Abstract
Objective
The aims of this study were to describe distributions of the prevalence of osteopenia and osteoporosis and identify the potential risk factors by gender in a Chinese rural population.
Design
A cross-sectional survey.
Setting and participants
A total of 8475 participants (18–79 years) were obtained from the Henan Rural Cohort Study. Bone mineral density (BMD) of the calcaneus for each individual was measured by ultrasonic bone density apparatus. Logistic regression models were used to evaluate associations of potential risk factors with prevalence of osteopenia and osteoporosis. Furthermore, a meta-analysis of prevalence of osteoporosis which included eight studies was conducted to confirm this study results.
Results
The mean of BMD were 0.42 and 0.32 g/cm2 for men with osteopenia and osteoporosis (p<0.001), as well as 0.40 and 0.30 g/cm2 (p<0.001) for women with osteopenia and osteoporosis, respectively. The overall age-standardised prevalence of osteopenia and osteoporosis were 42.09% and 11.76% in all participants. The age-standardised prevalence of osteopenia in men (45.98%) was significantly higher than that in women (39.73%), whereas the age-standardised prevalence of osteoporosis in men (7.82%) was lower than that in women (14.38%). Meta-analysis results displayed pooled prevalence of osteoporosis of 18.0% (10.1%–25.8%) in total sample, 7.7% (5.7%–9.7%) in men and 22.4% (17.1%–27.6%) in women. Multivariable logistic regression models showed that ageing, women, low education level or income, drinking or underweight was related to increased risk for osteopenia or osteoporosis.
Conclusions
About one-sixth of the participants suffered osteoporosis in rural China, and the prevalence in women was higher than men. Although the results were lower than that of meta-analysis, osteoporosis still accounts for huge burden of disease in rural population due to limited medical service and lack of health risk awareness rather than urban area.
Trial registration number
Chinese Clinical Trial Registry (ChiCTR-OOC-15006699; Pre-results).
Keywords: osteoporosis, osteopenia, prevalence, influencing factor, rural population
Strengths and limitations of this study.
This is the first study combining epidemiological survey and meta-analysis to analyse the prevalence of osteopenia and osteoporosis in Chinese rural area, and furthermore exploring related influencing factors.
Wide range of covariates were controlled to guarantee the reliability of the analysis.
The bone mineral density of the calcaneus was measured using an ultrasonic bone density apparatus (Hologic Sahara, America), a low-cost, radiation-free and more applicative measurement in the large epidemiological field investigations.
Since the present study was a cross-sectional design, a causal relationship between osteoporosis and risk factors cannot be made.
Introduction
Osteoporosis, as presenting low bone mass, structural deterioration and porous bone characteristics, is associated with skeletal fragility and increased risk of fracture.1 Osteoporosis has become an important public health problem along with an increased ageing population and longer life expectancy. According to the National Health and Nutrition Examination Survey, prevalence of osteoporosis and low bone mass in the USA adults aged ≥50 years in 2013–2014 were ranged from 6% to 11% and 28% to 45%, respectively.2 A meta-analysis that included 33 articles published from 2010 to 2016 on observational epidemiology studies in China reported that the total, men and women prevalence of osteoporosis at the age above 60 years was 36%, 23% and 49%, respectively.3 Osteoporosis is well known as the silent epidemic, because it does not manifest until a fracture occurs. For instance, a recent study indicated that prevalence of vertebral fractures is 18%–26%, 20%–24%, 11%–19% and 9%–24% in European women, North American white women ≥50, Latin American women ≥50 years and Asian women above ≥65, respectively.4 It is predicted that the annual number of osteoporosis-related fractures will increase to 5.99 million by 2050 in China.5
Osteoporosis has been associated with increased mortality and decreased health-related quality of life.6–8 Results from the National Health Insurance Research Database show that the annual direct medical costs of osteoporosis patients increased steadily in Taiwan from 2009 to 2013.9 It is predicted that by 2050 the annual costs of osteoporosis-related fractures will increase to $25.43 billion in China.5
With increasing in elderly population, osteoporosis and subsequent fractures have become important health problems. Although few epidemiological studies were available to estimate the prevalence of osteoporosis in China, the data on prevalence of osteoporosis by gender in the rural areas are scarce. Thus, the objectives of this study were to estimate the prevalence of osteopenia and osteoporosis and investigate potential influencing factors by using baseline data from the Henan Rural Cohort Study and a meta-analysis in China countryside areas.
