Abstract
Purpose
Pellucid marginal degeneration (PMD) is a rare disease that is often mistaken for keratoconus but can similarly be treated with corneal collagen crosslinking (CXL). We report a case followed though 6 years of progressive irregular corneal flattening and thinning in both eyes (OU) after eccentric CXL for PMD.
Observation
A 46-year-old man with bilateral PMD and corrected distance visual acuity (CDVA) of 20/20 (−2.00x80) in the right eye (OD) and 20/30 (+3.50–5.25x105) in the left eye (OS) underwent conventional 9 mm eccentric CXL in OU and intrastromal corneal ring implantation in the OS. An uneventful first year postoperative follow-up showed stabilization of the ectasia. In subsequent years, progressive inferior flattening was observed with decreased CDVA, corneal thinning and worsening of the haze. At the last follow-up, his CDVA was 20/40 (+5.00–2.00x55) OD and 20/60 (+6.00–1.50x80) OS.
Conclusion and Importance
The current report highlights the notion that mid- and long-term evaluations of customized crosslinking techniques may reveal progressive flattening and corneal irregularity.
Keywords: Corneal crosslinking, Pellucid marginal degeneration, Ectasia, Progressive flattening
1. Introduction
Pellucid marginal degeneration (PMD) is a rare, bilateral, asymmetric, ectatic disorder of the cornea that is characterized by an arcuate band of thinning in the inferior peripheral cornea with maximal protrusion superior to the thinned area.1 Differentiation between PMD and keratoconus is sometimes difficult because of their similar clinical and topographic presentations.1,2 Topography shows a flat vertical meridian with inferior peripheral steepening with a classical “crab-claw” shape; however, a similar shape can also be seen in keratoconus.3,4 Corneal topography, pachymetry mapping, elevation mapping, and, most importantly, slit-lamp examination are recommended for diagnosis and differentiation from keratoconus.5, 6, 7, 8
Treatment of this condition includes spectacles, contact lens, intrastromal corneal ring segments (ICRS), excimer laser and corneal transplantation.7,9 In addition, PMD tends to evolve even in older patients, and corneal collagen crosslinking (CXL) has therefore been used to stabilize it, similar to keratoconus. Despite good initial results, due to its rarity, only a few reports have evaluated the use of CXL in PMD9, 10, 11; hence, the safety, efficacy and complications of this treatment are not fully understood. We report a case of progressive irregular flattening and thinning in both eyes (OU) after CXL in a patient with PMD.
1.1. Case report
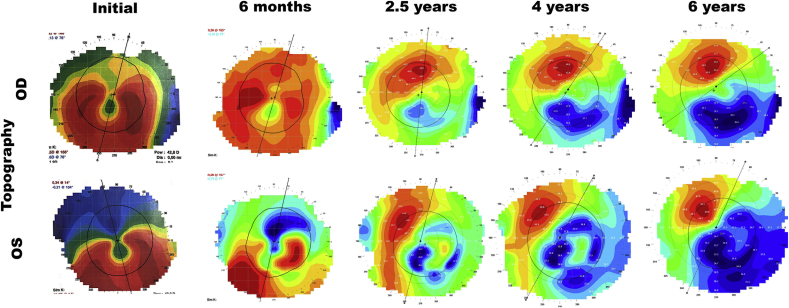
A 46-year-old man presented with progressive decreased visual acuity and an increase in his astigmatic prescription. Corrected distance visual acuity (CDVA) was 20/20 (−2.00x80) in the right eye (OD) and 20/30 (+3.50–5.25x105) in the left eye (OS). In a slit-lamp examination, he presented an evident band of inferior thinning with adjacent superior protrusion, and the rest of his examination was unremarkable. His topography (E300 Corneal Topographer, Medmont International PTY LTD, Australia) showed classical PMD findings (Fig. 1).
Fig. 1.
Topographic (E300 Corneal Topographer, Medmont International PTY LTD, Australia) evolution of both eyes over the years.
