Abstract
Renal fibrosis is considered to be the final common outcome of chronic kidney disease. Dipeptidyl peptidase-4 (DPP-4) inhibitors have demonstrated protective effects against diabetic kidney disease. However, the anti-fibrotic effect of evogliptin, a DPP-4 inhibitor, has not been studied. Here, we report the beneficial effects of evogliptin on unilateral ureteral obstruction (UUO)-induced renal fibrosis in mice. Evogliptin attenuated UUO-induced renal atrophy and tubulointerstitial fibrosis. Immunohistochemistry and Western blotting demonstrated that evogliptin treatment inhibits pro-fibrotic gene expressions and extracellular matrix production. In vitro findings showed that the beneficial effects of evogliptin on renal fibrosis are mediated by inhibition of the transforming growth factor-β/Smad3 signaling pathway. The present study demonstrates that evogliptin is protective against UUO-induced renal fibrosis, suggesting that its clinical applications could extend to the treatment of kidney disease of non-diabetic origin.
Keywords: Dipeptidyl-peptidase IV inhibitors; Kidney failure, chronic; Transforming growth factor beta
INTRODUCTION
Diabetic kidney disease (DKD) is a leading cause of chronic kidney disease (CKD), and a considerable number of cases of CKD progress to end-stage renal disease (ESRD) [1]. Renal fibrosis is a major pathologic finding of ESRD and is characterized by extracellular matrix (ECM) accumulation induced by activation of the transforming growth factor-β (TGF-β)/Smad signaling pathway. It is generally accepted that TGF-β/Smad signaling induces the expression of pro-fibrotic genes, such as α-smooth muscle actin (α-SMA), plasminogen activator inhibitor-1 (PAI-1), and type 1 collagen [2]. For this reason, inhibition of TGF-β/Smad signaling is considered a promising therapeutic strategy to delay the development of renal fibrosis [3].
Dipeptidyl peptidase-4 (DPP-4) inhibitors reduce blood glucose levels by decreasing the degradation of glucagon-like peptide-1 [4]. In addition to their glucose-lowing effect, previous studies have revealed the anti-fibrotic effect of DPP-4 inhibitors in various organ systems, including heart, lung, liver, and kidney [5,6,7,8].
Evogliptin is a novel DPP-4 inhibitor and has a low potential for interaction with other drugs [9]. However, few reports have described the effects of evogliptin on renal tubulointerstitial fibrosis. Thus, we investigated whether evogliptin has a protective effect against renal fibrosis following unilateral ureteral obstruction (UUO) in mice, a well-characterized animal model of renal fibrosis. We also evaluated whether evogliptin inhibits the TGF-β/Smad3 signaling pathway in vitro.
METHODS
To generate UUO-induced renal fibrosis, the left ureter of C57BL/6J mice was doubly ligated, as previously described [10]. To investigate the effect of evogliptin at early and late time points, mice were into two groups; those destined to be sacrificed on day 7 and those destined to be sacrificed on day 11 after UUO. For each group, mice were randomly divided into three subgroups: Sham operation+vehicle (n=6), UUO+vehi-cle (n=6), and UUO+evogliptin (n=6). Evogliptin at a dose of 300 mg/kg (Dong-A ST Co., Ltd., Seoul, Korea) [11] or vehicle was orally administered from 3 days before UUO and on each day until they were scarified at 7 or 11 days after UUO. All procedures were performed in accordance with the guidelines specified by the Committee on Laboratory Animal Ethics, Kyungpook National University (KNU 2017-0010, Daegu, Korea) [12]. Other experimental methods are described in Supplementary Materials.
