Abstract
Justice-involved youth (JIY) are at considerable risk for human immunodeficiency virus (HIV), but are disconnected from treatment and prevention. Juvenile justice agencies providing community supervision (CS) are well positioned to provide HIV prevention, testing, and prompt referral to treatment for JIY. However, we lack an understanding of juvenile CS agency responses to HIV/sexually transmitted infection (STI) needs among JIY. We conducted a nationwide systematic assessment of how juvenile CS agencies identify, refer, and move youth through the HIV care cascade using a nationally representative sample of 195 juvenile CS agencies across 20 states. Two-thirds of CS agencies did not offer any HIV-/STI-related services, and 82% reported no collaboration with health agencies. Screening or referral for HIV risk behaviors was reported by 32% of the CS agencies and 12% for any intervention or prevention for HIV/STI risk behaviors. Between 21% and 30% of agencies were unaware of the location of local HIV/STI services. HIV/STI prevention training was not a priority for directors and was ranked second to last out of 16 training topics. Agencies where staff expressed need for HIV risk training and where specific court programming was available were more likely to provide or refer for HIV/STI screening and/or testing. Agencies were more likely to provide or refer for services if they provided pre-trial/pre-adjudication supervision, parole, or court programming. Considering the low provision of HIV/STI-related services and limited collaboration between health and justice agencies, interventions that promote cross-system collaboration designed to minimize barriers and facilitate identification, referral, and linkage to HIV services for JIY are necessary.
Keywords: HIV/STI services, adolescents, juvenile justice
Introduction
Youth involved in the justice system [justice-involved youth (JIY)] report substantially higher rates of human immunodeficiency virus (HIV)/sexually transmitted infection (STI) risk behaviors1–4 and have markedly higher rates of STIs relative to their nonjustice-involved peers.5–7 Risk is further compounded for these youth by their gender identity,8 membership to disrupted and chaotic families,9 and contextual factors known to increase risk of HIV, such as residence in impoverished neighborhoods with high community viral load and low access to treatment and care.10,11 Recently, treatment as prevention (TasP) has come to the fore as an approach that mathematical models have shown will lead to HIV elimination by promoting identification of HIV through testing and ensuring successful linkage, engagement, and retention in care. This approach requires the infected individual to successfully move through the HIV care cascade and achieve viral load suppression, making it difficult to transmit the virus to other partners.12,13
Recent data suggest that youth are not sufficiently moving through the HIV care cascade.
Among high school-aged youth who are sexually active, 78% have never had an HIV test, ∼60% of youth with HIV do not know their status, and only 38% of those with known HIV status are linked to care within 12 months.14,15 Although data are not known about JIY specifically, given their high rates of risk behaviors, exposure to significant contextual risk factors, and frequent disconnection from systems of care, JIY are likely at even greater risk for HIV infection, yet unlikely to know their status compared to general population youth.
JIY engage in substantially higher rates of risk behaviors when in the community compared to locked facilities.3 Justice agencies providing CS are uniquely poised to provide timely HIV prevention, testing, and prompt referral to treatment for JIY who reside in their communities while completing their justice involvement, but who are likely disconnected from HIV-related services offered in schools, health, or behavioral health clinics. Provision of services in these settings is critical in assisting health departments to identify and treat previously unknown infections in a high-risk and hard-to-reach population, while also serving as an “entry point” for youth to engage in prevention services as well as the health care system in general. However, recent findings suggest that juvenile CS agency staff do not perceive HIV/STI testing as an activity that falls within their perceived role.16 Possible reasons for this include agency mission priorities for community safety rather than health,17 or potential stigmatizing attitudes and beliefs about HIV held by agency staff.18 While well-explored in the adult criminal justice system,9 our understanding of juvenile CS agency response to the HIV/STI health needs, specifically screening/testing, referral, and prevention of HIV/STI risk behaviors among adolescents under their care, remains unknown.
A nationwide systematic assessment of how juvenile CS agencies identify, refer, and move youth through the HIV care cascade is a critical first step that can provide information about service shortfalls, inform areas for intervention, and guide the development of targeted strategies to improve uptake of HIV/STI services for this vulnerable and often overlooked population. Using a nationally representative sample of 195 juvenile CS agencies across 192 counties and 20 states, the goals of this study are to (1) describe the type and prevalence of HIV service elements across the HIV care cascade (i.e., screening, assessment, prevention, referral, and treatment) that are provided either directly (on-site) or indirectly (through referral into the community) by juvenile CS agencies; (2) describe agency director knowledge of county HIV service availability and importance of training and technical assistance in HIV practices; and (3) examine youth, organizational, and contextual characteristics that may influence HIV service provision.
Methods
National survey description
A national survey of juvenile justice CS agencies was conducted as part of the Juvenile Justice Translational Research on Interventions for Adolescents in the Legal System (JJ-TRIALS) cooperative agreement funded by the National Institute on Drug Abuse.19 CS agencies play a vital role in processing adolescent offenders, while aiming to address the complex constellation of needs often presented by this population. The survey was therefore designed to document how these agencies currently address substance use, mental illness, and risk of HIV/STIs for youth who are under CS. The survey included questions on agency characteristics; youth characteristics; behavioral health and health (substance use, HIV, and mental health) screening; clinical assessment and referral; risk prevention and treatment practices; the questions also focused on whether services were provided directly or through referrals. Questions also included interagency collaborative activities, family engagement and technical assistance needs, staff educational levels, and training or experience needs.
