Abstract
Organisms respond to tissue damage through the upregulation of protective responses which restore tissue structure and metabolic function. Mitochondria are key sources of intracellular oxidative metabolic signals that maintain cellular homeostasis. Here we report that tissue and cellular wounding triggers rapid and reversible mitochondrial fragmentation. Elevated mitochondrial fragmentation either in fzo-1 fusion-defective mutants or after acute drug treatment accelerates actin-based wound closure. Wounding triggered mitochondrial fragmentation is independent of the GTPase DRP-1 but acts via the mitochondrial Rho GTPase MIRO-1 and cytosolic Ca2+. The fragmented mitochondria and accelerated wound closure of fzo-1 mutants are dependent on MIRO-1 function. Genetic and transcriptomic analyzes show that enhanced mitochondrial fragmentation accelerates wound closure via the upregulation of mtROS and Cytochrome P450. Our results reveal how mitochondrial dynamics respond to cellular and tissue injury and promote tissue repair.
Subject terms: Mitochondria, Developmental biology
Mitochondria are important organelles that generate and respond to signals to maintain cellular homeostasis. Here the authors show that wounding triggers GTPase MIRO-1- and calcium-dependent mitochondrial fragmentation, which aids tissue wound repair through cytochrome P450 and mitochondrial reactive oxygen species.
Introduction
Mitochondria are highly dynamic organelles organized in sophisticated intracellular networks linked to their physiological roles1. Mitochondria can rapidly and transiently change their morphology in response to environmental changes, altering their function in energy production, Ca2+ homeostasis, redox signaling, and metabolism2. Disrupted mitochondrial morphology is associated with many human diseases, including heart failure, neurodegenerative disorders, and cancer1.
Fusion and fission of mitochondrial membranes are coordinated. The balance between fusion and fission determines the shape, size, and connectedness of mitochondria, accounting for the variation in mitochondrial morphology in different cell types3. The core regulators of these dynamic transitions are highly conserved dynamin-like guanosine triphosphatases (GTPases)4. Mitochondrial fission is conducted by the dynamin-related protein 1(DRP1), which is recruited to the mitochondrial surface in response to a variety of cues5–8. A sophisticated fission-machinery, including DRP1-specific adapters, actin nucleating proteins9, and myosin10, assemble at contact sites between the endoplasmic reticulum and mitochondria. A recent finding indicates that Ca2+ signals can regulate a rapid mitochondrial shape transition (MiST) through DRP-1 independent but MIRO-1-dependent way11. Fusion, in contrast, is executed by the Mitofusins 1/2 (MFN1/2) and OPA1, which drive outer and inner mitochondrial membrane fusion, respectively4.
Fusion contributes to mitochondrial maintenance, whereas fission causes mitochondrial fragmentation, which allows removal of irreversibly damaged mitochondria by mitophagy12. Fragmentation of the mitochondrial network occurs in response to cellular stress and during cell death2. Although mitochondrial fragmentation can cause mitochondrial dysfunction in disease, mitochondrial fragmentation also plays a positive role. For example, mitochondrial fragmentation promotes continued clearance of apoptotic cells by macrophages13, accelerates cell proliferation14, and regulates systemic glucose homeostasis15. However, the mechanisms by which fragmented mitochondria protect against cellular stresses is not clear.
Tissue injury induces coordinated responses that allow for efficient wound repair, which is important for animal survival and reproduction. For example, in different species including mammals, wounding activates intracellular, and intercellular transcriptional growth factor and chemokine cascades that regulate gene expression during tissue repair16,17. Cellular and tissue injury also triggers multiple damage signals, such as Ca2+, reactive oxygen species (ROS), and ATP, which control transcription-independent wound responses to restore cellular architecture and function18–25. Studies in a variety of organisms suggest mitochondrial ROS (mtROS) signals can promote tissue repair26–30. However, the physiological roles of mitochondria in tissue damage responses and repair have not been extensively characterized.
Here we report that wounding C. elegans epithelial cells triggers rapid and reversible mitochondrial fragmentation, a process we refer to as wounding-induced mitochondrial fragmentation (WIMF). We show that enhanced mitochondrial fragmentation accelerates wound closure in vivo. WIMF is independent of the canonical DRP-1 mediated mitochondrial fission pathway but is dependent on wound-induced Ca2+ influx and the mitochondrial Rho GTPase MIRO-1. We define a protective mechanism initiated from mitochondrial fragmentation, which functions through the upregulation of mtROS and cytochrome P450 to promote wound closure. Our studies reveal a critical role for mitochondrial morphology in response to and promoting tissue repair.
Results
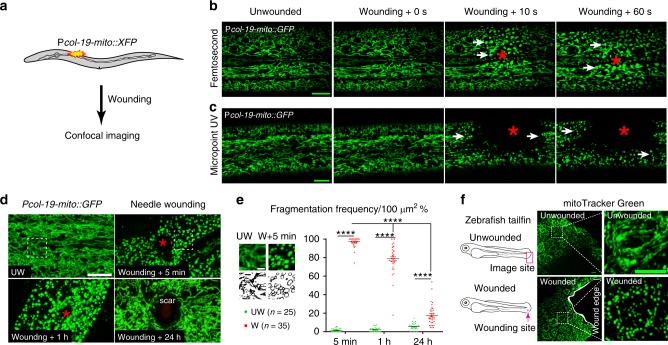
Tissue wounding induces rapid and reversible mitochondrial fragmentation
We visualized mitochondrial responses to acute skin wounding in C. elegans (Fig. 1a). In the lateral epidermis of late L4 or young adult animals, mitochondria are threadlike, forming elaborate branched networks that are stable over periods of tens of seconds (Fig. 1b, Supplementary Fig. 1a; Supplementary Movie 1). We observed rapid alterations in the morphology of the epidermal mitochondrial network after wounding (Fig. 1b–e). Laser wounding destroyed the local mitochondrial network within seconds (Fig. 1b, c); over the next 5–10 min, the surrounding mitochondria changed tubular shape to fragmented within 50–70 μm of the wound site (Supplementary Movies 1 and 2).
Fig. 1. Wounding triggers rapid and reversible mitochondrial fragmentation.
a Experimental design to investigate the mitochondrial response to epidermal wounding (laser or physical damage) in C. elegans. Mitochondria were labeled with matrix targeting sequence from cox 8 (mito) fused with XFP (including Pcol-19-mito::GFP(juEx4796), Phpy-7(y37a1b.5)-mito::GFP(yqIs157)70, Pcol-19-mito::mKate2(zjuSi47), or Pcol-19-mito::dendra2(juSi271)). b, c Laser wounding induces mitochondrial fragmentation in the epidermis. Representative confocal images of the epidermal mitochondrial network before and seconds after wounding by femtosecond laser (b) (see also Supplementary Movie 1, N = 5 independent experiments) and Micropoint UV laser (c) (see also Supplementary Movie 2, N = 7 independent experiments). Pcol-19-mito::GFP(juEx4796) was used to label mitochondria. We define mitochondrial fragmentation as a change from the interconnected tubular structure network to a rounded shape. d Mechanical needle wounding causes fragmentation of epidermal mitochondria, which return to normal morphology 24 hours after wounding except for a scar region at the center of the wound site. Representative confocal images of epidermal mitochondria before and after needle wounding. N = 3 independent experiments. Pcol-19-mito::GFP(juEx4796) was used to label mitochondria. Red asterisks in b–d indicate the wound site. White dashed squares indicate the zoom-in images for panel e. Scale bars b–d, 10 μm. e Quantitation of mitochondrial fragmentation frequency after needle wounding, measured in 100 μm2 regions of interest (white dash square in panel d) 10 μm adjacent to the wound site. Top panel shows enlarged images of mitochondria in unwounded (UW, n = 25) and wounded (W, n = 35) epidermis. Scale bars, 5 μm. Bars indicate mean ± SEM. ****P < 0.0001, Two-tailed unpaired t-test for wounded animals. Source data are provided as a Source Data file. f Wounding induce mitochondrial fragmentation in zebrafish tail fin. Left, experimental design for zebrafish tail fin wounding, 3 dpf larvae were first stained with mitoTracker Green for 2 h and then were wounded using needle. N = 3 independent experiments. Right, representative confocal image of mitochondria at the edge of zebrafish tail fin, Scale bar, 10 μm.
Epidermal mitochondrial fragmentation was also observed after needle wounding, both in the wounded syncytial epidermis (hyp7) and adjacent seam cells (Fig. 1d, Supplementary Fig. 1b). Mitochondria remained fragmented for several hours and returned to normal morphology and network by 24 hours post-wounding (Fig. 1d, e). Either needle or femtosecond laser triggered rapid fragmentation within 50 ± 10 μm of the wound site, while Micropoint UV wounding increased the fragmented region than a needle or femtosecond laser wounding (Supplementary Fig. 1c, d; Supplementary Movies 1 and 2). Together, these data show that wounded C. elegans epidermis displays a rapid and reversible change in mitochondrial morphology that we term wounding induced mitochondrial fragmentation (WIMF).
To investigate whether WIMF occurs in other tissue and cellular wound responses, we wounded the tail fin in zebrafish larvae and found widespread mitochondrial fragmentation around the wound edge 5 min after injury (Fig. 1f). We also observed similar mitochondrial fragmentation 5 min after scratch wounding of a monolayer of U2OS cells at the wounding edge (Supplementary Fig. 1e, f), suggesting WIMF is a general subcellular response to tissue wounding.
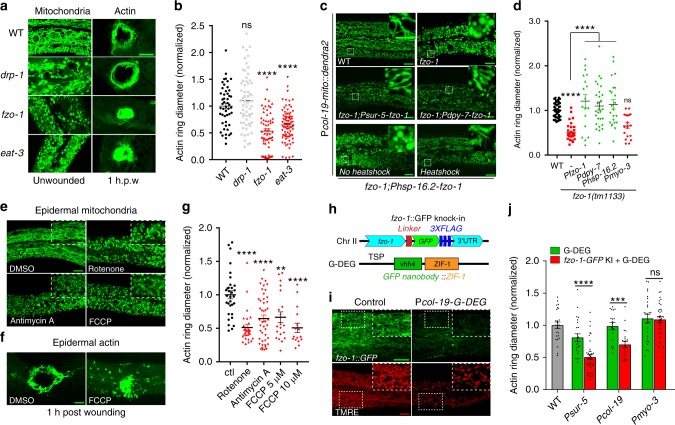
Chronic and acute induction of mitochondrial fragmentation accelerates epidermal wound closure
To investigate the function of mitochondrial fragmentation in epidermal wound repair, we examined actin-mediated wound closure23. The ring of actin polymerization at the wound site is surrounded by fragmented mitochondria (Supplementary Fig. 2a, Supplementary Movie 3). In C. elegans, mitochondrial fusion requires the outer membrane protein FZO-1 (orthologous to human MFN1/2) and the inner membrane protein EAT-3 (orthologous to human Opa1)31; fission requires the cytosolic protein DRP-1 (orthologous to human Drp1)5. fzo-1 and eat-3 null mutants are defective in mitochondrial fusion and display chronic mitochondrial fragmentation (Fig. 2a). Surprisingly, these animals displayed faster wound closure compared to the wild type (WT) (Fig. 2a, b, Supplementary Fig. 2b, c, Supplementary Movie 4). Conversely, loss of function in drp-1, which causes chronic mitochondrial elongation, did not significantly impair wound closure (Fig. 2a, b, Supplementary Fig. 2c). Depleting the mitochondrial fusion gene not only induces mitochondrial fragmentation but also results in defective ETC activity32,33. We observed that the oxygen consumption rate (OCR) was significantly reduced in fzo-1 and eat-3 as well as in drp-1 mutants (Supplementary Fig. 2f), suggesting the enhanced wound closure is not due to the reduced ETC activity. All these mitochondrial mutants showed normal survival post-wounding (Supplementary Fig. 2d, e). Expression of fzo-1 genomic DNA under the control of its own promoter or heat-shock promoter rescued fzo-1 mutant mitochondrial morphology and restored wound closure rates to normal (Fig. 2c, d).
