Abstract
Arthritis is a leading cause of disability in the United States, with the most efficacious treatments being physical activity (PA). Arthritis patients are less likely to meet PA recommendations and the neighborhood environment may play a role. This study examines the effect of neighborhood walkability and social cohesion on PA among arthritis patients in a sample of US adults. This cross-sectional study used 2015 National Health Interview Survey data. Eligible participants were age ≥45 years, had arthritis, recent leg-joint pain and complete data. Walkability was based on 6 questions regarding amenities and destinations that promote walking. Social cohesion was based on 4 validated questions. Meeting PA was defined as 150 min/week. Chi-squared testing and logistic regression determined associations between neighborhood environment and PA, including interaction between social cohesion and walkability. The final unweighted sample included 3,826 participants with mean age 64.6 years (SE = 0.26), 61.8% female and 78.1% non-Hispanic White. In adjusted, weighted analysis, not, slightly, and moderately-walkable neighborhoods all had lower odds of meeting PA recommendations verses highly-walkable neighborhood (OR = 0.61[95% CI 0.41–0.92], OR = 0.65[95% CI 0.50–0.85], OR = 0.75[95% CI 0.59–0.97], respectively). Social cohesion was independently associated with decreased odds of meeting PA guidelines (p = 0.003). No interaction with walkability was found (p = 0.405). Less than a highly-walkable neighborhood and lower social cohesion were independently associated with decreased odds of meeting PA recommendations among adults with arthritis and recent joint pain. Since walking is one of the most effective treatments for arthritis, clinicians should be sensitive to barriers patients may perceive to walking.
Keywords: Built environment, Arthritis, Physical activity, Epidemiology, Social environment
1. Introduction
Arthritis and musculoskeletal pain are among the most common causes of disability in the United States [1]. Further, data suggest that these conditions are on the rise [2]. Arthritis and musculoskeletal pain encompass a relatively broad group of painful conditions, such as osteoarthritis (OA), fibromyalgia (FM), and rheumatoid arthritis (RA). Although the arsenal of pharmacologic treatments for arthritic conditions is large, the data supporting the efficacy of many of these treatments are lacking. Some data even implicate these medications as potential health hazards [3], [4], [5]. Opioids, for instance, are commonly prescribed in arthritis but associated with many poor outcomes [6]. In the age of the opioid epidemic, it is imperative that we develop and implement alternatives that are economical, effective, and without harm.
Non-pharmacologic interventions, particularly physical activity, are by far the most effective in treating many musculoskeletal pain conditions [7], [8], [9]. Strong evidence suggests OA patients experience decreased pain and stiffness, as well as increases in physical function with physical activity such as walking [9], [10]. However, many patients with these musculoskeletal conditions do not meet physical activity recommendations [11]. The reasons why individuals with these conditions do not meet physical activity recommendations, however, remain unclear [11], [12], [13], [14]. Other studies have found that attributes of the patient’s built environment may facilitate physical activity, especially as walking in their neighborhood would be an easy, low-cost solution to improving patient outcomes [15].
Two commonly identified aspects of neighborhood characteristics are the physical environment, such as walkability, and the social environment, e.g. neighborhood cohesion [16]. Each appears to independently influence physical activity in mid to older adults, many of whom may have arthritis [17], [18]. Their results suggested that low social cohesion and perceived poor walkability were associated with worse physical functioning and disability, however these samples were restricted to particular geographic areas (North Carolina and Belgium). Further, Van Holle et al. identified social cohesion as modifying the effect of walkability, where some older adults walked despite low walkability when social cohesion was high [18]. Since alterations to the physical environment may not always be feasible, enhancing the social environment may present another opportunity to improve physical activity. This study examines the extent to which social cohesion and perceived neighborhood walkability are associated with physical activity and whether social cohesion modifies the effect of walkability on physical activity among mid to older adults with arthritis diagnosis and lower extremity joint pain.
2. Methods
2.1. Study population
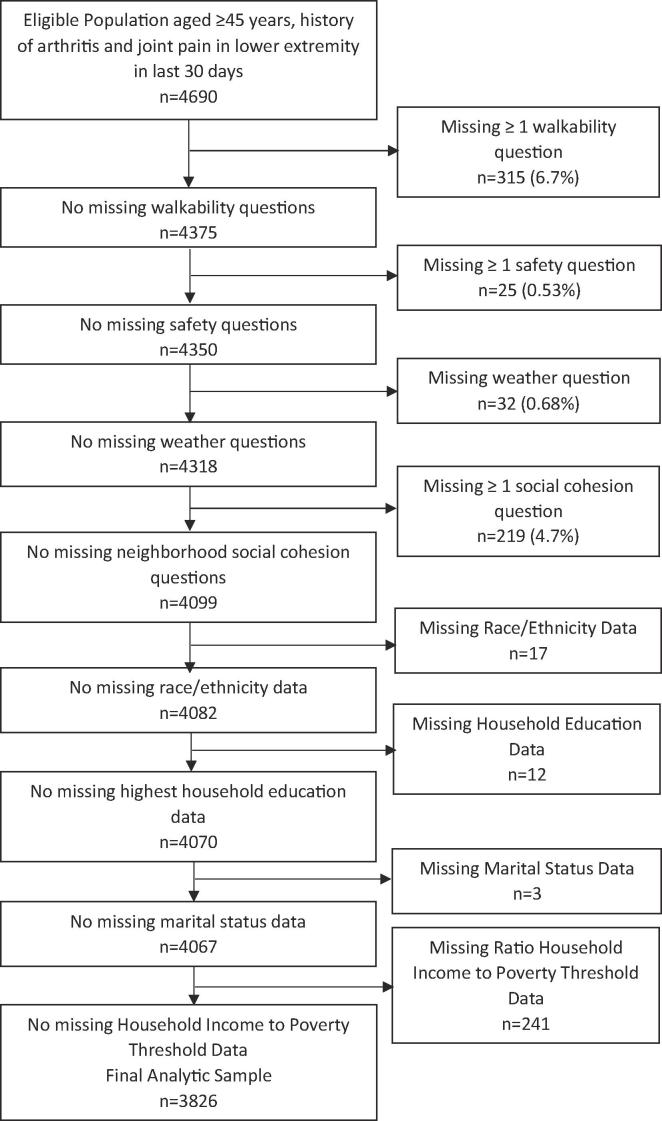
This cross-sectional study used self-reported data from the 2015 National Health Interview Survey (NHIS), which are collected through in-person survey by trained representatives from the United States Census Bureau. These data are collected using complex sampling techniques to allow for representation of the United States population. The 2015 annual response rate was approximately 70.1% of eligible households [19]. To be included in this study, participants were at least 45 years old with self-reported doctor-diagnosed arthritis, rheumatoid arthritis, fibromyalgia, gout or Lupus with pain in knee, hip or ankle in the last 30 days at the time of the survey, resulting in a target population of 4690 participants. Self-report of these conditions is considered accurate when compared to claims data [20], [21]. Participants were limited to those at least 45 years of age to be consistent with the literature regarding the beginning of symptoms, especially of osteoarthritis [22], [23]. Lower extremity joint pain was chosen as these are conceptually the joints that would be most limiting to walking, but also likely benefit the most from walking. A complete case analysis was undertaken to minimize bias, thus patients were excluded if they had incomplete data on demographics, social cohesion, walkability, physical activity, or covariates. After removing participants with missing variables, the eligible study population of 4690 was reduced to a final analytic sample of 3826 participants (Fig. 1).
