Abstract
Background and aims
DSM-5 includes Internet gaming disorder (IGD) as a condition for further study. While online and offline gaming may produce undesired negative effects on players, we know little about the nosology of IGD and its prevalence, especially in countries with emerging economies.
Methods
A self-administered survey has been employed to estimate prevalence of DSM-5 IGD and study the structure and performance of an instrument in Spanish to measure DSM-5 IGD among 7,022 first-year students in 5 Mexican universities that participated in the University Project for Healthy Students (PUERTAS), part of the World Health Organization’s World Mental Health International College Student Initiative.
Results
The scale for IGD showed unidimensionality with factor loadings between 0.694 and 0.838 and a Cronbach’s α = .816. Items derived from gaming and from substance disorders symptoms mixed together. We found a 12-month prevalence of IGD of 5.2% in the total sample; prevalence was different for males (10.2%) and females (1.2%), but similar for ages 18–19 years (5.0%) and age 20+ (5.8%) years. Among gamers, the prevalence was 8.6%. Students with IGD were more likely to report lifetime psychological or medical treatment [OR = 1.8 (1.4–2.4)] and any severe role impairment [OR = 2.4 (1.7–3.3)]. Adding any severe role impairment to the diagnostic criteria decreased the 12-month prevalence of IGD to 0.7%.
Discussion and conclusions
Prevalence of DSM-5 IGD and the performance of diagnostic criteria in this Mexican sample were within the bounds of what is reported elsewhere. Importantly, about one in every seven students with IGD showed levels of impairment that would qualify them for treatment under DSM-5.
Keywords: gaming, DSM-5, Mexico, college students, epidemiology
Introduction
In 2013, Internet gaming disorder (IGD) was included in the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) as a condition for further study (American Psychiatric Association [APA], 2013). The World Health Organization will include a category of gaming disorder (GD) in the forthcoming International Classification of Disease (ICD-11) manual (World Health Organization [WHO], 2018), thereby making a diagnosis of GD a real possibility for patients and clinicians (Rumpf et al., 2018). While gaming per se may have positive effects on one’s life (Billieux, Flayelle, Rumpf, & Stein, 2019), it is usually accepted that online and offline gaming may also produce undesired negative effects on players, but we still know little about the prevalence and nosology of IGD, particularly in countries with emerging economies that have less access to Internet services.
Studies of IGD prior to the publication of the DSM-5 tended to have lax inclusion criteria, usually selecting small samples of gamers with unknown backgrounds and using varied diagnostic criteria (Petry, Rehbein, Ko, & O’Brien, 2015; Saunders et al., 2017). Not surprisingly, estimates for the prevalence of gaming ranged widely from 0.7% to 27.5% (Mihara & Higuchi, 2017) when pre-DSM-5 studies are considered. Nevertheless, since the publication of DSM-5 in 2013, research has tended to be more unified in defining gaming using the nine symptoms suggested by DSM-5 (Petry et al., 2014). Recent reviews have shown an increasing number of studies in this area that aim to provide prevalence estimates for DSM-5 IGD and which evaluate different instruments to assess this disorder (Fam, 2018; Feng, Ramo, Chan, & Bourgeois, 2017). In new reviews, the prevalence of IGD was reported to be around 4.7% (Feng et al., 2017), and usually higher among males than females (Petry, Zajac, & Ginley, 2018). More studies are available among youth, placing the prevalence in this age group at about 4.6% (Fam, 2018).
Although the nine criteria used for defining IGD in the DSM-5 have become dominant, the implementation of these criteria varies at large extent. Pontes (2016) found 7 different scales for DSM-5 IGD and a more recent review increased the number to 11 scales (Almedia, 2018). The statistical techniques for assessing these scales have not been uniform but, in general, the nine criteria for IGD seem to form a unidimensional continuum of disorder with a single factor. Although studies focus on prevalence find differences by sex and age groups, very few studies document possible differences in sociodemographic performance of these scales, the so-called differential item functioning (DIF; Lemmens, Valkenburg, & Gentile, 2015). The study of DIF is important as possible differences in prevalences could be due to the way the key demographic groups (e.g., males and females) interpret the questions on gaming, rather than to their level of severity of the disorder. Another matter of relevance is that both the DSM-5 and the forthcoming ICD-11 state that symptoms for gaming should also lead to “clinically significant impairment or distress” (APA, 2013) or “the behavior pattern is of sufficient severity to result in significant impairment in personal, family, social, educational, occupational or other important areas of functioning” (WHO, 2018). While it has been suggested that studies on gaming should use measures of functional impairment to evaluate the clinical relevance of this condition (Rumpf et al., 2019), this is rarely done. To the best of our knowledge, only two studies included a diagnosis of IGD with impairment (Jeong et al., 2018; Przybylski, Weinstein, & Murayama, 2017). In the Przybylski et al.’s study, the inclusion of an additional criterion of impairment led to a reduction of about 17%–37% in the number of IGD cases identified purely with the nine DSM criteria. This large decrease found in the estimated prevalence of IGD when the criterion of impairment is added needs to be replicated.
Finally, while research is available in western high-income countries and among high-income countries from Asia and also from China (Feng et al., 2017), we are unaware of any studies on this topic in western countries with emerging economies and much less access/use of Internet. We simply do not know if the prevalences reported elsewhere can be applied in countries of emerging economies, besides China. Mexico has a large youth population, females still tend to live under traditional roles and the country has a large group of people living under poverty levels that reduces access to electronic means, including experiences with playing Internet games. Whether these factors might impact the prevalence of IGD is unknown. Our aim here is to report on the performance of a scale for DSM-5 IGD, estimate its prevalence, association with service use for emotional and substance use problems and role of impairment in a large sample of Mexican first-year college students.
Methods
Participants
The PUERTAS (University) Project (for Healthy Students) conducted in five Mexican universities during January 2018–February 2019 included 7,095 incoming first-year students out of which 7,022 had completed surveys with the IGD scale. The Mexican surveys were administered to a convenience sample of five universities that were not randomly selected and therefore the study participants are not representative of all university students in Mexico. Universities were chosen based on their interest in early detection of mental health problems. After the university approval, we used a census design in which all incoming students for the 2018–2019 academic years were invited to participate in a web-based self-report survey. The following universities from five different states of Mexico participated and included the IGD scale: Universidad Autónoma de Aguascalientes (n = 235), Universidad Autónoma de Baja California (n = 6,019), Universidad Autónoma Metropolitana (n = 392), Universidad de la Salle Noroeste (n = 164), and Universidad La Salle Cancún (n = 212). While a larger number of universities in Mexico are participating in the PUERTAS project, we report here only data from those universities that included the IGD scale.
