ABSTRACT
Muscular dystrophies (MDs) encompass a wide variety of inherited disorders that are characterized by loss of muscle tissue associated with a progressive reduction in muscle function. With a cure lacking for MDs, preclinical developments of therapeutic approaches depend on well-characterized animal models that recapitulate the specific pathology in patients. The mouse is the most widely and extensively used model for MDs, and it has played a key role in our understanding of the molecular mechanisms underlying MD pathogenesis. This has enabled the development of therapeutic strategies. Owing to advancements in genetic engineering, a wide variety of mouse models are available for the majority of MDs. Here, we summarize the characteristics of the most commonly used mouse models for a subset of highly studied MDs, collated into a table. Together with references to key publications describing these models, this brief but detailed overview would be useful for those interested in, or working with, mouse models of MD.
KEY WORDS: Disease pathology, Mouse models, Muscular dystrophy
Summary: This Review and its accompanying comprehensive table summarize the most commonly used mouse models for a subset of highly studied muscular dystrophies.
Introduction
Muscular dystrophies (MDs) are a clinically and genetically heterogeneous group of inherited disorders. They are characterized by progressive muscle weakness affecting skeletal muscles, but some MDs involve cardiac and/or smooth muscles (Emery, 2002; Mercuri and Muntoni, 2013). Age of onset, disease severity and progression varies markedly between the different MDs. To date, more than 50 causative genes have been identified. Historically, MDs were classified based on the main clinical manifestations and the age of onset. Later, the mode of inheritance was also taken into account, resulting in further sub-classification of limb-girdle muscular dystrophy (LGMD) and congenital muscular dystrophy (CMD).
Importance of mouse models for studying disease mechanism and potential therapies
The availability of animal models of MDs plays a key role in studying disease pathology. Despite differences in some pathological hallmarks compared to humans, animal models have provided important insights into causal gene relationships and into the functional cellular and molecular mechanisms of disease pathogenesis. Consequently, a variety of therapeutic approaches have been developed using these models for MDs. Animal models play a pivotal role in preclinical studies to progress therapies to the clinic, from proof-of-principle studies, dosage and efficacy studies to extended preclinical trials (Allamand, 2000; Durbeej and Campbell, 2002).
Mice are the most frequently used models of MDs, as they are easy and relatively inexpensive to breed and maintain in large numbers, and to handle, treat and genetically modify. They are ideal subjects for preclinical studies owing to their small body size, short gestation and life span, and the abundance of experimental reagents available, such as antibodies and expression constructs. In addition, the mouse genome is well characterized and is largely comparable to the human genome. Moreover, detailed natural life-history data are available for an increasing number of mouse strains, providing crucial information for the accurate design of preclinical studies. Especially in the last decade, the research community has highlighted the need for detailed natural life-history data from both MD patients and the mouse models. This call arose due to the failure of several drugs in clinical trials despite encouraging preclinical data (Kornegay et al., 2014; Straub and Mercuri, 2018). As such, multiple international initiatives aim to improve preclinical trial design and execution (Gordish-Dressman et al., 2018; Heslop et al., 2015; Nagaraju et al., 2009). The TREAT-NMD Alliance has coordinated the generation and maintenance of standard operating procedures (SOPs) for several widely used outcome measures for the most commonly used mouse models of Duchenne muscular dystrophy (DMD) (Nagaraju et al., 2009; Willmann et al., 2011a), spinal muscular atrophy (SMA) (Willmann et al., 2011b) and CMD (Saunier et al., 2016). Detailed information is available on the TREAT-NMD website (https://treat-nmd.org/research-overview/preclinical-research/). These SOPs have now been downloaded worldwide more than 11,000 times in the last 7 years, and have been implemented in many research publications (Carlson et al., 2011; Mantuano et al., 2018; Mele et al., 2019; Tam et al., 2015; Zschüntzsch et al., 2016). It is hoped that implementation of the SOPs reduces intra- and inter-variability between complying laboratories. For mouse models of other MDs, these initiatives are either ongoing or planned.
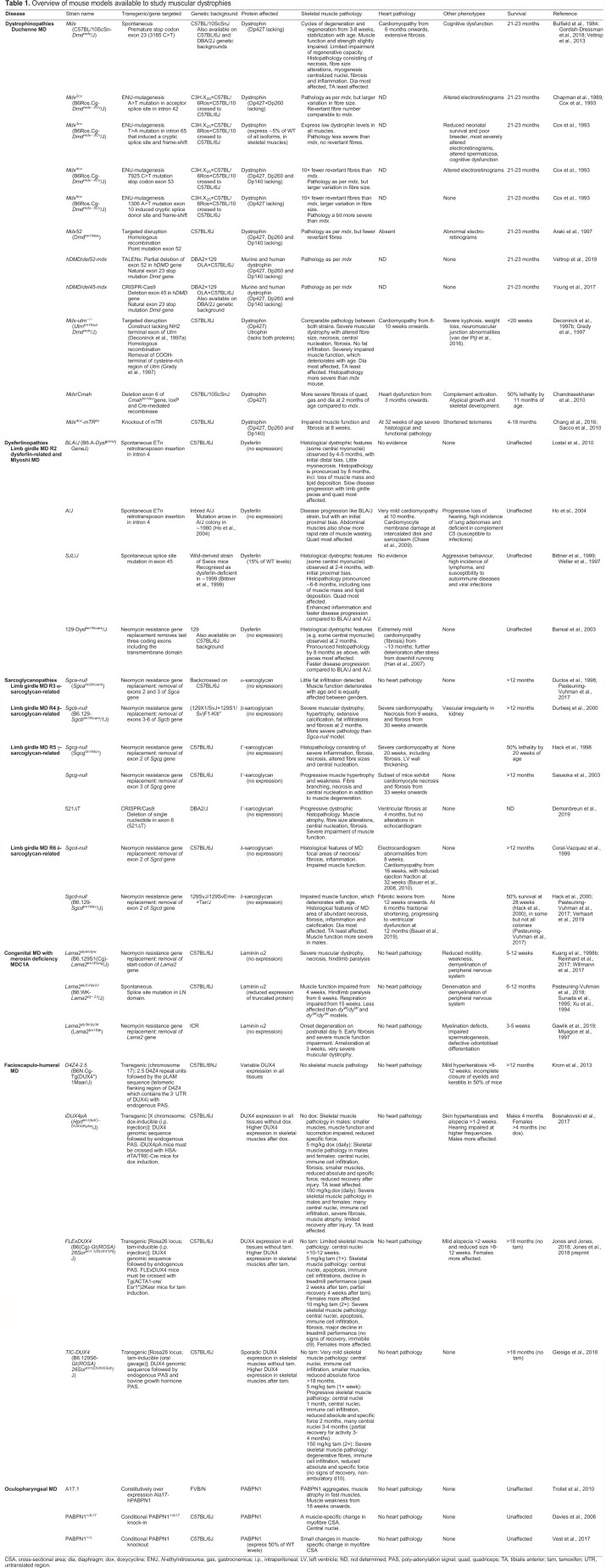
In Table 1, we provide a detailed overview of the main disease characteristics of the most commonly used mouse models in preclinical research for nine MDs, with a focus on those used extensively in preclinical trials and those that were crucial to elucidate aspects of the pathology of each MD.
Table 1.
Overview of mouse models available to study muscular dystrophies
Technologies to generate mouse models for MDs
Naturally occurring dystrophic mouse strains, in which a spontaneous mutation results in an MD phenotype (e.g. mdx, A/J, SJL/J and dy2J/dy2J), make up the minority of the available models. The majority of the mouse models have been genetically engineered, either by overexpressing the mutated gene or replacing the wild-type (WT) gene using a variety of non-targeted or targeted methods. Here, we briefly explain each of these approaches. For more comprehensive reviews on gene-editing techniques for the generation of mouse models, we refer the reader to Gurumurthy and Lloyd (2019), Hall et al. (2009) and Justice et al. (2011).
Non-targeted gene disruption
Some strains described in Table 1 have been generated using a non-targeted approach, by chemicals that randomly induce point mutations throughout the genome. N-ethylnitrosourea (ENU) is a commonly used mutagen that randomly mutates the DNA with a frequency of 1 mutation per 700 loci (Stottmann and Beier, 2014). The offspring of ENU-exposed mice are then screened for a marker for the disease: for instance, in the case of mdx2–5cv models, female offspring were screened for muscle dystrophy by assessing creatine kinase (CK) levels in blood, a marker of muscle leakiness (Chapman et al., 1989; Cox et al., 1993; Im et al., 1996). Carrier mice with elevated CK levels were then further investigated for muscle pathology, and their genomes were subsequently sequenced to identify the specific mutation.
