Abstract
Purpose:
To compare the accuracy of isolated manual marking and smartphone-assisted manual marking with the Verion image-guided system for toric intraocular lens (IOL) implantation.
Methods:
In this prospective observational study, 42 eyes of 36 patients planned for phacoemulsification with toric IOL implantation with corneal astigmatism >1D as measured on Lenstar LS 900 optical biometer were included. Patients were preoperatively registered and photographed on the Verion image-guided system. In the operating room, the patient's eye was manually marked at the 6 o′ clock limbus (Manual axis-90°) on slit-lamp in sitting position. Next, using the smartphone android app—iToric Patwardhan, the exact mark axis was confirmed (Smartphone axis). Following this, the patient was taken on the operation table where the mark axis was confirmed with Verion digital overlay on an external screen (Verion axis). The absolute angular deviation of manual axis from Verion was compared with the absolute angular deviation of the smartphone axis from Verion as the primary outcome measure.
Results:
The mean absolute angular deviation between the smartphone axis and the Verion axis was 2.62°, which was significantly lower (P < 0.05) than that between the manual axis and Verion axis (4.60°). Moreover, the intraclass correlation coefficient between the smartphone axis and Verion axis was 0.88 indicating a strong agreement between the two.
Conclusion:
Smartphone-assisted manual marking significantly improves the accuracy of manual marking alone when comparing with the Verion Digital Marker system for toric IOL implantation.
Keywords: Smartphone, toric, verion
The prevalence of corneal astigmatism greater than 1.5 dioptres in patients undergoing cataract surgery has been estimated to be between 15% to 29% from various studies.[1,2,3,4] Over the years, there have been many methods described to correct astigmatism in cataract surgery including arcuate keratotomy, limbal relaxing incisions, clear corneal incisions, etc. However, toric IOL implantation with phacoemulsification cataract surgery has been proven to be the most effective way to correct preop corneal astigmatism. The accuracy of toric IOLs depends on the following factors: Accuracy of keratometry measuring devices, accuracy of the calculator being used (accounting for posterior corneal astigmatism), accuracy of preoperative reference markings,[5,6] and finally accuracy of IOL placement in the capsular bag. The preoperative reference markings are done just prior to surgery with the patient in the sitting position and head erect. These markings are performed either freehand or with the help of various marking systems including bubble marker, pendulum marker, gravity marker, digital marker, etc.[7,8,9]
The Verion Digital Marker (Alcon Laboratories, Inc.) is a highly sophisticated instrument where toric IOLs can be aligned without the need for preoperative manual markings. The Verion Digital Marker (VDM) not only avoids the need for preop markings, but has also been shown to significantly reduce to IOL misalignment errors caused by manual marking methods.[10] However, due to its high cost, it may not be economically viable for a majority of ophthalmologists.
With constantly evolving technology, modern smartphones have inbuilt gyroscopes that are capable of measuring rotational acceleration and axis orientation. These gyroscopes along with high-resolution smartphone cameras have been used to develop “apps,” which can determine the exact axis of the corneal limbal marks as a reference to find the correct alignment for a toric IOL during surgery. Such apps include the “iToric Patwardhan” on the android platform (Dr S. Patwardhan) and the “toriCAM”[11] on the iOS platform (Dr G. Barrett – iOS), both of which are available free of cost.
In this study, using the “iToric Patwardhan” android app to assist manual marking, we intend to determine whether the accuracy of manual marking can be improved or not with respect to the VDM. The VDM system has been proven to reduce the inaccuracies caused by preoperative manual marking methods for toric IOL implantation; however, it may not be economically viable. Using the smartphone assist for manual marking can be an easy and cost-effective approach if it can improve the accuracy of isolated manual marking. To our knowledge, there have been no previous published reports that compare the use of smartphone-assisted manual marking with the VDM system.