Measures
DSM-5 IGD scale
The instrument used in PUERTAS was developed for the World Health Organization’s World Mental Health Surveys International College Student Initiative (WHO-WMH-ICS) and contains questions based on scales previously utilized and validated, with skip logic such that affirmative answers are further probed.
The section on IGD was developed independently of the main PUERTAS instrument and consisted of 23 items. It was based on the nine symptoms described in the DSM-5 and formulated by an international consensus led by Nancy Petry (Petry et al., 2015) that included an English version and a Spanish translation. For IGD, all 23 questions lead to dichotomous answers (yes/no) and each of the 9 symptoms were considered positive if any of the questions pertaining to a given symptom was positive (yes). As per DSM-5 rules, the presence of five out of nine symptoms means that someone has an IGD. While symptoms of Preoccupation, Withdraw, Tolerance, Loss of control, Giving-up activities, Deception, and Escape were measured by two questions each, symptoms of Continuation were measured with six questions and symptoms of Negative consequences had three questions, because they were more complex to understand (see Supplementary Table S1 for a full description of the 23 questions and how they formed the 9 symptoms). These symptoms are a combination of five items derived from substance use disorders and four items from gambling (Petry et al., 2015) developed by the DSM-5 workgroup in an effort to put together the clinical and research tradition of both substance use and gambling disorders. Whether these nine symptoms, from two different traditions, would hang together was not known during the DSM-5 formulation. Although others have used the DSM-5 formulation literally to construct a 9-item questionnaire for IGD (Pontes & Griffiths, 2015; Wang, Cho, & Kim, 2018), the DSM-5 language is sometimes difficult to follow especially for youth. We preferred here to breakdown the nine symptoms into short dichotomous questions that use a direct formulation and avoid subclauses. We aimed to produce an instrument that uses basic language, has a Spanish translation, and that would be especially apt for young people while remaining true to the DSM-5 formulation, as others have also done for the Netherlands (Lemmens et al., 2015). While this led to more questions (23 instead of 9), we believe that we gained in comprehension. Our aim is to measure IGD using DSM-5 criteria as the framework with a scale that would be easy to understand by young individuals.
Total population and gamers and active gamers
All participants who answered the IGD section (n = 7,022) were asked if they played video games in the past 12 months. Video game users (thereafter called “gamers”) are those who reported playing video games (on a computer, smartphone, console, or any other electronic device) in the past 12 months (yes = 4,262; no = 2,760). To avoid unnecessary respondent burden, the IGD scale is asked only to those gamers who screened positive to the following: if they played, on average, at least 1 day per week and their duration of gaming (during weekday or weekend) was at least 30 min (active gamers: yes = 2,547; no = 1,715) (see Supplementary Figure S1 for a chart description of the sample and Supplementary Table S2 for frequency and time played). The results are presented for the total sample (n = 7,022), for those who are gamers (n = 4,262) and for those who are active gamers (n = 2,547).
Service use
Service use was measured by a series of questions, which asked about current, 12-month, and lifetime treatment for an emotional or substance problem, whether the treatment was psychological counseling or medication, and willingness to seek services within and outside their university should they, during the coming school year, develop an emotional problem that would cause them a lot of distress or interference with school work (Benjet et al., 2019).
Role impairment
Severity of health-related role impairment during the past 12 months was assessed using an adapted version of the Sheehan Disability Scale (Leon, Olfson, Portera, Farber, & Sheehan, 1997; Ormel et al., 2008), and its implementation for this survey was described by Alonso et al. (2018). Four role domains included home management/chores, college-related and other work, close personal relationships, and social life. For example, “Close personal relationships” were specified as “the ability to initiate and maintain close personal relationships.” The scale was labeled as no interference (0), mild (1–3), moderate (4–6), severe (7–9), and very severe (10) interference. Severe self-reported role impairment was defined as having a 7–10 rating in at least one of the four areas. This version of the Sheehan was not specific to IGD.
Procedures
In all universities, incoming first-year students were given the survey link, time, and space to respond. How and when they were given the link and time depended on each university. For example, in the Universidad Autónoma Metropolitana, the survey was administered during the orientation for new students in which students were administered other general questionnaires, whereas in the Universidad de la Salle Noroeste, students were invited and given the link, time, and space to participate during a class of human development, a course for all first-year students. The overall response rate (i.e., the number of students with completed surveys/the number of total incoming first year students as reported by each university) for all participating universities, regardless of their inclusion of the IGD scale, was 79.3%, varying from 44.2% to 90.8% in individual universities (Benjet et al., 2019).
Statistical analyses
To assess the performance of the DSM-5 IGD scale, we followed the usual set of steps used in modern nosological work (Shmulewitz et al., 2011). That included the determination of: (a) internal consistency, where appropriate internal consistency was assessed with α values between 0.7 and 0.9 (Streiner & Geoffrey, 1995), and (b) dimensionality, assessed through factor analysis with the presence of only one eigenvalue >1, examination of the scree plot and adequate model fit indices: comparative fit index (CFI) or Tucker–Lewis index (TLI) ≥ 0.95 and root mean square error approximation (RMSEA) ≤ 0.06. Once unidimensionality was confirmed, we fit a two-parameter logistic (2PL) item response theory (IRT) model for dichotomous traits, to assess difficulty and discrimination of items, and to plot their corresponding item information curves and item characteristics curves. Akaike and Bayesian information criteria (AIC and BIC) as well as sample-size corrected BIC are reported as fit indices for this 2PL model (Muthén & Muthén, 2015).
DIF analysis was performed for two key demographic variables: sex (not males vs. males) and age group (18–19 vs. ≥20 years old). DIF analysis allows determining if subgroups experience differences in item difficulty or discrimination at the same level of the latent trait being measured. In other words, DIF is a procedure to inform if individuals in different subgroups (e.g., males or females) are more likely (or less likely) to endorse different criteria while holding constant underlying trait severity. We performed the IRT assessment of DIF for each of the nine IGD criteria and we also computed tests of DIF for all items jointly. IRT-based DIF assessment is considered a more sensitive method for short scales than the classical methods based on observed scores (Scientific Software International, 2003).
Since our main goal is to provide prevalence estimates for this population in Mexico, we focus on the total prevalence but, where appropriate, we also report results among the subsample of gamers and active gamers. A binomial exact confidence interval (Stata Corp, 2013) was computed for the prevalence of IGD. We report on the estimated prevalence of IGD by gender and age group. χ2 tests with 1 degree of freedom were performed to evaluate differences in the prevalence of DSM-5 IGD and IGD criteria on those variables. Finally, associations between IGD and use of treatment services and role impairment were estimated with multivariate logistic regression models, controlling for sex and age group (Hosmer & Lemeshow, 2000).
