Abstract
Objectives
To investigate the effect of pH and buffers on the degradation rate of flucloxacillin and to determine if flucloxacillin can be stabilised using a buffered diluent for up to 14 days when stored at 2°C–8°C including a 24-hour infusion period at 32°C in two elastomeric devices (Accufuser and INfusor LV) filled to 240 mL. Testing as per the NHS Pharmaceutical Quality Assurance Committee Yellow Cover Document (YCD) requirements.
Methods
A validated stability indicating high-performance liquid chromatography method was used for assessing the stability of flucloxacillin diluted in 0.3% w/v citrate-buffered saline pH 7.0 when stored at 2°C–8°C in two ambulatory devices (Accufuser and INfusor LV). Flucloxacillin at 10 and 50 mg/mL diluted in 0.3% w/v citrate-buffered saline pH 7.0 to a final volume of 240 mL and stored at 2°C–8°C, including 24 hours at 32°C, was tested from two batches in replicate (n=3) at five time points for up to 14 days according to the requirements of the YCD.
Results
Greater than 95% of the zero-time concentration of flucloxacillin at 10 and 50 mg/mL remained when stored at 2°C–8°C after 14 days including 24 hours at 32°C in both Accufuser and INfusor LV devices.
Conclusions
Flucloxacillin sodium stability was improved, and complied with UK national standards, by using a diluent of 0.3% w/v citrate-buffered saline pH 7 in both Accufuser and INfusor LV ambulatory devices when filled to 240 mL. The data support assigning a shelf-life of up to 14 days (13 days stored at 2°C–8°C and 24 hours at 32°C). Flucloxacillin may now be used appropriately as a continuous 24-hour infusion in outpatient parenteral antimicrobial therapy services, providing further opportunity to avoid or shorten patient hospital stays, as well as support ideal antimicrobial stewardship principles.
Keywords: flucloxacillin, stability, elastomeric pump, ambulatory, antimicrobial stewardship, outpatient parenteral antimicrobial chemotherapy
What this paper adds.
What is already known on this subject
Flucloxacillin is a narrow-spectrum Gram-positive antibiotic used for a number of serious infections in hospital including Staphylococcus aureus bacteraemia, skin and soft tissue infection, endocarditis and osteomyelitis.
The frequency of dosing required for flucloxacillin to maintain therapeutic efficacy renders it unsuitable for most outpatient parenteral antimicrobial therapy (OPAT) services and there is a need for data on flucloxacillin stability in extended infusions to suit OPAT services.
Flucloxacillin degrades rapidly in aqueous solutions during extended storage without chemical stabilisation.
What this study adds
The study presents data on the use of a citrate buffer to stabilise solutions of flucloxacillin (at concentrations 10–50 mg/mL) for up to 14 days at 2°C–8°C plus 24 hours at 32°C when reconstituted and diluted in a 0.3% w/v citrate-buffered saline diluent with storage in two ambulatory device reservoirs (Accufuser and INfusor L).
These data will support the use of extended infusions of flucloxacillin in OPAT services.
Introduction
It is common practice within outpatient parenteral antimicrobial therapy (OPAT) services to use daily administered, relatively broad-spectrum antibiotics such as ceftriaxone for indications that otherwise would be adequately treated with narrower spectrum agents which require more frequent dosing. This can be at odds with the principles of antimicrobial stewardship.1 The use of narrower spectrum agents which require multiple doses to be administered in a 24-hour period has been limited by the capacity of OPAT services to manage this, and the inconvenience to the patient. The availability of portable ambulatory (elastomeric) devices to administer intravenous antibiotics is an attractive option for OPAT services, as these devices enable the patient to receive prolonged infusions and repeated doses of intravenous antibiotics, either at home or in a clinic setting, avoiding the need for hospitalisation or patient/carer antibiotic reconstitution and administration. A significant barrier to the widespread use of narrow-spectrum antibiotics in portable ambulatory devices in OPAT is the availability of published stability data particularly in prolonged infusion.2 The British Society of Antimicrobial Chemotherapy OPAT Drug Stability Testing Working Group has recently reviewed the available stability data for antibiotics in ambulatory devices against national quality control standards and found insufficient evidence to support their use.3
The logistics of compounding these devices and delivering them to their point of use means that acceptable shelf-life must be in the order of days, and ideally, weeks. Another complication is that devices are worn close to the body, which results in a raised temperature during infusion, accelerating degradation of the antibiotic.4 5 These factors must be taken into account before an antibiotic can be administered by an ambulatory device, to ensure that patients receive the prescribed dose of antibiotic and therefore encourage favourable clinical outcomes.