Fig. 2. Enhanced mitochondrial fragmentation accelerates wound closure.
a Left, representative confocal images of mitochondria in WT and mutants; right, representative images of F-actin ring assembly (Pcol-19-GFP::moesin(juIs352)) at 1 h.p.w. (hour post-wounding). N = 4 independent experiments. b Quantitation of actin ring diameter in wounded animals (WT, n = 49; drp-1, n = 61; fzo-1, n = 62; eat-3, n = 79 animals). Bars indicate mean ± SEM, normalized to WT. ****P < 0.0001 (versus WT), One-way ANOVA, Dunnett’s post test. c Representative images of mitochondria in fzo-1(tm1133) or tissue-specific rescued strains. d Quantitation of actin ring diameter (WT, n = 51; fzo-1, n = 35; fzo-1;Pfzo-1-fzo-1, n = 18; fzo-1;Pdpy-7-fzo-1, n = 28; fzo-1;Phsp-16.2-fzo-1, n = 23; fzo-1;Pmyo-3-fzo-1, n = 23 animals) at 1 h.p.w. Bars indicate mean ± SEM. ****P < 0.0001 (versus fzo-1), One-way ANOVA Dunnett’s test. Two-tailed unpaired t-test for fzo-1 and WT animals. e Left top, representative images of mitochondria morphology. Rotenone (100 μM), antimycin A (100 μM). and FCCP (10 μM). f Actin ring formation after wounding. N = 3 independent experiments (e, f). g Quantitation of actin ring diameter in WT and drug treated animals (Ctl, n = 31; Rotenone, n = 28; antimycin A, n = 33; FCCP 5 μM, n = 20; FCCP 10 μM, n = 16 animals) at 1 h.p.w. Bars indicate mean ± SEM. **P = 0.016, ****P < 0.0001 (versus ctl), One-way ANOVA Dunnett’s test. h A scheme of fzo-1::GFP(zju136) and GFP nanobody mediated degradation system (G-DEG). i Representative images of fzo-1::GFP expression in animals with or without G-DEG. N = 3 independent experiments. j Quantitation of actin ring diameter after tissue-specific knockdown of fzo-1 (WT, n = 25; Psur-5;G-DEG, n = 39; Psur-5;G-DEG;fzo-1, n = 24; Pcol-19;G-DEG, n = 21; Pcol-19;G-DEG;fzo-1, n = 18; Pmyo-3;G-DEG, n = 26; Pmyo-3;G-DEG;fzo-1, n = 35 animals). Bars indicate mean ± SEM. ns, P = 0.8508, ***P = 0.0004, ****P < 0.0001, Two-tailed unpaired t-test. Scale, 10 μm (a, c, e, f, and i) and 5 μm (zoom-in c, e, and i). Source data are provided as a Source Data file.
To further test the role of mitochondrial fragmentation in wound closure, we treated WT animals with drugs that induce mitochondrial fragmentation through the inhibition of electron transport chain (ETC)34. In total, 2 hours treatment of young adult animals with either rotenone or antimycin A induced mitochondrial fragmentation (Fig. 2e) and accelerated actin-based wound closure (Fig. 2g). Moreover, acute treatment with Carbonyl cyanide-4-(trifluoromethoxy) phenylhydrazone (FCCP) before wounding, which also induces mitochondrial fragmentation (Fig. 2e), significantly accelerated wound closure 1 h.p.w. (Fig. 2f, g). Thus, chronic or acute mitochondrial fragmentation can accelerate epidermal wound closure.
Mitochondrial fragmentation accelerates epidermal wound closure cell-autonomously
We next examined whether mitochondrial fragmentation promotes wound closure in a cell-autonomous or cell-nonautonomous way by tissue-specific knockdown of fzo-1 using the GFP nanobody mediated protein degradation (G-DEG) system (Fig. 2h)35. fzo-1::GFP knock-in animals showed interconnected tubular mitochondrial morphology and normal wound closure (Fig. 2i). Expression of G-DEG either ubiquitously or specifically in the adult epidermis reduced the FZO-1::GFP signal and caused mitochondrial fragmentation (Fig. 2i). Moreover, these animals displayed accelerated wound closure 1 hour after injury (Fig. 2j). In contrast, the expression of G-DEG in muscles did not affect epidermal wound closure (Fig. 2j). Epidermal specific expression of fzo-1 rescued fragmented mitochondria and suppressed faster wound closure in fzo-1(tm1133) animal (Fig. 2c,d). However, muscle expression of fzo-1 could not suppress the enhanced wound closure in fzo-1(tm1133) animal (Fig. 2d). Collectively, these results show that mitochondrial fragmentation acts cell-autonomously in wound closure.
WIMF is independent of canonical mitochondrial fission regulators
To define how mitochondrial fragmentation enhances wound closure, we first examined how wounding triggers mitochondrial fragmentation. DRP-1 is essential for most mitochondrial fission5. Animals lacking drp-1 displayed constitutively fused epidermal mitochondria that nevertheless fragmented after wounding (Supplementary Fig. 3a, Supplementary Movie 5). To compare the effects of WIMF, we quantified the farthest extent of mitochondrial fragmentation from the wound site (Supplementary Fig. 3b). Loss of function of drp-1 increased the extent of WIMF compared to the WT (Supplementary Fig. 3b, c, Supplementary Movie 5), suggesting WIMF may be negatively regulated by DRP-1. Conversely, in fzo-1 and eat-3 mutants mitochondria are constitutively fragmented and swollen36,37 (Supplementary Fig. 3d), and did not appreciably change in morphology after needle or laser wounding (Supplementary Fig. 3d). Furthermore, the expression and overall localization of DRP-1 were not changed in a few mins after wounding (Supplementary Fig. 3e).
We tested whether other regulators of mitochondrial morphology were required for WIMF. Mitochondrial dynamics are regulated by DRP-1 adapters, actin nucleating factors and also apoptotic components9,10,31,38. However, WIMF still occurred in these loss-of-function mutants (Supplementary Fig. 3f–h, details in the supplementary information). Actin polymerization and myosin affect mitochondrial fission in other systems9,10; however, drug treatments inhibiting either actin polymerization or non-muscle myosin, and loss of function of actin regulators did not block WIMF (Supplementary Fig. 4a–e). Together, these results suggest that WIMF does not require DRP-1 or other known regulators of mitochondrial morphology.
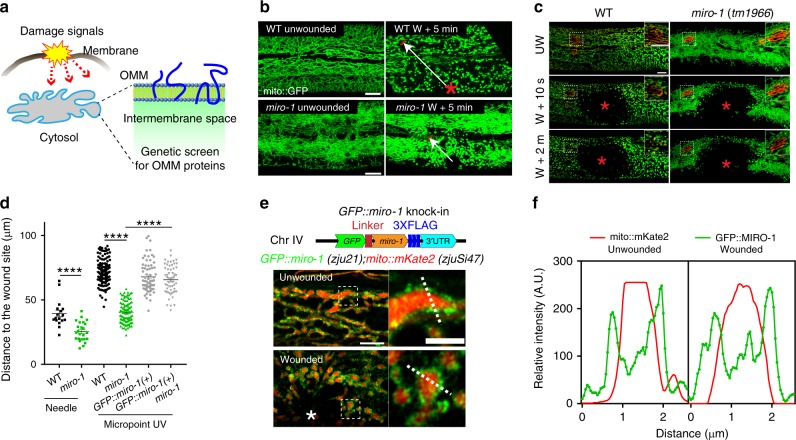
WIMF spreading is dependent on mitochondrial Rho GTPase MIRO-1
We then sought regulators of WIMF by a targeted candidate screen. We hypothesized that fragmentation signals might be sensed by the outer mitochondrial membrane (OMM) proteins (Fig. 3a). We screened ~170 predicted OMM proteins by RNAi, most of which displayed normal epidermal mitochondrial morphology and became fragmented after wounding (Supplementary Table 4). However, RNAi knockdown of the mitochondrial Rho GTPase miro-1 caused epidermal mitochondria to become straight and aligned, losing their typical interconnected network structure (Fig. 3b, Supplementary Fig. 5a). Moreover, in miro-1 null mutants, WIMF is tightly restricted to the injury site (Fig. 3b, d), indicating miro-1 is involved in the spread of WIMF. To confirm this, we performed laser wounding on mitochondria labeled with mito::dendra2, which can be locally converted to red fluorescence by photoconversion, making it possible to examine the morphology of single mitochondria (Fig. 3c, Supplementary Fig. 5a, Supplementary Movie 6). The distance of WIMF was reduced in miro-1(tm1966) mutants after wounding (Fig. 3c, d).
Fig. 3. WIMF is dependent on mitochondrial Rho GTPase MIRO-1.
a Diagram of a genetic screen for outer mitochondrial membrane (OMM) proteins involved in WIMF. The candidate genes and mitochondrial morphological phenotype before and after wounding are listed in Supplementary Table 4. b Representative confocal images of epidermal mitochondria before and after needle wounding. N = 5 independent experiments. Arrows indicate the farthest extent of fragmented mitochondria from the wound site, which we used for the quantitation of distance of mitochondrial fragmentation. c Representative confocal images of epidermal mitochondria before and after Micropoint UV laser wounding (see also Supplementary Movie 6). Mitochondria were labeled by Pcol-19-mito::dendra2(juSi271) (b, c). Red mitochondria were photo-converted with a 405-nm laser. N = 3 independent experiments. Note WIMF is restricted to the injury site and does not spread to adjacent mitochondria in miro-1(tm1966) mutants. Scale bars (b, c), 10 μm. d Quantitation of the distance of fragmented mitochondria to the wound site after needle or Micropoint UV wounding in miro-1(tm1966) and rescued animals (WT-needle, n = 17; miro-1-needle, n = 24; WT-laser, n = 144; miro-1-laser, n = 99; GFP::miro-1( + )-laser, n = 68; miro-1; GFP::miro-1( + )-laser, n = 56 animals). Typically, we generated 20 arrows, as shown in panel b and averaged for each animal, see detail in methods. Bars indicate mean ± SEM. ****P < 0.0001, Two-tailed unpaired t-test. Source data are provided as a Source Data file. e Localization of GFP::MIRO-1 before and after needle wounding. Top, diagram of GFP::miro-1 knock-in strategy. Bottom, representative confocal image of Pcol-19-GFP::miro-1(zju21); Pcol-19-mito::mKate2(zjuSi47) (see also Supplementary Movie 7). GFP::MIRO-1 is localized around mito::mKate2 and was remained at the wounding site immediately after wounding. Scale bar, 5 μm and 2 μm (zoom-in). N = 2 independent experiments. f Fluorescence profiles from line scan 1 and 2 illustrate the presence of GFP::MIRO-1 on a section of the mitochondrial membrane before and after needle wounding. A.U. arbitrary units. Images representative of five animals. Note, the GFP signal surrounds the mitochondrial matrix mito::mKate2 signal.
