Abstract
Purpose
Aberrant glycosylation of the histo-blood group antigens (including the angina bullosa haemorrhagica [ABH]) is often observed during malignant transformation in most types of carcinomas. Data concerning their ethnic distributions are diverse which explains why their biological characteristics have to be studied in different populations. Our aim was to analyze the expression of the histo-blood group (specifically the ABH) antigens in breast carcinoma.
Methods
The expression of the histo-blood group (specifically the ABH) antigens was studied in 109 patients with breast carcinoma using immunohistochemistry. Statistical analysis was performed using χ2 and Fisher analyses.
Results
The loss of expression of histo-blood group (ABH) antigens in breast carcinoma was observed in 81.13% of patients with blood group O, 37.93% with blood group A, and 96.30% with blood group B. One key finding of this study was that the loss of expression of the ABH antigen was also observed in normal tissues adjacent to the tumor. The loss of expression was associated with higher tumor grade (p < 0.05). Expression of H antigen was observed in 50% of cases with loss of expression of B antigen and was associated with human epidermal growth factor receptor 2 (HER2) overexpression (p < 0.05). The loss of H antigen in patients with blood group O was associated with estrogen receptor expression (p < 0.001). Incompatible A antigen in tumor was expressed in 20.75% of patients with blood group O.
Conclusion
Loss of the ABH antigens correlated with the Scarff-Bloom-Richardson histologic grading. H antigen was associated with HER2 overexpression in breast cancer. However, further studies are needed to determine the role of incompatible A antigen in mammary carcinogenesis.
Keywords: Antigens, Blood, Breast, Carcinoma, Histocompatibility
INTRODUCTION
Histo-blood group antigens are complex carbohydrate structures covalently bound to glycoproteins or glycosphingolipids. They were initially identified on erythrocytes and later found to be widely distributed in human tissues including the epithelium, neurons, platelets, and the vascular endothelium [1]. The synthesis of these antigens requires specific enzymatic machinery involving 3 transferases that add monosaccharides to a precursor molecule and that are coded for by distinct genes [2,3]. The α-(1, 2) fucosyltransferase forms the H antigen, precursor of the A and B antigens. N-acetyl galactosamine transferase and galactosamine transferase form the A and B antigens by a respective addition of a residue N-actylgalactosamine or D-galactose on the β-galactose of the H antigen [4]. In the tissues derived from mesoderm and ectoderm, the α-(1, 2) fucosyltransferase is encoded by FUT1 (H) gene, N-acetyl galactosamine transferase and galactosamine transferase are encoded by the ABO gene [5,6]. The expression patterns of the histo-blood group antigens vary according to the type of tissue, cell differentiation, and degrees of epithelial cell maturation. These antigens play an important role in cell recognition, proliferation, adhesion, motility, and therefore, in the organization of tissues and organs, such as the epidermal growth factor receptors, integrin, cadherin, and CD44 [5]. Changes in the structure of carbohydrates are key events in oncogenic transformation and may be involved in tumor progression and invasion [7]. Aberrant expression of blood group and related antigens is often observed in carcinomas of the colon, larynx, bladder, stomach, oral cavity, and lung and has been classified into 3 types: loss of expression, oncofetal, and incompatible expression such as A-like expression [8]. The expression of A and B antigens is associated with good prognosis in some cancers, while their complete deletion has been correlated with poor prognosis [9]. However, whether these antigens can be used as tumor markers in diagnosis or therapy remains to be verified. Furthermore, data concerning their ethnic distribution are different. Thus, their biological characteristics have to be studied in different populations. Breast cancer is a heterogeneous disease. It is the most common malignancy diagnosed among women and a leading cause of cancer death with over 400,000 deaths annually worldwide [10]. In Morocco, breast cancer is the most common cancer among women and the third most common among all registered cancer cases [11]. However, there are no studies concerning the alterations in the histo-blood group antigen expression in breast cancer. Our aims were to study the expression of histo-blood group antigens in breast carcinoma versus normal breast tissue and to investigate the association between ABH expression patterns and different prognostic factors such as tumor size and grade, overexpression of human epidermal growth factor receptor 2 (HER2), hormones receptors (estrogen and progesterone), and lymph nodes status.
METHODS
Specimens
The study was retrospectively performed on archived tissue samples fixed in formalin and embedded in paraffin. Access to all the samples and data concerning anatomopathology and blood groups was performed anonymously and in accordance with the Declaration of Helsinki. No patient informed consents were required. Experiments performed in this study were evaluated and approved by the Ethic Committee for Biomedical Research of Rabat of the Faculty of Sciences, Mohammed V University (N° Fsr-umv-1214-93).
