Abstract
Purpose
Surgical procedures, such as medial hamstring lengthening (MHL) and femoral derotational osteotomy (FDO), can improve the gait of children with cerebral palsy (CP); however, substantial variation exists in the factors that influence the decision to perform surgery. The purpose of this study was to use expert surgeon opinion through a Delphi technique to establish consensus for indications in ambulatory children with CP.
Methods
A 15-member panel, all established experts with at least nine years’ experience in the surgical management of children with CP, was created (mean of 20.81 years’ experience). All panel members also had expertise of the use of movement analysis for the assessment of gait disorders in children with CP. The group initially focused on two of the most commonly performed procedures, MHL and FDO, in an attempt to gain consensus (> 80%). This was obtained through a standardized, iterative Delphi process.
Results
For MHL, a total of 59 questions were surveyed: 41 indication questions and 18 outcome questions, for which there was consensus on ten indication questions and seven outcomes. For FDO, a total of 55 questions were surveyed: 43 indication questions and 12 outcome questions, for which there was consensus on 29 indication questions and eight outcomes.
Conclusion
This study is the first to use an expert panel to identify best-practice indications for common surgical procedures of children with CP. The results from this study will allow for more informed evaluation of practice and form the basis for future improvement efforts to standardize surgical recommendations internationally.
Level of Evidence
Level IV
Keywords: cerebral palsy, surgical indications, consensus
Introduction
Cerebral palsy (CP) is the most common cause of physical disability in children1 and improving the physical function of ambulatory children with CP positively impacts both their quality of life and that of their caregivers.2,3 Surgical procedures, such as medial hamstring lengthening (MHL) and femoral derotational osteotomy (FDO), can improve the gait and physical functioning of children with CP;4,5 however, substantial variation exists in the clinical and patient-level factors that influence the decision to perform surgery.6,7 This variation likely leads to both under- and overuse of these procedures in this population, who are already at higher risk of surgical complications than the general population. More traditional research approaches to the study of clinical decision making, such as case control studies and randomized controlled studies, have been performed but are limited due to the clinical heterogeneity of the patient population, the large menu of 30 to 40 commonly performed procedures and the variety of combinations of procedures and surgical techniques.
Consensus methodology, including indications for surgery and interpretation of gait analysis, has been successfully used to develop guidelines for the management of orthopaedic conditions.8,9 Our hypothesis is that it is feasible to use a combination of best available evidence and expert orthopaedic surgeon opinion through a Delphi technique to establish consensus for surgical indications for MHL and FDO in ambulatory children with CP. If successful, this process will serve as a model for developing indications for additional procedures and provide evidence for clinical equipoise for more traditional research techniques in specific areas with poor consensus.
Our methodology is broken down into four aims. First, convene an international group of experts with clinical experience in the treatment of children with CP and the use of 3D movement analysis. Second, create a defined list of commonly performed orthopaedic procedures from which to work to establish surgical indications. Third, establish and agree upon a construct for categorizing indications. Fourth, using the above structure, develop consensus around indications for MHL and FDO in ambulatory children with CP using the Delphi method.
Background and significance
CP is a heterogeneous group of motor disorders caused by nonprogressive injury to the brain during early development and is the most common cause of physical disability in children, with an estimated global prevalence of approximately 17 million people.1 The symptoms of CP include abnormalities in muscle tone, strength and motor control, along with other secondary symptoms, that can affect physical function and the ability to ambulate.1,6 Improving the physical function of ambulatory children with CP can positively impact both their quality of life and that of their caregivers.2,3 A primary goal in the orthopaedic surgical treatment of ambulatory children with CP is improvement in gait, often accomplished with single-event multilevel surgery (SEMLS), where multiple procedures such as musculotendinous lengthening and corrective osteotomies, are included in one surgery.6,10,11
Although SEMLS avoids repeat episodes of anaesthesia, hospitalization and recovery, the combination of procedures makes evaluation of surgical indications and outcomes of specific procedures challenging.11 A 2012 systematic review of SEMLS found a low level of evidence in support of SEMLS due to low quality of study design, short period of follow-up for outcome assessment and limited description of participants.12 Given the variability in outcomes, along with the potential risks that accompany surgery in children with CP, it is critical to identify which patients should undergo SEMLS and the optimal indications for each specific procedure. Two common procedures often performed as part of SEMLS are MHL and FDO. MHL is often considered for children with flexed-knee gait, which can lead to joint pain, arthritis and progressive gait deterioration,13 whereas FDO can be considered in patients with excessive femoral anteversion and increased internal hip rotation.5 Currently, no standardized indications exist to assist orthopaedic surgeons in deciding which patients would be good candidates for specific procedures.14-17 As a result, surgeons use a combination of history, physical examination awake or while under anaesthesia, radiographic findings, 3D gait analyses and past experience; however, some evidence suggests that a more standardized approach may lead to improved outcomes.18,19
Consensus methodology has been successfully used to develop guidelines for the management of orthopaedic conditions, including indications for surgery and interpretation of gait analysis.8,9 This process can lead to the development of specific indications for MHL and FDO for ambulatory children with CP, which when applied consistently, will allow for improved assessment of long-term outcomes. The results from this study will allow for more informed evaluation of practice and form the basis for future improvement efforts to standardize surgical recommendations worldwide, and they can be easily extended to assess indications for other surgical procedures.
