Abstract
Alcohol use among HIV-positive individuals in sub-Saharan Africa directly impacts adherence to antiretroviral therapy and HIV outcomes. Few studies have examined approaches to reduce alcohol use among HIV-affected couples, despite evidence that alcohol use is a couple-level concern. We conducted a qualitative study with 23 alcohol-using couples to identify multilevel barriers and facilitators of alcohol use, and potential intervention options with couples. Data were analyzed at individual and dyadic levels using framework analysis. All couples were married and had at least one partner on ART. Men were the primary alcohol drinkers with few women reporting alcohol use. Most women tried to persuade their partners to reduce their alcohol intake and when unsuccessful, enlisted help from relatives and HIV care providers. Effective couple negotiation around men’s alcohol use was constrained by negative peer influence and men’s desire for friendship to cope with life stressors. Women were primarily concerned about the expense of alcohol and described how alcohol prevented the family from meeting basic needs and investing in the future. Alcohol use was described as a major barrier to ART adherence, but was also viewed as the cause of couple and family violence, extramarital partnerships, food insecurity, and poverty. We conclude that multilevel interventions based on couples’ needs and preferences are urgently needed. Couple-based intervention approaches could include provider-led alcohol counseling with couples, alcohol reduction support groups for couples, couples’ counseling to bolster couple communication and problem-solving around alcohol, and economic-strengthening interventions for couples.
Keywords: Couples, Alcohol, Antiretroviral Therapy, Adherence, Sub-Saharan Africa
Introduction
Globally, alcohol consumption is common among people living with HIV (PLHIV) with around one-third of adults reporting recent alcohol use [1]. Sub-Saharan Africa (SSA) has been severely impacted by the HIV/AIDS epidemic, accounting for two-thirds of people living with HIV worldwide [2]. Although the majority of adults abstain from alcohol in SSA (70%), adults who drink have some of the highest rates of per capita alcohol consumption in the world [3]. In Malawi, 68% of adults do not drink alcohol, but among those who drink, 41% are heavy drinkers who consumed 60 grams or more of pure alcohol on at least one occasion in the past 30 days [4]. The harmful effects of alcohol use on people living with HIV are well-documented and include malnutrition [5], liver disease and toxicities [6, 7], poor adherence to antiretroviral therapy (ART) [8], HIV disease progression [9, 10], and unsuppressed viral load [11]. Alcohol use also increases the risk of HIV transmission to sexual partners [9, 12].
Primary partners such as spouses can play a key role in helping partners reduce alcohol use and its harms for PLHIV in SSA. According to couple interdependence theory, primary partners can positively influence each other’s drinking behaviors [13] and alcohol use can be both a cause and consequence of relationship distress [14], with research in the U.S. finding support for both directions [15-17]. However, in SSA, a couple-focused perspective on alcohol use has received relatively little attention, despite evidence that the couple unit is important for other health behaviors including sexual risk reduction [18], prevention-of-mother-to-child transmission [19], HIV counseling and testing [20-23], HIV status disclosure [24], and ART adherence [25, 26].
There are several arguments for why alcohol use may be best understood and intervened upon as a couple-level issue in SSA. Although alcohol use in SSA is less common among women than men, the health of women who abstain from alcohol use may still be at risk through their partners’ drinking. Qualitative research on HIV-affected couples in Malawi found that wives experience violence, food insecurity, poor mental health, and non-adherence to ART as a consequence of their husbands’ alcohol use [27, 28]. Alcohol drinkers may also fail to provide the necessary support for their partners’ ART adherence when spending time away from the household drinking, or forgetting to provide support while intoxicated [28]. Furthermore, PLHIV in SSA may intentionally skip pills while drinking alcohol [29, 30], which may be influenced by partners’ beliefs about mixing alcohol and ART [31]. On the other hand, primary partners can mitigate the deleterious effects of alcohol by helping HIV-positive partners manage alcohol use and maintain adherence to ART even while drinking [31].
Despite the importance of couple relationships for alcohol use and ART adherence, the majority of alcohol interventions for PLHIV have centered on individuals [32] and in SSA, these interventions have shown mixed results and have not addressed the interpersonal context surrounding alcohol use. In Uganda, an intervention using motivational interviewing to reduce hazardous drinking among PLHIV showed a significant reduction in alcohol use between the intervention and control arms, but only for women [33]. A cluster RCT of a clinic-based intervention in Kenya, Namibia, and Tanzania showed that the intervention significantly increased provider discussions about alcohol but failed to reduce alcohol use [34]. Similarly, a cognitive behavioral therapy (CBT) intervention offered to adolescents living with HIV in Uganda did not show an impact on alcohol use [35]. The most promising intervention to date was a CBT-based intervention for PLHIV in Kenya and showed significant reductions in alcohol use [36]. The intervention was delivered by trained professionals over multiple sessions and emphasized locally-salient motivations for quitting drinking such as promoting health and saving money, and placed a strong emphasis on men’s alcohol refusal skills [37].
Couple-based interventions could address some of the limitations of existing individual-level approaches by addressing the interpersonal context in which drinking takes place and could also help to reinforce messages and strategies around reducing alcohol use. Other research finds that couple-based interventions have been have been successful at improving ART adherence [38], uptake of couples HIV counseling and testing [23], gender and relationship dynamics [39], and reducing sexual risk [39]. Furthermore, it is imperative that interventions consider the detrimental effects of alcohol use on couples and households, such as poverty and food insecurity, which can worsen adherence and HIV clinical outcomes [40, 41]. This premise is supported by research from the U.S. showing that couple-based alcohol interventions are effective because they address important relationship dynamics that intersect with alcohol use [42, 43]. To our knowledge, few interventions in sub-Saharan Africa have used a couple-based approach to reduce alcohol use among PLHIV and their partners. One of the few couples-based interventions for alcohol use in Africa (the Couples Health Co-Op), while not specifically targeting PLHIV, was shown to be effective at reducing heavy drinking among men in the treatment arm (couples intervention) as compared to control arm (men-only groups) [44, 45].
We conducted a study with HIV-affected Malawian couples to understand the barriers and facilitators of alcohol use within the couples. The ultimate objective of this research is to inform a future alcohol intervention for couples living with HIV to reduce alcohol use and improve adherence to ART. In recognition of the complex interplay of multilevel determinants of alcohol use in SSA, we use a social-ecological framework to consider how alcohol use is shaped by structural and economic, social, couple, and individual-level factors [46]. We also draw on couple interdependence theory to argue that the dyad is central to this framework and that an individual’s alcohol use is regulated by the couple’s ability to effectively engage in healthy behaviors as a unit—in this case, alcohol reduction or cessation [46, 47]. Finally, we adopted an inductive approach in asking Malawian couples to suggest appropriate interventions with the goal of informing future interventions that are demand-driven, locally-grounded, and appropriate for couples’ needs.