Flucloxacillin is a narrow-spectrum penicillin antibiotic with activity against important Gram-positive pathogens including Staphylococcus aureus and Streptococcus pyogenes. In its intravenous form it is the preferred antibiotic for a number of serious infections in hospital including S. aureus bacteraemia, skin and soft tissue infection, endocarditis and osteomyelitis. However, the short shelf-life, accompanied with efficacy linked to the amount of time the drug concentration is above the bacterial minimum inhibitory concentration, requires four to six administrations per day. In addition, there is insufficient published evidence to support the extended storage of flucloxacillin. Ahmed and Parkinson report significant losses with infusions of flucloxacillin in water for injection (WFI) at 100 mg/mL when stored in syringes at 2°C–8°C for 7 days.6 These factors significantly limit its use in OPAT service models.
In this study, we first explored the use of buffers to control pH and improve flucloxacillin stability and then applied this to demonstrate acceptable stability of flucloxacillin sodium solutions at concentrations used in ambulatory devices. Furthermore, the study employed temperatures most likely encountered in clinical practice.7 8 The study provides a shelf-life for flucloxacillin in two ambulatory devices compatible with practical OPAT requirements.
Materials and methods
Materials
Chemicals used were high-performance liquid chromatography (HPLC) grade acetonitrile, CAS 75-05-08 (Thermo Fisher Scientific, Loughborough, UK), sodium phosphate dibasic (Acros Organics, Belgium), trisodium citrate dihydrate, CAS 6132-04-03 (Sigma Aldrich, UK) and citric acid, CAS 5949-29-1 (Fisher Scientific), all of analytical grade. MilliQ >18 Mega Ohm purified water was generated (Elix Merck Millipore, UK).
Flucloxacillin injection—flucloxacillin sodium powder for injection manufactured by Bowmed Ibisqus (Wrexham, UK) batch number 6056HH; phial size 1 g. Each phial was reconstituted in WFI (Hameln Pharmaceuticals, UK) as recommended by the manufacturer.
Ambulatory infusion devices used were a silicone balloon infuser (Accufuser C100L, supplied by Vygon, Oxford, UK) and an elastomeric reservoir (INfusor LV, supplied by Baxter Healthcare, UK). Both devices have a maximum capacity of 300 mL but were filled to a final volume of 240 mL.
Citrate (0.3 % w/v) buffered sodium chloride pH 7, 100 mL was supplied by Preston Pharmaceuticals (Preston Royal Hospital, Preston, UK).
Chromatographic apparatus and conditions
The following stability indicating liquid chromatography method was developed for the analysis of flucloxacillin employing a Thermo Fisher Scientific Ultimate (U) HPLC System with diode array detection and Chromeleon software V.6.9 (Thermo Fisher Scientific). The HPLC column was a Kinetex XB-C18 2.0 μm 100 A, 100 mm×2.1 mm (Phenomenex, Macclesfield, UK); mobile phase 70: 30, 0.05 M potassium dihydrogen orthophosphate adjusted to pH 7: acetonitrile; flow rate 0.3 mL/min; injection volume 10 µL, detection wavelength 225 nm; acquisition time 7.0 min; column temperature ambient; autosampler temperature 5°C.
Preparation of solutions for analysis
Flucloxacillin sodium standards (n=2) containing 0.1 and 0.05 mg/mL were prepared and injected (n=6) at the beginning of an HPLC run to demonstrate system precision. All standards (n=2) and test samples (n=2) were prepared and analysed (n=3) in replicate. Samples were stored at 5°C during HPLC analysis and were completed within 12 hours of sample preparation to avoid additional degradation.
