Abstract
Irritable bowel syndrome (IBS) is a common functional gastrointestinal disorder which accounts for a substantial proportion of a gastroenterologist’s time in the outpatient clinic. However, there is variability in approaches to diagnosis and investigation between physicians, dependent on expertise. Many patients express disappointment over the lack of a patient-centred approach. Consequently, there have been calls for the care of patients with IBS to be standardised, a process which aims to promote high-quality and high-value care. Making an early diagnosis, based on a clinical assessment of symptoms, while limiting use of investigations, are key tenets of this process. Exhaustive investigation to exclude all organic pathology is unnecessary, and may be counterproductive. Routine blood tests in suspected IBS have low yield, but are an acceptable part of routine practice. All patients should have coeliac serology tested, regardless of their predominant stool form. Patients with diarrhoea should have a faecal calprotectin measured, and should proceed to colonoscopy to exclude inflammatory bowel disease (IBD) if this is positive. Beyond this, the need for investigations should be made on a case-by-case basis, contingent on the reporting of known risk factors for organic pathology. Colonoscopy should be considered in any patient with alarm features for colorectal cancer, and in those whose clinical features are suggestive of microscopic colitis. A 23-seleno-25-homotaurocholic acid (SeHCAT) scan should be considered in patients with IBS-D, a third of whom may actually have bile acid diarrhoea. There is no role for routine hydrogen breath tests for lactose malabsorption or small intestinal bacterial overgrowth.
Keywords: irritable bowel syndrome
Introduction
Irritable bowel syndrome (IBS) is a common chronic functional gastrointestinal disorder, with an estimated population prevalence of 10%,1 which more commonly affects women2 and younger individuals.1 Patients with IBS experience abdominal pain in association with a change in the frequency or form of their stools, and are subdivided according to their predominant stool form into IBS with diarrhoea (IBS-D), constipation or a mixed stool pattern.3 The aetiology remains unclear, but a variety of factors have been implicated, including genetics, visceral hypersensitivity, disordered gastrointestinal motility, abnormalities of the brain–gut axis, and alterations in the gut microbiome.4 Although the identification of these potential pathophysiological mechanisms has yet to yield any useful diagnostic strategies for clinical practice, it does cast doubt on the concept that IBS is a purely functional condition.
Nonetheless, whatever uncertainties exist in our understanding of IBS, what is clear is that this disorder has a substantial impact on patients, many of whom report considerable impairment of quality of life as a consequence of their symptoms,5 and face daily challenges with working6 and socialising.7 This, in conjunction with other factors,8–11 such as the severity and chronicity of symptoms and fear of underlying organic disease, make individuals with IBS likely to seek the advice of a doctor. Up to 80% will consult in primary care,10 11 the majority of whom will be managed in this setting,12 but some will be referred for a specialist opinion.8 Consequently, patients with IBS account for between 10% and 25% of a gastroenterologist’s workload in the outpatient clinic.13 This highlights the importance of implementing a logical and evidenced-based approach to investigation and diagnosis.
Guidelines for the management of IBS advocate that a diagnosis is made on clinical grounds, without the need for exhaustive investigations in an attempt to rule out all possible organic pathology.14 15 Nevertheless, and due in part to the potential uncertainty that may surround the diagnosis, many physicians still consider IBS to be a diagnosis of exclusion.16 Although undertaking extensive testing may offer both the physician and the patient some reassurance, repeatedly normal investigations may instead make the patient feel that the cause of their symptoms remains elusive, or that organic disease has been ‘missed’. In preference, making an early and positive diagnosis of IBS following cogent use of limited investigations, together with a clear explanation, may help patients better accept the diagnosis and facilitate earlier treatment,17 as well as minimise associated healthcare costs.18 Indeed, direct care costs are considerable, estimated to be between £90 and £316 per patient per year in the UK,19 and close to $1 billion per annum in the USA.20
Unfortunately, patients with IBS often perceive a lack of a patient-centred approach to their care, and management strategies can vary between physicians, dependent on expertise. Consequently, there have been recent calls to standardise the management of patients with IBS, with a focus on early diagnosis, rational investigation and timely treatment, aiming to improve the overall quality and value of care in IBS.21 Accordingly, this review endeavours to present a practical and evidence-based approach to diagnosing and investigating IBS to assist physicians in their day-to-day clinical practice.
Making a diagnosis of IBS
A general approach
Making a diagnosis of IBS begins with a good clinical history. Questions should focus on establishing whether a patient has the cardinal symptoms of IBS: abdominal pain, often related to defaecation, which is associated with either a change in stool frequency, a change in stool form or both.3 Chronicity of symptoms should also be assessed, with attention paid to the presence of any alarm (red flag) features, such as weight loss or rectal bleeding. These raise concern for colorectal cancer (CRC), and require urgent lower gastrointestinal investigation, as per the National Institute for Health and Care Excellence (NICE) guidance (box 1).22 However, alarm features have only modest accuracy for predicting CRC, with sensitivity ranging from 5% for detection of an abdominal mass to 64% for rectal bleeding,23 and many patients with IBS will endorse them.24 Similarly, symptoms that are often felt to be associated with new onset IBD do not perform particularly well, with sensitivities ranging from 14.5% for mucus per rectum to 53% for abdominal pain once a week or more.25 Older patients (>50 years) presenting with a change in their bowel habit are likely to require further investigation before a diagnosis of IBS can be made.
