Abstract
Purpose:
To assess the quality and accuracy of glaucoma referrals from ophthalmologist.
Methods:
Retrospective review of patients chart with referral letter to a tertiary glaucoma center between January and December 2017. Patients aged <16 years, lens-induced glaucoma, uveitic glaucoma, and glaucoma following retinal and corneal surgery were excluded.
Results:
A total of 184 patients referred by 55 ophthalmologists were included. Mean patient age (SD) was 57.8 ± 14 years. Intraocular pressure was not documented in the referral letter in 113 (61%) patients, gonioscopy in 174 (95%) patients, disc findings in 149 (81%) patients, and visual fields in 175 (95%) patients. Thirteen (37%) of the 35 patients referred as open angle glaucoma were found to have angle closure glaucoma. Pseudoexfoliation glaucoma was diagnosed in 29 (16%) patients, of which 18 were missed by the referring ophthalmologist.
Conclusion:
In our study >90% of referral letter did not have the essential parameters. A standard template for glaucoma referral is suggested, which will help the patient to get better transfer of care.
Keywords: Angle closure glaucoma, glaucoma, gonioscopy, referral letter
Glaucoma is the leading cause of irreversible blindness in the world. Prevalence of primary open angle glaucoma (POAG) varies between 1.6 and 4%, and primary angle closure glaucoma (PACG) varies between 0.5 and 1.8% in south Indian population. Prevalence of blindness due to POAG ranges between 1.5 and 11.1% and PACG ranges between 5.9 and 20%.[1,2,3,4,5] Blindness due to glaucoma was more common with PACG than POAG despite the prevalence being lower. This demands the need to know the angle status in all patients suspected or diagnosed with glaucoma, so that angle closure glaucoma will not be missed. Treatment of angle closure glaucoma differs from open angle in a way that primary management was laser peripheral iridotomy in these eyes to get rid of pupillary block along with antiglaucoma medication.
Glaucoma largely being an asymptomatic disease warrants early diagnosis and treatment to prevent the patient from becoming blind. In a developing country like India, access to health care is poor; early diagnosis and treatment remain a challenge. Ophthalmologist working at the primary and secondary eye care level plays a major role in diagnosing and referring them to tertiary eye care for further management. To the best of our knowledge, there was no study from India which looked into the glaucoma referrals. Hence, the purpose of the study is to evaluate the quality of referral and the accuracy of diagnosis among the patients referred to a tertiary eye care center.
Methods
We retrospectively reviewed the records of patients referred to glaucoma clinic in a tertiary care center between January 2017 and December 2017. The study was approved by the Institute ethics committee. This study adhered to the tenets of the Declaration of Helsinki. Patients aged <16 years, lens-induced glaucoma, uveitic glaucoma, and glaucoma following retinal and corneal surgery were excluded from the study.
Data collected from the referral were age, gender, visual acuity, intraocular pressure (IOP), gonioscopy, disc findings, antiglaucoma medication (AGM), visual field analysis, diagnosis, and reason for referral. All patients underwent comprehensive eye examination including IOP with Goldmann applanation tonometer (GAT), central corneal thickness measurement, gonioscopy with Sussman 4 mirror gonioscope, and optic disc assessment with 90-D lens by glaucoma specialist. Angle was considered occludable if ≥180° of the posterior trabecular meshwork was not visible. In eyes with occludable angle, indentation was performed to look for the presence of peripheral anterior synechiae. Optic nerve was considered glaucomatous if there was neuroretinal rim thinning, notching, nerve fiber layer defect, or asymmetric disc cupping (difference in cup to disc ratio >0.2 between 2 eyes) in the absence of asymmetry in disc size between the 2 eyes. Visual field was assessed with Humphrey visual field analyzer.