National survey sampling methodology
Respondent selection was based on a three-stage national probability sampling process that included states, counties, and CS agencies within counties. States and counties were stratified by the number of youth 10 to 19 years of age residing in them, as documented in the 2010 Current Population Survey (CPS; US Census, 2012). In the first stage, the five largest states were selected with certainty. The remaining 15 were selected with probabilities proportionate to the number of youth in five population strata to ensure that less-populated states were included in the study. In the second stage, the largest county and any other mega-counties (with 250,000 or more youth or half or more of the state's youth in smaller states) within each state were selected with certainty. The remaining counties were selected with probabilities proportionate to the number of youth in those counties. In the two small sampled states organized by judicial district instead of counties, all counties/districts were sampled.
In the third stage, all CS agencies that served youth on CS in the 192 sampled counties, 203 agencies were identified and surveyed regardless of the number of youth they served. In states where CS agencies were managed at the state level, key stakeholders at the state level were contacted to help identify the CS agencies and appropriate contact within the sampled counties and to encourage participation in the survey. In states with decentralized systems, all CS agencies within the sampled counties were contacted directly.
National survey administration, completion, and weighting
The agencies were instructed to have staff who were familiar with the agency's organization, priorities, youth under CS, and the services they receive to fill out the survey. Instructions also stated that it was likely that several staff may need to provide input. Along with the survey instructions, each agency had a survey coach to help increase the likelihood of accurate and complete responding.
Surveys were completed for 195 of the 203 identified CS agencies (96% completion rate). Data were weighted based on the inverse of the inclusion probability at each of the three stages (1.0 for certainty state or counties and stage 3) and then adjusted for nonresponse within state. The number of agencies overall and those providing a specific service were estimated by multiplying the weighted average number of agencies per county times the actual number of counties (n = 3143) in the United States (excluding DC & territories). This generated a national estimate of 3202 CS agencies serving 770,323 youth under CS.
National survey HIV-related services, youth characteristics, and agency characteristics/item description
HIV service-related items included use of any screener instruments or clinical assessment tools by an agency, questions about perceived HIV risk behaviors of youth on the agency's caseload, and whether youth received HIV/STI prevention or treatment services at the agency or were referred to an external provider. Respondents were also asked if their agency provided testing for HIV, other STIs, and hepatitis B and/or C. Respondents for CS agencies were also asked about their relationship with external partners. These included external HIV prevention providers. When such a relationship was reported, there were follow-up questions on similarity of program requirements, providing office space, joint staffing, cross-training, and written protocols for sharing information.
Youth characteristics are based on the CS agency's caseload and not on individual youth. The CS agency respondent was asked to report the percentage of youth they served who met different characteristics (ages 10–11, 12–13, and so on, male, female, African American, Hispanic, engaging in HIV risk behavior, etc.). For the purposes of regression analyses (see Data Analysis section), we dichotomized these variables (1 = yes and 0 = no). To avoid having a small number of agencies in either cell (i.e., yes or no cells), answers were dichotomized with 1 representing a cell frequency of about 25% and 0 representing the rest. The cut-points for dichotomization of (1) gender, (2) age, (3) race/ethnicity, and (4) HIV risk variables were as follows: (1) high female caseload, defined as agencies with a caseload of ≥20% females; (2) older caseload, defined as agencies with a caseload in which 85% were 14 years of age and older; (3) high minority caseload, defined as agencies with a caseload of ≥20% minority (African American or Hispanic, the two largest minority groups); and (4) high HIV risk caseload, defined as agencies with a caseload in which ≥45% were perceived as engaging in HIV risk behavior (risky sexual activity and/or needle use). For all of the above youth characteristics, if the respondents reported that the data were not available, or the data are not collected, they were coded to no (0).
For agency characteristics used in the regression models (see Data Analysis section), agency characteristics were also dichotomized (1 = yes and 0 = no). The number of youth on CS served in the past year was divided by 100 so that odds ratios (OR) would be based on a difference of 100 youth served. Supervision variables captured the types of supervision an agency provided (y/n): pre-trial or pre-adjudication, post-adjudication supervision, probation, parole, and supervised release. Agency staff size was based on the total of the nonclinical, clinical, and medical full time employees (FTEs) reported [mean (M) = 9.9 and standard deviation (SD) = 26.49]. Staff in need of effective HIV risk behavior training is based on the respondent reporting agree or strongly agree that CS staff working with youth on CS need additional training or experience with effective HIV risk behavior prevention. Specialized programs include the respondent endorsing any diversion program the agency participates in; any specialized court programs (i.e., Juvenile drug court, Teen court, and so on) the agency participates in; and any system-level reforms the agency participates in (implemented management information system, agreements to take advantage of insurance to help pay for services, and grants).
County characteristics include any HIV testing services available in the county where the CS agency is located. County HIV prevalence rates were drawn from County Health Rankings & Roadmaps (www.countyhealthrankings.org/app/). The prevalence rate was transformed to a z-score, so the OR is based on the change of one SD. The average prevalence rate per 100,000 persons was 260.9 with a SD of 343.9. Urbanicity is based on three groups using rural urban continuum codes (RUCC): (1) urban area counties (RUCCs of 1, 2, and 3); (2) adjacent urban—rural counties adjacent to an urban area (RUCCs of 4, 6, and 8); and (3) rural—nonurban counties not adjacent to an urban area (RUCCs of 5, 7, and 9). These were retrieved from www.ers.usda.gov/data-products/rural-urban-continuum-codes/. The agencies in urban area counties were the referent group. Poverty level is from www.census.gov/data-tools/demo/saipe and reports the percentage of the county that is in poverty. Across the counties in this sample, the percent of the county in poverty ranged from 3% to 31%. The percentage was divided by 10, so the OR is based on a change of 10% points.
