Abstract
Introduction
Progressive neuromuscular spinal deformities with pelvic obliquity and loss of sitting balance are typical features of severely affected patients with cerebral palsy. The pelvis represents the key bone between the spine and the lower extremity when it comes to deciding whether and when to operate and if spine or hip surgery first is beneficial. The pelvis can be looked at as the lowest vertebra and as the rooftop of the lower extremities.
Biomechanical considerations
To allow for a normal spinal shape, the pelvis needs to be horizontal in the frontal plane and mildly anterior tilted in the sagittal plane, less for sitting and more for standing. Any abnormal pelvic position requires spinal compensation and challenges the equilibrium control of the individual. Both anatomical neighbourhoods – the spine and the hip joints — have to be considered when spinal deformities, hip instability and contractures evolve, in conservative therapy (bracing, physiotherapy, seating in the wheelchair) and when surgical interventions are weighed out against each other.
Surgical considerations
Multiple anatomical factors such as sagittal profile and pelvic orientiation, pelvic transverse plane asymmetries and lumbosacral malformations have to be considered in case the pelvis is instrumented with sacral and iliac screws. Rotational deformities and asymmetries of the pelvic bones make the safe insertion of long screws challenging. Advantages of primary pelvic fixation include correction of pelvic obliquity, especially considering the lever arm of the whole spinal construct. The risk of revision surgery due to progression of distal curves is also reduced. Disadvantages of pelvic fixation include the complexity of the additional intervention, which may result in longer operating times, increased risk of blood loss, infection and hardware malpositioning.
Keywords: cerebral palsy, spine, pelvis, deformity
Introduction
Young non-ambulatory patients with cerebral palsy (cP) bear a high risk of developing simultaneous progressive scoliotic spine deformities, pelvic obliquity, loss of sitting balance and hip subluxation/dislocation.1 The prevalence of scoliosis in cP rises in parallel with the degree of motor impairment as classified in the Gross Motor Function Classification System (GMFCS level), up to almost 100% in severely affected patients (GMFCS V).2,3
A vicious cycle of pathological muscle tone, increasing curvature and subsequent secondary inhibitory vertebral growth disturbances in the concavity of the curve fuels curve rigidity, as well as progressive vertebral and spinal deformity.4 Brace treatment at an early stage is an option to improve stability, trunk positioning, head control and upper extremity function but most likely may not alter the natural history of progressive deformity, not even after the end of growth.5,6 Curve size and stiffness, chest wall deformities, rib and skin fragility are limiting factors for trunk orthoses.
Progressive curves with pelvic obliquity and loss of sitting ability warrant surgical stabilization, usually around puberty. Surgery needs to address both, the deformity and the functional instability, in these cases. Curve severity and stiffness, associated hip (sub-) luxations, sagittal plane deformities, vertebral deformities, soft bones and chest deformities, as well as joint contractures and associated cardiopulmonary morbidities and nutritional deficits need to be considered.7
This paper aims at enlightening the role of the pelvis as the key bone between the spine and the lower extremity when it comes to deciding whether and when to operate and if spine or hip surgery first is beneficial.
This article was conceived by the neuromuscular and spine study groups of the European Paediatric Orthopaedic Society (EPOS) based on the presentations of the authors given at the society’s 37th annual meeting in Tel Aviv, Israel (05 April 2019) in a two-hour focus session on cP and associated spine deformities. Based on an additional literature review (PubMed, Cochrane) and two decades of surgical experience and functional analysis in the field of neuromuscular spine deformities during growth, the authors highlight current anatomical and biomechanical understanding, practical implications for the clinical and radiographical assessment and the surgical strategy when it comes to the decision whether or not to include the pelvis in the fusion.