Box 1. Alarm features raising concern for possible colorectal cancer22 .
Aged ≥40 with unexplained weight loss and abdominal pain.
Aged ≥50 with unexplained rectal bleeding.
Aged ≥60 with:
Iron deficiency anaemia.
Change in their bowel habit.
Tests show occult blood in faeces.
Aged <50 with rectal bleeding and any of the following unexplained symptoms or findings:
Abdominal pain.
Change in bowel habit.
Weight loss.
Iron deficiency anaemia.
Adults of any age with an abdominal or rectal mass.
Enquiring about a patient’s medical history is also important. In a patient with loose stools, a history of cholecystectomy or right hemicolectomy may suggest they have bile acid diarrhoea (BAD), rather than IBS-D. A family history of IBD, coeliac disease or CRC may also be relevant. Review of the patient’s medications might suggest drug-induced constipation, for example, secondary to opiates, or diarrhoea occurring as a side-effect of a drug such as metformin or an anti-depressant, particularly selective serotonin re-uptake inhibitors. Alternatively, it may identify use of non-steroidal anti-inflammatory drugs (NSAIDs) or proton-pump inhibitors (PPIs), which might indicate a diagnosis of microscopic colitis (MC), or NSAID-induced enteropathy.
Physical examination, including digital rectal examination (DRE), should be conducted to assist exclusion of organic gastrointestinal disease. A normal examination may be reassuring to both the physician and the patient, but, taken in isolation does not confirm a diagnosis of IBS. In patients with obstructive defaecation-type symptoms, pelvic dyssynergia should be considered; a DRE demonstrates paradoxical anal contraction on straining.26
Symptom-based diagnostic criteria
Manning and colleagues were the first to propose a method for diagnosing IBS based on the presence of certain gastrointestinal symptoms reported by the patient.27 These led on to the development of the Rome criteria which, over the past 20 years, have emerged as the accepted gold-standard for the diagnosis of IBS. The most recent iteration, Rome IV, were published in 2016,3 (box 2) and include a number of changes compared with their predecessor, the Rome III criteria.28 Unfortunately, their performance in diagnosing IBS is unclear, as they have not been validated in routine clinical practice. The Rome III criteria performed only modestly in previous validation studies in both the UK and Canada,29 30 although this can be augmented by incorporating blood results and other items from the clinical history.30
Box 2. The Rome IV criteria for the diagnosis of irritable bowel syndrome (IBS).
Rome IV IBS Diagnostic Criteria3
-
Recurrent abdominal pain, on average, at least 1 day per week in the last 3 months and associated with two or more or the following:
Related to defaecation.
Associated with a change in frequency of stool.
Associated with a change in stool form.
Criteria fulfilled for the last 3 months with symptom onset at least 6 months prior to diagnosis.
The Rome criteria were developed through a consensus of expert opinion among gastroenterologists and allied academics in the field of IBS.3 28 In primary care, surveys show that very few physicians are aware of, or use, symptom-based diagnostic criteria,31 yet they are still able to diagnose IBS with confidence, using a pragmatic approach.32 Nevertheless, management guidelines for IBS in both primary and secondary care recommend their use.14 15
Role of investigations in suspected IBS
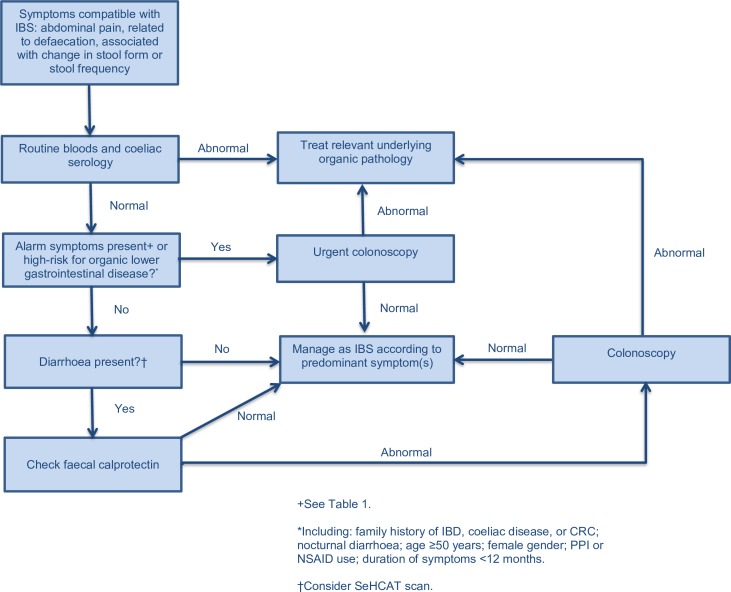
Careful deployment of investigations is important (see figure 1), as it has been suggested that repeated use of extraneous testing may lead to abnormal illness behaviour.17 A randomised controlled trial of a positive diagnostic strategy compared with exhaustive investigation in 302 patients with suspected IBS demonstrated higher costs and an extremely low yield for organic disease with exhaustive investigation, no difference in terms of effect on symptoms and similar rates of patient satisfaction.33
Figure 1.
Suggested diagnostic algorithm for patients with IBS. CRC, colorectal cancer; IBD, inflammatory bowel disease; IBS, irritable bowel syndrome; NSAID, non-steroidal anti-inflammatory disease; PPI, proton-pump inhibitor; SeHCAT, 23-seleno-25-homotaurocholic acid.