Methods
The current study was nested within the Umodzi M’Banja study in Malawi, which is a mixed-methods observational study consisting of qualitative interviews and survey to understand primary relationships and HIV care engagement. Briefly, couples in the larger study were recruited from two HIV care clinics in the Zomba district of southern Malawi (Zomba District Hospital, a large public hospital, and Pirimiti, a private rural hospital) when attending HIV clinic appointments or picking up their HIV medications. Couples had to be in a non-polygamous marriage or cohabitating union, with at least one partner on ART who had disclosed their HIV status to their primary partner in the study. Both partners had to be age 18 or older. Because all couples reported being in a legal or traditional marriage, we refer to partners as husbands and wives.
For this sub-study on alcohol use, we purposively selected couples with at least one partner who had used alcohol in the past year as indicated in the qualitative interviews or survey containing the AUDIT-C measure [48]. After selecting couples with at least one drinker, we verified that the alcohol use had also been reported by the drinker’s spouse. This verification ensured that spouses of drinkers would be able to describe their experiences with their partners’ alcohol use. Couples did not have to be currently using alcohol, and in the case of past alcohol use, they were asked to retrospectively recall their own or their partners’ alcohol use. After creating a list of eligible couples, couples were contacted via phone and asked if they would be willing to participate in the alcohol sub-study. We first contacted the member of the couple who reported alcohol use (usually the husband). If the husband agreed to participate, we would then speak with the wife to assess her interest in participating. Both partners had to be willing to participate in the study and provide informed consent to be enrolled. Couples who were interested were then scheduled for an in-person interview. Based on our prior qualitative studies with HIV-affected couples in SSA [26, 49], we estimated that a sample size of approximately 20 couples would be both feasible and sufficient for meeting data saturation. After interviewing 23 couples (46 individuals), we concluded that we had reached saturation.
Two Malawian interviewers (one male, one female) facilitated the interviews. They were fluent in English and Chichewa, had completed their Malawi School Certificate of Education (MSCE), had experience conducting in-depth interviews on other health-related research projects, and received further training by two study authors (AAC and SAM) before initiating interviews. The two interviewers were matched by gender to participants. Both partners were interviewed simultaneously, but separately, in private spaces at the two HIV clinics. We chose this approach for its validity when discussing sensitive topics such as alcohol use, providing a shared narrative on a given topic, and allowing opportunities for differing perspectives to arise [50]. Two interview guides were drafted, piloted, and revised—one for the male partner focused on his alcohol use (all male partners used alcohol) and one for the female partner focused on her partner’s alcohol use. We also asked female partners about their own alcohol use, although few women reported alcohol use. The interview guides were informed by couple interdependence theory using a conceptual framework from our prior study on alcohol use and ART in Malawi [28]. Drinkers were asked to describe their alcohol history, patterns of alcohol use and types of alcohol consumed, how alcohol positively and negatively affected their family and relationship, alcohol use as a barrier to ART adherence, couple communication around alcohol use, barriers and facilitators to reducing alcohol use, and communication with HIV care providers about alcohol and ART. Partners were asked to describe the drinker’s pattern of alcohol use, how alcohol affected family and couple dynamics, couple communication around alcohol use, their role (if any) in changing their partner’s alcohol use, and communication with HIV care providers about their partner’s alcohol use. Both partners were asked to suggest ideas for an intervention to reduce alcohol use among ART patients. All interviews lasted 30–60 minutes, and were audio-recorded, transcribed, and translated from Chichewa into English.
Data were analyzed at the individual and dyadic levels using framework analysis to allow for comparison of wives’ and husbands’ responses on a variety of topics and to support the analysis of couples as well as individuals. Framework analysis uses data matrices to organize the data by themes and cases, allowing for the synthesis of large dyadic qualitative datasets, and is conducted over five steps [51]. The first step of framework analysis was data familiarization. The authors (AAC, SAM) became immersed in the data by reading each couple’s transcripts and taking detailed notes on the couple. The second step was to identify a thematic framework based on the interview guide topics and issues raised by the couples themselves. The authors identified 15 codes (e.g., “husband’s drinking patterns”, “negative effects of drinking on family”, “positive effects of drinking on family”, “motivations for drinking”), based on a reading of the transcripts and the interview guide. Meeting were held to discuss the codes and come to a consensus. The third and fourth steps were to “index” or code the raw data and then “chart” the data to gain a complete picture of all couples, which was done simultaneously. Three study authors (AAC, SAM, AR) created a matrix for each couple, with a row for each of the 15 codes and a column for the responses of each member of the couple. These matrices were populated with summaries of participants’ stories and verbatim quotes related to the codes. We also created a summary matrix for the entire sample with a row for each couple, which noted areas of inconsistency and disagreement between partners on the 15 codes. The second author then coded the couple-specific matrices using NVivo 11 software (QSR International, 2017), which facilitated comparisons across couples (e.g., different ways in which alcohol affected couples), between partners (e.g., discrepancies in descriptions of alcohol use patterns), and across individuals (e.g., intervention preferences). The last step of framework analysis was mapping and interpretation. The three study authors held regular meetings to discuss similarities and differences between couples using the data matrices and raw data, and to identify underlying themes. This process led to several main themes as highlighted below. We included participant identifiers with the quotes below, with “F” or “M” denoting the female or male partner. We presented the findings to the research team and other stakeholders in Malawi for feedback, which validated our interpretation.
Findings
Sample characteristics
Twenty-three couples (46 individuals) were enrolled in the study. The mean age was 41 years and 78% had a primary school education or less. The mean relationship duration was 11 years on average and 74% of couples were HIV sero-concordant positive (the remainder were sero-discordant). The majority of all participants (87%) were currently on ART (all HIV-positive individuals were on ART). The majority of women (87%) reported currently abstaining from alcohol; three women had recently drank alcohol at a wedding or traditional celebration but otherwise abstained or drank rarely. In contrast, all but two men (91%) reported being current drinkers, which was confirmed by their wives. The remaining men stopped drinking several years prior. Almost half of men (42%) were hazardous drinkers based on the AUDIT-C. The sample was similar to drinkers enrolled in the parent study on these key characteristics.
Couple reports of men’s drinking behaviors: Discrepancies and confirmation
While most men described their drinking as being under control and not excessive, women generally portrayed their husband’s drinking as frequent and heavier than what the men described. For example, one man (7M) claimed to have drunk heavily in the past, but asserted that he now only drinks once or twice a month when he “bumped into some friends who say to me let’s go out drinking,” and not to the extent of getting drunk. His wife (7F) described a quite different pattern in which he sometimes went to drink rather than going to work or drank all night rather than coming home. When asked by the interviewer how many times in the previous week he had come home drunk, she replied “almost the whole week.”
