Abstract
Isolated celiac artery dissection (ICAD) is a rare entity with over 160 cases described in literature. We report a case of incidentally detected isolated celiac artery dissection during computed tomography evaluation for occult gastrointestinal bleeding. Though most cases of isolated celiac artery dissection are initially managed conservatively with antiplatelet and anticoagulants, some patients may require endovascular or occasionally surgical treatment. In our case, the celiac artery dissection had already progressed to cause hepatic artery occlusion and secondary collateral formation in the porta hepatis region. We retrospectively analyze the natural course of celiac artery dissection with hepatic artery occlusion in an asymptomatic patient for over 3 years.
Keywords: Celiac, Isolated, Dissection, Hepatic, Artery, Occlusion
Introduction
Isolated celiac artery dissection (ICAD) is a very uncommon condition that is increasingly being diagnosed recently with the advent of multislice CT scanners. Atherosclerosis, hypertension, diabetes, smoking, vasculitis, connective tissue disorder, pregnancy, fibromuscular dysplasia, and other congenital vessel wall abnormalities are known risk factors, though exact etiology is not known [1], [2], [3], [4]. In our current case, except for hypertension, the patient did not have any other associated risk factors. A review of the literature shows that the management of ICAD is debatable. Most of the authors favor conservative management than the endovascular or surgical approach [1,[5], [6], [7], [8], [9]. In this present case, we try to analyze the natural course of ICAD in a patient who was asymptomatic without any specific treatment or intervention for at least 42 months.
Clinical presentation and image findings
Sixty-four-year-old gentlemen presented with symptoms of lower gastrointestinal (GI) bleeding and clammy sweats. He was a nonsmoker but is a known hypertensive on treatment with amlodipine for 2 years and had previous inguinal hernia mesh repair and thoracotomy for retrosternal goiter. Laboratory investigations revealed low Hb (118 g/L), RBC (3.82 million /MCL), and hematocrit (0.33). An increase in serum lactate level noted (3.47 mmol/L). The white blood cells and platelet counts were normal.
He was referred for computed tomography (CT) abdominal angiogram as there was a suspicion of active GI bleeding. CT scan performed in a multislice scanner in plain, arterial, and venous phases. The arterial phase showed a dilated celiac artery measuring 13 mm with a true and false lumen separated by an intimal flap consistent with dissection (Fig. 1a). The common hepatic artery not opacified, and multiple collateral vessels were seen in porta hepatis, suggestive of long-standing hepatic artery occlusion (Fig. 1b and c). The splenic and superior mesenteric arteries were patent. There was no sign of any active GI bleeding.
Fig. 1.
(a) Recent CT angiogram (2019) shows celiac artery dissection (yellow arrow) in sagittal plane. (b) Axial CT angiogram (2019) shows celiac artery dissection (yellow arrow) and occluded common hepatic artery (pink arrow). (c) Axial MIP (2019) shows collateral vessels in porta hepatis region (red arrow). (Color version of figure is available online.)
Approximately 3 years ago, the patient underwent a CT examination in April 2016 for evaluation of retrosternal goiter, which included sections of the upper abdomen as well. Retrospective analysis of the celiac artery showed similar findings of a dilated vessel of 11 mm caliber with dissecting flap and hepatic artery occlusion (Fig. 2). However, there was no collateral in the porta hepatis region, as noted in the present CT.