Methods
Study subjects
The study subjects were derived from the Henan Rural Cohort Study performed in the rural areas of Henan province from July 2015 to September 2017 which has been registered before the start of patient enrolment in the Chinese Clinical Trial Register. A multistage, stratified cluster sampling method was used to select samples. Among 39 259 participants aged 18–79 years old, 8475 subjects who completed BMD measurement were included for the present study.
Assessment of bone mineral density
The bone mineral density (BMD, g/cm2) of the calcaneus was measured three times by the same investigator using an ultrasonic bone density apparatus (Hologic Sahara, America), a practical and reliable tool for detecting osteoporosis.10 The Sahara is a portable, dry ultrasound system using an oil-based couplant (gel) that measures the speed of sound (SOS) (coefficient of variation (CV) 0.22%) and broadband ultrasound attenuation (BUA) (CV 3.7%). BUA and SOS are combined linearly to form the quantitative ultrasound (QUS) index (CV 2.6%), which is used to obtain an estimate of the heel BMD in g/cm2 (CV 3%). The BMD T-score was calculated from the manufacturer-provided reference data, which was derived from a database of young healthy Chinese individuals, and the average of the three readings was taken for analysis. The diagnosis of osteoporosis/osteopenia was done according to T-score values: normal, T-score ≥−1.0; osteopenia, −2.5<T-score<−1.0; osteoporosis, T-score ≤−2.5.11
Assessment of potential covariates
The information on demographic, socioeconomic and lifestyle factors (eg, smoking, alcohol drinking, diet, physical activity levels and medical history) was collected through a face-to-face interview by trained research staff using a standardised questionnaire. Education level was classified into three categories: elementary school or below, junior high school and high school or above. According to the smoking index of the WHO,12 smoking status was grouped into never smoking, light smoking, moderate smoking and heavy smoking. In accordance with the daily alcohol intake of WHO and the dietary guidelines for Chinese residents,12 13 drinking was divided into four categories: never drinking, light drinking, moderate drinking and heavy drinking. High-fat diet was defined as a person who took an average of more than 75 g meat of livestock and poultry per day, and adequate vegetable and fruit intake was considered as a person who consumed an average of more than 500 g vegetable and fruit per day in accordance with the dietary guidelines for Chinese residents.13 Physical activity was grouped into low, moderate and high level, based on the International Physical Activity Questionnaire (2001).14
While the subjects wore light clothing and without shoes, hats and coats, their weights and heights were measured twice with a weight measurement device (V. BODY HBF-371, OMRON, Japan) and a standard right-angle device and a fixed measurement tape following a standardised protocol,15 and the reading was taken to the nearest 0.1 kg and 0.1 cm, respectively. The body mass index (BMI) was calculated as the weight (kg) divided by the square of the height (m). According to the criteria recommended by Working Group on Obesity in China,16 participants were categorised into four BMI groups: underweight, BMI<18.5 kg/m2; normal weight, BMI<24.0 kg/m2; overweight, 24.0 kg/m2≤BMI < 28.0 kg/m2 and general obesity, BMI≥28.0 kg/m2.