The retrospective study involved 109 samples from patients diagnosed with breast carcinoma between 2011 and 2012. Samples were obtained through mammary tumorectomy or mastectomy from the Department of Pathology, Ibn Rochd University Hospital in Casablanca. All samples were formalin fixed and paraffin-embedded (FFPE). Each sample contained representative portions of both tumor and adjacent normal mammary tissue, and cases without normal tissues were excluded. Tumors were analyzed by 3 pathologists to evaluate the histologic type and grade according to the World Health Organization classification and the modified Scarff-Bloom-Richardson (SBR) grading [12]. Clinical and pathological information including age, tumor size, expression of estrogen and progesterone receptors, and lymph node involvement were collected from the pathology department. The status of the HER2 was determined by immunohistochemistry. The blood group type was obtained from the Department of Maternity, Ibn Rochd University Hospital.
Antibodies
Murine monoclonal antibodies anti-A (clone A907; National Blood Transfusion Hematology Center, Rabat, Morocco), anti-B (clone B958IIH4; National Blood Transfusion Hematology Center), anti-H (R TransClone anti-H1 86343; Bio-Rad, Hercules, USA), and anti-human HER2 (HercepTestTM, K5204; Dako Company, Santa Clara, USA) protein were used for immunohistochemistry. The antibodies were diluted to appropriate working concentrations that resulted in maximum staining of endothelial and epithelial cells.
Staining
Briefly, FFPE tissue samples were cut into 3-µm thick sections, mounted on (Superfrost®; Menzel-Gläser-Thermo Scientific, France) adhesive slides and heated to 60°C for 1 hour to remove the paraffin from the surface. The sections were gradually dewaxed and rehydrated 3 times in toluene and ethanol. Then, they were heated with a solution of 0.3% hydrogen peroxide for 10 minutes to block the endogenous peroxide and then rinsed twice with Tris-buffered saline. To eliminate the nonspecific binding, sections were incubated for 20 minutes in a blocking solution (skimmed milk 2.5%) before incubating with the monoclonal antibody, at 22°C for 30 minutes. After washing with Tris-buffered saline, sections were incubated for 30 minutes with mouse anti-immunoglobulins conjugated to (Dako Real™ Envision™ Detection System-K5007; Dako Company) a peroxidase labeled dextran polymer. Serial sections were then developed in 3,3′ diaminobenzidine solution for 3 minutes, counterstained with hematoxylin, rinsed with running water, dehydrated with ethanol, cleared with toluene, and mounted on microscopic slides. The negative control was incubated with phosphate-buffered saline. Histological sections were viewed using an optical microscope. The evaluation of the immunohistochemical (IHC) staining of ABH antigens was carried out by assessing both the percentage of cells stained and the intensity of staining giving a score of 0 for negative, + for weak, ++ for moderate and +++ for strong. Staining was considered positive when the percentage of cells stained was greater than 5%.
The marking of each sample was compared based on the endothelial cells that served as an internal control. The intensity of staining of endothelial cells was found to be strong in all the cases and percentage of positive cells was ≥ 90%. HER2 staining was performed according to the manufacturer's instructions [13]. HER2 equivocal cases status (HercepTest score 2+) was confirmed using an in situ hybridisation technique.
Statistical analysis
The correlation between the staining results and different clinical and histopathological variables was analyzed using the χ2 and Fisher tests with Statistical Package for Social Science (SPSS) 28 software (17.0; IBM corp., Armonk, USA). The p = 0.05 was considered statistically significant.
RESULTS
The phenotypic and histological features of the 109 patients are shown in Table 1. The median age of at the time of breast cancer diagnosis was 51.60 years. Patients were of blood types O (n = 53), A (n = 29), and B (n = 27). The average tumor size was 4.58 cm (ranging between 0.7 and 20 cm).
Table 1. Clinical and histopathological features of 109 breast carcinoma patients.