Statistical analyses were performed among the total sample and among active gamers for the performance of the IGD scale. Factor analysis and IRT models were conducted with Mplus 7.4 (Muthén & Muthén, 2015), DIF analysis based on IRT models were computed in PARSCALE (Scientific Software International, 2003), and all other statistical analyses were conducted using Stata software version 13.1 (Stata Corp, 2014).
Ethics
The Research Ethics Committee of the National Institute of Psychiatry approved the research protocol. Participation was anonymous and voluntary. Informed consent was obtained from participants through the web platform. Only those aged 18 years or above were eligible to participate. For all participants who answered affirmatively to depressive symptomatology, alcohol or drug problems, any and all suicidal behavior or non-suicidal self-injury, and those experiencing an extremely stressful event in the prior year, an automatic message was displayed providing them with information of where they could obtain professional help. University-based, community-based, and online options were provided.
Results
Table 1 presents the distribution of the sample by key demographic factors. About 55.1% of the sample was female, the majority (72.4%) between 18 and 19 years old, mostly have parents with high-school education (33.6%), and mostly had a positive view of their own academic achievement (e.g., 40.0% think of themselves as in the top 20% of academic rank). Gamers (those who reported playing video games – on a computer, smartphone, console, or any other electronic device – in the past 12 months) were 60.7% of the sample, of which 59% of them being male and younger (74.4%). Active gamers (those who played, on average, at least 1 day per week during a minimum of 30 min) were 36.3% of the sample and more likely to be males. In Supplementary Table S2, we present the playing time distribution for the total sample and among gamers. In the total sample, 7.9% played daily and tended to spend more time playing during weekends than during weekdays. Among gamers, 13% played every day and spend more time playing overall.
Table 1.
Demographic and academic characteristics of the sample obtained from University Project for Healthy Students (PUERTAS), Mexico, 2018–2019
| Total sample (n = 7,022) | Gamers (n = 4,262; 60.7%) | Active gamers (n = 2,547; 36.3%) | ||||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| Gender | ||||||
| Male | 3,117 | 44.6 | 2,502 | 59.0 | 1,872 | 73.9 |
| Female | 3,856 | 55.1 | 1,723 | 40.6 | 657 | 25.9 |
| Other | 19 | 0.3 | 14 | 0.3 | 5 | 0.2 |
| Age (years) | ||||||
| 18–19 | 5,087 | 72.4 | 3,172 | 74.4 | 1,858 | 72.9 |
| 20+ | 1,935 | 27.6 | 1,090 | 25.6 | 689 | 27.1 |
| Maximum parent’s education | ||||||
| Do not know | 44 | 0.6 | 28 | 0.7 | 12 | 0.5 |
| None | 38 | 0.5 | 14 | 0.3 | 7 | 0.3 |
| Elementary | 333 | 4.7 | 140 | 3.3 | 79 | 3.1 |
| Middle school | 1,510 | 21.5 | 869 | 20.4 | 520 | 20.4 |
| High school | 2,361 | 33.6 | 1,454 | 34.1 | 878 | 34.5 |
| Undergraduate | 2,210 | 31.5 | 1,410 | 33.1 | 838 | 32.9 |
| Graduate | 526 | 7.5 | 347 | 8.1 | 213 | 8.4 |
| Self-ranked academic achievement | ||||||
| Top 20% | 2,803 | 40.0 | 1,719 | 40.4 | 1,022 | 40.1 |
| Middle | 2,501 | 35.7 | 1,552 | 36.4 | 930 | 36.5 |
| Bottom 25% | 90 | 1.3 | 57 | 1.3 | 33 | 1.3 |
| Do not know | 1,617 | 23.1 | 930 | 21.8 | 562 | 22.1 |
Note. Not all frequencies add up to the total sample size due to missing values.
In Supplementary Table S1, we present the responses to the 23 questions of the IGD scale (in English and Spanish) and symptom prevalence among the total population, gamers, and active gamers. In Table 2, we present an exploratory factor analysis of the nine symptoms for DSM-5 IGD among active gamers. As evident from these results, a one-factor solution with factor loadings from 0.838 to 0.694 has very good model fit indexes with both CFI and TLI indices above the 0.95 threshold and RMSEA = 0.030. This first factor produced an eigenvalue of 5.82 and a second factor of about 0.63 with a scree plot that suggests that more than one factor is unnecessary. Finally, Cronbach’s α for these nine symptoms was quite adequate (.816).
Table 2.
Exploratory factor analysis of DSM-5 IGD: active gamers (n = 2,547)
| Factor loadings | |
|---|---|
| Criterion | One factor |
| 1. Preoccupation (G) | 0.694* |
| 2. Withdrawal | 0.754* |
| 3. Tolerance | 0.796* |
| 4. Loss of control | 0.744* |
| 5. Giving-up activities | 0.819* |
| 6. Continuation | 0.838* |
| 7. Deception (G) | 0.800* |
| 8. Escape (G) | 0.730* |
| 9. Negative consequences (G) | 0.829* |
| Model fit indices | |
| CFI | 0.994 |
| TLI | 0.992 |
| RMSEA | 0.030 |
| Reliability | |
| Alpha | 0.816 |
Note. DSM-5: fifth edition of the Diagnostic and Statistical Manual of Mental Disorders; IGD: Internet gaming disorder; CFI: comparative fit index; TLI: Tucker–Lewis index; RMSEA: root mean square error of approximation; G: item from the DSM-IV Gambling Disorder Criteria.
*Significant at 5% level. Geomin rotated factors.