Meta-analysis
A meta-analysis of the prevalence of osteoporosis was also performed following the PRISMA statement17 in the present study. Relevant studies were searched in PubMed, Web of Science, CNKI (Chinese) and Wanfang (Chinese) databases for all articles published up to September 2018 which reported on the prevalence of osteoporosis among Chinese. The search terms were as follows: ‘osteoporosis or bone density or bone diseases’, ‘prevalence or epidemiology’, ‘China or Chinese’, ‘rural or countryside’, and these terms’ derivation and combinations. Detailed search strategies were presented in online supplementary table S1. At the same time, the reference lists of original and review articles were also researched to identify any additional relevant articles using the previous databases. Articles were included if they met the following criteria: (1) the participants of studies were from Chinese general population and (2) the study reported the sample size and the prevalence of osteoporosis in a rural area. The exclusion criteria were as follows: (1) concentrating on special population (such as children and pregnant women); (2) the study was based on population from foreign countries; (3) the participants were from an urban population; (4) having duplicated data and (5) reviews or editorials. Two investigators independently extracted information from the studies, including the first author, year of publication, study location, sample size, age range and prevalence of osteoporosis for the total sample and by gender in the rural areas. Moreover, any disagreements were resolved by discussion from literature search, inclusion, exclusion to data extraction process. A random-effects test was performed in accordance with the result of I2 statistic (I2 >50%).18 In addition, Begg’s and Egger’s tests were conducted to examine potential publication bias.
bmjopen-2018-028593supp001.pdf (61.1KB, pdf)
Statistical analysis
Participants were divided into normal, osteopenia and osteoporosis in a manner independent on gender. Characteristics of the participants were described as numbers (percentages) for categorical variables, and mean±SD or median and IQR for continuous variables. Differences in the characteristics of participants were determined with χ2 test for categorical variables and one-way ANOVA variance for continuous variables. The age-standardised prevalence of osteoporosis was calculated according to data from the sixth census in China. Multivariable logistic regression models were used to examine the associations between factors and osteoporosis and osteopenia based on OR and 95% CIs.
Statistical analyses were performed using SPSS software V.21.0. Meta-analysis was conducted using Stata software, V.11.0. All statistical tests were two-sided, and p<0.05 was considered statistically significant.
Results
Demographic characteristics
The demographic characteristics of the 8475 participants aged 18–79 years old were presented in table 1. Overall, a total of 1648 and 934 were diagnosed with osteopenia and osteoporosis in men, and 2123 and 982 were diagnosed with osteopenia and osteoporosis in women, respectively. The mean BMD were 0.42 and 0.32 g/cm2 for participants with osteopenia and osteoporosis in men (p<0.001), and the counterpart in women was 0.40 and 0.30 g/cm2 (p<0.001), respectively. The osteoporosis group was significantly older than the osteopenia and normal groups whether in men or women (p<0.001). At the same time, lower education level and lower high-fat diet were more common among osteoporosis group, while married/cohabitating and higher BMI were more prevalent among normal group. Furthermore, in men, the proportion of average monthly individual income <500 RMB was higher in osteoporosis group than the osteopenia and normal groups while never smoking cigarette was lower.
Table 1.