The pelvis: fundament of the spine
Functional considerations and sequelae of spinal deformities
The pelvis forms a functional unit with the spine and thereby represents the crucial pivot zone between the trunk and the lower extremities. It can be looked at as the lowest vertebra and as the rooftop of the lower extremities (intercalary bone). Both anatomical neighbourhoods have to be considered when spinal deformities, hip instability and contractures evolve, in conservative therapy (bracing, physiotherapy, seating in the wheelchair) and when surgical interventions are weighed out against each other: stability of the lumbosacral junction as the basis for correction of pelvic obliquity and adequate hip stability and movement as prerequisites and facilitators for free walking, standing and sitting. In ambulators the predominant role of the pelvis is to adapt posture in a 3D way, to conserve muscular energy (‘cone of economy’, a term coined by Jean Dubousset8) and to allow for an unrestrained field of action in the upper extremities. On the other side of the functional scale – in severely disabled non-ambulatory patients – the pelvis, the lumbosacral junction and their interplay with the hip joints need to provide a solid fundament for unsupported sitting and balanced positioning of the head, ideally on the upper extension of the central sacral vertical line. Again, stability improves the functionality of arms and hands.
Growth dynamics as well as the natural history of the underlying neuromuscular pathology entail a mostly long sweeping progressive (thoraco-) lumbar scoliosis and pelvic obliquity, painful costopelvic impingement and loss of intraabdominal volume with the eating disorder. Since the pelvis houses abdominal viscera and represents the solid floor of the abdominal cavity, the lost abdominal volume is partially regained by a secondary elevation of the diaphragm which in turn causes impairment of the space available for the lungs.
Therapeutic aspects
The complex mutual relationship between the pelvis, the spine and the lower extremities depends on multiple factors which require comprehensive consideration when it comes to non-surgical (seating, wheelchair adaption, sitting and walking aids) and surgical (positioning of the patient on the operating room table, use of traction, lumbosacral fixation, type of fixation, sagittal and coronal balancing etc) decision-making and choice of strategy (Table 1).
Table 1.
Anatomical factors influencing therapeutic decisions
| Sagittal spinal profile |
|---|
| (Thoraco-) lumbar scoliosis |
| Sagittal pelvic orientation (pelvic incidence,sacral slope, pelvic tilt) |
| Pelvic transverse plane orientation |
| Pelvic transverse plane asymmetry |
| Lumbosacral malformations |
| Hip and knee joint contractures |
| Leg-length differences |
| Muscle tone |
The lumbosacral junction
The degree of pelvic obliquity, the morphology and the stability of the lumbosacral junction are the key factors when it comes to the decision whether or not to include the pelvis in the surgical construct. A stable, deep seated fifth lumbar vertebra riding on a anatomical normal sacrum plateau and a mild pelvic obliquity (< 30°) are prerequisites for a limited fusion to L5. Vice versa, lumbosacral variations such as lumbalization of sacral vertebra (hemi-), sacralization of lumbar vertebra, oblique S1- or L5-take off, lumbosacral transitional vertebrae or caudal regression syndrome may influence this decision making process.9
Effects and limitations of intraoperative traction
This close mutual relation between the spine and the pelvis facilitates surgical manipulation of the spine and pelvis; usually the spine responds to pelvis movement and vice versa in the coronal, transverse and sagittal plane, thereby indirecty influencing more remote areas of the lower extremities and the spine. For example, by surgically inadvertently increasing pelvic tilt, flattening of the lumbar lordosis and overcorrection of hyperkyphosis, one may cause an upwards directed biomechanical chain reaction which increases the risk of proximal junctional kyphosis and of loss of upper fixation after instrumentation.10 Intraoperative skull-femoral traction is an effective means – particularly for severe (> 70° to 90°) neuromuscular spinal deformities – to achieve significant non-invasive deformity correction prior to posterior instrumentation, thereby avoiding first stage anterior release surgery in severe curvatures.11 Since the spine unfolds in 3D, surgical exposure is easier, quicker and the blood loss less.12 Moreover, pedicle screw placement is facilitated and the correction forces are reduced which is particularly helpful in the commonly soft bones of cP patients. However, one has to consider that the traction forces acting through the femur and the hip joints may be counterproductive in the presence of severe hip contractures. In those cases traction should be omitted since it causes hyperlordosis of the lumbar spine and may induce negative sagittal balance with subsequent risk of proximal junctional kyphosis.