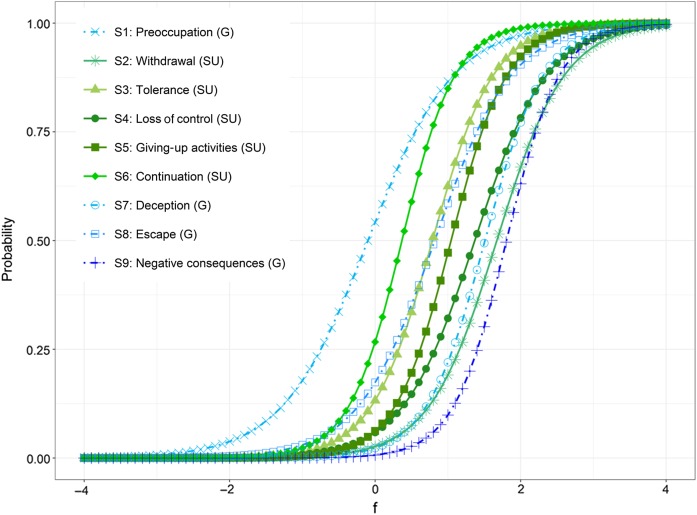
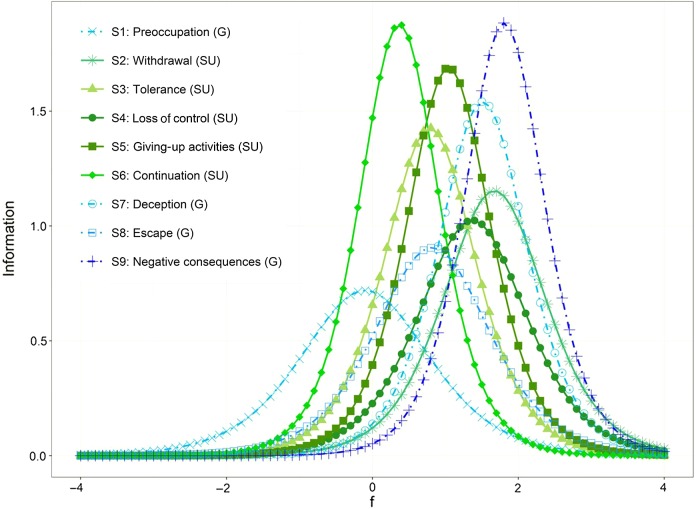
Table 3 presents the two parameters of the IRT analyses among active gamers and Figures 1 and 2 graphically resume this information. The item with higher difficulty (lower prevalence) was “S9-Negative Consequences” (an item from gambling) and the item with lower difficulty (higher prevalence) was “S1-Preocupation,” also from gambling. All other items are grouped closely in the difficulty parameters (Figure 1). Regarding the discrimination parameters, “S9-Negative Consequences” had greater discrimination and “S1-Preocupation” had the lowest.
Table 3.
Item response theory (IRT) analysis of DSM-5 IGD: active gamers (n = 2,547)
| Criterion | IRT parameters | |
|---|---|---|
| Discrimination (SE) | Difficulty (SE) | |
| 1. Preoccupation (G) | 1.70 (0.10) | −0.10 (0.04) |
| 2. Withdrawal | 2.15 (0.15) | 1.67 (0.07) |
| 3. Tolerance | 2.39 (0.14) | 0.79 (0.04) |
| 4. Loss control | 2.03 (0.13) | 1.37 (0.06) |
| 5. Giving-up activities | 2.60 (0.16) | 1.04 (0.04) |
| 6. Continuation | 2.74 (0.17) | 0.37 (0.03) |
| 7. Deception (G) | 2.48 (0.17) | 1.51 (0.06) |
| 8. Escape (G) | 1.90 (0.11) | 0.82 (0.04) |
| 9. Negative consequences (G) | 2.75 (0.24) | 1.81 (0.07) |
| Model fit indices | ||
| AIC | 17,800.8 | |
| BIC | 17,906.0 | |
| SS-BIC | 17,848.8 | |
Note. AIC: Akaike information criterion; BIC: Bayesian information criterion; SS-BIC: sample-size corrected BIC; SE: standard error. G: item from the DSM-IV Gambling Disorder Criteria; DSM-5: fifth edition of the Diagnostic and Statistical Manual of Mental Disorders; IGD: Internet gaming disorder.
Figure 1.
Item characteristic curves of active gamers
Figure 2.
Item information curves of active gamers
Analysis of DIF for age group did not show global differences for discrimination and difficulty, except for the difficulty estimate of “S1-Preocupation,” showing a lower probability for those at least 20 years old compared to those below 20; however, the joint test [χ2(9) = 11.8; p = .222] suggests no difference between age groups for the total scale. Greater DIF was found for sex. Overall, global differences for discrimination [χ2(9) = 21.1; p < .012] and difficulty [χ2(9) = 29.0; p = .001] were found. For the discrimination parameters, we found DIF for “S3-Tolerance,” “S5-Giving-up activities,” and “S7-Deception;” for the difficulty parameters, 4 items showed DIF: “S1-Preocupation,” “S3-Tolerance,” “S6- Continuation,” and “S7-Deception” (DIF results in Supplementary Table S3).
Table 4 presents the results for the endorsement of each symptom and the prevalence of DSM-5 IGD for this sample. About one in every five students expressed “S1-Preocupation” with gaming (one in every three gamers; one out of two active gamers), but “S9-Negative consequences” was rarely endorsed, as was “S2-Withdrawn.” The prevalence for the total population was 5.2% (95% CI = 4.7–5.8), among gamers 8.6% (95% CI = 7.8–9.5) and among active gamers 14.4% (95% CI = 13.1–15.8). The distribution of these symptoms is presented in Supplementary Table S1 for all groups. In the total population, the prevalence was higher for males (10.2%) than females (1.2%; p < .001) and was not different among those 20+ years old (5.8%) than among those 18–19 years old (5.0%; p = .154; Supplementary Table S4).
Table 4.
Prevalence of endorsed IGD criteria
| Criterion | n | Total sample (n = 7,022) | Gamers (n = 4,262) | Active gamers (n = 2,547) |
|---|---|---|---|---|
| % | % | % | ||
| 1. Preoccupation (G) | 1,348 | 19.2 | 31.6 | 52.9 |
| 2. Withdrawal | 247 | 3.5 | 5.8 | 9.7 |
| 3. Tolerance | 670 | 9.5 | 15.7 | 26.3 |
| 4. Loss control | 379 | 5.4 | 8.9 | 14.9 |
| 5. Giving-up activities | 491 | 7.0 | 11.5 | 19.3 |
| 6. Continuation | 969 | 13.8 | 22.8 | 38.1 |
| 7. Deception (G) | 274 | 3.9 | 6.4 | 10.8 |
| 8. Escape (G) | 692 | 9.9 | 16.3 | 27.2 |
| 9. Negative consequences (G) | 162 | 2.3 | 3.8 | 6.4 |
| DSM-5 IGD (positive to five or more criteria) | 367 | 5.2 | 8.6 | 14.4 |
Note. All other from the DSM-IV substance use disorder criteria. G: item from the DSM-IV Gambling Disorder Criteria; DSM-5: fifth edition of the Diagnostic and Statistical Manual of Mental Disorders; IGD: Internet gaming disorder.
Table 5 shows the association of DSM-5 IGD with lifetime treatment (psychological and pharmacological) and severe impairment in four domains. The most common form of treatment was psychological and almost all of those with an IGD who reported pharmacological treatment also reported psychological treatment. Among those with an IGD, 21.9% reported ever having any treatment and were 1.8 times more likely to report it, compared to those negative to IGD. More severe impairment was reported by those with IGD (statistically significant in all domains and total score). Those with IGD were 2.4 times more likely to report severe impairment than those free of IGD.
Table 5.