Targeted gene disruption
The majority of the knockout mouse models that are available for MDs were generated via gene targeting. There are several protocols, but they all employ the cell-intrinsic homologous recombination DNA repair mechanism to insert a targeting vector in a homologous genetic locus of interest (Hall et al., 2009). Consequently, cells lack the targeted sequences (i.e. one or multiple exons) and fail to express the corresponding protein. The procedure requires a vector, which has a specific make-up depending on the method used. Generally, this vector contains the sequences of the regions flanking the exon(s) of interest and, in the middle of this, a drug selection marker (like that for neomycin resistance), which replaces the exon(s) of interest in the cell and allows for cell selection (Bouabe and Okkenhaug, 2013). Some vectors also contain recombinase-binding elements such as LoxP or Flp recombination target sites. Via electroporation, the vector is introduced into murine embryonic stem cells, which are then cultured and selected based on the resistance for the selection marker of choice. The resistant cells are then injected into a mouse blastocyst from which a knockout offspring develops.
The transcription activator-like effector nuclease (TALEN) technology (Cermak et al., 2011) has been used to generate the hDMD/del52-mdx model (Veltrop et al., 2018). For this model, TALENs induced double-strand breaks in the region of interest of a gene. Consequently, cells repaired these breaks through the non-homologous end-joining (NHEJ) DNA repair process. This is the dedicated repair mechanism to restore double-strand DNA breaks in non-dividing cells, in which DNA ends are ligated without the use of a template in an error-prone manner that typically disrupts the open reading frame, knocking out the gene of interest.
Recently, CRISPR/Cas9 technology has been used to rapidly engineer precise human mutations, generating many new mouse models (Cong et al., 2013). Several variations of the CRISPR/Cas9 system have been used, e.g. to generate the hDMD/del45-mdx (Young et al., 2017) and Dmddel8-34 models for DMD (Egorova et al., 2019), and the 521ΔT model for LGMD R5 γ-sarcoglycan-related (Demonbreun et al., 2019). For the DMD models, guide RNAs were designed to target the region of interest and to guide the Cas9 nuclease to this region to execute the cuts. NHEJ ensured the deletion of this particular region. The 521ΔT model for LGMD R5 γ-sarcoglycan-related (Demonbreun et al., 2019), on the other hand, is a knock-in model: here, a mutated part of exon 6 was used as repair template, which replaced the intact intrinsic exon 6 sequence upon a CRISPR/Cas9-mediated DNA break and homology-directed repair.
Dystrophinopathies
DMD is an X-linked progressive disorder caused by mutations in the DMD gene that result in the lack or defective forms of the structural muscle protein dystrophin and manifests in young children. The most commonly used DMD model is the mdx mouse (Bulfield et al., 1984; Willmann et al., 2009) and, to a lesser extent, its genetic variants mdx2cv, mdx3cv, mdx4cv, mdx5cv (Cox et al., 1993), mdx52 (Araki et al., 1997) and DMDnull (Kudoh et al., 2005). Mdx mice are primarily affected from 3 weeks onwards, when cycles of muscle necrosis and regeneration occur during the intense growth period. These cycles continue until ∼12 weeks of age, when 80% of myofibres have central myonuclei indicating past events of necrosis and regeneration (Coulton et al., 1988). Thereafter, the pathology stabilizes and adult mice have greatly reduced incidence of myonecrosis and mildly increasing fibrosis (Grounds, 2008). The diaphragm is more severely affected than other skeletal muscles because of impaired regeneration. Unlike in DMD patients, fat infiltrates are rarely seen in mdx mice. Cardiomyopathy is observed in mdx mice from ∼6 months of age.
To allow the use of human-specific sequences when investigating the potential of gene therapies (Verhaart and Aartsma-Rus, 2019; Aartsma-Rus and van Putten, 2020), mice carrying mutations in the human DMD gene have been generated [e.g. with a deletion of exon 45 in hDMD/del45-mdx (Young et al., 2017) or exon 52 in hDMD/del52-mdx strains (Veltrop et al., 2018)]. Natural life-history data are not yet available for these new humanized mouse strains, but their pathology appears to be similar to that of the classic mdx mouse (Veltrop et al., 2018; Young et al., 2017).
The mdx model is limited by its mild disease presentation and only slightly reduced lifespan. To overcome this, several additional mutations were crossed onto the mdx background generating double knockout mice. The mdx-utrn−/− mouse, which lacks dystrophin and its homologue utrophin, is most widely used (Deconinck et al., 1998; Grady et al., 1997). As utrophin is important for neuromuscular transmission, this double knockout is more severely affected and dies before ∼13 weeks of age owing to muscle weakness and respiratory problems. The mdx-utrn−/− mice also develop kyphosis and heart pathology at <8 weeks of age. These mice are therefore more useful to study survival. However, when evaluating drugs targeting pathology in this model, it is unknown whether a potential improvement is due to addressing pathology induced by lack of dystrophin or that induced by lack of utrophin; thus, it is difficult to determine their translational relevance to DMD.
Two newer double knockouts are the mdx/Cmah−/− (Chandrasekharan et al., 2010) and mdx4cv/mTRko strains (Sacco et al., 2010). Unlike mice, humans carry an inactivating deletion in the cytidine monophospho-N-acetylneuraminic acid hydroxylase (CMAH; also known as CMAHP) gene, which prevents glycosylation with N-glycolylneurominic acid. The mdx/Cmah−/− model also has a ‘humanized’ mutation in the Cmah gene and exhibits a more severe pathology (Chandrasekharan et al., 2010). This double knockout mouse also has impaired life span, with a 50% survival rate at 11 months of age. They have abundant fibrosis in skeletal muscles from 6 weeks onwards, and impaired heart function at 3 months (Betts et al., 2019). Growth and skeletal development is, however, atypical and does not reflect the human DMD trajectory (Wood et al., 2020).
The mdx4cv/mTRko mouse lacks the RNA component of telomerase and consequently has shortened telomeres, which are closer to the size observed in humans (Sacco et al., 2010). Telomeres protect chromosome ends from deterioration, and their length dictates the replicative lifespan of cells. It was hypothesized that the excellent regenerative capacity of mdx mice partly results from long telomeres in mice, and thus shortening the telomeres would impair muscle regeneration. The regenerative capacity of mdx4cv/mTRko mice is indeed impaired. Skeletal muscle function is affected at 8 weeks, with severe cardiac dysfunction observed in 32-week-old mdx4cv/mTRG2 mice (Mourkioti et al., 2013). As telomere length shortens with each generation of mdx4cv/mTR mice, the lifespan of second-generation mice is shorter than that of the first generation (Sacco et al., 2010). Nonetheless, the mdx4cv/mTRko strain has not yet been widely used in the research community.
Another way to exacerbate the disease pathology of mdx mice is to cross them onto a different genetic background (McGreevy et al., 2015). For example, the dystropathology worsens when mdx mice are bred on the DBA2/J background. The muscle function of this strain, called D2-mdx, is severely affected; their muscles are atrophic with extensive fibrosis and initial calcification that largely disappears with age (Coley et al., 2016; Gordish-Dressman et al., 2018; van Putten et al., 2019). Lastly, there are also several immune-deficient mdx strains, and mdx strains with mutations in additional genes as described in McGreevy et al. (2015). Owing to space restrictions, we did not include these in Table 1.
Dysferlinopathies
Dysferlinopathies are caused by lack of functional dysferlin, a membrane-associated calcium-binding protein involved in membrane repair. The pathologies usually manifest in young adults as Myoshi myopathy or LGMD R2 dysferlin-related (previously known as LGMD2B; Straub et al., 2018). In general, dysferlin-deficient (dysf−/−) mice mimic human dysferlinopathies, show a comparable disease progression with late-onset and similar, though milder, histopathological features, including loss of muscle mass, lipid droplets within slow twitch myofibres, adipocyte replacement of myofibres and inflammation (Grounds et al., 2014; Hornsey et al., 2013; https://www.jain-foundation.org/scientific-resources/research-tools/mouse-models-dysferlin-deficiency). Symptoms manifest in a muscle-specific manner, with the psoas and quadriceps muscles being some of the most affected by ∼8 months of age.
The most commonly studied dysf−/− models are the naturally occurring A/J (A/Jdysf−/−), SJL/J (SJL/Jdysf−/−) and BLA/J (B6.A-Dysfprmd/GeneJ) mice. In addition, genetically modified knockout strains are also available; for example, the 129-Dysftm1Kcam/J strain, which is also available in a C57BL/6J background (B6.129-Dysftm1Kcam/J).