Demographic characteristics of the participants
| Characteristics | Men (n=3423) | Women (n=5052) | ||||||
| Normal (n=1381) |
Osteopenia (n=1648) |
Osteoporosis (n=394) |
P value | Normal (n=1938) |
Osteopenia (n=2132) |
Osteoporosis (n=982) |
P value | |
| Age (mean±SD) | 54.44±11.83 | 56.17±11.31 | 59.27±10.53 | <0.001 | 51.00±11.12 | 54.65±11.14 | 59.05±10.80 | <0.001 |
| Marital status, n (%) | 0.002 | <0.001 | ||||||
| Married/cohabitating | 1283 (92.90) | 1509 (91.57) | 344 (87.31) | 1810 (93.40) | 1932 (90.62) | 858 (87.37) | ||
| Unmarried/divorced /widowed |
98 (7.10) | 139 (8.43) | 50 (12.69) | 128 (6.60) | 200 (9.38) | 124 (12.63) | ||
| Education level, n (%) | <0.001 | <0.001 | ||||||
| Elementary school or below | 355 (25.71) | 558 (33.86) | 154 (39.09) | 810 (41.80) | 1131 (53.05) | 644 (65.58) | ||
| Junior high school | 593 (42.94) | 738 (44.78) | 171 (43.40) | 754 (38.91) | 751 (35.23) | 253 (25.76) | ||
| High school or above | 433 (31.35) | 352 (21.36) | 69 (17.51) | 374 (19.30) | 250 (11.73) | 85 (8.66) | ||
| Average monthly individual income, n (%) | <0.001 | 0.241 | ||||||
| <500 RMB | 416 (30.12) | 607 (36.83) | 155 (39.34) | 643 (33.18) | 720 (33.77) | 362 (36.86) | ||
| 500–1000 RMB | 401 (29.04) | 465 (28.22) | 128 (32.49) | 626 (32.30) | 655 (30.72) | 286 (29.12) | ||
| ≥1000 RMB | 564 (40.84) | 576 (34.95) | 111 (28.17) | 669 (34.52) | 757 (35.51) | 334 (34.01) | ||
| Smoking, n (%) | 0.009 | 0.728 | ||||||
| Never | 486 (36.56) | 499 (31.68) | 116 (30.61) | 1894 (99.79) | 2057 (99.66) | 947 (99.47) | ||
| Light | 173 (13.05) | 210 (13.33) | 40 (10.55) | 2 (0.11) | 4 (0.19) | 3 (0.32) | ||
| Moderate/heavy | 667 (50.30) | 866 (54.98) | 223 (58.84) | 2 (0.11) | 3 (0.15) | 2 (0.21) | ||
| Drinking, n (%) | 0.987 | 0.205 | ||||||
| Never | 622 (46.91) | 741 (47.05) | 175 (46.17) | 1853 (97.63) | 2006 (97.16) | 924 (97.06) | ||
| Light | 409 (30.84) | 495 (31.43) | 120 (31.66) | 40 (2.11) | 45 (2.18) | 19 (2.00) | ||
| Moderate/heavy | 295 (22.25) | 339 (21.52) | 84 (22.16) | 5 (0.26) | 13 (0.63) | 9 (0.95) | ||
| Physical activity, n (%) | <0.001 | <0.001 | ||||||
| Low | 538 (38.96) | 515 (31.25) | 124 (31.47) | 674 (34.78) | 533 (25.00) | 262 (26.68) | ||
| Moderate | 393 (28.46) | 447 (27.12) | 111 (28.17) | 787 (40.61) | 898 (42.12) | 362 (36.86) | ||
| High | 450 (32.59) | 686 (41.63) | 159 (40.36) | 477 (24.61) | 701 (32.88) | 358 (36.46) | ||
| High-fat diet, n (%) | 347 (25.13) | 432 (26.21) | 84 (21.32) | 0.132 | 310 (16.00) | 341 (15.99) | 122 (12.42) | 0.02 |
| More vegetables and fruits intake, n (%) | 656 (47.50) | 869 (52.73) | 195 (49.49) | 0.016 | 963 (49.69) | 1139 (53.42) | 440 (44.81) | <0.001 |
| BMI (kg/m2) (mean±SD) | 25.25±3.33 | 24.40±3.40 | 23.02±3.26 | <0.001 | 25.36±3.58 | 24.68±3.43 | 24.18±3.57 | <0.001 |
| BMD (g/cm2) (mean±SD) | 0.55±0.08 | 0.42±0.05 | 0.32±0.08 | <0.001 | 0.52±0.09 | 0.40±0.06 | 0.30±0.08 | <0.001 |
| T-score (mean±SD) | −0.13±0.73 | −1.72±0.41 | −2.87±0.34 | <0.001 | 0.07±0.88 | −1.75±0.42 | −2.97±0.38 | <0.001 |
BMI, body mass index; BMD, bone mineral density.