Patients were categorized into one of the following diagnosis:
Glaucoma suspect: IOP <21 mm Hg, open angle with suspicious disc changes and/or suspicious visual fields not definitive of glaucoma
Ocular hypertension (OHT): IOP >21 mm Hg, open angle with normal optic disc and visual fields
POAG: IOP >21 mm Hg, open angle and definite disc damage with or without visual field damage
Normal tension glaucoma (NTG): IOP <21 mm Hg, open angle and definite disc damage with or without visual field damage
Primary angle closure suspect (PACS): Eye with ≥180° of posterior trabecular meshwork not visible on goinioscopy in the absence of synechiae, elevated IOP and glaucomatous optic disc damage
Primary angle closure (PAC): PACS with elevated IOP and/or synechiae without glaucomatous optic disc damage
PACG: PAC with glaucomatous optic disc and visual field damage
Pseudoexfoliation glaucoma (PXG): IOP >21 mm Hg, open or occludable angle, definite optic disc damage with or without visual field damage and presence of pseudoexfoliation material.
Statistical analysis included mean and standard deviation (SD) for continuous variables and percentages for categorical variables. Statistical analysis was performed using commercial software (Stata ver. 13.1; StataCorp, College Station, Tx).
Results
A total of 232 patients were referred by 55 ophthalmologists during the study period, of which 184 met the inclusion criteria [Fig. 1]. Mean age (SD) of the study population was 57.8 ± 14 years; 109 (59%) patients were male and 75 (41%) were female. IOP was not mentioned in the referral letter in 113 (61%) patients. Of the 71 (39%) patients with documented IOP, GAT was used in 48 (68%), noncontact tonometer (NCT) in 14 (20%), and Schiotz tonometer in 9 (12%) patients.
Figure 1.
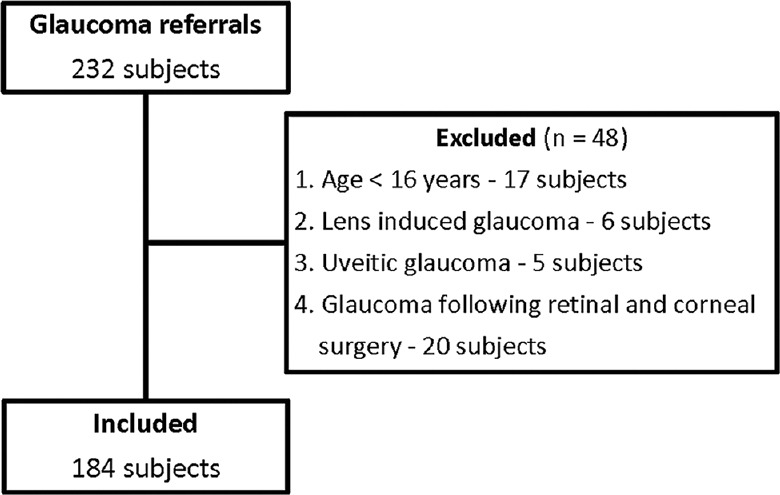
Flow chart of the study cohort
Gonioscopy was not documented in 174 (95%) patients. We found the angle to be occludable in 103 (59%) of the 174 patients. Ten patients had angle status (7 open and 3 occludable) mentioned in their referral letter. Of the 7 patients with open angle, 4 were found to have occludable angle necessitating laser iridotomy. Optic nerve head detail was available in 35 (19%) patients, visual field analysis was available in 9 (5%) patients, and central corneal thickness was documented in 8 patients (4.4%). Sixty (33%) patients were on AGM at the time of referral with a mean of 1.93 ± 1.7. Of these 60 patients, 2 were diagnosed to be normal and their AGM was stopped.
Among the 102 patients referred as glaucoma suspect, we concurred with the diagnosis of glaucoma suspect in 6 patients, and identified OHT in 7 patients, POAG in 17 patients, NTG in 1 patient, PXG in 11 patients, primary angle closure disease (PACD) in 54 patients, and 6 patients were normal. Six out of 11 patients with pseudoexfoliation had occludable angle. Of the 54 patients diagnosed with PACD, 18 had optic neuropathy.