MIRO-1 is an outer mitochondrial membrane protein that functions as an adapter for microtubule-mediated transport39. GFP::MIRO-1 fusion protein was localized external to the mitochondrial matrix (Fig. 3e, Supplementary Fig. 5b) and partially co-localized with the outer mitochondrial membrane protein Tomm-20 (Supplementary Fig. 5c). After wounding, GFP::MIRO-1 localized to the wounding site and encircled the mitochondria matrix (Fig. 3e, f, Supplementary Fig. 5b, c, Supplementary Movie 7). Expression of WT miro-1 genomic DNA specifically in the epidermis rescued the mitochondrial morphology in miro-1(tm1966) mutant, as did a constitutively active (CA) version of MIRO-1, but not MIRO-1 dominant-negative (DN) or EF-hand mutation (Supplementary Fig. 5d)40. Moreover, WIMF was also restored in miro-1 mutant with the expression of miro-1 genomic DNA in the epidermis (Fig. 3d). Thus, the outer mitochondrial membrane protein MIRO-1 is required for WIMF.
Wounding-induced microtubule depolymerization is not required for WIMF
MIRO-1 is a crucial regulator of mitochondrial motility and distribution along the microtubule in many cell types39,41. Microtubule stabilization also plays critical roles in wound closure42. We thus examined whether WIMF might involve altered microtubule dynamics after wounding. In the unwounded epidermis, mitochondria and microtubules were closely associated and relatively stable over periods of several minutes (Supplementary Fig. 4f, Supplementary Movie 8). In miro-1(tm1966) mutant mitochondria were more localized to the perinuclear region (Supplementary Fig. 4f); however, microtubule distribution and dynamic were normal (Supplementary Fig. 4f, Supplementary Movie 8), suggesting loss of function in miro-1 does not affect epidermal microtubule dynamics.
We found wounding triggers not only immediate mitochondrial fragmentation but also rapid local microtubule depolymerization (Supplementary Fig. 4g, Supplementary Movie 9). Moreover, mitochondrial fragmentation happens before microtubule depolymerization (Supplementary Fig. 4g). miro-1 mutants displayed normal microtubule depolymerization in response to wounding but more restricted mitochondrial fragmentation (Supplementary Fig. 4g Supplementary Movie 10). Treatment of young adult animals with Taxol or Colchicine, which stabilize and destabilize microtubule respectively, did not affect either mitochondrial morphology or WIMF (Supplementary Fig. 4h). Furthermore, knock out of microtubule dynamics regulators Kinesin/KLP-7 and PTRN-1 had no apparent effects on WIMF (supplementary Fig. 4i). Thus, microtubule stability or dynamics is not necessary for MIRO-1 regulated WIMF.
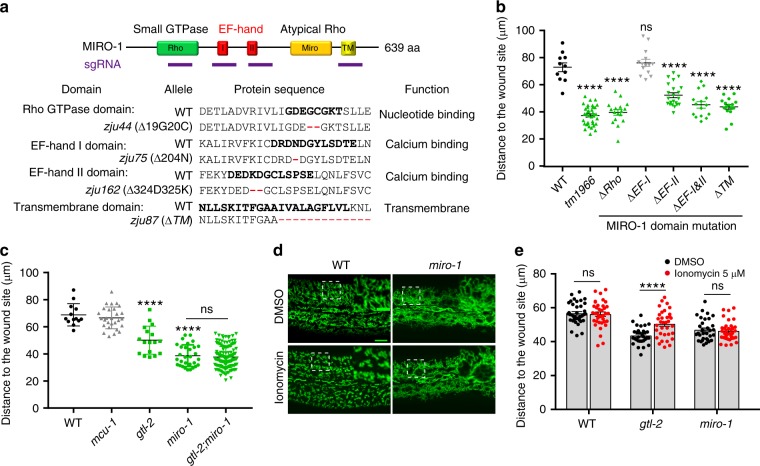
Ca2+-MIRO-1 signaling is required for the spreading of WIMF
MIRO-1 has a C-terminal transmembrane (TM) domain for OMM targeting and two Rho GTPase domains flanking two Ca2+ sensing EF-hand domains (Fig. 4a). To understand how MIRO-1 might regulate WIMF, we generated domain-specific alleles of the endogenous miro-1 locus (Fig. 4a, Supplemental Table 5). Rho, EF-hand, and TM domain mutants displayed similar mitochondrial morphology as in miro-1(tm1966) before wounding (Supplementary Fig. 5e), suggesting these domains are required for MIRO-1 to maintain mitochondrial morphology. Moreover, WIMF is more restricted in the animals with mutated Rho, EF-hand, or TM domains (Fig. 4b, Supplementary Fig. 5f, Supplementary Movie 11), indicating that outer mitochondrial membrane localization of MIRO-1 and cytosolic Ca2+ binding to EF-hand is important for the WIMF.
Fig. 4. WIMF is dependent on wound-induced Ca2+-MIRO-1 signaling.
a Top, experimental design to disrupt the function of MIRO-1 protein domains using CRISPR-Cas9 mediated mutagenesis. Bottom, miro-1 in-frame mutation alleles. Sequences in bold are key residues in each domain40. Details of indel mutations are in Supplementary Table 5. b Quantitation of the distance of the fragmented mitochondria to the injury site shown on the left in different animals (WT, n = 11; tm1966, n = 30; ΔRho, n = 19; ΔEF-I, n = 14; ΔEF-II, n = 22; ΔEF-I&II, n = 15; ΔTM, n = 16 animals). Note, mutations of the Rho, EF-hand II and TM domains show reduced spreading of WIMF compared to the WT and similar to miro-1(tm1966) animal, indicating that these mutations affect MIRO-1’s function. Bars indicate mean ± SEM. ns, P = 0.8321, ****P < 0.0001 (versus WT), One-way ANOVA Dunnett’s test. c Quantitation of the distance of the fragmented mitochondria to the injury site in TRPM/gtl-2(n2618), mcu-1(ju1154), and gtl-2(n2618);miro-1(zju19) mutant (WT, n = 13; gtl-2, n = 17; miro-1, n = 36; gtl-2;miro-1, n = 143 animals). miro-1(zju19) and miro-1(zju40) frameshift mutations were generated by CRISPR-Cas9 mediated mutagenesis in gtl-2 background. Bars indicate mean ± SEM. ns, P = 0.9558 (versus miro-1), two-tailed unpaired t-test; ns, P = 0.9558, ****P < 0.0001 (versus WT), One-way ANOVA Dunnett’s test. d Representative confocal image of mitochondrial morphology after treatment with Ca2+ ionophore ionomycin in both WT and miro-1 mutants. Scale bars, 10 μm, and 5 μm (zoom-in). N = 3 independent experiments. e Quantitation of the distance of the fragmented mitochondria to the injury site in gtl-2(n2618), miro-1(tm1966) mutant treated with low concentration of ionomycin (2.5 μΜ treated for 1 h) (WT-DMSO, n = 37; WT-ionomycin, n = 36; gtl-2-DMSO, n = 31; gtl-2-ionomycin, n = 34; miro-1-DMSO, n = 32; miro-1-ionomycin, n = 35). Bars indicate mean ± SEM. ns, P = 0.7435 (WT) or 0.6382 (miro-1), ***P < 0.0001, Two-tailed unpaired t-test. Source data are provided as a Source Data file.
Epidermal wounding also triggers rapid elevation of cytosolic Ca2+23,24,43; in the C. elegans skin, this is dependent on the TRPM/gtl-2 channel23. Ca2+ uptake into mitochondria mediated by the MCU-1 channel is also necessary for actin-based wound closure26. Moreover, MIRO-1 has been shown to be required for a cytosolic Ca2+ induced mitochondrial shape transition in cultured cells11. We tested whether wound-induced early Ca2+ signals were involved in WIMF. In gtl-2(n2618) or mcu-1(ju1154) loss of function mutants, which display reduced cytosolic or mitochondrial Ca2+ uptake after wounding respectively, epidermal mitochondria displayed normal steady-state morphology (Supplementary Fig. 5f, Supplementary Movie 12). gtl-2(n2618) mutant showed much reduced mitochondrial fragmentation, whereas mcu-1(ju1154) mutant underwent typical mitochondrial fragmentation (Fig. 4c, Supplementary Fig. 5f, Supplementary Movie 12). gtl-2 miro-1 double mutants resembled miro-1 single mutants in the distance of WIMF (Fig. 4c). Together, these data suggest that the GTL-2 mediated cytosolic Ca2+ signal acts in the same pathway as MIRO-1 to drive WIMF.
To further test this hypothesis, we treated animals with ionomycin to elevate cytosolic Ca2+ (Supplementary Fig. 5g) and observed widespread mitochondrial fragmentation in WT animals but not in miro-1 mutants (Fig. 4d), suggesting MIRO-1 is required for elevated Ca2+ to induce mitochondrial fragmentation, consistent with findings in cultured cells11. Furthermore, the elevation of Ca2+ by low doses of ionomycin rescued WIMF in gtl-2 mutants but not in miro-1 animals (Fig. 4e, Supplementary Movie 13), suggesting wounding-induced Ca2+ is necessary for WIMF and acts via MIRO-1.
Mitochondrial fragmentation acts downstream of Ca2+ signaling in wound closure
We next asked how mitochondrial fragmentation accelerates wound closure. Loss of function in either the Ca2+ channel TRPM/GTL-2 or the mitochondrial Ca2+ uniporter MCU-1 inhibits wound closure23,26. We thus performed epistasis analysis of fzo-1 with Ca2+ and the mitochondrial Ca2+ pathway. We found that loss of function in fzo-1 suppressed the low post-wounding survival of gtl-2 (Supplementary Fig. 2d) and restored its wound closure to normal (Fig. 5a). fzo-1 also rescued the defective wound closure in the mcu-1 mutant (Fig. 5a). Thus, constitutive fragmentation of mitochondria in fzo-1 mutants bypasses the need for cytosolic or mitochondrial Ca2+ signals in wound closure, consistent with Ca2+ acting upstream of WIMF (Fig. 4).
Fig. 5. Mitochondrial fragmentation acts downstream of Ca2+-MIRO-1 to accelerate wound closure.