| Patient characteristics | Blood groups | ||||
|---|---|---|---|---|---|
| O | A | B | Total | ||
| Median age (yr) | 50.87 (28–71) | 50.92 (31–70) | 54.04 (31–90) | 51.94 (28–90) | |
| Histologic type | |||||
| Invasive ductal carcinoma | 50 (94.34) | 27 (93.10) | 25 (92.60) | 102 (93.58) | |
| Invasive lobular carcinoma | 2 (3.77) | 2 (6.90) | 1 (3.70) | 5 (4.58) | |
| Sarcomatoid carcinoma | 0 (0) | 0 (0) | 1 (3.70) | 1 (0.92) | |
| Invasive micropapillary carcinoma | 1 (1.89) | 0 (0) | 0 (0) | 1 (0.92) | |
| Tumor size (cm) | |||||
| ≤ 2 | 11 (20.75) | 4 (13.79) | 4 (14.82) | 19 (17.43) | |
| > 2 | 42 (79.25) | 23 (79.31) | 22 (81.48) | 87 (79.82) | |
| Missing | 0 (0) | 2 (6.90) | 1 (3.70) | 3 (2.75) | |
| Tumor grade | |||||
| SBR 1 | 3 (5.66) | 2 (6.90) | 4 (14.81) | 9 (8.26) | |
| SBR 2 | 27 (50.94) | 21 (72.41) | 8 (29.63) | 56 (51.38) | |
| SBR 3 | 23 (43.40) | 6 (20.69) | 15 (55.56) | 44 (40.36) | |
| HER2+ status | |||||
| Negative | 38 (71.70) | 23 (79.30) | 13 (48.15) | 74 (67.89) | |
| Positive | 15 (28.30) | 6 (20.70) | 14 (51.85) | 35 (32.11) | |
| Estrogen receptor status | |||||
| Negative | 12 (22.64) | 8 (27.59) | 7 (25.92) | 27 (24.77) | |
| Positive | 28 (52.83) | 11 (37.93) | 10 (37.04) | 49 (44.96) | |
| Missing | 13 (24.53) | 10 (34.48) | 10 (37.04) | 33 (30.27) | |
| Progesterone receptor status | |||||
| Negative | 12 (22.64) | 8 (27.59) | 7 (25.92) | 27 (24.77) | |
| Positive | 28 (52.83) | 11 (37.93) | 10 (37.04) | 49 (44.96) | |
| Missing | 13 (24.53) | 10 (34.48) | 10 (37.04) | 33 (30.27) | |
| Lymph node status | |||||
| Negative | 29 (54.72) | 14 (48.27) | 10 (37.04) | 53 (48.62) | |
| Positive | 14 (26.41) | 7 (24.14) | 10 (37.04) | 31 (28.44) | |
| Missing | 10 (18.87) | 8 (27.59) | 7 (25.92) | 25 (22.94) | |
| No. of patients (n = 109) | 53 | 29 | 27 | 109 (100) | |
Values are presented as median (range) or number (%).
HER2 = human epidermal growth factor receptor 2.
Expression of histo-blood group antigens in normal and tumor breast tissue
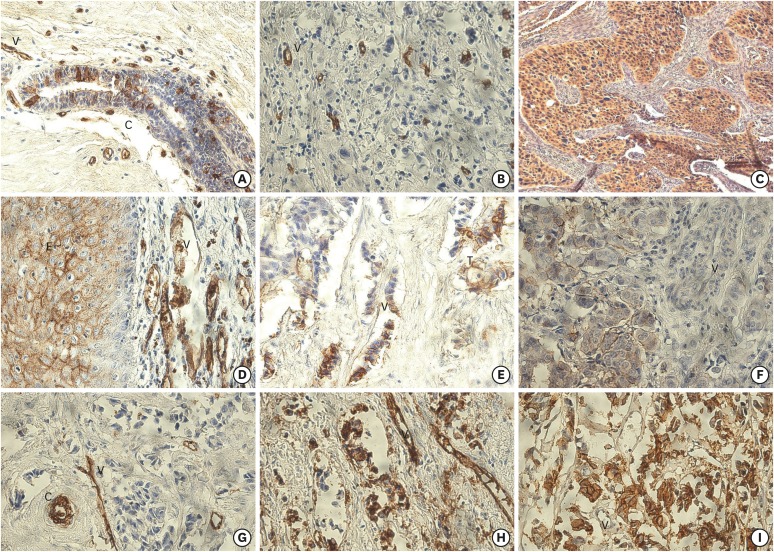
The expression of ABH antigens was observed in the vascular endothelium, erythrocytes, and normal epithelium of the breast tissue detected immunohistochemically using 3 antibodies (anti-A, anti-B, and anti-H). The 17 IHC expression patterns obtained for the 109 patients are presented in Table 2. Loss of expression of ABH antigens was observed in tumor and in breast tissues adjacent to tumor identified as ‘normal’ by the pathologists. In patients with blood type O (n = 53), a loss of H antigen was noted in 81.13% (43/53) of cases. This loss of expression was observed in the tumor tissue only and in both tumor and adjacent normal tissue the loss of expression was observed in 34.88% (15/43) and 65.12% (28/43) of cases, respectively. The H antigen was expressed in the tumor and normal tissue in 18.87% (10/53) of the cases. Among these, 20.75% (11/53) of cases showed cytoplasmic staining with A antibody in malignant cells (Figure 1A-C).
Table 2. ABH antigenes expression in normal and tumor tissues and endothelial cells (n = 109).
| Blood group | Anti-H | Anti-A | Anti-B | No. of patients | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| EC | N | T | EC | N | T | EC | N | T | ||
| O | + | + | + | − | − | − | − | − | − | 9 |
| O | + | + | − | − | − | − | − | − | − | 10 |
| O | + | − | − | − | − | − | − | − | − | 23 |
| O | + | + | + | − | − | + | − | − | − | 1 |
| O | + | + | − | − | − | + | − | − | − | 5 |
| O | + | − | − | − | − | + | − | − | − | 5 |
| A | − | − | − | + | + | + | − | − | − | 12 |
| A | − | + | + | + | + | + | − | − | − | 6 |
| A | − | − | − | + | + | − | − | − | − | 5 |
| A | − | − | + | + | + | − | − | − | − | 1 |
| A | − | − | + | + | − | − | − | − | − | 3 |
| A | − | − | − | + | − | − | − | − | − | 2 |
| B | − | − | − | − | − | − | + | + | + | 1 |
| B | − | − | − | − | − | − | + | + | − | 9 |
| B | − | − | + | − | − | − | + | + | − | 9 |
| B | − | − | − | − | − | − | + | − | − | 4 |
| B | − | − | + | − | − | − | + | − | − | 4 |
EC = endothelial cells; N = normal mammary epithelial cells; T = tumor cells; (+) = positive reaction; (−) = negative reaction.
