This cohort study assesses the extent of association of assisted reproductive technology with congenital heart defects independent of its known association with twin pregnancies.
Key Points
Question
Is assisted reproductive technology associated with increased risk of congenital heart defects independent of its association with twin pregnancies?
Findings
In this cohort study of 507 390 singleton or twin pregnancies, the prevalence of congenital heart defects was higher in assisted pregnancies (223 [2.2%]) than in nonassisted pregnancies (6057 [1.2%]). Twinning mediated 87.3% of the association between assisted pregnancy and congenital heart defects.
Meaning
The findings suggest the association between assisted reproductive technology and congenital heart defects may be mediated by twinning.
Abstract
Importance
The extent to which assisted reproductive technology is associated with increased risk of congenital heart defects independent of its known association with twinning remains uncertain.
Objective
To assess the extent to which assisted pregnancy is associated with increased risk of congenital heart defects independent of its known association with twinning.
Design, Setting, and Participants
This retrospective cohort study linked records of congenital heart defect diagnoses with assisted reproductive technology cycles in 507 390 singleton or twin pregnancies (10 149 assisted pregnancies and 497 241 nonassisted pregnancies), including singleton and twin early pregnancy losses, stillbirths, and live births (follow-up to 1 year of age) in Ontario, Canada, between April 1, 2012, and October 31, 2015. Statistical analysis was performed from January 1, 2017, to September 9, 2019.
Exposures
Assisted reproductive technology and its 2 subtypes: intracytoplasmic sperm injection and in vitro fertilization without intracytoplasmic sperm injection.
Main Outcomes and Measures
The main outcome was congenital heart defects (prevalence and relative risk measured as odds ratios [ORs]). Mediation analysis was performed to assess the extent to which the association between assisted reproductive technology and congenital heart defects was mediated by twinning.
Results
Of 507 390 mother-infant pairs with singleton or twin pregnancies evaluated, the prevalence of congenital heart defects in assisted pregnancies (223 [2.2%]) was higher than that in nonassisted pregnancies (6057 [1.2%]; crude OR, 1.82; 95% CI, 1.59-2.09). The strength of the association between assisted pregnancy and congenital heart defects decreased after adjusting for several risk factors simultaneously (adjusted OR, 1.70; 95% CI, 1.48-1.95). Further mediation analysis indicated that most of the association between assisted pregnancy and congenital heart defects was mediated by twinning (adjusted OR, 1.68; 95% CI, 1.44-1.92), and the natural direct association of assisted pregnancy with congenital heart defects among singleton pregnancies was 1.09 (95% CI, 0.93-1.25). Mediation of twinning accounted for 87.3% of the association.
Conclusions and Relevance
Our study results suggest that the association between assisted reproductive technology and congenital heart defects may be mediated by twinning.
Introduction
At present, approximately 2% of pregnancies are conceived by using assisted reproductive technology (ART), with upward trends in recent years.1,2 An increased risk of adverse pregnancy outcomes, including congenital heart defects (CHD), in ART pregnancies compared with non-ART pregnancies has been observed.1,2,3,4,5,6,7,8,9,10,11,12,13,14,15 Several maternal factors, such as maternal age, obesity, socioeconomic status, and preexisting health problems, have been associated with risks of both adverse pregnancy outcomes, including CHD and infertility requiring ART to conceive,1,2,16,17,18 and the association between ART and CHD tends to be reduced after adjustment for these maternal factors.3,4,5,6,7,8,9,10,11,12,13,14,15
One important consequence of increased use of ART is a substantially increased rate of twin pregnancies.1,2,19,20,21,22,23,24,25,26 Compared with singletons, the risks of adverse pregnancy outcomes including CHD have been shown to be increased in twins.21,22,24,25,26 Some studies have suggested that part of the increased risk of CHD observed in ART pregnancies may be attributable to the increased number of twin pregnancies.10,14,26
Congenital heart defect is a serious disease burden not only in infants but also in adolescents and adults.27,28,29 The pathophysiologic findings and pathogenesis of CHD are complicated and often are very different from other congenital anomalies.12,13,30,31 The American Institute of Ultrasound in Medicine, in collaboration with other professional organizations, has developed the Fetal Echocardiography Practice Parameter,32 and the American College of Radiology has endorsed this document. The association of ART and CHD should be further examined to decide whether fetal echocardiography, a costly procedure, should be used in ART pregnancies.32
We performed a large population-based study to examine the association between ART and CHD and to explore the associations of ART, twin pregnancies, and CHD, with twin status considered as a mediator in the analysis.
Methods
Study Design and Study Population
For this cohort study, ethical approval was obtained from the Ottawa Hospital Research Ethical Board, Ottawa, Ontario, Canada. Because this study used data collected by the province-approved registry with no additional data collection from patients, no informed consent was required. All singleton and twin stillbirths and live births (with follow-up to 1 year of age) and some early pregnancy losses that occurred between April 1, 2012, and October 31, 2015, in Ontario, Canada, and were captured by Better Outcomes Registry & Network (BORN) were included in the study. BORN is a provincial maternal child registry aiming to facilitate and improve care for mothers and children in Ontario.33 BORN has an internet-based data entry system administered by the Children’s Hospital of Eastern Ontario called the BORN Information System. There are 3 locations and periods in the BORN Information System in which CHD data can be captured: (1) prenatal screening records, (2) antenatal specialty clinic records, and (3) hospital records for birth or postpartum care or neonatal intensive care unit admissions. BORN has 100% capture for hospital and home births in Ontario. This database contains maternal demographic characteristics and health behaviors, preexisting maternal health problems, and birth outcomes. The national Canadian Assisted Reproductive Technologies Registry (CARTR Plus) is housed within BORN and is owned and administered by the medical directors of in vitro fertilization clinics and the Canadian Fertility and Andrology Society. The national CARTR Plus includes in vitro fertilization cycles for individuals undergoing ART-associated treatment in Canada.