The pelvis: rooftop of the hips
The shape of the spine depends of the position of the pelvis. To allow for a normal spinal shape, the pelvis needs to be horizontal in the frontal plane and mildly anterior tilted in the sagittal plane, less for sitting and more for standing. Any abnormal pelvic position requires spinal compensation and challenges the equilibrium control of the individual.13-15 Sitting requires a hip flexion of at least 90°. In the case of a bilateral and symmetrical restricition of flexion, lumbar kyphosis is the consequence. More severe deformities occur in unilateral or very asymmetrical restrictions of flexion when the pelvis is elevated on the more restricted side and usually anteriorly rotated (Fig. 1). The spine is pushed into scoliosis, rotation and kyphosis. The causes for the restriction of flexion, however, may be multiple: painful hip dislocations, anatomical joint deformities and hip extensor contractures are the most common ones. The spinal deformity can be prevented if the seating device accommodates for the abnormal position of the legs similar to what was used earlier after hip fusion which allowed for a normal position of the pelvis. The surgical option is to correct the causing deformity: to reconstruct the hip in case of dislocation (which provides mobility and stability of the joint), to correct the anatomical deformity by a compensating femoral osteotomy (what may affect hip extension) and to release contractures. Patients with severe balance problems require a larger support base for sitting which includes the thighs. Floppy hip joints as after proximal femoral resection or after excessive soft-tissue releases may thus interfere with stability and should be avoided. As sitting is usually more important than standing or walking, restrictions of hip extension are less important. The consequence is a hyperlordosis in any upright posture. Once fixed, it is present in sitting as well. Most cases with hyperlordosis, however, present with weak hip extensors, a still unsolved functional issue.
Fig. 1.

Patient with flexion deficit at the left hip in a poorly adapted seat. The pelvis is lifted and anteriorly rotated on the left. The spine is forced into a respective compensatory position with rotation and scoliosis.
Another problem is wind sweeping; a deformity which combines bilateral hip flexion with internal rotation and adduction on one side and external rotation and abduction on the other. In longstanding deformities, the femoral anteversion adapts to the situation and shows extreme anteversion on the intrarotated and retroversion on the extrarotated side. If the malposition of the legs is not accommodated the pelvis rotates and with it the trunk. On the anteriorly tilted side, the shoulder has no contact anymore with the back of the seating device. Usually, straps are introduced in this situation to pull the shoulder back which produces a rotation in the spine. Together with the asymmetry of hip movement, this twist may have the potential to initiate a scoliotic deformity.14,15 Conservatively, the seating device needs to accommodate for the abnormal leg position which again allows for a normal pelvic position. Surgically, soft-tissue surgery is one option. However, bony (femoral) corrective osteotomies seem to be more efficient.
The pelvis: spare it or fuse it?
Measurement of pelvic obliquity
Scoliosis is one of the most common musculoskeletal manifestations of patients with cP. In many cases, the spinal deformity may extend down to the pelvis and cause pelvic obliquity.
The assessment of pelvic obliquity is performed both clinically and radiographically. For ambulators, standing and walking with and without aids should be observed for general balance and posture. For non-ambulators, sitting apparatus including padding and elevated parts should be assessed, as well as corresponding pressure points on the patients’ skin. An additional clinical parameter to assess is the gait pattern; patients who flex and extend the pelvis significantly during walking will be unable to do so after spino-pelvic fixation.
The Stagnara test should be performed to determine the origin of the pelvic obliquity.16 The patient is placed prone on the edge of the bed with the hips flexed. The hips are then manipulated left to right and the scoliotic curve is re-examined. If the pelvic obliquity can be corrected by the manoeuvre, then it is secondary to a pelvis/hip-derived pathology. If the pelvic obliquity does not reduce – then the obliquity is secondary to the scoliotic curve itself. Radiographically, multiple methods have been described to assess the spinopelvic angle itself. The pelvic landmark universally used is a line connecting the superior aspect of the iliac crest bilaterally. The angle may be calculated with spinal landmarks (traditionally T1 vertebral body or a line connecting the spinous process of L4 and L5) or the edge of the film itself.17 Scoliotic curves can be divided into two groups as described by Lonstein, group 1 being idiopathic-like curves and group 2 being long ‘C-shaped’ curves with prominent pelvic obliquity.18 Modern radiation reduced systems should be employed if possible, such as the sterEOS® system.19 Preoperative use of traction films should also be considered to assess the flexibility of the spinal curve and the pelvic obliquity. If helpful, it can aid in planning for intra-operative skeletal traction.