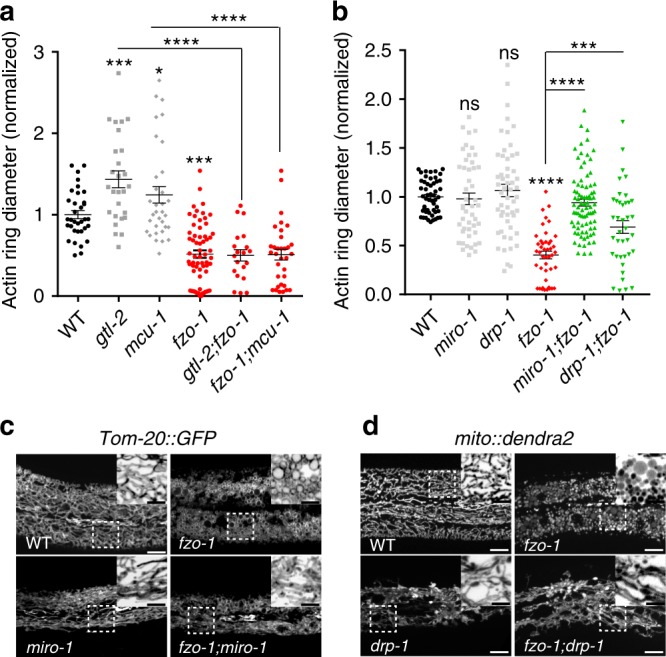
a Loss of function in the fusion gene fzo-1 suppresses wound closure defects of gtl-2(n2618) and mcu-1(ju1154) mutants. Quantitation of actin ring diameter in WT and mutants 1 h after needle wounding (WT, n = 50; gtl-2, n = 27; mcu-1, n = 33; fzo-1, n = 64; gtl-2;fzo-1, n = 20; fzo-1;mcu-1, n = 33 animals). gtl-2 and mcu-1 mutants display delayed actin ring closure, which is suppressed in double mutants with fzo-1(tm1133). The WT actin ring diameter was normalized to 1 and mutants normalized to WT. Bars indicate mean ± SEM. *P = 0.0328, ***P = 0.0001, ****P < 0.0001, One-way ANOVA Dunnett’s test (single mutant versus WT). two-tailed unpaired t-test (versus mcu-1 or gtl-2). b Quantitation of actin ring diameter in the mitochondrial mutants (WT, n = 34; drp-1, n = 54; miro-1, n = 47; fzo-1, n = 44; miro-1;fzo-1, n = 82; fzo-1;drp-1 RNAi, n = 39 animals). drp-1 partially suppresses fzo-1 while miro-1 significantly suppresses the fzo-1 in enhanced wound closure. Bars indicate mean ± SEM. ns, P = 0.7753 (drp-1) or 0.9893 (miro-1), ***P = 0.0002, ****P < 0.0001, two-tailed unpaired t-test (versus fzo-1). One-way ANOVA Dunnett’s test (single mutant versus WT). Source data are provided as a Source Data file. c Representative confocal images of mitochondrial morphology in fzo-1 and miro-1;fzo-1 mutants. Pcol-19-Tomm-20::GFP(zjuSi48) transgenic animals label the mitochondria. fzo-1 mutants display fragmented and round shaped mitochondria. miro-1;fzo-1 double mutants have tubular mitochondria, similar to miro-1 single mutants. N = 3 independent experiments. d Representative confocal images of mitochondrial morphology in fzo-1 and drp;fzo-1 mutants. Mitochondria were labeled with mito::dendra2(juSi271), the mitochondrial morphology of drp-1;fzo-1 mimics drp-1, without fragmented mitochondria. Note, drp-1 suppress fzo-1 in mitochondrial morphology. Scale (c, d), 10 μm and 5 μm (zoom-in image).
MIRO-1 is required for the accelerated wound closure of mutants with fragmented mitochondria
We then asked whether the enhanced wound closure in fzo-1 is due to fragmented mitochondria. Although miro-1 mutation did not significantly affect wound closure or post-wounding survival (Fig. 5b; Supplementary Fig. 5h), the faster wound closure of the fzo-1 mutant was suppressed by loss of function in miro-1 (Fig. 5b). Surprisingly, mitochondrial morphology of miro-1; fzo-1 mutants resembled that of miro-1 single mutants (Fig. 5c), indicating that miro-1 is required for the fragmented mitochondrial morphology of fzo-1 mutant and that mitochondrial fragmentation is required for fzo-1’s faster wound closure. To test this further, we made drp-1 fzo-1 double mutants, which displayed a hyper-fused mitochondrial morphology resembling that of drp-1 (Fig. 5d). drp-1 also significantly suppressed the faster wound closure phenotype of fzo-1 animals (Fig. 5b).
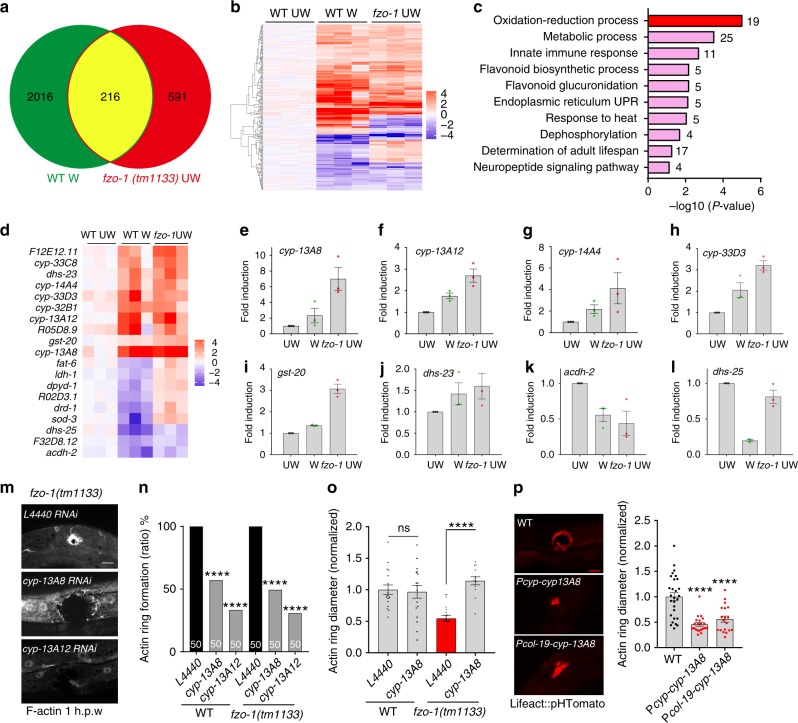
Oxidative signaling genes are upregulated by wounding and by mitochondrial fragmentation
To understand the genetic basis of the enhanced wound closure in animals with fragmented mitochondria, we analyzed the transcriptomes of wounded WT animals and fzo-1 mutants, using unwounded WT animals as the control (Fig. 6a). A large number of differentially expressed genes (DEGs) were induced in wounded animals compared to unwounded ones (Supplementary Fig. 6a, Supplementary Data 1). DAVID gene ontology (GO) analysis found that most such DEGs were enriched in the mitochondria and mitochondrial biogenesis (Supplementary Fig. 6b, c). We hypothesized that faster wound closure of fzo-1 mutants might reflect the elevated expression of genes induced by wounding. We compared RNA seq data in wounded WT animals and fzo-1 mutants and identified ~2200 and ~800 DEGs, respectively (adjusted p-value < 0.05) (Fig. 6a). Strikingly, 216 genes differentially expressed after skin wounding showed similar differential expression in fzo-1 (Fig. 6b, Supplementary Data 2). GO analysis of the 216 overlapping genes revealed enrichment for oxidation-reduction and metabolism-related terms (Fig. 6c), suggesting loss of function of fzo-1 or wounding affects the expression of genes involved in oxidative signaling. These included cytochrome P450 (cyp) family genes, dehydrogenases (dhs), and glutathione S-transferases (gst) (Fig. 6d, Supplementary Fig. 6d). Quantitative PCR of selected genes revealed similar changes as found in RNA seq (Fig. 6e–l).
Fig. 6. The upregulation of oxidative signals in fzo-1 mutants is required for faster wound closure.
a Venn diagram of differentially expressed genes (DEGs) in WT needle wounded and fzo-1(tm1133) unwounded animals, compared to WT unwounded controls, as measured by RNA-seq (Benjamini-Hochberg adjusted P value <0.001). See also Supplementary Data 1. b Gene expression heatmap of 216 DEGs shared by WT wounded and fzo-1 unwounded animals as described in a. c DAVID biological process GO terms of upregulated and downregulated genes in the 125/216 overlapping DEGs (Benjamini-Hochberg adjusted P value <0.001). See also Supplementary Data 2. d Heatmap of 19 overlapping oxidation-reduction processes genes. e–l Quantification of oxidation-reduction process-related genes in the WT, wounded, and fzo-1 animals as determined by qPCR. In both WT wounded and fzo-1 mutant, cyp-13A8, cyp-13A12, cyp-14A4, cyp-33D3, gst-20, dhs-23, and dhs-28 were upregulated while acdh-2, dhs-25 are down-regulated. N = 3 independent experiments; Bars indicate mean ± SEM. m Representative confocal images of actin ring formation 1 h.p.w. RNAi knockdown of cyp-13A8 and cyp-13A12 suppresses the accelerated actin ring formation in fzo-1(tm1133). Scale bar, 10 μm. N = 3 independent experiments. n Quantitation of actin ring formation percentage in the WT and fzo-1(tm1133) double mutants with RNAi knockdown cyp-13A8, and cyp-13A12 genes. N = 50, ****P < 0.0001, versus WT or fzo-1(tm1133), Two-sided Fisher’s exact test. o Quantitation of actin ring diameter in the WT and fzo-1(tm1133) double mutants with RNAi knock down cyp-13A8 (WT-L4440, n = 17; WT-cyp-13A8, n = 17; fzo-1-L4440, n = 19; fzo-1;cyp-13A8, n = 13 animals). Bars indicate mean ± SEM, ns, P = 0.803, ****P < 0.0001, versus WT or fzo-1(tm1133). two-tailed unpaired t-test. p Overexpression of CYP-13A8 in epidermis accelerates wound closure. Left, representative actin ring images, Scale bar, 10 μm. Right, quantitation of actin ring diameter 1 h.p.w (WT, n = 28; Pcyp-13A8-cyp-13A8, n = 21; Pcol-19-cyp-13A8, n = 19 animals). Bars indicate mean ± SEM, ****P < 0.0001, versus non transgenic animals. One-way ANOVA Dunnett’s test. Source data are provided as a Source Data file.
