Abstract
Acute tears or ruptures of the brachialis muscle are rare events, with only 10 cases reported to date and all of which have been in adults. We report a case of an acute, complete tear of brachialis in an 8-year-old female that occurred while the patient was practicing a gymnastic move. Although rare, this case underscores the need to include brachialis tears in the differential diagnosis for musculoskeletal injuries at the elbow in all age groups.
Keywords: Brachialis, Muscle tear, Pediatric
Introduction
Adolescent athletes are susceptible to an array of musculoskeletal injuries while participating in sports. At the elbow, biceps brachii is the most commonly injured of the flexor muscles [1]. A far less common injury is an isolated brachialis tear, first reported in the literature in 2001 in a 67-year-old male [2]. Since that time, several other reports of isolated brachialis muscle tears have been published [3], [4], [5], [6], [7], [8], [9], [10], [11]. These cases involved people across the age-spectrum who were participating in a diverse set of activities and with their upper extremity in a variety of positions at the time of injury. Due to the rarity of this injury it may not be included on the differential diagnosis and therefore may be misdiagnosed. We describe a case of an 8-year-old girl with an isolated, complete brachialis tear that, to the best of our knowledge, is the first report of a brachialis tear during the first 2 decades of life.
Clinical case
An 8-year-old Caucasian right-handed female presented with pain and swelling at the lateral side of her distal right forearm following an attempted gymnastic move. The patient was a nonelite, recreational gymnast. The local orthopedics department was consulted via telephone but no physical examination was performed. The patient subsequently underwent radiographic imaging of her right elbow in 3 views. The patient's height was 48 inches, weight 60 pounds, she had no history of musculoskeletal injuries or disorders, her body mass index was reported at ~18.3, and she had yet to undergo menarche. It was noted that she could achieve only 30° of flexion at the elbow, had normal pronation and supination, and displayed minimal bruising and no paresthesia. The injury was sustained while she was performing a “back-walkover” move, a move she had learned in her gymnastics class which she participated in twice a week for 1 year. She had reached the “bridge position” and was in the process of “walking” her legs over her head, when she felt an unexplainable but painful sensation in the distal portion of her right arm. She subsequently developed rapid swelling at the lateral side of her distal right arm.
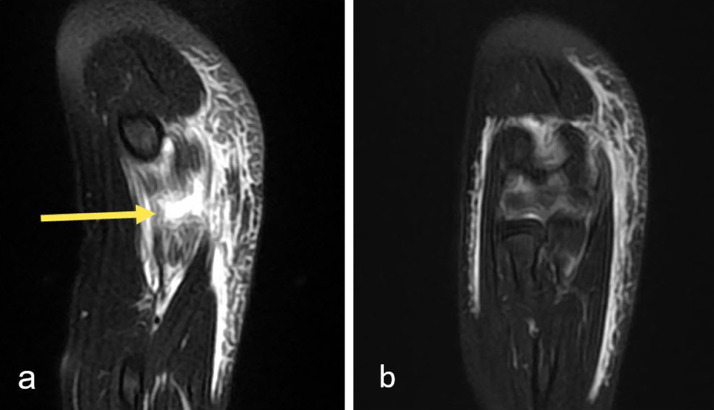
Imaging via radiography plain film demonstrated a small right elbow joint effusion with no evidence of acute osseous fracture. The elbow ossification centers were developmentally normal, no arthritis was present, and the radio, capitellar, and humeral lines were normal. Noncontrast magnetic resonance imaging (MRI) was performed the day after her injury, which revealed an isolated, complete, full thickness brachialis muscle tear without tendon damage (Figs. 1 and 2).
Fig. 1.
Serial sagittal noncontrast MRI images, T2-weighted fat-suppressed sequence, in an 8-year-old female with a complete, full thickness tear of the brachialis muscle. (a) Separation of torn muscle fibers is visible (arrow). (a and b) Post traumatic edema and blood in tissues surround the muscle tear.
Fig. 2.
Serial coronal noncontrast MRI images, T2-weighted fat-suppressed sequence, in an 8-year-old female with a complete brachialis muscle tear. (a) Muscle tear is visible (arrow). (b) Adjacent slice at level of elbow for reference.