RESULTS
Evogliptin attenuates UUO-induced renal fibrosis and inhibits pro-fibrotic gene expression
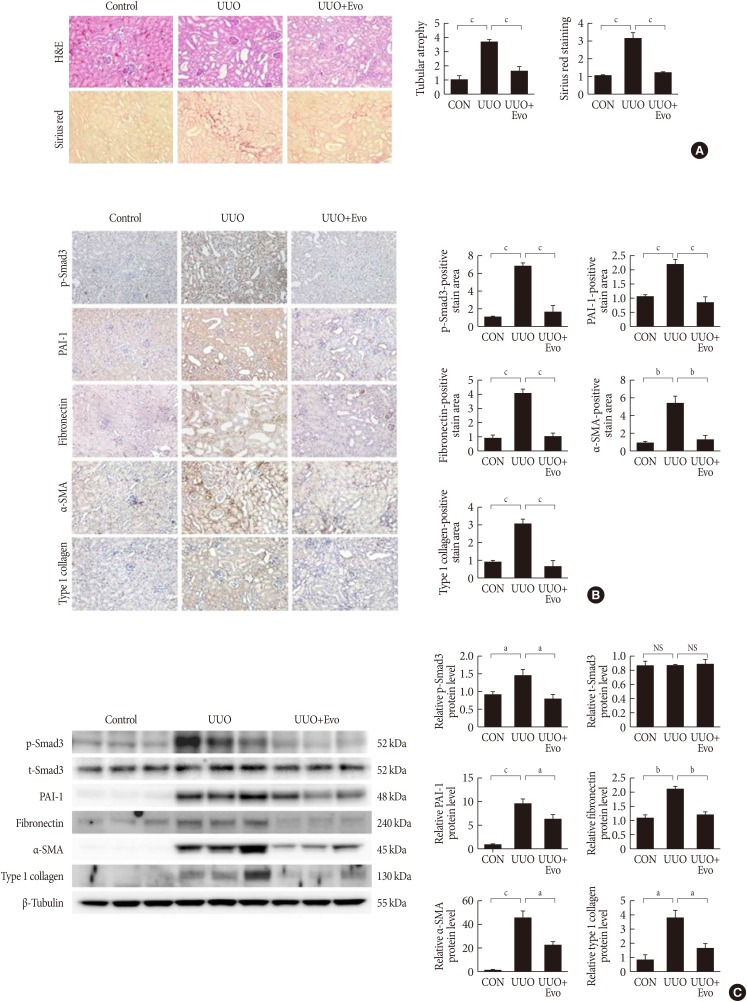
First, we investigated whether evogliptin ameliorates UUO-induced renal tubulointerstitial fibrosis by performing hematoxylin and eosin (H&E) and Sirius red staining. On day 11 after UUO, UUO induces prominent renal tubular atrophy and tubulointerstitial fibrosis. However, evogliptin-treated kidneys showed significant attenuation of both these pathological features (Fig. 1A). To evaluate the mechanism by which evogliptin attenuates UUO-induced renal fibrosis and ECM accumulation, we examined the effects of evogliptin on TGF-β/Smad3 signaling, which is a key mediator of renal fibrosis caused by UUO. Immunohistochemistry revealed that for phosphorylated Smad3, PAI-1, fibronectin, α-SMA, and type I collagen were markedly increased in the UUO kidneys, whereas these effects were ameliorated by evogliptin (Fig. 1B). These inhibitory effects of evogliptin on pro-fibrotic gene expression and ECM production were further evaluated by Western blot analysis. Consistent with the result of immunohistochemistry, the protein levels of phosphorylated Smad3, PAI-1, fibronectin, α-SMA, and type I collagen were lower in evogliptin-treated UUO kidneys than in vehicle-treated kidneys (Fig. 1C). We have also observed weak tubulointerstitial fibrosis 7 days after UUO, which was partially but significantly reduced by evogliptin treatment (Supplementary Fig. 1). As shown in Supplementary Figs. 2 and 3, body weight and food intake decreased at 3 days after UUO but fully recovered at 7 days after UUO. Blood glucose levels did not change after UUO or after evogliptin treatment in either the early or late time groups after UUO, suggesting that the anti-fibrotic effect of evogliptin was independent of its glucose-lowering effect. The kidney weights did not differ between groups.