Methods
This was a prospective observational study conducted at a tertiary eye care center in Western India which included 42 eyes of 36 patient undergoing phacoemulsification cataract surgery with toric IOL implantation. The sample size was calculated by using a pilot sample group of 11 eyes, which were not included in the study. Using the paired samples t-test for the primary outcome measure, the mean difference was found to be 2.18, and the standard deviation of differences was found to be 4.07. Based on this data, keeping the significance level as 0.05 with a power of 90%, the minimum required eyes for a valid study were 39. Thus, a total of 42 eyes were included. Institutional Review Board and Ethics committee clearance was obtained prior to commencement and the study was conducted in adherence to tenets of declaration of Helsinki.
Patients advised cataract extraction with phacoemulsification and toric IOL implantation were enrolled after an informed consent. The incision location, the axis of implantation, and the toric IOL power were decided preoperatively using online calculators. Initially, the Verion Reference Unit was used to capture a high-resolution reference image of the patient's eye in sitting position. Just before the surgery, these patients were reference marked on slit lamp in sitting position. Once the patient's face was comfortably positioned on the chin rest, a single freehand mark with a standard gentian violet marking pen was made at the 6 o′ clock limbus as accurately as possible at 90° [Fig. 1]. This mark at 90° would be considered as the manual axis (MA) mark. Next, using the android app “iToric Patwardhan,” an image of the eye was captured in 2× zoom with the smartphone flashlight on. Once the image was captured, the outer white circular ring was aligned manually with the limbus [Fig. 2: White arrow]. The red protractor line was then aligned such that one end of it passes through the central point of the circle and the other end through the central-most point of the 6 o′ clock limbal mark [Fig. 2: Red arrow). The exact axis of the mark was noted on the top right corner of the screen [Fig. 2: Blue arrow]. In Fig. 2, the axis of the mark can be seen at 89°. This would be considered as the smartphone axis (SA) of the mark. After this, the patient was shifted on the operating table and registration was done on the Verion system by the operating surgeon. The cases which would fail to register with the VDM were excluded from the study. Once the Verion overlay was turned on, the orientation and axis of the mark was noted by the operating surgeon in the operating microscope, and by an observer on the Verion monitor [Fig. 3: Red arrow]. In Fig. 3, the axis of the mark can be seen at 97°. This would be considered as the Verion axis (VA) of the mark.
Figure 1.

Manual marking at 6 o′ clock limbus (90°)
Figure 2.
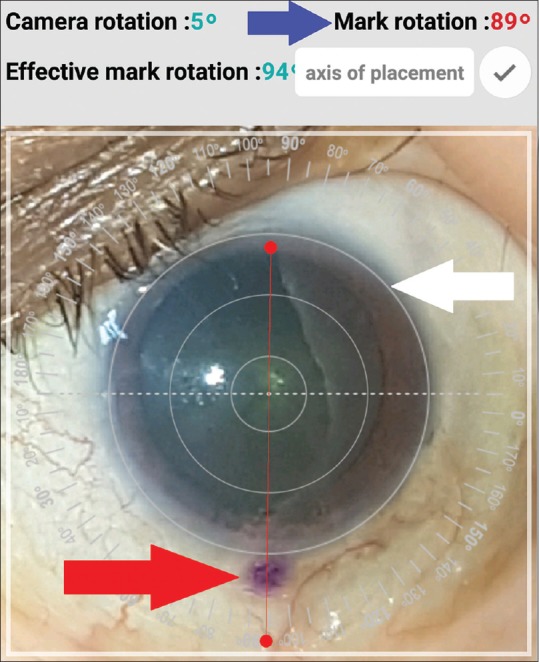
Finding the exact axis of the mark with itoric app, white arrow—align the outer ring with the limbus, red arrow—align the protractor line with the 6 o′ clock mark, and blue arrow—mark axis
Figure 3.