Fig. 1.
Flow of inclusion complete case analysis.
2.2. Exposures of interest
This study focused on perceived walkability and perceived neighborhood social cohesion. Perceived walkability was ascertained from six questions pertaining to the participant’s feelings about their neighborhood. These questions centered on destinations to which participants could walk, as well as amenities to allow for walking (see Table 1). These questions were answered as either “yes” or “no.” The number of “yes” answers were tallied up for a maximum total of 6 and a minimum of 0, then categorized as “not walkable” (0), “slightly walkable” (1–2), “moderately walkable” (3–4) and “highly walkable” (5–6). Internal validity of questions was assessed via Kuder-Richardson-20 resulting in a correlation of 0.793. Perceived social cohesion was based on four questions regarding the social nature of the neighborhood (Table 1).
Table 1.
Content of questions for walkability and social cohesion.
| Walkability “Where you live…” |
| “…are there roads, sidewalks, paths or trails where you can walk?” |
| “…are there shops, stores, or markets that you can walk to?” |
| “…are there bus or transit stops that you can walk to?” |
| “…are there places like movies, libraries, or churches that you can walk to?” |
| “…are there places that you can walk to that help you relax, clear your mind, and reduce stress?” |
| “…do most streets have sidewalks?” |
| Social Cohesion “How much do you agree with the following statements about your neighborhood?” |
| “People in this neighborhood can be trusted.” |
| “People in this neighborhood help each other out.” |
| “This is a close-knit neighborhood.” |
| “There are people I can count on in this neighborhood.” |
These questions were answered on a Likert scale ranging from “strongly agree” (1) to “strongly disagree” (4). These answers were tallied up with a maximum score of 16 (low social cohesion) and minimum score of four (high social cohesion). These totals were then quartiled within the entire participant population. The use of these questions in this manner was previously described by Yi et al in a national sample of NHIS participants [24]. Internal validity was assessed via Cronbach’s Alpha. A value of 0.893 was determined, supporting high internal validity.
2.3. Outcome of interest
All participants were asked a series of questions regarding their activity. These were then quantified into minutes/week of moderate or vigorous activity. This was converted into a bivariate construct of either meeting physical activity recommendations or not. Participants were categorized as meeting PA recommendations if they had greater than or equal to 150 min of PA and as not meeting if any number less than 150 min [25]. No delineation was available regarding type of activity. The questions in the NHIS data reliably measure physical activity [26].
2.4. Covariates
All covariates were previously found to be associated with the likelihood of meeting physical activity recommendations [14], [27], [28], [29], [30], [31]. Variables included in this analysis included gender, age, race/ethnicity, household highest educational attainment, household income-to-poverty threshold ratio, marital status, perceived neighborhood safety, length of time in the neighborhood, and weather. Age was categorized as 45–54 years, 55–64 years, 65–74 years, and age 85 plus. Race/Ethnicity was categorized as non-Hispanic White, non-Hispanic Black, Hispanic/Latino, or Other. Highest household educational attainment was categorized as less than high school diploma through diploma or GED, some college through bachelors or associates degree, and masters and above. Income-to-poverty ratio was categorized as less than 1.00 of threshold, 1–1.99 of threshold, 2.00–3.99 of threshold, and less than 4.00 of the threshold. Marital status was categorized as never married, widowed/separated/divorced, or married/living with partner. Perceived neighborhood safety was determined through answers to three questions regarding participant perception of whether traffic, animals, or crime make them feel it is unsafe to walk. The answers to these questions were “yes” or “no”. Participants answers were categorized as never (0 affirmative answers), low (1 affirmative answer), moderate (2 affirmative answers), or high (3 affirmative answers). These questions are similar to those used in other studies assessing safety [17], [32]. A single question asked how frequently weather served as a barrier to walking. The answers were categorized as never, a little of the time, some of the time, most of the time, or all of the time. Length of residence in the neighborhood was included in the statistical models as this may affect the knowledge a participant has about their neighborhood, or their opportunity interact with neighbors. Length of time was categorized as less than 1 year, 1–3 years, 4–10 years, 11–20 years, and greater than 20 years.