Thirty-five patients were referred as POAG, in which 13 were diagnosed with PACG, 5 with PXG and 2 with OHT. Among the 30 patients referred as PACD, 4 were found to be normal and 1 had PXG. All the 11 patients referred as PXG had the disease, of which 9 had occludable angle and underwent laser peripheral iridotomy. Comparison between referral diagnosis and actual diagnosis at our glaucoma clinic is shown in Table 1.
Table 1.
Comparison between referral and actual diagnosis
| Diagnosis | Referral diagnosis No (%) | Actual diagnosis No (%) |
|---|---|---|
| Glaucoma suspect | 102 (56) | 8 (4) |
| Ocular hypertension | 2 (1) | 10 (5.5) |
| Normal tension glaucoma | 4 (2) | 1 (0.5) |
| Primary open angle glaucoma | 35 (19) | 32 (17.5) |
| Primary angle closure disease | 30 (16) | 94 (51) |
| Pseudoexfoliation glaucoma | 11 (6) | 29 (16) |
| Normal | - | 10 (5.5) |
Positive predictive value of referral diagnosis was 32% (95% CI 25% to 39%) overall, with PXG having the highest (100%; 95% CI 68% to 100%) followed by PACD (83%; 65% to 94%), OHT (50%; 3% to 97%), POAG (43%; 27% to 60%), glaucoma suspect (6%; 2% to 13%), and NTG (0%).
Discussion
Glaucoma being a chronic and silent disease goes undiagnosed until late in the disease. Population-based studies from South India have reported that >80% of patients diagnosed with primary glaucoma were undetected previously.[2,3,4,5] This shows the magnitude of undiagnosed glaucoma in the country. The reasons for this were the asymptomatic nature of the disease in its early stages, poor access to health care, lack of awareness about the disease, and lack of comprehensive eye examination who seek eye care.
Intraocular pressure is the only modifiable risk factor in patients with glaucoma and information about the baseline IOP will help in determining the ideal target pressure for the patient. In our study, none of the referral letters had information about baseline IOP and only 39% had information about IOP. Measurement of IOP by GAT is still considered to be the gold standard even with the advent of newer modalities for measuring IOP. Of the 39% with documented IOP, 68% had IOP measured with GAT, which is better than 49% reported by Founti et al.[6] Sixty patients were on AGM when referred to us, of which 24 did not have documented IOP in the referral letter. Of the 36 patients on AGM with documented IOP, NCT was used to measure the IOP in 5 patients and Schiotz tonometer in 3 patients. Six patients referred as glaucoma suspect for elevated IOP (4 with NCT and 2 with Schiotz) were found to have normal IOP with GAT. Sheehan et al. had reported normal IOP with GAT in 63% of patients who had IOP >21 mmHg with NCT and concluded that the usage of GAT will reduce unnecessary referrals.[7]
Primary angle closure disease was more common among Asians than Caucasians and Africans. Even in Asians, POAG was more prevalent than PACG, but the prevalence of blindness was more with PACG due to the severity of the disease. This stresses the importance of knowing the angle status of the eye in a patient diagnosed with glaucoma. In our study, 174 (95%) referrals did not have the angle status. Varma et al. reported lack of angle status in 74% of the referrals in their study.[8] Hence, the problem of overlooking angle status is an issue worldwide and not only in India. Varma et al.[9] also reported Asian race as one of the important predictors for angle closure disease, with globalization and increasing number of Asians migrating throughout the world, the need to perform gonioscopy has to be stressed across the world.
In our study, 13 (37%) patients treated and referred to us as open angle glaucoma were diagnosed to be angle closure glaucoma, which is similar to 40% reported by Vijaya et al.[4] The reason for the misdiagnosis could be performing the procedure without dimming the room light, inadvertent indentation, and not repeating the gonioscopy at regular intervals, or diagnosing open angle based on Van-Herick's test without performing gonioscopy. The sensitivity and specificity of Van-Herick's test to diagnose angle closure disease were only 62% and 89%, respectively.[10] Hence, gonioscopy is mandatory in all patients with suspected or diagnosed glaucoma. Gonioscopy has to be repeated every year be it open or occludable angle, as open angle eyes can develop angle closure over a period of time due to increase in the lens thickness with age, and increase in synechiae could be the earliest sign of progression in an angle closure eye.