Routine blood tests
A panel of routine blood tests is commonly performed in patients with suspected IBS, often when they are first assessed and frequently prior to a referral to a gastroenterologist. However, in a study of 300 people with suspected IBS, measurements of C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) identified only three patients with organic disease, all of whom had IBD,34 and only one instance of organic pathology, biopsy-proven coeliac disease, following analysis of a full blood count (FBC). A meta-analysis of studies demonstrated a CRP <0.5 mg/dL in patients with typical IBS symptoms conferred a<1% risk of IBD, whereas ESR was of little clinical utility.35 Another study evaluating the yield of an FBC and serum biochemistry in 196 patients with IBS detected no cases of organic disease.36 In a pooled analysis of data from five studies examining yield of thyroid function tests (TFTs) in IBS, 91 of 1860 patients with IBS (4.2%) had an abnormal result37; the background prevalence of abnormal TFTs in the general population is almost identical. Overall, routine blood tests have a low yield in suspected IBS, but are an acceptable part of everyday clinical practice; a normal CRP appears to be reassuring.
Testing for coeliac disease
British Society of Gastroenterology guidelines for the management of coeliac disease recommend serological screening for the condition in any patient with suspected IBS.38 A recently updated meta-analysis identified 12 case-control studies, recruiting patients with suspected IBS and healthy controls, in whom testing for possible coeliac disease was conducted.39 Overall, odds of positive coeliac serology was almost three times higher, and odds of biopsy-proven coeliac disease more than four times higher, in patients with suspected IBS compared with healthy controls. This was the case irrespective of the patient’s predominant stool form. These findings support serological screening for coeliac disease among all patients with IBS-type symptoms in secondary care. However, the yield in population-based studies was lower40 41; the role of screening in a community setting remains uncertain.
Faecal calprotectin
IBD is an important differential for patients with suspected IBS-D. However, undertaking a colonoscopy, which is invasive and time-consuming, in all patients is neither feasible nor desirable, as it will be normal in a large proportion of those tested.42 Faecal calprotectin (FC), a protein found in the cytosol of inflammatory cells, can be detected in stool,43 and provides a non-invasive method for detecting possible IBD, and prioritising need for colonoscopy. Typically, this strategy is employed in primary care, as recommended by NICE and, until recently, a cut-off of ≥50 mcg/g was used for referral.44
In a meta-analysis of six studies, including 671 adults with suspected IBD, all of whom underwent FC testing and colonoscopy, the authors reported a pooled sensitivity and specificity of FC for the diagnosis of IBD of 93% and 96%, respectively.45 Using FC to screen those with suspected IBD would lead to a 67% reduction in the number of patients requiring colonoscopy but, in a small proportion of individuals, a diagnosis of IBD will be delayed due to a false negative result.
In primary care, lower gastrointestinal symptoms are common, but prevalence of IBD is low. Consequently, a 50 mcg/g cut-off for abnormal FC results in a high proportion of false positive tests among patients with IBS.46 An updated FC pathway, advocated by National Health Service England and endorsed by NICE,47 has been evaluated in over 1000 adult primary care patients with lower gastrointestinal symptoms.46 In patients with no alarm features, normal routine bloods and negative coeliac serology, an FC cut-off <100 mcg/g identified IBS with 98% certainty. For a FC of ≥100 mcg/g, repeat testing was recommended, with a referral to gastroenterology if persistently elevated. Overall, FC testing in patients with diarrhoea can facilitate a positive diagnosis of IBS-D without recourse to colonoscopy, while identifying the minority with possible IBD who require further investigation.
Colonoscopy
Despite advice to the contrary, colonoscopy is commonly performed in patients with suspected IBS. A national survey in the USA highlighted that around 25% of all colonoscopies were performed in patients with typical symptoms of IBS.48 In a prospective case-control study, enrolling 466 patients with suspected non-constipated IBS without alarm features there was no significant difference in the prevalence of structural abnormalities of the colon, when compared with 451 controls undergoing colonoscopy for CRC screening or polyp surveillance.49 There were seven cases of MC, but no cases of CRC, and only two individuals were found to have IBD.
A cross-sectional survey of over 4000 patients undergoing colonoscopy for assessment of lower gastrointestinal symptoms demonstrated no significant difference in the prevalence of organic disease between 203 patients who met the Rome III criteria for IBS and 3975 individuals who did not.50 Overall, 21 cases of organic disease were identified in those with suspected IBS, including five cases of CRC. However, around 70% of the cohort meeting Rome III criteria were over 50, and all five CRCs occurred in this group. These findings support lower gastrointestinal investigation in older patients with IBS-type symptoms.
Patients with MC can present with similar symptoms to IBS,51 but determining who should be referred for colonoscopy can be difficult. One study demonstrated that in patients with chronic diarrhoea, age ≥50 years, female sex, use of PPIs or NSAIDs, weight loss and absence of abdominal pain were significantly associated with biopsy-proven MC.52 In another study, presence of nocturnal stools and having diarrhoea for less than 12 months at presentation were also identified as independent predictors of MC.53
In spite of the low yield for organic pathology in suspected IBS without alarm features, some would argue a negative colonoscopy is reassuring for the patient. However, a study in 458 patients with IBS challenges this idea; there was no evidence of an independent association between a negative colonoscopy and reassurance, nor any evidence of an improvement in health-related quality of life.54 On the basis of available evidence, performing a colonoscopy in younger individuals with suspected IBS, without alarm features, cannot be recommended as it has a very low yield for organic disease. It should be reserved for older individuals or those with abnormal FC, alarm features, including a recent change in bowel habit, or features suggestive of MC.