Figure 1. Immunohistochemical staining of mammary histological sections: Patient with blood type O; (A) Normal breast tissue showing positive staining of endothelial (V) and ductal epithelial cells (C) with anti-H antibody (× 20). (B) Ductal carcinoma with positive staining of endothelial and negative staining of tumor cells using anti-H antibody (× 20). (C) Ductal carcinoma showing positive staining of cytoplasm in tumor cells using anti-A antibody (× 20). Patient with blood type A; (D) Normal breast tissue showing positive staining of endothelial and epidermal cells using anti-A antibody (× 20). (E) Ductal carcinoma with positive staining of endothelial cells and focal positive expression of tumor cells using of anti-A antibody (× 20). (F) Ductal carcinoma showing positive staining of tumor cells using of anti-H antibody (× 20). Patient with blood type B; (G) Normal breast tissue with positive staining of endothelial and ductal epithelial cells using anti-B antibody (× 20). (H) Ductal carcinoma showing positive staining of endothelial cells and tumor cells using anti-B antibody (× 20). (I) Ductal carcinoma with negative staining of endothelial cells and positive staining of infiltrating tumor cells using anti-H antibody (× 20).
C = galactophoric duct; V = vessel.
In patients with blood group A (n = 29), the loss of expression of A antigen was observed in the tumor and both in tumor tissue and the surrounding epithelial cells in 54.54% (6/11) and 45.45% (5/11) of the cases, respectively. Hence, the A antigen loss was observed in 37.93% overall. The expression of A antigen was maintained in the normal and tumor tissue in 62.07% (18/29). The expression of the H antigen was observed in 34.48% (10/29) cases with blood group A (Figure 1D-F).
In patients with blood group B (n = 27), the loss of B antigen expression was noted in 96.30% cases. It was observed in the tumor tissue only and both tumor and normal tissue in respectively 69.23% (18/26) and 30.77% (8/26) of the cases. Only one patient retained the B antigen expression in normal and tumor cells. Out of 26 patients who lost the B antigen, 50% (13/26) expressed H antigen in the tumor (Figure 1G-I).
The comparison of IHC results presented in Table 3, taking 2 groups N+T+ versus N+T− and N− T− together, reveals that the antigenic loss is observed more in patients with blood type B (96.30%) and O (81.13%) compared to blood type A (37.93%). The difference was statistically significant (p < 0.01).
Table 3. Number of patients maintained or lost the expression of appropriate antigens according to blood group type.
| Blood group | Appropriate antigen maintained expression in tumor | Appropriate antigen lost expression in tumor | p-value |
|---|---|---|---|
| O (n = 53) | 10 (18.87) | 43 (81.13) | 0.001 |
| A (n = 29) | 18 (62.07) | 11 (37.93) | |
| B (n = 27) | 1 (3.70) | 26 (96.30) |
Values are presented as number (%).
Expression of histo-blood group antigens and tumor grade
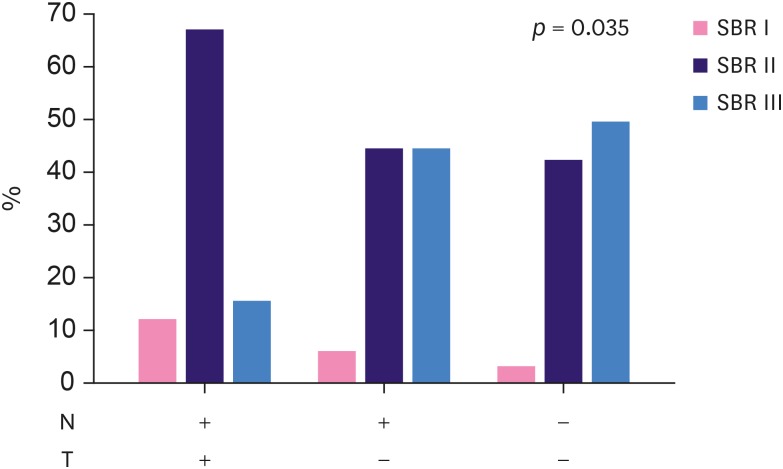
No correlation was found between the loss of expression of H and A antigens and SBR tumor grade among patients with blood group O and A. An association between the loss of expression of B antigen and SBR 3 grade was observed but it was not statistically significant (p = 0.056). The loss of expression of A, B, and H antigens studied in whole, was observed in 80/109 cases versus 29/109 that retained the expression. This loss of expression was associated with higher tumor grade SBR 3 (p < 0.05) (Figure 2).