Enhanced wound closure in fzo-1 is dependent on Cytochrome P450 and mtROS
How might oxidative signals affect wound closure in animals with fragmented mitochondria? To address this question, we examined CYP genes upregulated after wounding and in fzo-1 mutants. RNAi knockdown of either cyp-13A8 or cyp-13A12 strongly inhibited actin ring formation at wound sites in both WT and fzo-1 mutant (Fig. 6m, n). Importantly, in animals forming a visible actin ring, RNAi knockdown of cyp-13A8, which is highly induced after wounding and in fzo-1 (Fig. 6d), significantly inhibits actin ring closure (Fig. 6o). We observed cyp-13A8 mRNA expression was significantly increased a few minutes after wounding (Supplementary Fig. 6e), the time correlates with the rapid actin polymerization at the wound site (Supplementary Fig. 6e). cyp-13A8 is expressed in many tissues, including epidermis (Supplementary Fig. 6f). Overexpression of cyp-13A8 in epidermis either using its own promoter or col-19 promoter accelerated wound closure (Fig. 6p), suggesting CYP-13A8 acts cell-autonomously to promote wound closure.
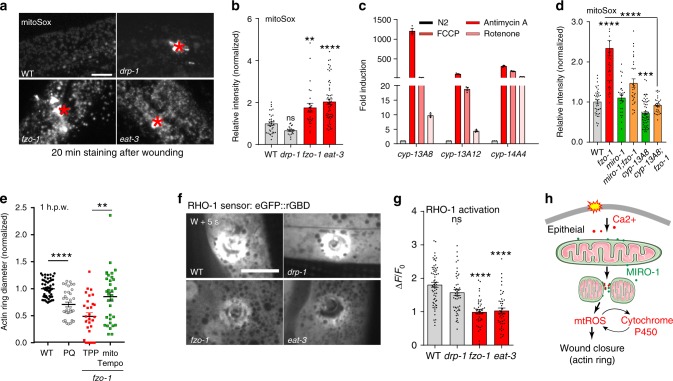
CYPs can generate reactive oxygen species (ROS)44,45, and CYP expression is subject to feedback regulation by mtROS46. Therefore, we examined mitochondrial ROS (mtROS) production in the fragmented mitochondrial mutants by staining with either the ROS sensor mitoSox or the genetically encoded sensor mito::cpYFP47. Both fzo-1(tm1133) and eat-3(tm1107) mutants displayed significantly increased mitoSox fluorescence (Fig. 7a) and mito::cpYFP intensity (Supplementary Fig. 7a), whereas drp-1(tm1108) mutants showed reduced mitoSox staining (Fig. 7a). Treatment of animals with mitochondrial fragmentation inducers Rotenone or FCCP significantly enhanced the mitoSox signal (Supplementary Fig. 7b) and also induced CYP expression (Fig. 7c). Conversely, overexpression of cyp-13A8 in the epidermis enhanced mitoSox fluorescence while cyp-13A8(zju212) knock out mutants (Supplementary Fig. 7b) displayed lower mitoSox signal (Supplementary Fig. 7c), suggesting CYPs are required and sufficient to increase mtROS. Together, these results suggest that mtROS and CYP-13A8 display positive feedback regulation that maintains elevated mtROS levels after wounding.
Fig. 7. Accelerated wound closure of fzo-1 mutant is dependent on mtROS.
a Representative confocal images of mitoSox staining in WT and mutants. b Representative confocal images of mitoSOX staining in WT, drp-1(tm1108), fzo-1(tm1133), and eat-3(tm1107) mutants 20 min after needle wounding. Red asterisks indicated wound sites. Right, Quantitation of mitoSOX intensity, normalized to WT (WT, n = 35; drp-1, n = 20; fzo-1, n = 25; eat-3, n = 56 animals). Bars indicate mean ± SEM, ns, P = 0.3413, **P = 0.0016, ****P < 0.0001, One-way ANOVA Dunnett’s test (versus WT). c qPCR analysis of Cytochrome P450 genes after treatment antimycin A, Rotenone and FCCP. N = 3 independent experiments. Bars indicate mean ± SEM. d Quantitation of mitoSOX intensity, normalized to WT (WT, n = 40; fzo-1, n = 38; miro-1, n = 29; fzo-1;miro-1, n = 30; fzo-1;cyp-13A8, n = 30; cyp-13A8, n = 62 animals). Bars indicate mean ± SEM, ns, P = 0.2472, ***P = 0.0005, ****P < 0.0001, versus WT or fzo-1 animal. two-tailed unpaired t-test. e Quantitation of F-actin ring diameter in TPP and mitoTempo treated worms (WT, n = 51; PQ, n = 35; fzo-1-TPP, n = 29; fzo-1-mitoTempo, n = 33 animals). Paraquat (PQ) treatment as a control. Bars indicate mean ± SEM, **P = 0.0015, ****P < 0.0001, two-tailed unpaired t-test. f, g Mitochondrial fusion mutants reduced local activation of RHO-1 small GTPase at wound sites (see also Supplementary Movie 14). f Representative confocal images of RHO-1 GTPase sensor eGFP::rGBD in the adult in WT or drp-1, fzo-1, and eat-3 mutant. Pcol-19-eGFP::rGBD(juEx3025) strain were used for wounding and imaging. Scale bars (a, f), 10 μm. g Quantitation of eGFP::rGBD fluorescent intensity change in WT and mutants after wounding (WT, n = 52; drp-1, n = 51; fzo-1, n = 44; eat-3, n = 46 animals). Bars indicate mean ± SEM, ns, P = 0.1448, ****P < 0.001, One-way ANOVA Dunnett’s test. Source data are provided as a Source Data file. h A model for how mitochondrial fragmentation promotes epidermal wound closure.
We next determined whether the elevated mtROS in fzo-1 mutants contributes to the enhanced wound closure. Loss of function in miro-1 suppressed the elevated mitoSox signal in the fzo-1 mutant (Fig. 7d), consistent with suppression of mitochondrial fragmentation and enhanced wound closure in fzo-1 (Fig. 5b). cyp-13A8 fzo-1 double mutants also showed significantly reduced mitoSox signal compared to fzo-1 single mutants (Fig. 7d), suggesting cyp-13A8 is required for the elevated mtROS levels in fzo-1 mutants. Treatment of fzo-1 or eat-3 mutants with antioxidants NAC or mitoTempo not only reduced mtROS levels (Supplementary Fig. 7d) but also suppressed the faster wound closure (Supplementary Fig. 7e, f, Fig. 7e), whereas mitochondrial specific prooxidant paraquat enhanced wound closure (Fig. 7e). mitoTempo treatment reduced the post-wound survival (Supplementary Fig. 7g) and delayed wound closure (Supplementary Fig. 7h), and these effects could be reverted by the addition of Rotenone (Supplementary Fig. 7h), suggesting elevated mtROS is required and sufficient to accelerate wound closure. We then tested whether mitochondrial fragmentation affects local activation of RHO-1, which is an inhibitory GTPase that regulating actin filaments formation in wound closure. Both fragmented mitochondrial mutants fzo-1 and eat-3 displayed reduced RHO-1 genetic sensor eGFP::rGBD intensity after wounding (Supplementary Fig. 7i, j, Supplementary Movie 14), suggesting mitochondrial fragmentation mutants inhibit the local action of RHO-1 in vivo. Together, these results suggest that enhanced wound closure in fragmented mitochondrial mutants is due to elevated mtROS signal and inhibition of RHO-1 activity.
Discussion
We have shown that epidermal injury triggers rapid and reversible fragmentation of mitochondrial morphology, wounding-induced mitochondrial fragmentation (WIMF), that promotes tissue repair through oxidative-reduction and mtROS signaling. Notably, WIMF is independent of the canonical fission regulator DRP-1, but requires the Ca2+-sensitive mitochondrial Rho GTPase MIRO-1. We find that mitochondrial fragmentation triggers mtROS production and induces expression of oxidative signaling genes such as CYP-13A8, which acts together to maintain an elevated protective level of mtROS. Thus, our findings demonstrate that mitochondrial fragmentation is beneficial in promoting tissue repair in vivo.
Mitochondria form a highly dynamic tubular network within cells such as the C. elegans epidermis, reflecting a balance of fusion and fission events that are linked to the energetic and oxidative metabolic requirements of the cell. The master regulator of fission is DRP1, which constricts tubular mitochondria to facilitate division in response to cellular signals or mechanical force48. In contrast, WIMF does not depend on DRP-1 but instead requires the mitochondrial Rho GTPase MIRO-1. Interestingly, Nemani et al. recently reported that elevated cytosolic Ca2+ induces a mitochondrial shape transition (MiST) in HeLa and MEF cells, dependent on MIRO1 but not DRP111. While WIMF and MiST may share some mechanistic overlap, we note that the Ca2+ induced MiST happens over several minutes11, whereas WIMF happens in seconds (see detail comparison in Supplementary Table 6). Possibly the amplitude or local nature of the wounding-induced Ca2+ transient is sufficient to trigger a more rapid fragmentation response. In both situations, Ca2+ binding of MIRO-1 is critical, although the mechanism by which Ca2+-activated MIRO1 can cause mitochondrial fragmentation remains to be determined.
Tissue damage is signaled at a cellular level via damage-associated molecular patterns (DAMPs)49 or wound response signals such as Ca2+ or ATP50. In Drosophila epidermis and zebrafish tail fin, Ca2+ stimulates DUOX2 dependent membrane production of ROS that recruit immune cells to the injury site24,25,43. However, Ca2+ mediates diverse biological processes unrelated to tissue injury, raising the question of how organisms distinguish between wound-induced and physiological Ca2+ transients. Previous studies have shown that wounding triggers mtROS production, mediated by MCU-dependent mitochondrial Ca2+ uptake, and that mtROS can promote wound healing26. Here we find that MIRO-1 is another key downstream target of Ca2+, independent of MCU-1 dependent Ca2+ uptake into mitochondria. Thus, wounding-induced Ca2+ signals may act via multiple effectors to generate a protective mtROS cascade in regulating tissue repair.
We have shown that WIMF occurs in a variety of cellular contexts, from in vitro scratch assays to zebrafish tail fin wounding. It will be valuable in the future to dissect whether similar pathways involving MIRO1, CYPs, and oxidative signals function in these other wound repair paradigms. Intriguingly, MIRO1 is required for MEF cell migration in vitro, at both collective and single-cell level51, potentially relevant to our finding that miro-1 is required for accelerated wound closure in the fzo-1 mutant, suggesting Ca2+-MIRO-1 signals may play a conserved role in responding to and regulating mitochondrial activity in tissue repair.
We find that wounding and mitochondrial fragmentation induce expression of cytochrome P450 monooxygenases, a large family of enzymes that generate mtROS44,46. Moreover, overexpression of cyp-13A8 in epidermis enhances mtROS and promote wound closure. CYPs respond to wounding and accelerate wound epithelization in diabetic mice52, hairless mouse ear53, and even in plants54. In this study, we demonstrated that CYPs are upregulated in the fragmented mitochondrial animals and are required for actin-based wound closure, suggesting CYPs may be vital in mediating oxidative signals that promote damage repair. By uncovering a link between mitochondrial fragmentation, oxidative signaling and tissue repair, our work may open a door to novel therapeutic interventions based on mitochondrial signals. For example, hyperbaric oxygen therapy has long been used to accelerate wound repair in chronic diabetic wounds and is thought to act in part by increasing oxidative metabolic stress55,56. Our results raise the possibility that hyperbaric oxygen treatment activates mitochondrial oxidative metabolic cascades, culminating in high levels of mtROS that protect tissues from damage.