Both the A/J and SJL/J mice have impairments that are not observed in dysferlinopathy patients or other dysf−/− mice (Ho et al., 2004). These include poor fertility and susceptibility to infection, which are proposed to be because of unknown modifiers within the genetic backgrounds rather than the dysferlin deficiency itself (Doetschman, 2009). Thus, the A/J and SJL/J dysf−/− mice were backcrossed onto the better-defined genetic backgrounds, C57BL/6J (producing the BLA/J mouse) and C57BL/10J strains, respectively; also providing each new strain with a genetically defined dysferlin-positive WT control.
Earlier studies, many of which were conducted before these strains were recognized as dysferlin-deficient, used A/J and SJL/J mice (identified by 2004 and 1999, respectively; see Table 1). More recently, the BLA/J mouse has become the more popular model owing to its similar phenotype to other dysf−/− models, reduced susceptibility to infections and the well-studied C57BL/6J background (Lostal et al., 2010).
Increased lipofuscin, a classical measure of cumulative oxidative damage, is an early histological change in dysf−/− muscles, detected at 3 months in A/J mice (Terrill et al., 2013). Marked histopathology is evident in selected muscles (psoas>quadriceps) by 8 months in all dysf−/− mice, with replacement of myofibres by adipocytes, which is more pronounced in older mice – studied up to 29 months of age (Albrecht et al., 2011; Hornsey et al., 2013; Terrill et al., 2013). However, the replacement of myofibres by adipocytes is not readily explained by myonecrosis, as this is relatively low (Terrill et al., 2013). The presence of conspicuous lipid droplets within dysf−/− myofibres of rodents and humans is recognized as a striking feature (Demonbreun et al., 2014; Grounds et al., 2014). Recent lipidomic studies in young BLA/J mice showed marked changes in lipid metabolism and lipid composition of dysf−/− muscles (Haynes et al., 2019).
Hornsey et al. provide a good review of the classic dysf−/− mouse models (Hornsey et al., 2013), and details of many dysf−/− strains are further provided on the Jain Foundation webpage (https://www.jain-foundation.org/scientific-resources/research-tools/mouse-models-dysferlin-deficiency).
Dysf−/− mice have also been crossed with many other strains that lack specific genes to further understand the role of dysferlin and associated proteins in disease pathogenesis, for example the C3-deficient (Han et al., 2010), dystrophin-deficient mdx (Han et al., 2011), myoferlin-null (Demonbreun et al., 2014), annexin A2 knockout (Defour et al., 2017) and ApoE-null mice (Sellers et al., 2018).
Sarcoglycanopathies
The α-, β-, γ- and δ-sarcoglycans are structural muscle proteins that are absent in sarcoglycanopathy patients, underlying progressive muscle wasting that manifests as LGMD R3, R4, R5 and R6, respectively (previously known as 2D, 2E, 2C and 2F). In sarcoglycanopathy patients, the medium age of onset is 6-8 years. The Sgca-null, Sgcb-null, Sgcg-null and Sgcd-null (Coral-Vazquez et al., 1999; Hack et al., 2000) mice are the classic models used to study the pathology of the α-, β-, γ- and δ-sarcoglycanopathies, respectively. These models display progressive muscle pathology and functional impairments of variable severity starting at 1 week of age, thereby emulating the human disease fairly accurately. Notably, all sarcoglycan-null models except the Sgca-null mice develop a cardiac phenotype from as early as 8 weeks (Coral-Vazquez et al., 1999; Durbeej et al., 2000; Hack et al., 1998).
As in the mdx strain, the pathology of Sgcg-null mice is more severe when crossed onto the DBA2/J genetic background (Heydemann et al., 2005). Recently, a novel variation of the Sgcg-null mouse has been generated, which, for the first time, allows investigation of exon skipping therapy for R5 γ-sarcoglycan-related LGMD patients (LGMD2C). The 521ΔT mouse has a single nucleotide deletion in exon 6, corresponding to the most common mutation found in patients (Demonbreun et al., 2019). Multi-skipping of exons 4, 5, 6 and 7 is required to restore the open reading frame, resulting in the expression of mini-γ sarcoglycan in these mice.
Congenital muscular dystrophies (CMDs)
CMDs are a large group of muscular dystrophies with an early age of onset. Here, we focus on two common CMDs that manifest at birth. In humans, defects in the α2 chain of laminin (also called merosin) and α-dystroglycan underlie merosin-deficient congenital muscular dystrophy type 1A (MDC1A) and the dystroglycanopathies, respectively (Durbeej, 2015; Gawlik and Durbeej, 2011; Saunier et al., 2016).
For laminin α2-deficiency, five mouse models have been regularly studied, with three described in Table 1: two knockouts (dy3K/dy3K and dyw/dyw) (Kuang et al., 1998a; Miyagoe et al., 1997), two spontaneous models (dy/dy and dy2J/dy2J) (Meier and Southard, 1970; Michelson et al., 1955) and an ENU-induced model (dy7J/dy7J) (Patton et al., 2008). They have mild to moderate muscular dystrophy evident at birth, with peripheral neuropathy and severely impaired life expectancy (5-12 weeks for dyw/dyw and 3 weeks for dy3K/dy3K mice), except for the dy2J/dy2J and dy7J/dy7J strains (life span of >6 months). The dyw/dyw strain is most commonly used, and the TREAT-NMD consortium have generated several SOPs for this model (https://treat-nmd.org/research-overview/preclinical-research/sops-for-cmd-animal-models/).
Detailed information on dystroglycanopathy models is provided on the Cure-CMD webpage (https://www.curecmd.org/resources-for-scientists).
Facioscapulohumeral muscular dystrophy (FSHD)
FSHD primarily affects the facial, shoulder and upper arm muscles. There is a large spread in the age of onset. Although most patients develop symptoms at ∼20 years of age, manifestations have been reported from infancy to 50 years of age. FSHD is caused by the epigenetic de-repression of the DUX4 retrogene encoded within each unit of the D4Z4 macrosatellite repeat array. The complex underlying genetics (Daxinger et al., 2015) have prevented the generation of a single mouse model that would represent the genetic and pathologic aspects of the human disease. There are several mouse models available where each recapitulates only specific aspects of the disease (Lek et al., 2015). As the D4Z4 repeat array encoding the DUX4 retrogene is specific to old-world primates, meaning that DUX4 is not expressed in mice (Leidenroth and Hewitt, 2010), this required the introduction of an exogenous genetic DUX4 construct. The first FSHD mouse model, the D4Z4-2.5 mouse, carries a contracted pathogenic FSHD allele of two and a half copies of the D4Z4 repeat unit. DUX4 expression can be detected in both skeletal muscles and non-muscle tissues and the D4Z4 locus is hypomethylated, as in FSHD patients. However, the mice do not present muscle weakness or wasting, which may partly be explained by the very low DUX4 expression levels in their skeletal muscles (Krom et al., 2013). More recently, several DUX4-inducible mice have been generated, which consequently show a dose-dependent severity of muscle histopathology and functional impairments (Bosnakovski et al., 2017; Giesige et al., 2018; Jones and Jones, 2018). It has, however, become apparent that the activation of the downstream targets of DUX4 in mice differs from that in humans. Finally, several xenograft models are also available, in which skeletal muscle tissue from FSHD patients (Chen et al., 2016; Zhang et al., 2014) or muscle precursor cells (Mueller et al., 2019; Sakellariou et al., 2016) are transplanted into a muscle of the mouse.
Oculopharyngeal muscular dystrophy (OPMD)
OPMD is a late-onset monogenic myopathy primarily affecting the eyelid and pharyngeal muscle groups, with symptom manifestation from 40-60 years of age. The genetic cause of the disease is an expansion of the alanine track at the N-terminus end of the gene encoding for poly(A) binding protein nuclear 1 (PABPN1). OPMD has been identified throughout the world. Most reported cases are autosomal dominant, but several recessive cases have also been reported (Brais, 2009; de Leeuw et al., 2019). On the protein level, the alanine expansion varies between +1 and +8 over the non-pathogenic 10 alanine track. The expanded PABPN1 forms insoluble nuclear aggregates, which represent the histopathological hallmark of the disease (Trollet et al., 1993). The first mouse models for OPMD were generated with a high and constitutive overexpression of the 17 alanine-expanded PABPN1, of which the A17.1 mouse is the most well-studied model (Davies et al., 2010). Studies in this mouse and in cellular models that were generated with overexpression of the expanded PABPN1 showed induction of cell death (Davies et al., 2006, 2010). However, cell death is not observed in the muscles of OPMD patients. Moreover, unlike the age-associated disease progression in OPMD patients, progression of muscle pathology in the A17.1 mouse is attenuated with age (Trollet et al., 2010). Interventions aimed at reducing PABPN1 aggregation were beneficial in mouse models that were generated by high overexpression. Whether these interventions are also beneficial for OPMD patients remains unresolved. Recently, Vest et al. generated a knock-in mouse model of Ala17, which captures some of OPMD pathological hallmarks (Vest et al., 2017). Additional studies in these mice are required to assess whether this is a good model for OPMD. So far, it is unclear whether PABPN1 aggregates are toxic and directly cause muscle weakness in OPMD. Several studies demonstrated that when PABPN1 expression levels are significantly reduced, below a certain threshold, it leads to muscle atrophy and wasting (Olie et al., 2019; Riaz et al., 2016; Vest et al., 2017). In muscles of OPMD patients, levels of PABPN1 correlate with disease progression (Anvar et al., 2013). It has been suggested that muscle weakness in OPMD is caused by a combination of accumulation and aggregation of expanded PABPN1 and an age-associated reduction in PABPN1 expression levels, which together reduce the availability of normal PABPN1 below a functional threshold (Raz and Raz, 2014). However, thus far, there is no animal model that emulates this combinatorial condition as in OPMD patients.