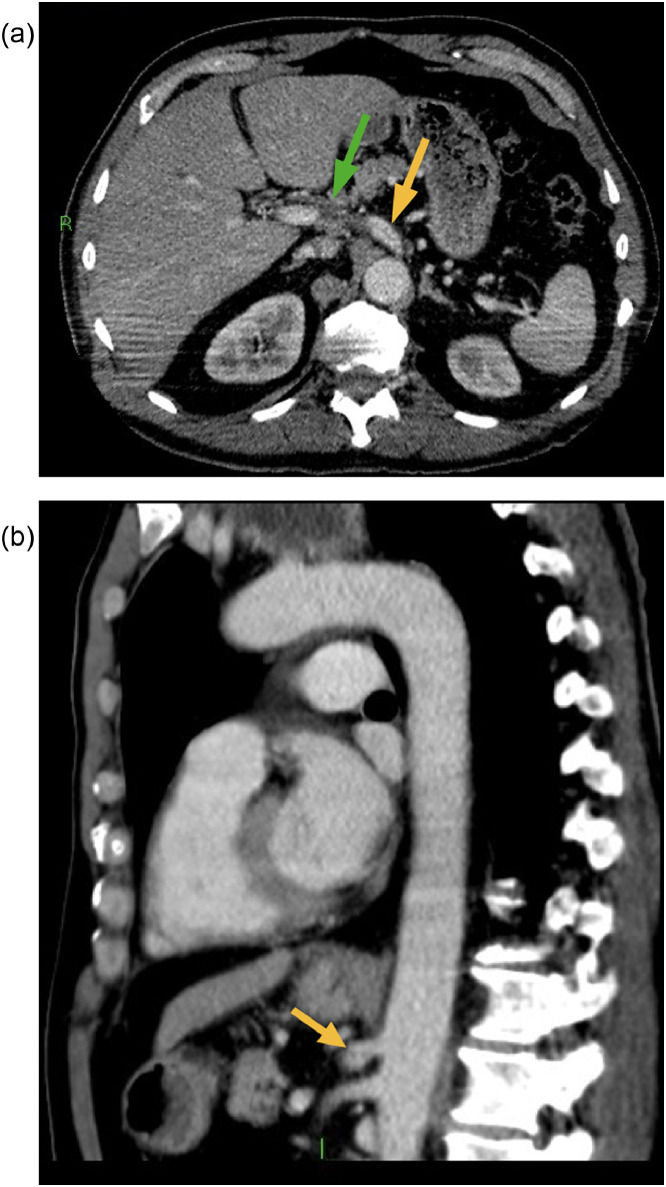
Fig. 2.
(a) Previous CT done on April 2016 shows celiac artery dissection (yellow arrow) in axial plane. Note common hepatic artery occlusion (green arrow). (b) Previous CT done on April 2016 shows celiac artery dissection (yellow arrow) in sagittal plane. (Color version of figure is available online.)
A review of preceding clinical notes did not reveal an episode of acute abdominal pain or admission to A&E for any other abdominal symptoms. We suppose that the patient might have had isolated celiac artery dissection with hepatic artery occlusion before this period (2016) and later developed collateral. Though the patient did not receive any specific treatment for dissection, yet, surprisingly, he was relatively symptom-free so far. Recent liver function tests, including Alanine aminotransferase, alkaline phosphatase, bilirubin, total protein, albumin, and globulin, were normal. The vascular team opinion sorted, and no further treatment proposed.
Discussion
In previously described case reports and case series of ICAD, the majority of the patients were symptomatic [5]. Abdominal pain is the most common symptom in a patient with celiac artery dissection [1,[7], [8], [9], [10], [11], [12], [13], [14]. Some may present with features of secondary ischemia, including pancreatitis, splenic infarction due to extension of dissection to celiac artery branches, or rarely intraperitoneal hemorrhage owing to arterial rupture [10,[15], [16], [17]. Asymptomatic ICAD cases were found incidentally in CT done for other causes. There are over 30 patients described in the literature with dissection extending to celiac artery branches, most of which were treated conservatively and remaining required either endovascular or surgical treatment due to organ malperfusion [5,[7], [8], [9], [10], [11],16,18,19]. It was quite unusual for our case to be asymptomatic even though the dissection had progressed to hepatic artery occlusion.
Some of the authors have proposed a morphological classification for ICAD, similar to existing classification for isolated dissection of superior mesenteric artery: type I, patent lumen with both entry and re-entry; type II, “cul-de-sac” shaped false lumen without re-entry; type III, thrombosed false lumen with an ulcer-like projection; type IV completely thrombosed false lumen without an ulcer-like projection; and type V, dissecting aneurysm. Type II, III, and IV had further subtypes determined by true lumen residual diameter [8,20].
The appearance of ICAD in our case was type II morphology showing nonthrombosed “cul-de-sac” type of false lumen. There was no interval change in the morphology of the ICAD in 3 years except for a marginal increase in diameter from 11 mm to 13 mm at present. The hepatic artery occlusion is presumably secondary to the extension of dissection to the common hepatic artery with subsequent collateral formation. In our case scenario, we assume that the patient had a previous asymptomatic event of ICAD, which had progressed to hepatic artery occlusion. However, there were not any ischemic changes in liver parenchyma due to its dual blood supply from the portal vein.
