Abstract
Introduction: Clinical hypnosis for pain management cultivates specific skills to enhance general self-regulation and address pain. Hypnosis is well suited to integrative medicine settings; however, questions persist about its feasibility. This article describes a financially viable hypnosis practice model implemented in an integrative medicine clinic, providing initial feasibility data about rates of referral, participation, reimbursement, and provider retention. The specific processes required to establish and implement hypnosis services were detailed, including instruction in billing, reimbursement data, and a training model to enhance reach of services.
Materials and methods: Insurer reimbursement data and operational costs were examined from three hypnosis groups conducted between September 2017 and March 2018. Furthermore, information on referral patterns and enrollment in treatment was collected from program initiation in September 2017 to January 2019. Provider retention in training with the expansion of supervision in the program's second year was also examined.
Results: Of 258 individuals referred to hypnosis, 124 (48%) enrolled in group treatment. Analysis of insurer reimbursement over a subset of enrollees from three completed groups (N = 26) indicated an average collection of $95.85 per patient per session, equating to $706.86 per patient for the eight-session treatment. This extrapolates to $4,926.82 in total per seven-person group for the entirety of the eight-session treatment. After an annual training workshop, provider retention significantly increased (to 81% of eligible trained providers) with the initiation of twice-monthly clinical supervision focusing on transitioning from training to practice.
Conclusion: This analysis indicates that a training- and practice-based research model of clinical hypnosis is feasible and financially sustainable in an integrative medicine setting.
Keywords: hypnosis, hypnotherapy, pain, chronic, integrative medicine, self-management
Introduction
Integrative health (IH) clinics serve patients referred from a variety of clinical settings, including orthopedic, spinal, oncology, rehabilitation, gastrointestinal, cardiovascular, and neurology.1,2 IH clinics primarily manage musculoskeletal and neuropathic pain-related conditions, through engagement in interventions intended to complement conventional medicine3 and promote positive health behaviors that foster agency and holistic wellness.3–5 Clinical hypnosis is a complementary psychosocial treatment that cultivates specific skills to enhance self-regulation, including the management of physical symptoms such as pain. Although similar to mindfulness meditation in its emphasis on focus and attention, clinical hypnosis differs in its direction and quality of the focus.6 Specifically, clinical hypnosis trains participants to manipulate focus in the service of pain reduction and self-regulation through the application of suggestions for changes in experience, cognition, thought, and behavior.7 For further discussion detailing similarities and differences between the constructs, see Yapko.6 The general aims of clinical hypnosis align well with both the needs of the population served through IH and the core principles of integrative care.
Overwhelming evidence supports the use of clinical hypnosis for chronic pain and its effects on well-being.8 Systematic reviews indicate hypnosis is a safe effective technique for pain relief,9 which can be applied to chronic pain management, medical procedures,10 and target symptoms from conditions such as irritable bowel syndrome10 and fibromyalgia.11 Moreover, the benefits of hypnosis extend to improved affect, relaxation, sleep quality, and increased energy, even when patients do not report pain relief as a result of treatment.12,13
IH environments are well suited to hypnosis training and practice, where evidence-based techniques are applied to myriad conditions to reduce suffering and improve patients' quality of life. Recognizing its benefits in managing pain, in 2017 the Veterans Health Administration (VHA) in the United States released a directive (VHA Directive 1137) mandating access to hypnosis and seven other IH services for veterans.
Despite applicability to IH, lack of awareness, education, and availability of trained providers currently limits patient access to clinical hypnosis. Although IH environments may welcome the service and as systems like the VHA mandate access, there is a risk that the limited number of trained providers of hypnosis could not meet a growing need. Hypnosis is not currently taught in recent cohorts of graduate psychology programs, medical schools, or nursing schools. In addition, limited provider awareness coupled with misconceptions about hypnosis can interfere with referral processes and accurate patient education on its potential use.14–17
Notably, between 70% and 90% of patients approached report a willingness to use hypnosis adjunctively to support medical treatment.18,19 Yet, some patients express reluctance to use hypnosis for fear of losing control and other unwarranted concerns.20 Education and training can improve provider attitudes toward hypnosis, patient engagement, and reduce concerns to patients that are often based on myths and misconceptions.19,21,22 Additional hurdles to IH implementation surround the perceived cost of the service.23,24
Hypnosis can be integrated into health care systems more widely by addressing access and education barriers while illuminating service reimbursement structures. Inspired to overcome these barriers, we developed a financially viable hypnosis practice model implemented in a tertiary clinic of an academic medical center that fluidly (1) cares for patients, (2) trains clinicians, and (3) gathers practice-based data for contributions to the literature. We reviewed our practice-based research model, providing practical guidance on the referral process and billing practices, and feasibility and retention rates were included. Furthermore, the program's financial viability was demonstrated with a preliminary analysis of claims processed for those who engaged in treatment, accounting for clinic operational costs. It is hoped this information can empower others to replicate this model in practice.
