Abstract
Extraintestinal manifestations of gastrointestinal disease can form an important aspect of the diagnosis, monitoring and management in these diseases. Ocular manifestations in particular are often disregarded and can, albeit rarely, present as an emergency.
Keywords: IBD clinical, wilson’s disease, primary biliary cirrhosis, nutrition, hepatobiliary disease
Specialty certificate exam style best-of-five questions.
A 45-year-old man with a medical history of Crohn’s disease calls the IBD nurse-led telephone helpline presenting a 3-day history of a painful left eye.
He is seen in the clinic that afternoon and also presents a light sensitivity. His eye is generally red (figure 3) with some tearing evident.3
What is the most appropriate initial treatment?
Topical steroids
Oral prednisolone
Intravenous hydrocortisone
Increase azathioprine dose
Start infliximab
Correct answer: (A) Topical steroids
He has symptoms suggestive of acute anterior uveitis. The disease course runs independent of bowel inflammation and is managed initially with topical steroids.
Question 2
A 43-year-old man with a medical history of hepatitis C in a sustained virologic response (SVR) is under investigation for deranged liver function tests.
His caeruloplasmin is <20 mg/dL.
He is referred to ophthalmologist for slit lamp investigation, which showed pigmented rings at the iris-scleral junction.
What gene is affected in this condition?
JAK
ATP7B
ALR
PIMZ
PNPLA3
Correct answer: (B) ATP7B
While molecular testing is not essential for the diagnosis of Wilson’s disease to be made, it can be helpful in the absence of Kayser-Fleischer rings, and in those with a normal caeruloplasmin or intermediate copper quantification (50–250 mcg/g dry weight) on liver histology.
Question 3
Which of the following ophthalmological manifestations are not related to vitamin A deficiency?
Bitot’s spots
Uveitis
Night blindness
Keratitis
Xerophthalmia
Correct answer: (B) Uveitis
Introduction
Gastrointestinal diseases can have many important extraintestinal features, and the early identification and resolution may impact current symptoms and is important for preventing long-term complications. Ophthalmological features can be varied and may rarely present as an ophthalmological emergency, with early identification and treatment being paramount to good outcomes. A good knowledge of these features can be advantageous in helping disease diagnosis and ruling out differentials, and it may play a role in monitoring disease progression or treatment toxicity. As gastroenterologists play a significant role in the follow-up of these patients, up-to-date knowledge of common ophthalmological signs, symptoms and management is vital to prevent long-term complications that may be sight threatening.
This review will detail common and important ocular features of inflammatory bowel disease (IBD) and other hepatobiliary disorders, including their epidemiology, features, treatment and complications. This is guided by competencies from the gastroenterology curriculum as outlined in table 1.
Table 1.
Curriculum competencies20
| Specialty Training Curriculum for Gastroenterology 2010 (Amendments 2013) | |
|
Knows the complications of IBD including stricturing, fistulae, extraintestinal manifestations. Able to recognise potential complications and take appropriate action to investigate and alter treatment as necessary including referral for surgery and involvement of other healthcare professionals. |
|
Aware of management and complications of autoimmune liver disease including extrahepatic manifestations and associations including malignant complications in PSC. Recognises the importance but also difficulty in diagnosing heavy metal-associated liver disease; has an understanding of the variants of both conditions. |
|
Recognises vitamin and mineral deficiencies and conditions in which they are likely to occur (eg, vitamin A deficiency with severe steatorrhoea) and be able to give appropriate treatment. |
IBD, inflammatory bowel disease; PSC, primary sclerosing cholangitis.
Ocular manifestations in IBD
Episcleritis
Episcleritis is one of three classic ocular complications of IBD, others including scleritis and uveitis (table 2). It is reported to occur in 29% of patients with IBD and is related to the severity of disease, with flares paralleling intestinal activity, thus may be used as an indicator of disease severity.1 It is benign and self-limiting, and more commonly affects women.2
Table 2.