Materials and methods
This study used established consensus (Delphi) methodology to identify indications for MHL and FDO in ambulatory children with CP.
The Delphi methodology is a well-established method to develop appropriateness criteria.20-22 Institutional review board approval for the study and from each participating member was obtained. No participants dropped out from the study.
Expert panel formation
We formed a 15-member panel; all are established experts in the surgical management of children with CP (Table 1). Members were chosen from experts around the world. All experts were trained orthopaedic surgeons with at least nine years of focused clinical expertise in the orthopaedic surgical care of children with CP and access to and experience with a clinical movement analysis laboratory. On average, the experts had a mean of over 20 years of experience (mean 20.81 years, range 6 to 30) with the orthopaedic treatment of children with CP, for a combined total of over 300 years of experience. All panel members also had expertise with the use of movement analysis for the assessment of gait disorders in children with CP, on average 18.81 years (6 to 30).
Table 1.
Surgeons included in the study
| Name and institution |
|---|
| 1. Hank Chambers. MD, Rady Children’s Hospital, San Diego California |
| 2. Jon Davids, MD, Shriners Hospitals for Children- Northern California |
| 3. Kerr Graham, MD, FRCS, FRACS, The Royal Children’s Hospital, Melbourne Australia |
| 4. Robert M. Kay, MD, Children’s Hospital Los Angeles, Los Angles California |
| 5. James McCarthy, MD, MHCM, Cincinnati Children’s Hospital Medical Center, Cincinnati Ohio |
| 6. Unni Narayanan, MBBS, MSc, FRCS, The Hospital for Sick Children, Toronto, Canada |
| 7. Tom F. Novacheck, MD, Gillette Children’s Specialty Healthcare, Saint Paul, Minnesota |
| 8. Kristan Pierz, MD, Connecticut Children’s Hospital, Hartford Connecticut |
| 9. Jason Rhodes, MD, Children’ s Hospital Colorado, Aurora, Colorado |
| 10. Erich Rutz, MD, PhD, University Children’s Hospital Basle, Basle Switzerland |
| 11. Wade Shrader, MD, Nemours A.I. DuPont Hospital for Children, Wilmington Delaware |
| 12. Jeffery Shilt, MD, Texas Children’s Hospital, Houston Texas |
| 13. Benjamin Shore, MD, MHCM, Children’s Hospital of Boston, Boston Massachusetts |
| 14. Tim Theologis, MD, MSc, PhD, FRCS, Oxford University Hospitals, England |
| 15. Anja Van Campenhout, MD, UZ Leuven, Belgium |
| 16. Matthew Veerkamp, BA, Cincinnati Children’s Hospital Medical Center, Cincinnati Ohio |
| 17. Laura Brower, MD, Cincinnati Children’s Hospital Medical Center, Cincinnati Ohio |
Our expert panel created a list of 23 commonly performed orthopaedic procedures (Table 2). From this list, we agreed to initially focus on two of the most commonly performed procedures, MHL and FDO as our initial attempt to gain consensus.
Table 2.