Clinical predictors of DSM-5 IGD, controlled by gender and age group
| IGD status | ||||||
|---|---|---|---|---|---|---|
| Negative (0–4 symptoms) | Positive (5–9 symptoms) | aOR | [95% CI] | |||
| n | % | n | % | |||
| Lifetime psychological treatment | ||||||
| No | 5,586 | 84.5 | 287 | 78.6 | 1.0 | – |
| Yes | 1,026 | 15.5 | 78 | 21.4 | 1.9* | [1.4–2.4] |
| Lifetime medical treatment | ||||||
| No | 6,293 | 96.6 | 342 | 94.5 | 1.0 | – |
| Yes | 224 | 3.4 | 20 | 5.5 | 1.8* | [1.1–3.0] |
| Lifetime any treatment | ||||||
| No | 5,541 | 84.0 | 286 | 78.1 | 1.0 | – |
| Yes | 1,054 | 16.0 | 80 | 21.9 | 1.8* | [1.4–2.4] |
| 12-month treatment | ||||||
| No | 6,456 | 98.0 | 360 | 98.4 | 1.0 | – |
| Yes | 130 | 2.0 | 6 | 1.6 | 1.0 | [0.4–2.4] |
| Severe impairment – home | ||||||
| Not severe | 6,486 | 98.1 | 351 | 96.4 | 1.0 | – |
| Severe | 128 | 1.9 | 13 | 3.6 | 2.1* | [1.1–3.8] |
| Severe impairment – work/school | ||||||
| Not severe | 6,400 | 96.9 | 337 | 92.8 | 1.0 | – |
| Severe | 206 | 3.1 | 26 | 7.2 | 2.6* | [1.7–4.1] |
| Severe impairment – relationships | ||||||
| Not severe | 6,298 | 95.7 | 339 | 93.1 | 1.0 | – |
| Severe | 285 | 4.3 | 25 | 6.9 | 1.8* | [1.1–2.8] |
| Severe impairment – social | ||||||
| Not severe | 6,300 | 95.8 | 337 | 92.6 | 1.0 | – |
| Severe | 276 | 4.2 | 27 | 7.4 | 1.9* | [1.3–3.0] |
| Severe impairment – total | ||||||
| Not severe | 6,145 | 92.8 | 313 | 85.8 | 1.0 | – |
| Severe | 478 | 7.2 | 52 | 14.2 | 2.4* | [1.7–3.3] |
Note. Total sample (n = 7,022). Not all frequencies add up to the total sample size due to missing values. aOR: adjusted odds ratio (by gender and age group); CI: confidence interval; DSM-5: fifth edition of the Diagnostic and Statistical Manual of Mental Disorders; IGD: Internet gaming disorder.
*p < .05.
As reported in Table 4, there were 367 cases of IGD. If we add to our definition of IGD the extra criteria of reporting clinical impairment (any severe impairment per our definition here), only 52 students would qualify for IGD + impairment for a total prevalence of 0.7% (1.2% among gamers). Only about 14% of the initial 367 IGD cases would classify with a disorder. That is, about one in every seven students with IGD showed levels of impairment that would qualify them as in need for treatment under the DSM-5 definition.
Discussion
To summarize, in this large sample of first-year college students, the 12-month prevalence of 5+ symptoms of IGD was of 5.2% in the total population, 8.6% among gamers, and 14.4% among active gamers. Males had a higher prevalence than females. The IGD scale that we used in this survey performed well and suggested that IGD has a unidimensional structure. The total scale suggested no clear signs of differential functioning for age groups, while DIF for gender was strong. Those with IGD showed increased use of mental health services and were more likely to report severe levels of impairment. While the total prevalence of IGD was sizable, few respondents with 5+ symptoms of IGD (1 in every 7) reported levels of “clinically significant impairment or distress” that could lead them to receive a DSM-5 clinical diagnosis.
A wide array of estimates for GD have been reported, with meta-analyses suggesting a prevalence of about 4.7% (Mihara & Higuchi, 2017). Our prevalence of 5.2% is just above this summary estimate, but within the range of what has been reported before, for example, in the Netherlands (5.4%; Lemmens et al., 2015) and in Germany (5.7%; Wartberg, Kriston, & Thomasius, 2017) but below what has been reported in South Korea of 10.8% (Wang et al., 2018). There is no other research in Mexico, Latin America, or in other developing Western countries for us to compare with. Nevertheless, for a comparison with other addictive disorders, it has been estimated that the 12-month prevalence of any substance use disorder in the general population of Mexico is 2.6% (Degenhardt et al., 2017), so that IGD would be about 2 times more frequent than a most common group of disorders in Mexico. The 12-month prevalence of drug abuse/dependence in the whole PUERTAS survey is 1.5% (Benjet et al., 2019), also below the estimated prevalence of IGD. This is particularly worrisome as the prevalence of this study pertains to college students, a relatively affluent and otherwise healthy group in our country. It is then possible that, when making a diagnosis of IGD, more attention needs to be paid to levels of impairment, which would reduce the prevalence to 0.7%. While impairment has been considered before to characterize patients with some form of Internet addiction (Bernardi & Pallanti, 2009), to the best of our knowledge, there are only two other studies that used DSM-5 coupled with impairment to define GD. In a multisite study (Przybylski et al., 2017), these authors reported on four samples with prevalences of 0.32%, 0.47%, 0.68%, and 1.04%, much lower prevalences that usually reported elsewhere. A second study (Jeong et al., 2018) reported a prevalence of 1.94% with impairment. Our own prevalence with impairment is nevertheless similar to those. Clearly, a careful consideration of the public health impact of IGD and need for treatment is necessary in the current discussion of this disorder (Rumpf et al., 2018).
The performance of our scale of IGD was very adequate by the usual psychometric properties and similar to that has been reported elsewhere with instruments with similar lengths (Lemmens et al., 2015). Of particular interest is that a single factor explained IGD (unidimensionality structure), similar to that has been reported in one of the mostly used 9-item scales available for IGD (Pontes & Griffiths, 2015). Unidimensionality has been reported in other studies around the globe that used the same instrument, in Italy (Monacis, De Palo, Griffiths, & Sinatra, 2016), Portugal (Pontes & Griffiths, 2016), Slovenia (Pontes, Macur, & Griffiths, 2016), Hungary (Király et al., 2017), combined samples in America, India, and the United Kingdom (Pontes, Stavropoulos, & Griffiths, 2017) and combined samples in America, Australia, and the United Kingdom (Stavropoulos et al., 2018). Others have found that while one factor may be sufficient to explain the structure of IGD, two factors or a second-order factor model may also be a better representation of the underlying psychometric structure of IGD (Lemmens et al., 2015; Wichstrøm, Stenseng, Belsky, von Soest, & Hygen, 2019). In general, a consensus is emerging in the field in which the nine symptoms that were described originally by the DSM-5 and first put forward by an international group (Petry et al., 2015) are a very appropriate representation of the psychological problems that some gamers may present. Our results regarding DIF for sex may mean that females and males (within the same level of IGD) are not answering similarly to the same questions on gaming. More research on this topic seems to be warranted and suggests caution in the interpretation of the results when comparing male/female differences (Wu et al., 2017). Overall, whether the problems derived from gaming may constitute or not a true psychiatric disorder of sufficient clinical impairment to require the use of health services is still discussed (Rumpf et al., 2018); the evidence from our own study and from others (Przybylski et al., 2017) show this to be the case for at least a minority of cases.