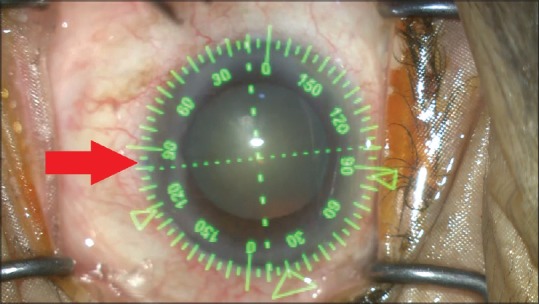
Finding the exact axis of the mark with Verion overlay
The angular deviations of the manual axis (MA) and smartphone axis (SA) were compared with the Verion axis (VA) and calculated as follows: Angular deviation in degrees of the manual axis mark from the Verion axis mark (MAD) was calculated by the formula: MAD = MA − VA. Similarly, angular deviation of smartphone axis mark from the Verion axis mark (SAD) was calculated as SAD = SA − VA. In the examples shown in Figs. 1-3: MA = 90, SA = 89, VA = 97, so MAD = 90 − 97= −7°, and SAD = 89 − 97= −8°. A “−” sign indicated an anticlockwise deviation, and a “+” sign indicated a clockwise deviation from Verion axis. Finally, the absolute angular deviation for both manual and smartphone axes were calculated by removing the “sign” (AMAD-Absolute manual angular deviation, ASAD-Absolute smartphone angular deviation).
The primary outcome measure was to compare the absolute angular deviation of manual marking from VDM (AMAD) versus the absolute angular deviation of smartphone-assisted marking from VDM (ASAD). Secondary outcome measures were to study the agreement level between smartphone-assisted marking and Verion digital marking; and the clockwise and anticlockwise angular deviation of manual and smartphone-assisted marking vs VDM.
Data were entered in MS Excel 2017(Microsoft Corporation, Redmond, USA) and analyzed using Stata Version 15 (StataCorp, College Station, Texas, USA) and MedCalc Statistical Software Version 18.6 (MedCalc Software bvba, Ostend, Belgium; http://www.medcalc.org; 2018). For the primary outcome variables, we calculated the means and standard deviations, or median and interquartile range. The Shapiro Wilk test was used to detect normality of variables and decide whether to use parametric or nonparametric tests. The means were compared using the paired t-test and the medians were compared using the Wilcoxon rank sum test. Agreement testing was done using the intraclass correlation coefficient (ICC) and Bland Altman plots.
Results
Forty-two eyes of 36 patients were included for data analysis, out of which there were 23 males (63.9%) and 13 females (36.1%). The mean age of the population was 62 (42–72) years. Out of the 42 eyes, 23 (54.8%) were right eyes and 19 (45.2%) were left eyes.
The mean absolute angular deviation of manual marking from Verion (AMAD) was 4.60 ± 2.96° and median was 4.00° (2.00–7.00 interquartile range). The mean absolute angular deviation of smartphone axis from Verion (ASAD) was 2.62° ± 2.40° and median was 2.00° (1.00–3.00 interquartile range). Because the Shapiro Wilk test accepted the data to be of normal distribution, the paired t-test was used to compare the data. The ASAD was found to be significantly lower than the AMAD (P-value = 0.0016) indicating increased accuracy of smartphone-assisted marking as compared to isolated manual marking in comparison to Verion.
The agreement testing between the Verion axis and smartphone axis demonstrated an ICC 0.88 with the 95% Confidence interval of 0.78 to 0.94. This indicated a strong agreement between Verion and smartphone axis marking.
The Bland Altman plot [Fig. 4] also confirmed the agreement between Verion axis and smartphone axis by demonstrating the mean difference line between the two being close to zero and most of the points lying between two standard deviations of the difference.
Figure 4.