A review of the literature shows that the management in most patients with ICAD of any morphology except dissecting aneurysm with or without symptoms is a conservative approach. Oh S et al (2011) reported 8 symptomatic patients with ICAD, out of which 3 had coexisting superior mesenteric artery dissection as well. Seven patients received anticoagulation, which improved their symptoms and was asymptomatic at 16 months follow-up. Only 1 patient underwent endovascular stent placement for persisting abdominal pain [14].
In a study by paul D et al (2015), out of 19 patients, 7 were symptomatic with abdominal pain, and 12 were incidental findings in CT done for other causes. None of the patients received specific antiplatelet or anticoagulation except one who was a known case of atrial fibrillation. Three patients underwent endovascular stenting for ongoing pain; 1 had an open surgical repair for 5 cm dissecting aneurysm, and rest managed conservatively. All patients remained stable for an average of 46 months follow-up except one who died of other causes [1].
In one study by Ichiba et al (2016), 13 cases of symptomatic ICAD were treated conservatively with antihypertensive and NSAID only. None of them received antiplatelets, anticoagulants, endovascular, or surgical treatment. All the patients were alive without any significant comorbidities on a median follow up for 376 days, though 2 had developed splenic infarction [12].
In another study of 23 patients by B Kim et al (2018), 13 were symptomatic and 8 asymptomatic. Irrespective of morphology, all patients were under conservative management with or without the use of antiplatelet or anticoagulants. After an average period of 42 weeks, 13 showed no interval change in morphology, 5 with some partial/complete remodeling, and 1 had deterioration. There was no morbidity associated with ICAD in all patients, though 2 patients died of cancer [5].
The involvement of the hepatic artery in the celiac artery dissection has been discussed earlier in several studies. However, only recently, Kang sh et al (2019), described collaterals in patients with ICAD. Accordingly, out of 16 patients, 4 had disease progression with conservative management, but the formation of collaterals prevented hepatic ischemia. Delayed intervention recommended for these patients, except for one who had extensive hepatic artery thrombus [21].
The decision for endovascular stenting or surgical management is guided by following 2 principles: First, clinical worsening of symptoms including persistent pain or signs of arterial rupture; Second, depending on the morphology of dissection which includes type V (dissecting aneurysm) or organ ischemia due to involvement of celiac artery branches. Though in our case, the dissection had presumably extended to hepatic artery branch occlusion, the patient was still asymptomatic, and hence no intervention was performed. Earlier described ICAD cases with branch involvement showed no associated liver or gastric ischemia, likely due to their abundant collateral circulation [7,12,16,[22], [23], [24], [25], [26], [27].
Our case supports prior studies favoring the conservative management of ICAD. The stable natural course of the ICAD for over 3 years without any specific treatment was evident in our case. Although we felt that the patient might have benefitted with antiplatelets and anticoagulants if he had presented at the time of dissection to preclude hepatic artery occlusion. Nevertheless, even after such an event, there was no ischemic damage in liver parenchyma due to its natural collateral flow from the portal vein. Does it imply that patients with dissection extending to celiac artery branches, especially the hepatic artery, can still be managed conservatively? A more large study might be required to analyze further the long-term follow-up in patients with celiac artery dissection involving its branches.
Conclusion
The rarity of this condition makes it difficult to establish a standard protocol. The decision on the management of ICAD should be individualized based on the patient's symptoms and morphology of the dissection. However, in asymptomatic patients with branch involvement as in our case, it would be a dilemma whether to initiate medical management or to let the disease have its natural course.