A list of 23 commonly performed orthopaedic procedures
| Procedures |
|---|
| Bony |
| 1. Acetabular/pelvic osteotomy |
| 2. Varus derotational osteotomy |
| 3. Proximal femoral derotational osteotomy |
| 4. Distal femoral derotational osteotomy |
| 5. Tibial derotational osteotomy |
| 6. Distal femoral extension osteotomy |
| 7. Patellar tendon/tibial tubercle advancement (shortening) |
| 8. Hindfoot arthrodesis |
| 9. Calcaneal sliding osteotomy (medial/lateral) |
| 10. Mid/forefoot arthrodesis |
| 11. Calcaneal opening wedge osteotomy |
| 12. Midfoot osteotomy |
| 13. Guided growth of the anterior distal femur |
| 14. Guided growth of the proximal femur |
| Soft tissue |
| 15. Hip adductor lengthening |
| 16. Psoas lengthening |
| 17. Hamstring lengthening |
| 18. Rectus femoris transfer/lengthening |
| 19. Gastrocnemius recession |
| 20. Gastrocsoleus lengthening/heel cord lengthening |
| 21. Posterior tibialis lengthening |
| 22. Split posterior tibialis transfer |
| 23. Split anterior tibialis transfer |
Our expert panel then created and agreed to a structured format for categorizing the indications as shown in Table 3. This format consisted of five categories including the clinical problem/history and symptoms, physical exam including observational gait analysis, imaging findings, 3D movement analysis data, intraoperative exam under anaesthesia and important outcome measures.23-25
Table 3.
Framework for support (if applicable to the patients)
| Framework |
|---|
| 1. The clinical problem we are addressing (or preventing), and the benefit that this will translate into for the patient (intended outcome) |
| 2. Features of the clinical history/symptoms that will point to the clinical problem above, including Gross Motor Function Classification System and age |
| 3. The physical examination finding(s) that support the decision |
| a. Observed gait deviation |
| b. Static (on table) exam |
| 4. The imaging findings (where applicable) to support the decision |
| 5. The video and/or 3D gait analysis findings (where applicable) that support (or suggest avoiding) the procedure |
| 6. The intraoperative examination under anaesthesia that supports (or suggests avoiding) the procedure |
| 7. Important outcome measures |
Round 1: based on the literature review and submitted indications, we then used this structure to create open-ended questions regarding the surgical indications for MHL and FDO. These questions were then collated by category, and a well-structured questionnaire was created.
Round 2: an anonymous electronic survey was created in REDcap (Vanderbilt University, Nashville, Tennessee, USA)26,27 to formally rate the level of evidence supporting each indication using a Likert 5 level scale.21,22 This survey was sent to all experts in the group. Response options were strong indication, indicated, neutral, not indicated and strongly not indicated. Consensus for an indicated criterion was awarded when at least 80% of experts agreed to the top two Likert scales (strong indication or indication) or to a non-indicated procedure if at least 80% of experts agreed to the bottom two Likert scales (not indicated or strongly not indicated). Opportunity for comments was provided for all questions. General agreement was awarded for questions with at least 60% but less than 80% of experts agreeing to the top two Likert scales, or general disagreement for questions with at least 60% but less than 80% of experts agreeing to the bottom two Likert scales.
Round 3: from this survey, results were compiled. Those questions in which consensus was not achieved were evaluated, comments were collated, and (if needed) the question was clarified. This summary report was sent to all participants and responses to all non-consensus questions were re-submitted.
Two in-person meetings occurred in conjunction with international academic meetings, making the scheduling of an in-person meeting feasible, but still difficult given our international group of experts. During this process, panel members discussed ratings from round one, explored reasons for disagreement and modified indications.
Results
MHL
A total of 59 questions were surveyed: 41 indication questions and 18 outcome questions, for which there was consensus on ten indication questions, general agreement on eight more and consensus on seven outcome measures with general agreement on eight more. Consensus and general agreement by category are listed in Table 4. Questions for which there was consensus (bolded) and general agreement (italics) are listed in Table 5.28
Table 4.
Consensus and general agreement by category for medial hamstring lengthening (MHL) and femoral derotational osteotomy (FDO)
| Category | MHL | FDO | ||
|---|---|---|---|---|
| Consensus | General agreement | Consensus | General agreement | |
| Clinical problem/history | 2/10 | 3/10 | 6/9 | 2/9 |
| Physical exam | 0/12 | 3/12 | 11/15 | 3/15 |
| Imaging | 0/4 | 1/12 | 1/2 | 0/2 |
| 3D movement analysis | 8/12 | 0/12 | 5/9 | 1/9 |
| Exam under anaesthesia | 0/3 | 1/3 | 6/8 | 1/8 |
| Outcome measures | 7/18 | 8/18 | 8/12 | 1/12 |
| Total questions | 29% | 27% | 67% | 15% |
Consensus in bold type and general agreement in italics.