A number of men reported that they had quit drinking or reduced their alcohol intake after an HIV diagnosis or initiating ART. In more than half of couples, wives confirmed that husbands had reduced or quit drinking because of their HIV diagnosis or other factors. Several men seemed to imply that they would not have changed their drinking habits if not for their HIV diagnosis and one woman explicitly stated that she believed her husband would still be drinking if not for ART. Other men reported a desire to reduce or quit drinking and said that they aimed to slowly reduce their alcohol intake over time. One man (2M) described his decision to quit drinking after his HIV diagnosis as follows (a change also described by his wife):
Since that time, I changed because I was drinking frequently. Sometimes I couldn’t even have an appetite for food. As soon as the day breaks, the first [thing] to do was to drink, and also I didn’t have interest in working to earn money because I was always at a drinking place so I could not find time to work. Now reaching that level, I thought that it is better to take care of my body so I decided to spend time working to earn a living. If I earn, that means my household needs will be met and I will have a healthy life.
The wife (3F) of another man also described her husband’s a dramatic change, post-HIV diagnosis.
I can say that he has changed in comparison to how he was drinking in the past. He has completely changed since he got his [HIV] results because he was told that he should not drink alcohol… he has changed because he wants to concentrate in his medication.
Couple negotiation around alcohol use and ART: Successes and challenges
Men’s changes in drinking behavior were often in response to couples’ communication around alcohol use, and all women tried to persuade their husbands to quit drinking. In some cases, men’s HIV diagnosis or initiation of ART triggered conversations about alcohol use, such as the woman who said, “It was the start of ART that helped me talk to my partner.” (17F) Some women addressed husbands’ drinking when their husbands came home drunk and others intentionally avoided conversations at this time, especially if they feared violence.
Women utilized a variety of other strategies to discourage their husbands’ alcohol use, such as staying home to monitor whether their husbands went out to drink, requesting that husbands stay home to spend time with the family or do chores, or brewing sweet beer (thobwa, a non-alcoholic fermented drink) to help with cravings. One woman described in desperation how her husband’s drinking had left them “failing to take care of the children,” and in response, she sought divine intervention through “fasting, climbing mountains, and going for prayers.” (17F) Another woman reported giving her husband the dire warning that beer would “destroy their relationship” and interfere with his ART adherence, to which he replied that he was “already dead.” (23F)
Around one-third of women reported that their husbands refused to listen to their advice about reducing drinking or that their husbands had promised to quit drinking, but did not keep the promise over time. These women generally seemed discouraged and resigned to their husbands’ continued drinking. One woman said advising her husband was “impossible,” and another commented, “A man is a man and cannot listen to a woman.” Multiple women voiced similar feelings to the woman who said, “We can have a talk, but he never changes… that’s why I just leave him like that. Maybe in future he will change.” (13F) Some women then focused on getting their husbands to reduce rather than quit drinking entirely. Both women and men reported that communication about alcohol often incited conflict and shouting, and one woman reported that her husband threatened to beat her if she persisted in talking about his alcohol use. Some men agreed their wives had not been able to change their alcohol habits. One man reported, “She said I should stop drinking, but I convinced her how important alcohol is to me.” He explained that alcohol helped him relax, forget about HIV, and mingle with friends which sometimes led to employment opportunities. (18M)
A minority of couples engaged in productive conversations about drinking, and agreed to reduce or stop drinking. One man (15M) reported, “We discussed that if we drink alcohol, it won’t do us good at our household,” an account which was confirmed by his wife. Another woman reported that her husband had reduced his drinking after she told him to choose between alcohol and her. A third woman said that after her husband had repeatedly missed ART doses while drunk, she persuaded him to reduce his drinking, although not to the levels she hoped for:
He has reduced… I told him that you are not doing the right thing because you miss a lot of medication. Then he changed… What discourages me most is when I try to sit down with him he pretends as if he has understood. But after some time when his friends come to take him for drinking, he accepts that and off he goes. He doesn’t consider my views. (19F)
Women’s constrained influence on men’s drinking: Leveraging outside social support
When approaches did not work as planned, some women enlisted the help of community leaders, marriage counselors, or relatives in persuading men to quit drinking. Some of these women noted that their partners reduced their drinking after talking with a relative, but then relapsed. One man reported how he stopped drinking after being counseled by his brother, although according to his wife’s account, the brother was only successful in persuading him to stop beating her, and not in changing his drinking habits.
Although it was rare for a wife to go behind her husband’s back and invoke the help of an HIV care provider, one woman did so out of concern for her husband’s habit of taking alcohol while on ART.
I told the HIV provider the drinking habit of my partner. I asked, “Is it possible for someone who is on ART should also drink alcohol?” Then they asked me, “Why have you asked that question?” Then I told them, my partner drinks alcohol and the medication cannot be combined with alcohol. I was told that he should [come back] for counseling. (17F)
Social influences beyond the couple: The role of friendship and social pressure
Women and men described a pattern of male socialization involving alcohol consumption and reported strong social pressure from other men to drink. Men occasionally drank at home but primarily consumed alcohol at drinking establishments in the company of male friends or family members. Women and men described men’s drinking as an activity to pass the time, to spend time with friends, and as a means of coping with stress and forgetting worries related to spousal conflict, poverty, and living with HIV. Some participants stated that if a man lacked money to buy alcohol, his friends would purchase alcohol for him. Local brews such as masese were often drunk from a communal pot, and other alcohol such as chibuku (commercially-produced beer) or kachasu (locally-made spirit) could be passed around or shared among a group.
Some men stated that they didn’t think men could quit drinking due to peer pressure and the draw of companionship while drinking. One man said, “I really want to stop, but I have many friends who drink alcohol so many times they invite me to drink with them.” (4M) Several men stated that they had quit drinking in the past, but started to drink again because of pressure or influence from friends. Stress, particularly related to poverty, could play a role in their relapses, in that men sought companionship during these times. One man said, “When there is something that has upset me, I go out to chat with friends and I find myself drinking alcohol, but it’s not my intention.” (8M) Women also recognized the strong social pressure exerted on their husbands. One woman calling her husband’s friends “bad company” and said, “They are the ones who encourage my partner to drink alcohol.” (1F) Another woman lamented,
The challenge are his friends. They are too bad, they encourage him to drink alcohol. Sometimes he tells me he wants to stop, but his friends encourage him. I also I ask him if I should chase them away, but he doesn’t give me permission to do so. (9F)
The economic strain of alcohol use on couple relationships and families
Most women expressed that there was nothing good that had come from their husbands’ drinking, but women’s primary concern was the expense. Multiple women reported that their families could not advance economically because their husband spent so much of the available money on alcohol, and a few wives reported that their husbands had bought alcohol despite the lack of food or basic necessities. One woman stated,
What I see is that when he is drunk… he wastes a lot of money that could have been used for something else… and when he is coming home, he comes without money. That affects the next day’s budget, and this keeps pulling us backward instead of going forward and that pains me. This really affects my family very much. (2F)
Women’s and men’s accounts often conflicted when it came to the financial impact of alcohol. One woman deemed her household situation a financial crisis, whereas her husband stated that his alcohol use had not really impacted his family. Another man drank away from home secretively so that his wife would not complain about the money he was spending on alcohol. She stated that he did not provide money for food and the children’s schooling, while he insisted his drinking did not negatively impact his family. Other wives were careful to say that their husbands made sure to purchase food before they went out drinking. One woman said she did not mind her husband’s drinking because “he drinks from his friends, so I feel better… I feel like I’m free since he doesn’t buy alcohol these days.” (4F) Another woman seemed to enjoy the damper that a lack of disposable income put on her husband’s drinking and recalled that when he had money, he spent it on alcohol.