The patient's affected arm was immobilized for 2 weeks in a sling and she ceased formal gymnastics training for 10 weeks, although she remained physically active by participating in karate within a month of injury and practiced gymnastics lightly. Noncontrast MRI at 8 weeks postinjury demonstrated persistent but minimal inflammation of the muscle and healing of the muscle with a closure in the gap between torn ends of the muscle (Fig. 3).Verbal follow-up was conducted at 9 months postinjury with the patient's family reporting no signs or symptoms of injury and an improvement in her overall skill level.
Fig. 3.
Noncontrast sagittal MRI image, T2-weighted fat-suppressed sequence. Follow-up exam 2 months after brachialis muscle tear in an 8-year-old female. Healing muscle fibers with closure of the gap between torn ends of the muscle are evident (arrow). High T2 signal at the healing muscle is presumed to be inflammation based on the injury history and close clinical follow-up.
Discussion
The patient presented is an 8-year-old female who suffered a right arm distal brachialis tear without tendon or bone involvement. Isolated brachialis muscle tears are exceedingly uncommon events [2,3,10] and to the best of our knowledge this is the first published record of such an injury during the first 2 decades of life.
In the upper extremity, 3 muscles are involved in elbow flexion: brachialis, biceps brachii, and brachioradialis. Brachialis is composed of 2 heads, specifically a larger superficial head (SH) and a smaller deep head (DH). The proximal attachment of the SH forms a cup underneath deltoid's distal attachment at the deltoid tuberosity, surrounding it anteriorly, inferiorly, and posteriorly. This attachment continues laterally on the humerus and onto the lateral intermuscular septum. The distal attachment of the SH is on anterior surface of the ulna at the ulnar tuberosity. The DH originates distally to the SH on the anterior surface of the humerus as well as the medial intermuscular septum. Distally, the fibers of the DH spread out and form an aponeurosis which inserts onto the ulna just proximal to the SH, with some fibers penetrating into the distal attachment of the SH, but they do not extend far enough proximally reach the coronoid process [12]. Because brachialis crosses the elbow joint anteriorly and its distal attachment is restricted to the ulna, its action is limited to elbow flexion and it assumes no role in elbow pronation/supination [12]. Of note, however, is that brachialis generates the greatest contractile force of any of the elbow flexors [13].
The injury sustained by this patient was the direct result of a biomechanical event and there is no reason to suspect it was precipitated by an underlying pathology or abnormality. The patient had no prior history of musculoskeletal injuries or disorders and with a body mass index of ~18.3, which corresponds to the 85th percentile, she presumably had sufficient brachialis cross-sectional area to withstand normal tensile forces during elbow flexion.
Based on the gymnastic move our patient was performing at the time of her injury, it is possible to identify the biomechanical events that led to her injury. Prior to injury, she was situated in the “bridge position” of the “back-walkover” move, with her elbows in slight flexion of approximately 10° to brace her body. The process of “walking” her legs over her head caused her elbows to fully extend, or perhaps hyperextend, which resulted in a lengthening of the brachialis muscle. Elbow extension is accomplished primarily by triceps brachii and anconeus; however, during the gymnastics move performed by our patient, brachialis would have assisted through eccentric contraction. Eccentric muscle contraction produces significantly more tensile force than concentric contraction [14] and consequently muscle tearing occurs most often when a muscle is subjected to excessive eccentric contraction [15]. In this case, the eccentric load ultimately overwhelmed the brachialis myofibrils, resulting in a complete tear of the muscle belly. Furthermore, muscle fibers near the myotendinous junction are more susceptible to injury from excessive tensile force than are muscle fibers located within the muscle belly [16], [17], [18], which fits with the location of the injury in this patient.
In this case, additional factors may have contributed to the muscle failure and tearing. First, the patient had not performed a proper “warm-up” prior to attempting the gymnastic move. Indeed, the injury occurred at school within minutes of the start of the patient's recess break. A well-designed warm-up can reduce muscle injury through a variety of mechanisms, including but not limited to improvements in muscle strength and power, lowered viscous resistance in muscles, and improvements in reaction time [19,20]. Moreover, a warm-up improves the sensitivity of muscle proprioreceptors, ultimately providing the individual with a better sense of the kinematics of the muscle during activity. This, in turn, helps minimize the risk excessive tensile force being placed on the muscle [21].