Table 5.
Questions for medial hamstring lengthening (MHL) that reached consensus or general agreement by category
| Clinical problems/history |
|---|
| Lack of knee extension while walking |
| Excessive knee flexion in early stance or late swing |
| Patient and family goal to improve walking step speed/length |
| Worsening crouch gait |
| Physical exam |
| None |
| Increased popliteal angle > 60° (but not if > 40° and </= 60°) |
| Flexed knee gait |
| Imaging |
| None |
| Assessment of bone age IF using guided growth techniques in combination with MHL |
| Formal 3D gait analysis kinematics |
| Increased knee flexion in stance, especially if > 20° |
| Increased knee flexion at initial contact, especially if > 30° |
| Increased knee flexion at terminal swing |
| Posterior pelvic tilt |
| Modelling of hamstring length that is short and activity that is slow28 |
| Preoperative exam under anaesthesia |
| Fixed flexion deformity of the knee of < 10° |
| Outcome measures/goals |
| Decreased crouch |
| Improved knee extension at initial contact and mid-stance |
| Improvement in step length |
| Improvement in satisfaction |
| Maintain pelvic tilt |
| No knee flexion contracture |
| Improvement in clinical outcome measures, FMS, FAQ, GMFM, GOAL, GVS, GPS |
Consensus in bold type and general agreement in italics; some similar questions were combined FMS, Functional Mobility Scale; FAQ, Functional Ability Questionnaire; GMFM, Gross Motor Function Measure; GOAL, Gait Outcomes Assessment List; GVS, Gait Variable Score; GPS, Gait Profile Score
Commonalities from the expert panel can be elucidated for MHL. Most experts lean heavily on instrumented 3D movement analysis, with a total of eight of their ten consensus points falling into this category. Indications are focused on data that directly support a shortened hamstring during gait as determined by computer modelling techniques or evaluation of excessive knee flexion at initial contact or terminal swing (when the hip is also flexed) and decreased (from normal) pelvic tilt. MHL is uncommonly performed as an isolated procedure by this group of experts, and the trend appears to be that fewer MHL are being performed and for more specific indications. MHL, if performed inappropriately, could contribute to worsening anterior pelvic tilt. The experts use the physical exam as a supplement to the movement analysis data, and caution against performing an MHL if the fixed knee flexion contracture is greater than 10°. In such cases, it was recommended that the knee flexion contracture be addressed at the time of surgery or beforehand. They also caution against vigorous testing of the popliteal angle while the patient is under anaesthesia (even gently) or after the MHL is performed, as it could lead to a stretch injury to the sciatic nerve.
FDO
A total of 55 questions were surveyed: 43 indication questions and 12 outcome questions, for which there was consensus on 29 indication questions, general agreement on seven more and consensus on eight outcome measures with general agreement on one more. Consensus and general agreement by category are listed in Table 4. Questions for which there was consensus (bolded) and general agreement (italics) are listed in Table 6.
Table 6.
