Abstract
Purpose
Tau is a microtubule-associated protein that can be found in both normal and abnormal breast cells. Whether the expression of Tau protein can predict the response to neoadjuvant chemotherapy (NACT) is still unclear. In this study, we assessed the role of Tau protein expression in predicting a pathological complete response (pCR) to NACT for different subtypes of breast cancer.
Methods
Four hundred and sixty-eight eligible patients were retrospectively recruited in our study. The relationship between clinicopathologic factors, including Tau protein expression, and pCR in different subtypes was evaluated using logistic regression analysis. Correlation between Tau and disease-free survival (DFS) and overall survival (OS) was performed using Kaplan–Meier analysis.
Results
The expression of Tau protein was negatively correlated with pCR, especially in triple-negative breast cancer (TNBC). No significant difference was observed in the luminal human epidermal growth factor receptor-2 (HER2)-negative subtype and HER2-positive subtype. Patients with pCR were associated with better DFS and OS (p < 0.05). However, Tau protein expression had no association with either DFS or OS (p > 0.05).
Conclusion
Tau protein expression can predict pCR before NACT in TNBC, but there was no correlation between Tau expression and DFS or OS.
Keywords: Neoadjuvant therapy, Survival, Tau proteins, Triple negative breast neoplasms
INTRODUCTION
Breast cancer is the malignancy with the highest incidence in women and cancer-related death due to breast carcinoma was second only to lung cancer among American women [1]. Neoadjuvant chemotherapy (NACT) has been considered a vital option for breast cancer treatment [2]. There are 4 known benefits of neoadjuvant systemic therapy, i.e., reducing the clinical stage of breast cancer, decreasing the extent of surgery, eradicating micrometastatic disease, and predicting chemotherapeutic sensitivity [3,4]. A pathological complete response (pCR) after neoadjuvant therapy was proven to be a predictive indicator for favorable disease-free survival (DFS) and overall survival (OS) [5] and was considered the primary endpoint for most clinical trials [6,7,8]. Selecting appropriate indicators to predict pCR is a current hot topic in research.
Taxane has been widely used in both neoadjuvant and adjuvant chemotherapeutic regimens. Taxane targets the microtubule and control spindle microtubule dynamics, which may result in cell cycle arrest in the G2/M phase and apoptosis in cancer cells [9,10]. Tau is a microtubule-associated protein (MAP) found in both normal and abnormal breast cells. It can maintain the stability of the microtubule by facilitating the assembly of microtubules and binds to the same point of beta-tubulin as taxane [11], leading to potential taxane-resistance with high levels of Tau expression. Previous studies have indicated that expression of Tau protein is associated with the reaction to neoadjuvant taxane-containing chemotherapy [4,12,13]. Some earlier articles reported low Tau expression is associated with a higher pCR rate [12,13], while others found that Tau expression could not predict the response to neoadjuvant therapy [14,15]. The correlation between Tau protein expression and response to NACT remains unclear and there are currently no studies that have explored the relationship between Tau protein expression and different subtypes of breast cancer.
This study aimed to retrospectively explore whether Tau protein expression can predict pCR before receiving neoadjuvant therapy and survival in different subtypes of breast cancer.
METHODS
Patients
This retrospective study was approved by the Ethics Committee of our hospital (No. GDREC2012058H[R3]) and was performed in accordance with the principles of the Declaration of Helsinki. The requirement for informed consent was waived. The inclusion criteria were as follows: 1) the patients underwent core-needle biopsy and were diagnosed with invasive breast carcinoma before neoadjuvant therapy; 2) the patients underwent surgery after receiving NACT and the final pathological results were available; and 3) the patients received neoadjuvant therapy and no treatment before neoadjuvant therapy (including chemotherapy, endocrine therapy, and radiotherapy). The exclusion criteria were as follows: 1) patients with distant metastatic breast cancer and 2) patients with other tumors that were found before treatment. Four hundred and sixty-eight female patients with breast carcinoma who received NACT between February 2009 and December 2018 were included in the analysis.
NACT regimen
All patients received a NACT regimen; 446 patients were administered a taxane-based regimen and 70 patients were administered an anthracycline-based regimen (among them, 57 patients had chemotherapy regimens that included taxane and anthracycline). Detailed descriptions of the NACT regimens are as follows: 1) only taxane-containing regimen: 225 patients received the TCb chemotherapeutic regimen (75 mg/m2 docetaxel and carboplatin with an area under the curve of 6, every 3 weeks); 124 patients received the TC chemotherapeutic regimen (75 mg/m2 docetaxel and 600 mg/m2 cyclophosphamide every, 3 weeks); 40 patients received the TX chemotherapeutic regimen (75 mg/m2 docetaxel every 3 weeks and 1,250 mg/m2 capecitabine twice, on day 1 to day 14, every 3 weeks); 2) only anthracycline-contained regimen: 13 patients received the FEC regimen (100 mg/m2 epirubicin, cyclophosphamide 500 mg/m2, and 5-fluorouracil 500 mg/m2, every 3 weeks); 3) chemotherapy regimens that contain both taxane and anthracycline: 49 patients received the EC followed by T regimen (90 mg/m2 epirubicin and 600 mg/m2 cyclophosphamide every 3 weeks for 4 cycles, followed by a 4-cycle period of 100 mg/m2 docetaxel every 3 weeks); 8 patients received the TAC regimen (500 mg/m2 cyclophosphamide, 75 mg/m2, docetaxel and 100 mg/m2, epirubicin, every 3 weeks); and 4) other regimens (i.e., a chemotherapy regimen that contains neither taxane nor anthracycline) were administered to 9 patients. Among 193 patients who had human epidermal growth factor receptor-2 (HER2)-positive breast cancer, 165 patients used trastuzumab for targeted therapy (loading dose, 8 mg/kg; maintenance dose, 6 mg/kg).