Validation of the HPLC method
Detector linearity was demonstrated from 0.01 to 0.25 mg/mL with R2 values (correlation coefficient) of 1.0000, 0.9971 and 0.9993 (n=3). Slopes were 1042, 996 and 998, respectively. Precision and accuracy were performed (n=5) with replicate injections (n=3) at a concentration of 0.1 mg/mL. The mean % relative SDs (RSD) were 1.9% and not greater than 0.3% respectively.
Forced degradation was undertaken using 0.1 M hydrochloric acid, 0.1 M sodium hydroxide and 3% hydrogen peroxide. Flucloxacillin was prepared in each solution at a concentration of 1 mg/mL, stored at ambient temperature, sampled immediately after preparation and after 30, 60 and 120 min.
In acid stored at ambient temperature the flucloxacillin peak area reduced by 50% after 60 min storage with evidence of precipitation. In hydroxide complete loss of the flucloxacillin peak occurred after 30 min at room temperature. In 3% (v/v) peroxide, >50% degradation occurred after 30 min storage at room temperature. All additional peaks were clearly resolved from the flucloxacillin peak.
Peak purity for the flucloxacillin peak with generation of a peak match under each stress condition was performed using Chromeleon V.6.9 software. Spectra of each peak were compared with a reference spectrum at three peak positions: front (50%), top (100%) and tail (−50%) and scored from 1000. The RSD of the peak match was reported. All spectra had a score match >900 and low RSDs. The above supports the method being stability-indicating for flucloxacillin.
pH was determined using a glass combination electrode and Orion 420A pH metre calibrated each day using the National Institute of Standards and Technology traceable standards (Thermo Fisher Scientific).
Subvisible particle counts were determined by light obscuration using the HIAC Royco 9703 liquid particle counting system (Beckman Coulter, High Wycombe, UK).
Results
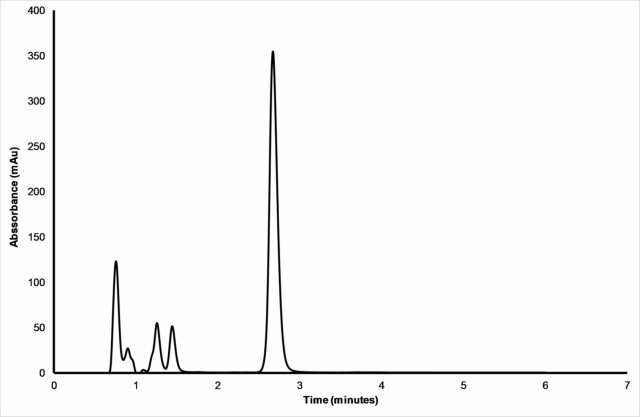
A stability indicating HPLC-diode array detector method was developed to fully separate all degradation species from the active flucloxacillin. This was achieved using standard methods including forced degradation as described in the Methods section. An example of a typical chromatogram showing separation of the active flucloxacillin peak at a retention time of 2.7 min from all degradant peaks is shown in figure 1.
Figure 1.
A typical chromatogram of flucloxacillin (retention time 2.7 min) at 1 mg/mL under forced degradation conditions of 0.1 M NaOH after 5 min incubation. Detection performed at 225 nm.
Effect of pH and buffers on flucloxacillin stability
The stability of flucloxacillin in solution was assessed under four separate storage conditions: (1) unbuffered water as diluent, (2) unbuffered normal saline as diluent, (3) a mixed citrate/phosphate (MCP) buffer at 0.2 M, and (4) a citrate buffer at 5.25% w/v in saline. These conditions allowed assessment of flucloxacillin stability over a range of pH values between pH 5 and 8 units and allowed a comparison of the stability of unbuffered flucloxacillin solutions in both 0.9% saline and water diluents to buffered flucloxacillin solutions. Flucloxacillin stability was assessed at two clinically relevant concentrations of 10 and 50 mg/mL. All solutions were stressed by heating at 37°C for 24 hours.