Fig. 1. Effects of evogliptin (Evo) on renal fibrosis and pro-fibrotic gene expression in kidneys of unilateral ureteral obstruction (UUO) mice. A UUO kidney from a mouse at day 11. (A) Representative images of hematoxylin and eosin (H&E) and Sirius red staining of kidney tissue sections from control (CON) mice and UUO mice treated with (300 mg/kg) or without Evo. The number of atrophic tubules was determined by measuring the amount of abnormal irregular and dilated tubular basement membranes in H&E-stained sections under high power magnification (×200). Areas of positive staining with Sirius red were quantitated by computer-based morphometric analysis. All morphometric data were normalized against the corresponding val-ues in CON animals. Data in all bar graphs are expressed as fold increases relative to the CON (n=6 in each group). (B) Representative images of immunohistochemical staining for phosphorylated-Smad3 (p-Smad3), plasminogen activator inhibitor 1 (PAI-1), fibronectin, α-smooth muscle actin (α-SMA), and type I collagen in kidney tissue sections from CON mice or UUO mice treated with (300 mg/kg) or without Evo (n=6 in each group). Areas of positive staining with p-Smad3, PAI-1, fibronectin, α-SMA, and type I collagen antibodies were quantitated by computer-based morphometric analysis. Data are the mean±standard error of the mean (SEM) of five random fields from each kidney. (C) Representative western blot analysis of p-Smad3, total-Smad3 (t-Smad3), PAI-1, fibronectin, α-SMA, and type I collagen protein level in UUO kidneys from mice treated with (300 mg/kg) or without Evo (n=6 in each group). Data in the bar graphs are the mean±SEM. NS, not significant. aP<0.05, bP<0.01, cP<0.001.
Evogliptin attenuates pro-fibrotic molecules via suppression of TGF-β/Smad3 signaling
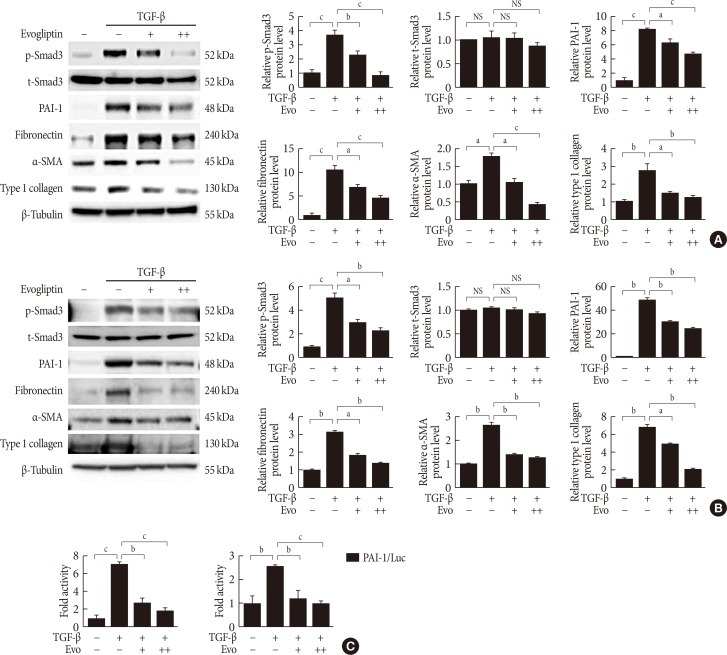
To determine whether the anti-fibrotic effect of evogliptin is mediated by effects on TGF-β-induced pro-fibrotic gene expression, we investigated whether evogliptin suppresses TGF-β-induced Smad3 phosphorylation, PAI-1, fibronectin, α-SMA, and type I collagen abundance in cultured renal cells (human proximal renal tubular epithelial [HK-2] and normal rat kidney fibroblast [NRK-49F] cells). In accordance with the in vivo findings, evogliptin inhibited TGF-β-stimulated Smad3 phosphorylation and upregulation of PAI-1, fibronectin, α-SMA, and type I collagen in renal tubular and fibroblast cells (Fig. 2A and B). We further examined whether evogliptin inhibits TGF-β/Smad3 signaling at the transcriptional levels by measuring PAI-1 luciferase activity, and, indeed, evogliptin treatment inhibited TGF-β-stimulated PAI-1 promoter activity in both NRK-49F and NRK-52E cells (Fig. 2C). These findings suggested that renoprotective effect of evogliptin is mediated by downregulation of Smad3 phosphorylation. Finally, we investigated the effect of evogliptin on plasma and renal DPP-4 activity after UUO. We observed that renal DPP-4 activity was significantly increased by UUO and that treatment with evogliptin markedly suppressed DPP-4 activity, in agreement with our previous finding (Supplementary Fig. 4A) [10]. Plasma DPP-4 activity was not significantly different between control and UUO mice; however, evogliptin treatment markedly reduced DPP-4 activity in UUO mice (Supplementary Fig. 4B).