2.5. Analysis
All analyses were weighted to account for complex survey sampling. All analyses used the entire dataset with a domain statement and inclusion variable in proc survey commands or additional layer in proc surveyfreq to correctly account for subpopulation analysis and preserve the integrity of the weights [33]. Unadjusted associations between covariates and perceived walkability and between covariates and meeting physical activity recommendations were tested using chi-square tests. Results were considered statistically significant at p < 0.05. Adjusted relationships between exposures, covariates, and outcomes were assessed using binomial logistic regression models to ascertain odds of meeting physical activity recommendations. If a covariate was found to be associated with either perceived walkability or meeting physical activity recommendations, it was included in the logistic regression model. To assess whether social cohesion modified the association between walkability and meeting physical activity recommendations, an interaction term was added to the unadjusted model including only perceived walkability, social cohesion, and meeting PA recommendations. To investigate for possible multicollinearity among variables, correlation coefficients were calculated between all variables as well as multicollinearity diagnostics, in particular variance inflation factor (VIF). All data were analyzed using SAS v9.4.
3. Results
3.1. Demographics
The final unweighted analytic sample consisted of 3826 participants. The average age was 64.6 years (SE = 0.26). The study population was 61.8% female and 78.1% non-Hispanic White. Among the study population, 30.7% achieved levels of activity consistent with PA recommendations (SE = 1.08).
3.2. Univariate analysis
Univariate analysis revealed that race/ethnicity, household income-to-poverty ratio, educational attainment, marital status, social cohesion, perceived safety, weather, and time living in the neighborhood were associated with perceived walkability (See Table A1, Table A2).
Table 2 shows unadjusted associations between exposures of interest, covariates and meeting physical activity recommendations. All covariates, with the exception of length of time in the neighborhood were found to be associated with meeting physical activity recommendations (all p < 0.05). Given all variables were found to be associated with either the exposure or the outcome, all variables were included in the final logistic regression model. This included social cohesion, found to be independently associated with walkability (p = 0.028).
Table 2.
Univariate associations exposure, covariates and outcome with unweighted frequency and weight percent.
| Variables | Meeting PA Recommendations n = 1128 | Not Meeting PA Recommendations n = 2698 | P-Value |
|---|---|---|---|
| Walkability | <0.001 | ||
| Not Walkable | 59 (6.84) | 284 (11.5) | |
| Slightly Walkable | 308 (27.2) | 866 (33.7) | |
| Moderately Walkable | 293 (27.7) | 700 (26.0) | |
| Highly Walkable | 468 (38.2) | 848 (28.7) | |
| Age | <0.001 | ||
| 45–54 | 221 (23.0) | 447 (19.3) | |
| 55–64 | 353 (33.3) | 788 (31.5) | |
| 65–74 | 370 (29.3) | 749 (26.2) | |
| 75–84 | 145 (11.9) | 485 (15.9) | |
| 85+ | 39 (2.51) | 229 (7.10) | |
| Sex | 0.018 | ||
| Male | 460 (42.0) | 885 (36.6) | |
| Female | 668 (58.0) | 1813 (63.4) | |
| Race/Ethnicity | 0.007 | ||
| Non-Hispanic White | 876 (80.6) | 1926 (77.0) | |
| Non-Hispanic Black | 128 (8.61) | 433 (12.9) | |
| Other | 47 (5.00) | 90 (3.43) | |
| Hispanic | 77 (5.75) | 249 (6.71) | |
| Education | <0.001 | ||
| HS Diploma/GED or less | 244 (16.2) | 1111 (36.8) | |
| Some College-AA/Bachelors | 615 (55.1) | 1350 (52.1) | |
| Masters and Above | 269 (28.7) | 237 (11.1) | |
| Income to Poverty Threshold Ratio | <0.001 | ||
| <1.00 | 111 (7.64) | 528 (14.4) | |
| 1.00–1.99 | 175 (12.9) | 763 (25.0) | |
| 2.00–3.99 | 316 (23.7) | 786 (32.1) | |
| 4.00 or More | 526 (55.7) | 621 (28.4) | |
| Marital Status | 0.006 | ||
| Married/Living with Partner | 575 (65.1) | 1166 (57.8) | |
| Widowed/Divorced/Separated | 455 (29.3) | 1276 (35.1) | |
| Never Married | 98 (5.59) | 256 (7.13) | |
| Perceived Social Cohesion | <0.001 | ||
| High | 451 (40.2) | 885 (33.0) | |
| High-Mid | 298 (26.5) | 597 (22.8) | |
| Low-Mid | 211 (21.2) | 618 (23.7) | |
| Low | 168 (12.1) | 598 (20.5) | |
| Safety | <0.001 | ||
| Never Barrier | 729 (64.7) | 1553 (58.8) | |
| Low Barrier | 281 (26.2) | 667 (25.2) | |
| Moderate Barrier | 88 (6.33) | 309 (10.8) | |
| High Barrier | 30 (2.68) | 169 (5.21) | |
| Weather As a Barrier | <0.001 | ||
| Almost Always | 226 (18.6) | 921 (33.2) | |
| Most of the Time | 137 (11.0) | 353 (14.3) | |
| Some of the Time | 341 (32.2) | 482 (18.0) | |
| A little of the Time | 203 (19.4) | 237 (8.37) | |
| Never | 221 (18.9) | 705 (26.2) | |
| Length of Time in Neighborhood | 0.306 | ||
| <1 year | 52 (4.34) | 151 (5.34) | |
| 1–3 years | 123 (11.5) | 337 (11.6) | |
| 4–10 years | 275 (24.2) | 596 (20.6) | |
| 11–20 years | 245 (22.5) | 564 (23.2) | |
| >20 years | 433 (37.3) | 1050 (39.2) | |
3.3. Multivariate analysis
Table 3 shows results of the logistic regression analysis for walkability and social cohesion. In unadjusted analysis, participants in not walkable and slightly walkable neighborhoods had 55% and 39% decreased odds of meeting physical activity recommendations compared to highly walkable neighborhoods (OR = 0.45 [95% CI = 0.31–0.64], OR = 0.61 [95% CI = 0.48–0.77], respectively). Moderately walkable perception was not statistically different from highly walkable (OR = 0.80 [95% CI = 0.63–1.02). In unadjusted analysis, Low and Low-Mid Social cohesion were also associated with decreased odds of meeting PA recommendations compared to high social cohesion (OR = 0.49 [95% CI = 0.36–0.65, OR = 0.74 [95% CI = 0.56–0.96], respectively). When adjusted for one another, they remains similarly associated with meeting PA recommendations (p < 0.001 for both) and relatively unchanged in separate models incorporating covariates. In an adjusted logistic regression, not walkable, slightly walkable, and moderately walkable groups were all less likely to meet physical activity recommendations compared to highly walkable perception (OR = 0.61 [95% CI = 0.41–0.92], OR = 0.65 [95% CI = 0.50–0.85], OR = 0.75 [95% CI = 0.59–0.97], respectively). Low and low-med perceived neighborhood social cohesion were independently associated with decreased odds of meeting recommendations verses high social cohesion (OR = 0.58 [95% CI = 0.43–0.78], OR = 0.71 [95% CI = 0.53–0.93], respectively).