Methods
C. elegans strains and genetics
All C. elegans strains were maintained by standard methods at 20–22.5 °C on nematode growth medium (NGM) agar plates seeded with E. coli OP50. New strains were constructed using standard procedures, and genotypes confirmed by PCR and sequencing. All the strains used are listed in Supplementary Table 1.
Constructs and transgenic worms
Epidermal mitochondria were labeled with the mitochondrial target sequence of Cytochrome C oxidase VIII fused to GFP or dendra2 or mKate2 under the control of the col-19 promoter. Extrachromosomal array transgenic worms were made by injection of constructs at 10 ng/μl with 50 ng/μl co-injection marker (Pttx-3-RFP). Single-copy insertion of Pcol-19-mito::dendra2(juSi271) was made by Mos-SCI57. The single-copy insertions Pcol-19-lifeact::PHtomato(zjuSi22) I, Pcol-19-mito::mKate2(zjuSi47) II, Pcol-19-Tomm-20::GFP(zjuSi48) I were made by CRISPR-Cas9 based insertion method58. New transgenic strains are listed in Supplementary Table 1. All constructs used in this study are listed in Supplementary Table 2.
Outer mitochondrial membrane proteins screen
RNAi was carried out as follows. Briefly, WT animals carrying the mitochondrial marker Pcol-19-mito::dendra2 (juSi271) were grown to the L4 stage and then fed RNAi bacteria for 12 h. Young adult animals were imaged on the spinning disk confocal microscope before and after needle wounding (Andor 100×, NA 1.46 objective). We screened C. elegans orthologs of about 170 putative OMM proteins in the mitoCarta database (https://www.broadinstitute.org/files/shared/metabolism/mitocarta/human.mitocarta2.0.html)59. Candidate genes are listed in Supplementary Table 4.
GFP fusion protein knock-in
GFP::miro-1(zju21), mKate2::miro-1(zju211), fzo-1::GFP(zju136) knock-in mutations were generated using CRISPR-Cas9 method60. Briefly, repair templates were generated into pDD282 plasmid by Gibson assembly. We injected sgRNAs, repair template, and dpy-10 sgRNA (as selection marker) into N2 animals. Roller animals were heat-shocked to remove markers. All primers and sgRNAs are listed in Supplementary Table 3.
Drug treatment
All drugs were added to the bacterial lawn from a high concentration stock and allowed to dry for 1–2 hr at room temperature before transferring the young adult animals. Rotenone (Sigma R8875) was dissolved in DMSO to make 40 mM stock solutions; mitoTempo (Sigma, SML0737), triphenylphosphonium chloride (TPP; Sigma 675121), PQ dichloride (Sigma 36541), and NAC (Sigma A7250) were dissolved in ddH2O to make 500 mM stocks; FCCP (Sigma C2920), Antimycin A (Sigma A8674), Ionomycin (Sigma 407953) were dissolved in ethanol as 10 mM, 45 mM, and 10 mM stock solutions, respectively. For acute drug treatments, young adults were transferred to freshly made NGM drug plates 1–2 hours at room temperature before needle wounding. The synchronized young adults were transferred to freshly made NGM drug plate and then imaged using Zeiss Discovery LSM880 or the spinning disk confocal.
Wounding, wound closure, and survival assay
We wounded animals using femtosecond or Micropoint UV laser or with single stabs of a microinjection needle to the anterior or posterior body 24 h after the L4 stage. Actin ring and mitochondrial images were taken using LSM710 confocal microscope (63×, NA 1.4 objective) or spinning disk microscope (100×, NA 1.46 objective), Laser wounding images were taken using spinning disk confocal microscope (Andor 100×, NA 1.46 objective with IQ CORE image software). Actin ring quantitation and survival rate were performed as previously described23. Fragmented mitochondria were counted in a region of interest (ROI) 100 μm2 within 20 μm to the wound site (4 ROI per animal) (Fig. 1d). The spread of mitochondrial fragmentation from the wound site was measured as the farthest distance of the fragmented mitochondria to the laser wounding site using ImageJ or MetaMorph software. Some metrics were normalized to WT = 1.
GFP nanobody mediated protein degradation
GFP nanobody tissue-specific knockdown was performed as follows. First we generated the strain fzo-1::GFP(zju136); Pcol-19-lifeactin::pHtomato (zjuSi22) to analyze actin ring diameter. Tissue-specific GFP nanobody degradation plasmids were generated using LR recombination. Plasmids for Pcol-19-vhh-ZIF1(zjuEx99), Psur-5-vhh-ZIF1(zjuEx220), Pmyo-3-vhh-ZIF1(zjuEx154) were injected into N2 animals and the transgenic animals were then crossed with either Pcol-19-Lifeact-pHtomato or fzo-1::GFP; Pcol-19-lifeactin::pHtomato. Needle wounding and actin ring diameter measurements were performed as above.
CRISPR-Cas9 mediated mutagenesis
MIRO-1 mutagenesis was performed using the CRISPR-Cas9 system58. A mixture of plasmids containing pSX709 (pU6-BseRI-BseRI-sgRNA-miro-1) 50 ng/μl, and pSX524(Peft-3-cas9-NLS-pU6-dpy-10 sgRNA) 50 ng/μl was injected into the animals with a different transgenic or mutant background (see Supplementary Table 5). We screened for in-frame deletion mutations by DNA sequencing. All alleles were outcrossed before analysis. sgRNAs and deletion information are listed in Supplementary Tables 3 and 5.
Heat shock
Phsp-16.2::fzo-1 transgenic animal heat shock experiment was performed as follows essentially described elsewhere61. Briefly, L1 worms were heat-shocked at 32 °C for 4 h, then incubated at 20 °C overnight before proceeding to needle wounding at the young adult stage.
The single worm RNA sequencing
Single worm RNA sequencing used a protocol modified from single-cell RNA sequencing for mouse cells62. A single young adult animal was transferred into 2 μl lysis buffer and lysed by grinding. In all, 1 μl of each oligo-dT primer (10 μM) and dNTP (10 mM) was added into the PCR tube and heated at 72°C for 3 mins then cooled for 2 min. 6 μl reverse transcription mixture (100 U SuperScript II reverse transcriptase (Takara), superscript II first-strand buffer, 1 U RNAase inhibitor (Vazyme),10 M betaine (Sigma), 6 mM MgCl2 (Ambion), and 100 μM TSO primer) was then added directly and incubated using thermal cycle: 90 min at 42 °C, 15 min at 72 °C and hold at 4 °C. cDNA samples were amplified with 10 μl KAPA HiFi HotStart ReadyMix (Kapa Biosystems) and 12.5 μl 10 μM IS PCR primers. The purified cDNA was fragmented by TruePrep DNA Library Prep Kit V2 for Illumina (Vazyme Inc) Hiseq X 10 system sequencing. Primers are listed in Supplementary Table 3.
RNA-sequencing analysis
Each sample was analyzed in three biological replicates. Paired-end RNA-seq reads were generated on the Illumina HiSeq X10 platform. Clean reads were mapped to rRNAs and tRNAs firstly, and those unmapped reads were mapped to the C. elegans genome (ce11) with gene annotation WS258 using STAR63 version 2.5.3a under default parameters except ‘out Filter Match N min 40′. The Feature Counts program from R subreads package64 was used to count reads mapped to each gene for all samples. The gene count by sample tables was used for differential expression analysis with DESeq265. The cutoff for differential expressed genes (DEGs) were: Benjamini-Hochberg adjusted p-value less than 0.05 and foldchange larger than 1.5. GO-term analysis of DEGs was done with DAVID66. Figures were made with the ggplot2 package and Complex Heatmap package in R67.
Mitosox staining and imaging
MitoSOX Red (Molecular Probes, M36008) staining was performed as follows. Briefly, young adult animals were wounded by needle and then transferred mitoSOX Red staining solution (5 μM) The animals were stained in the dark with gentle shaking for 20 min at room temperature. Stained worms were washed three times with M9 before imaging using a 561-nm excitation laser.
RNA isolation and quantitative PCR (qPCR) analysis
Total RNA was extracted from 30 young adult animals using TRIzol (Invitrogen, Carlsbad, CA, USA) and quantitated using a NanoDrop spectrophotometer (Thermo, USA). First-strand cDNA was synthesized by using the ReverTra Ace qPCR RT Kit (Toyobo, Japan). Primers for genes (Supplementary Table 3) were designed using Primer Premier 5 (Premier Biosoft). act-1 was used as an internal control. The reaction mixtures were prepared according to the SYBR green kit instructions (Vazyme, China) and real-time quantitative reverse transcription PCR (RT-PCR) was performed using a LightCycler 480 II (Roche, Switzerland). The cycling protocol was: 95 °C for 2 min, followed by 40 cycles at 95 °C for 10 s, and 60 °C for 40 s. Relative expression levels were calculated using the 2−ΔΔCt method.
Cell culture and scratch assay
U2OS cells (ATCC) were cultured in DMEM (GIBCO) supplemented with 10% FBS (Hyclone), 2 mM glutamine, 100U/100 μg/ml penicillin/streptomycin (GIBCO). The cells were seeded in a 4-well microplate and grown overnight to reach 90% confluence. To visualize mitochondrial morphology, cells were incubated in mitoTracker Green (Molecular Probes) and subjected to scratch wounding as described68. The mitochondrial morphology was taken using spinning disk confocal and images analyzed using MetaMorph. Each cell was classified as displaying tubular or fragmented mitochondria. The statistical details are in Source Data file.
Visualization of MIRO-1
GFP::miro-1(zju21) and mKate2::miro-1(zju211) knock-in strain were subjected to laser or needle wounding. Animals were mounted on 10% agarose pads in M9, in 12 mM levamisole and imaged before and after wounding using a Zeiss 880 confocal microscope. Green fluorescence was visualized with a 488-nm laser, and red fluorescence was visualized with a 561-nm laser. To score GFP::MIRO-1 on the membrane of mitochondria, fluorescence profiles at different sections of the mitochondria were obtained using the ‘Line Scan’ tool in MetaMorph. GFP::MIRO-1 was scored as localizing to the membrane if the peak of green intensity (GFP::MIRO-1) and the peak of red intensity (mitochondrial matrix mKate2) were not overlapping.
Imaging and mitochondrial morphology analysis
Images were taken using IQ image software (IQ CORE, Nikon) and analyzed using MetaMorph (Molecular Devices, San Jose, CA) and ImageJ (https://imagej.nih.gov/ij/). We scored mitochondria as fragmented if they were separate from other mitochondria and had a spherical or oval shape. The distance of fragmented mitochondrial to the wound site was defined as the farthest fragmented mitochondria to the wound site. We searched for fragmented mitochondria around the wound site and drew 20 lines for each wounded animal. The farthest distances were then averaged. All quantitation was performed by an observer blind to genotypes.