Since he was intolerant to contact lenses and wanted to improve his CDVA in the OS, CXL was proposed in the OU and ICRS in the OS.
The procedure began with the implantation of the ICRS under topical anesthesia. The implantation axis was marked under a slip-lamp with the patient in the supine position, and ultrasonic pachymetry was used intraoperatively. A micrometer diamond keratome was used to perform an 80% depth incision, and a 5 mm, 160-degree ICRS with a thickness of 200 μm (Keraring, Mediphacos, Belo Horizonte, Brazil) was implanted at 115°.
Subsequently, conventional CXL was performed with mechanical epithelium removal. Iso-osmolar Riboflavin (0.1%) with 20% dextran was applied every two minutes for 30 minutes, and then ultraviolet-A at 365 nm was applied continually for 30 minutes at 3 mW/cm2 (CBM X-Linker, CSO, Italy). A 9-mm UVA spot was used and decentered inferiorly to reach the peripheral area of the thinning but without crossing the limbus. The procedure occurred uneventful. A bandage soft contact lens was placed for one week. Postoperative medication included moxifloxacin (0.5%, Vigamox, Alcon, São Paulo, Brazil) four times daily for one week and prednisolone (1%, Pred Fort, Allergan, Sao Paulo, Brazil) four times daily for one month.
At 6 months after the procedure, the patient was satisfied, PMD was stabilized, and CDVA was 20/20 (−1.00x80) OD and 20/30 (+3.00–3.500x85) OS. A slit lamp examination revealed faint intrastromal haze in the OU.
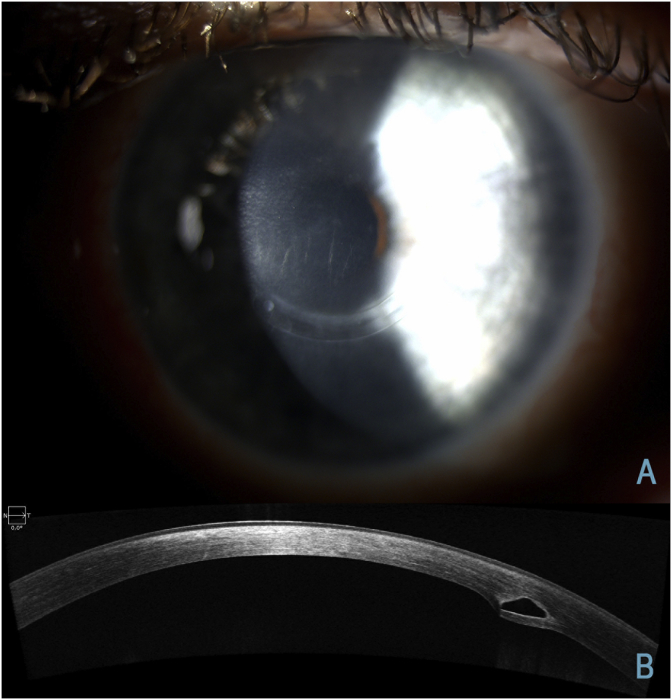
After 1 year, the patient returned and complained of progressive decreased visual acuity. CDVA was 20/30 (−1.00x70) OD and 20/40 (+1.50–2.00x30) OS, and haze was graded as 1+ OU (Fig. 2).
Fig. 2.
(A) Biomicroscopy of the left eye showing central stromal corneal haze and inferior ICRS. (B) Corneal image with optical coherence tomography (AS-OCT, Cirrus HD-OCT Model 5000, Carl Zeiss Meditec Inc., Dublin, CA, USA) of the left eye performed at the 6-year follow-up showing corneal haze and adequate ICRS placement.
After 3 years, CDVA decreased to 20/40 (+0.25–1.00x70) OD and 20/60 (+2.50–2.50x30) OS, and visible thinning and flattening was observed in the inferior cornea.