Fig. 2. Effects of evogliptin (Evo) on transforming growth factor-β (TGF-β)-induced pro-fibrotic gene expression in cultured kidney cell lines. Representative Western blot analysis of phosphorylated-Smad3 (p-Smad3), total-Smad3 (t-Smad3), plasminogen activator inhibitor 1 (PAI-1), fibronectin, α-smooth muscle actin (α-SMA), and type I collagen protein level in TGF-β-stimulated (A) human proximal renal tubular epithelial (HK-2) cells and (B) normal rat kidney fibroblasts (NRK-49F) cells. Cells were incubated with TGF-β (5 ng/mL) treated with (100 or 200 µg/mL) or without Evo co-treatment for 24 hours. Data are the mean±standard error of the mean (SEM) of three independent measurements. (C) Effects of Evo on PAI-1 promoter activity in NRK-49F and NRK-52E cells. Cells were treated with TGF-β (5 ng/mL) treated with (100 µg/mL) or without Evo co-treatment for 24 hours. Data are the mean±SEM of three independent measurements. NS, not significant; Luc, luciferase. aP<0.05, bP<0.01, cP<0.001.
DISCUSSION
This study was undertaken to address whether evogliptin directly ameliorates renal fibrosis induced by UUO in mice and to elucidate the potential mechanism. Here, we show that evogliptin protects against renal fibrosis in this mouse model and that it inhibits TGF-β-stimulated Smad3 phosphorylation and ECM protein production in cultured renal cells.
TGF-β/Smad3 signaling is a crucial pathway in the pathogenesis of renal fibrosis [2,3]. Among Smad family, Smad3 is considered to be the principal regulator of the transcription of genes associated with renal fibrosis [13]. Upon its phosphorylation and activation by TGF-β receptor, Smad3 transactivates collagen genes to induce synthesis of ECM components and inhibit matrix degradation [14]. Recent study has shown that sitagliptin improves renal fibrosis by suppressing TGF-β/Smad3 signaling [15]. Alogliptin treatment of UUO mice had renoprotective effects through downregulation of the expression of TGF-β mRNA and α-SMA [16]. Previously, we also found that gemigliptin improved renal fibrosis in streptozotocin-induced diabetic mice by reducing TGF-β-stimulated Smad3 phosphorylation, which lowers the expression of ECM proteins, including type 1 collagen and fibronectin [17]. In addition, it was previously demonstrated that DPP-4 plays a role in TGF-β-induced receptor hetero-dimerization and that TGF-β-induced formation of the TGFR1/2 heterodimer is suppressed by small interfering RNA (siRNA)-mediated inhibition of DPP-4 [18]. Moreover, vildagliptin and linagliptin were successful in lowering the renal TGF-β level in a streptozotocin-induced diabetic rat [19,20]. Although we did not investigate the TGF-β level, the mechanisms described above could be, at least in part, responsible for evogliptin-mediated inhibition of TGF-β signaling. Therefore, further studies using Smad3-null transgenic mouse model are warranted to clarify the molecular mechanism responsible for evogliptin's suppressive effect on TGF-β/Smad3 signaling. The present study provides evidence that evogliptin has a protective effect on renal fibrosis by inhibiting TGF-β-stimulated Smad3 phosphorylation and its downstream signaling.
In conclusion, we have shown that evogliptin can prevent renal fibrosis by inhibiting the TGF-β/Smad3 signaling pathway. Our data suggest that evogliptin could be applied to prevent the progression of CKD or other etiologies, as well as DKD. Therefore, the present study provides the rationale for further clinical trials to evaluate the therapeutic efficacy of evogliptin in patient with DKD.
ACKNOWLEDGMENTS
This work was supported by the National Research Foundation of Korea (NRF) grants (NRF-2017M3A9G7073086, NRF-2018R1A2A1A05077703 and NRF-2018R1A6A3A01011962) funded by the Ministry of Science and ICT, NRF grant (NRF-2017R1A6A3A04010231) funded by the Ministry of Education, and grants (HI16C1501 and HI15C0001) from the Korea Health technology R&D Project through the Korea Health Industry Development Institute funded by the Ministry of Health and Welfare, Republic of Korea.