23-Seleno-25-homotaurocholic acid scanning
BAD is common; the population prevalence is approximately 1%.55 It can be diagnosed using 23-seleno-25-homotaurocholic acid (SeHCAT) scanning, although access remains an issue in some parts of the UK.56 Among patients with IBS-D, a substantial proportion may have BAD, making this an important differential diagnosis, particularly as it can be treated effectively with bile acid sequestrants.
A meta-analysis, published in 2009, suggested that one in four patients with symptoms compatible with IBS-D had evidence of BAD, defined as a SeHCAT retention of <15% at 7 days.57 However, many of the included studies did not apply accepted symptom-based diagnostic criteria to define IBS, meaning that patients with chronic painless diarrhoea were likely included. This could have led to an overestimation of the prevalence of BAD. However, the findings of prospective studies using the Rome criteria are corroborative of this meta-analysis, with one study recruiting 118 patients with Rome III-defined IBS demonstrating BAD in 28 (23.7%) patients,58 and another conducted in 141 patients with Rome II-defined IBS reporting moderate BAD, with a SeHCAT retention of <10%, in 26 (18.4%).59 An updated meta-analysis, incorporating these studies with others using recognised diagnostic criteria to define IBS, reported a pooled prevalence of BAD in patients with IBS of 28%.60
Some clinicians may prefer to undertake a therapeutic trial of a bile acid sequestrant rather than requesting a SeHCAT scan. However, this approach risks missing a diagnosis of BAD if the dose used is suboptimal, or if patients discontinue treatment due to side-effects. In one study, 44% of patients with BAD confirmed by SeHCAT testing failed to respond to colestyramine.61 One study demonstrated that higher body mass index predicted presence of BAD in IBS-D58; however, it is unclear which other patient characteristics, if any, can discriminate patients with BAD from IBS-D. Overall, due to the relatively high yield, referring patients with suspected IBS-D for a SeHCAT scan, where available, is probably advisable.
Hydrogen breath test for lactose intolerance
A hydrogen breath test (HBT) can be used to screen for lactose malabsorption, which, if associated with clinical symptoms, such as bloating and abdominal pain, is referred to as lactose intolerance. A recent meta-analysis of 14 case–control studies, the majority of which diagnosed lactose malabsorption using a HBT, reported that prevalence of lactose malabsorption was not significantly higher among those with IBS.62 This remained the case when data were analysed according to the test used, as well as the dose of lactose ingested.
Four of the included studies presented data relating to the subjective assessment of lactose intolerance,62 with patients with IBS being significantly more likely than controls to report the occurrence of symptoms when eating lactose-containing foods. Only three studies provided data for objective lactose intolerance, whereby symptoms were reported during or shortly after the test in patients with confirmed lactose malabsorption.62 Those with IBS were significantly more likely to have objective lactose intolerance than healthy controls, but this analysis should be interpreted with caution, as there was significant heterogeneity between studies.
Knowledge of whether a patient with IBS also has lactose malabsorption does not appear to alter clinical outcomes. In one study of 161 patients with IBS, 23 (14.3%) identified lactose as a potential trigger prior to HBT, and lactose malabsorption was confirmed in 47 (29.2%),63 but during almost 4 years of follow-up, there was no difference in rates of symptom persistence or resolution between those with confirmed lactose malabsorption and those without. In another study, 23 patients with suspected IBS with confirmed lactose malabsorption followed a lactose exclusion diet for 3 weeks; only 9 (39.1%) reported symptom improvement.64 Current evidence does not support a role for routine exclusion of lactose malabsorption in IBS. In those reporting a dietary intolerance to lactose, referral to a dietitian for a trial of exclusion could be considered.
Tests for small intestinal bacterial overgrowth
Small intestinal bacterial overgrowth (SIBO) has been postulated as an aetiological factor in IBS. The prevalence of SIBO in suspected IBS has been reported to be almost 80% in some studies using lactulose HBT.65 Understandably, such findings sparked considerable interest in the use of non-absorbable antibiotics, such as rifaxmin, for the treatment of IBS. However, a Swedish case-control study using jejunal aspirate and culture, often considered to be the gold-standard for diagnosing SIBO, cast doubt on this66; prevalence of SIBO was no higher in 162 patients with Rome II-defined IBS than in 26 healthy controls. Another case-control study reported that the prevalence of a positive lactulose HBT was equivalent between 224 patients with IBS diagnosed according to the Rome II criteria and 40 healthy controls.67
A meta-analysis of 12 studies concluded the prevalence of SIBO was highest when HBT was used, compared with jejunal aspirate and culture, but varied between patients with IBS and controls depending on threshold used to define a positive test.68 Statistical heterogeneity in the analyses was substantial, despite exclusion of small studies with fewer than 90 participants.