In contrast to brachialis, biceps brachii is commonly injured. Of note, however, is that the vast majority of biceps brachii injuries involve the tendon, usually the proximal portion of the long head of the biceps tendon, with the mechanism of injury related to tendinopathies. Biceps muscle belly tears are exceedingly rare. When they do occur, the mechanism of injury most commonly reported is blunt trauma [22].
Muscle injuries at the elbow show no predilection for gender in this age group, with males and females having similar elbow flexion isometric torque capabilities, elbow flexor cross-sectional area, brachialis moment arm length, and mechanical advantage [23]. However, as women reach menarche, increases in estradiol decrease tendon collagen synthesis, lower mechanical strength, and ultimately result in differences in the adaptability of tendon to loading between women and men [24]. This, among many other factors, may be responsible for increased connective tissue injury rates in females post menarche.
Isolated brachialis tears are rare and therefore carry with them the risk of being misdiagnosed. Diagnosis is further complicated by the deep position of brachialis relative to the overlying biceps brachii, which makes palpation of the injured muscle difficult. Imaging investigations such as MRI are key to confirming the injury. This case demonstrates these injuries can occur within pediatric age group and it further underscores the need to include brachialis tears in the differential diagnosis for musculoskeletal injuries at the elbow in all age groups.
Footnotes
Competing Interest: The authors have declared that no competing interests exist.
References
- 1.Magnussen R.A., Chong P.Y., Oh L.S., Walch G. Springer; 2014. Acute biceps brachii injuries; pp. 105–116. [Google Scholar]
- 2.Van den Berghe G.R., Queenan J.F., Murphy D.A. Isolated rupture of the brachialis: a case report. J Bone Joint Surg Am. 2001;83-A(7):1074–1075. doi: 10.2106/00004623-200107000-00015. PMID: 11451979. [DOI] [PubMed] [Google Scholar]
- 3.Nishida Y., Tsukushi S., Yamada Y., Hosono K., Ishiguro N. Brachialis muscle tear mimicking an intramuscular tumor: a report of two cases. J Hand Surg Am. 2007;32(8):1237–1241. doi: 10.1016/j.jhsa.2007.06.002. PMID: 17923309. [DOI] [PubMed] [Google Scholar]
- 4.Winblad J.B., Escobedo E., Hunter J.C. Brachialis muscle rupture and hematoma. Radiol Case Rep. 2008;3(4):251. doi: 10.2484/rcr.v3i4.251. PMID: 27303568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wasserstein D., White L., Theodoropoulos J. Traumatic brachialis muscle injury by elbow hyperextension in a professional hockey player. Clin J Sport Med. 2010;20(3):211–212. doi: 10.1097/JSM.0b013e3181df1ed4. PMID: 20445363. [DOI] [PubMed] [Google Scholar]
- 6.Schonberger T.J., Ernst M.F. A brachialis muscle rupture diagnosed by ultrasound; case report. Int J Emerg Med. 2011;4(1):46. doi: 10.1186/1865-1380-4-46. PMID: 21791098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Krych A.J., Kohen R.B., Rodeo S.A., Barnes R.P., Warren R.F., Hotchkiss R.N. Acute brachialis muscle rupture caused by closed elbow dislocation in a professional American football player. J Shoulder Elbow Surg. 2012;21(7):e1–e5. doi: 10.1016/j.jse.2011.11.007. PMID: 22173267. [DOI] [PubMed] [Google Scholar]
- 8.Murugappan K.S., Mohammed K. Acute traumatic brachialis rupture in a young rugby player: a case report. J Shoulder Elbow Surg. 2012;21(6):e12–e14. doi: 10.1016/j.jse.2011.10.009. PMID: 22217639. [DOI] [PubMed] [Google Scholar]