Pathological examination and response evaluation
Through nuclear staining of the estrogen receptor (ER) and progesterone receptor (PR), the cut-off values for ER and PR were set at 1%; immunohistochemistry (IHC) staining of cancer cells < 1% was considered ER/PR negative and ≥ 1% was considered ER/PR positive. We regarded nuclear staining < 20% of tumor cells as Ki-67 negative and ≥ 20% as Ki-67 positive [16]. Further, cancer cells with IHC 0 and 1+ were regarded as HER2 negative and cancer cells with IHC 3+ were regarded as HER2 positive. If cancer cells were IHC 2+, further validation was performed with in situ hybridization (ISH) testing, and ISH amplified outcomes were regarded as HER2 positive.
Tau protein expression in normal breast epithelium cells was defined as the control and reference for scoring. Tumor cells that received no Tau expression were considered as score 0; lower expression than normal breast cells was considered IHC 1+; similar expression to normal breast epithelium was considered IHC 2+; higher expression than normal breast cells was considered IHC 3+. IHC 0 and 1+ were regarded as Tau expression negative and IHC 2+ and 3+ were regarded as Tau expression positive [17]. The pathological results were examined by 2 breast pathologists (with at least 10 years of breast pathological experience); discrepancies were discussed with a third breast pathologist and the final results were decided upon consensus.
pCR (ypT0N0 or ypTisN0) was considered as eradication of residual invasive carcinoma in both breast and lymph node [18,19].
Data and statistical analysis
The χ2 tests and Fisher's exact test were utilized to compare the relationship of Tau and other clinical characteristics. Logistic regression analysis was utilized to consider the relationship of ER, PR, HER2, Ki-67, and Tau status to response probability. Statistical significance was set at 0.05. DFS and OS were used as survival endpoints in this survey and were analyzed using the Kaplan–Meier method. DFS was considered as the time from confirming breast cancer to either recurrence, metastasis, or death from other diseases before recurrence or metastasis. OS was defined as the times between confirming breast cancer to any cause of death. The log-rank test was utilized to assess the hazard ratio (HR) and 95% confidence intervals for DFS and OS. Statistical analysis was performed using SPSS software (version 22; SPSS Inc., Chicago, USA).
RESULTS
Patients and Tau expression
Four hundred and sixty-eight patients with NACT and pathological findings of Tau expression were recruited in our study. Table 1 shows the relationship of Tau protein expression with clinical-pathological parameters. Two-hundred and eighty (59.8%) tumors had positive Tau protein expression, 188 (40.2%) tumors had negative Tau protein expression; 191 (40.8%) were luminal HER2-negative breast cancer, 193 (41.2%) were HER2-positive tumor, and 84 (18.0%) were triple-negative breast cancer (TNBC). Based on the AJCC Cancer Staging Manual (8th edition) [20], 85 (18.2%) patients had stage I tumors, 309 (66.0%) patients had stage II tumors, and 74 (15.8%) patients had stage III tumors. The mean age was 48.9 ± 9.9 years (range 19 to 74 years old). For breast surgery treatment after NACT, 163 (34.8%) patients underwent breast-conserving surgery.
Table 1. Baseline patient demographics and clinical characteristics (n = 468).
| Characteristics | Values | |
|---|---|---|
| Age (yr) | 48.9 ± 9.9 | |
| BMI | 23.5 ± 3.3 | |
| Menopausal state | ||
| Premenopausal | 229 (48.9) | |
| Postmenopausal | 239 (51.1) | |
| Clinical stage* | ||
| I | 85 (18.2) | |
| II | 309 (66.0) | |
| III | 74 (15.8) | |
| Tumor type | ||
| Ductal carcinoma | 443 (94.7) | |
| Lobular carcinoma | 10 (2.1) | |
| Other | 15 (3.2) | |
| Molecular subtype | ||
| Luminal HER2-negative | 191 (40.8) | |
| HER2-positive | 193 (41.2) | |
| TNBC | 84 (18.0) | |
| Pathological complete response | ||
| No | 278 (59.4) | |
| Yes | 190 (40.6) | |
| Breast surgery | ||
| Breast-conserving surgery | 163 (34.8) | |
| Mastectomy | 305 (65.2) | |
Data are shown as mean ± standard deviation or number (%).
BMI = body mass index; HER2 = human epidermal growth factor receptor-2; TNBC = triple-negative breast cancer.
*Based on the 8th AJCC staging system.
Tau expression and pCR
Tau protein level was an indicator of response to NACT; 190 (40.6%) patients had a pCR after receiving neoadjuvant therapy. Of these, 92 (32.9%) of 280 patients achieved a pCR in the Tau-positive group; 98 (52.1%) of 188 patients achieved a pCR in the Tau-negative group. Compared to that in the Tau-positive patients (92 [32.9%] of 280), Tau-negative patients (98 [52.1%] of 188) had a higher pCR rate after NACT (p < 0.001, Table 2). The percentage of Tau-negative tumors was higher in the TNBC (59 [70.2%] of 84) and HER2-positive breast cancer (82 [42.5%] of 193) groups than in luminal-HER2-negative breast cancer (47 [24.6%] of 191, p < 0.001, Table 2).