Materials and Methods
Establishing program infrastructure
A number of steps were made to establish and implement a clinical hypnosis program in a tertiary IH clinic at a major academic medical center. The program employed hypnosis for chronic pain and other medical concerns, including acute and chronic complaints. Implementation included educating providers, building an infrastructure for referrals, establishing clinical services, and training clinicians. Notably, this program was designed to collect empirical data at its outset, embedding research into clinical procedures.
Provider education
It was found that educating potential referring providers on the intervention and who it will best serve helps with beginning a referral stream. For clinical hypnosis, it was found important to dispel myths (i.e., correct misinformation), define hypnosis, and review empirical evidence. Taking such steps gives providers “language” to use with patients around hypnosis and hopefully increases their confidence in the intervention,22 which likely translates to increased patient interest in referrals for services.16
Referral and screening system
Immediately after provider education, a process was established by which providers internally referred patients to hypnosis when creating treatment plans. Consistent with a whole person care model for chronic pain,5 IH providers referred patients to clinical hypnosis as one of a series of multidisciplinary services coordinated to meet patient goals and needs. For each patient referred, a referral form (Supplementary Appendix S1) was created asking providers to indicate the primary medical diagnosis, review any exclusionary criteria to screen out individuals who may not benefit from hypnosis, and assess patient interest in research activities. Any external referrals occurred exclusively through some few IH providers who also worked at another site in the hospital system and applied the same referral criteria. A brief flyer (Supplementary Appendix S2) was also created for referral sources to give to patients about the intervention. Staff then contacted patients to schedule into a group or individual appointment, depending on the referral issue and patient scheduling availability.
Clinical services offered
Hypnosis group intervention
The clinical hypnosis intervention consists of an 8-week manualized protocol (unpublished manual*) that addressed chronic pain and trained patients in self-hypnosis. The structured group sessions follow the format of (1) psychoeducation, (2) reviewing previous material and home practice, (3) a hypnosis induction with varying suggestions, and (4) group process of experiences, problem solving, and recommendations for home practice. Participants are given workbooks to follow through the intervention each week. Group size typically ranged from 7 to 15 participants. Sessions occur for 90 min, allowing for time for patients to get settled and take a short break as needed.
During the intervention, participants underwent a hypnosis induction with different suggestions targeting pain relief, comfort, and relaxation (unpublished manual). Participants access prerecorded inductions coinciding with each week's exercise and were encouraged to practice self-hypnosis between appointments. Two providers cofacilitated groups, allowing participants to experience different voices during inductions and enhanced group discussions. It was found that including a nonbilling trainee (i.e., provider-in-training) as a cofacilitator with a billing provider has worked well.
Individual appointments
The mentioned group protocol easily adapted to individual sessions, which followed the same session structure. Hypnosis was offered individually in cases where participants could not attend group appointments. This barrier often arises due to logistical constraints (work, schedule, etc.) or the clinical issue at hand. For example, some participants with specific types of pain, such as vulvodynia, expressed hesitancy in discussing their experiences in a mixed group. This scenario also occurred in situations with pain related to a traumatic experience, which in practice is more appropriate for an individual appointment as additional precautions needed to be taken in addressing pain in the context of post-traumatic stress disorder.25 Individual sessions were conducted by trainees and were thus free to patients.
Additional individual applications
Although the standardized hypnosis protocol already described (unpublished manual) was appropriate for the vast majority of patients with chronic pain referred for hypnosis, some clinical circumstances required a different approach and timeframe. For example, individual hypnosis could support procedural interventions and other “acute” medical issues such as labor and delivery.8,26 Such cases often require under four sessions. Conversely, patients with extensive psychological trauma or affective vulnerability seemed to benefit from a titrated, highly supportive, and more slowly paced intervention extending beyond eight sessions.