At 5 years after the procedure, CDVA was stable, but the cornea showed progressive flattening (Fig. 1)-induced hyperopia OU (+2.25–1.50x60 OD and +4.25–2.50x60 OS).
His last visit was at 6 years after the procedure, when he showed stable CDVA but worsening hyperopia (+5.00–2.00x55 OD and +6.00–1.50x80 OS) with flattening and thinning (Fig. 1). He fitted rigid contact lenses in OU ((ROSE K2 Irregular Cornea IC; Menicon Co. Ltd., Nagoya, Japan), achieving a CDVA of 20/25 in OD and 20/50 in OS.
Table 1 summarizes the evolution of both eyes over the years.
Table 1.
Evolution of topographic and refractive data of both eyes though the years.
| Initial | 6 months | 1 year | 2.5 years | 4 years | 6 years | ||
|---|---|---|---|---|---|---|---|
| Refraction | OD | −2.00x80 | −1.00x80 | −1.00x70 | +0.25–1.00x70 | +2.25–1.50x60 | +5.00–2.00x55 |
| OS | +3.50–5.25x107 | +3.00–3.500x85 | +1.50–2.00x30 | +2.50–2.50x30 | +4.25–2.50x60 | +6.00–1.50x80 | |
| CDVA | OD | 20/20 | 20/20 | 20/30 | 20/40 | 20/40 | 20/40 |
| OS | 20/30 | 20/30 | 20/40 | 20/60 | 20/60 | 20/60 | |
| Flat K | OD | 42.6@76 | 42.5@73 | 41.5@70 | 40.8@56 | 40.5@36 | |
| OS | 40.8@104 | 39.9@77 | 37.7@70 | 37.2@61 | 38.5@66 | ||
| Steep K | OD | 44.5@166 | 44.1@163 | 43.6@160 | 43.0@146 | 42.5@126 | |
| OS | 46.6@14 | 44.8@167 | 43.1@160 | 42.9@151 | 43.5@156 | ||
| Topographic Astigmatism | OD | 1.9 | 1.6 | 2.1 | 2.2 | 2.0 | |
| OS | 5.8 | 4.9 | 5.4 | 5.5 | 5.0 | ||
| K Maximum | OD | 44.3 | 44.00 | 44.73 | 45.98 | 46.50 | |
| OS | 47.4 | 45.90 | 44.83 | 46.12 | 49.69 | ||
| I-S Asymmetry | OD | 0.6 | −2.0 | −5.4 | −7.6 | −10.0 | |
| OS | 5.9 | 4.1 | −4.6 | −8.1 | −13.7 |
CDVA – Corrected Distance Visual Acuity; I-S Asymmetry: Inferior-Superior Asymmetry – Difference between the keratometry of the superior and inferior from 1.5mm from the center.
2. Discussion
We report a well-documented case of irregular progressive corneal flattening and visual loss with haze formation after eccentric conventional CXL for PMD with long-term follow-up. Corneal flattening is common after CXL for keratoconus, with a mean flattening of 1.6 D observed after one year and up to 3 D observed after 5 years12, 13, 14; however, only a few cases of excessive flattening after CXL have been reported. Kymionis et al.15 was the first to report it in one eye of a keratoconus patient who underwent CXL in OU according to the Dresden protocol and had a 5-year follow-up with documented haze on AS-OCT. Koller et al.14 observed flattening in 38% of 151 keratoconus eyes after one year of follow-up, with a maximum flattening of 7.2D observed in one case; furthermore, these authors found that a kmax of 54 D or higher was a risk factor for excessive flattening.14 Santhiago et al.16 also reported two cases of progressive flattening after conventional CXL, both with a kmax of 64 D. In our case, the patient had a kmax of 44.3 D OD and 47.4 D OS. More recently, a long-term study of 433 progressive keratoconus eyes treated with classical CXL protocol revealed 3 cases of progressive flattening that were not associated with intense haze or loss of CDVA.17
Theoretically, the stiffening associated with CXL reduces central cornea strain and shifts the focus of maximum strain toward the limbus, enabling central cornea flattening and hyperopic optical shift.18 In our case, an eccentric CXL was performed, and this may have been the cause of unbalanced forces and excessive flattening. The resultant hyperopic shift and decrease of 3 lines of CDVA may be explained by significant excessive inferior flattening and corneal irregularities (I-S asymmetry shifted from inferior steepening to superior steepening) associated with central stromal haze, leading to high order aberration. This can be addressed with rigid contact lens which compensates the corneal irregularities, improving CDVA, as did in this reported case.