Table 2. Correlation between protein-Tau status and clinicopathological characteristics of neoadjuvant chemotherapeutic breast cancer patients.
| Characteristics | No. of patients | Tau-positive | Tau-negative | p-value | |
|---|---|---|---|---|---|
| Tumor stage* | 0.299 | ||||
| cT1 | 93 | 51 (54.8) | 42 (45.2) | ||
| cT2 | 311 | 185 (59.5) | 126 (40.5) | ||
| cT3 | 47 | 31 (66.0) | 16 (34.0) | ||
| cT4 | 17 | 13 (76.5) | 4 (23.5) | ||
| Clinical stage† | 0.709 | ||||
| I | 85 | 49 (57.6) | 36 (42.4) | ||
| II | 309 | 189 (61.2) | 120 (38.8) | ||
| III | 74 | 42 (56.8) | 32 (43.2) | ||
| Tumor type | 0.421 | ||||
| Ductal | 443 | 263 (59.4) | 180 (40.6) | ||
| Lobular | 10 | 8 (80.0) | 2 (20.0) | ||
| Other | 15 | 9 (60.0) | 6 (40.0) | ||
| Molecular subtype | < 0.001 | ||||
| Luminal-HER2(−) breast | 191 | 144 (75.4) | 47 (24.6) | ||
| HER2-positive | 193 | 111 (57.5) | 82 (42.5) | ||
| TNBC | 84 | 25 (29.8) | 59 (70.2) | ||
| pCR | < 0.001 | ||||
| No | 278 | 188 (67.6) | 90 (32.4) | ||
| Yes | 190 | 92 (48.4) | 98 (51.6) | ||
| ER | < 0.001 | ||||
| Negative | 165 | 64 (38.8) | 101 (61.2) | ||
| Positive | 303 | 216 (71.3) | 87 (28.7) | ||
| PR | < 0.001 | ||||
| Negative | 144 | 58 (40.3) | 86 (59.7) | ||
| Positive | 324 | 222 (68.5) | 102 (31.5) | ||
| HER2 | 0.392 | ||||
| Negative | 275 | 169 (61.5) | 106 (38.5) | ||
| Positive | 193 | 111 (57.5) | 82 (42.5) | ||
| Ki67 | 0.117 | ||||
| Low | 64 | 44 (68.8) | 20 (31.3) | ||
| High | 404 | 236 (58.4) | 168 (41.6) | ||
Data are shown as number (%).
pCR = pathological complete response; ER = estrogen receptor; PR = progesterone receptor; HER2 = human epidermal growth factor receptor 2.
*Inflammatory breast cancer was not included; †Based on the 8th AJCC staging system.
Analysis identified ER, PR, HER2, and Tau as significantly related to pCR after NACT (Table 3). In multivariate analysis, ER, HER2, and Tau status were found as independent predictors of pCR. Among patients with high Tau-positive expression, the odds of pCR achievement were lower in the Tau 2+ and Tau 3+ subset patients compared to the no Tau expression subset patients, respectively (odds ratio [OR] = 0.392, p = 0.014; OR = 0.312, p = 0.003, respectively). With the decline of Tau protein expression, the pCR rate was further increased in the Tau-positive group (Table 4).
Table 3. Correlation between pCR subset and pathological characteristics.
| Characteristics | No. of patients | pCR | Non-pCR | p-value | |
|---|---|---|---|---|---|
| ER | < 0.001 | ||||
| Negative | 165 | 104 (63.0) | 61 (37.0) | ||
| Positive | 303 | 86 (28.4) | 217 (71.6) | ||
| PR | < 0.001 | ||||
| Negative | 144 | 82 (56.9) | 62 (43.1) | ||
| Positive | 324 | 108 (33.3) | 216 (66.7) | ||
| HER2 | < 0.001 | ||||
| Negative | 275 | 74 (26.9) | 201 (73.1) | ||
| Positive | 193 | 116 (60.1) | 77 (39.9) | ||
| Ki67 | 0.414 | ||||
| Low | 64 | 23 (35.9) | 41 (64.1) | ||
| High | 404 | 167 (41.3) | 237 (58.7) | ||
| Tau | < 0.001 | ||||
| Negative | 188 | 98 (52.1) | 90 (47.9) | ||
| Positive | 280 | 92 (32.9) | 188 (67.1) | ||
Data are shown as number (%).
pCR = pathological complete response; ER = estrogen receptor; PR = progesterone receptor; HER2 = human epidermal growth factor receptor 2.
Table 4. Multivariate logistic regression analysis for pCR.
| Factors | OR (95% CI) | p-value | |
|---|---|---|---|
| ER | 0.232 (0.155–0.348) | < 0.001 | |
| PR | 0.673 (0.352–1.284) | 0.229 | |
| HER2 | 4.508 (2.944–6.903) | < 0.001 | |
| Tau | |||
| 0 | Reference | ||
| 1+ | 0.618 (0.309–1.236) | 0.174 | |
| 2+ | 0.392 (0.186–0.824) | 0.014 | |
| 3+ | 0.312 (0.145–0.667) | 0.003 | |
pCR = pathological complete response; OR = odds ratio; CI = confidence interval; ER = estrogen receptor; PR = progesterone receptor; HER2 = human epidermal growth factor receptor 2.