Summary of ocular manifestations in IBD
| Ocular clinical sign | Prevalence (approximate) | Signs/symptoms | Parallel GI disease activity | Treatment (in order of severity) |
| Episcleritis | 29% | Eye redness, mild pain, tearing. No visual disturbance. | Yes | Cool compress, topical steroids. Treat IBD. |
| Scleritis | 18% | Redness (may appear blue/purple), severe ocular pain, may have visual disturbance. | No | NSAIDs, systemic steroids, immunosuppressive agents. |
| Uveitis | 1.5%–3% | Ocular pain, photophobia, visual blurring, tearing. Perilimbal redness, miotic pupil, synechiae. | No | Cycloplegic agent (eg, atropine) and topical steroids, systemic steroids, immunosuppressives. |
| Cataracts | 6%10 | Progressive worsening acuity, glare around light at night. | No | Surgical lens removal and replacement. |
| Optic neuritis1 | Unknown | Ocular pain worse on eye movement, unilateral, impaired acuity, dyschromatopsia (red-green), visual field defects. | No | Withdrawal of anti-TNFα agents, intravenous methylprednisolone. |
| Retinal vasculitis1 | <1% | Painless impaired visual acuity, flashes, floaters, scotomas, metamorphopsia. | Unknown | Topical/systemic steroids, immunosuppressive agents.21 |
GI, gastrointestinal; IBD, inflammatory bowel disease; NSAID, non-steroidal anti-inflammatory drug; TNF, tumour necrosis factor.
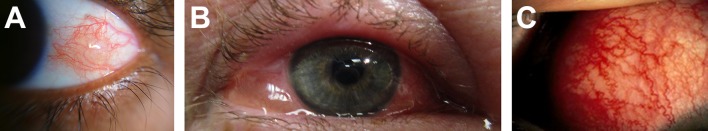
The episcleral layer is affected, which is a blood-rich layer between the conjunctiva and sclera (figure 1).3 Characteristically, it involves injection of superficial episcleral vessels and overlying conjunctiva, which are mobile to palpation and blanch with topical phenylephrine. There is sparing of the scleral vessels that give the sclera a white appearance between dilated red episcleral vessels (figure 2A).4 The pattern of inflammation may be nodular or diffuse, unilateral or bilateral. Symptoms include mild pain, tenderness on palpation and/or tearing. Notably, there is no change in vision and the pupillary response remains intact. It is diagnosed clinically and should be suspected in those with an active flare of IBD who present with acute unilateral or bilateral redness, irritation or burning. An important differential includes conjunctivitis (figure 2B),5 which may be differentiated by a more unilateral presentation initially, with a watery or purulent discharge, itching and a lesser degree of ocular pain. It is the most common cause of a red eye in the general population, however no known association with IBD has yet been proven.6
Figure 1.
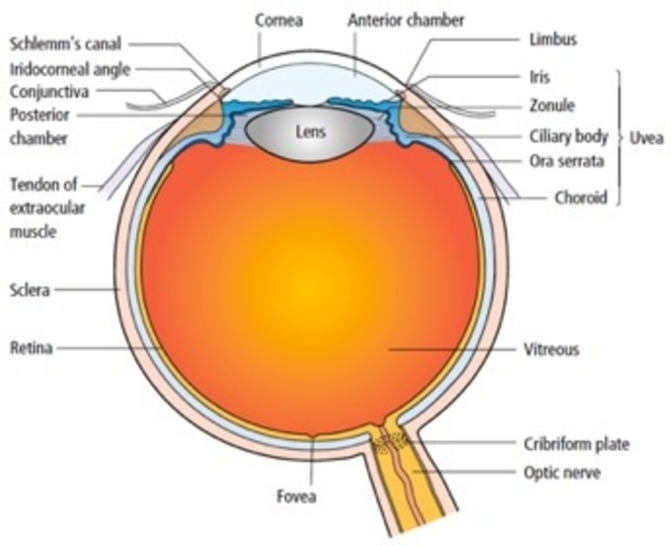
Anatomy of the eye.3
Figure 2.