Questions for femoral derotational osteotomy (FDO) that reached consensus or general agreement by category
| Clinical problems/history |
|---|
| In toeing (knees) rotating inward while walking especially with associated tripping |
| Hip displacement associated with gait deviations |
| In ambulatory patients with worsening activities of daily living and particularly with lever arm dysfunction |
| Anterior knee pain if other causes are ruled out and conservative measures not effective |
| Cosmetic concerns/appearance as voiced by the patient or family |
| Physical exam |
| Femoral neck angle (anteversion) > 35° (note > 30 did not reach consensus but did reach general agreement); < 30 was non consensus |
| Internal rotation > external rotation, or > 60° on exam, especially with limited (< 20°) external rotation |
| Internal rotation of the knees on observational gait review |
| Determining and differentiating other causes of internal rotation is important (i.e. foot and tibial) |
| FDO are combined with external tibial osteotomies if indicated (this is the focus on another Delphi consensus) |
| Imaging |
| Hip radiographs to assess coverage of the femoral heads and hip dysplasia |
| Formal 3D gait analysis kinematics |
| 3D instrumented movement analysis influenced the decision process |
| Internal rotation of > 15° is an indication |
| Internal foot progression is an indication only when it is a result of hip rotation |
| External pelvic rotation for children with hemiplegic (unilateral) cerebral palsy |
| Preoperative exam under anaesthesia |
| Perform an intraoperative exam under anaesthesia but also consensus that it was not as important as the preoperative exam |
| Similar to preoperative exam, internal rotation > 60°, especially if external rotation is limited to < 20° |
| Femoral neck angle > 30° |
| Use of intraoperative fluoroscopy during surgery to assess femoral anteversion |
| Outcome measures/goals |
| Goal femoral neck angle 5° to 10°, but not < 0° |
| Improved rotation on physical exam (i.e. decreased internal rotation) |
| Hip rotation normalized on 3D movement analysis |
| Subjective improvement |
| Improvement of FMS/FAQ |
| Improvement in the GOAL domain score |
Consensus in bold type and general agreement in italics; some similar questions were combined FMS, Functional Mobility Scale; FAQ, Functional Ability Questionnaire; GOAL, Gait Outcomes Assessment List
Commonalities from the expert panel can be elucidated for FDO. In general, there was much greater consensus for this procedure (67%) than for MHL. Excessive internal rotation was felt to be an important contributor to gait deviations. Physical exam was important and consistent but problems with reliability were recognized. As with MHL, the decision for surgery must be taken in context with the entire patient assessment. Consensus for consideration of FDO was reliably reached when the internal rotation was greater than 15° on instrumented 3D movement analysis or a femoral neck angle (anteversion) of greater than 30° and internal rotation of greater than 60° degrees on physical examination, especially with limited external rotation. Although these measurements loosely correlate, the instrumented movement analysis consensus data were the strongest. Many experts commented on incorporating mild overcorrection (rotation), especially in younger patients.
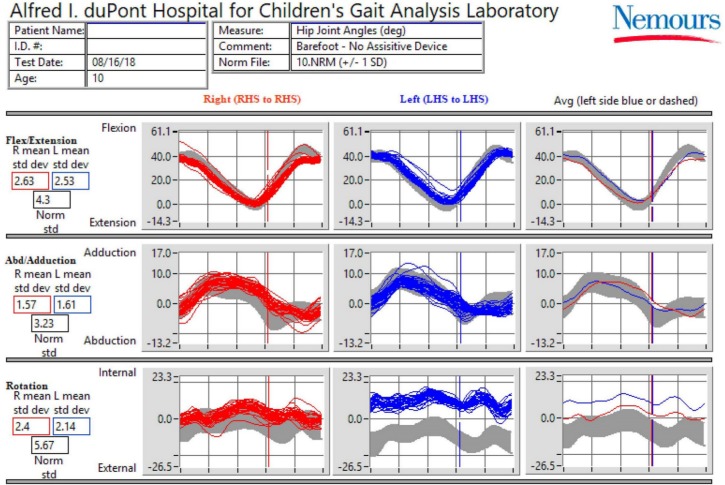
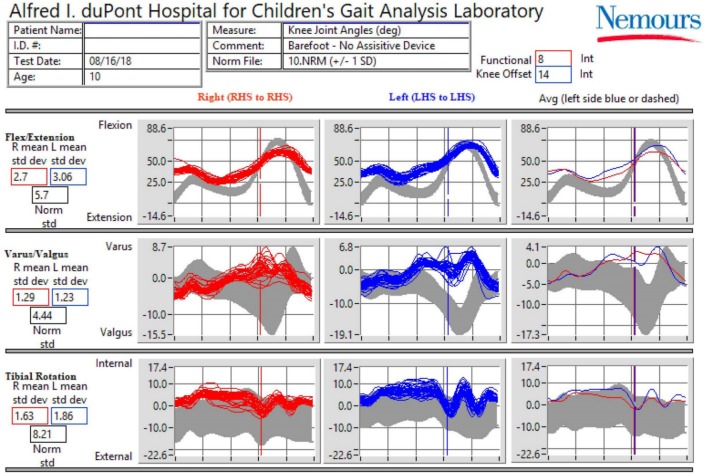
A case example demonstrates physical exam and instrumented gait analysis results (Figs 1 and 2) as indications for MHL and FDO. Specifically, the movement analysis shows increased knee flexion at initial contact and at midstance as the consensus indication for bilateral MHL. Additionally, the physical exam and movement analysis show asymmetric femoral rotation (internal > external) as the consensus indication for FDO on the left, and knee flexion contractures (less than 10°) as the consensus indication for MHL.