The two main outcomes in the regression analyses in this study are as follows: (1) any screening/assessment for HIV risk behaviors, either directly (onsite) or through referral (offsite) and (2) any HIV risk intervention/prevention provided directly (on-site) or through referral (off-site). Due to the small percentages and number of respondents reporting directly providing these services, we collapsed directly providing a service with any referral for that service. If a respondent endorsed screening for or administering a clinical assessment for HIV risk behavior, or reported they referred for screening or assessment of HIV risk behaviors, it was coded as provision of any screening or assessment. The same process was used to create the dichotomy for provision of any intervention or prevention, directly or through referral.
Data analysis
All analyses were run using IBM SPSS version 25.01. Since our outcomes (i.e., any HIV/STI screening or assessment and any HIV/STI prevention or treatment) are dichotomous, we used the Complex Samples Logistics Regression (CSLOGISTIC) procedure. This procedure performs the analysis on the sample using complex sampling methods and weights (described above). This procedure estimates the variances based on the sampling design and reduces the number of agencies/providers back to the original sample size, thus avoiding “artificially” decreasing the standard errors and inflating the power of these analyses. Using a backward stepwise method of the logistic regression analyses to maximize power, in which independent variables were removed until only significant (p < 0.05) independent variables were left in the model, we fit two multivariable models to examine agency and county characteristics that are associated with any provision of HIV/STI screening or assessment services (either on-site or off-site), and any prevention or treatment services (Table 3).
Table 3.
Youth, Agency, and County Predictors of HIV Service Delivery (On-Site or Off-Site) (Weighted Number Agencies, n = 3202)
| Predictors | Any screening/assessment |
Any intervention/prevention |
||
|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | |
| Agency predictors | ||||
| Characteristics on youth served | ||||
| Gender (>20% female) | ||||
| Age (>85% 14 years old) | ||||
| Race/ethnicity (>10% minority) | ||||
| % HIV risk (>45% with HIV risk) | ||||
| Number of youth served | ||||
| Supervision type | ||||
| Probation | ||||
| Pre-trial or pre-adjudication | 5.19 | 1.30–20.70 | ||
| Post-adjudication supervision of minors with only status offenses | ||||
| Supervised release | ||||
| Parole | 8.52 | 2.19–33.17 | ||
| Agency staff size | ||||
| Clinical/medical staff on staff | ||||
| Staff in need of effective HIV risk behavior training | 4.47 | 1.51–14.85 | ||
| Specialized programs | ||||
| Diversion | 0.01 | 0.003–0.05 | ||
| Court programs | 3.24 | 1.08–9.76 | 5.22 | 1.35–20.21 |
| System level reforms | ||||
| County predictors | ||||
| HIV testing services available in county | ||||
| HIV incidence in county (accessed by) | ||||
| Urbanicity | ||||
| Adjacent urban | ||||
| Rural | ||||
| Poverty level | ||||
A backward stepwise method of the logistic regression analyses was used; presented models are final.
CI, confidence interval; OR, odds ratio.
Results
Youth and agency characteristics
The characteristics of the youth served and the agencies sampled in the survey are presented in Table 1.
Table 1.
Agency and Youth Characteristics (Weighted Number of Agencies, n = 3202)
| n | % | |
|---|---|---|
| Youth characteristics (n = 770,323) | ||
| Male | 562,336 | 73 |
| Race/ethnicity | ||
| White/Caucasian | 408,271 | 53 |
| Black/African American | 200,284 | 26 |
| Hispanic/Latino | 138,658 | 18 |
| Asian/Hawaiian/ Pacific Island Native | 15,406 | 2 |
| American/Alaskan | 7703 | 1 |
| Other race | 15,406 | 2 |
| Mixed race | 15,406 | 2 |
| Age | ||
| 10–11 | 15,406 | 2 |
| 12–13 | 77,032 | 10 |
| 14–15 | 277,316 | 36 |
| 16–17 | 338,942 | 44 |
| ≥18 | 61,626 | 8 |
| Any substance use | 392,865 | 51 |
| Alcohol use problems | 192,581 | 25 |
| Marijuana use problems | 377,458 | 49 |
| Prescription drug misuse | 146,361 | 19 |
| Other drug use problems | 138,658 | 18 |
| Tobacco use | 323,536 | 42 |
| Risky sexual activity | 392,865 | 51 |
| External disorders | 269,613 | 35 |
| Internal disorders | 269,613 | 35 |
| Agency characteristics | ||
| Youngest age of youth served | ||
| ≤9 | 704 | 22 |
| 10–11 | 637 | 20 |
| 12–13 | 544 | 17 |
| Not specified | 1312 | 41 |
| Oldest age of youth served | ||
| 14–16 | 160 | 5 |
| 17 | 1217 | 38 |
| 18–20 | 801 | 25 |
| 21+ | 768 | 24 |
| Not specified | 224 | 7 |
| Type of CS | ||
| Probation | 3170 | 99 |
| Pre-trial or pre-adjudication | 2081 | 65 |
| Post-adjudication supervision of minors with only status offenses | 2113 | 66 |
| Supervised release | 736 | 23 |
| Parole | 704 | 22 |
| Other | 320 | 10 |
| Staff | ||
| Clinical staff | 1223 | 38 |
| Medical staff | 179 | 6 |
| Probation or parole officersa | 3199 | M = 7.75 (SD = 18.3) |
| Inter-agency collaboration between CS and HIV agencies | ||
| No collaboration | 2613 | 82 |
| Share information | 458 | 14 |
| Similar requirements | 247 | 8 |
| Written protocol | 134 | 4 |
| Joint staffing | 102 | 3 |
| Cross-train | 99 | 3 |
| Provide office space | 22 | 1 |
Mean and standard deviation.