(A) Episcleritis. © 2017 Imrankabirhossain Published under a CC BY SA licence. (B) Allergic conjunctivitis with chemosis. © 2013 James Heilman, MD Published under a CC BY SA licence. (C) Scleritis.4 6 2
Management includes treatment of the underlying IBD, resulting in a rapid resolution of the inflammation of the episcleral vessels. For short-term symptomatic relief, use of a cool compresses or topical steroids may be effective. More severe symptoms may warrant the use of topical non-steroidal anti-inflammatory drugs (NSAID), although its use is limited due to its potential association with IBD flares. Infliximab has been shown to be effective in refractory episcleritis associated with IBD.6
Scleritis
Scleritis is a less common extraintestinal manifestation of IBD, occurring in roughly 18% of patients with IBD, commonly affecting women and an older patient group than that seen in episcleritis. Conversely, only approximately 2% of scleritis cases are associated with IBD, with more common systemic disease associations including rheumatoid arthritis and granulomatosis with polyangiitis.7 It may occur during inactive IBD phases and thus may not be a reliable disease-severity indicator.1
The inflammation mostly affects the anterior sclera, it may be diffuse or focal, and is unilateral in up to two-thirds of cases. In scleritis, injection of the deeper scleral vessels (as well as episcleral and conjunctival involvement) results in hyperaemia (figure 2C). The injected vessels are non-blanching with phenylephrine application and are immobile on palpation with a cotton-tipped applicator, in contrast to episcleritis. Classically, the inflamed sclera have been described as appearing blue or violet under natural light. Typically, a deeper more severe ocular and periorbital pain is reported compared with episcleritis, with tenderness on palpation. Rarely, involvement of the posterior sclera results in visual loss, which may be complicated by retinal detachment or optic neuritis (swelling of the nerve head) which may result in a permanent visual impairment. Thus, prompt referral to an ophthalmologist is important for rapid diagnosis and aggressive management. Scleritis can commonly recur, although effective control of the underlying IBD may reduce this risk.6 This is significant as scleromalacia perforans (thinning of the sclera) may occur as a consequence of recurrences.2 Due to the potentially serious complications, management is aggressive and includes NSAIDs, systemic steroids or immunosuppressant drugs (eg, methotrexate) in order of increasing severity.6
Uveitis
Uveitis is thought to present less commonly than episcleritis, with a prevalence of roughly 1.5%–3% in those with IBD, occurring more commonly in females. It does not parallel the underlying activity of the IBD, and often presents insidiously, with a chronic course of up to 6 months, with a risk of recurrence.8 There is an association between dermatological (namely erythema nodosum) and joint symptoms in IBD where uveitis presents. Furthermore, a link between acute iritis and HLA-B27 expression, sacroiliitis and Crohn’s disease has been described.3
Uveitis can be separated by anatomical structures involved (figure 1), with anterior uveitis referring to the inflammation of the iris and ciliary body (iritis). Posterior uveitis is significantly rarer, and includes inflammation of the vitreous (vitritis), choroid or retina (choroidoretinitis). The most common uveitis includes an acute non-granulomatous anterior uveitis, with a panuveitis (all layers involved) or posterior uveitis presenting more rarely with poorer prognosis if left untreated.6
Characteristic symptoms include ocular pain, photophobia, visual blurring and tearing. Signs include a typical perilimbal (concentrated centrally and radiating outwards) injection and miotic pupils which may have an abnormal response to light. Slit lamp examination provides a definitive diagnosis and shows corneal clouding due to inflammatory ‘cells and flare’, with a hypopyon (sterile pus in anterior chamber) in severe cases (figure 3). Synechiae can form (figure 4), where the miotic pupil results in an attachment between the iris and cornea or lens, which can result in long-term complications including secondary glaucoma and cataract formation.6 Prompt management is required and includes a cycloplegic agent to avoid synechiae formation and provide pain relief, alongside topical steroids. In more severe cases, systemic steroids or immunomodulatory drugs may be used.6
Figure 3.