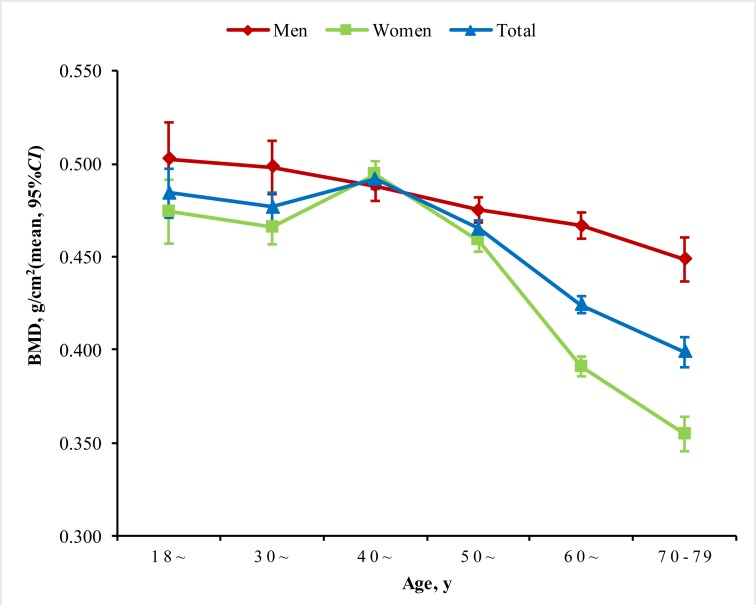
Figure 1 displays the gender-specific distributions of BMD according to age. The age-adjusted mean levels (95% CI) of BMD were 0.47 (0.47–0.48) g/cm2 and 0.44 (0.43–0.44) g/cm2 for men and women (p<0.001), respectively. In general, the mean values of BMD declined significantly along with the increase of age both in men and in women (p trend <0.001), and men had higher gender-specific mean levels of BMD than women.
Figure 1.
Mean of bone mineral density (BMD) according to age error bars indicates 95% CIs and it was adjusted for age and gender in total population.
Prevalence of osteopenia and osteoporosis
In this study, the overall crude prevalence of osteopenia and osteoporosis were 44.60% (43.54%–45.66%) and 16.24% (15.45%–17.02%), and the corresponding age-standardised rates were 42.09% (41.04%–43.14%) and 11.76% (11.07%–12.45%), respectively. The crude prevalence of osteopenia in men was 48.14% (48.13%–48.15%) which was significantly higher than that for women, 42.20% (42.19%–42.21%) (p<0.001). However, the crude prevalence of osteoporosis in men was 11.51% (11.51%–11.51%) which was significantly lower than that in women, 19.44% (19.44%–19.44%) (p<0.001). The age-standardised prevalence of osteopenia and osteoporosis were 45.98% (44.92%–47.04%) vs 39.73% (38.69%–40.77%) and 7.82% (7.25%–8.39%) vs 14.38% (13.63%–15.13%) for men and women (p<0.001), respectively. The prevalence of osteopenia in men was significantly higher than women; on the contrary, the prevalence of osteoporosis in men was significantly lower than women in all demographic characteristics and lifestyle strata.
Subgroups study showed that men participants with older age, unmarried/divorced/widowed, lower education level, lower per capita monthly income, smoking, high-fat diet and inadequate vegetable and fruit intake were predisposed to having osteopenia and osteoporosis. Among women, participants with older age, unmarried/divorced/widowed, lower education level, high-fat diet, and inadequate vegetable and fruit intake showed higher prevalence of osteopenia and osteoporosis (table 2). The trend χ2 test showed that the tendency of prevalence of osteopenia and osteoporosis were increased with ageing, smoking state and higher physical activity but decreased with higher education level and per capita monthly income in men, similar results were observed in women apart from average monthly individual income and smoking state.
Table 2.