Whether a positive HBT in IBS truly represents SIBO, and hence whether SIBO is genuinely being missed in patients with IBS-type symptoms, is debatable. In a Canadian study, patients ingested a radio-labelled meal and 10 g of lactulose simultaneously, and underwent subsequent scintigraphic scanning to estimate orocaecal transit time, as well as a lactulose HBT.69 The high rate of positive HBTs in patients with IBS appeared to be related to rapid intestinal transit; the rise in breath hydrogen corresponded to the time at which the meal entered the caecum in almost 90% of patients. Overall, therefore, current evidence does not support the use of testing for SIBO routinely in patients with suspected IBS unless there are other documented risk factors, such as previous gastric or intestinal surgery, intestinal dysmotility or known structural abnormalities,70 although prior surgery was associated with a 65% rate of false-positive results in one study.71
Conclusion
The majority of patients with suspected IBS can be diagnosed confidently following a detailed history, eliciting the cardinal symptoms as described by the Rome criteria. Exhaustive investigation is not required and may be counter-productive. Routine blood tests are reasonable, although they have a low yield, and all patients should have serological testing for coeliac disease, irrespective of their predominant stool pattern. Any patient with suspected IBS-D should have a FC measured and, if this is positive, proceed to colonoscopy to exclude IBD. Need for further testing should then be assessed on a case-by-case basis, and guided by the presence of known risk factors for organic pathology. Colonoscopy should be considered in any patient reporting alarm features for CRC, and in those whose clinical features suggest a possible diagnosis of MC. A SeHCAT scan should be considered in patients with IBS-D, a third of whom may actually have BAD. There is no role for routine HBT for lactose malabsorption or SIBO, unless there are clear risk factors for the latter, although patients who report a dietary sensitivity to lactose may benefit from a dietitian review and a trial of dietary exclusion.
In conclusion, encouraging physicians to make an early positive diagnosis of IBS, limiting the need for clinical investigations, creates the opportunity for initiation of earlier symptom-specific treatment, while reducing associated healthcare costs. Adopting a standardised and evidence-based approach is vital to achieve high-quality and high-value care for patients with IBS.
Footnotes
Contributors: CJB and ACF drafted the article.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Not required.
Provenance and peer review: Commissioned; externally peer reviewed.
References
- 1. Lovell RM, Ford AC. Global prevalence of and risk factors for irritable bowel syndrome: a meta-analysis. Clin Gastroenterol Hepatol 2012;10:712–21. 10.1016/j.cgh.2012.02.029 [DOI] [PubMed] [Google Scholar]
- 2. Lovell RM, Ford AC. Effect of gender on prevalence of irritable bowel syndrome in the community: systematic review and meta-analysis. Am J Gastroenterol 2012;107:991–1000. 10.1038/ajg.2012.131 [DOI] [PubMed] [Google Scholar]
- 3. Mearin F, Lacy BE, Chang L, et al. . Bowel disorders. Gastroenterology 2016. [DOI] [PubMed] [Google Scholar]
- 4. Holtmann GJ, Ford AC, Talley NJ. Pathophysiology of irritable bowel syndrome. Lancet Gastroenterol Hepatol 2016;1:133–46. 10.1016/S2468-1253(16)30023-1 [DOI] [PubMed] [Google Scholar]
- 5. Gralnek IM, Hays RD, Kilbourne A, et al. . The impact of irritable bowel syndrome on health-related quality of life. Gastroenterology 2000;119:654–60. 10.1053/gast.2000.16484 [DOI] [PubMed] [Google Scholar]
- 6. Frändemark Åsa, Törnblom H, Jakobsson S, et al. . Work productivity and activity impairment in irritable bowel syndrome (IBS): a multifaceted problem. Am J Gastroenterol 2018;113:1540–9. 10.1038/s41395-018-0262-x [DOI] [PubMed] [Google Scholar]
- 7. Buono JL, Carson RT, Flores NM. Health-related quality of life, work productivity, and indirect costs among patients with irritable bowel syndrome with diarrhea. Health Qual Life Outcomes 2017;15 10.1186/s12955-017-0611-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Thompson WG, Heaton KW, Smyth GT. Irritable bowel syndrome in general practice: prevalence, characteristics, and referral. Gut 2000;46:78–82. 10.1136/gut.46.1.78 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Talley NJ, Zinsmeister AR, Melton LJ. Irritable bowel syndrome in a community: symptom subgroups, risk factors, and health care utilization. Am J Epidemiol 1995;142:76–83. 10.1093/oxfordjournals.aje.a117548 [DOI] [PubMed] [Google Scholar]
- 10. Koloski NA, Talley NJ, Huskic SS, et al. . Predictors of conventional and alternative health care seeking for irritable bowel syndrome and functional dyspepsia. Aliment Pharmacol Ther 2003;17:841–51. 10.1046/j.1365-2036.2003.01498.x [DOI] [PubMed] [Google Scholar]