Outcome
Congenital heart defect was the outcome of interest in this study. To reduce misclassifications, only major structural CHD was considered (for a list of major structural CHD, see eTable 1 in the Supplement). Newborn diagnoses including CHD were collected at birth and during the postpartum period. Information on congenital anomalies in lost or terminated pregnancies was captured from prenatal screening follow-up visits if the anomaly was diagnosed through prenatal screening and antenatal specialty clinics if the anomaly was diagnosed through an antenatal clinic in Ontario. For CHD cases that were not captured by BORN, an additional ascertainment occurred through linkage with the Canadian Institute for Health Information (CIHI) Discharge Abstract Database and National Ambulatory Care Reporting System metadata. In CIHI records, CHD cases were identified based on a standardized diagnostic coding system, International Classification of Diseases and Related Health Problems, Tenth Revision, Canada (ICD-10-CA). We were able to capture CHD at birth and up to 1 year through linkage with CIHI records. Because of difficulties in separately identifying in utero fetal CHD cases in twins and limited further linking to infant records, we used individual pregnancy as the unit of analysis (ie, if 1 member of a twin pair was affected, that pregnancy was considered to be affected).
Exposure
Assisted reproductive technology was the exposure of interest in the study. We followed the Centers for Disease Control and Prevention definition for ART,34 which included both intracytoplasmic sperm injection (ICSI) and in vitro fertilization (IVF) without ICSI. The report of treatment cycles by fertility centers is not uniformly required, and some cycles may be missed. Moreover, BORN started incorporating CARTR Plus data starting in January 2013. To maximize ascertainment of ART, we used BORN records on conception type to supplement CARTR Plus records.
Confounders
Potential confounding variables accounted for were maternal age, parity, prepregnancy obesity (defined by prepregnancy body mass index), maternal smoking, social drug use or alcohol consumption, folic acid intake during pregnancy, mental health illness during prepregnancy or pregnancy (a composite measure of psychiatric disorders, depression, and anxiety), and prepregnancy physical health problems (a composite measure of chronic hypertension, diabetes, heart disease, thyroid disease, lupus, alcoholism, asthma, HIV infection, and hepatitis B). We also attempted to account for maternal educational level and family income. Because no individual records on maternal educational level and family income are available in the BORN Information System, we created 2 neighborhood-level variables for Ontario by converting postal codes affiliated with the mother into dissemination areas from the Canada census data nearest to the study period: (1) percentage of having a university degree among the adult population aged 25 to 64 years and (2) median family income, both measured in quintiles according to methods established in an earlier study.35 Dissemination areas were small, relatively stable geographic units with a population of 400 to 700 persons of relative homogenous socioeconomic status.36 We were careful in selecting confounders to be adjusted in the analysis so that no overadjustment would occur.37,38 All confounders included in the analysis were considered to be independently associated with CHD (outcome) and ART (exposure), and we verified the potential confounders by examining the association between confounders and outcome among unexposed study participants only.39
Mediator
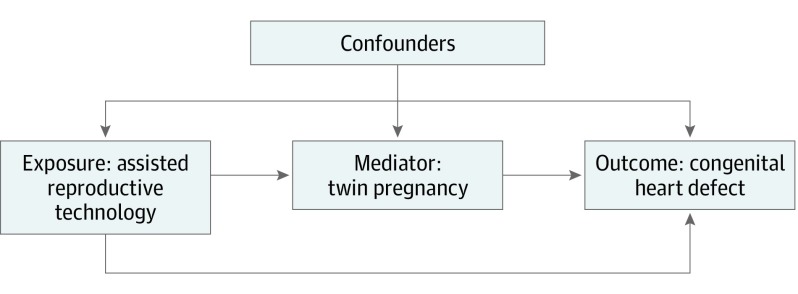
Twins have remarkably higher risks of adverse perinatal outcomes including CHD,21,22,24,25,26 and the proportion of twins in ART pregnancies is substantially higher than natural pregnancies.1,2,19,20,21,22,23 Because twin status is the intermediate step between ART and CHD (twin status is determined before the development of CHD), it qualified as a potential mediator.40,41,42,43
The pregnancy identification (an internal identifier assigned by BORN) was used to link records of the infant with the same pregnancy to obtain maternal information, and the birth identification (an internal identifier assigned by BORN) was used to link the records of the same infant across different periods within the BORN Information System. Unencrypted health card numbers were used to link BORN Information System records with CIHI records. The record linkage process is shown in the eFigure in the Supplement.
Statistical Analysis
Statistical analysis was performed from January 1, 2017, to September 9, 2019. All analyses were performed using SAS, version 9.4 (SAS Institute Inc). We first compared baseline characteristics between ART and non-ART pregnancies and between the 2 subgroups of ART. We then described the prevalence of CHD as associated with potential confounding risk factors. Before multivariable regression analysis, multiple imputation using a fully conditional specification method44,45,46 was applied to create complete data sets. Details of missing imputation are provided in the eMethods in the Supplement. Multivariable logistic regression analyses were then performed in both exposure-outcome and mediator-outcome models while accounting for covariates. The variable ART was assessed as a binary variable. Because CHD is a rare outcome (<5%), we used odds ratios (ORs) to estimate relative risk in logistic regression models. All prespecified risk factors were included in the analysis.
To assess potential mediation of twinning in the association between ART and CHD, the Causalmed procedure47 in SAS was performed. The specific issue to be addressed by the mediation analysis was (1) how much of the overall association of ART with CHD risk was attributable to the association of ART with increased risk of twinning, which in turn affects CHD risk, and (2) how much of the association of ART and CHD did not involve twinning.40,41,42,43 The mediation analysis was done to parse the total association of ART with CHD prevalence into 2 components. The natural direct association of ART with CHD risk in the study population would occur if the pathway from ART to twin status were disabled. The Figure gives the contribution of the ART-CHD pathway to the overall association of ART with CHD risk. The natural indirect association, which is the association of ART with CHD risk in the study population, would occur if the direct ART-CHD pathway were disabled so that ART was associated with CHD risk only via the ART-twin-CHD pathway. The proportion mediated was defined as the natural indirect association divided by the total association, although it is only meaningful when both components of the total association have the same mathematical sign. Mediation analysis allows for control of confounding factors in estimating these results.
Figure. Framework of the Association Between Assisted Reproductive Technology and Congenital Heart Defects With Twin Pregnancy as the Mediator.