Prevalence and 95% CI of osteopenia and osteoporosis in men and women stratified by the various predictor variables (n=8475)
| Characteristics | Men | Women | ||||
| Osteopenia (n=1648) |
Osteoporosis (n=394) |
P value | Osteopenia (n=2132) |
Osteoporosis (n=982) |
P value | |
| Total | 48.14 (48.13 to 48.15) | 11.51 (11.51,11.51) | 42.20 (42.19 to 42.21) | 19.44 (19.44,19.44) | ||
| Age | <0.001 | <0.001 | ||||
| 18~ | 44.30 (43.99 to 44.61) | 2.53 (2.50 to 2.56) | 36.00 (35.85 to 36.15) | 9.33 (9.27 to 9.39) | ||
| 30~ | 42.40 (42.29 to 42.51) | 5.99 (5.96 to 6.02) | 40.69 (40.63 to 40.75) | 9.80 (9.78 to 9.82) | ||
| 40~ | 46.48 (46.44 to 46.52) | 8.70 (8.69 to 8.71) | 37.32 (37.30 to 37.34) | 11.67 (11.66 to 11.68) | ||
| 50~ | 50.88 (50.86 to 50.90) | 10.90 (10.89 to 10.91) | 44.18 (44.17 to 44.19) | 15.80 15.79 to 15.81) | ||
| 60~ | 47.90 (47.88 to 47.92) | 12.62 (12.61 to 12.63) | 44.45 (44.43 to 44.47) | 28.26 (28.25 to 28.27) | ||
| 70~79 | 48.48 (48.42 to 48.54) | 19.70 (19.66 to 19.74) | 42.82 (42.77 to 42.87) | 37.36 (37.31 to 37.41) | ||
| Ptrend | <0.001 | <0.001 | <0.001 | <0.001 | ||
| Marital status | 0.002 | <0.001 | ||||
| Married/cohabitating | 48.12 (48.11 to 48.13) | 11.00 (11.00 to 11.00) | 42.00 (41.99 to 42.01) | 18.65 (18.65 18.65) | ||
| Unmarried/divorced /widowed |
48.43 (48.34 to 48.52) | 17.42 (17.37 to 17.47) | 44.25 (44.20 to 44.30) | 27.43 (27.39 to 27.47) | ||
| Education level | <0.001 | <0.001 | ||||
| Elementary school or below | 52.30 (52.28 to 52.32) | 14.43 (14.42 to 14.44) | 43.75 (43.74 to 43.76) | 24.91 (24.90 to 24.92) | ||
| Junior high school | 49.13 (49.11 to 49.15) | 11.38 (11.37 to 11.39) | 42.72 (42.71 to 42.73) | 14.39 (14.38 to 14.40) | ||
| High school or above | 41.22 (41.19 to 41.25) | 8.08 (8.07 to 8.09) | 35.26 (35.23 to 35.29) | 11.99 (11.98 to 12.00) | ||
| Ptrend | <0.001 | <0.001 | <0.001 | <0.001 | ||
| Average monthly individual income | <0.001 | 0.241 | ||||
| <500 RMB | 51.53 (51.51 to 51.55) | 13.16 (13.15 to 13.17) | 41.74 (41.73 to 41.75) | 20.99 (20.98 to 21.00) | ||
| 500–1000 RMB | 46.78 (46.76 to 46.80) | 12.88 (12.87 to 12.89) | 41.80 (41.78 to 41.82) | 18.25 (18.24 to 18.26) | ||
| ≥1000 RMB | 46.04 (46.02 to 46.06) | 8.87 (8.86 to 8.88) | 43.01 (43.00 to 43.02) | 18.98 (18.97 to 18.99) | ||