Decision making: associated factors
The goals of posterior spinal fusion for scoliosis are to achieve a stable, solid fusion with a compensated spine over a level pelvis without decrease of neurological function. Achieving these goals should accomplish a reduction in pain and improvement in quality of life, without need for additional surgeries. Advantages of primary pelvic fixation include correction of pelvic obliquity, especially considering the lever arm of the whole spinal construct. The risk of revision surgery due to progression of distal curves is also reduced.20 Traditionally, pelvic fixation was contraindicated in ambulators, due to the risk of deterioration of ambulation status probably related to their dependence on minimal sacroiliac joint motion. However, there is sufficient evidence that this is not a true contraindication and that ambulatory status can be preserved.21 Sparing the pelvis also allows for the iliac bone to be utilized as a bone graft.22
Disadvantages of pelvic fixation include the complexity of the additional intervention, which may result in longer operating times, increased risk of blood loss, a lumbosacral cavity and haematoma, infection and hardware malpositioning, implant prominence (ilium screw), skin breakdown, pain and higher costs.23,24
In contrast to patients with syndromic deformities, cP patients have a normal primary anatomy of the pelvis, however, since the pelvis, particularly the ilium, is part of the spinal lumbar deformity secondary supraacetabular transverse plane deformities may develop in parallel with the progressive spinal deformity and particularly in patients with windswept hips (Fig. 2).25 Accordingly, intrapelvic asysmmetries (pelvic scoliosis) are common in cP patients with severe scoliosis and make the safe insertion of long screws challenging.25 They need to be considered when placing ilium or sacral alar iliac (SAI) screws: 3D orientation, size, shape, thickness and bone density may vary significantly beween the concave (highsided) and convex hemipelvis (Fig. 3).
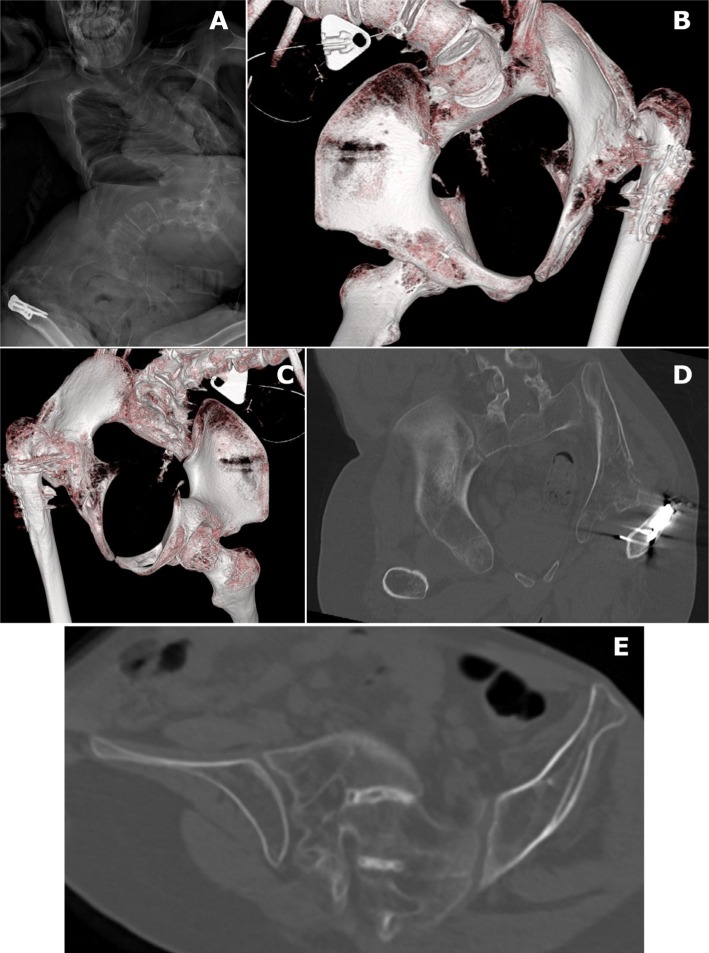
Fig. 2.