Provider qualifications for conducting hypnosis
Eligible providers for hypnosis training and supervision included those performing clinical services at all levels of training, such as psychologists, medical doctors, nurse practitioners, and social workers. Familiarity with the treatment protocol was required. To perform the group intervention, within this clinic specifically,practicing providers are required to attend an annual 2-day 14-h workshop on hypnosis and enroll in monthly supervision for 1 year. Similar basic requirements are outlined in the manualized protocol (unpublished manual, pp. 3–4). In terms of billing, insurers only reimburse licensed psychologists under the codes that were applied and detailed hereunder. Centers of Medicaid and Medicare Services (CMS) billing guidelines indicate that a medical professional defers to more appropriate evaluation and management codes for medical group visits. The data provided hereunder are restricted to services billed by clinical psychologists.
Results of Program Performance
Billing practices
In detailing financial performance of the service, it is key to first detail billing practices for the service. Services performed by psychologists billed for hypnosis fall under “Health and Behavior Group Intervention” in CMS Current Procedural Terminology (CPT) code 96153 (4–6 units). This specific code bills in units of 15 min, generally for between 60 and 90 min for a group appointment. Health and Behavior codes apply to services that address factors affecting the recovery of progression of a diagnosed physical health problem or illness, such as chronic pain. Therefore, this set of codes (CPT codes 96150-4) bill physical health conditions diagnosed by a medical provider (e.g., M54.5 Low Back Pain) as the primary diagnosis for services using International Statistical Classification of Diseases and Related Health Problems codes, as opposed to Diagnostic and Statistical Manual of Mental Disorders codes traditionally billed in psychologic contexts.
According to the American Psychological Association,27 services under Health and Behavior codes promote physical function, address psychologic barriers to recovery, and manage and enhance coping with medical conditions. Hypnosis in IH teaches a specific skill to manage a physical health problem, and not a “mental health problem” per se. As such, services were performed by clinical psychologists and billed under this code (CPT-96153).
Financial analysis
To conduct a cost analysis including operations and payor reimbursement, both the final billing ledger and insurer collections information were examined. To have reliable collections information, only groups that ended with ample intervening time for payments to be fulfilled up to the analysis were selected. Thus, three groups were selected spanning from September 2017 to March 2018 who completed all eight sessions of the protocol.
For accuracy, the overhead costs of implementing these groups within the clinical operations were examined. All of these costs were relatively independent of the number of patients attending a given session. For space, room costs were $22.50 per session or $180 for all eight sessions. Support staff costs were $36 per session or $288 for all sessions, accounting for check-in procedures, scheduling, and patient calls. Provider time was $58 per session or $464 for all eight sessions. Overall, total overhead costs for the eight-session protocol were $932. There were 26 patients enrolled for the three groups (two of nine and one of eight). Average attendance per session across the eight group sessions was stable, mean (standard deviation) = 6.97 (1.69). Average charges per group session were $2,950 per group, or $441.92 per patient. To extrapolate, average charges for the entire eight-session protocol were $22,766.67 per group or $3,266.28 per patient. Average collections per session were $635.91 per group or $95.85 per patient. Accordingly, collections for the whole protocol were $4,926.82 per group or $706.86 per patient. Taken together, the group model covered the cost of provider time, along with the space and resources used, and still provided profit for the clinic. For illustration, a two-patient group would cover all overhead costs involved.
The insurance coverage of these 26 patients was examined to contextualize approved billings. All patients had active health insurance, with 57.59% (n = 15) covered by governmental and 42.31% (n = 11) by commercial insurance. The authors did not have data on out-of-pocket costs for patients.
Feasibility and retention
Figure 1 shows feasibility and retention of the hypnosis group treatment model. These data spanned nine group cohorts and ∼19 months (June 2017–January 2019). A total of 258 referrals were received, 48% of whom (N = 124) enrolled into the treatment protocol. Most of those enrolled in the treatment protocol also consented to participate in a research study: 24% did not (n = 30). Of those enrolled in the protocol and agreed to research (n = 94), 70% completed both the treatment (attended at least four sessions) and the research questionnaires. The authors do not have data to situate this referral rate in comparison with other settings, though it was sufficient to regularly hold groups.
FIG. 1.
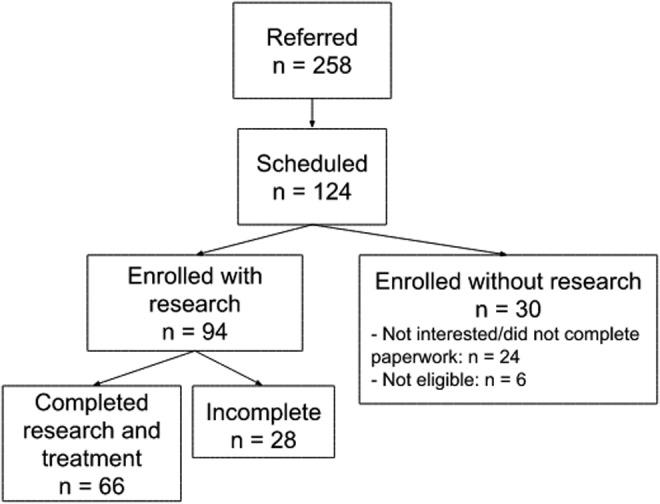
Clinical hypnosis program referral flow.