Fig. 1.
Hip kinematic data example of indications for femoral derotational osteotomy and medial hamstring lengthening L (HS, left heel strike; RHS, right heel strike).
Fig. 2.
Knee kinematic data example of indications for femoral derotational osteotomy and medial hamstring lengthening (LHS, left heel strike; RHS, right heel strike).
Discussion
This study has multiple strengths. It is the first, to our knowledge, to use a panel of experts in the field of orthopaedic surgery in children with CP to combine best available evidence and expert opinion to identify best-practice indications MHL and FDO, common surgical procedures. The results from this study will allow for more informed evaluation of practice and form the basis for future improvement efforts to standardize surgical recommendations internationally, and are well set up for future multicentre evaluation and improvement studies through the relationships established via the consensus process.
This consensus is especially important for children with CP, who present with a very heterogeneous and often unique combination of biomechanical, neurological and social characteristics. In addition, the treatment options are numerous and often implemented in different combinations. This nearly infinite combination of procedures, in such a diverse group of patients, makes traditional comparison studies very difficult. Gaining consensus from an international group of experts with over 300 years of combined clinical experience can provide insights and help identify areas of consensus, and also bolster clinical equipoise in support of more traditional clinical research study designs.
Our experts lean heavily on the dynamically derived data from 3D instrumented movement analysis for both decision making and outcomes assessment. This certainly is partly due to having access to movement analysis and also a great deal of experience with the evaluation and interpretation of this assessment. Because these treatments are administered in an effort to improve dynamic function and because numerous decisions are made to perform (or importantly not to perform) a particular surgery, it seems the only way to know whether one is making the right decisions. Not everyone will have access to these types of data but as the technology evolves, this barrier will likely be lowered.
No procedure can have a list of surgical indications that can be applied without full assessment of the patient as a whole. These consensus points are only meant as a guide. The process, though, can be applied quickly and provide the foundation for further study. Future plans will be to use this modelled process for additional procedures in the care of the ambulatory patients with CP, including plantar flexor lengthening and tibial osteotomies, as examples.
In conclusion, this expert panel of paediatric orthopaedists with experience in CP and gait analysis were able to achieve consensus on the surgical indications for MHL and FDO in ambulatory children with CP. This project serves as a model for further surgical indication consensus projects in the area of CP, and will hopefully lead to additional research in improving quality and decreasing practice variability in the care of these children.
Open access
This article is distributed under the terms of the Creative Commons Attribution-Non Commercial 4.0 International (CC BY-NC 4.0) licence (https://creativecommons.org/licenses/by-nc/4.0/) which permits non-commercial use, reproduction and distribution of the work without further permission provided the original work is attributed.
Compliance with Ethical Standards
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Ethical statement
Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors.
Informed consent: All subjects were given informed consent and agreed to participate in the project.
ICMJE Conflict of interest statement
JM has received research support in royalties and as a consultant for Nuvasive, has received consulting fees from Synthes and has received royalties from Wolters-Kluwer-Health-Lippincott Williams & Wilkins, all outside of the scope of the submitted work. He has also been an unpaid consultant for OrthoPediatrics and is a board member of the Pediatric Orthopaedic Society of North America, all outside the submitted work.
KG has received research support from NHMRC-CRE outside the scope of the submitted work and is on the Surgeon’s Advisory Board of OrthoPediatrics Corp, all outside the submitted work.
HC has received personal fees from OrthoPediatrics Corp. and Allergan Corp., outside the scope of the submitted work.
JRD is a consultant and board member of OrthoPediatrics Corp., outside the submitted work.
RMK owns stock in Zimmer/Biomet, Medtronic and Johnson and Johnson. He is also on the Editorial Board of the Journal of Pediatric Orthopaedics and his son works for Intrinsic Therapeutics.
JR has received personal fees from OrthoPediatrics Corp., outside the scope of the submitted work.
All other authors declare no conflict of interest.
Author contributions
JM: Conception and design, Acquisition of the data, Analysis and interpretation of the data, Drafting of the article, Critical revision of the article for important intellectual content, Final approval of the article, Obtaining of funding,; Administrative, technical or logistical support, Collection and assembly of data.