| Ptrend | <0.001 | <0.001 | 0.879 | 0.197 | ||
| Smoking | 0.009 | 0.728 | ||||
| Never | 50.66 (47.53 to 53.79) | 19.27 (16.11 to 22.43) | 52.06 (50.50 to 53.62) | 33.33 (31.60 to 35.07) | ||
| Light | 54.83 (49.82 to 59.84) | 18.78 (13.49 to 24.07) | 66.67 (12.47 to 120.86) | 60.00 (-8.01 to 128.01) | ||
| Moderate/heavy | 56.49 (54.01 to 58.98) | 25.06 (22.20 to 27.91) | 60.00 (-8.01 to 128.01) | 50.00 (-41.87 to 141.87) | ||
| Ptrend | 0.005 | 0.007 | 0.513 | 0.218 | ||
| Drinking | 0.987 | 0.205 | ||||
| Never | 54.37 (51.72 to 57.01) | 21.96 (19.08 to 24.84) | 51.98 (50.41. 53.56) | 33.27 (31.52 to 35.03) | ||
| Light | 54.76 (51.51 to 58.01) | 22.68 (19.10 to 26.26) | 52.94 (42.11 to 63.77) | 32.20 (19.92 to 44.48) | ||
| Moderate/heavy | 53.47 (49.58 to 57.36) | 22.16 (17.96 to 26.36) | 72.22 (49.30 to 95.14) | 64.29 (35.58 to 93.00) | ||
| Ptrend | 0.770 | 0.888 | 0.198 | 0.112 | ||
| Physical activity | <0.001 | <0.001 | ||||
| Low | 43.76 (43.74 to 43.780 | 10.53 (10.52 to 10.54) | 36.28 (36.26 to 36.30) | 17.84 (17.83 to 17.85) | ||
| Moderate | 47.00 (46.97 to 47.03) | 11.67 (11.66 to 11.68) | 43.87 (43.86 to 43.88) | 17.68 (17.67 to 17.69) | ||
| High | 52.97 (52.95 to 52.99) | 12.28 (12.27 to 12.29) | 45.64 (45.62 to 45.66) | 23.31 (23.30 to 23.32) | ||
| Ptrend | <0.001 | 0.002 | <0.001 | <0.001 | ||
| High-fat diet | 50.06 (50.03 to 50.09) | 9.73 (9.72 to 9.74) | 0.132 | 44.11 (44.08 to 44.14) | 15.78 (15.76 to 15.80) | 0.020 |
| More vegetables and fruits intake | 50.52 (48.16 to 52.89) | 11.34 (9.84 to 12.84) | 0.016 | 44.81 (44.80 to 44.82) | 17.31 (17.30 to 17.32) | <0.001 |
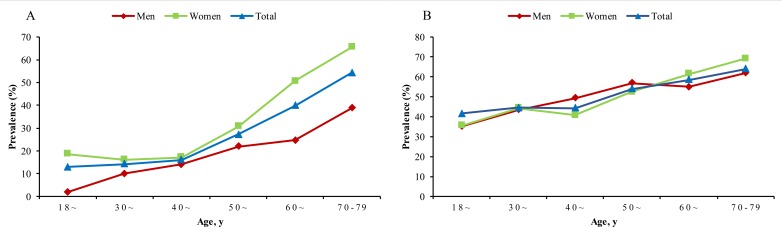
The age-standardised prevalence of osteoporosis among men and women showed increasing trend with age groups (Ptrend <0.0001), particularly after the age of 40 years in women and 60 years in men (figure 2A), and women had higher prevalence than men did in all age groups. With regards osteopenia, men had higher age-standardised prevalence of osteopenia than women at age of 40–59 group, but lower prevalence in younger and older age groups (figure 2B).
Figure 2.
The age-standardised prevalence of osteoporosis (A) and osteopenia (B) between different age groups and gender.