CS, community supervision.
Youth
The majority of youth served were male (73%) and white (53%). The vast majority of agencies served youth between the age range of 14 and 17. Youth 16 and 17 years of age comprised 44% of the sample, while 36% were 14 and 15 years of age. Half of the youth were reported as having some form of a substance use problem, with marijuana use problems (49%) being the most common, followed closely by tobacco use (42%). Alcohol use (25%), prescription drug use (19%), and other drug use problems (18%) were less frequently identified. In addition to substance use, 51% of youth were reported to be engaged in risky sexual activity. With respect to mental health, about one-third were reported as experiencing external (35%) and internal (35%) disorders.
Agency and county
In terms of the ages served by CS agencies, the youngest age that the agencies served included youth younger than 9 (22%), ages 10 to 11 (20%), or ages 12 to 13 (17%); 41% did not have a minimum age range. Nearly one-quarter of agencies served individuals older than 21 years (24%), although the largest proportion of agencies capped the age of service at 17 (38%); 7% did not specify a maximum age served. Agencies provided a variety of CS services. Almost all (99%) CS agencies offered probation, while pre-trial supervision (65%) and post-adjudication supervision of status offenders (66%) were provided in about two-thirds of agencies. Parole (22%), supervised release (23%), and other forms of supervision (10%) were offered less frequently.
With respect to agency staff, the average number of probation or parole officers per agency was just shy of eight (M = 7.75, SD = 18.3). About one-third of agencies reported having clinicians (38%) and only 6% reported having medical staff to treat health- and behavioral health-related issues. When asked about interagency collaboration, 82% of agencies reported that collaboration between juvenile justice (JJ) and HIV agencies does not currently exist. The most commonly reported type of collaboration between JJ and HIV agencies is the sharing of information (14%). Less than 5% of agencies reported collaborating through written protocol, cross-training, joint staffing, or use of dedicated office space.
Type and prevalence of HIV-/STI-related services provided on-site or referred off-site
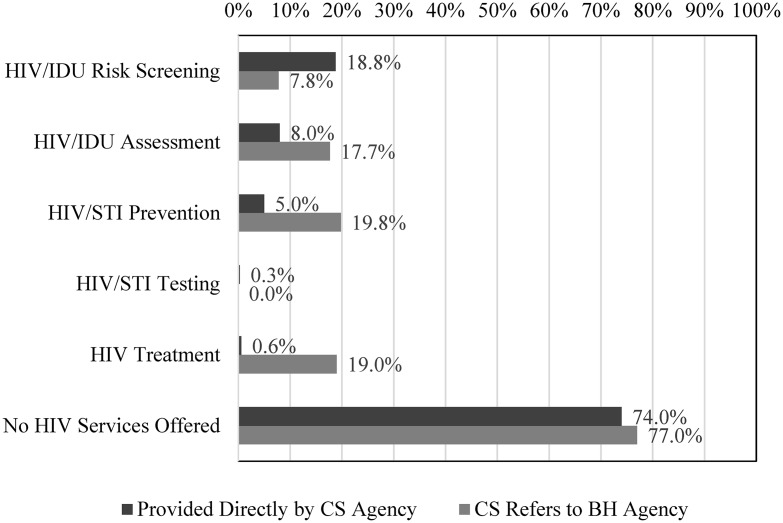
JJ agencies were asked to report whether they provided a series of HIV-/STI-related services on-site or whether they referred their clients to outside providers for services. The majority (63.4%) of CS agencies neither provide HIV/STI services on-site nor off-site through referral to services in the community; 74% do not provide any services on-site and 77% do not provide any services off-site. When services are provided on-site by CS agencies, those on-site services typically occurred earlier in the service cascade, whereas off-site referrals to outside providers were more frequently for services that occur later in the service cascade (Fig. 1).
FIG. 1.
HIV-/STI-related services provided directly on-site or by referral (off-site) (weighted number of agencies, n = 3202). HIV, human immunodeficiency virus; STI, sexually transmitted infection.
Over 18% of JJ agencies provided on-site behavioral screening for HIV/sexual risk or injection drug use (IDU), whereas 7.8% reported referring off-site for behavioral risk screening (Table 2). Among JJ agencies conducting behavioral screening on-site, it was more common for them to report screening for HIV risk and risky sexual behaviors (18.6%) than for IDU risk (3.3%).
Table 2.
Prevalence of HIV Services Provided on or Referred Off-Site in Community Supervision Agencies (Weighted Number of Agencies, n = 3202)
| n | %/mean | |
|---|---|---|
| On-site HIV-related services | ||
| Screening | ||
| Any behavioral screening HIV, IDU risk | 603 | 18.8 |
| HIV/sex risky | 596 | 18.6 |
| IDU risk | 106 | 3.3 |
| Assessment | ||
| Any HIV/IDU behavioral risk assessment | 256 | 8.0 |
| IDU risk assessment questions | 256 | 8.0 |
| Conduct a comprehensive HIV assessment | 30 | 0.6 |
| Prevention | ||
| Any prevention program | 161 | 5.0 |
| Brief HIV intervention | 98 | 3.1 |
| HIV prevention, education, counseling | 68 | 2.1 |
| STI prevention, education, counseling | 63 | 2.0 |
| Prevention services | 51 | 1.6 |
| Other HIV, HCV or other STI prevention program(s) | 36 | 1.1 |
| HIV testing/treatment | ||
| Any testing or treatment | 36 | 1.1 |
| HIV testing | —a | —a |
| STI testing | 10 | 0.3 |
| HIV treatment (on-site) | 19 | 0.6 |
| Referral to off-site HIV-related services | ||
| Screening | ||
| Referred to an external agency for HIV risk behavior screening | 248 | 7.8 |
| Assessment | ||
| Any referral for HIV assessment | 576 | 18.0 |
| Prevention | ||
| Any referral for intervention/prevention | 634 | 19.8 |
| Refer off-site for prevention services | 464 | 14.5 |
| Refer off-site for support group | 426 | 13.3 |
| Refer off-site for brief intervention | 208 | 6.5 |
| HIV treatment | ||
| Refer off-site for HIV treatment | 622 | 19.42 |
| County HIV-related services | ||
| Have HIV testing available by external agency within county | 2488 | 77.7 |
Estimates <0.3% too unreliable to report.