Table 3.
Logistic regression models for odds of meeting PA recommendations.
| OR (95%CI) | p-value | OR* (95%CI) | p-value | aOR**(95%CI) | p-value | aOR*** | p-value | |
|---|---|---|---|---|---|---|---|---|
| Walkability | <0.001 | <0.001 | 0.016 | 0.008 | ||||
| Not Walkable | 0.45 (0.31–0.64) | 0.43(0.30–0.61) | 0.64(0.42–0.96) | 0.61(0.41–0.92) | ||||
| Slightly Walkable | 0.61 (0.48–0.77) | 0.57(0.44–0.73) | 0.67(0.52–0.87) | 0.65(0.50–0.85) | ||||
| Moderate Walkable | 0.80 (0.63–1.02) | 0.78(0.62–0.99) | 0.76(0.60–0.98) | 0.75(0.59–0.97) | ||||
| High Walkable | 1.00 (ref) | 1.00 (ref) | 1.00(ref) | 1.00 (ref) | ||||
| Social Cohesion | <0.001 | <0.001 | 0.005 | 0.003 | ||||
| Low | 0.49 (0.36–0.65) | 0.45(0.34–0.60) | 0.60(0.45–0.81) | 0.58(0.43–0.78) | ||||
| Low-Mid | 0.74 (0.56–0.96) | 0.69(0.53–0.90) | 0.73(0.55–0.96) | 0.71(0.53–0.93) | ||||
| High-Mid | 0.96 (0.74–1.23) | 0.90(0.69–1.16) | 0.92(0.71–1.20) | 0.90(0.69–1.17) | ||||
| High | 1.00 (ref) | 1.00(ref) | 1.00(ref) | 1.00(ref) | ||||
| Interaction Term | 0.405 |
*Model includes Walkability and social cohesion.
**Model includes Walkability and covariates or Social Cohesion and covariates.
***Model Includes Walkability, social cohesion, and covariates.
3.4. Interaction analysis
The introduction of the social cohesion*walkability interaction term to the univariate model resulted in no significant effect modification by social cohesion on the effect of walkability on meeting PA recommendations (p = 0.405).
3.5. Sensitivity analysis
Sensitivity analyses were conducted to examine any risk of bias due to inclusion criteria, as well as multicollinearity. Examination of demographics between final population (n = 3826) and those removed for incomplete data (n = 863) revealed only one significant difference. The included population did tend to have a higher population of white members compared to those with incomplete data (data available upon request). Further, analysis for multicollinearity utilizing VIF demonstrated no multicollinearity (all VIF < 2.0). These data are available upon request.
4. Discussion
This study found that a highly walkable neighborhood and high social cohesion were independently associated with meeting physical activity recommendations. For clinicians, inquiry into a patient’s perception of their neighborhood may allow for more focused counseling on topics that seem to matter most. Clinicians may instead be understanding of a poorly walkable neighborhood and direct the patient to other ways to be active. This may include local, affordable gyms within a reasonable distance from the patient’s residence. A clinician’s counseling on exercise has been shown to be effective in influencing patient activity [34]. In addition, community engagement around physical activity, such as walking groups or free community exercises classes may also boost activity in capitalizing on the potential impact of social cohesion and social support [35].
These data add to the continually growing landscape of evidence suggesting that high perceived walkability is associated with increases in physical activity [17], [36], [37], [38]. Martin et al found similar results in a population of North Carolina residents with arthritis [17]. Maisel et al found similar results in a cohort of older adults in Erie County, New York [38]. This study extends these geographic areas assessed to the rest of the country, allowing for further generalizability. However, in contrast to the van Holle study, no effect modification was identified on the part of social cohesion [18]. This population was, on average younger, than the van Holle study. Older adults have been noted to be more heavily tied to their community than younger individuals, which may explain why this effect was not found [39]. The mechanism of connection between neighborhood walkability perception and physical activity has yet to be fully explained, with causation particularly difficult to nail down [40]. However, a recent study assessed patients around the time of a move from a less walkable to a more walkable neighborhood and found that physical activity increased post-move [41]. Further, certain types of PA seem to be more strongly tied to walkability, particularly active transport [42]. This study offers a glimpse into how neighborhood environment seems to influence PA, with further attention warranted to the specific questions utilized to assess walkability and which seem to influence PA the most.