Many men acknowledged their wives’ concerns as well as the negative impact their drinking had on their families, including on family finances. One man called alcohol “very bad” and admitted he had spent money on alcohol rather than food for his family. Another man said he “squandered” money that could have been used for household needs. Remarkably, one man seemed to say that he spent half of the household’s disposable income on alcohol.
I was spending more money on alcohol although I didn’t realize that was not a good idea. But my wife was complaining about that. Sometimes I could find money and I was dividing it into equal shares, half was used to buy alcohol and the other half was used to buy food… My wife was complaining because we were unable to achieve our goals. (1M)
In addition to financial strain, wives’ accounts also provided evidence of other costs of alcohol use including the inability to take ART as prescribed, weight loss and ill health, difficulties engaging in livelihoods and productive activities, loss of time with their children and families, and strife with wives and neighbors. A common refrain in women’s accounts was that men were often away from home and at drinking establishments. Some men admitted that after drinking heavily, they were unable to work, such as the man who said,
We don’t do the work as we planned because of the alcohol. For example, the work that we were supposed to do in one or two hours, we only work for only one hour because of me being weak with the alcohol and that will make her to obviously hate the alcohol. (16M)
Furthermore, some women stated that they believed drinking contributed to their husband’s extramarital partnerships, such as the woman who said, “When someone is busy drinking, he also thinks of other women. But if he can stop drinking, he can’t think of other women.” (19F) Another woman complained that her husband’s financial support of other sexual partners acquired at drinking establishments further depleted household resources.
I know that when he has gone for beer drinking, he has other girls as sexual partners. When I hear that, it pains me more and I get very angry with him. He does not leave money at home with me but he is able to give it to other girls. (22F)
Men’s alcohol use caused conflict and instability in most couples, as did the financial strain which resulted from men’s expenditure on alcohol. Several men acknowledged that their relationships were better when they were sober, observing that their wives hated their alcohol usage and that when they drank there was “no peace at home.” One man described how his drinking nearly cost him his family, saying, “I was afraid that due to beer drinking, my family would end soon, that my wife will leave me and go.” (23M) Nearly half of women reported that their husbands had beaten them or the children while drunk. Furthermore, in some cases men broke or destroyed household resources while drunk, either through malice or clumsiness. In a particularly poignant account, one woman recounted how while in a drunken rage, her husband had intentionally broken multiple crates of eggs that she intended to sell.
Multilevel preferences for an alcohol reduction intervention
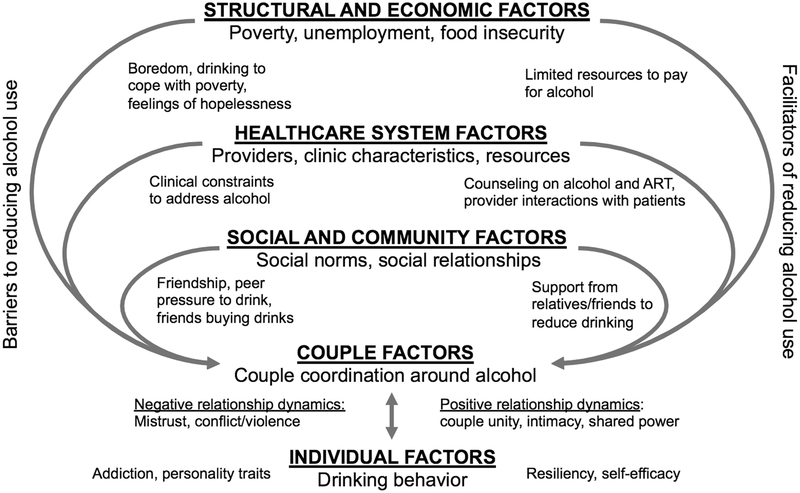
Despite the many challenges of alcohol use for couples, most women and men expressed strong support for an intervention, which could help men to reduce drinking. Participants described interventions targeting different levels of the socio-ecological model (see Figure 1). At the structural and economic level, several participants believed that an intervention addressing underlying poverty could reduce men’s alcohol use. For example, one woman suggested that providing food support could curb the practice of using alcohol as a meal replacement, saying “food is something that gives men power so that they cannot go to drink beer.” (participant 23F) In Malawi, commercially-produced beer (e.g., chibuku) and even local brews (e.g., masese) have been marketed as a source of food and nutrition. Several men with a family brewing operation stated that although the business was necessary to the family’s survival, they preferred a different type of business, which did not tempt them to consume alcohol. For example, one man stated:
Figure 1.
Multilevel determinants of alchohol use in couples affected by HIV in Malawi
We brew the alcohol to find money so that we should be buying one piece by piece of the iron sheets to roof our house. Alcohol is prohibited by the HIV providers but you just find yourself tasting it [the alcohol]. Help us… by providing us with money…[for] our necessities or business startup capital. (8M)
At the social and community level, participants suggested that village chiefs could host meetings in the community to educate people on the harms of alcohol. It was believed that these individuals might be influential in talking to men about their alcohol use or persuading them to change their drinking habits. Participants believed that villagers were usually respectful in front of the chief and “all people attend the meeting while they are sober so it’s easy to advise them on the issue of alcohol.” (1M) Others suggested widespread community-based radio campaigns to disseminate messages on alcohol and ART and interventions to address the social pressures to drink. One man explicitly requested an intervention that “could help me to get away from the friends that pull me to drinking.” (15M) Another man suggested that community-based drama performances could offer a social alternative to drinking alcohol.
At the healthcare system level, participants indicated that alcohol use was infrequently addressed in the clinics, and more communication about alcohol with an HIV care provider would be helpful. Some participants requested that health providers explain more about ART-alcohol interactions and the effect of alcohol on the body. Both women and men communicated clear respect for health providers and took their health advice very seriously. Women expressed hope that support from health providers would be the catalyst for their husbands to stop drinking, such as the woman who said, “I have all hope that when health providers can talk to him he can change because I know that my partner loves me a lot.” (1F)
At the couple level, many women expressed an interest in being involved in an alcohol intervention to help their partners reduce their intake. Around half of women were receptive to a couples-based counseling intervention with providers, which would help them to reinforce alcohol messages with their partners. One woman who was experiencing violence from her husband thought that she had a right to be involved in an intervention because she was a victim of his alcohol abuse, and that couples’ counseling would help them. She and others suggested that providers ask wives if their husbands drink alcohol, and then tell them to come as a couple for counseling at their next HIV care appointment. Other women believed that their husbands would be more comfortable and forthcoming with providers if wives were not present.