Four-way decompositions of the total excess association were further estimated considering the potential interaction of ART with twinning in the association with risk of CHD using risk difference.42 The question of 4-way decompositions analysis is the following: To what extent is ART associated with CHD risk differently in twin pregnancies than in singleton pregnancies? The ART twin-status interaction can be operative regardless of the relative contributions of the direct and indirect paths (Figure). The ART twin-status interaction could be important for 2 reasons. First, it could help toward understanding the biologic mechanisms that underlie the association between ART and CHD. Why might ART affect twin pregnancies differently from how it affects singleton pregnancies in terms of CHD risk? Second, the amount of ART-twin interaction affects the degree to which results of mediation analysis obtained from this study are generalizable to other populations. The first of 4 components assessed in the 4-way decompositions was the controlled direct association, which was the CHD risk difference between ART and non-ART pregnancies among singleton births (the baseline risk difference in the absence of mediation or interaction). The second was reference interaction, which was the contribution of the ART-twin interaction if the frequency of twinning in ART pregnancies was set to what was observed among non-ART pregnancies (the association between CHD risk and the ART-twin interaction in the absence of mediation). The third component was the mediated interaction, which was the contribution of the ART-twin interaction when applied only to the added increase in the frequency of twinning seen in ART pregnancies (the combined association between CHD risk and mediation and the ART-twin interaction). The fourth component was the pure indirect association, which was the increase in CHD risk associated with the increased proportion of twins seen in ART pregnancies apart from the ART-twin interaction (mediation by twin status in the absence of an ART-twin interaction).
Preliminary analysis showed that there was no major difference between IVF and ICSI in terms of their association with CHD. To preserve the statistical precision and to simplify the interpretation, mediation analysis was performed for overall ART only. To assess robustness of the results, analyses deleting missing data without missing imputation and CHDs ascertained at birth or up to 1 year after birth (ie, without linking CHDs with fetal losses or terminations) were performed.
Results
Baseline Characteristics
A total of 507 390 mother-infant pairs with a singleton or twin birth were matched and included in final analysis. Among these, 10 149 (2.0%) were assisted pregnancies and 497 241 (98.0%) were nonassisted pregnancies. Women who conceived by ART were more likely to be older, to be experiencing their first pregnancy, and to have a higher body mass index. They were more likely to live in higher-income and higher-educational-level neighborhoods and have physical health problems but were less likely to have major mental health problems (such as schizophrenia or bipolar disease) and less likely to engage in smoking, social drug use, or alcohol consumption during pregnancy compared with women who conceived without ART (Table 1). The twin rate differed between groups: 18.5% (1881 of 10 149) in assisted pregnancies and 1.4% (7082 of 497 241) in nonassisted pregnancies. Women who conceived by ICSI were more likely to experience their first pregnancy (73.7% [2825 of 3835] vs 60.0% [3655 of 6094]) but less likely to be obese (16.8% [534 of 3187] vs 19.2% [945 of 4929]) than women who conceived by IVF. Twin rates were 17.5% in pregnancies conceived by ICSI and 19.2% in pregnancies conceived by IVF.
Table 1. Demographic Characteristics and Medical History of Women With ART and Non-ART Pregnanciesa.
| Variable | ART Pregnancy | Non-ART Pregnancy (n = 497 241) | ||
|---|---|---|---|---|
| ICSI (n = 3938) | IVF (n = 6211) | Total (n = 10 149) | ||
| Maternal age at birth, mean (SD), y | 35.7 (4.7) | 35.8 (5.2) | 35.8 (5.0) | 30.3 (5.3) |
| Primaparous | 2825 (73.7) | 3655 (60.0) | 6480 (65.3) | 209 768 (42.9) |
| Obesityb | 534 (16.8) | 945 (19.2) | 1479 (18.2) | 77 034 (18.1) |
| Median family income at dissemination-area level, % | ||||
| >80 | 1179 (31.1) | 1598 (27.2) | 2777 (28.7) | 77 548 (16.4) |
| 60-80 | 1077 (28.4) | 1661 (28.3) | 2738 (28.3) | 109 972 (23.2) |
| 40-59 | 661 (17.4) | 1076 (18.3) | 1737 (18.0) | 90 770 (19.1) |
| 20-39 | 471 (12.4) | 817 (13.9) | 1288 (13.3) | 85 745 (18.1) |
| <20 | 408 (10.8) | 714 (12.2) | 1122 (11.6) | 110 344 (23.3) |
| University degree at dissemination-area level, % | ||||
| >80 | 1307 (34.2) | 1763 (29.9) | 3070 (31.6) | 87 828 (18.4) |
| 60-80 | 1135 (29.7) | 1708 (28.9) | 2843 (29.2) | 114 984 (24.0) |
| 40-59 | 665 (17.4) | 1225 (20.7) | 1890 (19.4) | 104 229 (21.8) |
| 20-39 | 465 (12.2) | 751 (12.7) | 1216 (12.5) | 90 568 (18.9) |
| <20 | 246 (6.4) | 460 (7.8) | 706 (7.3) | 80 656 (16.9) |
| Maternal | ||||
| Smoking | 43 (1.1) | 99 (1.6) | 142 (1.4) | 50 929 (10.2) |
| Alcohol consumption | 43 (1.1) | 57 (0.9) | 100 (1.0) | 9936 (2.0) |
| Social drug use | 8 (0.2) | 31 (0.5) | 39 (0.4) | 9962 (2.0) |
| Folic acid intake | 2919 (74.1) | 4536 (73.0) | 7455 (73.5) | 348 655 (70.1) |
| Mental health illness during prepregnancy or pregnancy | ||||
| All types | 405 (10.3) | 706 (11.4) | 1111 (11.0) | 68 778 (13.8) |
| Schizophrenia or bipolar disorders | 10 (0.3) | 16 (0.3) | 26 (0.3) | 2698 (0.5) |
| Depression | 191 (4.9) | 356 (5.7) | 547 (5.4) | 34 633 (7.0) |
| Anxiety | 233 (5.9) | 366 (5.9) | 599 (5.9) | 34 738 (7.0) |
| Prematernal health condition | ||||
| Any | 1142 (29.0) | 1770 (28.5) | 2912 (28.7) | 86 304 (17.4) |
| Chronic hypertension | 74 (1.9) | 112 (1.8) | 186 (1.8) | 4563 (0.9) |
| Diabetes, type 1 or type 2 | 37 (0.9) | 91 (1.5) | 128 (1.3) | 4846 (1.0) |
| History of disease | ||||
| Heart | 126 (3.2) | 195 (3.1) | 321 (3.2) | 10 108 (2.0) |
| Pulmonary | 108 (2.7) | 213 (3.4) | 321 (3.2) | 19 570 (3.9) |
| Endocrine | 584 (14.8) | 856 (13.8) | 1440 (14.2) | 22 445 (4.5) |
| Twin birth | 687 (17.5) | 1194 (19.2) | 1881 (18.5) | 7082 (1.4) |
Abbreviations: ART, assisted reproductive technology; ICSI, intracytoplasmic sperm injection; IVF, in vitro fertilization.