n, based on the weighted estimate of community supervision agencies.
HCV, hepatitis C virus; IDU, injection drug use; STI, sexually transmitted infection.
A higher proportion of JJ agencies referred to off-site providers for HIV/IDU behavioral risk assessments (18.0%) rather than providing the service in-house (8.0%). In contrast to in-house screening practices, JJ agencies conducting on-site assessments focused on IDU risk (8.0%) more often than HIV risk (0.6%). It was also more common for JJ agencies to refer to outside providers for HIV/STI intervention and/or prevention services (19.8%). JJ agencies referred youth to outside agencies for prevention (14.5%), support group (14.5%), and brief intervention (6.5%) services. Only 5% of JJ agencies provided these services on-site (5.0%).
Among JJ agencies offering intervention and/or prevention programs, an average of 74.29 youth (SD = 33.15) received HIV prevention, education, and counseling services, while an average of 77.63 youth (SD = 31.84) received STI prevention, education, and counseling services in the past year.
On-site HIV or STI testing and treatment services are virtually nonexistent with about one percent of agencies providing these services on-site. Among those providing STI testing, an average of 1.16 youth received testing in the past year; estimates for on-site HIV testing were too unreliable to report. HIV treatment was offered in 0.6% of JJ agencies, whereas nearly 20% of agencies reported referring youth to outside providers for HIV treatment services. While estimates for referral for off-site HIV testing were not collected for off-site providers, more than three-quarters (77.7%) of JJ agencies stated that there was an external agency within their county available to conduct HIV testing.
Agency respondent knowledge of HIV-/STI-related service availability
When asked about the availability of a variety of HIV-related services within their county, anywhere from 21% to 30% of agency directors stated they were unaware of where youth could receive particular services. Among the services discussed, the largest proportion (30%) of directors stated they did not know where to send youth to get services related to HIV/AIDS prevention. Twenty-four percent were unsure where to find hepatitis prevention service, while 23% stated they were unaware of where to procure STI prevention and STI, hepatitis B, hepatitis C, or tuberculosis testing. Between 3% and 4% reported services as being unavailable in their county.
Training priorities
Although 42% of agencies endorsed “Evidence-based prevention and treatment for HIV risk behaviors” as important, when asked to rank 17 training and technical assistance topics in order of priority, it ranked second to last (number 16). The highest priority issues were (1) “Impact of trauma and other mental health disorders on adolescent behavior,” (2) “Effective substance use prevention,” and (3) “Integrating screens and assessments with case planning and implementation.” Only training on “Effectively Monitoring Youth Progress” was ranked lower than HIV-related services.
Associations between contextual characteristics and HIV service provision
Table 3 presents any HIV/STI screening/assessment and any HIV/STI intervention/prevention service provided, (either directly on-site or by referral to off-site providers), and their association to agency or county characteristics. A backward stepwise method of the logistic regression analyses was used. Any screening or referral for HIV risk behaviors was reported for 32% of the CS agencies and 12% for any intervention or prevention for HIV risk behaviors.
Agencies were over four times more likely to directly provide or refer to HIV screening when agency staff expressed a need for effective HIV risk behavior training [OR: 4.47; confidence interval (CI): 1.51–14.85] and over three times more likely to do so when the agency ran specialized court programs (e.g., drug court OR: 3.24; CI: 1.08–9.76). HIV screening and assessment were significantly less likely when agencies ran specialty diversion programs (OR: 0.01; CI: 0.003–0.05).
Agencies were nearly five times more likely to directly provide/refer youth to any HIV/STI intervention/prevention service when pre-adjudication supervision was available (OR: 5.19; CI: 1.30–20.7), and over eight times more likely to do so when probation supervision was available (OR: 8.52; CI: 2.19–33.17). Service provision was also over five times more likely in agencies responding they provided specialized court programs (OR: 5.22; CI: 1.35–20.21).