Footnotes
CONFLICTS OF INTEREST: No potential conflict of interest relevant to this article was reported.
- Conception or design: M.J.K., N.Y.K., Y.K.C., K.G.P.
- Acquisition, analysis, or interpretation of data: M.J.K., Y.A.J., S.H.L., G.S.J., J.G.K., I.K.L., S.L.
- Drafting the work or revising: N.Y.K., Y.K.C., K.G.P.
- Final approval of the manuscript: Y.K.C., K.G.P.
SUPPLEMENTARY MATERIALS
Supplementary materials related to this article can be found online at https://doi.org/10.4093/dmj.2018.0271.
Effects of evogliptin on renal fibrosis and pro-fibrotic gene expression in kidneys of unilateral ureteral obstruction (UUO) mice. (A, B) A UUO kidney from a mouse at day 7. (A) Representative images of hematoxylin and eosin (H&E) and Sirius red staining of kidney tissue sections from control (CON) mice and UUO mice treated with (300 mg/kg) or without evogliptin (Evo). The number of atrophic tubules was determined by measuring the amount of abnormal irregular and dilated tubular basement membranes in H&E-stained sections under high power magnification (×200). Areas of positive staining with Sirius red were quantitated by computer-based morphometric analysis. All morphometric data were normalized against the corresponding values in CON animals. Data in all bar graphs are expressed as fold increases relative to the CON (n=6 in each group). (B) Representative images of immunohistochemical staining for phosphorylated-Smad3 (p-Smad3), plasminogen activator inhibitor 1 (PAI-1), fibronectin, α-smooth muscle actin (α-SMA), and type I collagen in kidney tissue sections from CON mice or UUO mice treated with (300 mg/kg) or without Evo (n=6 in each group). Areas of positive staining with p-Smad3, PAI-1, fibronectin, α-SMA, and type I collagen antibodies were quantitated by computer-based morphometric analysis. Data are the mean±standard error of the mean of five random fields from each kidney. aP<0.05, bP<0.01, cP<0.001.
Effect of evogliptin (Evo) on metabolic parameters on day 11 post-unilateral ureteral obstruction (UUO). UUO mice were treated with (300 mg/kg) or without Evo. (A) Body weight, (B) food intake, (C) blood glucose, and (D) kidney weight were measured. CON, control; NS, not significant.
Effect of evogliptin (Evo) on metabolic parameters on day 7 post-unilateral ureteral obstruction (UUO). UUO mice were treated with (300 mg/kg) or without Evo. (A) Body weight, (B) food intake, (C) blood glucose, and (D) kidney weight were measured. CON, control; NS, not significant.
Effects of evogliptin (Evo) on renal and plasma dipeptidyl peptidase-4 (DPP-4) activity on days 7 post-unilateral ureteral obstruction (UUO). (A) DPP-4 activity in the kidney. (B) DPP-4 activity in the plasma. Data are the mean±standard error of the mean of five random fields from each kidney. CON, control; NS, not significant. aP<0.05, bP<0.001.