Limitations
Prevalence estimates are based on a convenience sample of colleges, limiting generalizability of results, and were obtained using a self-report web-based survey rather than a comprehensive clinical diagnostic interview and therefore should be considered a screening of possible cases rather than a confirmed diagnosis. In addition, the IGD scale was not validated by a clinical interview for Mexican youth specifically. The universities included were both public and private, but they were not randomly selected and therefore the study participants are not representative of all university students in Mexico. They are nevertheless representative of first-year’s students of the participating universities and are not a convenience sample of unknown gamers from Internet sites of video gamers, for which we know nothing about their basic demographic distribution and most importantly the population from where they come (Rumpf et al., 2019).
In the DSM-5, functional impairment is not specifically operationalized. Instead, it is stated that the disorder should result in significant impairment. In this study, functional impairment was assessed in general by the Sheehan Disability Scale and was not specifically related to gaming. Therefore, other conditions like comorbid mental or physical disorders might have been the underlying cause for impairment. This limitation might have overestimated the prevalence of IGD with the inclusion of the impairment criterion. In addition, functional impairment was defined as having at least severe impairment based on the Sheehan Disability Scale, corresponding to a score between 7 and 10. However, significant impairment might even be observed in lower scores. Moreover, this conservative approach might detect cases in early, nevertheless severe stages of the disorder. The current definition of IGD (5 out 9 symptoms) means that heterogeneity of cases is likely to occur. At this stage, we cannot know with certainty if our detected cases of IGD are composed mainly of highly involved individuals or by gamers with a disorder-like pattern that could be considered pathological. The addition of an impairment criterion, as has been proposed before and implemented here, has the advantage of adding a severity threshold to the definition of IGD.
Another point that needs to be discussed is that in our questionnaire the assessment of “continued use despite negative consequences” was assessed by experiencing a number of adverse consequences. These negative consequences were not necessarily due to continued use. Because of this, the high endorsement rate for this criterion might be explained. This very sensitive conceptualization of continued use despite negative consequences might have overestimated prevalence without consideration of functional impairment. However, it is solely related to one of the nine criteria and does not impede the general finding that the inclusion of an additional assessment of functional impairment reduces the prevalence markedly. Nevertheless, the difference between assessments with/without functional impairment might have been overestimated.
Finally, our current analyses are limited in our inability to report on other psychometric properties such as types of validity, test–retest reliability, etc., for which another study would be necessary, but is beyond the scope of this project.
Despite these limitations, this study has clear advantages compared to the two other studies that added impairment to the IGD definition. This is the first study that assessed functional impairment with a sound and well-established independent measure of functional impairment. Second, this study does not include participants from convenience samples recruited online or via treatment settings. Therefore, it provides important findings from young adults in an unselected sample.
Conclusions
With rates of Internet use of about 64% in 2017, far below what is reported by developed countries such as Denmark (97%; The World Bank, 2018), GD has not been studied much in Mexico, or for that matter in other countries with emerging economies. Our results show that among a large sample of college students, where Internet use is pervasive, about 2/3 of these students are gamers and 5+ symptoms from DSM-5 IGD were present in almost 1 out of 12 gamers, not too different from what is found elsewhere. For a minority of these student gamers, clinical responses may already be needed and will need to be scaled up in the near future with wider availability of Internet.
Acknowledgements
The survey was carried out in conjunction with the WHO World Mental Health International College Surveys Initiative (WHO-WMH-ICS). The authors would like to thank the WHO-WMH-ICS collaborators and staff for assistance with instrumentation.They would also like to acknowledge the participation of Nancy Petry on an early stage of this research. Nancy shared her work and scale with the authors and supervised the translation and back translation of the Spanish version of her questionnaire. Nancy was a generous colleague, a leading scholar and the authors state that they are in great debt to her legacy.
Funding Statement
Funding sources: Dr. CB received support from the National Council on Science and Technology (CONACyT; CB 285548) and the Fundación Miguel Alemán A.C.
Authors’ contribution
The initial draft of this paper was prepared by GB in cooperation with RO and CB. CB was responsible for obtaining funding. GB, CB, MEM-M, RAG-G, YA, HUW, and PM participated in the study concept and design. YA and RAGG coordinated the universities and supervised the study implementation. KIMM, EVC, ALJP, AJPC, PCHU, GEQC, and ACD implemented the study in their universities. GB, RO, and EM participated in the analysis and interpretation of data. All authors reviewed and approved the final version of the manuscript.
Conflict of interest
The authors declare no conflict of interest.