Discussion
This is the first known nationally representative study to examine the availability of services within the HIV care cascade framework in juvenile CS agencies. Study strengths include the robust sampling strategies to ensure a nationally representative sample, which increases representativeness and generalizability of this study's findings. Overall, the state of the HIV/STI service access for youth on CS is concerning. There is tremendous untapped potential for CS agencies to serve as an “entry point” for youth to engage in early HIV prevention as well as access other needed mental and physical health services. For example, despite high rates of perceived sexual risk behavior among JIY in this study, as well as documented in the literature,1,3,20 no more than 20% of CS agencies provided on-site or off-site prevention programming, and <1% provided on-site HIV or STI testing. Instilling the importance of safer sex practices among youth may reduce infectious disease transmission throughout the life course. Similarly, about 3% of CS agencies screen for IDU risk despite high rates of JIY reporting prescription drug misuse,21,22 and IDU as a primary transmission route for HIV and hepatitis C virus. This is particularly significant in light of the current US opioid epidemic, which calls for the lack of IDU and opioid use screening to be remedied.23,24
It is important to note that, while CS agencies perceived that half of JIY were at risk for HIV/STI due to sexual or drug use behaviors, about three-fourths of JJ agencies do not provide any HIV/STI service (either on-site or through referrals). While HIV/STI prevention and testing services are readily available within these counties, it is concerning that 21–30% of CS agencies do not know where to locate community-based HIV/STI testing or where to access HIV prevention services, indicating a need to promote interagency collaboration. This may be an opportunity for health departments or community-based HIV agencies to reach out to CS agencies. CS staff understand the importance of HIV/STI service for JIY and thus may be open to service expansion, but are not motivated to seek out additional training due to the perception that other training needs are more pressing (e.g., behavioral health). Moreover, training that addresses stigma related to HIV and providing HIV-related services may also be necessary as part of this outreach. Research has shown that various providers, including those in correctional settings, hold stigmatizing attitudes and beliefs related to HIV and people living with HIV (PLWH), which can impede provision of services and therefore limit the ability to identify those who are undiagnosed and successfully link them to treatment and care.18,25 Packaging mental health and substance use prevention and treatment with evidence-based prevention and treatment for HIV risk behaviors would prove fruitful in the light of agency directors' ranking of importance of training in behavioral health.
Furthermore, findings indicate that youth were not moving sufficiently through the HIV case cascade and that service availability becomes more limited as youth transition further into the cascade, especially for on-site services. The first step in the HIV service cascade is the identification of HIV through routine testing. Given the very low rate of HIV and STI testing identified in this study and lack of collaboration between JJ and HIV agencies, currently, the TasP approach will not work in community-based juvenile justice settings. Barriers to implementation of HIV/STI prevention programming and service delivery in adult and juvenile correctional institutions, as identified by prior studies, included a lack of staff knowledge about HIV and poor understanding of line staff roles in facilitating these services.26 Attitudes and beliefs of juvenile court and probation staff can also present challenges to the provision of HIV prevention, testing, and treatment linkage practices with youth under CS. A survey of JJ staff found that less than one-third rated their role in the provision of HIV testing for all youth on their caseloads as important.16 Although importance ratings for HIV prevention education and treatment linkage were somewhat higher, these same JJ staff rated the importance of substance use prevention, screening (including biological testing), and treatment linkages significantly higher compared with HIV/STI services.27
Implementation science research is critical to addressing barriers to HIV/STI service delivery for JIY. Contextual factors influencing the implementation process28 and strategies to promote the adoption, implementation, and sustainment of evidence-based practices29 have been identified and tested in behavioral health settings.30 Future research should continue to identify challenges associated with implementing HIV testing, prevention interventions, and linkages to treatment among justice-involved populations.31–33
Implementation science studies are also needed to test strategies for overcoming the identified barriers and for enhancing productive collaboration among juvenile justice, public health, and community-based service organizations.
Limitations
Although the data were drawn from a nationally representative sample of 20 states and 192 counties, data were collected through agency-completed surveys and not completed by the same type of agency staff member (e.g., chief administrator and specific program director).
Hence, it is likely different types and durations of experiences are reflected in the respondents' replies to the survey questions. Second, while it is known that the agencies varied in how they completed the surveys, the researchers could not directly observe or code how this was done (e.g., whether the survey responses were based on systematic data or a group review, or by an individual). Finally, the survey did not capture information on staff attitudes or describe characteristics and needs of youth drawn from agency staff or youth respondents, respectively. The purposes of this survey precluded the collection of data from multiple types of respondents (e.g., probation staff, youth, and caregivers).
Implications for research and practice
Despite these limitations, findings from this study have important implications for research and practice. Although the epidemiologic data provide ample evidence of the excessive risk for HIV/STI acquisition and transmission for this adolescent population,1,3,6 the findings highlight myriad gaps in research and service availability. Although at substantially greater risk for HIV/STI, data demonstrate that the majority of CS agencies offer no HIV services to JIY on their caseloads. This represents a significant missed opportunity. The threat posed by this lack of prevention and screening services is that adolescents will remain in their communities, disconnected from health and other protective systems, not screened, and ill-equipped to address the prevalent risk behaviors in their socio-sexual networks, which often exist in high HIV/STI prevalence communities. Thus, there is an urgent need for greater research to design, implement, and evaluate demonstrably effective HIV/STI screening and prevention programs in CS facilities.34,35
In addition, the data highlight the fragmentation of services in the systems that directly provide services to JIY. Most concerning was the disconnect between the juvenile justice system and community-based service providers, primarily the county health department. The survey identified poor interagency collaboration; for instance, 82% reported that collaboration between juvenile justice agencies and HIV/STI agencies, such as the county health department, does not currently exist. Thus, we need to develop and evaluate interventions to promote cross-system collaboration, designed to minimize barriers and facilitate identification, referral, and importantly, linkage to HIV services for those youth detected with HIV or other STIs. And, although developing effective prevention and screening programs is important, ultimately, it is imperative that programs be adopted, integrated, and sustained by juvenile justice systems and community-based health partners. One such approach is utilization of service delivery models in which health and justice systems develop partnerships so that health providers are integrated or embedded within the justice settings to provide on-site HIV-related services that are perceived as beyond the purview of the justice staff.36,37
Finally, implementation science can be valuable in identifying effective dissemination strategies that increase adoption of information and programs by clinicians, other health practitioners, juvenile justice systems, social service providers, and program managers in community-based organizations. One example of this research is a multi-site cooperative initiative by the National Institute on Drug Abuse, called JJ-TRIALS, a randomized cluster trial that tests innovative and theory-driven models to promote the adoption and sustainment of evidence-based screening, assessment, and referral to community agencies.38 Any effort to provide greater integration of services will need to accommodate the different organizational cultures, finances, and management expertise of the agencies. Finally, system-level reform must be a priority. Creating change across the systems of care will require a coordinated and systematic approach that leverages the expertise of all agencies engaged in relevant systems' reform.35,39
Acknowledgments
The authors gratefully acknowledge the collaborative contributions of NIDA. NIDA Science Officer on this project is Tisha Wiley.