Hypnosis Training to Expand Clinical Services
Initial training in hypnosis
To learn the provision of hypnosis, the center recruited interested providers and providers-in-training to an annual workshop consisting of 14 h of basic instruction in hypnosis, providing continuing medical education credits for psychologists, medical providers, dentists, and nurse practitioners. Two clinical psychologists with extensive training and clinical experience using hypnosis have led this workshop. Topics covered include basic education on hypnosis, hypnotic analgesia, ethical practice, formulating inductions and suggestions, specific hypnotic inductions for pain, and tailoring inductions and suggestions to different clinical issues. The workshop contained a large experiential component with practice in dyads and groups. Similar introductory workshops are offered regularly through The American Society of Clinical Hypnosis and Society for Clinical and Experimental Hypnosis.
Supervision and continuing education
At the conclusion of the intensive training, the importance of ongoing supervision to both develop competency and transition to practice was emphasized. Trainees then registered for (at least) one of two monthly supervision groups led by a clinical psychologist conducted in the late afternoons on alternate days, to accommodate those in full-time practice. For internal trainees eligible to see patients on-site, the opportunity to colead groups and see individual patients was given through staffing cases at these ongoing supervisions. Training covered a standardized pain protocol, individualized interventions, and provider-specific needs. Thus, individual goals were established in group supervision for applying the manualized protocol and the provision of hypnosis within one's specialty or scope of practice. For example, one provider in group learned to apply hypnosis before pediatric stem cell transplants, whereas another used hypnosis for college-age adults with somatic complaints, and another specifically for irritable bowel disease. Each provider required regular supervision in foundational principles of hypnosis, and instruction on various inductions and suggestions for specific populations evolved throughout the year to support individual-level needs.
Ongoing supervision followed three general phases. First, supervision focused on reviewing inductions, the treatment process, and overcoming barriers to practice. Supervision sought to enhance provider confidence in transitioning between structured scripted interventions to using hypnosis spontaneously and creatively applying clinical and intervention principles. Second, trainees were assigned new cases, and the group collaborated on generating suggestions based on new case material and establishing treatment plans for different types of patients. Trainees followed these cases throughout the year and reviewed cases at each supervision session. Last, and as comfort increased with conducting hypnosis, trainees learned more advanced techniques, inductions, supportive versus expressive approaches to hypnosis,28,29 and began experimenting with new techniques.
In each of the 2 years of the program, feedback from trainees was elicited and the structure and content of supervision were adjusted accordingly. For example, a consistent point of feedback from providers highlighted the helpfulness of initially working from structured scripts and transitioning (through being gently “pushed in supervision”) to practice unscripted hypnosis through general principles guided by clinical judgment over time. In its first year, monthly supervision was offered, and trainees indicated a desire for increased supervision offerings.
With the integration of twice-monthly supervision immediately after the training workshop, provider retention and transition to practice increased from 53% in 2017 to 81% in 2018, where 13 of 16 eligible workshop attendees ultimately incorporated hypnosis into their respective clinical services under supervision. This group of 13 included 5 trainees at masters, doctoral, or postdoctoral levels. The remaining eight were licensed providers from various disciplines, including psychology, psychiatry, nursing, gastroenterology, and Traditional Chinese Medicine. The authors do not have data on how many providers heard of the workshop by year nor the effects of any marketing strategies. Although it seemed that the integration of supervision immediately after the workshop and increased sessions may have improved retention to clinical practice, the change from 2017 to 2018 should be interpreted with caution.
Although the service was financially viable, a benefit of engaging providers-in-training in the provision of hypnosis has allowed the uninsured (or underinsured) patient access to hypnosis services at no cost. Doing so disseminated the service across the community,21 while enabling assessment of outcomes across a diverse sample of participants.