This study has several strengths, including a large, nationally-representative sample of the US population, valid physical activity data, adjustment for a large number of covariates and confounders, a high response rate, excellent measures of reliability for the scales created, as well as standardized collection of data. The walkability index used was also novel to this data set, as these questions regarding walkability were new to the NHIS in 2015 and only one study has examined them in any context [43]. This study also as several limitations. All data are self-reported, though evidence suggests these data are reliable [26], [44]. Although walkability was the reported perception by the participants, perception of walkability is more likely to influence walking than objective measures [45]. Additionally, the creation of the walkability index may not fully capture the influence of particular elements of walkability that may vary by patient population, with older adults potentially being more influence by route attributes [46]. Further studies are warranted to examine which elements may be most predictive of physical activity, and thus have the most potential as public health targets. This study is also limited by the definition of arthritis as a wide array of self-reported chronic conditions, although previous studies have shown this to be a reliable measure [20]. In addition, the five conditions grouped together as arthritis all benefit from exercise. Further investigation in to each of these disease states may also yield disease-specific recommendations. This study was limited by the available variables in the NHIS data and the questions used to assess these variables, such as safety. The present study fails to establish causality, given its cross-sectional nature, but seems to add support to the notion that walkable perception may influence physical activity. Further, we are unable to distinguish particular type of activity engaged in for physical activity. This study is also limited by response bias resulting in a population that is disproportionately white. However, this is unfortunately common to these national data sets, but does warrant further investigation [47]. Finally, this study grapples with the directionality of the associations in that “walkers” may choose to live in walkable neighborhoods. In addition, meeting physical activity recommendations does not necessarily mean participants are doing so by walking in their neighborhood. However, older adults tend to do most of their walking within their neighborhood [32].
5. Conclusions
In this nationally-representative study of mid to older adults with arthritis and active joint pain, any perception less than a highly walkable neighborhood was associated with decreased odds of meeting physical activity recommendations. Low social cohesion was independently associated with decreased odds of meeting physical activity recommendations, as well. This study brings further understanding to the distinct contributions of built and social environment, illustrating their individual roles and the complexity of how neighborhoods affect health. Further studies examining which specific elements of neighborhoods may be most influential on physical activity and investigating the potential of augmentation of social ties to improve physical activity may bring further clarity to these associations.
CRediT authorship contribution statement
Sarah Gebauer: Conceptualization, Methodology, Software, Validation, Formal analysis, Data curation, Writing - original draft. Mario Schootman: Methodology, Writing - review & editing, Supervision. Hong Xian: Methodology, Writing - review & editing, Supervision. Pamela Xaverius: Conceptualization, Methodology, Writing - review & editing, Supervision.
Contributor Information
Sarah Gebauer, Email: sarah.gebauer@health.slu.edu.
Mario Schootman, Email: Mario.schootman@ssmhealth.com.
Hong Xian, Email: Hong.xian@slu.edu.
Pamela Xaverius, Email: Pam.xaverius@slu.edu.
Appendix
Table A1.
Distribution of covariates and univariate analysis by walkability perception group. Unweighted frequencies (weighted percent).
| Demographics | Total Population n = 3826 | Not Walkable n = 343 | Low Walkable n = 1174 | Moderate Walkable n = 993 | Highly Walkable n = 1316 | p-value |
|---|---|---|---|---|---|---|
| Age | 0.096 | |||||
| 45–54 | 668 (20.4) | 40 (15.3) | 168 (18.4) | 179 (21.7) | 281 (23.0) | |
| 55–64 | 1141 (32.1) | 107 (35.8) | 350 (30.6) | 291 (30.5) | 393 (33.6) | |
| 65–74 | 1119 (27.2) | 101 (25.9) | 342 (27.7) | 285 (27.4) | 391 (26.9) | |
| 75–84 | 630 (14.6) | 70 (16.1) | 214 (16.6) | 166 (15.3) | 180 (11.6) | |
| 85+ | 268 (5.7) | 25 (6.91) | 100 (6.67) | 72 (5.07) | 71 (4.84) | |
| Sex | 0.586 | |||||
| Male | 1345 (38.2) | 114 (34.9) | 438 (39.6) | 337 (38.1) | 456 (38.0) | |
| Female | 2481 (61.8) | 229 (65.1) | 736 (60.4) | 656 (61.9) | 860 (62.0) | |
| Race/Ethnicity | <0.001 | |||||
| Non-Hispanic White | 2802 (78.1) | 274 (84.3) | 990 (87.8) | 725 (78.2) | 813 (66.3) | |