Figure 2. Distribution of ABH antigens expression profiles based on the SBR grade in 109 patients.
N = normal mammary epithelial cells; T = tumor tissue; ABH = angina bullosa haemorrhagica; SBR = Scarff-Bloom-Richardson.
Expression of histo-blood group antigens and estrogenic receptor status
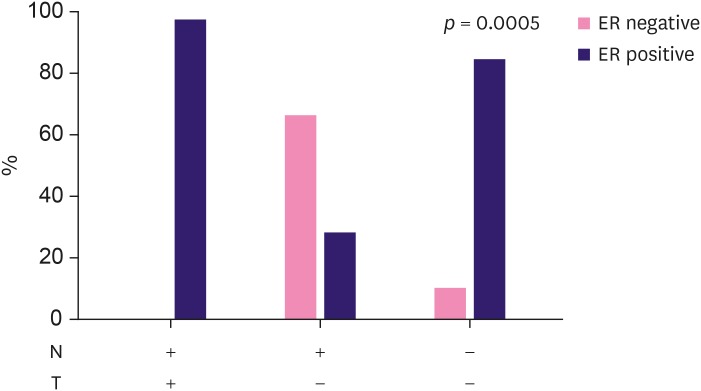
Figure 3 shows that in patients with blood type O, when the H antigen is absent in both tumor and adjacent normal tissue (23 out of 53), other than the cases of incompatible A antigen expression, the malignant cells expressed the estrogenic receptor in 86.95% (20/23) of cases. This association was statistically significant (p < 0.001). However, it was not significant in the case of the loss of expression of A and B antigens.
Figure 3. Distribution of H antigen expression profiles based on the status of ER in patients with blood group O.
ER = estrogen receptor.
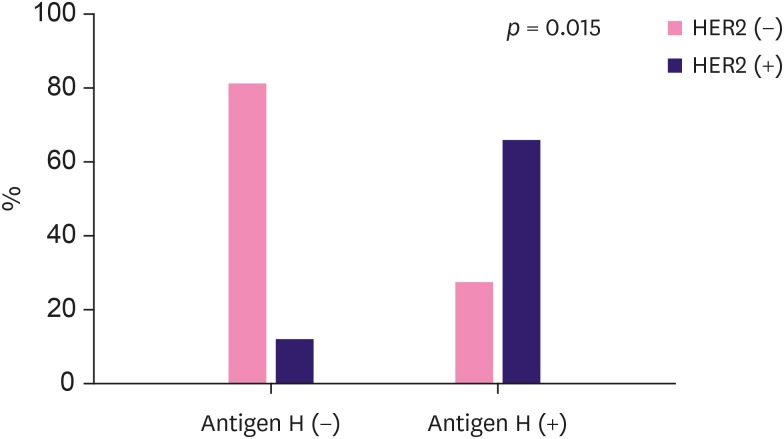
Expression of histo-blood group antigens and HER2 status
The patients with blood type B that expressed H antigen after loss of B antigen (13 out of 26 patients), showed overexpression of HER2 in 69.23% (9/13) of cases. This association is statistically significant (p < 0.05) (Figure 4). However, for blood types A and O, no association was observed regardless of the expression profile of A and H antigens and HER2 status. Our results show that there is no relationship between ABH profile and either tumor size and presence of lymph node metastasis.
Figure 4. Expression of antigen H in tumor and HER2 status among patients with blood group B.
HER2 = human epidermal growth factor receptor 2.
DISCUSSION
Our study is the first to show a loss of the ABH antigens in breast tumor and normal tissue adjacent to the tumor. Altered glycosylation is a hallmark of tumor cells in different types of cancers, particularly in breast cancer. Aberrant glycosylation can appear very early and occurs in carcinoma at an early stage and in lesions considered as non-malignant. Loss of expression of the ABH antigens, even in the adjacent tissues that surround the tumor and appear healthy, could suggest an early aberrant glycosylation preceding the appearance of tumor cells.
Aberrant expression of ABH antigen is associated with higher grade of breast tumor. The loss of ABH antigens was reported for the first time in cervical neoplasia [14]. Changes in ABH antigens has also been reported in several studies in colorectal, oral, bladder, and lung adenocarcinomas, and is associated with late-tumor stage, high risk, and poor prognosis [15]. Other studies have shown that ABH antigens are present in the distal colon in postnatal life and disappear after the 14th week. These antigens reappear in colorectal carcinoma and their expression is associated with poor prognosis [16]. Nevertheless, many researchers believe that there is no association between the expression of blood group antigens and the type or histological grade cancers [17,18]. The analysis of our results from the 109 patients shows the existence of a correlation between higher tumor grade and the loss of ABH antigens, although it is not statistically significant when the blood types A, B, and O are studied separately. This could be due to the relatively small sample size studied. It has been suggested that when acquisition of the cancerous phenotype is complete and the immune system becomes tolerant to the tumor cells, a loss of A and B antigens could facilitate metastasis by increasing cell motility [19]. Our study showed that the loss of A and B antigens correlates with the tumor expression of their fucosylated precursor H in the tumor. It is possible that the strong staining intensity, proportional to the increased number of H antigen sites, is due to the decrease or absence of glycosyltransferase A and B activity. The H substrate remains unsaturated and reveals binding sites to the antibody [20]. The high expression of H antigen in the tumor has been described in many studies as being related to angiogenic activity, aggressiveness of cancer cells, and an unfavorable prognosis for carcinomas [21]. Goupille et al. [22] suggested that α-(1, 2) fucosylation increases in vitro tumorigenicity of rat colon cancer cells. This tumorigenicity depends on the ability of cells expressing the H antigen to escape the immune control and is associated with resistance to apoptosis.