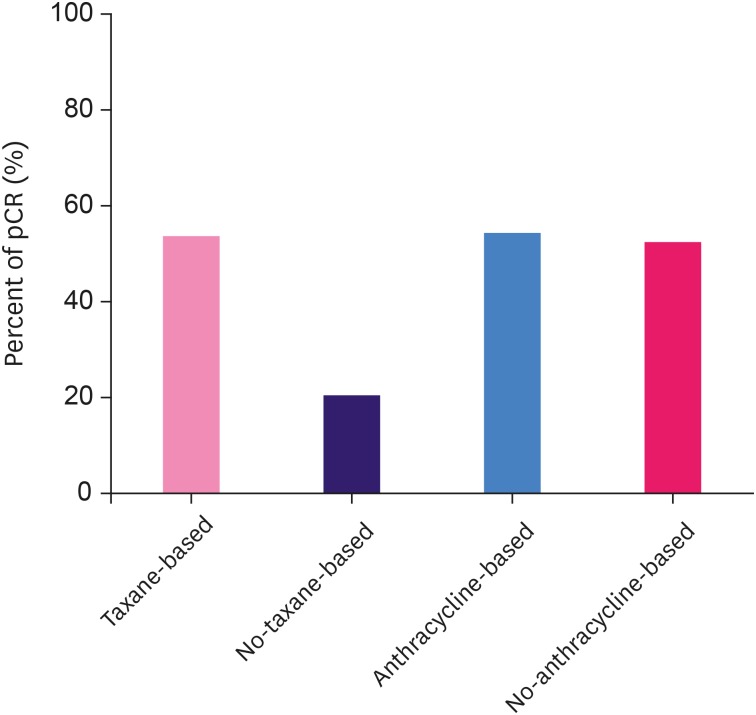
For Tau-positive breast cancers, the pCR rate was 33.5% and 23.5% in the taxane-based group and non-taxane-based group, respectively; the pCR rate was 38.6% and 31.8% in the anthracycline-based group and non-anthracycline-based group, respectively. For Tau-negative breast cancers, the pCR rate of the taxane-based group was numerically twice as high as the non-taxane-based group (53.0% [97/183] and 20.0% [1/5], respectively); however, the pCR rates were similar in the anthracycline-based group and non-anthracycline-based group (53.8% [14/26] and 51.9% [84/162] for Tau-negative breast cancers; Figure 1).
Figure 1. pCR rate of different chemotherapy regimens in Tau-negative groups.
pCR = pathological complete response.
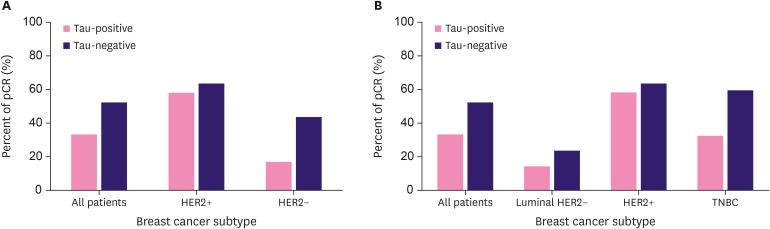
pCR rates in patients with different Tau protein levels among different molecular subtypes
When all patients were divided into 3 molecular subtypes; in patients with the HER2-positive subtype, pCR was achieved in 64 (57.7%) of 111 patients with Tau-positive protein and 52 (63.4%) of 82 with Tau-negative protein. In patients with the HER2-negative subtype, pCR was achieved in 28 (16.6%) of 169 patients with Tau-positive protein and 46 (43.4%) of 106 with Tau-negative protein (p < 0.001 for HER2-negative breast cancer, Table 5 and Figure 2A).
Table 5. The rate of pCR in different protein-Tau group with the 2 different molecular subtypes.
| Factors | pCR rate in Tau+ patients | pCR rate in Tau− patients | p-value |
|---|---|---|---|
| All patients (n = 468) | 92/280 (32.9) | 98/188 (52.1) | < 0.001 |
| HER2-negative (n = 275) | 28/169 (16.6) | 46/106 (43.4) | < 0.001 |
| HER2-positive (n = 193) | 64/111 (57.7) | 52/82 (63.4) | 0.419 |
Data are shown as number (%).
pCR = pathological complete response; HER2= human epidermal growth factor receptor 2.
Figure 2. pCR rates in patients with different Tau protein levels among different molecular subtypes. (A) All patients were divided into 2 molecular subtypes. (B) All patients were divided into 3 molecular subtypes. p-values are from the χ2 test for trend. pCR is defined as ypT0N0 or ypTisN0.
pCR = pathological complete response; HER2 = human epidermal growth factor receptor 2; TNBC = triple-negative breast cancer.
When all patients were classified into 3 molecular subtypes, in patients with the luminal HER2-negative breast carcinoma, pCR was achieved in 20 (13.9%) of 144 patients with Tau-positive protein and 11 (23.4%) of 47 with Tau-negative protein. In patients with the HER2-positive breast carcinoma, pCR was achieved in 64 (57.7%) of 111 patients with Tau-positive protein and 52 (63.4%) of 82 with Tau-negative protein. In patients with TNBC breast carcinoma, pCR was achieved in 8 (32.0%) of 25 patients with Tau-positive protein and 35 (59.3%) of 59 with Tau-negative protein (p = 0.022 for TNBC; Table 6 and Figure 2B).