The results of tests over the pH range 4–7 indicated that, while degradation was lowest within the pH range 6–7, the overall rates of degradation were too high to be able to assign a useful shelf-life. Evidence of precipitation was also observed. The tests were repeated using citrate buffer at 5.25% w/v, which gave a pH of 7.8 unadjusted. The results showed that degradation of flucloxacillin was substantially lower compared with the MCP buffer, and pH was unimportant compared with selecting citrate buffer to control the pH as opposed to using an MCP diluent system. However, the improved degradation rates with the 5.25% w/v citrate buffer (<10%) did not comply with the Yellow Cover Document (YCD) stipulated acceptable limit of less than 5% loss of active drug.7
Finally, a lower concentration of citrate buffer (0.3% w/v, 0.01 M) pH 7 was evaluated. Flucloxacillin was tested (n=3) at both 10 and 50 mg/mL using the lower concentration 0.3% w/v citrate buffer. Heating of flucloxacillin in 0.3% w/v citrate buffer solution at 37°C for 24 hours resulted in recoveries of between 96% and 102% of active drug irrespective of pH adjustment or the drug concentration used.
Investigations showed that employing 0.3% w/v citrate buffer as the diluent for flucloxacillin solutions provided appropriate stability for at least 24 hours when heated to 37°C. This was also independent of drug concentration over the range required in clinical practice. The 0.3% w/v citrate buffer was then taken forward for use in the main stability study.
Stability of flucloxacillin in elastomeric device reservoirs during extended storage and administration
The stability of flucloxacillin solutions containing 10 and 50 mg/mL flucloxacillin was assessed using a citrate-buffered saline at pH 7 containing 0.3% w/v sodium citrate as a diluent in two different ambulatory devices.
To prepare the devices, a sufficient volume of each flucloxacillin solution was prepared using 0.3% w/v citrate-buffered saline for reconstitution and dilution. Phials were manually shaken to ensure complete dissolution. The nominal reservoir fill volume of 240 mL was transferred from this solution to each device (n=3) using a 60 mL syringe, thus ensuring each of the devices contained the same drug concentration. Devices were tested in triplicate. Filled devices were stored for 7 days at 2°C–8°C, followed by 24 hours at 32°C. A second batch was prepared and stored for 13 days at 2°C–8°C, followed by 24 hours at 32°C. At each test point, a 35 mL aliquot was taken via the administration tube for analysis.
The results showed that all flucloxacillin solutions throughout the study period remained colourless, clear in appearance and free from visible particles. Subvisible counts remained within acceptable limits throughout the study.9 The pH range for both concentrations at the commencement of the study was 6.5–7.0 pH units. A small trend to lower pH was observed during storage, in particular for solutions after storage at the elevated temperature.
Flucloxacillin concentrations in the device reservoirs after storage for 7 and 13 days at 2°C–8°C, followed by 24 hours at 32°C are shown in tables 1 and 2.
Table 1.
Flucloxacillin content during storage in Accufuser device reservoirs
| Storage at 2oC–8oC (days) | 10 mg/mL | 50 mg/mL | ||||||
| Batch 1 | Batch 2 | Batch 1 | Batch 2 | |||||
| FLU concentration % of initial remaining | 95% CI (±) | FLU concentration % of initial remaining | 95% CI (±) | FLU concentration % of initial remaining | 95% CI (±) | FLU concentration % of initial remaining | 95% CI (±) | |
| 0 | 10.05* | 1.19 | 10.26* | 0.61 | 50.55* | 1.01 | 49.68* | 1.01 |
| 3 | 103.8 | 0.60 | – | – | 99.7 | 1.15 | – | – |
| 7 | – | – | 99.9 | 0.25 | – | – | 101.4 | 1.21 |
| 7+1† | – | – | 100.8 | 1.39 | – | – | 101.7 | 1.53 |
| 10 | 102.5 | 0.22 | – | – | 99.2 | 0.93 | – | |
| 13 | 101.6 | 0.50 | – | – | 97.8 | 0.46 | – | – |
| 13+1† | 100.1 | 0.63 | – | – | 97.2 | 0.71 | – | – |
*Concentration in mg/mL at zero time. 95% CI.