Conclusions
The availability of a variety of MD mouse models has greatly improved our understanding of pathogenesis and enabled the (pre)clinical development of several therapeutic approaches. Although these models allowed unprecedented opportunities for fundamental and applied research, their ever-increasing number also adds to the complexity of selecting the most appropriate model for a particular research question. The suitability of a certain model not only depends on the existence of the same genetic defect, but also on how well it emulates specific aspects of the human disease. Unfortunately, many MD mouse models are limited in their presentation of the human pathologies. These limitations, therefore, also add to the fact that the effects of a drug observed in mice may not necessarily predict the outcome in the clinical setting. To partly overcome these issues, the availability of natural life-history data for mouse models and of standardized operational procedures for in vivo outcome measures are pivotal for accurate study design and execution of high-quality preclinical research. Fortunately, these issues have received more attention in the last decade and are now in place for some MDs.
This article is part of a special subject collection ‘A Guide to Using Neuromuscular Disease Models for Basic and Preclinical Studies’, which was launched in a dedicated issue guest edited by Annemieke Aartsma-Rus, Maaike van Putten and James Dowling. See related articles in this collection at http://dmm.biologists.org/collection/neuromuscular.
Footnotes
Competing interests
The authors declare no competing or financial interests.
Funding
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
References
- Aartsma-Rus A. and van Putten M. (2020). The use of genetically humanized animal models for personalized medicine approaches. Dis. Model. Mech. 13, dmm041673 10.1242/dmm.041673 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Albrecht D. E., Garg N., Rufibach L. E., Williams B. A., Monnier N., Hwang E. and Mittal P. (2011). 4th annual dysferlin conference 11-14 september 2010, Washington, USA. Neuromuscul. Disord. 21, 304-310. 10.1016/j.nmd.2011.02.001 [DOI] [PubMed] [Google Scholar]
- Allamand V. (2000). Animal models for muscular dystrophy: valuable tools for the development of therapies. Hum. Mol. Genet. 9, 2459-2467. 10.1093/hmg/9.16.2459 [DOI] [PubMed] [Google Scholar]
- Anvar S. Y., Raz Y., Verway N., van der Sluijs B., Venema A., Goeman J. J., Vissing J., van der Maarel S. M., ‘t Hoen P. A. C., van Engelen B. G. M. et al. (2013). A decline in PABPN1 induces progressive muscle weakness in oculopharyngeal muscle dystrophy and in muscle aging. Aging 5, 412-426. 10.18632/aging.100567 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Araki E., Nakamura K., Nakao K., Kameya S., Kobayashi O., Nonaka I., Kobayashi T. and Katsuki M. (1997). Targeted disruption of exon 52 in the mouse dystrophin gene induced muscle degeneration similar to that observed in duchenne muscular dystrophy. Biochem. Biophys. Res. Commun. 238, 492-497. 10.1006/bbrc.1997.7328 [DOI] [PubMed] [Google Scholar]
- Bansal D., Miyake K., Vogel S. S., Groh S., Chen C.-C., Williamson R., McNeil P. L. and Campbell K. P. (2003). Defective membrane repair in dysferlin-deficient muscular dystrophy. Nature 423, 168-172. 10.1038/nature01573 [DOI] [PubMed] [Google Scholar]
- Bauer R., MacGowan G. A., Blain A., Bushby K. and Straub V. (2008). Steroid treatment causes deterioration of myocardial function in the δ-sarcoglycan-deficient mouse model for dilated cardiomyopathy. Cardiovasc. Res. 79, 652-661. 10.1093/cvr/cvn131 [DOI] [PubMed] [Google Scholar]
- Bauer R., Blain A., Greally E., Bushby K., Lochmüller H., Laval S., Straub V. and MacGowan G. A. (2010). Intolerance to β-blockade in a mouse model of δ-sarcoglycan-deficient muscular dystrophy cardiomyopathy. Eur. J. Heart Fail. 12, 1163-1170. 10.1093/eurjhf/hfq129 [DOI] [PubMed] [Google Scholar]
- Bauer R., Enns H., Jungmann A., Leuchs B., Volz C., Schinkel S., Koch W. J., Raake P. W., Most P., Katus H. A. et al. (2019). Various effects of AAV9-mediated βARKct gene therapy on the heart in dystrophin-deficient (mdx) mice and δ-sarcoglycan-deficient (Sgcd−/−) mice. Neuromuscul. Disord. 29, 231-241. 10.1016/j.nmd.2018.12.006 [DOI] [PubMed] [Google Scholar]
- Betts C. A., McClorey G., Healicon R., Hammond S. M., Manzano R., Muses S., Ball V., Godfrey C., Merritt T. M., Van Westering T. et al. (2019). Cmah-dystrophin deficient mdx mice display an accelerated cardiac phenotype that is improved following peptide-PMO exon skipping treatment. Hum. Mol. Genet. 28, 396-406. 10.1093/hmg/ddy346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bittner R. E., Anderson L. V. B., Burkhardt E., Bashir R., Vafiadaki E., Ivanova S., Raffelsberger T., Maerk I., Höger H., Jung M. et al. (1999). Dysferlin deletion in SJL mice (SJL-Dysf) defines a natural model for limb girdle muscular dystrophy 2B [2]. Nat. Genet. 23, 141-142. 10.1038/13770 [DOI] [PubMed] [Google Scholar]
- Bosnakovski D., Chan S. S. K., Recht O. O., Hartweck L. M., Gustafson C. J., Athman L. L., Lowe D. A. and Kyba M. (2017). Muscle pathology from stochastic low level DUX4 expression in an FSHD mouse model. Nat. Commun. 8, 550 10.1038/s41467-017-00730-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bouabe H. and Okkenhaug K. (2013). Gene targeting in mice: a review. Methods Mol. Biol. 1064, 315-336. 10.1007/978-1-62703-601-6_23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brais B. (2009). Oculopharyngeal muscular dystrophy: a polyalanine myopathy. Curr. Neurol. Neurosci. Rep. 9, 76-82. 10.1007/s11910-009-0012-y [DOI] [PubMed] [Google Scholar]
- Bulfield G., Siller W. G., Wight P. A. and Moore K. J. (1984). X chromosome-linked muscular dystrophy (mdx) in the mouse. Proc. Natl. Acad. Sci. USA 81, 1189-1192. 10.1073/pnas.81.4.1189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlson C. G., Bruemmer K., Sesti J., Stefanski C., Curtis H., Ucran J., Lachey J. and Seehra J. S. (2011). Soluble activin receptor type IIB increases forward pulling tension in the mdx mouse. Muscle Nerve 43, 694-699. 10.1002/mus.21944 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cermak T., Doyle E. L., Christian M., Wang L., Zhang Y., Schmidt C., Baller J. A., Somia N. V., Bogdanove A. J. and Voytas D. F. (2011). Efficient design and assembly of custom TALEN and other TAL effector-based constructs for DNA targeting. Nucleic Acids Res. 39, 7879 10.1093/nar/gkr739 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chandrasekharan K., Yoon J. H., Xu Y., DeVries S., Camboni M., Janssen P. M. L., Varki A. and Martin P. T. (2010). A human-specific deletion in mouse Cmah increases disease severity in the mdx model of duchenne muscular dystrophy. Sci. Transl. Med. 2, 42ra54 10.1126/scitranslmed.3000692 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang A. C. Y., Ong S.-G., LaGory E. L., Kraft P. E., Giaccia A. J., Wu J. C. and Blau H. M. (2016). Telomere shortening and metabolic compromise underlie dystrophic cardiomyopathy. Proc. Natl. Acad. Sci. USA 113, 13120-13125. 10.1073/pnas.1615340113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chapman V. M., Miller D. R., Armstrong D. and Caskey C. T. (1989). Recovery of induced mutations for X chromosome-linked muscular dystrophy in mice. Proc. Natl. Acad. Sci. USA 86, 1292-1296. 