The consequence of the expression of the molecule H is linked to strong angiogenic activity and poor prognosis in breast carcinoma. Lin et al. [23] reported the co-expression of H antigen with CD44 and CD133, molecules known to initiate cancer and highly expressed in cases with poor prognosis. This hypothesis is supported by our results which showed that the expression of H antigen after loss of B determinant correlated with the overexpression of HER2; a transmembrane protein overexpressed in approximately 30% of metastatic breast cancers. The tumors overexpressing HER2 are associated with high rates of cell division, high grade, greater metastatic potential, and strong aggressiveness [24]. In contrast, when H antigen is absent, mammary tumor cells may be less aggressive. This is supported by our results which show a correlation between the disappearance of H antigen and expression of estrogen receptor in blood type O patients (p < 0.05). Breast carcinoma expressing the estrogen receptor has a good prognosis with a low proliferation index [25]. Furthermore, the loss of expression of the H antigen in 81.13% of the cases suggests that the protective effect of blood group O reported by the majority of studies, may be due to the disappearance of the H antigen.
Several mechanisms could be involved in the aberrant expression of the ABH antigens. The ABO glycosyltransferase gene becomes inactive due to hypermethylation of the promoter gene. Therefore, alterations, deletions, mutations or reading shifts that affect the catalytic site of the enzyme can lead to a decrease in its activity. Gao et al. [26] demonstrated that the loss of A/B antigens corresponds to the absence of glycosyltransferases A/B, which is due to an allelic loss and/or methylation, and the rate of methylation correlates directly with the degree of malignancy [7]. In addition, we have observed the incompatible expression of the A antigen in nearly 21% of patients with blood group O. These results are consistent with studies in different types of cancers such as colorectal and gastric carcinomas showing that 10% to 20%, respectively, of blood group O patients express antigen A in their cancer tissues [27]. For a long time, the A-like antigen was confused with Tn and Forssman antigens that are expressed differently in embryogenesis. Tn (GalNAcα1-O-Ser/Thr) is the most specific marker for human cancers and its expression correlates with poor prognosis [28]. The antigen Forssman (GalNAcα1-3GalNAcβ1-3Galα1-4Galβ1-4Glcβ1 1′ceramide) absent in most human individuals is one of glycolipids associated with cancer. The terminal residue (GalNAcα1-) of A antigen is present in both the Tn and Forssman antigen. Kapadia et al. [18] indicate that the aberrant expression of the antigen is not due to the presence of the Forssman antigen which could create a cross reaction with anti-A serum but due to the presence of the A-like epitope. This expression could be associated with carcinogenesis, since the terminal residue of these antigens is the same [29]. Also, Marionneau et al. [30] suggested that A antigen-positive carcinoma cells escape from immune surveillance at early stages of tumor progression.
To conclude, the pattern of loss of expression of ABH antigens in tumor and adjacent normal tissue correlated with the SBR histologic grading. Given the existing association between HER2 overexpression and H antigen, the latter could be related to HER2 overexpression in breast cancer. The loss of expression of A, B, and H antigens in the healthy adjacent tissue in many cases could indicate an aberrant glycosylation which precedes the appearance of tumor cells. However, further studies are needed to determine the role of incompatible A antigen in mammary carcinogenesis.
ACKNOWLEDGMENTS
We are extremely grateful to Prof. S. Zamiati who facilitated our access to the Department of Pathology and Prof. M. Matar who facilitated our access to the Maternity Ward L 9 C.H.U Ibn Rochd Casablanca. We thank the entire team of the Department of Pathology at C.H.U Ibn Rochd in Casablanca, especially Prof. S. Benayad, the residents, secretary, and technicians for their kind support and encouragement.
Footnotes
Conflicts of Interest: The authors declare that they have no competing interests.
- Conceptualization: Zouine S, Otmani N, Kojok K.
- Data curation: Zouine S.
- Formal analysis: Zouine S, Marnissi F, Zaid N.
- Funding acquisition: Zouine S.
- Investigation: Zouine S, Bennani Othmani M.
- Methodology: Zouine S, Marnissi F, Bennani Othmani M, Zaid N, Kojok K, Habti N.
- Resources: Marnissi F, Bennani Othmani M, Tahiri Jouti N, Habti N.