References
- 1.DiMusto P.D., Oberdoerster M.M., Criado E. Isolated celiac artery dissection. J Vasc Surg. 2015;61(4):972–976. doi: 10.1016/j.jvs.2014.10.108. PMID 25601505. [DOI] [PubMed] [Google Scholar]
- 2.Zhang T., Zhang X., Zhang X., Jiang J., Zhou B. Endovascular treatment of isolated spontaneous celiac artery dissection. Vascular. 2012;20:118–120. doi: 10.1258/vasc.2011.cr0302. PMID 22472366. [DOI] [PubMed] [Google Scholar]
- 3.Choi J.Y., Kwon O.J. Approaches to the management of spontaneous isolated visceral artery dissection. Ann Vasc Surg. 2013;27:750–757. doi: 10.1016/j.avsg.2012.09.016. PMID 23790761. [DOI] [PubMed] [Google Scholar]
- 4.Neychev V., Krol E., Dietzek A. Unusual presentation and treatment of spontaneous celiac artery dissection. J Vasc Surg. 2013;58:491–495. doi: 10.1016/j.jvs.2012.10.136. PMID 23466182. [DOI] [PubMed] [Google Scholar]
- 5.Kim B., Lee B.S., Kwak H.K., Kang H., Ahn J.H. Natural course and outcomes of spontaneous isolated celiac artery dissection according to morphological findings on computed tomography angiography: STROBE compliant article. Medicine (Baltimore) Feb 2018;97(5):e9705. doi: 10.1097/MD.0000000000009705. PMID. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Garrett H.E., Jr. Options for treatment of spontaneous mesenteric artery dissection. J Vasc Surg. May 2014;59(5):1433–1439. doi: 10.1016/j.jvs.2014.01.040. e1-2PMID 24655752. [DOI] [PubMed] [Google Scholar]
- 7.Galastri F.L., Cavalcante R.N., Motta-Leal-Filho J.M., De Fina B., Affonso B.B., De Amorim J.E. Evaluation and management of symptomatic isolated spontaneous celiac trunk dissection. Vasc Med. 2015;20:358–363. doi: 10.1177/1358863X15581447. PMID25910918. [DOI] [PubMed] [Google Scholar]
- 8.Sun J., Li D.L., Wu Z.H., He Y.Y., Zhu Q.Q., Zhang H.K. Morphologic findings and management strategy of spontaneous isolated dissection of the celiac artery. J Vasc Surg. 2016;64:389–394. doi: 10.1016/j.jvs.2015.12.050. PMID26926933. [DOI] [PubMed] [Google Scholar]
- 9.Hosaka A., Nemoto M., Miyata T. Outcomes of conservative management of spontaneous celiac artery dissection. J Vasc Surg. 2017;65 doi: 10.1016/j.jvs.2016.09.058. 760– 5.765.e1PMID 28017582. [DOI] [PubMed] [Google Scholar]
- 10.D’Ambrosio N., Friedman B., Siegel D., Katz D., Newatia A., Hines J. Spontaneous isolated dissection of the celiac artery: CT findings in adults. AJR Am J Roentgenol. 2007;188:W506–W511. doi: 10.2214/AJR.06.0315. PMID:17515339. [DOI] [PubMed] [Google Scholar]
- 11.Li S., Cheng L., Tu J., Jiao Y., Wu X., Wang Z. Effectiveness of the conservative therapy for symptomatic isolated celiac artery dissection. Cardiovasc Intervent Radiol. 2017;40:994–1002. doi: 10.1007/s00270-017-1680-7. PMID28493109. [DOI] [PubMed] [Google Scholar]
- 12.Ichiba T., Hara M., Yunoki K., Urashima M., Naitou H. Impact of noninvasive conservative medical treatment for symptomatic isolated celiac artery dissection. Circ J. 2016;80:1445–1451. doi: 10.1253/circj.CJ-16-0132. PMID27074825. [DOI] [PubMed] [Google Scholar]
- 13.Alcantara S., Yang C.K., Sasson J., Goss S., Benvenisty A., Todd G. The evidence for nonoperative management of visceral artery dissections: a single-center experience. Ann Vasc Surg. 2015;29:103–108. doi: 10.1016/j.avsg.2014.09.004. PMID. [DOI] [PubMed] [Google Scholar]