In our study, 29 (16%) patients had PXG, of which 18 were missed by the referring ophthalmologist. Prevalence of pseudoexfoliation in South Indian population was reported to be 6%.[11] Pseudoexfoliation is a strong independent risk factor for progression with faster progression rate than high tension glaucoma.[12] Prevalence of occludable angle is twice as common in patients with pseudoexfoliation as those without.[13] We found occludable angle in 19 out of 29 (65%) patients in our study.
Nine (5%) patients had proper documentation of relevant parameters in the referral letter in our study compared to 24% reported by Cheng et al.[14] Based on the Canadian glaucoma referral template,[15] we propose a new referral template [Table 2]. We have included 17 components in the template which we felt necessary in a glaucoma referral letter and will greatly help in the management of a patient. One of the important parameter we added in our template is the angle status, and another one is the details of the referring doctor, which immensely helps us in sending the detailed report regarding the diagnosis and the plan of management of the patient. This also helps us in creating a mutual relationship between the tertiary eye care centre and the referring doctor in the care of patient. We will be sending this referral format to all doctors in our referral database and request them to use it when they are referring a patient. This format also reminds everyone of the checklist that needs to be completed while managing a patient with glaucoma.
Table 2.
Referral letter template for glaucoma
| Patient details | 1. Name | |||
| 2. Date of birth | ||||
| Patient systemic details | 3. Medical illness | |||
| 4. Allergies | ||||
| Ophthalmic details | Right eye | Left eye | ||
| 5. Visual acuity | ||||
| 6. IOP (by ) | Maximum/pretreatment | |||
| Recent | ||||
| 7. Angle status - Open or occludable | ||||
| 8. Disc details - past and recent | ||||
| 9. Field changes - past and recent | ||||
| 10. Antiglaucoma medication - Number and duration | ||||
| 11. Surgery - glaucoma/other | ||||
| 12. Condition associated with glaucoma -Pseudoexfoliation or Pigment dispersion | ||||
| 13. Other ocular pathology | ||||
| Ophthalmic diagnosis | 14. Diagnosis | |||
| 15. Duration of glaucoma | ||||
| 16. Reason for referral | ||||
| Referral doctor details | 17. Name, address, contact number and e-mail id | |||
Major limitation of our study is its retrospective nature. We did not contact the referring doctor to get information about the missed parameters in the referral letter. Nondocumentation of relevant parameters in the referral letter does not necessarily mean that the referring doctor has not performed the procedure.
Conclusion
Our study highlights the need for improvement in glaucoma referral letter. Using a standard referral template will help in better transfer of care from the primary physician to the tertiary eye care center.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We would like to thank all our referral doctors for the dedication and the care they give to the patients despite their limited resources and logistics, and play a major role in eliminating needless blindness.