- 9.Costa J.H., Marques T.P. Traumatic rupture of the brachialis muscle in a 52-year-old man. BMJ Case Rep. 2015;2015 doi: 10.1136/bcr-2015-209421. PMID: 26163553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sharma P., Mehta N., Narayan A. Isolated traumatic brachialis muscle tear: a case report and review of literature. Bull Emerg Trauma. 2017;5(4):307–310. doi: 10.18869/acadpub.beat.5.4.476.. PMID: 29177180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Curry E.J., Cusano A., Elattar O., Bogart A., Murakami A., Li X. Brachialis muscle tendon rupture of the distal ulnar attachment in a competitive weight lifter. Orthopedics. 2019;42(3):e339–e342. doi: 10.3928/01477447-20190221-04. PMID: 30810756. [DOI] [PubMed] [Google Scholar]
- 12.Leonello D.T., Galley I.J., Bain G.I., Carter C.D. Brachialis muscle anatomy: a study in cadavers. J Bone Joint Surg Am. 2007;89(6):1293–1297. doi: 10.2106/JBJS.F.00343. PMID: 17545433. [DOI] [PubMed] [Google Scholar]
- 13.Kawakami Y., Nakazawa K., Fujimoto T., Nozaki D., Miyashita M., Fukunaga T. Specific tension of elbow flexor and extensor muscles based on magnetic resonance imaging. Eur J Appl Physiol Occup Physiol. 1994;68(2):139–147. doi: 10.1007/BF00244027. PMID: 81945423. [DOI] [PubMed] [Google Scholar]
- 14.Lieder R.L. Biomechanical response of skeletal muscle to eccentric contractions. J Sport Health Sci. 2018;7(3):294–309. doi: 10.1016/j.jshs.2018.06.005. PMID: 30356666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jde Souza, Gottried C. Muscle injury: review of experimental models. J Electromyogr Kinesiol. 2013;23(6):1253–1260. doi: 10.1016/j.jelekin.2013.07.009. [DOI] [PubMed] [Google Scholar]
- 16.Silder A., Heiderscheit B., Thelen D.G., Enright T., Tuite M.J. MR observations of long-term musculotendon remodeling following a hamstring strain injury. Skeletal Radiol. 2008;37(12):1101–1109. doi: 10.1007/s00256-008-0546-0. PMID: 18649077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Charvet B., Ruggiero F., Le Guellec D. The development of the myotendinous junction. A review. Muscles Ligaments Tendons J. 2012;2(2):53–63. PMID: 23738275. [PMC free article] [PubMed] [Google Scholar]
- 18.Curzi D., Sartini S., Guescini M., Lattanzi D., Di Palma M., Ambrogini P. Effect of different exercise intensities on the myotendinous junction plasticity. PLoS One. 2016;11(6) doi: 10.1371/journal.pone.0158059. PMID: 27337061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bergh U., Ekblom B. Influence of muscle temperature on maximal muscle strength and power output in human skeletal muscles. Acta Physiol Scand. 1979;107(1):33–37. doi: 10.1111/j.1748-1716.1979.tb06439.x. PMID: 525366. [DOI] [PubMed] [Google Scholar]
- 20.Woods K., Bishop P., Jones E. Warm-up and stretching in the prevention of muscular injury. Sports Med. 2007;37(12):1089–1099. doi: 10.2165/00007256-200737120-00006. PMID: 18027995. [DOI] [PubMed] [Google Scholar]
- 22.Subasi S.S., Gelecek N., Aksakoglu G. Effects of different warm-up periods on knee proprioception and balance in healthy young individuals. J Sport Rehabil. 2008;17(2):186–205. doi: 10.1123/jsr.17.2.186. PMID: 18515917. [DOI] [PubMed] [Google Scholar]
- 21.Chen H.W., Chew F.S. Complete rupture of both heads of biceps brachii muscle belly by blunt trauma. Radiol Case Rep. 2006;1(4):145–148. doi: 10.2484/rcr.v1i4.28. PMID: 27298705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kuczmarski R.J., Ogden C.L., Guo S.S., Grummer-Strawn L.M., Flegal K.M., Mei Z. 2000 CDC growth charts for the United States: methods and development. National Center for Health Statistics. Vital Health Stat. 2002;11(246):1–190. PMID: 12043359. [PubMed] [Google Scholar]
- 24.Magnusson S.P., Hansen M., Langberg H., Miller B., Haraldsson B., Westh E.K. The adaptability of tendon to loading differs in men and women. Int J Exp Pathol. 2007;88(4):237–240. doi: 10.1111/j.1365-2613.2007.00551.x. PMID: 17696904. [DOI] [PMC free article] [PubMed] [Google Scholar]