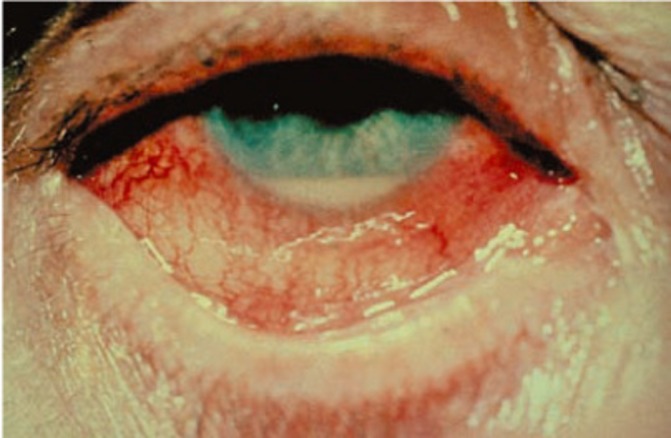
A 45-year-old man with red eye.2
Figure 4.
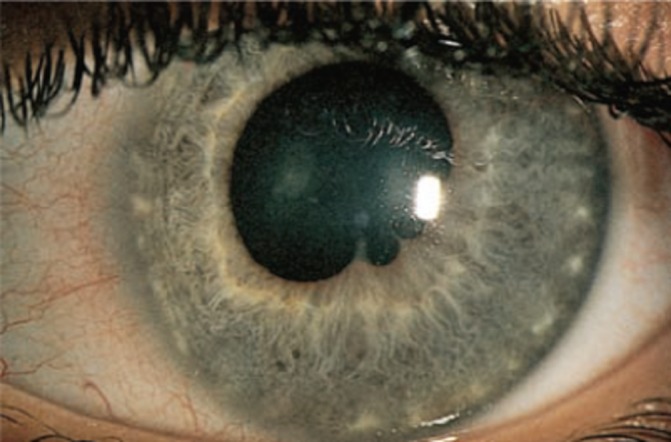
Synechiae formation in uveitis.3
Cataracts
Cataract formation occurs as a treatment-related ophthalmological manifestation of IBD, with prolonged steroid use resulting in posterior subcapsular cataract formation. There is thought to be a dose-dependent relationship, although individual predisposition and genetic factors complicate this relationship. For example, children are more vulnerable and experience a more rapid progression of cataract formation. A ‘safe dose’ is controversial, although it has previously been quoted as less than 10 mg daily of prednisolone, for less than a year.9 It is also thought that other prior ocular manifestations of IBD (eg, uveitis) can lead to secondary cataract formation.10 This may be asymptomatic, or may cause insidious and progressive reduced acuity, and patients may typically report glare at night around light sources. Treatment includes surgical lens removal and replacement.6
Cataract formation can also occur as a complication of congenital galactosaemia, due to accumulation of by-products (galactitol) from alternate galactose metabolism pathways. This can occur in the neonatal period, with a prevalence of roughly 6%–25%. It presents bilaterally with a characteristic appearance on slit lamp examination, notably with no impact on visual acuity. Management includes maintaining a galactose-restricted diet (including using milk substitutes), which will often result in cataract resolution. Dietary adherence is also important in preventing severe cataracts in later life, although reduced visual acuity requiring surgery is very rare.11
Ocular manifestations in hepatobiliary disorders
Keratoconjunctivitis sicca
Dry eye disease (keratoconjunctivitis sicca) affects up to 30% of the normal population, up to 90% of which are females. Its aetiology can be multifactorial and may be directly or indirectly associated with an underlying gastrointestinal condition. It can occur as part of Sjögren’s syndrome (xerostomia, xerophthalmia, dry skin), which can occur secondarily to primary biliary cirrhosis (PBC) in up to 10% of patients with PBC, or chronic hepatitis C infection. Vitamin A deficiency may contribute, occurring secondary to malabsorption in IBD or bowel resection. Furthermore, it is reported to occur secondary to high doses of 5-ASA, especially doses over 3 mg/day.12 Common complaints include a foreign body or gritty sensation of the eye, dryness, redness, itching, with photophobia or visual blurring occurring less commonly. Schirmer’s test is used for diagnosis severity grading, which includes measuring eye moisture using filter paper (normal ≥10 mm in Schirmer’s I test). Treatment includes artificial tear substitutes for milder symptoms, with ophthalmology referral for topical anti-inflammatory agents, and punctal plugging reserved for more severe and refractory symptoms (table 3).13
Table 3.