Table 6. The rate of pCR in different protein-Tau group with the 3 different molecular subtypes.
| Factors | pCR rate in Tau+ patients | pCR rate in Tau− patients | p-value |
|---|---|---|---|
| All patients (n = 468) | 92/280 (32.9) | 98/188 (52.1) | < 0.001 |
| Luminal HER2-negative (n = 191) | 20/144 (13.9) | 11/47 (23.4) | 0.125 |
| HER2-positive (n = 193) | 64/111 (57.7) | 52/82 (63.4) | 0.419 |
| TNBC (n = 84) | 8/25 (32.0) | 35/59 (59.3) | 0.022 |
Data are shown as number (%).
pCR = pathological complete response; HER2 = human epidermal growth factor receptor 2; TNBC = triple-negative breast cancer.
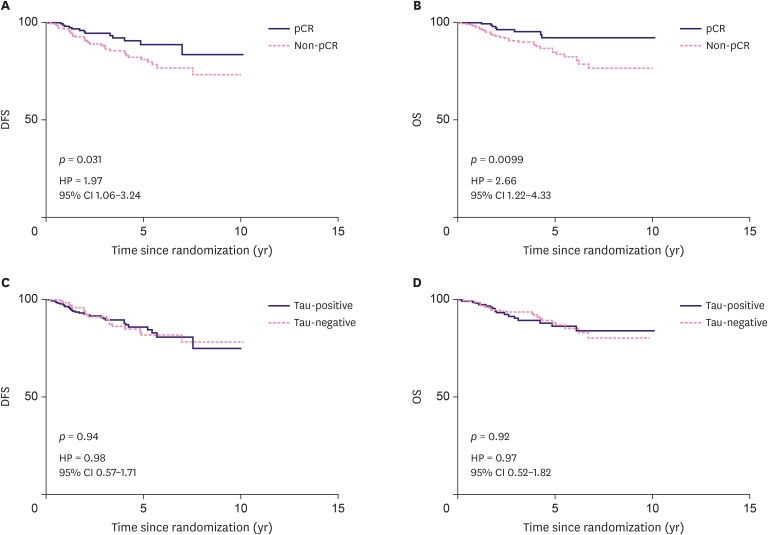
Survival and Tau expression
The median follow-up for DFS in our study was 3 years. Fifty-one patients experienced recurrence and metastasis and 40 patients died; the median DFS and OS were not reached. There was a positive association between pCR and DFS (HR = 1.97, p = 0.03, Figure 3A) and OS (HR = 2.66, p = 0.01, Figure 3B). However, the DFS and OS were not statistically different between different Tau expression levels (HR = 0.98, p = 0.94, Figure 3C; HR = 0.97, p = 0.92, Figure 3D, respectively). Regarding different NACT regimens, in Tau-positive tumors, no significant interaction was found in DFS and OS between taxane-based and non-taxane-based groups; a similar result was found for Tau-negative tumors.
Figure 3. Kaplan–Meier analysis for prognosis of different patients. (A) Associations between pCR and DFS. (B) Associations between pCR and OS. (C) Associations between Tau protein expression and DFS. (D) Associations between Tau protein expression and OS. p-values were derived from a log-rank test. HR and 95% CI were derived from univariate Cox-regression.
CI = confidence interval; HR = hazard ratio; DFS = disease-free survival; OS = overall survival; pCR = pathological complete response.
DISCUSSION
Patients who achieved a pCR after neoadjuvant therapy have a better prognosis than those had residual invasive cancer in all molecular subtypes of breast cancer [5,21]. Finding proper biomarkers that can predict pCR before NACT is a priority. Tau protein is a MAP that can be found both in normal and cancer cells. Opinions differ as to whether Tau expression can predict the pCR in clinical therapy.
The aim of our study was to analyze the correlation between Tau protein status, pCR, and survival. The present study retrospectively analyzed 468 patients with breast cancer who received neoadjuvant therapy before surgery. The expression of Tau protein was assessed in all patients. In our study, both univariate and multivariate logistic regression suggested that Tau protein expression is a predictive indicator of pCR. We found a negative correlation of decreased Tau expression with increased pCR, especially in the TNBC subtype. In the multivariate regression analysis, it is worth noting that no difference was found in the pCR rate of the Tau 1+ group and Tau-0 group; and in patients with Tau-2+ and -3+, the pCR rate decreased with increasing Tau expression. Tau protein status was positively related with ER and PR. The pCR related to better survival prognosis, but no significant difference was found in survival between the Tau-positive and Tau-negative groups.