Zebrafish tail-fin wounding and mitochondrial imaging
WT zebrafish (AB line) larvae from the zebrafish center at ZJU. 3 days post-fertilization (3 dpf) larvae were cultured in E3 medium (5 mM NaCl, 0.17 mM KCl, 0.33 mM CaCl2, 0.33 mM MgSO4) containing 5 μM mitoTracker Green (Molecular Probes) for 2 h. Larvae were then washed three times before imaging. To examine the mitochondrial morphology, the larvae with mitoTracker Green staining were subjected to tail-fin tip wounding and then transferred to the imaging plate for confocal imaging22. No ethics approval was necessary for work with zebrafish larvae.
Oxygen Consumption Rate (OCR) measurement
OCR was measured using Seahorse Bioscience XF9669. Briefly, approximately 10-25 young adult worms were placed in each well and then measured by the XF96 respirometer. The experiment was repeated two times, with 8 wells for each genotype in each experiment. OCR per single worm was then normalized to the total number of animals.
Statistical analysis
All statistical analyses used Prism (GraphPad, CA). Two-way comparisons used a two-tailed unpaired t-test. One-way ANOVA for multiple comparisons, or the Fisher exact test for proportions.
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Supplementary information
Description of Additional Supplementary Files
Acknowledgements
We thank C.L. Yang, Y. Jin, and W. Mair for reagents, L. Yu, G. Bai, Q. Sun, W. Liu, G. Ou for comments on the manuscript, and Xu lab members for support and discussion. We thank P. Xu and Z. Hong for help with zebrafish larvae and U2OS cell culture, and T. Zhuang for making strains. Some super-resolution images were taken using Zeiss 880 at the imaging center of the core facility at Zhejiang University School of Medicine. Several C. elegans strains were provided by the CGC, which is supported by the NIH Office of Research Infrastructure Programs (P40OD010440). This work is supported by the Ministry of Science and Technology of China (National Key Research and Development Program of China grant 2016YFC1100204), the National Natural Science Foundation of China (91754111, 31972891, 31671522), and ‘One Thousand’ Youth Talent Program to S.X., National Natural Science Foundation of China (31701271) and the China Postdoctoral Science Foundation (2018M630668) to J.Z., ‘One Thousand’ Youth Talent Program to Y.Z. Initial stages of this work were supported by NIH grant R01 GM054657 to A.D.C.
Source data
Author contributions
S.X. conceived the study, designed the experiments, and performed initial mitochondrial fragmentation analysis as postdoctoral researcher in A.D.C.’s lab, with NIGMS support. S.X., H.Z., and Jz.Z. performed RNAi screen. H.F. made constructs, performed the wound closure, TMRE staining, Tissue-specific knockdown, RNAi, and fluorescence microscopy. H.Z. made constructs, performed CRISPR-Cas9 mutagenesis, knock-in, and wounding experiments. Jh.Z. performed single worm RNA sequencing, X.Y. and Y.Z. performed RNA sequencing data analysis. X.M. made transgene constructs and fzo-1 GFP knock-in animals. J.X. performed qPCR experiments. H.F. and H.Z. performed microinjection experiments. S.X. performed cell scratch assay and zebrafish wounding experiment. S.X. and A.D.C. wrote the manuscript.
Data availability
The authors declare that all data supporting the findings of this study are available within this article, its supplementary information files, the peer-review file, the source data file, or are available from the corresponding author upon reasonable request. The RNA sequencing data generated and analyzed in this study are available upon request as well as from the Sequence Read Archive (SRA) at NCBI at the following accession code: PRJNA523321 [https://www.ncbi.nlm.nih.gov/sra/?term=PRJNA523321]. The source data underlying Figs. 1e, 2b, d, g, i, 3d, f, 4b, c, f, 5a, b, 6e–I, n–p, and 7b-e, and Supplementary Figs. 1d, f, 2c–e, 3c, 4f, g, 5a, g, and 7a, c, d, e, g–i are provided as a Source Data file.
Competing interests
The authors declare no competing interests.
Footnotes
Peer review information Nature Communications thanks the anonymous reviewer(s) for their contribution to the peer review of this work. Peer reviewer reports are available.
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Hongying Fu, Hengda Zhou.
Supplementary information
Supplementary information is available for this paper at 10.1038/s41467-020-14885-x.
References
- 1.Chan DC. Mitochondrial fusion and fission in mammals. Annu Rev. Cell Dev. Biol. 2006;22:79–99. doi: 10.1146/annurev.cellbio.22.010305.104638. [DOI] [PubMed] [Google Scholar]
- 2.Youle RJ, van der Bliek AM. Mitochondrial fission, fusion, and stress. Science. 2012;337:1062–1065. doi: 10.1126/science.1219855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tilokani L, Nagashima S, Paupe V, Prudent J. Mitochondrial dynamics: overview of molecular mechanisms. Essays Biochem. 2018;62:341–360. doi: 10.1042/EBC20170104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chan DC. Fusion and fission: interlinked processes critical for mitochondrial health. Annu. Rev. Genet. 2012;46:265–287. doi: 10.1146/annurev-genet-110410-132529. [DOI] [PubMed] [Google Scholar]
- 5.Labrousse AM, Zappaterra MD, Rube DA, van der Bliek AM. C. elegans dynamin-related protein DRP-1 controls severing of the mitochondrial outer membrane. Mol. Cell. 1999;4:815–826. doi: 10.1016/S1097-2765(00)80391-3. [DOI] [PubMed] [Google Scholar]
- 6.Kalia R, et al. Structural basis of mitochondrial receptor binding and constriction by DRP1. Nature. 2018;558:401–405. doi: 10.1038/s41586-018-0211-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lee JE, Westrate LM, Wu H, Page C, Voeltz GK. Multiple dynamin family members collaborate to drive mitochondrial division. Nature. 2016;540:139–143. doi: 10.1038/nature20555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Smirnova E, Griparic L, Shurland DL, van der Bliek AM. Dynamin-related protein Drp1 is required for mitochondrial division in mammalian cells. Mol. Biol. Cell. 2001;12:2245–2256. doi: 10.1091/mbc.12.8.2245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Korobova F, Ramabhadran V, Higgs HN. An actin-dependent step in mitochondrial fission mediated by the ER-associated formin INF2. Science. 2013;339:464–467. doi: 10.1126/science.1228360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Korobova F, Gauvin TJ, Higgs HN. A role for myosin II in mammalian mitochondrial fission. Curr. Biol. 2014;24:409–414. doi: 10.1016/j.cub.2013.12.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nemani N, et al. MIRO-1 determines mitochondrial shape transition upon GPCR activation and Ca(2+) stress. Cell Rep. 2018;23:1005–1019. doi: 10.1016/j.celrep.2018.03.098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Frank M, et al. Mitophagy is triggered by mild oxidative stress in a mitochondrial fission dependent manner. Biochim. Biophys. Acta. 2012;1823:2297–2310. doi: 10.1016/j.bbamcr.2012.08.007. [DOI] [PubMed] [Google Scholar]
- 13.Wang Y, et al. Mitochondrial fission promotes the continued clearance of apoptotic cells by macrophages. Cell. 2017;171:331–345 e322. doi: 10.1016/j.cell.2017.08.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Parker DJ, et al. A new mitochondrial pool of cyclin E, regulated by Drp1, is linked to cell-density-dependent cell proliferation. J. Cell Sci. 2015;128:4171–4182. doi: 10.1242/jcs.172429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Toda C, et al. UCP2 regulates mitochondrial fission and ventromedial nucleus control of glucose responsiveness. Cell. 2016;164:872–883. doi: 10.1016/j.cell.2016.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gurtner GC, Werner S, Barrandon Y, Longaker MT. Wound repair and regeneration. Nature. 2008;453:314–321. doi: 10.1038/nature07039. [DOI] [PubMed] [Google Scholar]
- 17.Werner S, Grose R. Regulation of wound healing by growth factors and cytokines. Physiol. Rev. 2003;83:835–870. doi: 10.1152/physrev.2003.83.3.835. [DOI] [PubMed] [Google Scholar]
- 18.Cordeiro JV, Jacinto A. The role of transcription-independent damage signals in the initiation of epithelial wound healing. Nat. Rev. Mol. Cell Biol. 2013;14:249–262. doi: 10.1038/nrm3541. [DOI] [PubMed] [Google Scholar]
- 19.Eming SA, Wynn TA, Martin P. Inflammation and metabolism in tissue repair and regeneration. Science. 2017;356:1026–1030. doi: 10.1126/science.aam7928. [DOI] [PubMed] [Google Scholar]
- 20.Davalos D, et al. ATP mediates rapid microglial response to local brain injury in vivo. Nat. Neurosci. 2005;8:752–758. doi: 10.1038/nn1472. [DOI] [PubMed] [Google Scholar]
- 21.Yin J, Xu K, Zhang J, Kumar A, Yu FS. Wound-induced ATP release and EGF receptor activation in epithelial cells. J. Cell Sci. 2007;120:815–825. doi: 10.1242/jcs.03389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Niethammer P, Grabher C, Look AT, Mitchison TJ. A tissue-scale gradient of hydrogen peroxide mediates rapid wound detection in zebrafish. Nature. 2009;459:996–999. doi: 10.1038/nature08119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Xu S, Chisholm AD. A Galphaq-Ca(2)(+) signaling pathway promotes actin-mediated epidermal wound closure in C. elegans. Curr. Biol. 2011;21:1960–1967. doi: 10.1016/j.cub.2011.10.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Razzell W, Evans IR, Martin P, Wood W. Calcium flashes orchestrate the wound inflammatory response through DUOX activation and hydrogen peroxide release. Curr. Biol. 2013;23:424–429. doi: 10.1016/j.cub.2013.01.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Soto X, et al. Inositol kinase and its product accelerate wound healing by modulating calcium levels, Rho GTPases, and F-actin assembly. Proc. Natl Acad. Sci. USA. 2013;110:11029–11034. doi: 10.1073/pnas.1217308110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Xu S, Chisholm AD. C. elegans epidermal wounding induces a mitochondrial ROS burst that promotes wound repair. Dev. Cell. 2014;31:48–60. doi: 10.1016/j.devcel.2014.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Horn A, et al. Mitochondrial redox signaling enables repair of injured skeletal muscle cells. Sci. Signal. 2017;10:eaaj1978. doi: 10.1126/scisignal.aaj1978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Janda J, Nfonsam V, Calienes F, Sligh JE, Jandova J. Modulation of ROS levels in fibroblasts by altering mitochondria regulates the process of wound healing. Arch. Dermatol. Res. 2016;308:239–248. doi: 10.1007/s00403-016-1628-9. [DOI] [PubMed] [Google Scholar]