References
- 1.Tham YC, Li X, Wong TY, Quigley HA, Aung T, Cheng CY. Global prevalence of glaucoma and projections of glaucoma burden through 2040: A systematic review and mata-analysis. Ophthalmology. 2014;121:2081–90. doi: 10.1016/j.ophtha.2014.05.013. [DOI] [PubMed] [Google Scholar]
- 2.Ramakrishnan R, Nirmalan PK, Krishnadas R, Thulasiraj RD, Tielsch JM, Katz J, et al. Glaucoma in a rural population of southern India: The Aravind comprehensive eye survey. Ophthalmology. 2003;110:1484–90. doi: 10.1016/S0161-6420(03)00564-5. [DOI] [PubMed] [Google Scholar]
- 3.Vijaya L, George R, Baskaran M, Arvind H, Raju P, Ramesh S, et al. Prevalence of primary open angle glaucoma in an urban South Indian population and comparison with a rural population: The Chennai glaucoma study. Ophthalmology. 2008;115:648–54. doi: 10.1016/j.ophtha.2007.04.062. [DOI] [PubMed] [Google Scholar]
- 4.Vijaya L, George R, Arvind H, Baskaran M, Ramesh S, Raju P, et al. Prevalence of primary angle closure disease in an urban South Indian population and comparison with a rural population: The Chennai glaucoma study. Ophthalmology. 2008;115:655–60. doi: 10.1016/j.ophtha.2007.05.034. [DOI] [PubMed] [Google Scholar]
- 5.Garudadri C, Senthil S, Khanna RC, Sannapaneni K, Rao HB. Prevalence and risk factors for primary glaucomas in adult urban and rural populations in the Andra Pradesh eye disease study. Ophthalmology. 2010;117:1352–9. doi: 10.1016/j.ophtha.2009.11.006. [DOI] [PubMed] [Google Scholar]
- 6.Founti P, Topouzis F, Hollo G, Cvenkel B, Lester M, Haidich AB, et al. Prospective study of glaucoma referrals across Europe: Are we using resources wisely? Br J Ophthalmol. 2018;102:329–37. doi: 10.1136/bjophthalmol-2017-310249. [DOI] [PubMed] [Google Scholar]
- 7.Sheehan W, Adams D, Wells C, Booth A. Does Goldmann applanation tonometry performed by community optometrists reduce referrals? A pilot study. Br J Ophthalmol. 2011;95:295. doi: 10.1136/bjo.2010.189852. [DOI] [PubMed] [Google Scholar]
- 8.Varma DK, Simpson SM, Rai AS, Ahmed IIK. Undetected angle closure in patients with a diagnosis of open-angle glaucoma. Can J Ophthalmol. 2017;52:373–8. doi: 10.1016/j.jcjo.2016.12.010. [DOI] [PubMed] [Google Scholar]
- 9.Varma DK, Kletke SN, Rai AS, Ahmed IIK. Proportion of undetected narrow angles or angle closure in cataract surgery referrals. Can J Ophthalmol. 2017;52:366–72. doi: 10.1016/j.jcjo.2017.01.008. [DOI] [PubMed] [Google Scholar]
- 10.Thomas R, George T, Braganza A, Muliyil J. The flashlight test and van Herick's test are poor predictors for occludable angles. Aust N Z J Ophthalmol. 1996;24:251–6. doi: 10.1111/j.1442-9071.1996.tb01588.x. [DOI] [PubMed] [Google Scholar]
- 11.Krishnadas R, Nirmalan PK, Ramakrishnan R, Thulasiraj RD, Katz J, Tielsch JM, et al. Pseudoexfoliation in a rural population of Southern India: The Aravind comprehensive eye survey. Am J Ophthalmol. 2003;135:830–7. doi: 10.1016/s0002-9394(02)02271-7. [DOI] [PubMed] [Google Scholar]
- 12.Heijl A, Bengtsson B, Hyman L, Leske C for the Early Manifest Glaucoma Trial Group. Natural history of Open-angle glaucoma. Ophthalmology. 2009;116:2271–6. doi: 10.1016/j.ophtha.2009.06.042. [DOI] [PubMed] [Google Scholar]
- 13.Arvind H, Raju P, Paul PG, Baskaran M, Ramesh SV, George RJ, et al. Pseudoexfoliation in South India. Br J Ophthalmol. 2003;87:1321–3. doi: 10.1136/bjo.87.11.1321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cheng J, Beltran-Agullo L, Trope GE, Buys YM. Assessment of the quality of glaucoma referral letters based on a survey of glaucoma specialists and a glaucoma guideline. Ophthalmology. 2014;121:126–33. doi: 10.1016/j.ophtha.2013.08.027. [DOI] [PubMed] [Google Scholar]
- 15.Canadian Ophthalmological Society Glaucoma Clinical Practice Guideline Expert Committee. Canadian Ophthalmological Society evidence-based clinical practice guidelines for the management of glaucoma in the adult eye. Can J Ophthalmol. 2009;44:s7–54. doi: 10.3129/cjo44s1. [DOI] [PubMed] [Google Scholar]