Data are presented as number (percentage) of women unless otherwise indicated. Only singleton or twin births were included in this cohort (N = 507 390); 71 records were excluded because of missing number of fetuses, and 185 records were excluded because the number of fetuses was more than 2. Percentages were calculated after missing values on individual variables were excluded from the group denominators showing on top of the table.
Obesity defined as body mass index of at least 30 (calculated as weight in kilograms divided by height in meters squared).
Association of CHD With Potential Confounding Risk Factors
Table 2 shows the association of CHD found in infants with potential maternal confounding risk factors. The prevalence of CHD was higher among infants born to older mothers (adjusted OR, 1.40 [95% CI, 1.31-1.51] for women >35 years vs <30 years); lower-income mothers (adjusted OR, 1.10 [95% CI, 1.00-1.20] for women of family income at 40%-59% levels; 1.06 [95% CI, 0.96-1.16] at 20%-39% levels; and 1.12 [95% CI, 1.02-1.22] at <20% levels compared with women of family income >80% level); mothers residing in lower-educational-level neighborhoods (adjusted OR, 1.13 [95% CI, 1.04-1.24] for women residing in neighborhoods at 60%-80% levels of university degree; 1.19 [95% CI, 1.09-1.31] at 40%-59% levels; 1.27 [95% CI, 1.16-1.40] at 20%-39% levels; and 1.28 [95% CI, 1.16-1.41] at <20% levels compared with women residing in >80% level neighborhoods); those who smoked or used drugs or consumed alcohol (adjusted OR, 1.39 [95% CI, 1.30-1.50] compared with those who did not); those who did not receive folic acid during pregnancy (adjusted OR, 1.08 [95% CI, 1.02-1.14] compared with those who did); those who had major physical problems (adjusted OR, 1.77 [95% CI, 1.67-1.88] compared with those who did not); those who had major mental health problems (adjusted OR, 1.26 [95% CI, 1.18-1.35] compared with those who did not); and those with obesity (adjusted OR, 1.21 [95% CI, 1.13-1.30] compared with those who were nonobese).
Table 2. Association of Congenital Heart Defects With Potential Confounding Risk Factors Among Non-ART Pregnanciesa.
| Exposure | Total No. | Congenital Heart Defects, No. (%) | OR (95% CI) | |
|---|---|---|---|---|
| Crude | Adjusted | |||
| Maternal age, y | ||||
| <30 | 209 661 | 2491 (1.2) | 1 [Reference] | 1 [Reference] |
| 30-34 | 205 291 | 2285 (1.1) | 0.94 (0.88-0.99) | 1.02 (0.96-1.08) |
| >35 | 82 198 | 1275 (1.6) | 1.31 (1.22-1.4) | 1.40 (1.31-1.51) |
| Missing data | 91 | 6 (6.6) | NA | NA |
| Parity | ||||
| None | 209 768 | 2454 (1.2) | 0.93 (0.88-0.98) | 0.99 (0.93-1.04) |
| ≥1 | 279 673 | 3524 (1.3) | 1 [Reference] | 1 [Reference] |
| Missing data | 7800 | 79 (1.0) | NA | NA |
| Family income at dissemination-area level, median, % | ||||
| >80 | 77 548 | 838 (1.1) | 1 [Reference] | 1 [Reference] |
| 60-80 | 109 972 | 1190 (1.1) | 1.00 (0.92-1.09) | 0.96 (0.87-1.05) |
| 40-59 | 90 770 | 1170 (1.3) | 1.20 (1.09-1.31) | 1.10 (1.00-1.20) |
| 20-39 | 85 745 | 1092 (1.3) | 1.18 (1.08-1.29) | 1.06 (0.96-1.16) |
| <20 | 110 344 | 1508 (1.4) | 1.27 (1.17-1.38) | 1.12 (1.02-1.22) |
| Missing data | 22 862 | 259 (1.1) | NA | NA |
| University degree at dissemination-area level, % | ||||
| >80 | 87 828 | 877 (1.0) | 1 [Reference] | 1 [Reference] |
| 60-80 | 114 984 | 1304 (1.1) | 1.14 (1.04-1.24) | 1.13 (1.04-1.24) |
| 40-59 | 104 229 | 1281 (1.2) | 1.23 (1.13-1.34) | 1.19 (1.09-1.31) |
| 20-39 | 90 568 | 1233 (1.4) | 1.37 (1.25-1.49) | 1.27 (1.16-1.40) |
| <20 | 80 656 | 1163 (1.4) | 1.45 (1.33-1.58) | 1.28 (1.16-1.41) |
| Missing data | 18 976 | 199 (1.1) | NA | NA |
| Maternal smoking, social drug use, or alcohol consumption | ||||
| Yes | 60 310 | 1081 (1.8) | 1.58 (1.48-1.69) | 1.39 (1.30-1.50) |
| No | 436 931 | 4976 (1.1) | 1 [Reference] | 1 [Reference] |
| Folic acid intake during pregnancy | ||||
| Yes | 348 655 | 4186 (1.2) | 1 [Reference] | 1 [Reference] |
| No | 148 586 | 1871 (1.3) | 1.05 (0.99-1.11) | 1.08 (1.02-1.14) |
| All types of mental health illness during prepregnancy or pregnancy | ||||
| Yes | 68 778 | 1181 (1.7) | 1.52 (1.42-1.62) | 1.26 (1.18-1.35) |
| No | 428 463 | 4876 (1.1) | 1 [Reference] | 1 [Reference] |
| All types of prepregnancy maternal health conditions | ||||
| Yes | 86 304 | 1716 (2.0) | 1.90 (1.80-2.01) | 1.77 (1.67-1.88) |
| No | 410 937 | 4341 (1.1) | 1 [Reference] | 1 [Reference] |
| Maternal prepregnancy obesity, body mass indexb | ||||
| Obese | 77 034 | 1196 (1.6) | 1.37 (1.28-1.46) | 1.21 (1.13-1.30) |
| Nonobese | 348 386 | 3973 (1.1) | 1 [Reference] | 1 [Reference] |
| Missing data | 71 821 | 888 (1.2) | NA | NA |
Abbreviations: ART, assisted reproductive technology; NA, not applicable; OR, odds ratio.