Despite this unfortunate case, eccentric CXL has been successfully used in PMD. Bayraktar et al.10 reported 4 eyes with PMD in which conventional eccentric CXL was performed and achieved good stability after 12 months. Bashir et al.11 described 15 patients with PMD who underwent CXL with good results over a short follow-up period (6 months); however, without topographic documentation and incomplete CXL technique information.
3. Conclusion
The current report highlights the importance of mid- and long-term evaluation of customized crosslinking techniques and stresses the risks associated with long-term corneal remodeling, which can lead to progressive flattening and corneal irregularity.
3.1. Patient consent
The consent is attached to the submission. It consists of the surgical consent form which has the following information on page 2 (translated to English): “I authorize, in case feasible, the recording of imagens or photographs of before, during and after the surgery, specifically for teaching or scientific research purposes.”
Also, on page 6 there is another authorization (translated to English): “I authorize the above-described surgery to be performed by signing this agreement, in addition to allowing it to be filmed and/or photographed and I agree that the data obtained from my examination may be used for scientific or teaching purposes.”
Funding
No funding or grant support.
Authorship
All authors attest that they meet the current ICMJE criteria for Authorship.
Declaration of competing interest
The following authors have no financial disclosures: GAF, VCG and RCG.
Acknowledgements
None.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ajoc.2020.100621.
Appendix A. Supplementary data
The following is/are the supplementary data to this article:
References
- 1.Krachmer J.H., Feder R.S., Belin M.W. Keratoconus and related noninflammatory corneal thinning disorders. Surv Ophthalmol. 1984;28(4):293–322. doi: 10.1016/0039-6257(84)90094-8. [DOI] [PubMed] [Google Scholar]
- 2.Belin M.W., Asota I.M., Ambrosio R., Jr., Khachikian S.S. What's in a name: keratoconus, pellucid marginal degeneration, and related thinning disorders. Am J Ophthalmol. 2011;152(2):157–162 e1. doi: 10.1016/j.ajo.2011.03.028. [DOI] [PubMed] [Google Scholar]
- 3.Maguire L.J., Klyce S.D., McDonald M.B., Kaufman H.E. Corneal topography of pellucid marginal degeneration. Ophthalmology. 1987;94(5):519–524. doi: 10.1016/s0161-6420(87)33416-5. [DOI] [PubMed] [Google Scholar]
- 4.Lee B.W., Jurkunas U.V., Harissi-Dagher M., Poothullil A.M., Tobaigy F.M., Azar D.T. Ectatic disorders associated with a claw-shaped pattern on corneal topography. Am J Ophthalmol. 2007;144(1):154–156. doi: 10.1016/j.ajo.2007.02.032. [DOI] [PubMed] [Google Scholar]
- 5.Panos G.D., Hafezi F., Gatzioufas Z. Pellucid marginal degeneration and keratoconus; differential diagnosis by corneal topography. J Cataract Refract Surg. 2013;39(6):968. doi: 10.1016/j.jcrs.2013.04.020. [DOI] [PubMed] [Google Scholar]
- 6.Walker R.N., Khachikian S.S., Belin M.W. Scheimpflug photographic diagnosis of pellucid marginal degeneration. Cornea. 2008;27(8):963–966. doi: 10.1097/ICO.0b013e318170ae98. [DOI] [PubMed] [Google Scholar]