Participants expressed different views regarding whether a couple-focused intervention should be offered privately to couples or in a group setting, the latter of which was viewed by some as superior because it could offer peer support. A few participants expressed concerns about a group setting such as a loss of privacy and ineffective group dynamics with men “making noise instead of getting the message.” While other participants believed that a group setting would help facilitate discussion around alcohol and help couples learn from each other.
Discussion
In this study of couples affected by HIV, there was a general belief among participants that alcohol use had an impact on couple relationships and family dynamics, including economic functioning of the household. It is important to note that in our sample of mostly sero-concordant couples, men were the primary drinkers. Participants also described how men’s alcohol use had an impact on ART adherence, consistent with a large body of literature in SSA. Previous research showed that determinants of alcohol use in SSA operate at multiple levels of the socio-ecological model spanning the individual level (e.g., personality traits), social and community level (e.g., peer pressure, social benefits), healthcare level (e.g., advice from healthcare providers), and structural or economic level (e.g., unemployment, to reduce poverty-related stress) [52-54]. Our findings expand on this knowledge by illuminating factors at the couple level, and how other multilevel factors such as peer pressure may affect the couple’s ability to jointly manage men’s alcohol use (see Figure 1).
Table 1 summarizes the main themes presented in this paper, their implications, and suggestions for possible interventions at each level (couple, healthcare, social/community, and structural/economic). At the couple level, we found that most women actively coached their partners to reduce alcohol use, with some having more success than others. Women employed both direct and indirect tactics as a form of social control—an interpersonal interaction that involves influence, regulation, and constraint of health practices [55]. Similar to other research showing that different tactics can vary in their effectiveness, women tried verbally communicating with partners about the dangers of alcohol, providing ultimatums, monitoring a partner’s drinking patterns, providing distractions to prevent drinking, brewing non-alcoholic beer as a substitute, seeking outside support, or praying to God when other strategies failed. Social control practices have consistently predicted better health practices in studies of married couples [56, 57]. Future research with HIV-affected couples in SSA could illuminate new measurement tools and identify the most effective alcohol tactics that women could use to reduce their partner’s alcohol use.
Table 1.
Implications of the findings for multilevel alcohol interventions with couples
| Theme | Level of intervention |
Interpretations | Potential interventions to consider |
|---|---|---|---|
| 1. Couple negotiation around alcohol use and ART | Couple level |
|
|
| 2. Women’s constrained influence on men’s drinking: leveraging other social relationships | Social and community level Healthcare system level |
|
|
| 3. Social influences beyond the couple: the role of friendship and peer pressure | Social and community level |
|
|
| 4. The economic strain of alcohol use on couple relationships and families | Structural and economic level |
|
|
Gender-based power dynamics, at times, circumscribed women’s strategies. Some women delayed communication about alcohol if they believed their safety was at risk, while others simply gave up trying, based on the perception that the gender norms underlying male drinking were too difficult to overcome. Frequently, men’s responses to women’s warnings against alcohol use were similarly rooted in inequitable gender dynamics and men’s privileged position. Arguments over drinking could sometimes lead to conflict, or in many cases, violence. While some men actively listened to their wives’ advice and changed their drinking habits, overall, couples faced formidable challenges in jointly managing men’s alcohol use. Conversations around alcohol could be unproductive or contentious, suggesting that couples might benefit from improvements in their communication and problem-solving skills.
An additional strategy that women employed after seeing no changes in their partners’ drinking was invoking the assistance of outside support from relatives and to a lesser extent, HIV care providers. In recognition of their own limited power, women leveraged more accessible forms sources of social power when a husband was perceived as not fulfilling his family obligations or putting the family at risk [58]. In Malawi, traditional marriage advisors (ankhoswe) who are assigned to the couple at marriage can be an important source of social power for women. A wife who believes she has been unfairly treated can summon her relatives to mediate disputes with her husband—including around alcohol use; although, these strategies can be costly or unhelpful, and sometimes an option of last resort.
Alcohol interventions at the couple level aimed at improving relationship dynamics and increasing skills to effectively coordinate health behaviors have been successful for other HIV-related behaviors [23, 38, 39] and could be adapted for HIV-positive couples with an alcohol drinker. Other alcohol interventions employed outside of Africa such as couples behavioral therapy could provide a useful starting point for developing couple-based alcohol interventions in SSA and have also been shown to reduce IPV [59, 60]. A relationship-skills intervention could include a “gender transformative” component focused on shifting hegemonic norms of masculinity to promote positive forms of masculinity. Gender transformative interventions have been shown to reduce IPV and sexual risk behaviors [61], and could impact alcohol use by shifting harmful gender norms that promote drinking in male groups. In South Africa, qualitative research by Nkosi and colleagues described how men adopting a “health-oriented masculinity” viewed ART adherence as being strong and powerful, and reduced their alcohol intake [29]. Also in South Africa, couple-based interventions that have included gender issues and gender roles for alcohol and other drug use have found modest improvements in gender and power relations [39, 62]. Men could be similarly encouraged to renegotiate their masculine identity around being a good provider and guarding their health, rather than drinking alcohol.
At the healthcare system level, participants expressed a strong interest in receiving alcohol education and counseling in the HIV clinics and described how the influential role of HIV care providers could be leveraged when a partner’s advice was ineffective (Figure 1). Brief alcohol interventions such as the WHO brief intervention [63] are evidence-based, low-cost, and feasible interventions that could be integrated into HIV clinical practice [64] and could be expanded to include partners as a sustainable “booster” who could reinforce alcohol reduction messages at home. Primary partners could provide stronger and more directed social support if involved in clinical efforts and given more information around alcohol and health, and practical tools to help partners reduce drinking. A clinical trial in the US to test a brief intervention that incorporated primary partners was found to be efficacious at reducing prenatal alcohol consumption [65]. However, research from South Africa found that men were reluctant to discuss their alcohol use with HIV care providers and perceived providers as universally condemning alcohol intake [29]. This would indicate that providers should also be educated on approaches that emphasize the importance of non-judgmental communication and patient-centered care before intervening on alcohol.
At the social and community level, we found that men’s motivations for drinking were related to desires for male companionship as well as social pressure from other men (Figure 1). These factors constrained the ability of couples to work collaboratively to reduce men’s alcohol use. However, some men argued that they drank in order to cope with problems in their marriage, meaning that poor couple communication around alcohol may reinforce alcohol use in a cyclical way. Peer pressure was one of the most common explanations given by participants for why men could not reduce their alcohol intake, and some men described how they felt compelled to give in to their friends’ pressure to drink even when they did not want to. This moral conflict or “tug of war” has been noted in other studies on HIV-positive drinkers in Uganda [52]. The formation of peer groups for alcohol users could provide social benefits while also helping men support each other in reducing their alcohol use and maintaining ART adherence.