MWS: Conception and design, Drafting of the article, Critical revision of the article for important intellectual content, Final approval of the article, Obtaining of funding.
KG: Conception and design, Drafting of the article, Critical revision of the article for important intellectual content, Final approval of the article.
MV: Conception and design, Acquisition of the data, Analysis and interpretation of the data, Drafting of the article, Critical revision of the article for important intellectual content, Final approval of the article, Statistical expertise, Obtaining of funding, Administrative, technical or logistical support, Collection and assembly of data.
LB: Conception & design, Drafting of the article, Critical revision of the article for important intellectual content, Final approval of the article
HC: Conception and design, Drafting of the article, Critical revision of the article for important intellectual content, Final approval of the article.
JRD: Conception and design, Drafting of the article, Critical revision of the article for important intellectual content, Final approval of the article.
RMK: Conception and design, Drafting of the article, Critical revision of the article for important intellectual content, Final approval of the article.
UN: Conception and design, Drafting of the article, Critical revision of the article for important intellectual content, Final approval of the article.
TFN: Conception and design, Drafting of the article, Critical revision of the article for important intellectual content, Final approval of the article.
KP: Conception and design, Drafting of the article, Critical revision of the article for important intellectual content, Final approval of the article.
JR: Conception and design, Drafting of the article, Critical revision of the article for important intellectual content, Final approval of the article.
ER: Conception and design, Drafting of the article, Critical revision of the article for important intellectual content, Final approval of the article.
JS: Conception and design, Drafting of the article, Critical revision of the article for important intellectual content, Final approval of the article.
BJS: Conception and design, Drafting of the article, Critical revision of the article for important intellectual content, Final approval of the article.
TT: Conception and design, Drafting of the article, Critical revision of the article for important intellectual content, Final approval of the article.
AVC: Conception and design, Drafting of the article, Critical revision of the article for important intellectual content, Final approval of the article.
References
- 1.Colver A, Fairhurst C, Pharoah PO. Cerebral palsy. Lancet 2014;383:1240-1249. [DOI] [PubMed] [Google Scholar]
- 2.Mann K, Tsao E, Bjornson KF. Physical activity and walking performance: influence on quality of life in ambulatory children with cerebral palsy (CP). J Pediatr Rehabil Med 2016;9:279-286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Raina P, O’Donnell M, Rosenbaum P, et al. The health and well-being of caregivers of children with cerebral palsy. Pediatrics 2005;115:e626-e636. [DOI] [PubMed] [Google Scholar]
- 4.Dreher T, Vegvari D, Wolf SI, et al. Development of knee function after hamstring lengthening as a part of multilevel surgery in children with spastic diplegia: a long-term outcome study. J Bone Joint Surg [Am] 2012;94-A:121-130. [DOI] [PubMed] [Google Scholar]
- 5.McMulkin ML, Gordon AB, Caskey PM, Tompkins BJ, Baird GO. Outcomes of orthopaedic surgery with and without an external femoral derotational osteotomy in children with cerebral palsy. J Pediatr Orthop 2016;36:382-386. [DOI] [PubMed] [Google Scholar]
- 6.Narayanan UG. Management of children with ambulatory cerebral palsy: an evidence-based review. J Pediatr Orthop 2012;32(suppl 2):S172-S181. [DOI] [PubMed] [Google Scholar]
- 7.Lofterød B, Terjesen T, Skaaret I, Huse AB, Jahnsen R. Preoperative gait analysis has a substantial effect on orthopedic decision making in children with cerebral palsy: comparison between clinical evaluation and gait analysis in 60 patients. Acta Orthop 2007;78:74-80. [DOI] [PubMed] [Google Scholar]