The authors would also like to thank Bruce Spencer for his invaluable assistance developing the sampling and weighting strategies; the JJ-TRIALS Survey Advisory Board (Nancy Arrigona, Patrick Flynn, Craig E. Henderson, Matt Hiller, Hannah K. Knudsen, Mark W. Lipsey, Edward (Ned) Loughran, Sharon Marsh, David Morse, Anne Spaulding, Faye Taxman, Gail Wasserman, Carl Wicklund, and Tisha Wiley) for input on the survey and design; the staff who worked on the project; and most of all, the respondents for completing the surveys.
Author Disclosure Statement
No competing financial interests exist.
Funding Information
This study was funded under the JJ-TRIALS cooperative agreement, funded at the National Institute on Drug Abuse (NIDA) by the National Institutes of Health (NIH) from the following grant awards: Chestnut Health Systems (U01DA036221); Columbia University (U01DA036226); Emory University (U01DA036233); Mississippi State University (U01DA036176); Temple University (U01DA036225); Texas Christian University (U01DA036224); and University of Kentucky (U01DA036158). The opinions expressed here, however, are those of the authors and do not represent official positions of the government.
References
- 1. Teplin LA, Mericle AA, McClelland GM, Abram KM. HIV and AIDS risk behaviors in juvenile detainees: Implications for public health policy. Am J Public Health 2003;93:906–912 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Pack RP, DiClemente RJ, Hook EW III, Oh KM. High prevalence of asymptomatic STDs in incarcerated minority male youth: A case of screening. Sex Transm Dis 2000;27:175–177 [DOI] [PubMed] [Google Scholar]
- 3. Romero EG, Teplin LA, McClelland GM, Abram KM, Welty LJ, Washburn JJ. A longitudinal study of the prevalence, development, and persistence of HIV/STI risk behaviors in delinquent youth: Implications for health care in the community. Pediatrics 2007;119:e1126–e1141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Elkington KS, Bauermeister JA, Zimmerman MA. Psychological distress, substance use, and HIV/STI risk behaviors among youth. J Youth Adolesc 2010;39:514–527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Spaulding AC, Miller J, Trigg BG, et al. . Screening for sexually transmitted diseases in short-term correctional institutions: Summary of evidence reviewed for the 2010 centers for disease control and prevention sexually transmitted diseases treatment guidelines. Sex Transm Dis 2013;40:679–684 [DOI] [PubMed] [Google Scholar]
- 6. Wiehe SE, Rosenman MB, Aalsma MC, Scanlon ML, Fortenberry JD. Epidemiology of sexually transmitted infections among offenders following arrest or incarceration. Am J Public Health 2015;105:e26–e32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Robertson AA, Baird Thomas C, St. Lawrence JS, OPack R. Predictors of infection with Chlamydia or Gonorrhea in incarcerated adolescents. Sex Transm Dis 2005;32:115–122 [DOI] [PubMed] [Google Scholar]
- 8. Reisner SL, Jadwin-Cakmak L, Sava L, Liu S, Harper GW. Situated vulnerabilities, sexual risk, and sexually transmitted infections' diagnoses in a sample of transgender youth in the United States. AIDS Patient Care STDS 2019;33:120–130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Elkington KS, Jaiswal J, Spector AY, et al. . Can TasP approaches be implemented in correctional settings? A review of HIV testing and linkage to community HIV treatment programs. J Health Care Poor Underserved 2016;27:71–100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Fox BH, Perez N, Cass E, Baglivio MT, Epps N. Trauma changes everything: Examining the relationship between adverse childhood experiences and serious, violent and chronic juvenile offenders. Child Abuse Negl 2015;46:163–173 [DOI] [PubMed] [Google Scholar]
- 11. Chung HL, Steinberg L. Relations between neighborhood factors, parenting behaviors, peer deviance, and delinquency among serious juvenile offenders. Dev Psychol 2006;42:319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Granich RM, Gilks CF, Dye C, De Cock KM, Williams BG. Universal voluntary HIV testing with immediate antiretroviral therapy as a strategy for elimination of HIV transmission: A mathematical model. Lancet 2009;373:48–57 [DOI] [PubMed] [Google Scholar]
- 13. Dieffenbach CW, Fauci AS. Universal voluntary testing and treatment for prevention of HIV transmission. JAMA 2009;301:2380–2382 [DOI] [PubMed] [Google Scholar]
- 14. Van Handel M, Kann L, Olsen EOM, Dietz P. HIV testing among US high school students and young adults. Pediatrics 2016;137:e20152700. [DOI] [PubMed] [Google Scholar]
- 15. Zanoni BC, Mayer KH. The adolescent and young adult HIV cascade of care in the United States: Exaggerated health disparities AIDS Patient Care STDS 2014;28:128–135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Gardner SK, Elkington KS, Robertson A, et al. Using interagency workgroups to increase HIV/STI testing among youth on community supervision: Successes and challenges. Paper presented at the American Public Health Association Annual Meeting; November 10–14, 2018; San Diego. Abstract 413318