As the responses to neoadjuvant therapy vary between different molecular subtypes [22], how to use biomarkers to predict pCR efficiently is still a hot research topic at present. Based on previously published findings, the predictive value of Tau protein status for pCR remains ambiguous. The study of Rody et al., [14] analyzing 50 patients who received NACT, demonstrated that there was non-significant relationship between Tau status and response to NACT; other studies have reached similar conclusions [12,23,24]. However, Andre et al. [4] analyzed 82 patients treated with NACT and found Tau expression was an independent predictor of pCR. Another study also suggested that Tau is a new molecular marker for predicting pCR in NACT and low Tau status is associated with higher sensitivity, both in messenger RNA expression and IHC [13,25,26]. There is still no consensus as to whether Tau expression can be an indicator for pCR before NACT. In our study, 92 (32.9%) of 280 patients in the Tau-positive group and 98 (52.1%) of 188 patients in the Tau-negative group achieved pCR after neoadjuvant therapy. The χ2 test demonstrated that the difference was significant. Furthermore, the multivariate analysis showed that with the decline of Tau protein expression, the pCR rate was further increased in the Tau-positive group (Tau 2+ and Tau 3+). Our findings are consistent with the idea that Tau protein expression is a predictive biomarker to predict NACT response. After further analysis of the different molecular subtypes, the correlation between pCR rate and Tau protein expression is significantly different only for TNBC. There was no specific analysis of the association between Tau protein and NACT efficacy for different molecular subtypes. Our study proved that Tau protein has particular implications for predicting neoadjuvant therapy, especially in TNBC.
Since neoadjuvant therapy has become a common approach for the treatment of patients with TNBC and previous studies have proven that patients with pCR have a much better prognosis than those who have residual invasive carcinoma after neoadjuvant therapy [27,28], it is clearly advantageous to predict the pCR rate in patients with TNBC. Previously, the value of Tau protein expression for predicting the pCR rate of neoadjuvant therapy in different subtypes has rarely been investigated and studied. Our study confirmed that Tau expression could predict pCR and deeply explored the different roles of Tau expression in different molecular subtypes. It was found that Tau expression is an independent indicator of pCR in TNBC but has no predictive value in luminal HER2-negative or HER2-positive patients. In the pooled analysis of Collaborative Trials in Neoadjuvant Breast Cancer [5], patients with luminal HER2-negative breast cancer were insensitive to neoadjuvant therapy and achieved a relatively lower pCR rate of 7.5%; patients with HER2-positive breast cancer obtained a higher pCR because of targeted therapy; and patients with TNBC were sensitive to neoadjuvant therapy and achieved a relatively higher pCR rate of 33.6%, which may explain why Tau expression can be used to predict the pCR rate in TNBC.
Rouzier et al. [12] performed a small interfering RNA experiment to explore whether Tau affects the sensitivity of taxane and anthracycline in vitro. Their results showed that downregulation of Tau increased the sensitivity to taxane but did not influence the susceptibility to anthracycline. The study by Pusztai et al. [17] incorporated 1,942 patients from NSABP B-28 and showed that in ER-positive and ER-negative groups, Tau-positive patients could not benefit from taxane-based therapeutic regimen. In the present study, the pCR rate of the taxane-based group was numerically twice as high as the non-taxane-based group, the difference was statistically significant for Tau-negative breast cancers in the taxane-based group. The reason may be that taxane is the cornerstone of neoadjuvant and adjuvant chemotherapy and only 23 patients were given non-taxane-based NACT in our study. There are differences between in vitro and clinical studies. Furthermore, bias might exist when analyzing pCR differences between variant chemo-regimen groups, since the majority (95.1%) of patients received taxane-based regimen. More clinical trials should be conducted to verify the relationship between Tau expression and taxane-based chemotherapy regimen.
pCR after NACT is related to excellent survival [5]. Our research also demonstrated this opinion. Patients with pCR had a better DFS and OS than non-pCR patients. The analysis of Pusztai et al. [17] also showed that Tau-negative status was related to poor survival, especially in ER-positive patients. In our study, DFS and OS demonstrated no difference between Tau-positive and Tau-negative patients. We concluded that this result was probably related to the relatively small number of patients in this study. More patients or multi-center data can be included to discuss this issue in the future.
We still have some expectations for our study. First, the present study was a retrospective study and incorporated a relatively small number of patients. Second, the expression of Tau-protein may differ between different countries or races. The patients in our study are all from China, which probably produced a sampling bias. The predictive value of Tau needs to be verified by further multi-center and prospective studies.
In conclusion, our present study indicated that Tau protein expression might be a predictive indicator for NACT, especially in TNBC. The baseline status of Tau protein is a useful indicator for selecting individuals who might achieve pCR and can be added into other predictive models to increase their predictive value. However, the complicated relationship between Tau-expression and other molecular makers needs to be demonstrated in further studies. Eventually, these results will help clinicians to make individual accurate treatment decisions for patients.
ACKNOWLEDGMENTS
We thank all the patients for their participation and contribution.
Footnotes
Funding: This study was supported by National Natural Science Foundation of China (81871513), Natural Science Foundation of Guangdong Province (2017A030313882), Guangdong Medical Science and Technology Research Fund (A2019494, A2019252) and The Doctor Launch Fund of Guangdong Provincial People's Hospital (2018bq04).
Conflict of Interest: The authors declare that they have no competing interests.
- Conceptualization: Lei C.
- Data curation: Lei C, Xia B, Ji F, Zhang Y, Xiong Q, Lin Y, Zhuang X, Zhang L, Cheng M, Yang M.
- Formal analysis: Lei C, Yang C, Ji F, Zhang Y, Lin Y, Zhuang X, Zhang L, Zhu T, Yang M.
- Funding acquisition: Yang C, Ji F.
- Investigation: Gao H, Zhuang X, Cheng M.
- Methodology: Zhang Y, Gao H.
- Project administration: Gao H, Zhu T.
- Resources: Yang C, Xiong Q.
- Software: Xia B, Zhu T.