| Non-Hispanic Black | 561 (11.6) | 46 (9.55) | 116 (7.50) | 144 (11.6) | 255 (16.4) | |
| Other | 137 (3.91) | 6 (3.18) | 22 (2.11) | 37 (3.78) | 72 (6.10) | |
| Hispanic | 326 (6.42) | 17 (2.97) | 46 (2.66) | 87 (6.42) | 176 (11.3) | |
| Education | 0.005 | |||||
| HS Diploma/GED or less | 1355 (30.4) | 167 (42.2) | 434 (33.2) | 329 (25.5) | 425 (28.1) | |
| Some College-AA/Bachelors | 1965 (53.0) | 154 (47.2) | 575 (50.6) | 523 (55.8) | 713 (55.0) | |
| Masters and Above | 506 (16.5) | 22 (10.6) | 165 (16.2) | 141 (18.7) | 178 (16.9) | |
| Income to Poverty Threshold Ratio | <0.001 | |||||
| <1.00 | 639 (12.3) | 58 (12.9) | 161 (9.80) | 159 (10.9) | 261 (15.9) | |
| 1.00–1.99 | 938 (21.3) | 109 (31.2) | 307 (23.0) | 225 (17.2) | 297 (19.8) | |
| 2.00–3.99 | 1102 (29.5) | 99 (25.5) | 360 (32.2) | 286 (30.3) | 357 (27.5) | |
| 4.00 or More | 1147 (36.8) | 77 (30.4) | 346 (34.9) | 323 (41.6) | 401 (36.7) | |
| Marital Status | 0.001 | |||||
| Married/Living with Partner | 1741 (60.0) | 163 (61.0) | 610 (64.9) | 439 (59.9) | 529 (55.0) | |
| Widowed/Divorced/Separated | 1731 (33.3) | 161 (34.4) | 500 (30.3) | 458 (34.3) | 612 (35.1) | |
| Never Married | 354 (6.67) | 19 (4.58) | 64 (4.85) | 96 (5.81) | 175 (9.83) | |
| Perceived Social Cohesion | <0.001 | |||||
| High | 1336 (35.2) | 138 (42.3) | 492 (40.6) | 325 (32.5) | 381 (29.9) | |
| High-Mid | 895 (23.9) | 56 (15.1) | 270 (23.9) | 256 (27.1) | 313 (24.1) | |
| Low-Mid | 829 (22.9) | 80 (25.9) | 213 (19.7) | 209 (21.8) | 327 (26.2) | |
| Low | 766 (17.9) | 69 (16.7) | 199 (15.8) | 203 (18.6) | 295 (19.8) | |
| Safety | <0.001 | |||||
| Never Barrier | 2282 (60.6) | 145 (40.8) | 677 (57.1) | 591 (62.5) | 869 (69.0) | |
| Low Barrier | 948 (25.5) | 115 (34.3) | 329 (30.1) | 240 (24.4) | 264 (19.0) | |
| Moderate Barrier | 397 (9.43) | 49 (16.4) | 115 (8.57) | 100 (8.93) | 133 (8.50) | |
| High Barrier | 199 (4.43) | 34 (8.47) | 53 (4.22) | 62 (4.23) | 50 (3.53) | |
| Weather as a Barrier | <0.001 | |||||
| Almost Always | 1147 (28.7) | 124 (35.2) | 379 (31.7) | 300 (29.1) | 344 (23.2) | |
| Most of the Time | 490 (13.3) | 40 (12.5) | 150 (14.5) | 124 (12.6) | 176 (12.8) | |
| Some of the Time | 823 (22.4) | 34 (10.0) | 222 (20.1) | 239 (25.9) | 328 (25.6) | |
| A little of the Time | 440 (11.7) | 24 (6.08) | 117 (10.2) | 118 (11.4) | 181 (14.5) | |
| Never | 926 (24.0) | 121 (36.2) | 306 (23.5) | 212 (21.1) | 287 (22.9) | |
| Length of Time in Neighborhood | 0.001 | |||||
| <1 year | 203 (5.03) | 9 (2.30) | 57 (4.75) | 47 (4.06) | 90 (7.01) | |
| 1–3 years | 460 (11.6) | 30 (9.88) | 122 (10.2) | 121 (11.3) | 187 (13.7) | |
| 4–10 years | 871 (21.7) | 64 (19.2) | 247 (20.4) | 242 (23.0) | 318 (22.8) | |
| 11–20 years | 809 (23.0) | 64 (19.8) | 239 (22.5) | 221 (24.2) | 285 (23.6) | |
| >20 years | 1483 (38.6) | 176 (48.8) | 509 (42.1) | 362 (37.3) | 436 (32.9) | |
Table A2.
Full results of logistic regression models for odds of meeting PA recommendations.
| OR | 95% CI | p-value | aOR | 95% CI | P-value | |
|---|---|---|---|---|---|---|
| Walkability | <0.001 | 0.008 | ||||
| Not Walkable | 0.45 | 0.31–0.64 | 0.61 | 0.41–0.92 | ||
| Slightly Walkable | 0.61 | 0.48–0.77 | 0.65 | 0.50–0.85 | ||
| Moderately Walkable | 0.80 | 0.63–1.02 | 0.75 | 0.59–0.97 | ||
| Highly Walkable | 1.00 | Reference | 1.00 | Reference | ||
| Age | 0.020 | |||||
| 45–54 | 1.00 | Reference | ||||
| 55–64 | 0.80 | 0.59–1.09 | ||||
| 65–74 | 0.83 | 0.61–1.12 | ||||
| 75–84 | 0.68 | 0.47–0.99 | ||||
| 85+ | 0.36 | 0.19–0.67 | ||||
| Sex | 0.203 | |||||
| Male | 1.00 | Reference | ||||
| Female | 0.87 | 0.69–1.08 | ||||
| Race/Ethnicity | 0.223 | |||||
| Non-Hispanic White | 1.00 | Reference | ||||
| Non-Hispanic Black | 0.83 | 0.59–1.17 | ||||
| Other | 1.51 | 0.95–2.40 | ||||
| Hispanic | 1.07 | 0.71–1.62 | ||||
| Education | <0.001 | |||||
| HS Diploma/GED or less | 0.34 | 0.24–0.49 | ||||
| Some College-AA/Bachelors | 0.60 | 0.44–0.82 | ||||
| Masters and Above | 1.00 | Reference | ||||
| Income to Poverty Threshold Ratio | <0.001 | |||||
| <1.00 | 0.41 | 0.28–0.61 | ||||
| 1.00–1.99 | 0.42 | 0.31–0.56 | ||||
| 2.00–3.99 | 0.49 | 0.39–0.62 | ||||
| 4.00 or More | 1.00 | Reference | ||||
| Marital Status | 0.039 | |||||
| Married/Living with Partner | 1.00 | Reference | ||||
| Widowed/Divorced/Separated | 1.35 | 1.07–1.70 | ||||
| Never Married | 1.12 | 0.73–1.71 | ||||
| Perceived Social Cohesion | 0.003 | |||||
| High | 1.00 | Reference | ||||
| High-Mid | 0.90 | 0.69–1.17 | ||||
| Low-Mid | 0.71 | 0.53–0.93 | ||||
| Low | 0.58 | 0.43–0.78 | ||||
| Safety | 0.359 | |||||
| Never Barrier | 1.00 | Reference | ||||
| Low Barrier | 1.19 | 0.94–1.51 | ||||
| Moderate Barrier | 0.87 | 0.59–1.28 | ||||
| High Barrier | 0.91 | 0.48–1.70 | ||||
| Weather as a Barrier | <0.001 | |||||
| Almost Always | 0.73 | 0.53–1.01 | ||||
| Most of the Time | 0.95 | 0.67–1.34 | ||||
| Some of the Time | 2.01 | 1.50–2.68 | ||||
| A little of the Time | 2.23 | 1.59–3.12 | ||||