†+1=24 hours at 32°C.
FLU, flucloxacillin.
Table 2.
Flucloxacillin content during storage in INfusor LV device reservoirs
| Storage at 2oC–8oC (days) | 10 mg/mL | 50 mg/mL | ||||||
| Batch 1 | Batch 2 | Batch 1 | Batch 2 | |||||
| FLU concentration % of initial remaining | 95% CI (±) | FLU concentration % of initial remaining | 95% CI (±) | FLU concentration % of initial remaining | 95% CI (±) | FLU concentration % of initial remaining | 95% CI (±) | |
| 0 | 10.01* | 0.29 | 10.86* | 3.19 | 49.84* | 1.37 | 49.63* | 2.20 |
| 3 | 104.9 | 3.08 | – | – | 104.25 | 0.58 | – | – |
| 7 | 100.6 | 0.37 | 95.21 | 1.50 | 97.97 | 0.50 | 102.58 | 1.87 |
| 7+1† | – | – | 96.59 | 1.07 | – | – | 104.74 | 0.57 |
| 10 | 103.89 | 1.03 | – | – | 105.22 | 2.20 | – | |
| 13 | 99.6 | 0.46 | – | – | 98.25 | 1.23 | – | – |
| 13+1† | 99.6 | 0.31 | – | – | 96.47 | 0.96 | – | – |
*Concentration in mg/mL at zero time. 95% CI.
†+1=24 hours at 32°C.
FLU, flucloxacillin.
The concentrations of flucloxacillin during storage at 2°C–8°C for 6 and 13 days followed by 24 hours at 32°C remained >95% (p=0.95) of the starting concentrations in all the solutions tested, with one exception. In the INfusor LV, at a concentration of 50 mg/mL, after 13 days plus 24 hours at 32°C, while containing 96.5% of the starting concentration of flucloxacillin, the mean intersample variation was 1.5%.
Discussion
Tests performed on unbuffered flucloxacillin reconstituted in WFI and 0.9% w/v saline showed significant loss of antibiotic confirming a very limited shelf-life. A precipitate was also observed after storage, probably indicating an insoluble degradation product. This is consistent with other published studies for flucloxacillin in ambulatory devices, for example, 6 days of storage at 4°C plus 24 hours at 37°C giving a reduction from 120 to 86.4 mg/mL (28% loss) when saline was used as diluent.4 In another study, solutions stored in elastomeric devices for 6 days at 2°C–8°C plus 24 hours at 31°C resulted in a loss of active pharmaceutical ingredient concentration from 50 to 46 mg/mL (8% loss) and then to 43.5 mg/mL (13% loss) if stored at 37°C for 7 hours, all with 0.9% w/v saline as diluent.5
All β-lactam antibiotics undergo degradation in aqueous solution; the primary mechanism is nucleophilic attack leading to opening of the lactam ring. Degradation is greatest at extremes in pH; therefore, a neutral pH buffer system should reduce degradation. The nucleophilicity of the buffer can also affect degradation rates. Like flucloxacillin, benzylpenicillin sodium degrades rapidly in saline, with losses of 5%–7% in 24 hours at 2°C–8°C. However, 28-day storage is possible using 0.3% w/v citrate-buffered saline at pH 5–7 with the same losses.10 In another study, phosphate buffer was demonstrated to improve the stability of ampicillin.11 The effectiveness of buffering β-lactam antibiotics has therefore been demonstrated.
In this study, flucloxacillin degradation following reconstitution and dilution was assessed using two buffers of different nucleophilicity over a range of pH. The optimum pH for maximising the stability of β-lactam antibiotics is approximately 6–7 and citrate, which is non-nucleophilic, can further limit degradation.