- Supervision: Wang K.
- Validation: Yang C, Xia B, Zhang L, Wang K.
- Visualization: Yang C, Xia B.
- Writing - original draft: Lei C, Xia B.
- Writing - review & editing: Lei C, Wang K.
References
- 1.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018. CA Cancer J Clin. 2018;68:7–30. doi: 10.3322/caac.21442. [DOI] [PubMed] [Google Scholar]
- 2.Gradishar WJ, Anderson BO, Balassanian R, Blair SL, Burstein HJ, Cyr A, et al. Breast cancer, version 4.2017, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2018;16:310–320. doi: 10.6004/jnccn.2018.0012. [DOI] [PubMed] [Google Scholar]
- 3.Kaufmann M, von Minckwitz G, Bear HD, Buzdar A, McGale P, Bonnefoi H, et al. Recommendations from an international expert panel on the use of neoadjuvant (primary) systemic treatment of operable breast cancer: new perspectives 2006. Ann Oncol. 2007;18:1927–1934. doi: 10.1093/annonc/mdm201. [DOI] [PubMed] [Google Scholar]
- 4.Andre F, Hatzis C, Anderson K, Sotiriou C, Mazouni C, Mejia J, et al. Microtubule-associated protein-tau is a bifunctional predictor of endocrine sensitivity and chemotherapy resistance in estrogen receptor-positive breast cancer. Clin Cancer Res. 2007;13:2061–2067. doi: 10.1158/1078-0432.CCR-06-2078. [DOI] [PubMed] [Google Scholar]
- 5.Cortazar P, Zhang L, Untch M, Mehta K, Costantino JP, Wolmark N, et al. Pathological complete response and long-term clinical benefit in breast cancer: the CTNeoBC pooled analysis. Lancet. 2014;384:164–172. doi: 10.1016/S0140-6736(13)62422-8. [DOI] [PubMed] [Google Scholar]
- 6.de Azambuja E, Holmes AP, Piccart-Gebhart M, Holmes E, Di Cosimo S, Swaby RF, et al. Lapatinib with trastuzumab for HER2-positive early breast cancer (NeoALTTO): survival outcomes of a randomised, open-label, multicentre, phase 3 trial and their association with pathological complete response. Lancet Oncol. 2014;15:1137–1146. doi: 10.1016/S1470-2045(14)70320-1. [DOI] [PubMed] [Google Scholar]
- 7.Gianni L, Pienkowski T, Im YH, Tseng LM, Liu MC, Lluch A, et al. 5-year analysis of neoadjuvant pertuzumab and trastuzumab in patients with locally advanced, inflammatory, or early-stage HER2-positive breast cancer (NeoSphere): a multicentre, open-label, phase 2 randomised trial. Lancet Oncol. 2016;17:791–800. doi: 10.1016/S1470-2045(16)00163-7. [DOI] [PubMed] [Google Scholar]
- 8.von Minckwitz G, Schneeweiss A, Loibl S, Salat C, Denkert C, Rezai M, et al. Neoadjuvant carboplatin in patients with triple-negative and HER2-positive early breast cancer (GeparSixto; GBG 66): a randomised phase 2 trial. Lancet Oncol. 2014;15:747–756. doi: 10.1016/S1470-2045(14)70160-3. [DOI] [PubMed] [Google Scholar]
- 9.McGrogan BT, Gilmartin B, Carney DN, McCann A. Taxanes, microtubules and chemoresistant breast cancer. Biochim Biophys Acta. 2008;1785:96–132. doi: 10.1016/j.bbcan.2007.10.004. [DOI] [PubMed] [Google Scholar]
- 10.Russell P, Hennessy BT, Li J, Carey MS, Bast RC, Freeman T, et al. Cyclin G1 regulates the outcome of taxane-induced mitotic checkpoint arrest. Oncogene. 2012;31:2450–2460. doi: 10.1038/onc.2011.431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Li ZH, Xiong QY, Tu JH, Gong Y, Qiu W, Zhang HQ, et al. Tau proteins expressions in advanced breast cancer and its significance in taxane-containing neoadjuvant chemotherapy. Med Oncol. 2013;30:591. doi: 10.1007/s12032-013-0591-y. [DOI] [PubMed] [Google Scholar]
- 12.Rouzier R, Rajan R, Wagner P, Hess KR, Gold DL, Stec J, et al. Microtubule-associated protein tau: a marker of paclitaxel sensitivity in breast cancer. Proc Natl Acad Sci U S A. 2005;102:8315–8320. doi: 10.1073/pnas.0408974102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wang K, Deng QT, Liao N, Zhang GC, Liu YH, Xu FP, et al. Tau expression correlated with breast cancer sensitivity to taxanes-based neoadjuvant chemotherapy. Tumour Biol. 2013;34:33–38. doi: 10.1007/s13277-012-0507-z. [DOI] [PubMed] [Google Scholar]
- 14.Rody A, Karn T, Gätje R, Ahr A, Solbach C, Kourtis K, et al. Gene expression profiling of breast cancer patients treated with docetaxel, doxorubicin, and cyclophosphamide within the GEPARTRIO trial: HER-2, but not topoisomerase II alpha and microtubule-associated protein tau, is highly predictive of tumor response. Breast. 2007;16:86–93. doi: 10.1016/j.breast.2006.06.008. [DOI] [PubMed] [Google Scholar]