References
- Almedia S. J. (2018). A Pertubacao do Jogo pela Internet (Instituto de Ciências Biomédicas Abel Salazar da Universidade do Porto, Mestrado Integrado em Medicina) [Disturbance of gaming by the Internet (Institute of Biomedical Sciences Abel Salazar, University of Porto, Integrated Master Degree in Medicine)]. Retrieved from https://repositorio-aberto.up.pt/bitstream/10216/114082/2/277622.pdf
- Alonso J., Vilagut G., Mortier P., Auerbach R. P., Bruffaerts R., Cuijpers P., Demyttenaere K., Ebert D. D., Ennis E., Gutiérrez-García R. A., Green J. G., Hasking P., Lee S., Bantjes J., Nock M. K., Pinder-Amaker S., Sampson N. A., Zaslavsky A. M., Kessler R. C. (2018). The role impairment associated with mental disorder risk profiles in the WHO World Mental Health International College Student Initiative. International Journal of Methods in Psychiatric Research, 28(2), e1750. doi: 10.1002/mpr.1750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association [APA]. (2013). Diagnostic and statistical manual of mental disorders: DSM-5 (1st ed.). Washington, DC: American Psychiatric Association. [Google Scholar]
- Benjet C., Gutiérrez-García R., Abrego-Ramírez A., Borges G., Covarrubias-Díaz A., Durán M. D. S., González-González R., Hermosillo-de la Torre A. E., Martínez-Martínez K. I., Medina-Mora M. E., Mejía-Zarazúa H., Pérez-Tarango G., Zavala-Berbena M. A., Mortier P. (2019). Psychopathology and self-harm among incoming first-year students in six Mexican universities. Salúd Pública de México, 61(1), 16–26. doi: 10.21149/9158 [DOI] [PubMed] [Google Scholar]
- Bernardi S., Pallanti S. (2009). Internet addiction: A descriptive clinical study focusing on comorbidities and dissociative symptoms. Comprehensive Psychiatry, 50(6), 510–516. doi: 10.1016/j.comppsych.2008.11.011 [DOI] [PubMed] [Google Scholar]
- Billieux J., Flayelle M., Rumpf H. J., Stein D. J. (2019). High involvement versus pathological involvement in video games: A crucial distinction for ensuring the validity and utility of gaming disorder. Current Addiction Reports, 6(3), 323–330. doi: 10.1007/s40429-019-00259-x [DOI] [Google Scholar]
- Degenhardt L., Glantz M., Evans-Lacko S., Sadikova E., Sampson N., Thornicroft G., Aguilar-Gaxiola S., Al-Hamzawi A., Alonso J., Helena Andrade L., Bruffaerts R., Bunting B., Bromet E. J., Miguel Caldas de Almeida J., de Girolamo G., Florescu S., Gureje O., Maria Haro J., Huang Y., Karam A., Karam E. G., Kiejna A., Lee S., Lepine J. P., Levinson D., Elena Medina-Mora M., Nakamura Y., Navarro-Mateu F., Pennell B. E., Posada-Villa J., Scott K., Stein D. J., Ten Have M., Torres Y., Zarkov Z., Chatterji S., Kessler R. C., & WMH Surveys Collaborators. (2017). Estimating treatment coverage for people with substance use disorders: An analysis of data from the World Mental Health Surveys. World Psychiatry, 16(3), 299–307. doi: 10.1002/wps.20457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- du Toit M. (Ed.). (2003). IRT from SSI: Bilog-MG, multilog, parscale, testfact. Lincolnwood, IL: Scientific Software International, Inc. [Google Scholar]
- Fam J. Y. (2018). Prevalence of Internet gaming disorder in adolescents: A meta-analysis across three decades. Scandinavian Journal of Psychology, 59(5), 524–531. doi: 10.1111/sjop.12459 [DOI] [PubMed] [Google Scholar]
- Feng W., Ramo D. E., Chan S. R., Bourgeois J. A. (2017). Internet gaming disorder: Trends in prevalence 1998–2016. Addictive Behaviors, 75, 17–24. doi: 10.1016/j.addbeh.2017.06.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hosmer D. W., Lemeshow S. (2000). Applied logistic regression (2nd ed.). New York, NY: Wiley & Sons. [Google Scholar]
- Jeong H., Yim H. W., Lee S. Y., Lee H. K., Potenza M. N., Kwon J. H., Koo H. J., Kweon Y.-S., Bhang S.-Y., Choi J. S. (2018). Discordance between self-report and clinical diagnosis of Internet gaming disorder in adolescents. Scientific Reports, 8(1), 10084. doi: 10.1038/s41598-018-28478-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Király O., Sleczka P., Pontes H. M., Urbán R., Griffiths M. D., Demetrovics Z. (2017). Validation of the Ten-Item Internet Gaming Disorder Test (IGDT-10) and evaluation of the nine DSM-5 Internet Gaming Disorder criteria. Addictive Behaviors, 64, 253–260. doi: 10.1016/j.addbeh.2015.11.005 [DOI] [PubMed] [Google Scholar]
- Lemmens J. S., Valkenburg P. M., Gentile D. A. (2015). The Internet Gaming Disorder Scale. Psychological Assessment, 27(2), 567–582. doi: 10.1037/pas0000062 [DOI] [PubMed] [Google Scholar]
- Leon A. C., Olfson M., Portera L., Farber L., Sheehan D. V. (1997). Assessing psychiatric impairment in primary care with the Sheehan Disability Scale. The International Journal of Psychiatry in Medicine, 27(2), 93–105. doi: 10.2190/T8EM-C8YH-373N-1UWD [DOI] [PubMed] [Google Scholar]
- Mihara S., Higuchi S. (2017). Cross-sectional and longitudinal epidemiological studies of Internet gaming disorder: A systematic review of the literature. Psychiatry and Clinical Neurosciences, 71(7), 425–444. doi: 10.1111/pcn.12532 [DOI] [PubMed] [Google Scholar]
- Monacis L., De Palo V., Griffiths M. D., Sinatra M. (2016). Validation of the Internet Gaming Disorder Scale-Short-Form (IGDS9-SF) in an Italian-speaking sample. Journal of Behavioral Addictions, 5(4), 683–690. doi: 10.1556/2006.5.2016.083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén L., Muthén B. (2015). MPlus: Statistical analysis with latent variables – User’s guide (7th ed.). Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- Ormel J., Petukhova M., Chatterji S., Aguilar-Gaxiola S., Alonso J., Angermeyer M. C., Bromet E. J., Burger H., Demyttenaere K., de Girolamo G., Haro J. M., Hwang I., Karam E., Kawakami N., Lépine J. P., Medina-Mora M. E., Posada-Villa J., Sampson N., Scott K., Ustün T. B., Von Korff M., Williams D. R., Zhang M., Kessler R. C. (2008). Disability and treatment of specific mental and physical disorders across the world. The British Journal of Psychiatry, 192(5), 368–375. doi: 10.1192/bjp.bp.107.039107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petry N. M., Rehbein F., Gentile D. A., Lemmens J. S., Rumpf H. J., Mößle T., Bischof G., Tao R., Fung D. S., Borges G., Auriacombe M., González Ibáñez A., Tam P., O’Brien C. P. (2014). An international consensus for assessing Internet gaming disorder using the new DSM-5 approach. Addiction, 109(9), 1399–1406. doi: 10.1111/add.12457 [DOI] [PubMed] [Google Scholar]
- Petry N. M., Rehbein F., Ko C. H., O’Brien C. P. (2015). Internet gaming disorder in the DSM-5. Current Psychiatry Reports, 17(9), 72. doi: 10.1007/s11920-015-0610-0 [DOI] [PubMed] [Google Scholar]