- 29.Demyanenko IA, et al. Mitochondria-targeted antioxidant SkQ1 improves dermal wound healing in genetically diabetic mice. Oxid. Med. Cell. Longev. 2017;2017:6408278. doi: 10.1155/2017/6408278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Muliyil S, Narasimha M, Mitochondrial ROS. regulates cytoskeletal and mitochondrial remodeling to tune cell and tissue dynamics in a model for wound healing. Dev. Cell. 2014;28:239–252. doi: 10.1016/j.devcel.2013.12.019. [DOI] [PubMed] [Google Scholar]
- 31.Rolland SG, Lu Y, David CN, Conradt B. The BCL-2-like protein CED-9 of C. elegans promotes FZO-1/Mfn1,2- and EAT-3/Opa1-dependent mitochondrial fusion. J. Cell Biol. 2009;186:525–540. doi: 10.1083/jcb.200905070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chen H, Chomyn A, Chan DC. Disruption of fusion results in mitochondrial heterogeneity and dysfunction. J. Biol. Chem. 2005;280:26185–26192. doi: 10.1074/jbc.M503062200. [DOI] [PubMed] [Google Scholar]
- 33.Chen H, et al. Mitochondrial fusion is required for mtDNA stability in skeletal muscle and tolerance of mtDNA mutations. Cell. 2010;141:280–289. doi: 10.1016/j.cell.2010.02.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.De Vos KJ, Allan VJ, Grierson AJ, Sheetz MP. Mitochondrial function and actin regulate dynamin-related protein 1-dependent mitochondrial fission. Curr. Biol. 2005;15:678–683. doi: 10.1016/j.cub.2005.02.064. [DOI] [PubMed] [Google Scholar]
- 35.Wang S, et al. A toolkit for GFP-mediated tissue-specific protein degradation in C. elegans. Development. 2017;144:2694–2701. doi: 10.1242/dev.150094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kanazawa T, et al. The C. elegans Opa1 homologue EAT-3 is essential for resistance to free radicals. PLoS Genet. 2008;4:e1000022. doi: 10.1371/journal.pgen.1000022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ichishita R, et al. An RNAi screen for mitochondrial proteins required to maintain the morphology of the organelle in Caenorhabditis elegans. J. Biochem. 2008;143:449–454. doi: 10.1093/jb/mvm245. [DOI] [PubMed] [Google Scholar]
- 38.Toyama EQ, et al. Metabolism. AMP-activated protein kinase mediates mitochondrial fission in response to energy stress. Science. 2016;351:275–281. doi: 10.1126/science.aab4138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wang X, Schwarz TL. The mechanism of Ca2+ -dependent regulation of kinesin-mediated mitochondrial motility. Cell. 2009;136:163–174. doi: 10.1016/j.cell.2008.11.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Fransson S, Ruusala A, Aspenstrom P. The atypical Rho GTPases Miro-1 and Miro-2 have essential roles in mitochondrial trafficking. Biochem. Biophys. Res. Commun. 2006;344:500–510. doi: 10.1016/j.bbrc.2006.03.163. [DOI] [PubMed] [Google Scholar]
- 41.Reis K, Fransson A, Aspenstrom P. The Miro GTPases: at the heart of the mitochondrial transport machinery. FEBS Lett. 2009;583:1391–1398. doi: 10.1016/j.febslet.2009.04.015. [DOI] [PubMed] [Google Scholar]
- 42.Chuang M, Hsiao TI, Tong A, Xu S, Chisholm AD. DAPK interacts with Patronin and the microtubule cytoskeleton in epidermal development and wound repair. eLife. 2016;5:e15833. doi: 10.7554/eLife.15833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Yoo SK, Freisinger CM, LeBert DC, Huttenlocher A. Early redox, Src family kinase, and calcium signaling integrate wound responses and tissue regeneration in zebrafish. J. Cell Biol. 2012;199:225–234. doi: 10.1083/jcb.201203154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gottlieb RA. Cytochrome P450: major player in reperfusion injury. Arch. Biochem. Biophys. 2003;420:262–267. doi: 10.1016/j.abb.2003.07.004. [DOI] [PubMed] [Google Scholar]
- 45.Davydov DR. Microsomal monooxygenase in apoptosis: another target for cytochrome c signaling? Trends Biochem. Sci. 2001;26:155–160. doi: 10.1016/S0968-0004(00)01749-7. [DOI] [PubMed] [Google Scholar]
- 46.Bhattacharyya S, Sinha K, Sil PC. Cytochrome P450s: mechanisms and biological implications in drug metabolism and its interaction with oxidative stress. Curr. Drug Metab. 2014;15:719–742. doi: 10.2174/1389200215666141125121659. [DOI] [PubMed] [Google Scholar]
- 47.Wang W, et al. Superoxide flashes in single mitochondria. Cell. 2008;134:279–290. doi: 10.1016/j.cell.2008.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Helle SCJ, et al. Mechanical force induces mitochondrial fission. eLife. 2017;6:e30292. doi: 10.7554/eLife.30292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Zhang Q, et al. Circulating mitochondrial DAMPs cause inflammatory responses to injury. Nature. 2010;464:104–107. doi: 10.1038/nature08780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Niethammer P. The early wound signals. Curr. Opin. Genet. Dev. 2016;40:17–22. doi: 10.1016/j.gde.2016.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Schuler MH, et al. Miro1-mediated mitochondrial positioning shapes intracellular energy gradients required for cell migration. Mol. Biol. Cell. 2017;28:2159–2169. doi: 10.1091/mbc.e16-10-0741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zhao H, et al. Cytochrome P450 (CYP) epoxygenases as potential targets in the management of impaired diabetic wound healing. Lab. Invest. 2017;97:782–791. doi: 10.1038/labinvest.2017.21. [DOI] [PubMed] [Google Scholar]
- 53.Sander AL, et al. Cytochrome P450-derived epoxyeicosatrienoic acids accelerate wound epithelialization and neovascularization in the hairless mouse ear wound model. Langenbecks Arch. Surg. 2011;396:1245–1253. doi: 10.1007/s00423-011-0838-z. [DOI] [PubMed] [Google Scholar]
- 54.Noordermeer MA, Veldink GA, Vliegenthart JF. Fatty acid hydroperoxide lyase: a plant cytochrome p450 enzyme involved in wound healing and pest resistance. Chembiochem. 2001;2:494–504. doi: 10.1002/1439-7633(20010803)2:7/8<494::AID-CBIC494>3.0.CO;2-1. [DOI] [PubMed] [Google Scholar]
- 55.Thom SR. Oxidative stress is fundamental to hyperbaric oxygen therapy. J. Appl. Physiol. 2009;106:988–995. doi: 10.1152/japplphysiol.91004.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Zamboni WA, Browder LK, Martinez J. Hyperbaric oxygen and wound healing. Clin. Plast. Surg. 2003;30:67–75. doi: 10.1016/S0094-1298(02)00068-8. [DOI] [PubMed] [Google Scholar]
- 57.Frokjaer-Jensen C, et al. Random and targeted transgene insertion in Caenorhabditis elegans using a modified Mos1 transposon. Nat. Methods. 2014;11:529–534. doi: 10.1038/nmeth.2889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Xu S, Wang Z, Kim KW, Jin Y, Chisholm AD. Targeted mutagenesis of duplicated genes in Caenorhabditis elegans using CRISPR-Cas9. J. Genet. Genomics. 2016;43:103–106. doi: 10.1016/j.jgg.2015.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Calvo SE, Clauser KR, Mootha VK. MitoCarta2.0: an updated inventory of mammalian mitochondrial proteins. Nucleic Acids Res. 2016;44:D1251–D1257. doi: 10.1093/nar/gkv1003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Dickinson DJ, Pani AM, Heppert JK, Higgins CD, Goldstein B. Streamlined genome engineering with a self-excising drug selection cassette. Genetics. 2015;200:1035–1049. doi: 10.1534/genetics.115.178335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Yan D, Wu Z, Chisholm AD, Jin Y. The DLK-1 kinase promotes mRNA stability and local translation in C. elegans synapses and axon regeneration. Cell. 2009;138:1005–1018. doi: 10.1016/j.cell.2009.06.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Han X, et al. Mapping the mouse cell atlas by microwell-seq. Cell. 2018;172:1091–1107 e1017. doi: 10.1016/j.cell.2018.02.001. [DOI] [PubMed] [Google Scholar]
- 63.Dobin A, et al. STAR: ultrafast universal RNA-seq aligner. Bioinformatics. 2013;29:15–21. doi: 10.1093/bioinformatics/bts635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Liao Y, Smyth GK, Shi W. featureCounts: an efficient general purpose program for assigning sequence reads to genomic features. Bioinformatics. 2014;30:923–930. doi: 10.1093/bioinformatics/btt656. [DOI] [PubMed] [Google Scholar]
- 65.Love MI, Huber W, Anders S. Moderated estimation of fold change and dispersion for RNA-seq data with DESeq2. Genome Biol. 2014;15:550. doi: 10.1186/s13059-014-0550-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Huang da W, Sherman BT, Lempicki RA. Systematic and integrative analysis of large gene lists using DAVID bioinformatics resources. Nat. Protoc. 2009;4:44–57. doi: 10.1038/nprot.2008.211. [DOI] [PubMed] [Google Scholar]
- 67.Gu Z, Eils R, Schlesner M. Complex heatmaps reveal patterns and correlations in multidimensional genomic data. Bioinformatics. 2016;32:2847–2849. doi: 10.1093/bioinformatics/btw313. [DOI] [PubMed] [Google Scholar]
- 68.Liang CC, Park AY, Guan JL. In vitro scratch assay: a convenient and inexpensive method for analysis of cell migration in vitro. Nat. Protoc. 2007;2:329–333. doi: 10.1038/nprot.2007.30. [DOI] [PubMed] [Google Scholar]
- 69.Koopman M, et al. A screening-based platform for the assessment of cellular respiration in Caenorhabditis elegans. Nat. Protoc. 2016;11:1798–1816. doi: 10.1038/nprot.2016.106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Zhou Junxiang, Wang Xin, Wang Min, Chang Yuwei, Zhang Fengxia, Ban Zhaonan, Tang Ruofeng, Gan Qiwen, Wu Shaohuan, Guo Ye, Zhang Qian, Wang Fengyang, Zhao Liyuan, Jing Yudong, Qian Wenfeng, Wang Guodong, Guo Weixiang, Yang Chonglin. The lysine catabolite saccharopine impairs development by disrupting mitochondrial homeostasis. The Journal of Cell Biology. 2018;218(2):580–597. doi: 10.1083/jcb.201807204. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Description of Additional Supplementary Files
Data Availability Statement
The authors declare that all data supporting the findings of this study are available within this article, its supplementary information files, the peer-review file, the source data file, or are available from the corresponding author upon reasonable request. The RNA sequencing data generated and analyzed in this study are available upon request as well as from the Sequence Read Archive (SRA) at NCBI at the following accession code: PRJNA523321 [https://www.ncbi.nlm.nih.gov/sra/?term=PRJNA523321]. The source data underlying Figs. 1e, 2b, d, g, i, 3d, f, 4b, c, f, 5a, b, 6e–I, n–p, and 7b-e, and Supplementary Figs. 1d, f, 2c–e, 3c, 4f, g, 5a, g, and 7a, c, d, e, g–i are provided as a Source Data file.