Adjusted ORs and 95% CIs were generated from 1 logistic regression model adjusting for all independent variables listed in the table simultaneously.
Obesity defined as body mass index of at least 30 (calculated as weight in kilograms divided by height in meters squared).
Association of CHD With ART and Twin Pregnancies
Table 3 displays the results of the analysis of the association of CHD with ART and twinning and ART-twin interactions. Infants born to mothers who conceived by ART had a higher prevalence of CHD than did infants born to mothers who conceived without using ART (2.2% [223 of 10 149] vs 1.2% [6057 of 497 241]; crude OR, 1.82; 95% CI, 1.59-2.09). This association decreased after adjusting for several risk factors simultaneously. For specific ART techniques, infants born to mothers who conceived by ICSI had higher risk of CHD than did infants born to mothers who conceived by IVF (2.3% vs 2.1%). Twins had a higher prevalence of CHD than singletons (5.5% vs 1.2%; OR, 4.91; 95% CI, 4.47-5.40). This association decreased after adjusting for several risk factors simultaneously. Prevalence of CHD was the highest in non-ART twin pregnancies (5.6%), second highest in ART twin pregnancies (5.1%), second lowest in ART singleton pregnancies (1.6%), and lowest in non-ART singleton pregnancies (1.2%).
Table 3. Association of Congenital Heart Defects With ART and Twin Status.
| Exposure Status | Congenital Heart Defects, No. (%) | Risk Difference vs Reference | OR (95% CI) | |
|---|---|---|---|---|
| Crude | Adjusted | |||
| Main Associationsa | ||||
| Intracytoplasmic sperm injection (n = 3938) | 91 (2.3) | 1.1 | 1.92 (1.56-2.37) | 1.82 (1.47-2.25) |
| In vitro fertilization (n = 6211) | 132 (2.1) | 0.9 | 1.76 (1.48-2.10) | 1.63 (1.36-1.94) |
| Overall ART (n = 10 149) | 223 (2.2) | 1.0 | 1.82 (1.59-2.09) | 1.70 (1.48-1.95) |
| Non-ART pregnancies (n = 497 241)b | 6057 (1.2) | [Reference] | 1 [Reference] | 1 [Reference] |
| Twins (n = 8963) | 489 (5.5) | 4.3 | 4.91 (4.47-5.40) | 4.69 (4.24-5.18) |
| Singletons (n = 498 427) | 5791 (1.2) | [Reference] | 1 [Reference] | 1 [Reference] |
| ART-Twin Interactionb | ||||
| ART pregnancies | ||||
| Twin (n = 1881) | 95 (5.1) | 3.9 | 4.55 (3.70-5.60) | 4.29 (3.47-5.30) |
| Singleton (n = 8268) | 128 (1.6) | 0.4 | 1.35 (1.13-1.61) | 1.26 (1.05-1.51) |
| Non-ART pregnancies | ||||
| Twin (n = 7082) | 394 (5.6) | 4.4 | 5.04 (4.54-5.60) | 4.93 (4.43-5.47) |
| Singleton (n = 490 159) | 5663 (1.2) | [Reference] | 1 [Reference] | 1 [Reference] |
Abbreviations: ART, assisted reproductive technology; OR, odds ratio.
Adjusted covariates included maternal age; parity; quintiles of median family income at the dissemination-area level; quintile of percentage of university degree at the dissemination-area level; prepregnancy obesity; folic acid intake during pregnancy; maternal smoking, social drug use, and alcohol consumption; mental health illness during prepregnancy or pregnancy; and prepregnancy health condition and obesity status.
Adjusted for ART in addition to all covariates listed above.
Mediation Analysis
Table 4 presents results of mediation analysis with twinning acting as the mediator between ART and CHD. The results showed that the association between ART and CHD was largely mediated by twinning (adjusted OR, 1.68; 95% CI, 1.44-1.92). The OR of the natural direct association of ART with CHD among singleton pregnancies was 1.09 (95% CI, 0.93-1.25).
Table 4. Analysis of ART and Congenital Heart Defects Association With Twin Pregnancy as a Mediatora.
| Mediation Association | Estimate, Odds Ratio (95% CI) |
|---|---|
| Total | 1.68 (1.44-1.92) |
| Natural direct | 1.09 (0.93-1.25) |
| Natural indirect | 1.55 (1.47-1.62) |
Abbreviation: ART, assisted reproductive technology.
The proportion mediated was 87.3%. Exposure variable: ART; mediator: twin pregnancy; interaction: ART × twin pregnancy; and covariates: maternal age; parity; quintiles of median family income at the dissemination-area level; quintile of percentage of university degree at the dissemination-area level; prepregnancy obesity; maternal smoking, social drug use, or alcohol consumption; folic acid intake during pregnancy; all types of mental health illness during prepregnancy or pregnancy; and all types of prepregnancy maternal health conditions.
The results of 4-way decompositions analysis found that reference interaction and mediated interaction together accounted for 7.9% of the total association, and neither component was statistically significantly different from 0. Mediation through twinning accounted for more than 80% of the excess association (eTable 2 in the Supplement). Results of multiple logistical regression analysis deleting missing data or restricting to pregnancy outcome yielded similar results in terms of direction and magnitude of the association of CHD with ART and twinning (eTable 3 in the Supplement).
Discussion
This large population-based study found that compared with infants born to mothers who conceived without using ART, infants born to mothers who conceived with ART were at higher risk of CHD. The association between ART and CHD was largely mediated by twinning. The contributions to overall excess risk from other associations of ART (not involving twinning) and from the ART-twin interaction were smaller and not statistically significant. However, the results do not rule out possible small contributions of those mechanisms to excess risk.
Our mediation analysis is different from previous studies of the contribution of twinning in the literature. Previous studies40,41,42,43 have used different strategies to analyze the association of ART, twinning, and CHD, with most considering twinning as a confounder. Treating a mediator as a confounder in an analysis is flawed.40,41,42,43 Mediation analysis helped to assess the association between ART (exposure) and CHD (outcome). We believe that ignoring twinning as a mediator would lead to unexplainable or paradoxical findings. The finding that twinning contributed up to 87% of the association between ART and CHD may be important in the clinical practice of perinatal medicine. For example, instead of performing fetal echocardiography in ART pregnancies,32 it may be more cost-efficient to perform this procedure in twin pregnancies. Policy makers may consider a policy of single embryo transfer. Since 2015, Ontario government-provided public funding for IVF treatment required single embryo transfer in most women younger than 38 years.48 Some other adverse perinatal outcomes may share mechanisms of CHD,49 and a similar analytic strategy could be applied in future studies to assess these associations as well.