- 11. Koloski NA, Talley NJ, Boyce PM. Epidemiology and health care seeking in the functional Gi disorders: a population-based study. Am J Gastroenterology 2002;97:2290–9. 10.1111/j.1572-0241.2002.05783.x [DOI] [PubMed] [Google Scholar]
- 12. Yawn BP, Locke GR. 3rd, Lydick E, Wollan PC, Bertram SL, Kurland MJ. Diagnosis and care of irritable bowel syndrome in a community-based population. Am J Manag Care 2001;7:585–92. [PubMed] [Google Scholar]
- 13. Shivaji UN, Ford AC. Prevalence of functional gastrointestinal disorders among consecutive new patient referrals to a gastroenterology clinic. Frontline Gastroenterol 2014;5:266–71. 10.1136/flgastro-2013-100426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hookway C, Buckner S, Crosland P, et al. . Irritable bowel syndrome in adults in primary care: summary of updated NICE guidance. BMJ 2015;350:h701 10.1136/bmj.h701 [DOI] [PubMed] [Google Scholar]
- 15. Spiller R, Aziz Q, Creed F, et al. . Guidelines on the irritable bowel syndrome: mechanisms and practical management. Gut 2007;56:1770–98. 10.1136/gut.2007.119446 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Spiegel BMR, Farid M, Esrailian E, et al. . Is irritable bowel syndrome a diagnosis of exclusion?: a survey of primary care providers, Gastroenterologists, and IBS experts. Am J Gastroenterol 2010;105:848–58. 10.1038/ajg.2010.47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Drossman DA, Thompson WG. The irritable bowel syndrome: review and a graduated multicomponent treatment approach. Ann Intern Med 1992;116:1009–16. 10.7326/0003-4819-116-12-1009 [DOI] [PubMed] [Google Scholar]
- 18. Williams M, Barclay Y, Benneyworth R, et al. . Using best practice to create a pathway to improve management of irritable bowel syndrome: aiming for timely diagnosis, effective treatment and equitable care. Frontline Gastroenterol 2016;7:323–30. 10.1136/flgastro-2016-100727 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Canavan C, West J, Card T. Review article: the economic impact of the irritable bowel syndrome. Aliment Pharmacol Ther 2014;40:1023–34. 10.1111/apt.12938 [DOI] [PubMed] [Google Scholar]
- 20. Everhart JE, Ruhl CE. Burden of digestive diseases in the United States Part I: overall and upper gastrointestinal diseases. Gastroenterology 2009;136:376–86. 10.1053/j.gastro.2008.12.015 [DOI] [PubMed] [Google Scholar]
- 21. Lacy BE, Ford AC, Talley NJ. Quality of care and the irritable bowel syndrome: is now the time to set standards? Am J Gastroenterol 2018;113:167–9. 10.1038/ajg.2017.442 [DOI] [PubMed] [Google Scholar]
- 22. NICE NICE guideline NG12. suspected cancer: recognition and referral, 2015. updated 2017 Available: https://www.nice.org.uk/guidance/ng12 [Accessed 12/04/2019].
- 23. Ford AC, Veldhuyzen van Zanten SJO, Rodgers CC, et al. . Diagnostic utility of alarm features for colorectal cancer: systematic review and meta-analysis. Gut 2008;57:1545–53. 10.1136/gut.2008.159723 [DOI] [PubMed] [Google Scholar]
- 24. Whitehead WE, Palsson OS, Feld AD, et al. . Utility of red flag symptom exclusions in the diagnosis of irritable bowel syndrome. Aliment Pharmacol Ther 2006;24:137–46. 10.1111/j.1365-2036.2006.02956.x [DOI] [PubMed] [Google Scholar]
- 25. Ford AC, Moayyedi P, Bercik P, et al. . Lack of utility of symptoms and signs at first presentation as predictors of inflammatory bowel disease in secondary care. Am J Gastroenterol 2015;110:716–24. 10.1038/ajg.2015.117 [DOI] [PubMed] [Google Scholar]
- 26. Talley NJ. How to do and interpret a rectal examination in gastroenterology. Am J Gastroenterology 2008;103:820–2. 10.1111/j.1572-0241.2008.01832.x [DOI] [PubMed] [Google Scholar]
- 27. Manning AP, Thompson WG, Heaton KW, et al. . Towards positive diagnosis of the irritable bowel. BMJ 1978;2:653–4. 10.1136/bmj.2.6138.653 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Longstreth GF, Thompson WG, Chey WD, et al. . Functional bowel disorders. Gastroenterology 2006;130:1480–91. 10.1053/j.gastro.2005.11.061 [DOI] [PubMed] [Google Scholar]
- 29. Ford AC, Bercik P, Morgan DG, et al. . Validation of the Rome III criteria for the diagnosis of irritable bowel syndrome in secondary care. Gastroenterology 2013;145:1262–70. 10.1053/j.gastro.2013.08.048 [DOI] [PubMed] [Google Scholar]
- 30. Sood R, Camilleri M, Gracie DJ, et al. . Enhancing diagnostic performance of symptom-based criteria for irritable bowel syndrome by additional history and limited diagnostic evaluation. Am J Gastroenterol 2016;111:1446–54. 10.1038/ajg.2016.308 [DOI] [PubMed] [Google Scholar]
- 31. Shivaji UN, Ford AC. Beliefs about management of irritable bowel syndrome in primary care: cross-sectional survey in one locality. Prim Health Care Res Dev 2015;16:263–9. 10.1017/S1463423614000383 [DOI] [PubMed] [Google Scholar]