a) A 17-year-old male tetraspastic patient with cerebral palsy Gross Motor Function Classification System level V and severe double curved scoliosis; b-e) the computertomography with 3D reconstruction views from anterior (b) and posterior (c) as well as the coronal (d) and transverse (e) sections clearly show a marked left-right asymmetry of the iliac bones in terms of size, spatial orientation and shape.
Fig. 3.
A 15-year-old tetraspastic boy with cerebral palsy Gross Motor Function Classification System level V; a-b) the typically longsweeping L convex thoracolumbar kyphoscoliosis entails a marked pelvic obliquity, rotation and asymmetry with concomittant costopelvic impingement; c-d) the postoperative radiographs display the hook-screw hybrid construct which was used for spinal deformity and pelvic obliquity correction and in particular the Iliosacral screw fixation of the rotated and asymmetric pelvis.
Other significant determinants of pelvic versus L5 fixation are the anatomy of L5 and the lumbo-sacral joint itself (see previous paragraph, ‘the lumbosacral junction’), as well as the sagittal balance of the whole spine. Severe sagittal deformities may include lumbar hyperlordosis and anterior truncal shift, among others. The final element in the decision making is the functional capacity of the patient, as stratified by the GMFCS. Patients with GMFCS level V, unable to even support their own head, are candidates for pelvic fixation to avoid distal adding on and for the lack of possible functional deterioration. Community ambulators (GMFCS levels I to II) will mostly present with smaller curves and without pelvic obliquity. In these patients pelvic fixation is rarely done, to avoid the offset chance of walking status decrease. The remaining patients, with GMFCS levels III to IV, are the most challenging and their treatment should be tailored individually.
Conclusions
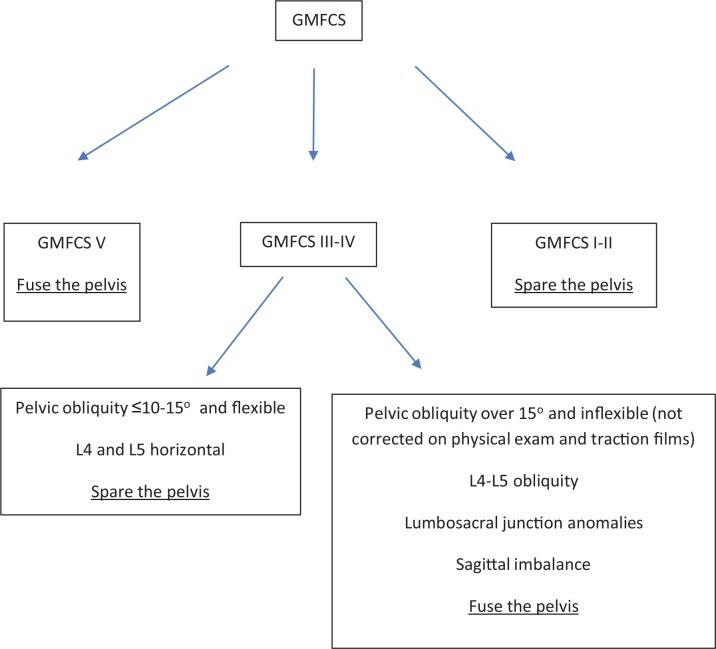
There are evidently both pros and cons to containing the pelvis within the spinal fusion in patients with cP. We offer this algorithm to try and aid the surgeon in the decision-making process as to whether to include the pelvis in the construct. It should be mentioned that while this paper and this algorithm are aimed at posterior spinal fusion, it can also be taken as a general guideline when considering pelvic obliquity in the context of growth friendly surgery for younger patients (Fig. 4).
Fig. 4.
Treatment algorithm for spinal fusion in patients with cerebral palsy (GMFCS, Gross Motor Function Classification System).