References
- 1.Atkins RC, Zimmet P IFKF World Kidney Day 2010 Steering Committee. Diabetes: diabetic kidney disease: act now or pay later. Nat Rev Nephrol. 2010;6:134–136. doi: 10.1038/nrneph.2010.10. [DOI] [PubMed] [Google Scholar]
- 2.Meng XM, Nikolic-Paterson DJ, Lan HY. TGF-β: the master regulator of fibrosis. Nat Rev Nephrol. 2016;12:325–338. doi: 10.1038/nrneph.2016.48. [DOI] [PubMed] [Google Scholar]
- 3.Lan HY, Chung AC. TGF-β/Smad signaling in kidney disease. Semin Nephrol. 2012;32:236–243. doi: 10.1016/j.semnephrol.2012.04.002. [DOI] [PubMed] [Google Scholar]
- 4.Salvo F, Moore N, Arnaud M, Robinson P, Raschi E, De Ponti F, Begaud B, Pariente A. Addition of dipeptidyl peptidase-4 inhibitors to sulphonylureas and risk of hypoglycaemia: systematic review and meta-analysis. BMJ. 2016;353:i2231. doi: 10.1136/bmj.i2231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hirakawa H, Zempo H, Ogawa M, Watanabe R, Suzuki J, Akazawa H, Komuro I, Isobe M. A DPP-4 inhibitor suppresses fibrosis and inflammation on experimental autoimmune myocarditis in mice. PLoS One. 2015;10:e0119360. doi: 10.1371/journal.pone.0119360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kaji K, Yoshiji H, Ikenaka Y, Noguchi R, Aihara Y, Douhara A, Moriya K, Kawaratani H, Shirai Y, Yoshii J, Yanase K, Kitade M, Namisaki T, Fukui H. Dipeptidyl peptidase-4 inhibitor attenuates hepatic fibrosis via suppression of activated hepatic stellate cell in rats. J Gastroenterol. 2014;49:481–491. doi: 10.1007/s00535-013-0783-4. [DOI] [PubMed] [Google Scholar]
- 7.Suzuki T, Tada Y, Gladson S, Nishimura R, Shimomura I, Karasawa S, Tatsumi K, West J. Vildagliptin ameliorates pulmonary fibrosis in lipopolysaccharide-induced lung injury by inhibiting endothelial-to-mesenchymal transition. Respir Res. 2017;18:177. doi: 10.1186/s12931-017-0660-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Eun Lee J, Kim JE, Lee MH, Song HK, Ghee JY, Kang YS, Min HS, Kim HW, Cha JJ, Han JY, Han SY, Cha DR. DA-1229, a dipeptidyl peptidase IV inhibitor, protects against renal injury by preventing podocyte damage in an animal model of progressive renal injury. Lab Invest. 2016;96:547–560. doi: 10.1038/labinvest.2016.34. [DOI] [PubMed] [Google Scholar]
- 9.Tan X, Hu J. Evogliptin: a new dipeptidyl peptidase inhibitor for the treatment of type 2 diabetes. Expert Opin Pharmacother. 2016;17:1285–1293. doi: 10.1080/14656566.2016.1183645. [DOI] [PubMed] [Google Scholar]
- 10.Min HS, Kim JE, Lee MH, Song HK, Kang YS, Lee MJ, Lee JE, Kim HW, Cha JJ, Chung YY, Hyun YY, Han JY, Cha DR. Dipeptidyl peptidase IV inhibitor protects against renal interstitial fibrosis in a mouse model of ureteral obstruction. Lab Invest. 2014;94:598–607. doi: 10.1038/labinvest.2014.50. [DOI] [PubMed] [Google Scholar]
- 11.Kim MK, Chae YN, Kim HD, Yang EK, Cho EJ, Choi SH, Cheong YH, Kim HS, Kim HJ, Jo YW, Son MH, Kim SH, Shin CY. DA-1229, a novel and potent DPP4 inhibitor, improves insulin resistance and delays the onset of diabetes. Life Sci. 2012;90:21–29. doi: 10.1016/j.lfs.2011.10.007. [DOI] [PubMed] [Google Scholar]
- 12.Jung GS, Kim MK, Jung YA, Kim HS, Park IS, Min BH, Lee KU, Kim JG, Park KG, Lee IK. Clusterin attenuates the development of renal fibrosis. J Am Soc Nephrol. 2012;23:73–85. doi: 10.1681/ASN.2011010048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Iwano M, Plieth D, Danoff TM, Xue C, Okada H, Neilson EG. Evidence that fibroblasts derive from epithelium during tissue fibrosis. J Clin Invest. 2002;110:341–350. doi: 10.1172/JCI15518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sato M, Muragaki Y, Saika S, Roberts AB, Ooshima A. Targeted disruption of TGF-beta1/Smad3 signaling protects against renal tubulointerstitial fibrosis induced by unilateral ureteral obstruction. J Clin Invest. 