10.1073/pnas.86.4.1292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chase T. H., Cox G. A., Burzenski L., Foreman O. and Shultz L. D. (2009). Dysferlin deficiency and the development of cardiomyopathy in a mouse model of limb-girdle muscular dystrophy 2B. Am. J. Pathol. 175, 2299-2308. 10.2353/ajpath.2009.080930 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen J. C. J., King O. D., Zhang Y., Clayton N. P., Spencer C., Wentworth B. M., Emerson C. P. and Wagner K. R. (2016). Morpholino-mediated knockdown of DUX4 toward facioscapulohumeral muscular dystrophy therapeutics. Mol. Ther. 24, 1405-1411. 10.1038/mt.2016.111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coley W. D., Bogdanik L., Vila M. C., Yu Q., Van Der Meulen J. H., Rayavarapu S., Novak J. S., Nearing M., Quinn J. L., Saunders A. et al. (2016). Effect of genetic background on the dystrophic phenotype in mdx mice. Hum. Mol. Genet. 25, 130-145. 10.1093/hmg/ddv460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cong L., Ran F. A., Cox D., Lin S., Barretto R., Habib N., Hsu P. D., Wu X., Jiang W., Marraffini L. A. et al. (2013). Multiplex genome engineering using CRISPR/Cas systems. Science 339, 819-823. 10.1126/science.1231143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coral-Vazquez R., Cohn R. D., Moore S. A., Hill J. A., Weiss R. M., Davisson R. L., Straub V., Barresi R., Bansal D., Hrstka R. F. et al. (1999). Disruption of the sarcoglycan-sarcospan complex in vascular smooth muscle: a novel mechanism for cardiomyopathy and muscular dystrophy. Cell 98, 465-474. 10.1016/S0092-8674(00)81975-3 [DOI] [PubMed] [Google Scholar]
- Coulton G. R., Morgan J. E., Partridge T. A. and Sloper J. C. (1988). The mdx mouse skeletal muscle myopathy: I. A histological, morphometric and biochemical investigation. Neuropathol. Appl. Neurobiol. 14, 53-70. 10.1111/j.1365-2990.1988.tb00866.x [DOI] [PubMed] [Google Scholar]
- Cox G. A., Phelps S. F., Chapman V. M. and Chamberlain J. S. (1993). New mdx mutation disrupts expression of muscle and nonmuscle isoforms of dystrophin. Nat. Genet. 4, 87-93. 10.1038/ng0593-87 [DOI] [PubMed] [Google Scholar]
- Davies J. E., Sarkar S. and Rubinsztein D. C. (2006). Trehalose reduces aggregate formation and delays pathology in a transgenic mouse model of oculopharyngeal muscular dystrophy. Hum. Mol. Genet. 15, 23-31. 10.1093/hmg/ddi422 [DOI] [PubMed] [Google Scholar]
- Davies J. E., Rose C., Sarkar S. and Rubinsztein D. C. (2010). Cystamine suppresses polyalanine toxicity in a mouse model of oculopharyngeal muscular dystrophy. Sci. Transl. Med. 2, 34ra40 10.1126/scitranslmed.3000723 [DOI] [PubMed] [Google Scholar]
- Daxinger L., Tapscott S. J. and van der Maarel S. M. (2015). Genetic and epigenetic contributors to FSHD. Curr. Opin. Genet. Dev. 33, 56-61. 10.1016/j.gde.2015.08.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Leeuw R. H., Garnier D., Kroon R. M. J. M., Horlings C. G. C., de Meijer E., Buermans H., van Engelen B. G. M., de Knijff P. and Raz V. (2019). Diagnostics of short tandem repeat expansion variants using massively parallel sequencing and componential tools. Eur. J. Hum. Genet. 27, 400-407. 10.1038/s41431-018-0302-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deconinck A. E., Potter A. C., Tinsley J. M., Wood S. J., Vater R., Young C., Metzinger L., Vincent A., Slater C. R. and Davies K. E. (1997a). Postsynaptic abnormalities at the neuromuscular junctions of utrophin-deficient mice. J. Cell Biol. 136, 883-894. 10.1083/jcb.136.4.883 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deconinck A. E., Rafael J. A., Skinner J. A., Brown S. C., Potter A. C., Metzinger L., Watt D. J., Dickson J. G., Tinsley J. M. and Davies K. E. (1997b). Utrophin-dystrophin-deficient mice as a model for Duchenne muscular dystrophy. Cell 90, 717-727. 10.1016/S0092-8674(00)80532-2 [DOI] [PubMed] [Google Scholar]
- Deconinck N., Rafael J. A., Beckers-Bleukx G., Kahn D., Deconinck A. E., Davies K. E. and Gillis J. M. (1998). Consequences of the combined deficiency in dystrophin and utrophin on the mechanical properties and myosin composition of some limb and respiratory muscles of the mouse. Neuromuscul. Disord. 8, 362-370. 10.1016/S0960-8966(98)00048-0 [DOI] [PubMed] [Google Scholar]
- Defour A., Medikayala S., Van der Meulen J. H., Hogarth M. W., Holdreith N., Malatras A., Duddy W., Boehler J., Nagaraju K. and Jaiswal J. K. (2017). Annexin A2 links poor myofiber repair with inflammation and adipogenic replacement of the injured muscle. Hum. Mol. Genet. 26, 1979-1991. 10.1093/hmg/ddx065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Demonbreun A. R., Rossi A. E., Alvarez M. G., Swanson K. E., Deveaux H. K., Earley J. U., Hadhazy M., Vohra R., Walter G. A., Pytel P. et al. (2014). Dysferlin and myoferlin regulate transverse tubule formation and glycerol sensitivity. Am. J. Pathol. 184, 248-259. 10.1016/j.ajpath.2013.09.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Demonbreun A. R., Wyatt E. J., Fallon K. S., Oosterbaan C. C., Page P., Hadhazy M., Quattrocelli M., Barefield D. Y. and McNally E. M. (2019). A gene-edited mouse model of Limb-Girdle muscular dystrophy 2C for testing exon skipping. Dis. Model. Mech. 13, dmm040832 10.1242/dmm.040832 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doetschman T. (2009). Influence of genetic background on genetically engineered mouse phenotypes. Methods Mol. Biol. 530, 423-433. 10.1007/978-1-59745-471-1_23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duclos F., Straub V., Moore S. A., Venzke D. P., Hrstka R. F., Crosbie R. H., Durbeej M., Lebakken C. S., Ettinger A. J., van der Meulen J. et al. (1998). Progressive muscular dystrophy in alpha-sarcoglycan-deficient mice. J. Cell Biol. 142, 1461-1471. 10.1083/jcb.142.6.1461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Durbeej M. (2015). Laminin-alpha2 chain-deficient congenital muscular dystrophy: pathophysiology and development of treatment. Curr. Top. Membr. 76, 31-60. 10.1016/bs.ctm.2015.05.002 [DOI] [PubMed] [Google Scholar]
- Durbeej M. and Campbell K. P. (2002). Muscular dystrophies involving the dystrophin-glycoprotein complex: an overview of current mouse models. Curr. Opin. Genet. Dev. 12, 349-361. 10.1016/S0959-437X(02)00309-X [DOI] [PubMed] [Google Scholar]
- Durbeej M., Conn R. D., Hrstka R. F., Moore S. A., Allamand V., Davidson B. L., Williamson R. A. and Campbell K. P. (2000). Disruption of the β-sarcoglycan gene reveals pathogenetic complexity of limb-girdle muscular dystrophy type 2E. Mol. Cell 5, 141-151. 10.1016/S1097-2765(00)80410-4 [DOI] [PubMed] [Google Scholar]
- Egorova T. V., Zotova E. D., Reshetov D. A., Polikarpova A. V., Vassilieva S. G., Vlodavets D. V., Gavrilov A. A., Ulianov S. V., Buchman V. L. and Deykin A. V. (2019). CRISPR/Cas9-generated mouse model of Duchenne muscular dystrophy recapitulating a newly identified large 430 kb deletion in the human DMD gene. Dis. Model. Mech. 12, dmm037655 10.1242/dmm.037655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Emery A. E. H. (2002). Muscular dystrophy into the new millennium. Neuromuscul. Disord. 12, 343-349. 10.1016/S0960-8966(01)00303-0 [DOI] [PubMed] [Google Scholar]