Summary of ocular signs in hepatobiliary disorders
| Ocular clinical sign | Presentation | GI disease association | Treatment/additional facts |
| Keratoconjunctivitis sicca | Gritty sensation, dryness, redness, itching | Sjögren’s syndrome/PBC, chronic hepatitis C, high-dose 5-ASA | Artificial tears, topical anti-inflammatory agents (ophthalmological referral)14 |
| Jaundice | Yellowing of conjunctiva | GI causes of jaundice15 | Bilirubin >34 µmol/L14 |
| Xanthelasma | Yellow plaques around inner canthus of eyelids | Hyperlipidaemia | Corneal arcus also seen in hyperlipidaemic states14 |
| Optic disc drusen | Irregular disc margins on funduscopy | Alagille syndrome, 15% of normal population | Not shown to have poor prognosis on vision16 |
| Kayser-Fleischer ring | Brown/green/red ring in peripheral cornea | Wilson’s disease | Indicator of copper burden17 |
GI, gastrointestinal; PBC, primary biliary cirrhosis.
Jaundice
Conjunctival icterus may become apparent when bilirubin levels rise above 34 µmol/L, where a yellowing of the conjunctiva (sometimes incorrectly termed scleral jaundice) can be seen under natural light,14 with no visual symptoms. Causes of jaundice can be classified as prehepatic (typically not related to gastrointestinal disease), hepatic and posthepatic.15 Treatment of the underlying condition results in resolution of the jaundice.14
Xanthelasma
Xanthelasma (figure 5) can occur as a manifestation of chronic liver disease, in PBC and in hyperlipidaemic states. It presents as yellow plaques often occurring bilaterally, located around the inner canthus of the upper (more common) or lower eyelids.16 Other manifestations of hyperlipidaemic states include corneal arcus, presenting as a white opaque ring located at the periphery of the cornea, without visual symptoms. Treatment of the underlying disorder often only has a limited effect on the plaques, and surgical removal could be considered for cosmetic reasons.14
Figure 5.