2003;112:1486–1494. doi: 10.1172/JCI19270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wang D, Zhang G, Chen X, Wei T, Liu C, Chen C, Gong Y, Wei Q. Sitagliptin ameliorates diabetic nephropathy by blocking TGF-β1/Smad signaling pathway. Int J Mol Med. 2018;41:2784–2792. doi: 10.3892/ijmm.2018.3504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Uchida T, Oda T, Matsubara H, Watanabe A, Takechi H, Oshima N, Sakurai Y, Kumagai H. Renoprotective effects of a dipeptidyl peptidase 4 inhibitor in a mouse model of progressive renal fibrosis. Ren Fail. 2017;39:340–349. doi: 10.1080/0886022X.2017.1279553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jung GS, Jeon JH, Choe MS, Kim SW, Lee IK, Kim MK, Park KG. Renoprotective effect of gemigliptin, a dipeptidyl peptidase-4 inhibitor, in streptozotocin-induced type 1 diabetic mice. Diabetes Metab J. 2016;40:211–221. doi: 10.4093/dmj.2016.40.3.211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shi S, Srivastava SP, Kanasaki M, He J, Kitada M, Nagai T, Nitta K, Takagi S, Kanasaki K, Koya D. Interactions of DPP-4 and integrin β1 influences endothelial-to-mesenchymal transition. Kidney Int. 2015;88:479–489. doi: 10.1038/ki.2015.103. [DOI] [PubMed] [Google Scholar]
- 19.Liu WJ, Xie SH, Liu YN, Kim W, Jin HY, Park SK, Shao YM, Park TS. Dipeptidyl peptidase IV inhibitor attenuates kidney injury in streptozotocin-induced diabetic rats. J Pharmacol Exp Ther. 2012;340:248–255. doi: 10.1124/jpet.111.186866. [DOI] [PubMed] [Google Scholar]
- 20.Kanasaki K, Shi S, Kanasaki M, He J, Nagai T, Nakamura Y, Ishigaki Y, Kitada M, Srivastava SP, Koya D. Linagliptin-mediated DPP-4 inhibition ameliorates kidney fibrosis in streptozotocin-induced diabetic mice by inhibiting endothelial-to-mesenchymal transition in a therapeutic regimen. Diabetes. 2014;63:2120–2131. doi: 10.2337/db13-1029. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Effects of evogliptin on renal fibrosis and pro-fibrotic gene expression in kidneys of unilateral ureteral obstruction (UUO) mice. (A, B) A UUO kidney from a mouse at day 7. (A) Representative images of hematoxylin and eosin (H&E) and Sirius red staining of kidney tissue sections from control (CON) mice and UUO mice treated with (300 mg/kg) or without evogliptin (Evo). The number of atrophic tubules was determined by measuring the amount of abnormal irregular and dilated tubular basement membranes in H&E-stained sections under high power magnification (×200). Areas of positive staining with Sirius red were quantitated by computer-based morphometric analysis. All morphometric data were normalized against the corresponding values in CON animals. Data in all bar graphs are expressed as fold increases relative to the CON (n=6 in each group). (B) Representative images of immunohistochemical staining for phosphorylated-Smad3 (p-Smad3), plasminogen activator inhibitor 1 (PAI-1), fibronectin, α-smooth muscle actin (α-SMA), and type I collagen in kidney tissue sections from CON mice or UUO mice treated with (300 mg/kg) or without Evo (n=6 in each group). Areas of positive staining with p-Smad3, PAI-1, fibronectin, α-SMA, and type I collagen antibodies were quantitated by computer-based morphometric analysis. Data are the mean±standard error of the mean of five random fields from each kidney. aP<0.05, bP<0.01, cP<0.001.
Effect of evogliptin (Evo) on metabolic parameters on day 11 post-unilateral ureteral obstruction (UUO). UUO mice were treated with (300 mg/kg) or without Evo. (A) Body weight, (B) food intake, (C) blood glucose, and (D) kidney weight were measured. CON, control; NS, not significant.
Effect of evogliptin (Evo) on metabolic parameters on day 7 post-unilateral ureteral obstruction (UUO). UUO mice were treated with (300 mg/kg) or without Evo. (A) Body weight, (B) food intake, (C) blood glucose, and (D) kidney weight were measured. CON, control; NS, not significant.
Effects of evogliptin (Evo) on renal and plasma dipeptidyl peptidase-4 (DPP-4) activity on days 7 post-unilateral ureteral obstruction (UUO). (A) DPP-4 activity in the kidney. (B) DPP-4 activity in the plasma. Data are the mean±standard error of the mean of five random fields from each kidney. CON, control; NS, not significant. aP<0.05, bP<0.001.