- Gawlik K. I. and Durbeej M. (2011). Skeletal muscle laminin and MDC1A: pathogenesis and treatment strategies. Skelet Muscle 1, 9 10.1186/2044-5040-1-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gawlik K. I., Körner Z., Oliveira B. M. and Durbeej M. (2019). Early skeletal muscle pathology and disease progress in the dy3K/dy3K mouse model of congenital muscular dystrophy with laminin α2 chain-deficiency. Sci. Rep. 9, 14324 10.1038/s41598-019-50550-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giesige C. R., Wallace L. M., Heller K. N., Eidahl J. O., Saad N. Y., Fowler A. M., Pyne N. K., Al-Kharsan M., Rashnonejad A., Chermahini G. A. et al. (2018). AAV-mediated follistatin gene therapy improves functional outcomes in the TIC-DUX4 mouse model of FSHD. JCI Insight 3, 123538 10.1172/jci.insight.123538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordish-Dressman H., Willmann R., Dalle Pazze L., Kreibich A., van Putten M., Heydemann A., Bogdanik L., Lutz C., Davies K., Demonbruen A. R. et al. (2018). “Of mice and measures”: a project to improve how we advance duchenne muscular dystrophy therapies to the clinic. J. Neuromuscul. Dis. 5, 407-417. 10.3233/JND-180324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grady R. M., Teng H., Nichol M. C., Cunningham J. C., Wilkinson R. S. and Sanes J. R. (1997). Skeletal and cardiac myopathies in mice lacking utrophin and dystrophin: a model for Duchenne muscular dystrophy. Cell 90, 729-738. 10.1016/S0092-8674(00)80533-4 [DOI] [PubMed] [Google Scholar]
- Grounds M. D. (2008). Two-tiered hypotheses for Duchenne muscular dystrophy. Cell. Mol. Life Sci. 65, 1621-1625. 10.1007/s00018-008-7574-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grounds M. D., Terrill J. R., Radley-Crabb H. G., Robertson T., Papadimitriou J., Spuler S. and Shavlakadze T. (2014). Lipid accumulation in dysferlin-deficient muscles. Am. J. Pathol. 184, 1668-1676. 10.1016/j.ajpath.2014.02.005 [DOI] [PubMed] [Google Scholar]
- Gurumurthy C. B. and Lloyd K. C. K. (2019). Generating mouse models for biomedical research: technological advances. Dis. Model. Mech. 12, dmm029462 10.1242/dmm.029462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hack A. A., Ly C. T., Jiang F., Clendenin C. J., Sigrist K. S., Wollmann R. L. and McNally E. M. (1998). γ-sarcoglycan deficiency leads to muscle membrane defects and apoptosis independent of dystrophin. J. Cell Biol. 142, 1279-1287. 10.1083/jcb.142.5.1279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hack A. A., Lam M. Y., Cordier L., Shoturma D. I., Ly C. T., Hadhazy M. R. A., Hadhazy M. R. A., Sweeney H. L. and McNally E. M. (2000). Differential requirement for individual sarcoglycans and dystrophin in the assembly and function of the dystrophin-glycoprotein complex. J. Cell Sci. 113, 2535-2544. [DOI] [PubMed] [Google Scholar]
- Hall B., Limaye A. and Kulkarni A. B. (2009). Overview: generation of gene knockout mice. Curr. Protoc. Cell Biol. 44, 19.12.1-19.12.17. 10.1002/0471143030.cb1912s44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han R., Bansal D., Miyake K., Muniz V. P., Weiss R. M., McNeil P. L. and Campbell K. P. (2007). Dysferlin-mediated membrane repair protects the heart from stress-induced left ventricular injury. J. Clin. Invest. 117, 1805-1813. 10.1172/JCI30848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han R., Frett E. M., Levy J. R., Rader E. P., Lueck J. D., Bansal D., Moore S. A., Ng R., Beltrán-Valero de Bernabé D., Faulkner J. A. et al. (2010). Genetic ablation of complement C3 attenuates muscle pathology in dysferlin-deficient mice. J. Clin. Invest. 120, 4366-4374. 10.1172/JCI42390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han R., Rader E. P., Levy J. R., Bansal D. and Campbell K. P. (2011). Dystrophin deficiency exacerbates skeletal muscle pathology in dysferlin-null mice. Skelet. Muscle l, 35 10.1186/2044-5040-1-35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haynes V. R., Keenan S. N., Bayliss J., Lloyd E. M., Meikle P. J., Grounds M. D. and Watt M. J. (2019). Dysferlin deficiency alters lipid metabolism and remodels the skeletal muscle lipidome in mice. J. Lipid Res. 60, 1350-1364. 10.1194/jlr.M090845 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heslop E., Csimma C., Straub V., McCall J., Nagaraju K., Wagner K. R., Caizergues D., Korinthenberg R., Flanigan K. M., Kaufmann P. et al. (2015). The TREAT-NMD advisory committee for therapeutics (TACT): an innovative de-risking model to foster orphan drug development. Orphanet. J. Rare. Dis. 10, 49 10.1186/s13023-015-0258-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heydemann A., Huber J. M., Demonbreun A., Hadhazy M. and McNally E. M. (2005). Genetic background influences muscular dystrophy. Neuromuscul. Disord. 15, 601-609. 10.1016/j.nmd.2005.05.004 [DOI] [PubMed] [Google Scholar]
- Ho M., Post C. M., Donahue L. R., Lidov H. G. W., Bronson R. T., Goolsby H., Watkins S. C., Cox G. A. and Brown R. H. (2004). Disruption of muscle membrane and phenotype divergence in two novel mouse models of dysferlin deficiency. Hum. Mol. Genet. 13, 1999-2010. 10.1093/hmg/ddh212 [DOI] [PubMed] [Google Scholar]
- Hornsey M. A., Laval S. H., Barresi R., Lochmüller H. and Bushby K. (2013). Muscular dystrophy in dysferlin-deficient mouse models. Neuromuscul. Disord. 23, 377-387. 10.1016/j.nmd.2013.02.004 [DOI] [PubMed] [Google Scholar]
- Im W. B., Phelps S. F., Copen E. H., Adams E. G., Slightom J. L. and Chamberlain J. S. (1996). Differential expression of dystrophin isoforms in strains of mdx mice with different mutations. Hum. Mol. Genet. 5, 1149-1153. 10.1093/hmg/5.8.1149 [DOI] [PubMed] [Google Scholar]
- Jones T. and Jones P. L. (2018). A cre-inducible DUX4 transgenic mouse model for investigating facioscapulohumeral muscular dystrophy. PLoS ONE 13, e0192657 10.1371/journal.pone.0192657 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones T. I., Chew G.-L., Barraza-Flores P., Schreier S., Ramirez M., Wuebbles R. D., Burkin D. J., Bradley R. K. and Jones P. L. (2018). Transgenic mice expressing tunable levels of DUX4 develop characteristic facioscapulohumeral muscular dystrophy-like pathophysiology ranging in severity. bioRxiv 471094 10.1101/471094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Justice M. J., Siracusa L. D. and Stewart A. F. (2011). Technical approaches for mouse models of human disease. Dis. Model. Mech. 4, 305-310. 10.1242/dmm.000901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kornegay J. N., Spurney C. F., Nghiem P. P., Brinkmeyer-Langford C. L., Hoffman E. P. and Nagaraju K. (2014). Pharmacologic management of duchenne muscular dystrophy: Target identification and preclinical trials. ILAR J. 55, 119-149. 10.1093/ilar/ilu011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krom Y. D., Thijssen P. E., Young J. M., den Hamer B., Balog J., Yao Z., Maves L., Snider L., Knopp P., Zammit P. S. et al. (2013). Intrinsic epigenetic regulation of the D4Z4 macrosatellite repeat in a transgenic mouse model for FSHD. PLoS Genet. 9, e1003415 10.1371/journal.pgen.1003415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuang W., Xu H., Vachon P. H., Liu L., Loechel F., Wewer U. M. and Engvall E. (1998a). Merosin-deficient congenital muscular dystrophy. Partial genetic correction in two mouse models. J. Clin. Invest. 102, 844-852. 10.1172/JCI3705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuang W., Xu H., Vachon P. H. and Engvall E. (1998b). Disruption of the lama2 gene in embryonic stem cells: Laminin α2 is necessary for sustenance of mature muscle cells. Exp. Cell Res. 241, 117-125. 10.1006/excr.1998.4025 [DOI] [PubMed] [Google Scholar]
- Kudoh H., Ikeda H., Kakitani M., Ueda A., Hayasaka M., Tomizuka K. and Hanaoka K. (2005). A new model mouse for Duchenne muscular dystrophy produced by 2.4 Mb deletion of dystrophin gene using Cre-loxP recombination system. Biochem. Biophys. Res. Commun. 328, 507-516. 10.1016/j.bbrc.2004.12.191 [DOI] [PubMed] [Google Scholar]