- 17. Henderson CE, Taxman FS. Competing values among criminal justice administrators: The importance of substance abuse treatment. Drug Alcohol Depend 2009;103S:S7–S16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Geter A, Herron AR, Sutton MY. HIV-related stigma by healthcare providers in the United States: A systematic review. AIDS Patient Care STDS 2018;32:418–24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Scott CK, Dennis ML, Grella CE, Funk RR, Lurigio AJ. Juvenile justice systems of care results of a national survey of community supervision agencies and behavioral health providers on services provision and cross-system interactions. Health Justice 2019;7:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Elkington KS, Belmonte K, Latack JA, et al. . An exploration of family and juvenile justice systems to reduce youth HIV/STI risk. J Res Adolesc 2015;25:700–716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Alemagno SA, Stephens P, Shaffer-King P, Teasdale B. Prescription drug abuse among adolescent arrestees: Correlates and implications. J Correct Health Care 2009;15:35–46 [DOI] [PubMed] [Google Scholar]
- 22. Vaughn MG, Freedenthal S, Jenson JM, Howard MO. Psychiatric symptoms and substance use among juvenile offenders: A latent profile investigation. Crim Justice Behav 2007;34:1296–1312 [Google Scholar]
- 23. Zibbell JE, Asher JK, Patel RC, et al. . Increases in acute hepatitis C virus infection related to a growing opioid epidemic and associated injection drug use, United States, 2004 to 2014. Am J Public Health 2018;108:175–181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Madras BK. The surge of opioid use, addiction, and overdoses: Responsibility and response of the US health care system. JAMA Psychiatry 2017;74:441–442 [DOI] [PubMed] [Google Scholar]
- 25. Eaton LA, Driffin DD, Kegler C, et al. . The role of stigma and medical mistrust in the routine healthcare engagement of black men who have sex with men. Am J Public Health 2015;105:75–82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Robillard AG, Gallito-Zaparaniuk P, Arriola KJ, Kennedy S, Hammett T, Braithwaite RL. Partners and processes in HIV services for inmates and ex-offenders: Facilitating collaboration and service delivery. Eval Rev 2003;27:535–562 [DOI] [PubMed] [Google Scholar]
- 27. Robertson AA, Gardner SK, Knight D, et al. Is there a place for HIV and STI services in juvenile justice? Staff attitudes towards HIV and STI testing, prevention and treatment. Paper presented at the American Public Health Association Annual Meeting; 2018; San Diego, CA. Abstract 413485
- 28. Powell BJ, Beidas RS. Advancing implementation research and practice in behavioral health systems. Adm Policy Ment Health 2016;43:825–833 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Powell BJ, McMillen JC, Proctor EK, et al. . A compilation of strategies for implementing clinical innovations in health and mental health. Med Care Res Rev 2012;69:123–157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Rosen CS, Matthieu MM, Wiltsey Stirman S, et al. . A review of studies on the system-wide implementation of evidence-based psychotherapies for posttraumatic stress disorder in the Veterans Health Administration. Adm Policy Ment Health 2016;43:957–977 [DOI] [PubMed] [Google Scholar]
- 31. Robillard AG, Braithwaite RL, Gallito-Zaparaniuk P, Kennedy S. Challenges and strategies of frontline staff providing HIV services for inmates and releasees. J Correct Health Care 2011;17:344–360 [DOI] [PubMed] [Google Scholar]
- 32. Taxman FS, Belenko S. Organizational change–technology transfer processes: A review of the literature. In: Implementing Evidence-Based Practices in Community Corrections and Addiction Treatment. F Taxman and S Belenko, eds. Springer: Verlag; 2012:91–128 [Google Scholar]
- 33. Tolou-Shams M. Challenges to conducting adolescent HIV prevention services research with court-involved youth. Child Youth Serv Rev 2017;83:201–208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Brent RJ, Maschi T. An estimate of the benefits of not having HIV/AIDS in a prison setting. Clin Res HIV/AIDS 2015;2:1022 [Google Scholar]
- 35. DiClemente RJ, Davis TL, Swartzendruber A, et al. . Efficacy of an HIV/STI sexual risk-reduction intervention for African American adolescent girls in juvenile detention centers: A randomized controlled trial. Women Health 2014;54:726–749 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Elkington KS, Cohall A, Cohall R, et al. (2019). Working with justice-involved young adults, a justice agency, and a community-based health agency to develop of a novel service delivery model to prevent HIV, STIs and substance abuse delivered within an alternative justice setting. Paper presented for presentation at the 12th Academic & Health Policy Conference on Correctional Health, March 20–22, Las Vegas, NV
- 37. Elkington KS, Spaulding A, Gardner S, et al. A system-level intervention to encourage collaboration between juvenile justice and public health agencies to promote HIV/STI testing. AIDS Patient Care and STDS (in press) [DOI] [PMC free article] [PubMed]
- 38. Knight DK, Belenko S, Wiley T, et al. . Juvenile Justice-Translational Research on Interventions for Adolescents in the Legal System (JJ-TRIALS): A cluster randomized trial targeting system-wide improvement in substance use services. Implement Sci 2016;11:57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Donenberg G, Emerson E, Kendall AD. HIV-risk reduction intervention for juvenile offenders on probation: The PHAT Life group randomized controlled trial. Health Psychol 2018;37:364–374 [DOI] [PMC free article] [PubMed] [Google Scholar]