Xanthelasma. ©2005 Klaus D Peter. Published under a CC BY licence.16
Optic disc drusen
Ocular disc drusen are one of the many ophthalmological findings that may be seen in Alagille syndrome, although they may also be seen in up to 15% of the normal population. Along with evidence of posterior embryotoxon (white line appearing anterior to limbus during slit lamp examination due to displacement of Schwalbe’s line), these ocular signs can be used to form part of the clinical diagnostic criteria of the syndrome.17
Other ocular findings are less common, and include retinal pigment granularity, microcornea and diffuse fundus hypopigmentation. These ocular abnormalities have not been shown to have a poor prognosis on vision, although evidence via follow-up studies in an older population is lacking. Ophthalmological examination and B scan ultrasound can be used to identify the stated ocular abnormalities and optic disc drusen, respectively. This can be used as a simple non-invasive technique of differentiating from other causes of neonatal intrahepatic jaundice.17
Kayser-Fleischer ring
Kayser-Fleischer rings are a hallmark of Wilson’s disease, and occur in up to 95% of patients with neurological signs, and 50%–60% of those without.18 They are due to copper deposition in Descemet membrane, which is the basement membrane of cornea. Physical examination or slit lamp examination may reveal a brown, green or red ring in the peripheral (perilimbal) cornea, beginning superiorly before spreading to the inferior pole to become circumferential. No visual symptoms are associated. Notably, it can be used as an indicator of copper burden, and can resolve with treatment, thus may be used as part of monitoring.14
Retinal vitamin A deficiency
Several ophthalmological manifestations occur due to a state of hypovitaminosis A including xerophthalmia, night blindness, Bitot’s spots, keratitis and keratomalacia (table 4). These can be divided into features of chronic or acute low vitamin A levels, and may not reverse with replenishment of vitamin A. As the ocular tissues are sensitive to low vitamin A levels, ocular signs and symptoms can be early although uncommon indicators of hypovitaminosis A, and it can be considered a poor prognostic indicator in low vitamin A states. Gastrointestinal causes of low vitamin A levels include those leading to malabsorption; including IBD, short gut syndrome (eg, postbariatric surgery), chronic pancreatitis, cirrhosis and infection (Ascaris infestation, Giardia).19
Table 4.
Features of ocular manifestations in hypovitaminosis A
| Signs and symptoms (pathophysiology) | |
| Chronic hypovitaminosis | |
| Bitot’s spots | White or black raised spots, frothy appearance on perilimbal conjunctiva, no visual symptoms, pathognomonic (keratin deposits due to squamous metaplasia) |
| Night blindness | Poor vision in dark conditions, common ocular symptom in children and pregnant women (due to destruction of retinal rod cells) |
| Acute hypovitaminosis | |
| Xerophthalmia | Gritty eyes, foreign body sensation, tearing, redness |
| Keratitis | Inflammation of cornea resulting in ulceration (keratomalacia is severe ulceration) due to xerophthalmia, punched-out appearance on cornea. Complications include secondary infection and scarring, with long-term decreased visual acuity.22 |
Diagnosis includes measuring serum retinol levels (deficient levels <0.3 mg/L), in conjunction with investigations for underlying cause. Ophthalmological examinations may include examination with fluorescein dye and Schirmer’s test. Treatment may include vitamin A replacement in conjunction with management of the underlying condition.19
Conclusion
Gastrointestinal and systemic disease can result in many varied ocular features, and the early identification of these can be important in the diagnosis and monitoring of the underlying condition, as well as prevention of potentially sight-threatening complications. Thus, through fundamental understanding of ocular and other extraintestinal features, the gastroenterologist can most effectively work within a multidisciplinary team to provide holistic care with a systemic approach.
Acknowledgments
Thanks to Dr Napoleon Dhevarajan for reviewing and providing suggestions for the manuscript as an expert opinion in Ophthalmology.
Footnotes
Contributors: HNH developed the idea for the article and contributed to writing the article. LI contributed to writing the article under the supervision of HNH.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Mady R, Grover W, Butrus S. Ocular complications of inflammatory bowel disease. The Scientific World Journal 2015;2015:1–5. 10.1155/2015/438402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ghanchi FD, Rembacken BJ. Inflammatory bowel disease and the eye. Surv Ophthalmol 2003;48:663–76. 10.1016/j.survophthal.2003.08.004 [DOI] [PubMed] [Google Scholar]
- 3. James B, Bron B. Ophthalmology lecture notes, chichester. Wiley-Blackwell, 2011. [Google Scholar]
- 4. Hossain IK. “Wikimedia Commons,” 9 May, 2017. Available: https://upload.wikimedia.org/wikipedia/commons/4/41/Episcleritis.jpg [Accessed 12 Dec 2018].
- 5. Hellman J. “Wikimedia Commons,” 14 November, 2013. Available: https://upload.wikimedia.org/wikipedia/commons/d/d7/Allergicconjunctivitis.jpg [Accessed 12 Dec 2018].