As suggested by participants, alcohol interventions at the social and community level could involve key opinion leaders such as village chiefs and church leaders who could help to disseminate health messages on alcohol and ART. Given the key role of relatives and ankhoswe in promoting health in families, alcohol interventions could include designated “sponsors” who work with couples to mediate disputes and help couples meet joint goals around alcohol reduction and maintaining family harmony. Community members may first need to be sensitized to the dangers of heavy alcohol consumption to obtain buy-in, given the pervasive role of alcohol in everyday social life, celebrations, and traditions.
Finally, at the structural and economic level, couples described being caught in a vicious cycle of poverty and alcohol abuse (Figure 1). Alcohol use exacerbated the negative effects of poverty on couple and family dynamics. At the same time, men described the stress of living in poverty and boredom due to unemployment as primary reasons for drinking. Women viewed men’s alcohol use as a waste of household resources which limited their ability to improve their households, provide food for the family, invest in small businesses, or further a child’s education. Furthermore, women suffered high rates of physical violence that they believed was linked to men’s alcohol use. Alcohol was also believed to trigger financial troubles in indirect ways by diverting money to extramarital partners, physically limiting men’s ability to engage in productive work, or inciting men’s destruction of household property. These findings contribute to a growing body of literature from non-African settings on alcohol’s harm to others, including communities (e.g., vandalism, property damage, assaults), families (e.g., spousal abuse, child neglect), and workplaces (e.g., accidents, negative interactions with coworkers) [66]. Although it seems intuitive that spouses and close family would be most impacted by a drinker’s alcohol use, little research has documented these effects [67, 68].
Alcohol interventions at the structural and economic level might emphasize the economic advantages of reducing alcohol use, and negative consequences of drinking on household economic development and couple relationships. Few economic interventions have focused on couples or on alcohol use, and such interventions could provide a new opportunity to improve household functioning and health. Providing men with opportunities to earn income and remain productive members of their households may in turn reduce men’s desires to drink due to boredom, the stress of poverty, and feelings of hopelessness in a setting with few employment opportunities. Given women’s complaints around alcohol and household development, this could also reduce couple conflict and tension in the household, and improve relationship functioning. Although this is a new and growing area of research, economic empowerment interventions designed to increase ART adherence provide a promising model. Such interventions can take many forms including food assistance, savings-based interventions, financial training, income-generating activities, micro-credit, and employment support [69]. For example, a systematic review concluded that micro-finance interventions for HIV-positive women have been successful in increasing self-efficacy and ART adherence, reducing intimate partner violence, and increasing savings [70]. Savings and loan associations could encourage redirection of household resources in ways that would help families to meet their economic needs and reduce food insecurity, while also reducing expenditure on alcohol. There is evidence in the literature that savings associations help develop important social bonds, even if members begin as strangers [71].
Limitations
As recruitment depended on a couple having a working cell phone, some couples may have been excluded from the study, such as those who were poorer or lived in more remote rural areas. Thus there is the possibility that this research may not have captured the experiences of certain groups of alcohol-using couples in this part of Malawi. There is also the potential for social desirability bias around alcohol use frequency and severity, as with any study using self-reports. Underreporting could have limited our ability to fully understand the influence of alcohol use on couple relationships, family, and health. This risk is mitigated by the fact that we interviewed both partners and were able to gain a more wholistic account from multiple perspectives. We believe that the portrait of alcohol use among married couples living with HIV in Malawi is accurate; however, our qualitative findings cannot be generalized to other populations of HIV-affected couples—including those who are sero-discordant or not on ART.
Conclusions
In sum, participants described the multitude of ways that alcohol use negatively impacts couple relationships and the different tactics used by partners to address alcohol use in their families. Participants also illuminated multilevel factors that could interfere with or promote couple coordination around alcohol and ART. Finally, we highlighted several novel opportunities to involve primary partners in alcohol reduction interventions for PLHIV. Couples-based approaches were acceptable to many couples in this study and previous research suggests that they would be feasible. Intervention options could include provider-led alcohol counseling for couples, alcohol support groups for couples, relationship-skill building exercises to bolster couple communication and problem-solving skills around alcohol, and economic-strengthening interventions for couples. Couples-based interventions may yield the greatest impact if multiple levels such as social and economic are addressed simultaneously, which could otherwise limit effective couple coordination around alcohol use and ART adherence.
Acknowledgments:
This research was funded by the National Institute of Mental Health (NIMH) under grant K01MH107331 and the National Institute of Allergy and Infectious Diseases under grant P30AI027763 (awards to AAC). AR was funded by the National Institute of Drug Abuse under grant T32DA13911. JYT was funded by the NIMH under grant K01MH106416. JAH was funded by the National Institute of Alcohol Abuse and Alcoholism under grant K24AA022586. The authors would like to thank the tireless efforts of the research staff at Invest in Knowledge in Malawi for data collection.