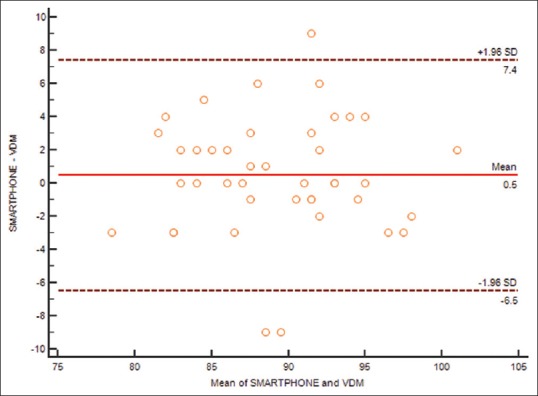
Bland Altman plot for the agreement between smartphone and VDM axis
The percentage of eyes with clockwise, anticlockwise, and no deviation for manual and smartphone axis are summarized in Table 1.
Table 1.
Orientation of Manual and Smartphone axis in comparison with Verion axis
| MA−VA | SA−VA | |
|---|---|---|
| Percentage of eyes with clockwise deviation | 52.38 | 45.24 |
| Percentage of eyes with anticlockwise deviation | 45.24 | 35.71 |
| Percentage of eyes with no deviation | 2.38 | 19.05 |
| Percentage of eyes with same orientation in both groups | 76.19 | |
| Percentage of eyes with opposite orientation in both groups | 23.81 | |
Discussion
Our results demonstrated that the mean absolute angular deviation between smartphone-assisted marking and VDM (2.62) was significantly lower than that between manual marking and VDM (4.6), proving that smartphone-assisted marking improves accuracy.
Both manual and smartphone-assisted axes showed a greater clockwise error than anticlockwise error as compared to VDM [Table 1], though this was not clinically significant. While in almost 20% of eyes smartphone-assisted manual marking showed no deviation from VDM, only 2.38% of isolated manual markings matched with VDM. In both manual and smartphone axes, more than 75% of eyes showed similar orientation error from VDM (either clockwise or anticlockwise), indicating that even though smartphone axis has a lower mean error than manual axis, in most cases the orientation of error from VDM remains the same.
For toric IOLs, because a deviation of 3° from intended axis roughly corresponds to a 10% loss of toricity, marking inaccuracy of > 3° should be considered as a significant source of error. Hence, if VDM is considered the reference, as per our study performing manual marking alone can potentially translate into significant postoperative refractive errors, although this was not evaluated in our study. However, with the above results, we can conclude that if smartphone assistance is used along with manual marking, it can reduce the risk of potential postop refractive errors.
By using ICC and Bland Altman plots, we could study the agreement between the smartphone axis and Verion axis. The results demonstrated strong agreement between the two (0.88), reinforcing the fact that smartphone assistance with manual marking can improve the accuracy of isolated manual marking to nearly match up to Verion's accuracy.
One of the drawbacks in our study is of the assumption that the Verion image-guided system is the gold standard for accurate alignment of the toric IOLs. Both manual and smartphone axis comparisons have been made with the Verion axis. Even though Verion has been shown to have superiority over manual marking methods, there could be some machine errors that may reduce its accuracy.
The study by Pallas et al.[11] was very similar to ours, testing the accuracy of the “toriCAM” application of the iphone. The only difference was that they used the Zaldivar calipers on the iTrace Topographer (Tracey Technologies, Houston, TX) as a reference, whereas we used the Verion system as the reference. The mean absolute error before toriCAM adjustment was 3.18° ± 2.22° which was significantly reduced to 1.28° ± 1.34° after using the application, emphasizing the use of smartphone technology to improve accuracy. In our experience, both the “iToric Patwardhan” and the “toriCAM” apps work equally well, but the former is much easier to use as compared to the latter.
Teichman et al.[12] also demonstrated the effectiveness of using smartphone photography for measuring toric IOL axis in situ, although in this study, they used computer software to measure the axis and only used the smartphone as a camera.
Conclusion
Smartphone-assisted manual marking significantly improves the accuracy of manual marking alone when comparing with the VERION™ Digital Marker system for toric IOL implantation.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
The “itoric Patwardhan” app mentioned in this study is a free application available on all android smartphones. This app has been developed by Dr Saurabh Patwardhan (MD, FRCS) and the authors have no financial or propriety interests in it.