- 32. Thompson WG, Heaton KW, Smyth GT, et al. . Irritable bowel syndrome: the view from general practice. Eur J Gastroenterol Hepatol 1997;9:689–92. 10.1097/00042737-199707000-00008 [DOI] [PubMed] [Google Scholar]
- 33. Begtrup LM, Engsbro AL, Kjeldsen J, et al. . A positive Diagnostic strategy is noninferior to a strategy of exclusion for patients with irritable bowel syndrome. Clin Gastroenterol Hepatol 2013;11:956–62. 10.1016/j.cgh.2012.12.038 [DOI] [PubMed] [Google Scholar]
- 34. Sanders DS, Carter MJ, Hurlstone DP, et al. . Association of adult coeliac disease with irritable bowel syndrome: a case-control study in patients fulfilling Rome II criteria referred to secondary care. The Lancet 2001;358:1504–8. 10.1016/S0140-6736(01)06581-3 [DOI] [PubMed] [Google Scholar]
- 35. Menees SB, Powell C, Kurlander J, et al. . A meta-analysis of the utility of C-reactive protein, erythrocyte sedimentation rate, fecal calprotectin, and fecal lactoferrin to exclude inflammatory bowel disease in adults with IBS. Am J Gastroenterol 2015;110:444–54. 10.1038/ajg.2015.6 [DOI] [PubMed] [Google Scholar]
- 36. Tolliver BA, Herrera JL, DiPalma JA. Evaluation of patients who meet clinical criteria for irritable bowel syndrome. Am J Gastroenterol 1994;89:176–8. [PubMed] [Google Scholar]
- 37. Aoki Y, Belin RM, Clickner R, et al. . Serum TSH and Total T 4 in the United States Population and Their Association With Participant Characteristics: National Health and Nutrition Examination Survey (NHANES 1999–2002). Thyroid 2007;17:1211–23. 10.1089/thy.2006.0235 [DOI] [PubMed] [Google Scholar]
- 38. Ludvigsson JF, Bai JC, Biagi F, et al. . Diagnosis and management of adult coeliac disease: guidelines from the british society of gastroenterology. Gut 2014;63:1210–28. 10.1136/gutjnl-2013-306578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Irvine AJ, Chey WD, Ford AC. Screening for celiac disease in irritable bowel syndrome: an updated systematic review and meta-analysis. Am J Gastroenterol 2017;112:65–76. 10.1038/ajg.2016.466 [DOI] [PubMed] [Google Scholar]
- 40. Katz KD, Rashtak S, Lahr BD, et al. . Screening for celiac disease in a North American population: sequential serology and gastrointestinal symptoms. Am J Gastroenterol 2011;106:1333–9. 10.1038/ajg.2011.21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Choung RS, Rubio-Tapia A, Lahr BD, et al. . Evidence against routine testing of patients with functional gastrointestinal disorders for celiac disease: a population-based study. Clin Gastroenterol Hepatol 2015;13:1937–43. 10.1016/j.cgh.2015.05.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Lasson A, Kilander A, Stotzer P-O. Diagnostic yield of colonoscopy based on symptoms. Scand J Gastroenterol 2008;43:356–62. 10.1080/00365520701679116 [DOI] [PubMed] [Google Scholar]
- 43. Røseth AG, Fagerhol MK, Aadland E, et al. . Assessment of the neutrophil dominating protein calprotectin in feces. A methodologic study. Scand J Gastroenterol 1992;27:793–8. 10.3109/00365529209011186 [DOI] [PubMed] [Google Scholar]
- 44. NICE Diagnostics guidance (DG11). faecal calprotectin diagnostic tests for inflammatory diseases of the bowel, 2013. Available: https://www.nice.org.uk/guidance/DG11 [Accessed 12/04/2019].
- 45. van Rheenen PF, Van de Vijver E, Fidler V. Faecal calprotectin for screening of patients with suspected inflammatory bowel disease: diagnostic meta-analysis. BMJ 2010;341:c3369 10.1136/bmj.c3369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Turvill J, Turnock D, Holmes H, et al. . Evaluation of the clinical and cost-effectiveness of the York faecal calprotectin care pathway. Frontline Gastroenterol 2018;9:285–94. 10.1136/flgastro-2018-100962 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. NICE The new faecal calprotectin care pathway, 2018. Available: https://www.nice.org.uk/sharedlearning/the-new-faecal-calprotectin-care-pathway [Accessed 15/04/2019].
- 48. Lieberman DA, Holub J, Eisen G, et al. . Utilization of colonoscopy in the United States: results from a national Consortium. Gastrointestinal Endoscopy 2005;62:875–83. 10.1016/j.gie.2005.06.037 [DOI] [PubMed] [Google Scholar]
- 49. Chey WD, Nojkov B, Rubenstein JH, et al. . The yield of colonoscopy in patients with non-constipated irritable bowel syndrome: results from a prospective, controlled us trial. Am J Gastroenterol 2010;105:859–65. 10.1038/ajg.2010.55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Ishihara S, Yashima K, Kushiyama Y, et al. . Prevalence of organic colonic lesions in patients meeting Rome III criteria for diagnosis of IBS: a prospective multi-center study utilizing colonoscopy. J Gastroenterol 2012;47:1084–90. 10.1007/s00535-012-0573-4 [DOI] [PubMed] [Google Scholar]
- 51. Kamp EJCA, Kane JS, Ford AC. Irritable bowel syndrome and microscopic colitis: a systematic review and meta-analysis. Clin Gastroenterol Hepatol 2016;14:659–68. quiz e54-5 10.1016/j.cgh.2015.09.031 [DOI] [PubMed] [Google Scholar]