References
- 1.Scott-Sheldon LA, Walstrom P, Carey KB, et al. Alcohol use and sexual risk behaviors among individuals infected with HIV: a systematic review and meta-analysis 2012 to early 2013. Curr HIV/AIDS Rep. 2013;10(4):314–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.UNAIDS. The Gap Report: Beginning of the End of AIDS. Geneva, Switzerland: UNAIDS; 2014. [Google Scholar]
- 3.World Health Organization. Global status report on alcohol and health. Geneva, Switzerland: World Health Organization; 2014. [Google Scholar]
- 4.World Health Organization. Global Status Report on Alcohol and Health (Country Profiles: Malawi). https://www.who.int/substance_abuse/publications/global_alcohol_report/profiles/mwi.pdf?ua=1 (accessed April 19, 2019). Geneva, Switzerland: 2014. [Google Scholar]
- 5.Hahn JA, Samet JH. Alcohol and HIV disease progression: weighing the evidence. Curr HIV/AIDS Rep. 2010;7(4):226–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Braithwaite RS, Bryant KJ. Influence of alcohol consumption on adherence to and toxicity of antiretroviral therapy and survival. Alcohol Research & Health. 2010;33(3):280. [PMC free article] [PubMed] [Google Scholar]
- 7.Barve S, Kapoor R, Moghe A, et al. Focus on the liver: alcohol use, highly active antiretroviral therapy, and liver disease in HIV-infected patients. Alcohol Research & Health. 2010;33(3):229. [PMC free article] [PubMed] [Google Scholar]
- 8.Hendershot CS, Stoner SA, Pantalone DW, Simoni JM. Alcohol use and antiretroviral adherence: review and meta-analysis. J Acquir Immune Defic Syndr. 2009;52(2):180–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shuper PA, Neuman M, Kanteres F, et al. Causal considerations on alcohol and HIV/AIDS—a systematic review. Alcohol Alcohol. 2010;45(2):159–66. [DOI] [PubMed] [Google Scholar]
- 10.Samet JH, Cheng DM, Libman H, et al. Alcohol consumption and HIV disease progression. Journal of acquired immune deficiency syndromes (1999). 2007;46(2):194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wu ES, Metzger DS, Lynch KG, Douglas SD. Association between alcohol use and HIV viral load. Journal of acquired immune deficiency syndromes (1999). 2011;56(5):e129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Baliunas D, Rehm J, Irving H, Shuper P. Alcohol consumption and risk of incident human immunodeficiency virus infection: a meta-analysis. International journal of public health. 2010;55(3):159–66. [DOI] [PubMed] [Google Scholar]
- 13.Rusbult C, Arriaga X. Interdependence theory In: Duck S, editor. Handbook of personal relationships. 2nd ed. London, UK: Wiley; 1997. [Google Scholar]
- 14.Rodriguez LM, Neighbors C, Knee CR. Problematic alcohol use and marital distress: An interdependence theory perspective. Addiction Research & Theory. 2014;22(4):294–312. [Google Scholar]
- 15.Marshal MP. For better or for worse? The effects of alcohol use on marital functioning. Clin Psychol Rev. 2003;23(7):959–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Levitt A, Cooper ML. Daily alcohol use and romantic relationship functioning: Evidence of bidirectional, gender-, and context-specific effects. Personality and Social Psychology Bulletin. 2010;36(12):1706–22. [DOI] [PubMed] [Google Scholar]
- 17.Leonard KE, Rothbard JC. Alcohol and the marriage effect. Journal of studies on Alcohol, supplement. 1999(13):139–46. [DOI] [PubMed] [Google Scholar]
- 18.Leddy A, Chakravarty D, Dladla S, Bruyn Gd, Darbes L. Sexual communication self-efficacy, hegemonic masculine norms and condom use among heterosexual couples in South Africa. AIDS Care. 2015;28(2):228–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rogers AJ, Achiro L, Bukusi EA, et al. Couple interdependence impacts HIV-related health behaviours among pregnant couples in southwestern Kenya: a qualitative analysis. J Int AIDS Soc. 2016;19(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Conroy AA. The Influence of Relationship Power Dynamics on HIV Testing in Rural Malawi. J Sex Res. 2014;52(3):347–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Conroy AA. ‘It means there is doubt in the house’: Perceptions and experiences of HIV testing in rural Malawi. Culture Health & Sexuality. 2014;16(4): 397–411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Turan JM, Darbes LA, Musoke PL, et al. Development and Piloting of a Home-Based Couples Intervention During Pregnancy and Postpartum in Southwestern Kenya. AIDS Patient Care STDS. 2018;32(3):92–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Darbes LA, McGrath NM, Hosegood V, et al. Results of a couples-based randomized controlled trial aimed to increase testing for HIV. JAIDS Journal of Acquired Immune Deficiency Syndromes. 2019;80(4):404–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Conroy AA, Wong LH. How reliable are self-reports of HIV status disclosure? Evidence from couples in Malawi. Soc Sci Med. 2015;144:28–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Conroy A, Ruark A, Darbes L, et al. Relationship dynamics and dyadic coordination are associated with ART adherence among married couples from Malawi. Paper presented at the Conference on HIV Treatment and Prevention Adherence; 8–10 June 2018 Miami2018. [Google Scholar]
- 26.Conroy A, Leddy A, Johnson M, et al. ‘I told her this is your life’: relationship dynamics, partner support and adherence to antiretroviral therapy among South African couples. Culture, Health & Sexuality. 2017;19(11):1239–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kalichman SC, Simbayi LC, Kaufman M, Cain D, Jooste S. Alcohol Use and Sexual Risks for HIV/AIDS in Sub-Saharan Africa: Systematic Review of Empirical Findings. Prev Sci. 2007;8:141–51. [DOI] [PubMed] [Google Scholar]
- 28.Conroy AA, Mckenna SA, Ruark A. Couple interdependence impacts alcohol use and adherence to antiretroviral therapy in Malawi. AIDS Behav. 2019;23(1):201–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nkosi S, Rich EP, Kekwaletswe CT, Morojele NK. Experiences of alcohol consumption and taking antiretroviral medication among men living with HIV in Tshwane, South Africa. Afr J AIDS Res. 2016;15(4):367–76. [DOI] [PubMed] [Google Scholar]
- 30.Fatch R, Emenyonu NI, Muyindike W, et al. Alcohol Interactive Toxicity Beliefs and ART Non-adherence Among HIV-Infected Current Drinkers in Mbarara, Uganda. AIDS Behav. 2016:1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Conroy AA, McKenna SA, Leddy A, et al. “If She is Drunk, I Don’t Want Her to Take it”: Partner Beliefs and Influence on Use of Alcohol and Antiretroviral Therapy in South African Couples. AIDS Behav. 2017;21(7):1885–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Scott-Sheldon LA, Carey KB, Johnson BT, Carey MP, Team MR. Behavioral interventions targeting alcohol use among people living with HIV/AIDS: a systematic review and meta-analysis. AIDS Behav. 2017;21(2):126–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wandera B, Tumwesigye NM, Nankabirwa JI, et al. Efficacy of a single, brief alcohol reduction intervention among men and women living with HIV/AIDS and using alcohol in Kampala, Uganda: a randomized trial. Journal of the International Association of Providers of AIDS Care (JIAPAC). 2017;16(3):276–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bachanas P, Kidder D, Medley A, et al. Delivering prevention interventions to people living with HIV in clinical care settings: results of a cluster randomized trial in Kenya, Namibia, and Tanzania. AIDS Behav. 2016;20(9):2110–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Senyonyi RM, Underwood LA, Suarez E, Musisi S, Grande TL. Cognitive behavioral therapy group intervention for HIV transmission risk behavior in perinatally infected adolescents. Health (N Y). 2012;4(12):1334. [Google Scholar]