References
- 1.Lyall D, Srinivasan S, Ng J, Kerr E. Changes in corneal astigmatism among patients with visually significant cataract. Can J Ophthalmol. 2014;49:297–303. doi: 10.1016/j.jcjo.2014.02.001. [DOI] [PubMed] [Google Scholar]
- 2.Yuan X, Song H, Peng G, Hua X, Tang X. Prevalence of corneal astigmatism in patients before cataract surgery in Northern China. J Ophthalmol. 2014;2014 doi: 10.1155/2014/536412. Article ID 536412, 7 pages. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ninn-Pedersen K, Stenevi U, Ehinger B. Cataract patients in a defined Swedish population 1986–1990 II Preoperative observations. Acta Ophthalmol (Copenh) 1994;72:10–5. doi: 10.1111/j.1755-3768.1994.tb02729.x. [DOI] [PubMed] [Google Scholar]
- 4.Hoffer KJ. Biometry of 7500 cataractous eyes. Am J Ophthalmol. 1980;90:360–8. doi: 10.1016/s0002-9394(14)74917-7. [DOI] [PubMed] [Google Scholar]
- 5.Visser N, Berendschot TT, Bauer NJ, Jurich J, Kersting O, Nuijts RM. Accuracy of toric intraocular lens implantation in cataract and refractive surgery. J Cataract Refract Surg. 2011;37:1394–402. doi: 10.1016/j.jcrs.2011.02.024. [DOI] [PubMed] [Google Scholar]
- 6.Farooqui JH, Sharma M, Koul A, Dutta R, Shroff NM. Evaluation of a new electronic pre-operative reference marker for toric IOL implantation by two different methods of analysis: Adobe photoshop versus iTrace. Adv Ophthalmol Vis Syst. 2015;2:57. doi: 10.4103/ojo.OJO_163_2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ma JJK, Tseng SS. Simple method for accurate alignment in toric phakic and aphakic intraocular lens implantation. J Cataract Refract Surg. 2008;34:1631–6. doi: 10.1016/j.jcrs.2008.04.041. [DOI] [PubMed] [Google Scholar]
- 8.Carey PJ, Leccisotti A, McGilligan VE, Goodall EA, Moore CB. Assessment of toric intraocular lens alignment by a refractive power/corneal analyzer system and slitlamp observation. J Cataract Refract Surg. 2010;36:222–9. doi: 10.1016/j.jcrs.2009.08.033. [DOI] [PubMed] [Google Scholar]
- 9.Cha D, Kang SY, Kim S-H, Song J-S, Kim H-M. New axis-marking method for a toric intraocular lens: Mapping method. J Refract Surg. 2011;27:375–9. doi: 10.3928/1081597X-20101005-01. [DOI] [PubMed] [Google Scholar]
- 10.Webers VSC, Bauer NJC, Visser N, Berendschot TT, van den Biggelaar FJ, Nuijts RMMA. Image-guided system versus manual marking for toric intraocular lens alignment in cataract surgery. J Cataract Refract Surg. 2017;43:781–8. doi: 10.1016/j.jcrs.2017.03.041. [DOI] [PubMed] [Google Scholar]
- 11.Pallas A, Yeo TK, Trevenen M, Barrett G. Evaluation of the accuracy of two marking methods and the novel toriCAM application for toric intraocular lens alignment. J Cataract Refract Surg. 2018;34:150–5. doi: 10.3928/1081597X-20180115-03. [DOI] [PubMed] [Google Scholar]
- 12.Teichman J, Baig K, Ahmed I. Simple technique to measure toric intraocular lens alignment and stability using a smartphone. J Cataract Refract Surg. 2014;40:1949–52. doi: 10.1016/j.jcrs.2014.09.029. [DOI] [PubMed] [Google Scholar]