Strengths and Limitations
Our study has several strengths. First, the study sample was based on the entire population from 1 Canadian province (Ontario). Because BORN has 100% capture for hospital and home births in Ontario, our study was free from bias caused by selective inclusion of births. Second, the quality of BORN data has been evaluated by a number of studies,50 and it has been considered to be high. Third, the sample size of our study was the largest reported to date in this field. Fourth, we used multiple sources to identify CHD, including birth records, pregnancies that were lost or terminated after prenatal screening and in antenatal clinics (a total of 198 CHD cases were ascertained from losses or terminations), and cases diagnosed after birth (≤1 year) through record linkage with CIHI databases, with better ascertainment of outcome. Ascertainment of CHD cases in aborted fetuses might be more complete in ART pregnancies than in non-ART pregnancies, resulting in an artificially higher prevalence of CHD after ART. To address this possibility, we performed a sensitivity analysis restricted to pregnancy outcomes. The result of this sensitivity analysis was similar to the main results (eTable 3 in the Supplement), suggesting that ascertainment bias is not a serious threat to the validity of our study results. Fifth, rich demographic and clinical information collected by BORN allowed a thorough adjustment for confounding, assessment of mediation, and subgroup analyses. The use of mediation analysis helped to sort the associations of ART with twinning and CHD. Although the data contain no information on infertility, some important risk factors that are associated with both infertility and CHD have been adjusted. As a result, we were able to control some of the confounding by infertility, although not completely.
Several limitations of our study should be recognized. First, some important variables, such as ethnicity, household income, and maternal education, were either not available or not measured at an individual level. Second, the higher socioeconomic status and healthy behaviors of couples who underwent ART compared with couples who conceived without ART may confound the observed results. Although we adjusted several maternal characteristics to mitigate confounding, administrative data cannot guarantee complete and accurate data collection. As a result, residual confounding may still exist. As VanderWeele and Ding50 suggested, a central concern about observational data are unmeasured or uncontrolled confounding, and with observational data, we can never be certain that the adjustments are adequate.51 Third, we were not able to address the issue of donor gametes, which may have a different association with the outcome for ART pregnancies compared with own gametes.1 Fourth, there were missing values for variables included in the regression analysis. We used multiple imputation to create a complete data set to mitigate the consequences of missing values in the analysis. However, analysis deleting records with missing variables or deleting CHDs ascertained from fetal losses or termination yielded similar results, suggesting the robustness of the data used in this study. Fifth, if the ART-twin interaction was present, both the natural indirect association and the natural direct association depended on the population frequency of twinning.43 The ART-twin interaction was small and not clinically significant, whereas the difference between the natural direct association and the natural indirect association was large and clinically significant, and the interpretation of the natural direct association and the natural indirect association was unaffected by the ART-twin interaction. Sixth, we were not able to address zygosity and chronicity of twins. Because the main focus of this study was the indirect association of twinning with CHD and ART, and zygosity and chronicity of twins may be a lesser concern in the assessment of indirect association than an assessment of direct association. Seventh, because CARTR Plus data on IVF cycles is not completely captured by BORN, we used information from BORN to supplement the ascertainment of ART. As a result, some ICSI cases in BORN may have been misclassified as IVF because BORN data sometimes lack details to differentiate ICSI from IVF. Because the focus of this study was an ART and non-ART comparison, it may be acceptable to have some IVF or ICSI misclassification to ensure a complete ascertainment of ART.
Conclusions
This study found that the observed association between ART and CHD may be substantially mediated by twinning. We believe that this finding is important to the clinical practice of perinatal medicine and to policy making. The robustness of this analytic strategy should be tested in the assessment of the association of ART with CHD in other populations and ART with other perinatal outcomes that may share similar mechanisms of CHD.
eMethods. Description of Missing Imputation Process
eTable 1. ICD-10-CA Diagnosis Code for CHD in CIHI DAD and NACRS Databases
eTable 2. Four-way Decompositions of Risk Difference
eTable 3. Results of Sensitivity Analysis for the Association of ART with CHD, Ontario, Canada, April 1, 2012, and October 31, 2015
eFigure. Record Linkage Strategy for the Study of the Association between ART and CHD, Ontario, Canada, April 1, 2012, to October 31, 2015
References
- 1.Allen VM, Wilson RD, Cheung A; Genetics Committee; Reproductive Endocrinology and Infertility Committee . Pregnancy outcomes after assisted reproductive technology. J Obstet Gynaecol Can. 2006;28(3):220-233. doi: 10.1016/S1701-2163(16)32112-0 [DOI] [PubMed] [Google Scholar]
- 2.Toner JP, Coddington CC, Doody K, et al. . Society for Assisted Reproductive Technology and assisted reproductive technology in the United States: a 2016 update. Fertil Steril. 2016;106(3):541-546. doi: 10.1016/j.fertnstert.2016.05.026 [DOI] [PubMed] [Google Scholar]
- 3.Bahtiyar MO, Campbell K, Dulay AT, et al. . Is the rate of congenital heart defects detected by fetal echocardiography among pregnancies conceived by in vitro fertilization really increased? a case-historical control study. J Ultrasound Med. 2010;29(6):917-922. doi: 10.7863/jum.2010.29.6.917 [DOI] [PubMed] [Google Scholar]
- 4.Giorgione V, Parazzini F, Fesslova V, et al. . Congenital heart defects in IVF/ICSI pregnancy: systematic review and meta-analysis. Ultrasound Obstet Gynecol. 2018;51(1):33-42. doi: 10.1002/uog.18932 [DOI] [PubMed] [Google Scholar]
- 5.Hansen M, Kurinczuk JJ, Bower C, Webb S. The risk of major birth defects after intracytoplasmic sperm injection and in vitro fertilization. N Engl J Med. 2002;346(10):725-730. doi: 10.1056/NEJMoa010035 [DOI] [PubMed] [Google Scholar]