- Supervision: Tahiri Jouti N, Habti N, Zaid Y.
- Validation: Zouine S, Marnissi F, Otmani N, Zaid N, Tahiri Jouti N, Habti N, Zaid Y.
- Visualization: Zouine S, Otmani N, Tahiri Jouti N, Habti N, Zaid Y.
- Writing - original draft: Zouine S, Marnissi F, Otmani N, Zaid N, Kojok K, Tahiri Jouti N, Habti N, Zaid Y.
- Writing - review & editing: Marnissi F, Otmani N, Tahiri Jouti N, Habti N, Zaid Y.
References
- 1.Storry JR, Olsson ML. The ABO blood group system revisited: a review and update. Immunohematology. 2009;25:48–59. [PubMed] [Google Scholar]
- 2.Wang B, Akiyama K, Jia JT, Kimura H. Measuring H type 1 and H type 2 antigens in human saliva by immunoassay using artificial antigens as standard substances. Forensic Sci Int. 1994;67:1–8. doi: 10.1016/0379-0738(94)90405-7. [DOI] [PubMed] [Google Scholar]
- 3.Orntoft TF, Holmes EH, Johnson P, Hakomori S, Clausen H. Differential tissue expression of the Lewis blood group antigens: enzymatic, immunohistologic, and immunochemical evidence for Lewis a and b antigen expression in Le(a-b-) individuals. Blood. 1991;77:1389–1396. [PubMed] [Google Scholar]
- 4.Alfaro JA, Zheng RB, Persson M, Letts JA, Polakowski R, Bai Y, et al. ABO(H) blood group A and B glycosyltransferases recognize substrate via specific conformational changes. J Biol Chem. 2008;283:10097–10108. doi: 10.1074/jbc.M708669200. [DOI] [PubMed] [Google Scholar]
- 5.Ravn V, Dabelsteen E. Tissue distribution of histo-blood group antigens. APMIS. 2000;108:1–28. doi: 10.1034/j.1600-0463.2000.d01-1.x. [DOI] [PubMed] [Google Scholar]
- 6.Eastlund T. The histo-blood group ABO system and tissue transplantation. Transfusion. 1998;38:975–988. doi: 10.1046/j.1537-2995.1998.381098440863.x. [DOI] [PubMed] [Google Scholar]
- 7.Dabelsteen E, Gao S. ABO blood-group antigens in oral cancer. J Dent Res. 2005;84:21–28. doi: 10.1177/154405910508400103. [DOI] [PubMed] [Google Scholar]
- 8.Le Pendu J, Marionneau S, Cailleau-Thomas A, Rocher J, Le Moullac-Vaidye B, Clément M. ABH and Lewis histo-blood group antigens in cancer. APMIS. 2001;109:9–31. doi: 10.1111/j.1600-0463.2001.tb00011.x. [DOI] [PubMed] [Google Scholar]
- 9.Ichikawa D, Handa K, Hakomori S. Histo-blood group A/B antigen deletion/reduction vs. continuous expression in human tumor cells as correlated with their malignancy. Int J Cancer. 1998;76:284–289. doi: 10.1002/(sici)1097-0215(19980413)76:2<284::aid-ijc17>3.0.co;2-c. [DOI] [PubMed] [Google Scholar]
- 10.Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61:69–90. doi: 10.3322/caac.20107. [DOI] [PubMed] [Google Scholar]
- 11.El Fakir S, Najdi A, Khazraji YC, Bennani M, Belakhel L, Abousselham L, et al. Breast cancer screening in Morocco: performance indicators during two years of an organized programme. Asian Pac J Cancer Prev. 2015;16:6285–6288. doi: 10.7314/apjcp.2015.16.15.6285. [DOI] [PubMed] [Google Scholar]
- 12.Bloom HJ, Richardson WW. Histological grading and prognosis in breast cancer; a study of 1409 cases of which 359 have been followed for 15 years. Br J Cancer. 1957;11:359–377. doi: 10.1038/bjc.1957.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Penault-Llorca F, Balaton A, Sabourin JC, Le Doussal V. Immunochemistry evaluation of HER2 status in infiltration breast cancer: technical protocol and interpretation guidelines. Ann Pathol. 2002;22:150–157. [PubMed] [Google Scholar]
- 14.Davidsohn I, Kovarik S, Ni LY. Isoantigens A, B, and H in benign and malignant lesions of the cervix. Arch Pathol. 1969;87:306–314. [PubMed] [Google Scholar]
- 15.Orntoft TF, Hvid H, Clausen H, Hakomori S, Dabelsteen E. Loss of blood group ABO-related antigen expression in urothelium from patients with chronic cystitis. Lab Invest. 1989;60:305–310. [PubMed] [Google Scholar]
- 16.Nakagoe T, Fukushima K, Hirota M, Kusano H, Ayabe H, Tomita M, et al. An immunohistochemical study of the distribution of blood group substances and related antigens in primary colorectal carcinomas and metastatic lymph node and liver lesions, using monoclonal antibodies against A, B, H type 2, Le(a), and Le(x) antigens. J Gastroenterol. 1994;29:265–275. doi: 10.1007/BF02358364. [DOI] [PubMed] [Google Scholar]