- 15.Kawase M, Toyama T, Takahashi S, Sato S, Yoshimoto N, Endo Y, et al. FOXA1 expression after neoadjuvant chemotherapy is a prognostic marker in estrogen receptor-positive breast cancer. Breast Cancer. 2015;22:308–316. doi: 10.1007/s12282-013-0482-2. [DOI] [PubMed] [Google Scholar]
- 16.Liu Z, Li Z, Qu J, Zhang R, Zhou X, Li L, et al. Radiomics of multiparametric MRI for pretreatment prediction of pathologic complete response to neoadjuvant chemotherapy in breast cancer: a multicenter study. Clin Cancer Res. 2019;25:3538–3547. doi: 10.1158/1078-0432.CCR-18-3190. [DOI] [PubMed] [Google Scholar]
- 17.Pusztai L, Jeong JH, Gong Y, Ross JS, Kim C, Paik S, et al. Evaluation of microtubule-associated protein-Tau expression as a prognostic and predictive marker in the NSABP-B 28 randomized clinical trial. J Clin Oncol. 2009;27:4287–4292. doi: 10.1200/JCO.2008.21.6887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mazouni C, Peintinger F, Wan-Kau S, Andre F, Gonzalez-Angulo AM, Symmans WF, et al. Residual ductal carcinoma in situ in patients with complete eradication of invasive breast cancer after neoadjuvant chemotherapy does not adversely affect patient outcome. J Clin Oncol. 2007;25:2650–2655. doi: 10.1200/JCO.2006.08.2271. [DOI] [PubMed] [Google Scholar]
- 19.Symmans WF, Peintinger F, Hatzis C, Rajan R, Kuerer H, Valero V, et al. Measurement of residual breast cancer burden to predict survival after neoadjuvant chemotherapy. J Clin Oncol. 2007;25:4414–4422. doi: 10.1200/JCO.2007.10.6823. [DOI] [PubMed] [Google Scholar]
- 20.Amin MB, Greene FL, Edge SB, Compton CC, Gershenwald JE, Brookland RK, et al. The eighth edition AJCC cancer staging manual: continuing to build a bridge from a population-based to a more "personalized" approach to cancer staging. CA Cancer J Clin. 2017;67:93–99. doi: 10.3322/caac.21388. [DOI] [PubMed] [Google Scholar]
- 21.Early Breast Cancer Trialists' Collaborative Group (EBCTCG) Long-term outcomes for neoadjuvant versus adjuvant chemotherapy in early breast cancer: meta-analysis of individual patient data from ten randomised trials. Lancet Oncol. 2018;19:27–39. doi: 10.1016/S1470-2045(17)30777-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.von Minckwitz G, Untch M, Blohmer JU, Costa SD, Eidtmann H, Fasching PA, et al. Definition and impact of pathologic complete response on prognosis after neoadjuvant chemotherapy in various intrinsic breast cancer subtypes. J Clin Oncol. 2012;30:1796–1804. doi: 10.1200/JCO.2011.38.8595. [DOI] [PubMed] [Google Scholar]
- 23.Pentheroudakis G, Kalogeras KT, Wirtz RM, Grimani I, Zografos G, Gogas H, et al. Gene expression of estrogen receptor, progesterone receptor and microtubule-associated protein Tau in high-risk early breast cancer: a quest for molecular predictors of treatment benefit in the context of a Hellenic Cooperative Oncology Group trial. Breast Cancer Res Treat. 2009;116:131–143. doi: 10.1007/s10549-008-0144-9. [DOI] [PubMed] [Google Scholar]
- 24.Dumontet C, Krajewska M, Treilleux I, Mackey JR, Martin M, Rupin M, et al. BCIRG 001 molecular analysis: prognostic factors in node-positive breast cancer patients receiving adjuvant chemotherapy. Clin Cancer Res. 2010;16:3988–3997. doi: 10.1158/1078-0432.CCR-10-0079. [DOI] [PubMed] [Google Scholar]
- 25.Hess KR, Anderson K, Symmans WF, Valero V, Ibrahim N, Mejia JA, et al. Pharmacogenomic predictor of sensitivity to preoperative chemotherapy with paclitaxel and fluorouracil, doxorubicin, and cyclophosphamide in breast cancer. J Clin Oncol. 2006;24:4236–4244. doi: 10.1200/JCO.2006.05.6861. [DOI] [PubMed] [Google Scholar]
- 26.Peintinger F, Anderson K, Mazouni C, Kuerer HM, Hatzis C, Lin F, et al. Thirty-gene pharmacogenomic test correlates with residual cancer burden after preoperative chemotherapy for breast cancer. Clin Cancer Res. 2007;13:4078–4082. doi: 10.1158/1078-0432.CCR-06-2600. [DOI] [PubMed] [Google Scholar]
- 27.Liedtke C, Mazouni C, Hess KR, André F, Tordai A, Mejia JA, et al. Response to neoadjuvant therapy and long-term survival in patients with triple-negative breast cancer. J Clin Oncol. 2008;26:1275–1281. doi: 10.1200/JCO.2007.14.4147. [DOI] [PubMed] [Google Scholar]
- 28.Harbeck N, Gluz O. Neoadjuvant therapy for triple negative and HER2-positive early breast cancer. Breast. 2017;34(Suppl 1):S99–S103. doi: 10.1016/j.breast.2017.06.038. [DOI] [PubMed] [Google Scholar]