- 14.Oh S., Cho Y.P., Kim J.H., Shin S., Kwon T.W., Ko G.Y. Symptomatic spontaneous celiac artery dissection treated by conservative management: serial imaging findings. Abdom Imaging. 2011;36:79–82. doi: 10.1007/s00261-010-9657-x. PMID20981421. [DOI] [PubMed] [Google Scholar]
- 15.Amabile P., Ouaissi M., Cohen S., Piquet P. Conservative treatment of spontaneous and isolated dissection of mesenteric arteries. Ann Vasc Surg. 2009;23(6):738–744. doi: 10.1016/j.avsg.2008.01.016. PMID. [DOI] [PubMed] [Google Scholar]
- 16.Glehen O., Feugier P., Aleksic Y., Delannoy P., Chevalier J.M. Spontaneous dissection of the celiac artery. Ann Vasc Surg. 2001;15(6):687–692. doi: 10.1007/s10016-001-0012-0. PMID. [DOI] [PubMed] [Google Scholar]
- 17.Nordanstig J., Gerdes H., Kocys E. Spontaneous isolated dissection of the celiac trunk with rupture of the proximal splenic artery: a case report. Eur J Vasc Endovasc Surg. 2009;37(2):194–197. doi: 10.1016/j.ejvs.2008.10.009. PMID. [DOI] [PubMed] [Google Scholar]
- 18.Takayama T., Miyata T., Shirakawa M., Nagawa H. Isolated spontaneous dissection of the splanchnic arteries. J Vasc Surg. 2008;48:329–333. doi: 10.1016/j.jvs.2008.03.002. PMID. [DOI] [PubMed] [Google Scholar]
- 19.Tokue H., Tsushima Y., Endo K. Imaging findings and management of isolated dissection of the visceral arteries. Jpn J Radiol. 2009;27:430–437. doi: 10.1007/s11604-009-0366-8. PMID. [DOI] [PubMed] [Google Scholar]
- 20.Li D.L., He Y.Y., Alkalei A.M., Chen X.D., Jin W., Li M. Management strategy for spontaneous isolated dissection of the superior mesenteric artery based on morphologic classification. J Vasc Surg. 2014;59:165–172. doi: 10.1016/j.jvs.2013.07.014. PMID. [DOI] [PubMed] [Google Scholar]
- 21.Kang S.H., Park H.S, Yoon C.J., Shin C.S, Yoo K.C., Lee T. Mid- to long-term outcomes in management of spontaneous isolated coeliac artery dissection (SICAD) Eur J Vasc Endovasc Surg. 2019 Dec 5 doi: 10.1016/j.ejvs.2019.09.510. pii: S1078-5884(19)32023-4PMID. [DOI] [PubMed] [Google Scholar]
- 22.Obon-Dent M., Shabaneh B., Dougherty K.G., Strickman N.E. Spontaneous celiac artery dissection case report and literature review. Tex Heart Inst J. 2012;39:703–706. PMID. [PMC free article] [PubMed] [Google Scholar]
- 23.Schrijvers R., Van De Mierop F., De Schepper B., Sprengers D., Dero I., D'Archambeau O. Spontaneous dissection of the celiac trunk: a rare cause of abdominal pain: Case report and review of the literature. Acta Gastroenterol Belg. 2013;76:335–339. PMID. [PubMed] [Google Scholar]
- 24.Takayama Y., Takao M., Inoue T., Yoshimi F., Koyama K., Nagai H. Isolated spontaneous dissection of the celiac artery: report of two cases. Ann Vasc Dis. 2014;7:64–67. doi: 10.3400/avd.cr.13-00102. PMID. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wang H.C., Chen J.H., Hsiao C.C., Jeng C.M., Chen W.L. Spontaneous dissection of the celiac artery: a case report and literature review. Am J Emerg Med. 2013;31:1000.e3–1000.e5. doi: 10.1016/j.ajem.2013.02.007. PMID. [DOI] [PubMed] [Google Scholar]
- 26.Patel K.S., Benshar O., Vrabie R., Patel A., Adler M., Hines G. A major pain in the back and epigastrium: an unusual case of spontaneous celiac artery dissection. J Community Hosp Intern Med Perspect. 2014;25:1–4. doi: 10.3402/jchimp.v4.23840. PMID. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chaillou P., Moussu P., Noel S.F., Sagan C., Pistorius M.A., Langlard J.M. Spontaneous dissection of the celiac artery. Ann Vasc Surg. 1997;11:413–415. doi: 10.1007/s100169900070. PMID. [DOI] [PubMed] [Google Scholar]