- 6. Mintz R, Feller ER, Bahr RL, et al. . Ocular manifestations of inflammatory bowel disease. Inflamm Bowel Dis 2004;10:135–9. 10.1097/00054725-200403000-00012 [DOI] [PubMed] [Google Scholar]
- 7. Manganelli C, Turco S, Ballestrazzi E. “Ophthalmological aspects of IBD,”. Eur Rev Med Pharmacol Sci 2009;13:11–13. [PubMed] [Google Scholar]
- 8. Rothfuss KS, Stange EF, Herrlinger KR. Extraintestinal manifestations and complications in inflammatory bowel diseases. World J Gastroenterol 2006;12:4819–31. 10.3748/wjg.v12.i30.4819 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Jobling AI, Augusteyn RC. What causes steroid cataracts? A review of steroid-induced posterior subcapsular cataracts. Clin Exp Optom 2002;85:61–75. 10.1111/j.1444-0938.2002.tb03011.x [DOI] [PubMed] [Google Scholar]
- 10. Walldorf J, Twarz M, Schober C, et al. . High frequency of secondary, but not primary ocular manifestations of inflammatory bowel disease in patients treated at a tertiary care center. Eur J Gastroenterol Hepatol 2018;30:1502–6. 10.1097/MEG.0000000000001248 [DOI] [PubMed] [Google Scholar]
- 11. Welling L, Bernstein LE, Berry GT, et al. . International clinical guideline for the management of classical galactosemia: diagnosis, treatment, and follow-up. J Inherit Metab Dis 2017;40:171–6. 10.1007/s10545-016-9990-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Cury DB, Moss AC. Ocular manifestations in a community-based cohort of patients with inflammatory bowel disease. Inflamm Bowel Dis 2010;16:1393–6. 10.1002/ibd.21180 [DOI] [PubMed] [Google Scholar]
- 13. Foster S. “Dry Eye Syndrome (Keratoconjunctivitis Sicca),” 2017, 2017. [Accessed 30 May 2017].
- 14. Tooley AA, Sweetser S. Clinical examination: eyes. Clin Liver Dis 2016;7:154–7. 10.1002/cld.561 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Roche SP, Kobos R. Jaundice in the adult patient. Am Fam Physician 2004;69:299–304. [PubMed] [Google Scholar]
- 16. Klaus PD. “Wikimedia Commons,” 1 November, 2005. Available: https://upload.wikimedia.org/wikipedia/commons/2/25/Xanthelasma.jpg [Accessed 12 Dec 2018].
- 17. Hingorani M, Nischal KK, Davies A, et al. . Ocular abnormalities in Alagille syndrome. Ophthalmology 1999;106:330–7. 10.1016/S0161-6420(99)90072-6 [DOI] [PubMed] [Google Scholar]
- 18. Ferenci P. Review article: diagnosis and current therapy of Wilson's disease. Aliment Pharmacol Ther 2004;19:157–65. 10.1046/j.1365-2036.2003.01813.x [DOI] [PubMed] [Google Scholar]
- 19. Faustino JF, Ribeiro-Silva A, Dalto RF, et al. . Vitamin A and the eye: an old tale for modern times. Arq Bras Oftalmol 2016;79:56–61. 10.5935/0004-2749.20160018 [DOI] [PubMed] [Google Scholar]
- 20. Joint Royal Colleges of Physicians Training Board “Specialty training curriculum for gastroenterology,” August 2013. Available: https://www.jrcptb.org.uk/sites/default/files/2010%20Gastroenterology%20%28amendment%202013%29_0.pdf [Accessed 26 Apr 2018].
- 21. Agarwal A, Tripathy K. “Retinal Vasculitis,” In: American academy of ophthalmology, 2017. [Google Scholar]
- 22. Gilbert C. “The eye signs of vitamin A deficiency,”. Community Eye Health Journal 2013;26:66–7. [PMC free article] [PubMed] [Google Scholar]