- Leidenroth A. and Hewitt J. E. (2010). A family history of DUX4: phylogenetic analysis of DUXA, B, C and Duxbl reveals the ancestral DUX gene. BMC Evol. Biol. 10, 364 10.1186/1471-2148-10-364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lek A., Rahimov F., Jones P. L. and Kunkel L. M. (2015). Emerging preclinical animal models for FSHD. Trends Mol. Med. 21, 295-306. 10.1016/j.molmed.2015.02.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lostal W., Bartoli M., Bourg N., Roudaut C., Bentaïb A., Miyake K., Guerchet N., Fougerousse F., McNeil P. and Richard I. (2010). Efficient recovery of dysferlin deficiency by dual adeno-associated vector-mediated gene transfer. Hum. Mol. Genet. 19, 1897-1907. 10.1093/hmg/ddq065 [DOI] [PubMed] [Google Scholar]
- Mantuano P., Sanarica F., Conte E., Morgese M. G., Capogrosso R. F., Cozzoli A., Fonzino A., Quaranta A., Rolland J.-F., De Bellis M. et al. (2018). Effect of a long-term treatment with metformin in dystrophic mdx mice: a reconsideration of its potential clinical interest in Duchenne muscular dystrophy. Biochem. Pharmacol. 154, 89-103. 10.1016/j.bcp.2018.04.022 [DOI] [PubMed] [Google Scholar]
- McGreevy J. W., Hakim C. H., McIntosh M. A. and Duan D. (2015). Animal models of Duchenne muscular dystrophy: From basic mechanisms to gene therapy. DMM Dis. Model. Mech. 8, 195-213. 10.1242/dmm.018424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meier H. and Southard J. L. (1970). Muscular dystrophy in the mouse caused by an allele at the dy-locus. Life Sci. 9, 137-144. 10.1016/0024-3205(70)90306-1 [DOI] [PubMed] [Google Scholar]
- Mele A., Mantuano P., De Bellis M., Rana F., Sanarica F., Conte E., Morgese M. G., Bove M., Rolland J.-F., Capogrosso R. F. et al. (2019). A long-term treatment with taurine prevents cardiac dysfunction in mdx mice. Transl. Res. 204, 82-99. 10.1016/j.trsl.2018.09.004 [DOI] [PubMed] [Google Scholar]
- Mercuri E. and Muntoni F. (2013). Muscular dystrophies. Lancet 381, 845-860. 10.1016/S0140-6736(12)61897-2 [DOI] [PubMed] [Google Scholar]
- Michelson A. M., Russell E. S. and Harman P. J. (1955). Dystrophia muscularis: a hereditary primary myopathy in the house mouse. Proc. Natl. Acad. Sci. USA 41, 1079-1084. 10.1073/pnas.41.12.1079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miyagoe Y., Hanaoka K., Nonaka I., Hayasaka M., Nabeshima Y., Arahata K., Nabeshima Y. and Takeda S. (1997). Laminin alpha2 chain-null mutant mice by targeted disruption of the Lama2 gene: a new model of merosin (laminin 2)-deficient congenital muscular dystrophy. FEBS Lett. 415, 33-39. 10.1016/S0014-5793(97)01007-7 [DOI] [PubMed] [Google Scholar]
- Mourkioti F., Kustan J., Kraft P., Day J. W., Zhao M. M., Kost-Alimova M., Protopopov A., Depinho R. A., Bernstein D., Meeker A. K. et al. (2013). Role of telomere dysfunction in cardiac failure in Duchenne muscular dystrophy. Nat. Cell Biol. 15, 895-904. 10.1038/ncb2790 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mueller A. L., O'Neill A., Jones T. I., Llach A., Rojas L. A., Sakellariou P., Stadler G., Wright W. E., Eyerman D., Jones P. L. et al. (2019). Muscle xenografts reproduce key molecular features of facioscapulohumeral muscular dystrophy. Exp. Neurol. 320, 113011 10.1016/j.expneurol.2019.113011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagaraju K. and Willmann R. and TREAT-NMD Network and the Wellstone Muscular Dystrophy Cooperative Research Network (2009). Developing standard procedures for murine and canine efficacy studies of DMD therapeutics: report of two expert workshops on “Pre-clinical testing for Duchenne dystrophy”: Washington DC, October 27th-28th 2007 and Zurich, June 30th-July 1st 2008. Neuromuscul. Disord. 19, 502-506. 10.1016/j.nmd.2009.05.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olie C. S., Riaz M., Konietzny R., Charles P. D., Pinto-Fernandez A., Kiełbasa S. M., Aartsma-Rus A., Goeman J. J., Kessler B. M. and Raz V. (2019). Deacetylation inhibition reverses PABPN1-dependent muscle wasting. iScience 12, 318-332. 10.1016/j.isci.2019.01.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pasteuning-Vuhman S., Putker K., Tanganyika-De Winter C. L., Boertje-Van Der Meulen J. W., Van Vliet L., Overzier M., Plomp J. J., Aartsma-Rus A. and Van Putten M. (2017). Natural disease history of mouse models for limb girdle muscular dystrophy types 2D and 2F. PLoS ONE 12, e0182704 10.1371/journal.pone.0182704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pasteuning-Vuhman S., Putker K., Tanganyika-de Winter C. L., Boertje-van der Meulen J. W., Van Vliet L., Overzier M., Plomp J. J., Aartsma-Rus A. and Van Putten M. (2018). Natural disease history of the dy2Jmouse model of laminin α2 (merosin)-deficient congenital muscular dystrophy. PLoS ONE 13, e0197388 10.1371/journal.pone.0197388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patton B. L., Wang B., Tarumi Y. S., Seburn K. L. and Burgess R. W. (2008). A single point mutation in the LN domain of LAMA2 causes muscular dystrophy and peripheral amyelination. J. Cell Sci. 121, 1593-1604. 10.1242/jcs.015354 [DOI] [PubMed] [Google Scholar]
- Raz Y. and Raz V. (2014). Oculopharyngeal muscular dystrophy as a paradigm for muscle aging. Front. Aging Neurosci. 6, 317 10.3389/fnagi.2014.00317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reinhard J. R., Lin S., McKee K. K., Meinen S., Crosson S. C., Sury M., Hobbs S., Maier G., Yurchenco P. D. and Rüegg M. A. (2017). Linker proteins restore basement membrane and correct LAMA2-related muscular dystrophy in mice. Sci. Transl. Med. 9, eaal4649 10.1126/scitranslmed.aal4649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riaz M., Raz Y., van Putten M., Paniagua-Soriano G., Krom Y. D., Florea B. I. B. I. and Raz V. (2016). PABPN1-dependent mRNA processing induces muscle wasting. PLoS Genet. 12, e1006031 10.1371/journal.pgen.1006031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sacco A., Mourkioti F., Tran R., Choi J., Llewellyn M., Kraft P., Shkreli M., Delp S., Pomerantz J. H., Artandi S. E. et al. (2010). Short telomeres and stem cell exhaustion model Duchenne muscular dystrophy in mdx/mTR mice. Cell 143, 1059-1071. 10.1016/j.cell.2010.11.039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sakellariou P., O'Neill A., Mueller A. L., Stadler G., Wright W. E., Roche J. A. and Bloch R. J. (2016). Neuromuscular electrical stimulation promotes development in mice of mature human muscle from immortalized human myoblasts. Skelet. Muscle 6, 4 10.1186/s13395-016-0078-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sasaoka T., Imamura M., Araishi K., Noguchi S., Mizuno Y., Takagoshi N., Hama H., Wakabayashi-Takai E., Yoshimoto-Matsuda Y., Nonaka I. et al. (2003). Pathological analysis of muscle hypertrophy and degeneration in muscular dystrophy in γ-sarcoglycan-deficient mice. Neuromuscul. Disord. 13, 193-206. 10.1016/s0960-8966(02)00220-1 [DOI] [PubMed] [Google Scholar]
