the likelihood that the study results are generalizable to routine surgical practice. In addition, by very effectively diagnosing the acute appendicitis and excluding patients with complicated acute appendicitis by CT in the APPAC trial,4 this study population accurately represents patients with uncomplicated acute appendicitis.
As this observational study is based on the original APPAC trial, it has limitations based on the initial study protocol described in detail in the previous trial reports4,34 as well as this additional study assessing the post hoc outcomes of postintervention QOL and patient satisfaction. One of the limitations of the initial trial includes the open approach for appendectomy, as currently laparoscopic appendectomy is the criterion standard associated with shorter hospital stays and less postoperative pain.35 Another limitation of the initial protocol was the long duration of antibiotic treatment and hospitalization for the antibiotic group patients, who had to spend time in the hospital regardless of their clinical status. All of these limitations most likely have an effect on patient satisfaction. A strong limitation of this analysis is that it is a post hoc secondary outcome, as at the time of study protocol planning, the importance of patient preference or QOL was not yet recognized and the focus was on assessing whether antibiotic therapy was an effective and safe treatment option for treating uncomplicated acute appendicitis. Thus, baseline QOL is not available for comparison. In addition, the QOL measurement tools for acute care conditions can also be seen as a limitation as QOL is difficult to measure, especially in the case of emergency conditions that for most only have a short-term effect on a patient’s life.
Conclusions
Long-term QOL is similar after appendectomy and antibiotic therapy for treating uncomplicated acute appendicitis. Patients taking antibiotics who later underwent appendectomy were less satisfied than patients with successful antibiotic treatment or appendectomy, underlining the importance of discovering potential parameters predictive of appendicitis recurrence.
Trial protocol.
Data sharing statement.
References
- 1.McBurney C. Experience with early operative interference in cases of disease of the vermiform appendix. NY Med J. 1889;50:676-684. [Google Scholar]
- 2.Stewart B, Khanduri P, McCord C, et al. Global disease burden of conditions requiring emergency surgery. Br J Surg. 2014;101(1):e9-e22. doi: 10.1002/bjs.9329 [DOI] [PubMed] [Google Scholar]
- 3.Livingston EH, Fomby TB, Woodward WA, Haley RW. Epidemiological similarities between appendicitis and diverticulitis suggesting a common underlying pathogenesis. Arch Surg. 2011;146(3):308-314. doi: 10.1001/archsurg.2011.2 [DOI] [PubMed] [Google Scholar]
- 4.Salminen P, Paajanen H, Rautio T, et al. Antibiotic therapy vs appendectomy for treatment of uncomplicated acute appendicitis: the APPAC Randomized Clinical Trial. JAMA. 2015;313(23):2340-2348. doi: 10.1001/jama.2015.6154 [DOI] [PubMed] [Google Scholar]
- 5.Hansson J, Körner U, Khorram-Manesh A, Solberg A, Lundholm K. Randomized clinical trial of antibiotic therapy versus appendicectomy as primary treatment of acute appendicitis in unselected patients. Br J Surg. 2009;96(5):473-481. doi: 10.1002/bjs.6482 [DOI] [PubMed] [Google Scholar]
- 6.Styrud J, Eriksson S, Nilsson I, et al. Appendectomy versus antibiotic treatment in acute appendicitis. a prospective multicenter randomized controlled trial. World J Surg. 2006;30(6):1033-1037. doi: 10.1007/s00268-005-0304-6 [DOI] [PubMed] [Google Scholar]