- 6.Hansen M, Bower C, Milne E, de Klerk N, Kurinczuk JJ. Assisted reproductive technologies and the risk of birth defects—a systematic review. Hum Reprod. 2005;20(2):328-338. doi: 10.1093/humrep/deh593 [DOI] [PubMed] [Google Scholar]
- 7.Hansen M, Kurinczuk JJ, Milne E, de Klerk N, Bower C. Assisted reproductive technology and birth defects: a systematic review and meta-analysis. Hum Reprod Update. 2013;19(4):330-353. doi: 10.1093/humupd/dmt006 [DOI] [PubMed] [Google Scholar]
- 8.Lancaster PA. Congenital malformations after in-vitro fertilisation. Lancet. 1987;2(8572):1392-1393. doi: 10.1016/S0140-6736(87)91277-3 [DOI] [PubMed] [Google Scholar]
- 9.Wen SW, Leader A, White RR, et al. . A comprehensive assessment of outcomes in pregnancies conceived by in vitro fertilization/intracytoplasmic sperm injection. Eur J Obstet Gynecol Reprod Biol. 2010;150(2):160-165. doi: 10.1016/j.ejogrb.2010.02.028 [DOI] [PubMed] [Google Scholar]
- 10.Panagiotopoulou O, Fouzas S, Sinopidis X, Mantagos SP, Dimitriou G, Karatza AA. Congenital heart disease in twins: the contribution of type of conception and chorionicity. Int J Cardiol. 2016;218:144-149. doi: 10.1016/j.ijcard.2016.05.029 [DOI] [PubMed] [Google Scholar]
- 11.Votava-Smith JK, Glickstein JS, Simpson LL, Williams IA. Comparison of method of conception in fetuses undergoing echocardiography at a tertiary referral center. Prenat Diagn. 2014;34(5):445-449. doi: 10.1002/pd.4327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tararbit K, Houyel L, Bonnet D, et al. . Risk of congenital heart defects associated with assisted reproductive technologies: a population-based evaluation. Eur Heart J. 2011;32(4):500-508. doi: 10.1093/eurheartj/ehq440 [DOI] [PubMed] [Google Scholar]
- 13.Tararbit K, Lelong N, Thieulin AC, et al. ; EPICARD Study Group . The risk for four specific congenital heart defects associated with assisted reproductive techniques: a population-based evaluation. Hum Reprod. 2013;28(2):367-374. doi: 10.1093/humrep/des400 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tararbit K, Lelong N, Houyel L, Bonnet D, Goffinet F, Khoshnood B; EPICARD Study Group . Assessing the role of multiple pregnancies in the association between tetralogy of Fallot and assisted reproductive techniques: a path-analysis approach. Orphanet J Rare Dis. 2014;9:27. doi: 10.1186/1750-1172-9-27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Davies MJ, Moore VM, Willson KJ, et al. . Reproductive technologies and the risk of birth defects. N Engl J Med. 2012;366(19):1803-1813. doi: 10.1056/NEJMoa1008095 [DOI] [PubMed] [Google Scholar]
- 16.Simeone RM, Tinker SC, Gilboa SM, et al. ; National Birth Defects Prevention Study . Proportion of selected congenital heart defects attributable to recognized risk factors. Ann Epidemiol. 2016;26(12):838-845. doi: 10.1016/j.annepidem.2016.10.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cedergren MI, Källén BA. Maternal obesity and infant heart defects. Obes Res. 2003;11(9):1065-1071. doi: 10.1038/oby.2003.146 [DOI] [PubMed] [Google Scholar]
- 18.Pasquali R, Patton L, Gambineri A. Obesity and infertility. Curr Opin Endocrinol Diabetes Obes. 2007;14(6):482-487. doi: 10.1097/MED.0b013e3282f1d6cb [DOI] [PubMed] [Google Scholar]
- 19.Hur YM, Song TB. A recent rise in twin birth rates and demographic changes in mothers of twins in South Korea: 2003-2007. Twin Res Hum Genet. 2009;12(1):118-122. doi: 10.1375/twin.12.1.118 [DOI] [PubMed] [Google Scholar]
- 20.Kurosawa K, Masuno M, Kuroki Y. Trends in occurrence of twin births in Japan. Am J Med Genet A. 2012;158A(1):75-77. doi: 10.1002/ajmg.a.34362 [DOI] [PubMed] [Google Scholar]
- 21.Dawson AL, Tinker SC, Jamieson DJ, et al. ; National Birth Defects Prevention Study . Twinning and major birth defects, National Birth Defects Prevention Study, 1997-2007. J Epidemiol Community Health. 2016;70(11):1114-1121. doi: 10.1136/jech-2015-206302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Huang CT, Au HK, Chien LW, Chang CW, Chien YY, Tzeng CR. Twin pregnancy outcome among cases of spontaneous conception, intrauterine insemination, and in vitro fertilization/intracytoplasmic sperm injection. Fertil Steril. 2006;86(4):1017-1019. doi: 10.1016/j.fertnstert.2006.02.109 [DOI] [PubMed] [Google Scholar]
- 23.Thurin A, Hausken J, Hillensjö T, et al. . Elective single-embryo transfer versus double-embryo transfer in in vitro fertilization. N Engl J Med. 2004;351(23):2392-2402. doi: 10.1056/NEJMoa041032 [DOI] [PubMed] [Google Scholar]
- 24.Koudstaal J, Bruinse HW, Helmerhorst FM, Vermeiden JP, Willemsen WN, Visser GH. Obstetric outcome of twin pregnancies after in-vitro fertilization: a matched control study in four Dutch university hospitals. Hum Reprod. 2000;15(4):935-940. doi: 10.1093/humrep/15.4.935 [DOI] [PubMed] [Google Scholar]
- 25.Pharoah PO. Twins and cerebral palsy. Acta Paediatr Suppl. 2001;90(436):6-10. doi: 10.1111/j.1651-2227.2001.tb01620.x [DOI] [PubMed] [Google Scholar]
- 26.Hardin J, Carmichael SL, Selvin S, Lammer EJ, Shaw GM. Increased prevalence of cardiovascular defects among 56,709 California twin pairs. Am J Med Genet A. 2009;149A(5):877-886. doi: 10.1002/ajmg.a.32745 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bernier PL, Stefanescu A, Samoukovic G, Tchervenkov CI. The challenge of congenital heart disease worldwide: epidemiologic and demographic facts. Semin Thorac Cardiovasc Surg Pediatr Card Surg Annu. 2010;13(1):26-34. doi: 10.1053/j.pcsu.2010.02.005 [DOI] [PubMed] [Google Scholar]
- 28.Canobbio MM. Health care issues facing adolescents with congenital heart disease. J Pediatr Nurs. 2001;16(5):363-370. doi: 10.1053/jpdn.2001.26570 [DOI] [PubMed] [Google Scholar]
- 29.Lui GK, Rogers IS, Ding VY, et al. . Risk estimates for atherosclerotic cardiovascular disease in adults with congenital heart disease. Am J Cardiol. 2017;119(1):112-118. doi: 10.1016/j.amjcard.2016.09.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jay PY, Akhirome E, Magnan RA, et al. . Transgenerational cardiology: one way to a baby’s heart is through the mother. Mol Cell Endocrinol. 2016;435:94-102. doi: 10.1016/j.mce.2016.08.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kloesel B, DiNardo JA, Body SC. Cardiac embryology and molecular mechanisms of congenital heart disease: a primer for anesthesiologists. Anesth Analg. 2016;123(3):551-569. doi: 10.1213/ANE.0000000000001451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.American Institute of Ultrasound in Medicine AIUM practice parameter for the performance of fetal echocardiography. J Ultrasound Med. 2020;39(1):E5-E16. [DOI] [PubMed] [Google Scholar]
- 33.Better Outcomes Registry & Network (BORN). Ottawa, Ontario, Canada. http://www.bornontario.ca. Accessed March 25, 2019.