- Petry N. M., Zajac K., Ginley M. K. (2018). Behavioral addictions as mental disorders: To be or not to be? Annual Review of Clinical Psychology, 14(1), 399–423. doi: 10.1146/annurev-clinpsy-032816-045120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pontes H. (2016). Current practices in the clinical and psychometric assessment of Internet gaming disorder in the era of the DSM-5: A mini review of existing assessment tools. Mental Health and Addiction Research, 1(1), 18–19. doi: 10.15761/MHAR.1000105 [DOI] [Google Scholar]
- Pontes H., Griffiths M. (2015). Measuring DSM-5 Internet gaming disorder: Development and validation of a Short Psychometric Scale. Computers in Human Behavior, 45, 137–143. doi: 10.1016/j.chb.2014.12.006 [DOI] [Google Scholar]
- Pontes H., Griffiths M. (2016). Portuguese validation of the Internet Gaming Disorder Scale-Short-Form. Cyberpsychology, Behavior, and Social Networking, 19(4), 288–293. doi: 10.1089/cyber.2015.0605 [DOI] [PubMed] [Google Scholar]
- Pontes H., Macur M., Griffiths M. (2016). Internet gaming disorder among Slovenian primary schoolchildren: Findings from a nationally representative sample of adolescents. Journal of Behavioral Addictions, 5(2), 304–310. doi: 10.1556/2006.5.2016.042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pontes H., Stavropoulos V., Griffiths M. (2017). Measurement invariance of the Internet Gaming Disorder Scale-Short-From (IGDS9-SF) between the United States of America, India and the United Kingdom. Psychiatry Research, 257, 472–478. doi: 10.1016/j.psychres.2017.08.013 [DOI] [PubMed] [Google Scholar]
- Przybylski A. K., Weinstein N., Murayama K. (2017). Internet gaming disorder: Investigating the clinical relevance of a new phenomenon. American Journal of Psychiatry, 174(3), 230–236. doi: 10.1176/appi.ajp.2016.16020224 [DOI] [PubMed] [Google Scholar]
- Rumpf H. J., Achab S., Billieux J., Bowden Jones H., Carragher N., Demetrovics Z., Higuchi S., King D. L., Mann K., Potenza M., Saunders J. B., Abbott M., Ambekar A., Aricak O. T., Assanangkornchai S., Bahar N., Borges G., Brand M., Chan E. M., Chung T., Derevensky J., Kashef A. E., Farrell M., Fineberg N. A., Gandin C., Gentile D. A., Griffiths M. D., Goudriaan A. E., Grall-Bronnec M., Hao W., Hodgins D. C., Ip P., Király O., Lee H. K., Kuss D., Lemmens J. S., Long J., Lopez-Fernandez O., Mihara S., Petry N. M., Pontes H. M., Rahimi-Movaghar A., Rehbein F., Rehm J., Scafato E., Sharma M., Spritzer D., Stein D. J., Tam P., Weinstein A., Wittchen H. U., Wölfling K., Zullino D., Poznyak V. (2018). Including gaming disorder in the ICD-11: The need to do so from a clinical and public health perspective. Journal of Behavioral Addictions, 7(3), 556–561. doi: 10.1556/2006.7.2018.59 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rumpf H. J., Brandt D., Demetrovics Z., Billieux J., Carragher N., Brand M., Bowden-Jones H., Rahimi-Movaghar A., Assanangkornchai S., Tkalić R. G., Borges G., Lee H.-K., Rehbein F., Fineberg N. A., Mann K., Potenza M., Stein D. J., Higuchi S., King D. L., Saunders J. B., Poznyak V. (2019). Epidemiological challenges in the study of behavioral addictions: A call for high standard methodologies. Current Addiction Reports, 6(3), 331–337. doi: 10.1007/s40429-019-00262-2 [DOI] [Google Scholar]
- Saunders J. B., Hao W., Long J., King D. L., Mann K., Fauth M., Rumpf H. J., Bowden-Jones H., Rahimi-Movaghar A., Chung T., Chan E., Bahar N., Achab S., Lee H. K., Potenza M., Petry N., Spritzer D., Ambekar A., Derevensky J., Griffiths M. D., Pontes H. M., Kuss D., Higuchi S., Mihara S., Assangangkornchai S., Sharma M., Kashef A. E., Ip P., Farrell M., Scafato E., Carragher N., Poznyak V. (2017). Gaming disorder: Its delineation as an important condition for diagnosis, management, and prevention. Journal of Behavioral Addictions, 6(3), 271–279. doi: 10.1556/2006.6.2017.039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shmulewitz D., Keyes K. M., Wall M. M., Aharonovich E., Aivadyan C., Greenstein E., Spivak B., Weizman A., Frisch A., Grant B. F., Hasin D. S. (2011). Nicotine dependence, abuse and craving: Dimensionality in an Israeli sample. Addiction, 106(9), 1675–1686. doi: 10.1111/j.1360-0443.2011.03484.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stata Corp. (2013). Stata 13 base reference manual [Computer software]. College Station, TX: Stata Press. [Google Scholar]
- Stata Corp. (2014). Stata Statistical Software. Release 13.1 [Computer software]. College Station, TX: Stata Corp LP. [Google Scholar]
- Stavropoulos V., Beard C., Griffiths M. D., Buleigh T., Gomez R., Pontes H. M. (2018). Measurement invariance of the Internet Gaming Disorder Scale–Short-Form (IGDS9-SF) between Australia, the USA, and the UK. International Journal of Mental Health and Addiction, 16(2), 377–392. doi: 10.1007/s11469-017-9786-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Streiner D. L., Geoffrey R. N. (1995). Health measurement scales: A practical guide to their development and use (2nd ed). New York, NY: Oxford University Press. [Google Scholar]
- The World Bank. (2018). Individuals using the Internet (% of population). Retrieved from https://data.worldbank.org/indicator/IT.NET.USER.ZS
- Wang H. R., Cho H., Kim D.-J. (2018). Prevalence and correlates of comorbid depression in a nonclinical online sample with DSM-5 Internet gaming disorder. Journal of Affective Disorders, 226, 1–5. doi: 10.1016/j.jad.2017.08.005 [DOI] [PubMed] [Google Scholar]
- Wartberg L., Kriston L., Thomasius R. (2017). The prevalence and psychosocial correlates of Internet gaming disorder. Deutsches Arzteblatt International, 114(25), 419–424. doi: 10.3238/arztebl.2017.0419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wichstrøm L., Stenseng F., Belsky J., von Soest T., Hygen B. W. (2019). Symptoms of Internet gaming disorder in youth: Predictors and comorbidity. Journal of Abnormal Child Psychology, 47(1), 71–83. doi: 10.1007/s10802-018-0422-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization [WHO]. (2018). ICD-11 international classification of diseases for mortality and morbidity statistics (11th rev. ed.). Geneva, Switzerland: World Health Organization. [Google Scholar]
- Wu T.-Y., Lin C.-Y., Årestedt K., Griffiths M. D., Broström A., Pakpour A. H. (2017). Psychometric validation of the Persian Nine-Item Internet Gaming Disorder Scale-Short Form: Does gender and hours spent online gaming affect the interpretations of item descriptions? Journal of Behavioral Addictions, 6(2), 256–263. doi: 10.1556/2006.6.2017.025 [DOI] [PMC free article] [PubMed] [Google Scholar]