Discussion and Conclusion
Clinical hypnosis has been feasible in an IH setting and of likely benefit to the patient population. Ultimately, for health care providers and organizations to increase support for hypnosis, widening its evidence base is key, including demonstration of financial viability and implementation.21 This preliminary analysis suggests hypnosis as financially viable. Providers trained in hypnosis at the institution and around the community were retained through ongoing supervision, which helped with their transition to independent practice and to expand the reach of services.
In comparison with mindfulness-based stress reduction (MBSR), an advantage of clinical hypnosis for chronic pain lies in its relative brevity, lending it more likely to be reimbursed by insurance carriers as a medical service. However, insurance billing was rated the least important source of revenue across 24 medical programs with an integrated mindfulness intervention.30 Traditional MBSR includes 8 weeks of classes that last between 2 and 2.5 h each and a day-long (>6 h) silent retreat.31 Services often follow fee-based schedules, offered by trained facilitators from a variety of disciplines.32 Even though MBSR may meet billing criteria under certain group intervention codes (e.g., CPT codes 90853, 96153), reimbursement varies by system and payor, and common restrictions on the billable duration may prevent full reimbursement for services rendered.
Lastly, an embedded research process into clinical procedures showed that patients were willing to complete research procedures with treatment. Although regular clinical practice usually cannot support randomized trials, one can answer important questions by collecting basic data on clinical programs, patient-level data, utilization, and by assessing change over time in well-conceptualized single case studies. This builds evidence for the feasibility and effectiveness of hypnosis in real-world settings across diverse clinical contexts.33
Supplementary Material
Author Disclosure Statement
Two of the authors of this paper (MPJ and DRP) have published books on the topic of this paper, and receive royalties from the sale of those books.
Funding Information
The project was partially supported by CTSA No. UL1 TR002243 from the National Center for Advancing Translational Sciences. Its contents are solely the responsibility of the authors and do not necessarily represent official views of NCATS or the National Institute of Health.
Supplementary Material
Jensen MP. Self-Hypnosis for Chronic Pain: Treatment Manual, Vol 4.02016 (unpublished treatment manual shared by Dr. Mark Jensen, its creator. Manual was developed as a part of an NIH-funded investigation).
References
- 1. Griffin KH, Nate KC, Rivard RL, et al. Referrals to integrative medicine in a tertiary hospital: Findings from electronic health record data and qualitative interviews. BMJ Open 2016;6:e012006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Rhee TG, Leininger BD, Ghildayal N, et al. Complementary and integrative healthcare for patients with mechanical low back pain in a US hospital setting. Complement Ther Med 2016;24:7–12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Horrigan B, Lewis S, Abrams DI, Pechura C. Integrative medicine in America—How integrative medicine is being practiced in clinical centers across the United States. Global Adv Health Med 2012;1:18–94 [Google Scholar]
- 4. Eisenberg DM, Kaptchuk T, Post DE, et al. Establishing an integrative medicine program within an academic health center: Essential considerations. Acad Med 2016;91:1223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Hansen KA, McKernan LC, Carter SD, et al. A replicable and sustainable whole person care model for chronic pain. J Altern Complement Med 2019;25(Suppl. 1):S86–S94 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Yapko MD. Mindfulness and Hypnosis: The Power of Suggestion to Transform Experience. New York: Norton, 2011. [Google Scholar]
- 7. Kihlstrom JF. Hypnosis. Annu Rev Psychol 1985;36 385–418 [DOI] [PubMed] [Google Scholar]
- 8. Patterson DR. Clinical Hypnosis for Pain Control. Washington, D.C.: American Psychological Association, 2010 [Google Scholar]
- 9. Thompson T, Terhune DB, Oram C, et al. The effectiveness of hypnosis for pain relief: A systematic review and meta-analysis of 85 controlled experimental trials. Neurosci Biobehav Rev 2019;99:298–310 [DOI] [PubMed] [Google Scholar]