- 52. Kane JS, Rotimi O, Everett SM, et al. . Development and validation of a scoring system to identify patients with microscopic colitis. Clin Gastroenterol Hepatol 2015;13:1125–31. 10.1016/j.cgh.2014.12.035 [DOI] [PubMed] [Google Scholar]
- 53. Macaigne G, Lahmek P, Locher C, et al. . Microscopic colitis or functional bowel disease with diarrhea: a French prospective multicenter study. Am J Gastroenterol 2014;109:1461–70. 10.1038/ajg.2014.182 [DOI] [PubMed] [Google Scholar]
- 54. Spiegel BMR, Gralnek IM, Bolus R, et al. . Is a negative colonoscopy associated with reassurance or improved health-related quality of life in irritable bowel syndrome? Gastrointest Endosc 2005;62:892–9. 10.1016/j.gie.2005.08.016 [DOI] [PubMed] [Google Scholar]
- 55. Khalid U, Lalji A, Stafferton R, et al. . Bile acid malabsoption: a forgotten diagnosis? Clinical Medicine 2010;10:124–6. 10.7861/clinmedicine.10-2-124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Summers JA, Peacock J, Coker B, et al. . Multicentre prospective survey of SeHCAT provision and practice in the UK. BMJ Open Gastroenterol 2016;3:e000091 10.1136/bmjgast-2016-000091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Wedlake L, A'Hern R, Russell D, et al. . Systematic review: the prevalence of idiopathic bile acid malabsorption as diagnosed by SeHCAT scanning in patients with diarrhoea-predominant irritable bowel syndrome. Aliment Pharmacol Ther 2009;30:707–17. 10.1111/j.1365-2036.2009.04081.x [DOI] [PubMed] [Google Scholar]
- 58. Aziz I, Mumtaz S, Bholah H, et al. . High prevalence of idiopathic bile acid diarrhea among patients with diarrhea-predominant irritable bowel syndrome based on Rome III criteria. Clin Gastroenterol Hepatol 2015;13:1650–5. 10.1016/j.cgh.2015.03.002 [DOI] [PubMed] [Google Scholar]
- 59. Bajor A, Törnblom H, Rudling M, et al. . Increased colonic bile acid exposure: a relevant factor for symptoms and treatment in IBS. Gut 2015;64:84–92. 10.1136/gutjnl-2013-305965 [DOI] [PubMed] [Google Scholar]
- 60. Slattery SA, Niaz O, Aziz Q, et al. . Systematic review with meta-analysis: the prevalence of bile acid malabsorption in the irritable bowel syndrome with diarrhoea. Aliment Pharmacol Ther 2015;42:3–11. 10.1111/apt.13227 [DOI] [PubMed] [Google Scholar]
- 61. Orekoya O, McLaughlin J, Leitao E, et al. . Quantifying bile acid malabsorption helps predict response and tailor sequestrant therapy. Clinical Medicine 2015;15:252–7. 10.7861/clinmedicine.15-3-252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Varjú P, Gede N, Szakács Z, et al. . Lactose intolerance but not lactose maldigestion is more frequent in patients with irritable bowel syndrome than in healthy controls: a meta-analysis. Neurogastroenterol Motil 2019;31:e13527 10.1111/nmo.13527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Tolliver BA, Jackson MS, Jackson KL, et al. . Does lactose maldigestion really play a role in the irritable bowel? J Clin Gastroenterol 1996;23:15–17. 10.1097/00004836-199607000-00005 [DOI] [PubMed] [Google Scholar]
- 64. Parker TJ, Woolner JT, Prevost AT, et al. . Irritable bowel syndrome: is the search for lactose intolerance justified? Eur J Gastroenterol Hepatol 2001;13:219–25. 10.1097/00042737-200103000-00001 [DOI] [PubMed] [Google Scholar]
- 65. Pimentel M, Chow EJ, Lin HC. Eradication of small intestinal bacterial overgrowth reduces symptoms of irritable bowel syndrome. Am J Gastroenterol 2000;95:3503–6. 10.1111/j.1572-0241.2000.03368.x [DOI] [PubMed] [Google Scholar]
- 66. Posserud I, Stotzer P-O, Bjornsson ES, et al. . Small intestinal bacterial overgrowth in patients with irritable bowel syndrome. Gut 2007;56:802–8. 10.1136/gut.2006.108712 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Bratten JR, Spanier J, Jones MP. Lactulose breath testing does not discriminate patients with irritable bowel syndrome from healthy controls. Am J Gastroenterol 2008;103:958–63. 10.1111/j.1572-0241.2008.01785.x [DOI] [PubMed] [Google Scholar]
- 68. Ford AC, Spiegel BMR, Talley NJ, et al. . Small intestinal bacterial overgrowth in irritable bowel syndrome: systematic review and meta-analysis. Clin Gastroenterol Hepatol 2009;7:1279–86. 10.1016/j.cgh.2009.06.031 [DOI] [PubMed] [Google Scholar]
- 69. Yu D, Cheeseman F, Vanner S. Combined oro-caecal scintigraphy and lactulose hydrogen breath testing demonstrate that breath testing detects oro-caecal transit, not small intestinal bacterial overgrowth in patients with IBS. Gut 2011;60:334–40. 10.1136/gut.2009.205476 [DOI] [PubMed] [Google Scholar]
- 70. Quigley EMM. The spectrum of small intestinal bacterial overgrowth (SIBO). Curr Gastroenterol Rep 2019;21 10.1007/s11894-019-0671-z [DOI] [PubMed] [Google Scholar]
- 71. Lin EC, Massey BT. Scintigraphy demonstrates high rate of false-positive results from glucose breath tests for small bowel bacterial overgrowth. Clin Gastroenterol Hepatol 2016;14:203–8. 10.1016/j.cgh.2015.07.032 [DOI] [PubMed] [Google Scholar]