- 34.Centers for Disease Control and Prevention, US Department of Health & Human Services Assisted reproductive technology (ART). https://www.cdc.gov/art/whatis.html. Accessed March 25, 2019.
- 35.Zhai D, Guo Y, Smith G, Krewski D, Walker M, Wen SW. Maternal exposure to moderate ambient carbon monoxide is associated with decreased risk of preeclampsia. Am J Obstet Gynecol. 2012;207(1):57.e1-57.e9. doi: 10.1016/j.ajog.2012.03.022 [DOI] [PubMed] [Google Scholar]
- 36.Wilkins R, Khan S Automated geographic coding based on the statistics Canada postal code conversion files: including postal codes through October 2010. https://mdl.library.utoronto.ca/sites/default/files/mdldata/open/canada/national/statcan/postalcodes/pccfplus/2006/2010oct/MSWORD.PCCF5H.pdf. Accessed July 15, 2019.
- 37.Hernán MA, Hernández-Díaz S, Werler MM, Mitchell AA. Causal knowledge as a prerequisite for confounding evaluation: an application to birth defects epidemiology. Am J Epidemiol. 2002;155(2):176-184. doi: 10.1093/aje/155.2.176 [DOI] [PubMed] [Google Scholar]
- 38.Schisterman EF, Cole SR, Platt RW. Overadjustment bias and unnecessary adjustment in epidemiologic studies. Epidemiology. 2009;20(4):488-495. doi: 10.1097/EDE.0b013e3181a819a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rothman KJ, Greenland S, Lash TL. Modern Epidemiology. 3rd ed New York, NY: Wolters Kluwer/Lippincott Williams & Wilkins; 2008. [Google Scholar]
- 40.VanderWeele TJ. Explanation in Causal Inference: Methods for Mediation and Interaction. New York, NY: Oxford University Press, 2015. [Google Scholar]
- 41.VanderWeele TJ. Mediation analysis: a practitioner’s guide. Annu Rev Public Health. 2016;37:17-32. doi: 10.1146/annurev-publhealth-032315-021402 [DOI] [PubMed] [Google Scholar]
- 42.VanderWeele TJ. A unification of mediation and interaction: a 4-way decomposition. Epidemiology. 2014;25(5):749-761. doi: 10.1097/EDE.0000000000000121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Richiardi L, Bellocco R, Zugna D. Mediation analysis in epidemiology: methods, interpretation and bias. Int J Epidemiol. 2013;42(5):1511-1519. doi: 10.1093/ije/dyt127 [DOI] [PubMed] [Google Scholar]
- 44.van Buuren S. Multiple imputation of discrete and continuous data by fully conditional specification. Stat Methods Med Res. 2007;16(3):219-242. doi: 10.1177/0962280206074463 [DOI] [PubMed] [Google Scholar]
- 45.Little RJA, Rubin DB. Statistical Analysis With Missing Data. 2nd ed New York, NY: John Wiley & Sons; 2002. doi: 10.1002/9781119013563 [DOI] [Google Scholar]
- 46.Rubin DB. Multiple Imputation for Nonresponse in Surveys. New York, NY: John Wiley & Sons Inc; 2004. [Google Scholar]
- 47.Muzyka D, Lypka M The benefits of keeping it casual: investigating stress mediated health outcomes with PROC CAUSALMED. https://www.sas.com/content/dam/SAS/support/en/sas-global-forum-proceedings/2019/3897-2019.pdf. Accessed July 15, 2019.
- 48.Procrea Fertility. Ontario treatment coverage and payment options. https://procrea.ca/financial-guidance/ontario-treatment-coverage-payment-options/ Accessed September 3, 2019.
- 49.Oberg AS, VanderWeele TJ, Almqvist C, Hernandez-Diaz S. Pregnancy complications following fertility treatment-disentangling the role of multiple gestation. Int J Epidemiol. 2018;47(4):1333-1342. doi: 10.1093/ije/dyy103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.VanderWeele TJ, Ding P. Sensitivity analysis in observational research: introducing the E-value. Ann Intern Med. 2017;167(4):268-274. doi: 10.7326/M16-2607 [DOI] [PubMed] [Google Scholar]
- 51.Better Outcomes Registry & Network. BORN data quality report, 2012-2014—executive summary. https://www.bornontario.ca/en/data/resources/Documents/BORN-Data-Quality-Report-2012-2014---Executive-Summary.pdf. Published April 2016. Accessed March 25, 2019.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods. Description of Missing Imputation Process
eTable 1. ICD-10-CA Diagnosis Code for CHD in CIHI DAD and NACRS Databases
eTable 2. Four-way Decompositions of Risk Difference
eTable 3. Results of Sensitivity Analysis for the Association of ART with CHD, Ontario, Canada, April 1, 2012, and October 31, 2015
eFigure. Record Linkage Strategy for the Study of the Association between ART and CHD, Ontario, Canada, April 1, 2012, to October 31, 2015