- 7.Moshirfar M., Edmonds J.N., Behunin N.L., Christiansen S.M. Current options in the management of pellucid marginal degeneration. J Refract Surg. 2014;30(7):474–485. doi: 10.3928/1081597X-20140429-02. [DOI] [PubMed] [Google Scholar]
- 8.Sridhar M.S., Mahesh S., Bansal A.K., Nutheti R., Rao G.N. Pellucid marginal corneal degeneration. Ophthalmology. 2004;111(6):1102–1107. doi: 10.1016/j.ophtha.2003.09.035. [DOI] [PubMed] [Google Scholar]
- 9.Kymionis G.D., Grentzelos M.A., Plaka A.D. Simultaneous conventional photorefractive keratectomy and corneal collagen cross-linking for pellucid marginal corneal degeneration. J Refract Surg. 2014;30(4):272–276. doi: 10.3928/1081597X-20140320-06. [DOI] [PubMed] [Google Scholar]
- 10.Bayraktar S., Cebeci Z., Oray M., Alparslan N. Corneal collagen cross-linking in pellucid marginal degeneration: 2 patients, 4 eyes. Case Rep Ophthalmol Med. 2015;2015 doi: 10.1155/2015/840687. 840687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mamoosa B., Razmjoo H., Peyman A., Ashtari A., Ghafouri I., Moghaddam A.G. Short-term result of collagen crosslinking in pellucid marginal degeneration. Adv Biomed Res. 2016;5:194. doi: 10.4103/2277-9175.192732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hersh P.S., Stulting R.D., Muller D., Durrie D.S., Rajpal R.K., United States Crosslinking Study G. United States multicenter clinical trial of corneal collagen crosslinking for keratoconus treatment. Ophthalmology. 2017;124(9):1259–1270. doi: 10.1016/j.ophtha.2017.03.052. [DOI] [PubMed] [Google Scholar]
- 13.Kymionis G.D., Grentzelos M.A., Liakopoulos D.A. Long-term follow-up of corneal collagen cross-linking for keratoconus--the Cretan study. Cornea. 2014;33(10):1071–1079. doi: 10.1097/ICO.0000000000000248. [DOI] [PubMed] [Google Scholar]
- 14.Koller T., Pajic B., Vinciguerra P., Seiler T. Flattening of the cornea after collagen crosslinking for keratoconus. J Cataract Refract Surg. 2011;37(8):1488–1492. doi: 10.1016/j.jcrs.2011.03.041. [DOI] [PubMed] [Google Scholar]
- 15.Kymionis G.D., Tsoulnaras K.I., Liakopoulos D.A., Paraskevopoulos T.A., Kouroupaki A.I., Tsilimbaris M.K. Excessive corneal flattening and thinning after corneal cross-linking: single-case report with 5-year follow-up. Cornea. 2015;34(6):704–706. doi: 10.1097/ICO.0000000000000424. [DOI] [PubMed] [Google Scholar]
- 16.Santhiago M.R., Giacomin N.T., Medeiros C.S., Smadja D., Bechara S.J. Intense early flattening after corneal collagen cross-linking. J Refract Surg. 2015;31(6):419–422. doi: 10.3928/1081597X-20150521-09. [DOI] [PubMed] [Google Scholar]
- 17.Noor I.H., Seiler T.G., Noor K., Seiler T. Continued long-term flattening after corneal cross-linking for keratoconus. J Refract Surg. 2018;34(8):567–570. doi: 10.3928/1081597X-20180607-01. [DOI] [PubMed] [Google Scholar]
- 18.Sinha Roy A., Dupps W.J., Jr. Effects of altered corneal stiffness on native and postoperative LASIK corneal biomechanical behavior: a whole-eye finite element analysis. J Refract Surg. 2009;25(10):875–887. doi: 10.3928/1081597X-20090917-09. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.