- 10. Häuser W, Hagl M, Schmierer A, Hansen E. The efficacy, safety and applications of medical hypnosis. Dtsch Arztebl Int 2016;113:289–296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Zech N, Hansen E, Bernardy K, Häuser W. Efficacy, acceptability and safety of guided imagery/hypnosis in fibromyalgia—A systematic review and meta-analysis of randomized controlled trials. Eur J Pain 2017;21:217–227 [DOI] [PubMed] [Google Scholar]
- 12. Jensen MP, Patterson DR. Hypnotic approaches for chronic pain management: Clinical implications of recent research findings. Am Psychol 2014;69:167–177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Chamine I, Atchley R, Oken BS. Hypnosis intervention effects on sleep outcomes: A systematic review. J Clin Sleep Med 2018;14:271–283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Stone AB, Sheinberg R, Bertram A, Seymour AR. Are anesthesia providers ready for hypnosis? Anesthesia providers' attitudes toward hypnotherapy. Am J Clin Hypn 2016;58:411–418 [DOI] [PubMed] [Google Scholar]
- 15. Iserson KV. An hypnotic suggestion: Review of hypnosis for clinical emergency care. J Emerg Med 2014;46:588–596 [DOI] [PubMed] [Google Scholar]
- 16. McAllister S, Coxon K, Murrells T, Sandall J. Healthcare professionals' attitudes, knowledge and self-efficacy levels regarding the use of self-hypnosis in childbirth: A prospective questionnaire survey. Midwifery 2017;47:8–14 [DOI] [PubMed] [Google Scholar]
- 17. Kravits K. Hypnosis: Adjunct therapy for cancer pain management. J Adv Pract Oncol 2013;4:83–88 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Sohl SJ, Stossel L, Schnur JB, et al. Intentions to use hypnosis to control the side effects of cancer and its treatment. Am J Clin Hypn 2010;53:93–100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Hermes D, Hakim SG, Sieg P. Acceptance of medical hypnosis by oral and maxillofacial patients. Int J Clin Exp Hypn 2004;52:389–399 [DOI] [PubMed] [Google Scholar]
- 20. Johnson ME, Hauck C. Beliefs and opinions about hypnosis held by the general public: A systematic evaluation. Am J Clin Hypn 1999;42:10–20 [DOI] [PubMed] [Google Scholar]
- 21. Yeh VM, Schnur JB, Montgomery GH. Disseminating hypnosis to health care settings: Applying the RE-AIM framework. Psychol Conscious (Washington, DC) 2014;1:213–228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Capafons A, Cabañas S, Alarcón A, et al. Effects of different types of preparatory information on attitudes toward hypnosis. Contemp Hypn 2005;22:67–76 [Google Scholar]
- 23. Elkins G, Jensen MP, Patterson DR. Hypnotherapy for the management of chronic pain. Int J Clin Exp Hypn 2007;55:275–287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Mizrahi T, Sultan S, Charest M-C, et al. Training nurses in basic hypno-analgesia techniques to reduce procedural distress and pain in children: A feasibility trial. Cogent Med 2016;3:1165083 [Google Scholar]
- 25. Peebles MJ. Trauma-related disorders and dissociation. In: Nash MR, Barnier AJ, eds. The Oxford Handbook of Clinical Hypnosis. New York: Oxford, 2008:647–680 [Google Scholar]
- 26. Montgomery GH, David D, Winkel G, et al. The effectiveness of adjunctive hypnosis with surgical patients: A meta-analysis. Anesth Analg 2002;94:1639–1645 [DOI] [PubMed] [Google Scholar]
- 27. APA Government Relations Staff. Health and Behavior CPT Codes [homepage on the Internet]. 2018. Online document at: https://www.apaservices.org/practice/reimbursement/billing/new-codes, accessed July18, 2019
- 28. Nash MR. Foundations of clinical hypnosis. In: Nash MR, Barnier AJ, eds. Oxford Handbook of Hypnosis: Theory, Research, and Practice. New York: Oxford, 2008:487–502 [Google Scholar]
- 29. Nash M. A psychoanalytic theory of hypnosis: a clinically informed approach. In: Nash MR, Barnier AJ, eds. The Oxford Handbook of Hypnosis: Theory, Research, and Practice. New York: Oxford, 2008:201–224 [Google Scholar]
- 30. Barnes N, Hattan P, Black DS, Schuman-Olivier Z. An examination of mindfulness-based programs in US medical schools. Mindfulness 2017;8:489–494 [Google Scholar]
- 31. Blacker M, Meleo-Meyer F, Kabat-Zinn J, Santorelli S. Mindfulness-based stress reduction curriculum guide. In Santorelli S, Kabat-Zinn J, eds. Mindfulness-Based Stress Reduction Professional Education and Training Resource Manual: Integrating Mindfulness Meditation into Medicine and Healthcare. Worcester, MA: Center for Mindfulness in Medicine, Health Care, and Society, 2012 [Google Scholar]
- 32. Buchholz L. Exploring the promise of mindfulness as medicine. JAMA 2015;314:1327–1329 [DOI] [PubMed] [Google Scholar]
- 33. Singal AG, Higgins PDR, Waljee AK. A primer on effectiveness and efficacy trials. Clin Transl Gastroenterol 2014;5:e45. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