- 36.Papas RK, Sidle JE, Gakinya BN, et al. Treatment outcomes of a stage 1 cognitive–behavioral trial to reduce alcohol use among human immunodeficiency virus‐infected out‐patients in western Kenya. Addiction. 2011;106(12):2156–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Papas RK, Sidle JE, Martino S, et al. Systematic cultural adaptation of cognitive-behavioral therapy to reduce alcohol use among HIV-infected outpatients in western Kenya. AIDS Behav. 2010;14(3):669–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Remien RH, Stirratt MJ, Dolezal C, et al. Couple-focused support to improve HIV medication adherence: a randomized controlled trial. AIDS. 2005;19:807–14. [DOI] [PubMed] [Google Scholar]
- 39.Speizer IS, Zule WA, Carney T, et al. Changing sex risk behaviors, gender norms, and relationship dynamics among couples in Cape Town, South Africa: Efficacy of an intervention on the dyad. Soc Sci Med. 2018;209:95–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Weiser SD, Palar K, Frongillo EA, et al. Longitudinal assessment of associations between food insecurity, antiretroviral adherence and HIV treatment outcomes in rural Uganda. AIDS. 2014;28:115–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kagee A, Remien RH, Berkman A, et al. Structural barriers to ART adherence in Southern Africa: challenges and potential ways forward. Global Public Health. 2011;6(1):83–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.O’farrell TJ, Murphy CM. Marital violence before and after alcoholism treatment. J Consult Clin Psychol. 1995;63(2):256. [DOI] [PubMed] [Google Scholar]
- 43.Fals-Stewart W, Birchler GR, Kelley ML. Learning sobriety together: A randomized clinical trial examining behavioral couples therapy with alcoholic female patients. J Consult Clin Psychol. 2006;74(3):579. [DOI] [PubMed] [Google Scholar]
- 44.Wechsberg WM, Zule WA, El-Bassel N, et al. The male factor: Outcomes from a cluster randomized field experiment with a couples-based HIV prevention intervention in a South African township. Drug Alcohol Depend. 2016;161:307–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wechsberg WM, El-Bassel N, Carney T, et al. Adapting an evidence-based HIV behavioral intervention for South African couples. Substance abuse treatment, prevention, and policy. 2015;10(1):6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Brofenbrenner U The Ecology of Human Development Cambridge, MA: Harvard University Press; 1979. [Google Scholar]
- 47.Karney BR, Hops H, Redding CA, et al. A Framework for Incorporating Dyads in Models of HIV-Prevention. AIDS Behav. 2010;14(2):189–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bush K, Kivlahan D, McDonell M, Fihn S, Bradley K. The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Arch Intern Med. 1998;158:1789–95. [DOI] [PubMed] [Google Scholar]
- 49.Conroy AA, McKenna SA, Comfort ML, et al. Marital infidelity, food insecurity, and couple instability: A web of challenges for dyadic coordination around antiretroviral therapy. Soc Sci Med. 2018;214:110–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Eisikovits Z, Koren C. Approaches to and outcomes of dyadic interview analysis. Qual Health Res. 2010;20(12):1642–55. [DOI] [PubMed] [Google Scholar]
- 51.Spencer L, Ritchie J. Qualitative data analysis for applied policy research. Analyzing qualitative data: Routledge; 2002. p. 187–208. [Google Scholar]
- 52.Sundararajan R, Wyatt MA, Woolf-King S, et al. Qualitative study of changes in alcohol use among HIV-infected adults entering care and treatment for HIV/AIDS in rural southwest Uganda. AIDS Behav. 2015;19(4):732–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Woolf-King SE, Maisto SA. Alcohol use and high-risk sexual behavior in Sub-Saharan Africa: a narrative review. Arch Sex Behav. 2011;40(1):17–42. [DOI] [PubMed] [Google Scholar]
- 54.Kalichman SC, Simbayi L, Jooste S, Vermaak R, Cain D. Sensation seeking and alcohol use predict HIV transmission risks: prospective study of sexually transmitted infection clinic patients, Cape Town, South Africa. Addict Behav. 2008;33(12):1630–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lewis MA, Butterfield RM. Social Control in Marital Relationships: Effect of One’s Partner on Health Behaviors 1. J Appl Soc Psychol. 2007;37(2):298–319. [Google Scholar]
- 56.Umberson D Gender, marital status, and the social control of health behavior. Soc Sci Med. 1992;34(8):907–17. [DOI] [PubMed] [Google Scholar]
- 57.Lewis MA, Rook KS. Social control in personal relationships: Impact on health behaviors and psychological distress. Health Psychol. 1999;18(1):63. [DOI] [PubMed] [Google Scholar]
- 58.Tan JY, Conroy A, Lee I, Pratto F. Leveraging Power in Intimate Partner Relationships A Power Basis Perspective: Cambridge University Press; Cambridge, UK; 2017. [Google Scholar]
- 59.Fals-Stewart W, Clinton-Sherrod M. Treating intimate partner violence among substance-abusing dyads: The effect of couples therapy. Professional Psychology: Research and Practice. 2009;40(3):257. [Google Scholar]
- 60.Klostermann KC, Fals-Stewart W. Intimate partner violence and alcohol use: Exploring the role of drinking in partner violence and its implications for intervention. Aggression and Violent Behavior. 2006;11(6):587–97. [Google Scholar]
- 61.Dworkin SL, Treves-Kagan S, Lippman SA. Gender-transformative interventions to reduce HIV risks and violence with heterosexually-active men: A review of the global evidence. AIDS Behav. 2013;17(9):2845–63. [DOI] [PubMed] [Google Scholar]
- 62.Minnis AM, Doherty IA, Kline TL, et al. Relationship power, communication, and violence among couples: results of a cluster-randomized HIV prevention study in a South African township. International journal of women’s health. 2015;7:517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Babor TF, Higgins-Biddle JC, Organization WH. Brief intervention for hazardous and harmful drinking: a manual for use in primary care. 2001. [Google Scholar]
- 64.Kaner EF, Dickinson HO, Beyer F, et al. The effectiveness of brief alcohol interventions in primary care settings: a systematic review. Drug and alcohol review. 2009;28(3):301–23. [DOI] [PubMed] [Google Scholar]
- 65.Chang G, McNamara TK, Orav EJ, et al. Brief intervention for prenatal alcohol use: a randomized trial. Obstet Gynecol. 2005;105(5 Pt 1):991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Karriker-Jaffe KJ, Room R, Giesbrecht N, Greenfield TK. Alcohol’s harm to others: Opportunities and challenges in a public health framework. Journal of studies on alcohol and drugs. 2018;79(2):239–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Velleman R, Orford J. Young adult offspring of parents with drinking problems: Recollections of parents’ drinking and its immediate effects. Br J Clin Psychol. 1990;29(3):297–317. [DOI] [PubMed] [Google Scholar]
- 68.Christoffersen MN, Soothill K. The long-term consequences of parental alcohol abuse: a cohort study of children in Denmark. J Subst Abuse Treat. 2003;25(2):107–16. [DOI] [PubMed] [Google Scholar]
- 69.Swann M Economic strengthening for retention in HIV care and adherence to antiretroviral therapy: a review of the evidence. AIDS Care. 2018;30(sup3):85–98. [DOI] [PubMed] [Google Scholar]
- 70.Arrivillaga M, Salcedo JP. A systematic review of microfinance-based interventions for HIV/AIDS prevention. AIDS Educ Prev. 2014;26(1):13–27. [DOI] [PubMed] [Google Scholar]
- 71.Wagner G, Rana Y, Linnemayr S, Balya J, Buzaalirwa L. A qualitative exploration of the economic and social effects of microcredit among people living with HIV/AIDS in Uganda. AIDS Res Treat. 2012;2012. [DOI] [PMC free article] [PubMed] [Google Scholar]