- 7.Vons C, Barry C, Maitre S, et al. Amoxicillin plus clavulanic acid versus appendicectomy for treatment of acute uncomplicated appendicitis: an open-label, non-inferiority, randomised controlled trial. Lancet. 2011;377(9777):1573-1579. doi: 10.1016/S0140-6736(11)60410-8 [DOI] [PubMed] [Google Scholar]
- 8.Svensson JF, Patkova B, Almström M, et al. Nonoperative treatment with antibiotics versus surgery for acute nonperforated appendicitis in children: a pilot randomized controlled trial. Ann Surg. 2015;261(1):67-71. doi: 10.1097/SLA.0000000000000835 [DOI] [PubMed] [Google Scholar]
- 9.Sallinen V, Akl EA, You JJ, et al. Meta-analysis of antibiotics versus appendicectomy for non-perforated acute appendicitis. Br J Surg. 2016;103(6):656-667. doi: 10.1002/bjs.10147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Harnoss JC, Zelienka I, Probst P, et al. Antibiotics versus surgical therapy for uncomplicated appendicitis: systematic review and meta-analysis of controlled trials (PROSPERO 2015: CRD42015016882). Ann Surg. 2017;265(5):889-900. doi: 10.1097/SLA.0000000000002039 [DOI] [PubMed] [Google Scholar]
- 11.Poprom N, Numthavaj P, Wilasrusmee C, et al. The efficacy of antibiotic treatment versus surgical treatment of uncomplicated acute appendicitis: systematic review and network meta-analysis of randomized controlled trial. Am J Surg. 2019;218(1):192-200. [DOI] [PubMed] [Google Scholar]
- 12.Salminen P, Tuominen R, Paajanen H, et al. Five-year follow-up of antibiotic therapy for uncomplicated acute appendicitis in the APPAC Randomized Clinical Trial. JAMA. 2018;320(12):1259-1265. doi: 10.1001/jama.2018.13201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sippola S, Grönroos J, Tuominen R, et al. Economic evaluation of antibiotic therapy versus appendicectomy for the treatment of uncomplicated acute appendicitis from the APPAC randomized clinical trial. Br J Surg. 2017;104(10):1355-1361. doi: 10.1002/bjs.10575 [DOI] [PubMed] [Google Scholar]
- 14.Hanson AL, Crosby RD, Basson MD. Patient preferences for surgery or antibiotics for the treatment of acute appendicitis. JAMA Surg. 2018;153(5):471-478. doi: 10.1001/jamasurg.2017.5310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Paajanen H, Grönroos JM, Rautio T, et al. A prospective randomized controlled multicenter trial comparing antibiotic therapy with appendectomy in the treatment of uncomplicated acute appendicitis (APPAC trial). BMC Surg. 2013;13:3. doi: 10.1186/1471-2482-13-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.EuroQol Group . EuroQol—a new facility for the measurement of health-related quality of life. Health Policy. 1990;16(3):199-208. doi: 10.1016/0168-8510(90)90421-9 [DOI] [PubMed] [Google Scholar]
- 17.Herdman M, Gudex C, Lloyd A, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res. 2011;20(10):1727-1736. doi: 10.1007/s11136-011-9903-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Devlin NJ, Krabbe PF. The development of new research methods for the valuation of EQ-5D-5L. Eur J Health Econ. 2013;14(suppl 1):S1-S3. doi: 10.1007/s10198-013-0502-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dolan P. Modeling valuations for EuroQol health states. Med Care. 1997;35(11):1095-1108. doi: 10.1097/00005650-199711000-00002 [DOI] [PubMed] [Google Scholar]
- 20.Minneci PC, Mahida JB, Lodwick DL, et al. Effectiveness of patient choice in nonoperative vs surgical management of pediatric uncomplicated acute appendicitis. JAMA Surg. 2016;151(5):408-415. doi: 10.1001/jamasurg.2015.4534 [DOI] [PubMed] [Google Scholar]