We suggest starting by assessing the functional capacity (i.e. GMFCS) of the patient. With wheelchair bound patients, we recommend fusing the pelvis in order to optimize the seating and minimizing the risk of revision surgeries. In patients with good ambulation capabilities (GMFCS I to II), on the other hand, we would opt for ending the construct at either L4 or L5. These patients may also present with curves that are idiopathic-like (i.e. Lonstein type 1), in which case the levels of the fusion can be decided in a matter consistent with guidelines for adolescent idiopathic scoliosis patients. For the remaining patients, pelvic fixation should be given thoughtful consideration; how oblique is the pelvis, how flexible is the curve, does the deformity extend to L5, the articulation with the sacrum, is the patient sagitally balanced? The physical exam, including the gait patterns, will be crucial in the surgical planning of these patients.
Open access
This article is distributed under the terms of the Creative Commons Attribution-Non Commercial 4.0 International (CC BY-NC 4.0) licence (https://creativecommons.org/licenses/by-nc/4.0/) which permits non-commercial use, reproduction and distribution of the work without further permission provided the original work is attributed.
Compliance with ethical standards
Funding Statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Ethical Statement
Ethical approval: This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent: Not required for this work.
ICMJE Conflict of Interest Statement
CH reports personal fees from Consultant DePuy Synthes, outside the submitted work.
The other authors declare no conflict of interest.
Author Contributions
CH: Paper basic concept and structure, Abstract, Introduction, Table 1, Figures 2 and 3, References, Layout, Submission.
RB: Paper basic concept and structure, Section about the role of the hip joints, Figure 1.
AG: Literature review, Section about to fuse or not fuse to the pelvis, Treatment algorithm.
DO: Paper basic concept and structure, Section about to fuse or not to fuse to the pelvis, Treatment algorithm.
References
- 1.Patel J, Shapiro F. Simultaneous progression patterns of scoliosis, pelvic obliquity, and hip subluxation/dislocation in non-ambulatory neuromuscular patients: an approach to deformity documentation. J Child Orthop 2015;9:345-356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Master DL, Son-Hing JP, Poe-Kochert C, Armstrong DG, Thompson GH. Risk factors for major complications after surgery for neuromuscular scoliosis. Spine (Phila Pa 1976) 2011;36:564-571. [DOI] [PubMed] [Google Scholar]
- 3.Hägglund G, Pettersson K, Czuba T, Persson-Bunke M, Rodby-Bousquet E. Incidence of scoliosis in cerebral palsy. Acta Orthop 2018;89:443-447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yoshida K, Kajiura I, Suzuki T, Kawabata H. Natural history of scoliosis in cerebral palsy and risk factors for progression of scoliosis. J Orthop Sci 2018;23:649-652. [DOI] [PubMed] [Google Scholar]
- 5.Pettersson K, Rodby-Bousquet E. Prevalence and goal attainment with spinal orthoses for children with cerebral palsy. J Pediatr Rehabil Med 2019;12:197-203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kajiura I, Kawabata H, Okawa A, et al. . Concept and treatment outcomes of dynamic spinal brace for scoliosis in cerebral palsy. J Pediatr Orthop B 2019;28:351-355. [DOI] [PubMed] [Google Scholar]
- 7.Jones-Quaidoo SM, Yang S, Arlet V. Surgical management of spinal deformities in cerebral palsy. A review. J Neurosurg Spine 2010;13:672-685. [DOI] [PubMed] [Google Scholar]
- 8.Dubousset J. Reflections of an orthopaedic surgeon on patient care and research into the condition of scoliosis. J Pediatr Orthop 2011;31 (suppl):S1-S8. [DOI] [PubMed] [Google Scholar]