- 17.Kay HE, Wallace DM. A and B antigens of tumors arising from urinary epithelium. J Natl Cancer Inst. 1961;26:1349–1365. [PubMed] [Google Scholar]
- 18.Kapadia A, Feizi T, Jewell D, Keeling J, Slavin G. Immunocytochemical studies of blood group A, H, I, and i antigens in gastric mucosae of infants with normal gastric histology and of patients with gastric carcinoma and chronic benign peptic ulceration. J Clin Pathol. 1981;34:320–337. doi: 10.1136/jcp.34.3.320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ichikawa D, Handa K, Withers DA, Hakomori S. Histo-blood group A/B versus H status of human carcinoma cells as correlated with haptotactic cell motility: approach with A and B gene transfection. Cancer Res. 1997;57:3092–3096. [PubMed] [Google Scholar]
- 20.Dabelsteen E, Vedtofte P, Hakomori S, Young WW., Jr Accumulation of a blood group antigen precursor in oral premalignant lesions. Cancer Res. 1983;43:1451–1454. [PubMed] [Google Scholar]
- 21.Halloran MM, Carley WW, Polverini PJ, Haskell CJ, Phan S, Anderson BJ, et al. Ley/H: an endothelial-selective, cytokine-inducible, angiogenic mediator. J Immunol. 2000;164:4868–4877. doi: 10.4049/jimmunol.164.9.4868. [DOI] [PubMed] [Google Scholar]
- 22.Goupille C, Marionneau S, Bureau V, Hallouin F, Meichenin M, Rocher J, et al. α1,2Fucosyltransferase increases resistance to apoptosis of rat colon carcinoma cells. Glycobiology. 2000;10:375–382. doi: 10.1093/glycob/10.4.375. [DOI] [PubMed] [Google Scholar]
- 23.Lin WM, Karsten U, Goletz S, Cheng RC, Cao Y. Co-expression of CD173 (H2) and CD174 (Lewis Y) with CD44 suggests that fucosylated histo-blood group antigens are markers of breast cancer-initiating cells. Virchows Arch. 2010;456:403–409. doi: 10.1007/s00428-010-0897-5. [DOI] [PubMed] [Google Scholar]
- 24.Ross JS, Fletcher JA. The HER-2/neu oncogene in breast cancer: prognostic factor, predictive factor, and target for therapy. Stem Cells. 1998;16:413–428. doi: 10.1002/stem.160413. [DOI] [PubMed] [Google Scholar]
- 25.Carey LA, Perou CM, Livasy CA, Dressler LG, Cowan D, Conway K, et al. Race, breast cancer subtypes, and survival in the Carolina Breast Cancer Study. JAMA. 2006;295:2492–2502. doi: 10.1001/jama.295.21.2492. [DOI] [PubMed] [Google Scholar]
- 26.Gao S, Worm J, Guldberg P, Eiberg H, Krogdahl A, Liu CJ, et al. Genetic and epigenetic alterations of the blood group ABO gene in oral squamous cell carcinoma. Int J Cancer. 2004;109:230–237. doi: 10.1002/ijc.11592. [DOI] [PubMed] [Google Scholar]
- 27.Hirohashi S, Clausen H, Yamada T, Shimosato Y, Hakomori S. Blood group A cross-reacting epitope defined by monoclonal antibodies NCC-LU-35 and -81 expressed in cancer of blood group O or B individuals: its identification as Tn antigen. Proc Natl Acad Sci U S A. 1985;82:7039–7043. doi: 10.1073/pnas.82.20.7039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kawaguchi T, Takazawa H, Imai S, Morimoto J, Watanabe T, Kanno M, et al. Expression of Vicia villosa agglutinin (VVA)-binding glycoprotein in primary breast cancer cells in relation to lymphatic metastasis: is atypical MUC1 bearing Tn antigen a receptor of VVA? Breast Cancer Res Treat. 2006;98:31–43. doi: 10.1007/s10549-005-9115-6. [DOI] [PubMed] [Google Scholar]
- 29.Nakagoe T, Fukushima K, Nanashima A, Sawai T, Tsuji T, Jibiki MA, et al. Comparison of the expression of ABH/Lewis-related antigens in polypoid and non-polypoid growth types of colorectal carcinoma. J Gastroenterol Hepatol. 2001;16:176–183. doi: 10.1046/j.1440-1746.2001.02425.x. [DOI] [PubMed] [Google Scholar]
- 30.Marionneau S, Le Moullac-Vaidye B, Le Pendu J. Expression of histo-blood group A antigen increases resistance to apoptosis and facilitates escape from immune control of rat colon carcinoma cells. Glycobiology. 2002;12:851–856. doi: 10.1093/glycob/cwf103. [DOI] [PubMed] [Google Scholar]