| Never | 1.00 | Reference | ||||
| Length of Time in Neighborhood | 0.341 | |||||
| <1 year | 0.93 | 0.58–1.47 | ||||
| 1–3 years | 1.01 | 0.71–1.42 | ||||
| 4–10 years | 1.19 | 0.91–1.55 | ||||
| 11–20 years | 0.84 | 0.63–1.14 | ||||
| >20 years | 1.00 | Reference |
References
- 1.Centers for Disease Control Prevalence and most common causes of disability among adults--United States, 2005. Morbidity and Mortality Weekly Report. 58(16): p. 421-426. [PubMed]
- 2.Hootman J.M. Updated Projected prevalence of self-reported doctor-diagnosed arthritis and arthritis-attributable activity limitation among US adults, 2015–2040. Arthritis Rheumatol. 2016;68(7):1582–1587. doi: 10.1002/art.39692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Machado G.C. Efficacy and safety of paracetamol for spinal pain and osteoarthritis: systematic review and meta-analysis of randomised placebo controlled trials. BMJ. 2015;350 doi: 10.1136/bmj.h1225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.da Costa B.R., Nuesch E., Kasteler R., Husni E., Welch V., Rutjes A.W.S., Juni P. Oral or transdermal opioids for osteoarthritis of the knee and hip. Cochrane Database System. Rev. 2014;2014(9) doi: 10.1002/14651858.CD003115.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bannuru R.R. Comparative effectiveness of pharmacologic interventions for knee osteoarthritis: a systematic review and network meta-analysis. Ann. Intern. Med. 2015;162(1):46–54. doi: 10.7326/M14-1231. [DOI] [PubMed] [Google Scholar]
- 6.Birtwhistle R. Prevalence and management of osteoarthritis in primary care: an epidemiologic cohort study from the Canadian Primary Care Sentinel Surveillance Network. CMAJ Open. 2015;3(3):E270–E275. doi: 10.9778/cmajo.20150018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sosa-Reina M.D. Effectiveness of therapeutic exercise in fibromyalgia syndrome: a systematic review and meta-analysis of randomized clinical trials. Biomed Res. Int. 2017;2017:2356346. doi: 10.1155/2017/2356346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hurkmans E. Dynamic exercise programs (aerobic capacity and/or muscle strength training) in patients with rheumatoid arthritis. Cochrane Database Syst. Rev. 2009;(4) doi: 10.1002/14651858.CD006853.pub2. p. CD006853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vignon E., Valat J.P., Rossignol M., Avouac B., Rozenberg S., Thoumie P., Avouac J., Nordin M., Hilliquin P. Osteoarthritis of the knee and hip and activity: a systematic international review and synthesis (OASIS) Joint Bone Spine. 2006;73:442–455. doi: 10.1016/j.jbspin.2006.03.001. [DOI] [PubMed] [Google Scholar]
- 10.Fransen M., McConnell S., Harmer A.R., Van der Esch M., Simic M., Bennell K.L. Exercise for osteoarthritis of the knee. Cochrane Database Syst. Rev. 2015 doi: 10.1002/14651858.CD004376.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hootman J.M., Macera C.A., Ham S.A., Helmick C.G., Sniezek J.E. Physical activity levels among the general US adult population and in adults with and without arthritis. Arthritis Rheum. 2003;49(1):129–135. doi: 10.1002/art.10911. [DOI] [PubMed] [Google Scholar]
- 12.Shih M. Physical activity in men and women with arthritis National Health Interview Survey, 2002. Am. J. Prev. Med. 2006;30(5):385–393. doi: 10.1016/j.amepre.2005.12.005. [DOI] [PubMed] [Google Scholar]
- 13.Segura-Jimenez V. Differences in sedentary time and physical activity between female patients with fibromyalgia and healthy controls: the al-Andalus project. Arthritis Rheumatol. 2015;67(11):3047–3057. doi: 10.1002/art.39252. [DOI] [PubMed] [Google Scholar]
- 14.Fontaine K.R., Heo, Moonseong H., Bathon J. Are US adults with arthritis meeting public health recommendations for physical activity? Arthritis Rheum. 2004;50(2):624–628. doi: 10.1002/art.20057. [DOI] [PubMed] [Google Scholar]
- 15.Sugiyama T. Do relationships between environmental attributes and recreational walking vary according to area-level socioeconomic status? J. Urban Health-Bull. New York Acad. Med. 2015;92(2):253–264. doi: 10.1007/s11524-014-9932-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rollings K.A., Wells N.M., Evans G.W. Measuring physical neighborhood quality related to health. Behav. Sci. (Basel) 2015;5(2):190–202. doi: 10.3390/bs5020190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Martin K.R. Associations of perceived neighborhood environment on health status outcomes in persons with arthritis. Arthritis Care Res. (Hoboken) 2010;62(11):1602–1611. doi: 10.1002/acr.20267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Van Holle V. Interactions between neighborhood social environment and walkability to explain Belgian older adults' physical activity and sedentary time. Int. J. Environ. Res. Public Health. 2016;13(6) doi: 10.3390/ijerph13060569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.CDC. About the National Health Interview Survey. 2016 [cited 2017; Available from: https://www.cdc.gov/nchs/nhis/about_nhis.htm.