- 9.Taskaynatan MA, Izci Y, Ozgul A, et al. . Clinical significance of congenital lumbosacral malformations in young male population with prolonged low back pain. Spine (Phila Pa 1976) 2005;30:E210-E213. [DOI] [PubMed] [Google Scholar]
- 10.Chen X, Chen ZH, Qiu Y, et al. . Proximal junctional kyphosis after posterior spinal instrumentation and fusion in young children with congenital scoliosis: a preliminary report on its incidence and risk factors. Spine (Phila Pa 1976) 2017;42:E1197-E1203. [DOI] [PubMed] [Google Scholar]
- 11.Jackson TJ, Yaszay B, Pahys JM, et al. . Intraoperative traction may be a viable alternative to anterior surgery in cerebral palsy scoliosis ≥100 degrees. J Pediatr Orthop 2018;38:e278-e284. [DOI] [PubMed] [Google Scholar]
- 12.Jhaveri SN, Zeller R, Miller S, Lewis SJ. The effect of intra-operative skeletal (skull femoral) traction on apical vertebral rotation. Eur Spine J 2009;18:352-356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Allam AM, Schwabe AL. Neuromuscular scoliosis. PM R 2013;5:957-963. [DOI] [PubMed] [Google Scholar]
- 14.Holmes C, Brock K, Morgan P. Postural asymmetry in non-ambulant adults with cerebral palsy: a scoping review. Disabil Rehabil 2019;41:1079-1088. [DOI] [PubMed] [Google Scholar]
- 15.Porter D, Michael S, Kirkwood C. Patterns of postural deformity in non-ambulant people with cerebral palsy: what is the relationship between the direction of scoliosis, direction of pelvic obliquity, direction of windswept hip deformity and side of hip dislocation? Clin Rehabil 2007;21:1087-1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vialle R, Thévenin-Lemoine C, Mary P.. Neuromuscular scoliosis. Orthop Traumatol Surg Res 2013;99 (suppl):S124-S139. [DOI] [PubMed] [Google Scholar]
- 17.Shrader MW, Andrisevic EM, Belthur MV, et al. . Inter- and intraobserver reliability of pelvic obliquity measurement methods in patients with cerebral palsy. Spine Deform 2018;6:257-262. [DOI] [PubMed] [Google Scholar]
- 18.Lonstein JE, Akbarnia A. Operative treatment of spinal deformities in patients with cerebral palsy or mental retardation. An analysis of one hundred and seven cases. J Bone Joint Surg [Am] 1983;65-A:43-55. [PubMed] [Google Scholar]
- 19.Rouissi J, Arvieu R, Dubory A, et al. . Intra and inter-observer reliability of determining degree of pelvic obliquity in neuromuscular scoliosis using the EOS-CHAIR(R) protocol. Childs Nerv Syst 2017;33:337-341. [DOI] [PubMed] [Google Scholar]
- 20.Nielsen E, Andras LM, Bellaire LL, et al. . Don’t you wish you had fused to the pelvis the first time: a comparison of reoperation rate and correction of pelvic obliquity. Spine (Phila Pa 1976) 2019;44:E465-E469. [DOI] [PubMed] [Google Scholar]
- 21.Tsirikos AI, Chang WN, Shah SA, Dabney KW, Miller F. Preserving ambulatory potential in pediatric patients with cerebral palsy who undergo spinal fusion using unit rod instrumentation. Spine (Phila Pa 1976) 2003;28:480-483. [DOI] [PubMed] [Google Scholar]
- 22.McCall RE, Hayes B. Long-term outcome in neuromuscular scoliosis fused only to lumbar 5. Spine (Phila Pa 1976) 2005;30:2056-2060. [DOI] [PubMed] [Google Scholar]
- 23.Sponseller PD, Zimmerman RM, Ko PS, et al. . Low profile pelvic fixation with the sacral alar iliac technique in the pediatric population improves results at two-year minimum follow-up. Spine (Phila Pa 1976) 2010;35:1887-1892. [DOI] [PubMed] [Google Scholar]
- 24.Phillips JH, Gutheil JP, Knapp DR Jr. Iliac screw fixation in neuromuscular scoliosis. Spine (Phila Pa 1976) 2007;32:1566-1570. [DOI] [PubMed] [Google Scholar]
- 25.Ko PS, Jameson PG II, Chang TL, Sponseller PD. Transverse-plane pelvic asymmetry in patients with cerebral palsy and scoliosis. J Pediatr Orthop 2011;31:277-283. [DOI] [PubMed] [Google Scholar]