- 21.Minneci PC, Sulkowski JP, Nacion KM, et al. Feasibility of a nonoperative management strategy for uncomplicated acute appendicitis in children. J Am Coll Surg. 2014;219(2):272-279. doi: 10.1016/j.jamcollsurg.2014.02.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Efthymiadou O, Mossman J, Kanavos P. Health related quality of life aspects not captured by EQ-5D-5L: Results from an international survey of patients. Health Policy. 2019;123(2):159-165. doi: 10.1016/j.healthpol.2018.12.003 [DOI] [PubMed] [Google Scholar]
- 23.Koumarelas K, Theodoropoulos GE, Spyropoulos BG, Bramis K, Manouras A, Zografos G. A prospective longitudinal evaluation and affecting factors of health related quality of life after appendectomy. Int J Surg. 2014;12(8):848-857. doi: 10.1016/j.ijsu.2014.06.015 [DOI] [PubMed] [Google Scholar]
- 24.Ehlers AP, Talan DA, Moran GJ, Flum DR, Davidson GH. Evidence for an antibiotics-first strategy for uncomplicated appendicitis in adults: a systematic review and gap analysis. J Am Coll Surg. 2016;222(3):309-314. doi: 10.1016/j.jamcollsurg.2015.11.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.O’Connell EP, White A, Cromwell P, et al. Non-operative treatment of appendicitis: public perception and decision-making. Ir J Med Sci. 2018;187(4):1029-1038. doi: 10.1007/s11845-018-1758-5 [DOI] [PubMed] [Google Scholar]
- 26.Althans AR, Tamer P, Brady JT, Steinhagen E, Ho VP. Surgery versus antibiotics for uncomplicated appendicitis: which would a medical student want? Surg Infect (Larchmt). 2017;18(8):868-873. doi: 10.1089/sur.2017.129 [DOI] [PubMed] [Google Scholar]
- 27.Di Saverio S, Birindelli A, Kelly MD, et al. WSES Jerusalem guidelines for diagnosis and treatment of acute appendicitis. World J Emerg Surg. 2016;11:34. doi: 10.1186/s13017-016-0090-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hasday SJ, Chhabra KR, Dimick JB. Antibiotics vs surgery for acute appendicitis: toward a patient-centered treatment approach. JAMA Surg. 2016;151(2):107-108. doi: 10.1001/jamasurg.2015.4065 [DOI] [PubMed] [Google Scholar]
- 29.Livingston EH. Antibiotic treatment for uncomplicated appendicitis really works: results from 5 years of observation in the APPAC Trial. JAMA. 2018;320(12):1245-1246. doi: 10.1001/jama.2018.13368 [DOI] [PubMed] [Google Scholar]
- 30.Talan DA, Saltzman DJ, DeUgarte DA, Moran GJ. Methods of conservative antibiotic treatment of acute uncomplicated appendicitis: a systematic review. J Trauma Acute Care Surg. 2019;86(4):722-736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Prasad VK, Cifu AS. Ending Medical Reversal: Improving Outcomes, Saving Lives. Baltimore, MD: Johns Hopkins University Press; 2015. [Google Scholar]
- 32.Park HC, Kim MJ, Lee BH. Randomized clinical trial of antibiotic therapy for uncomplicated appendicitis. Br J Surg. 2017;104(13):1785-1790. doi: 10.1002/bjs.10660 [DOI] [PubMed] [Google Scholar]
- 33.Sippola S, Grönroos J, Sallinen V, et al. A randomised placebo-controlled double-blind multicentre trial comparing antibiotic therapy with placebo in the treatment of uncomplicated acute appendicitis: APPAC III trial study protocol. BMJ Open. 2018;8(11):e023623. doi: 10.1136/bmjopen-2018-023623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Haijanen J, Sippola S, Grönroos J, et al. ; APPAC study group . Optimising the antibiotic treatment of uncomplicated acute appendicitis: a protocol for a multicentre randomised clinical trial (APPAC II trial). BMC Surg. 2018;18(1):117. doi: 10.1186/s12893-018-0451-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jaschinski T, Mosch CG, Eikermann M, Neugebauer EA, Sauerland S. Laparoscopic versus open surgery for suspected appendicitis. Cochrane Database Syst Rev. 2018;11:CD001546. doi: 10.1002/14651858.CD001546.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Trial protocol.
Data sharing statement.