Preliminary studies were performed using an MCP buffer system to achieve buffering at pH values above 6. The test conditions of 37°C for 24 hours represented the worst case for a drug solution inside an ambulatory device reservoir.
In this study, we investigated both MCP and pure citrate buffers in terms of their ability to stabilise flucloxacillin in solution. Since phosphate is more nucleophilic it was anticipated that the attack of the β-lactam ring may lead to accelerated losses of flucloxacillin using this buffer. The results supported this hypothesis and indicated the use of a non-nucleophilic citrate buffer to provide the greater stabilising effect.
Results obtained for buffered flucloxacillin mirror those obtained for benzylpenicillin, where a low strength 0.3% w/v sodium citrate concentration caused the least degradation of flucloxacillin solutions over extended storage.10 Therefore, it was decided to adopt 0.3% w/v citrate-buffered saline pH 7 as the vehicle for reconstitution and dilution in the main study within the ambulatory devices.
Studies were conducted at 10 and 50 mg/mL representing the clinically relevant flucloxacillin concentration range with storage/administration conditions of up to 13 days of storage time plus 24 hours at 32°C. A commercially available 0.3% w/v citrate-buffered saline was used to prepare all flucloxacillin solutions stored in the two ambulatory device reservoirs (Accufuser and INfusor LV) under test.
Results from both devices show that flucloxacillin can be stored for up to 13 days at 2°C–8°C followed by 24 hours of infusion at 32°C when using a buffered citrate vehicle. This allows for adequate refrigerated storage times in the pharmacy and/or patient’s house before use.
We did not assess moisture loss from the elastomeric devices, as is usually done for drugs in intravenous bag container systems, as this would be have been impractical for these devices. The requirement of removing samples at several time points makes it difficult to accurately perform a mass balance and small losses may be achieved during sampling from the device. Therefore, we relied on manufacturers’ own data on the devices in the study regarding the physical integrity of the container systems used.
The availability of a 24-hour continuous flucloxacillin infusion has broad application with OPAT services while supporting antimicrobial stewardship. Commonly, within OPAT services in the UK, ceftriaxone, a third-generation cephalosporin, is administered in place of flucloxacillin to treat Gram-positive infections, due to its long half-life and once-daily dosing12; however, its Gram-negative activity is often not required. A 24-hour continuous infusion of flucloxacillin in an ambulatory device shares the benefits of once-daily dosing of ceftriaxone, while limiting the potential to cause antimicrobial resistance and healthcare-associated infection, such as Clostridium difficile.
The availability of validated stability data, which meets the standards required by the NHS Pharmaceutical Quality Assurance Committee (YCD),7 for extended infusions of buffered flucloxacillin in two commercially available portable ambulatory infusion devices, facilitates the use of such infusions within the wider OPAT community both within the UK and potentially internationally. Previously, the application and use of unbuffered flucloxacillin infusions in ambulatory devices has been limited by shelf-life.
Conclusions
This study shows that flucloxacillin 10–50 mg/mL is stable for up to 13 days at 2°C–8°C plus 24 hours at 32°C when reconstituted and diluted in a 0.3% w/v citrate-buffered saline diluent with storage in two ambulatory device reservoirs (Accufuser and INfusor LV) filled to a volume of 240 mL. For the first time, doctors, nurses and pharmacists, together with associated pharmacy production staff, can use flucloxacillin in ambulatory devices within the wider OPAT community. This development in OPAT drug stability provides the opportunity for more patients to be treated under an OPAT service where clinical experience and confidence with ceftriaxone is lacking (eg, sensitive staphylococcal endocarditis). In addition, in OPAT services where flucloxacillin is given by multiple daily dosing, the option to give it by continuous infusion will increase convenience for patients and increase capacity where nurse administration occurs.
Acknowledgments
The authors thank all members of the BSAC Drug Stability Working Party who contributed to the study and production of the manuscript. The BSAC Drug Stability Working Party comprises CJ (chair), Mark Gilchrist, TH, Mark Santillo, Andrew Seaton and representatives from the stability testing laboratory: MCA and ASW.