- 20.Murphy L.B. Defining Arthritis for Public Health Surveillance: Methods and Estimates in Four US Population Health Surveys. Arthritis Care Res. (Hoboken) 2017;69(3):356–367. doi: 10.1002/acr.22943. [DOI] [PubMed] [Google Scholar]
- 21.Peeters G.M.E.E., Alshurafa M., Schaap L., de Vet H.C.W. Diagnostic accuracy of self-reported arthritis in the general adult population is acceptable. J. Clin. Epidemiol. 2015;68:452–459. doi: 10.1016/j.jclinepi.2014.09.019. [DOI] [PubMed] [Google Scholar]
- 22.Murphy L.B. Annual incidence of knee symptoms and four knee osteoarthritis outcomes in the Johnston county osteoarthritis project. Arthritis Care Res. (Hoboken) 2016;68(1):55–65. doi: 10.1002/acr.22641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Collins J.E., Katz J.N., Dervan E.E., Losina E. Trajectories and risk profiles of pain in persons with radiographic, sympomatic knee osteoarthritis: data from the osteoarthritis initiative. Osteoarthritis Cartilage. 2014;22:622–630. doi: 10.1016/j.joca.2014.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yi S.S. Racial/ethnic differences in associations between neighborhood social cohesion and meeting physical activity guidelines, United States, 2013–2014. Prev. Chronic Dis. 2016;13:E165. doi: 10.5888/pcd13.160261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Centers for Disease Control and Prevention Current Physical Activity Guidelines. 11/29/2016 [cited 2018 04/10/2018]; Available from: https://www.cdc.gov/cancer/dcpc/prevention/policies_practices/physical_activity/guidelines.htm.
- 26.Sun F., Norman I.J., While A.E. Physical activity in older people: a systematic review. BMC Public Health. 2013;13:449. doi: 10.1186/1471-2458-13-449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Villanueva K. The impact of neighborhood walkability on walking: Does it differ across adult life stage and does neighborhood buffer size matter? Health Place. 2014;25:43–46. doi: 10.1016/j.healthplace.2013.10.005. [DOI] [PubMed] [Google Scholar]
- 28.Becerra M.B. Social determinants of physical activity among adult Asian-Americans: results from a population-based survey in California. J. Immigr. Minor. Health. 2015;17(4):1061–1069. doi: 10.1007/s10903-014-0074-z. [DOI] [PubMed] [Google Scholar]
- 29.Gidlow C. A systematic review of the relationship between socio-economic position and physical activity. Health Educ. J. 2006;65(4):338–367. [Google Scholar]
- 30.Pratt M. Does perceived neighborhood walkability and safety mediate the association between education and meeting physical activity guidelines? Prev Chronic Dis. 2015;12:E46. doi: 10.5888/pcd12.140570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wilcox S., Der Ananian C., Abbott J., Vrazel J., Ramsey C., Sharpe P.A., Brady T. Perceived Exercise bariers, enablers, and benefits among exercising and nonexercising adults with arthritis: results from a qualitative study. Arthritis Rheum. 2006;55(4):616–627. doi: 10.1002/art.22098. [DOI] [PubMed] [Google Scholar]
- 32.Ory M.G. Social and environmental predictors of walking among older adults. BMC Geriatr. 2016;16:155. doi: 10.1186/s12877-016-0327-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lewis T.H. CRC Press, Taylor & Francis Group; Boca Raton: 2017. Complex Survey Data Analysis with SAS; p. 326. xiii. [Google Scholar]
- 34.Orrow G. Effectiveness of physical activity promotion based in primary care: systematic review and meta-analysis of randomised controlled trials. BMJ. 2012;344 doi: 10.1136/bmj.e1389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bauman A.E. Correlates of physical activity: why are some people physically active and others not? Lancet. 2012;380(9838):258–271. doi: 10.1016/S0140-6736(12)60735-1. [DOI] [PubMed] [Google Scholar]
- 36.Van Holle V., Van Cauwenberg J., Van Dyck D., Deforche B., Van de Weghe N., De Bourdeaudhuij I. Relationship between neighborhood walkability and older adults' physical activity: results from the Belgain Environmental Physical Activity Study in Seniors (BEPAS Seniors) Int. J. Behav. Nutrit. Phys. Activity. 2014;11(110) doi: 10.1186/s12966-014-0110-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Forjuoh S.N. Determinants of walking among middle-aged and older overweight and obese adults: sociodemographic, health, and built environmental factors. J. Obes. 2017;2017:9565430. doi: 10.1155/2017/9565430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Maisel J.L. Impact of older adults' neighborhood perceptions on walking behavior. J. Aging. Phys. Act. 2016;24(2):247–255. doi: 10.1123/japa.2014-0278. [DOI] [PubMed] [Google Scholar]
- 39.Berke E.M. Association of the built environment with physical activity and obesity in older persons. Am. J. Public Health. 2007;97(3):486–492. doi: 10.2105/AJPH.2006.085837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.McCormack G.R., Shiell A. In search of causality: a systematic review of the relationship between the built environment and physical activity among adults. Int. J. Behav. Nutr. Phys. Activity. 2011;8(125) doi: 10.1186/1479-5868-8-125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zhu X. A retrospective study on changes in residents' physical activities, social interactions, and neighborhood cohesion after moving to a walkable community. Prev. Med. 2014;69(Suppl. 1):S93–S97. doi: 10.1016/j.ypmed.2014.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Smith M. Systematic literature review of built environment effects on physical activity and active transport - an update and new findings on health equity. Int. J. Behav. Nutr. Phys. Act. 2017;14(1):158. doi: 10.1186/s12966-017-0613-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Whitfield G.P. Environmental supports for physical activity, national health interview survey-2015. Am. J. Prev. Med. 2018;54(2):294–298. doi: 10.1016/j.amepre.2017.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Echeverria S.E., Diez-Roux A.V., Link B.G. Reliability of self-reported neighborhood characteristics. J. Urban Health. 2004;81(4):682–701. doi: 10.1093/jurban/jth151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Tuckel P., Milczarski W. Walk score(TM), perceived neighborhood walkability, and walking in the US. Am. J. Health Behav. 2015;39(2):242–256. doi: 10.5993/AJHB.39.2.11. [DOI] [PubMed] [Google Scholar]
- 46.Sugiyama T. Destination and route attributes associated with adults' walking: a review. Med. Sci. Sports Exerc. 2012;44(7):1275–1286. doi: 10.1249/MSS.0b013e318247d286. [DOI] [PubMed] [Google Scholar]
- 47.Moreno-John G. Ethnic minority older adults participating in clinical research: developing trust. J Aging Health. 2004;16(5 Suppl.):93S–123S. doi: 10.1177/0898264304268151. [DOI] [PubMed] [Google Scholar]