- Saunier M., Bönnemann C. G., Durbeej M., Allamand V., Bönnemann C. G., Durbeej M. and Allamand V. and CMD Animal Model Consortium (2016). 212th ENMC International Workshop: Animal models of congenital muscular dystrophies, Naarden, The Netherlands, 29-31 May 2015. Neuromuscul. Disord. 26, 252-259. 10.1016/j.nmd.2016.02.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sellers S. L., Milad N., White Z., Pascoe C., Chan R., Payne G. W., Seow C., Rossi F., Seidman M. A. and Bernatchez P. (2018). Increased nonHDL cholesterol levels cause muscle wasting and ambulatory dysfunction in the mouse model of LGMD2B. J. Lipid Res. 59, 261-272. 10.1194/jlr.M079459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stottmann R. and Beier D. (2014). ENU mutagenesis in the mouse. Curr. Protoc. Hum. Genet. 2014, 15.4.1-15.4.10. 10.1002/0471142905.hg1504s82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Straub V. and Mercuri E. (2018). Report on the workshop: Meaningful outcome measures for Duchenne muscular dystrophy, London, UK, 30–31 January 2017. Neuromuscul. Disord. 28, 690-701. 10.1016/j.nmd.2018.05.013 [DOI] [PubMed] [Google Scholar]
- Straub V., Murphy A. and Udd B. (2018). 229th ENMC international workshop: Limb girdle muscular dystrophies – Nomenclature and reformed classification Naarden, the Netherlands, 17–19 March 2017. Neuromuscul. Disord. 28, 702-710. 10.1016/j.nmd.2018.05.007 [DOI] [PubMed] [Google Scholar]
- Sunada Y., Bernier S. M., Utani A., Yamada Y. and Campbell K. P. (1995). Identification of a novel mutant transcript of laminin alpha 2 chain gene responsible for muscular dystrophy and dysmyelination in dy2J mice. Hum. Mol. Genet. 4, 1055-1061. 10.1093/hmg/4.6.1055 [DOI] [PubMed] [Google Scholar]
- Tam C. S., Power J. E., Markovic T. P., Yee C., Morsch M., McLennan S. V. and Twigg S. M. (2015). The effects of high-fat feeding on physical function and skeletal muscle extracellular matrix. Nutr. Diabetes 5, e187 10.1038/nutd.2015.39 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terrill J. R., Radley-Crabb H. G., Iwasaki T., Lemckert F. A., Arthur P. G. and Grounds M. D. (2013). Oxidative stress and pathology in muscular dystrophies: focus on protein thiol oxidation and dysferlinopathies. FEBS J. 280, 4149-4164. 10.1111/febs.12142 [DOI] [PubMed] [Google Scholar]
- Trollet C., Gidaro T., Klein P., Périé S., Butler-Browne G. and Lacau St Guily J. (1993). Oculopharyngeal Muscular Dystrophy. New York, NY: Springer New York. [Google Scholar]
- Trollet C., Anvar S. Y., Venema A., Hargreaves I. P., Foster K., Vignaud A., Ferry A., Negroni E., Hourde C., Baraibar M. A. et al. (2010). Molecular and phenotypic characterization of a mouse model of oculopharyngeal muscular dystrophy reveals severe muscular atrophy restricted to fast glycolytic fibres. Hum. Mol. Genet. 19, 2191-2207. 10.1093/hmg/ddq098 [DOI] [PubMed] [Google Scholar]
- van der Pijl E. M., van Putten M., Niks E. H., Verschuuren J. J. G. M., Aartsma-Rus A. and Plomp J. J. (2016). Characterization of neuromuscular synapse function abnormalities in multiple Duchenne muscular dystrophy mouse models. Eur. J. Neurosci. 43, 1623-1635. 10.1111/ejn.13249 [DOI] [PubMed] [Google Scholar]
- van Putten M., Putker K., Overzier M., Adamzek W. A., Pasteuning-Vuhman S., Plomp J. J. and Aartsma-Rus A. (2019). Natural disease history of the D2-mdx mouse model for Duchenne muscular dystrophy. FASEB J. 33, 8110-8124. 10.1096/fj.201802488R [DOI] [PMC free article] [PubMed] [Google Scholar]
- Veltrop M., van der Kaa J., Claassens J., van Vliet L., Verbeek S. and Aartsma-Rus A. (2013). Generation of embryonic stem cells and mice for duchenne research. PLoS Curr. 5, ecurrents.md.cbf1d33001de80923ce674302cad7925 10.1371/currents.md.cbf1d33001de80923ce674302cad7925 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Veltrop M., Van Vliet L., Hulsker M., Claassens J., Brouwers C., Breukel C., Van der Kaa J., Linssen M. M., den Dunnen J. T., Verbeek S. et al. (2018). A dystrophic Duchenne mouse model for testing human antisense oligonucleotides. PLoS ONE 13, e0193289 10.1371/journal.pone.0193289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verhaart I. E. C. and Aartsma-Rus A. (2019). Therapeutic developments for Duchenne muscular dystrophy. Nat. Rev. Neurol. 15, 373-386. 10.1038/s41582-019-0203-3 [DOI] [PubMed] [Google Scholar]
- Verhaart I. E. C., Putker K., van de Vijver D., Tanganyika-de Winter C. L., Pasteuning-Vuhman S., Plomp J. J., Aartsma-Rus A. M. and van Putten M. (2019). Cross-sectional study into age-related pathology of mouse models for limb girdle muscular dystrophy types 2D and 2F. PLoS ONE 14, e0220665 10.1371/journal.pone.0220665 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vest K. E., Phillips B. L., Banerjee A., Apponi L. H., Dammer E. B., Xu W., Zheng D., Yu J., Tian B., Pavlath G. K. et al. (2017). Novel mouse models of oculopharyngeal muscular dystrophy (OPMD) reveal early onset mitochondrial defects and suggest loss of PABPN1 may contribute to pathology. Hum. Mol. Genet. 26, 3235-3252. 10.1093/hmg/ddx206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weller A. H., Magliato S. A., Bell K. P. and Rosenberg N. L. (1997). Spontaneous myopathy in the SJL/J mouse: Pathology and strength loss. Muscle Nerve 20, 72-82. [DOI] [PubMed] [Google Scholar]
- Willmann R., Possekel S., Dubach-Powell J., Meier T. and Ruegg M. A. (2009). Mammalian animal models for Duchenne muscular dystrophy. Neuromuscul. Disord. 19, 241-249. 10.1016/j.nmd.2008.11.015 [DOI] [PubMed] [Google Scholar]
- Willmann R., De Luca A., Benatar M., Grounds M., Dubach J., Raymackers J.-M. and Nagaraju K. (2011a). Enhancing translation: guidelines for standard pre-clinical experiments in mdx mice. Neuromuscul. Disord. 22, 43-49. 10.1016/j.nmd.2011.04.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willmann R., Dubach J. and Chen K. (2011b). Developing standard procedures for pre-clinical efficacy studies in mouse models of spinal muscular atrophy: report of the expert workshop “Pre-clinical testing for SMA”, Zurich, March 29-30th 2010. Neuromuscul. Disord. 21, 74-77. 10.1016/j.nmd.2010.09.014 [DOI] [PubMed] [Google Scholar]
- Willmann R., Gordish-Dressman H., Meinen S., Rüegg M. A., Yu Q., Nagaraju K., Kumar A., Girgenrath M., Coffey C. B. M., Cruz V. et al. (2017). Improving reproducibility of phenotypic assessments in the DyW mouse model of laminin-α2 related congenital muscular dystrophy. J. Neuromuscul. Dis. 4, 115-126. 10.3233/JND-170217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wood C. L., Suchaki K. J., van ‘t Hof R., Cawthorn W. P., Dillon S., Straub V., Wong S. C., Ahmed S. F. and Farquharson C. (2020). A comparison of the bone and growth phenotype of mdx, mdx:Cmah −/− and mdx:Utrn +/− murine models with the C57BL/10 wild-type mouse. Dis. Model. Mech. 13, dmm040659 10.1242/dmm.040659 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu H., Wu X.-R., Wewer U. M. and Engvall E. (1994). Murine muscular dystrophy caused by a mutation in the laminin alpha 2 (Lama2) gene. Nat. Genet. 8, 297-302. 10.1038/ng1194-297 [DOI] [PubMed] [Google Scholar]
- Young C. S., Mokhonova E., Quinonez M., Pyle A. D. and Spencer M. J. (2017). Creation of a novel humanized dystrophic mouse model of duchenne muscular dystrophy and application of a CRISPR/Cas9 gene editing therapy. J. Neuromuscul Dis. 4, 139-145. 10.3233/JND-170218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y., King O. D., Rahimov F., Jones T. I., Ward C. W., Kerr J. P., Liu N., Emerson C. P., Kunkel L. M., Partridge T. A. et al. (2014). Humanskeletal musclexenograft as anewpreclinical model for muscle disorders. Hum. Mol. Genet. 23, 3180-3188. 10.1093/hmg/ddu028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zschüntzsch J., Zhang Y., Klinker F., Makosch G., Klinge L., Malzahn D., Brinkmeier H., Liebetanz D. and Schmidt J. (2016). Treatment with human immunoglobulin G improves the early disease course in a mouse model of Duchenne muscular dystrophy. J. Neurochem. 136, 351-362. 10.1111/jnc.13269 [DOI] [PubMed] [Google Scholar]