- 8.de Kleuver M, Lewis SJ, Germscheid NM, et al. Optimal surgical care for adolescent idiopathic scoliosis: an international consensus. Eur Spine J 2014;23:2603-2618. [DOI] [PubMed] [Google Scholar]
- 9.Nieuwenhuys A, Õunpuu S, Van Campenhout A, et al. Identification of joint patterns during gait in children with cerebral palsy: a Delphi consensus study. Dev Med Child Neurol 2016;58:306-313. [DOI] [PubMed] [Google Scholar]
- 10.Nene AV, Evans GA, Patrick JH. Simultaneous multiple operations for spastic diplegia. Outcome and functional assessment of walking in 18 patients. J Bone Joint Surg [Br] 1993;75-B:488-494. [DOI] [PubMed] [Google Scholar]
- 11.Schwartz MH, Viehweger E, Stout J, Novacheck TF, Gage JR. Comprehensive treatment of ambulatory children with cerebral palsy: an outcome assessment. J Pediatr Orthop 2004;24:45-53. [PubMed] [Google Scholar]
- 12.McGinley JL, Dobson F, Ganeshalingam R, et al. Single-event multilevel surgery for children with cerebral palsy: a systematic review. Dev Med Child Neurol 2012;54:117-128. [DOI] [PubMed] [Google Scholar]
- 13.Rose GE, Lightbody KA, Ferguson RG, Walsh JC, Robb JE. Natural history of flexed knee gait in diplegic cerebral palsy evaluated by gait analysis in children who have not had surgery. Gait Posture 2010;31:351-354. [DOI] [PubMed] [Google Scholar]
- 14.Narayanan UG. The role of gait analysis in the orthopaedic management of ambulatory cerebral palsy. Curr Opin Pediatr 2007;19:38-43. [DOI] [PubMed] [Google Scholar]
- 15.DeLuca PA, Davis RB III, Ounpuu S, Rose S, Sirkin R. Alterations in surgical decision making in patients with cerebral palsy based on three-dimensional gait analysis. J Pediatr Orthop 1997;17:608-614. [DOI] [PubMed] [Google Scholar]
- 16.Cook RE, Schneider I, Hazlewood ME, Hillman SJ, Robb JE. Gait analysis alters decision-making in cerebral palsy. J Pediatr Orthop 2003;23:292-295. [PubMed] [Google Scholar]
- 17.Wren TA, Otsuka NY, Bowen RE, et al. Outcomes of lower extremity orthopedic surgery in ambulatory children with cerebral palsy with and without gait analysis: results of a randomized controlled trial. Gait Posture 2013;38:236-241. [DOI] [PubMed] [Google Scholar]
- 18.MacWilliams BA, Stotts AK, Carroll KL, D’Astous JL. Utilization and efficacy of computational gait analysis for hamstring lengthening surgery. Gait Posture 2016;49:394-397. [DOI] [PubMed] [Google Scholar]
- 19.Brook RH. The RAND/UCLA appropriateness method. In McCormick KAMSSR. Clinical practice guidelines development: methodology perspectives. Rockville, MD: Agency for Health Care Policy and Research, 1994. [Google Scholar]
- 20.Clark E, Burkett K, Stanko-Lopp D. Let Evidence Guide Every New Decision (LEGEND): an evidence evaluation system for point-of-care clinicians and guideline development teams. J Eval Clin Pract 2009;15:1054-1060. [DOI] [PubMed] [Google Scholar]
- 21.Hsu CC, Sandford BA. The Delphi technique: making sense of consensus. Pract Assess Res Eval. 2017;12:1-8. [Google Scholar]
- 22.Diamond IR, Grant RC, Feldman BM, et al. Defining consensus: a systematic review recommends methodologic criteria for reporting of Delphi studies. J Clin Epidemiol. 2014;67:401-419. [DOI] [PubMed] [Google Scholar]
- 23.Davids JR, Ounpuu S, DeLuca PA, Davis RB 3rd. Optimization of walking ability of children with cerebral palsy. J Bone Joint Surg [Am] 2003;85-A:2224-2234. [PubMed] [Google Scholar]
- 24.Davids JR. Quantitative gait analysis in the treatment of children with cerebral palsy. J Pediatr Orthop 2006;26:557-559. [DOI] [PubMed] [Google Scholar]
- 25.Bickley C, Linton J, Scarborough N, et al. Correlation of technical surgical goals to the GDI and investigation of post-operative GDI change in children with cerebral palsy. Gait Posture 2017;55:121-125. [DOI] [PubMed] [Google Scholar]
- 26.Arnold AS, Liu MQ, Schwartz MH, et al. Do the hamstrings operate at increased muscle-tendon lengths and velocities after surgical lengthening? J Biomech 2006;39:1498-1506. [DOI] [PubMed] [Google Scholar]
- 27.Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377-381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Harris PA, Taylor R, Minor BL, et al. Building an international community of software partners. J Biomed Inform. 95: July 2019, 103-208. [DOI] [PMC free article] [PubMed] [Google Scholar]