Footnotes
Contributors: ASW and CJ planned the study. DS and AW performed the study and collected the data. ASW, MCA and DS analysed the data and wrote the manuscript. CJ and TH, plus other members of the BSAC Drug Stability Working Party, critically reviewed the manuscript.
Funding: This study was commissioned and funded by the British Society for Antimicrobial Chemotherapy (BSAC) as part of their Drug Stability Testing programme in the UK to support Outpatient Parenteral Antimicrobial Therapy (OPAT) services.
Competing interests: None declared.
Patient consent: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: The outputs of the research are published open access in line with BSAC policy and will be freely disseminated, including being made available through the BSAC Drug Stability Testing programme website: www.bsac-dsp.com
Collaborators: The BSAC Drug Stability Working Party comprises Conor Jamieson (chair), Mark Gilchrist, Tim Hills, Mark Santillo, Andrew Seaton and representatives from the stability testing laboratory: Michael Allwood and Alan-Shaun Wilkinson.
Contributor Information
on behalf of the BSAC Drug Stability Working Party:
References
- 1. Public Health England, 2015. Start smart then focus – antimicrobial stewardship toolkit for english hospitals. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/417032/Start_Smart_Then_Focus_FINAL.PDF (accessed 14 May 2018).
- 2. Gilchrist M, Seaton RA. Outpatient parenteral antimicrobial therapy and antimicrobial stewardship: challenges and checklists. J Antimicrob Chemother 2015;70:965–70. 10.1093/jac/dku517 [DOI] [PubMed] [Google Scholar]
- 3. Jenkins A, Hills T, Santillo M, et al. Drug stability working group of the BSAC UK OPAT initiative. Extended stability of antimicrobial agents in administration devices. J Antimicrob Chemother 2017;72:1217–20. [DOI] [PubMed] [Google Scholar]
- 4. To TP, Ching M, et al. Stability of intravenous flucloxacillin solutions used for Hospital-in-the-Home. J Pharm Pract Res 2010;40:101–5. [Google Scholar]
- 5. Carroll JA. Stability of flucloxacillin in elastomeric infusion devices. J Pharm Pract 2005;35:90–3. 10.1002/j.2055-2335.2005.tb00313.x [DOI] [Google Scholar]
- 6. Ahmed ST, Parkinson R. The stability of drugs in pre-filled syringes: flucloxacillin, ampicillin, cefuroxime, cefotaxime and ceftazidime. Hosp Pharm Pract 1992;2:285–9. [Google Scholar]
- 7. NHS Pharmaceutical Quality Assurance Committee. A standard protocol for deriving and assessment of stability: part 1 - aseptic preparations (small molecules). edn 4, 2017. https://www.sps.nhs.uk/wp-content/uploads/2017/06/Stability-part-1-small-molecules-v4-April-17.pdf (accessed 01 Oct 17).
- 8. Voumard R, Van Neyghem N, Cochet C, et al. Antibiotic stability related to temperature variations in elastomeric pumps used for outpatient parenteral antimicrobial therapy (OPAT). J Antimicrob Chemother 2017;72:1462–5. 10.1093/jac/dkw582 [DOI] [PubMed] [Google Scholar]
- 9. British Pharmacopoeia Commission. British Pharmacopoeia 2017. London: TSO, 2017. [Google Scholar]
- 10. Allwood MC, Brown PW. The effect of buffering on the stability of reconstituted benzylpenicillin injection. Int J Pharm Pract 1992;1:242–4. 10.1111/j.2042-7174.1992.tb00580.x [DOI] [Google Scholar]
- 11. Allwood MC, Brown PW. Stability of ampicillin infusions in unbuffered and buffered saline. Int J Pharm 1993;97:219–22. 10.1016/0378-5173(93)90142-3 [DOI] [Google Scholar]
- 12. eMC, 2017. Summary of product characteristics for ceftriaxone. https://www.medicines.org.uk/emc/product/1361/smpc (accessed 24 Jan 18).