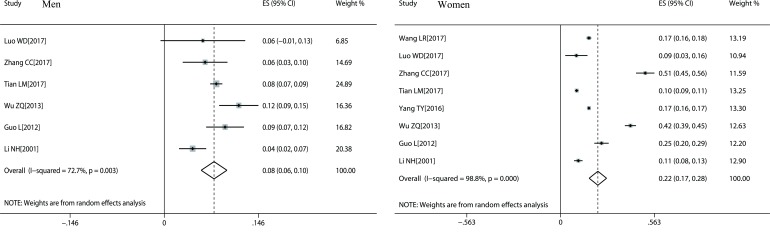
Meta-analysis
According to our inclusion and exclusion criteria, a total of eight studies were enrolled in the meta-analysis, and the details were shown in online supplementary figure S1 and online supplementary table S2. Six studies19–24 contained the prevalence of osteoporosis in total sample, men and women, while two studies25 26 reported the prevalence of osteoporosis only in women. The pooled prevalence of osteoporosis in the total sample was 18.0% (10.1%–25.8%), and the pooled prevalence of men and women were 7.7% (5.7%–9.7%) and 22.4% (17.1%–27.6%), respectively (figure 3). There was obvious heterogeneity (I2 >50%), and publication bias was not found by the Begg’s and Egger’s tests (p>0.05).
Figure 3.
Forest plots of prevalence of osteoporosis of all selected studies.
Analysis of influencing factors
In the multivariate logistic regression models, subjects who were much older, low education level, low average monthly individual income and low BMI had a higher risk of osteopenia and osteoporosis (table 3). In addition, women who had moderate/heavy drinking were 3.95 times more likely to suffer from osteoporosis, and who had adequate vegetable and fruit intake had a higher risk of osteopenia.
Table 3.
Association between potential risk factors and osteopenia and osteoporosis
| Variable | Men | Women | ||
| Osteopenia (n=1648) |
Osteoporosis (n=394) |
Osteopenia (n=2132) |
Osteoporosis (n=982) |
|
| Age | ||||
| 18– | 1.00 | 1.00 | 1.00 | 1.00 |
| 40– | 1.08 (0.79 to 1.48) | 1.57 (0.82 to 2.99) | 0.88 (0.69 to 1.13) | 1.15 (0.77 to 1.70) |
| 50– | 1.49 (1.11 to 2.01) | 2.37 (1.28 to 4.36) | 1.35 (1.07 to 1.70) | 2.13 (1.48 to 3.07) |
| 60– | 1.13 (0.84 to 1.54) | 1.99 (1.07 to 3.70) | 1.95 (1.51 to 2.51) | 5.02 (3.42 to 7.37) |
| 70–79 | 1.32 (0.91 to 1.92) | 3.52 (1.80 to 6.87) | 2.67 (1.88 to 3.80) | 9.77 (6.15 to 15.50) |
| Ptrend | 0.249 | <0.001 | <0.001 | <0.001 |
| Marital status | ||||
| Married/cohabiting | 1.00 | 1.00 | 1.00 | 1.00 |
| Widowed/single /divorced/separation |
1.14 (0.85 to 1.53) | 1.48 (0.97 to 2.27) | 1.16 (0.90 to 1.50) | 1.07 (0.79 to 1.45) |
| Education level | ||||
| Elementary school or below | 1.00 | 1.00 | 1.00 | 1.00 |
| Junior high school | 0.80 (0.67 to 0.96) | 0.84 (0.63 1.12) | 0.52 (0.42 to 0.65) | 0.61 (0.50 to 0.75) |
| High school or above | 0.55 (0.44 to 0.68) | 0.65 (0.45 to 0.95) | 1.16 (0.90 to 1.50) | 0.49 (0.36 to 0.68) |
| Ptrend | <0.001 | 0.021 | <0.001 | <0.001 |
| Average monthly individual income | ||||
| <500 RMB | 1.00 | 1.00 | 1.00 | 1.00 |
| 500–1000 RMB | 0.83 (0.69 to 1.01) | 1.01 (0.75 to 0.36) | 1.04 (0.89 to 1.23) | 1.04 (0.84 to 1.29) |
| ≥1000 RMB | 0.78 (0.65 to 0.95) | 0.71 (0.52 to 0.97) | 1.20 (1.02 to 1.41) | 1.35 (1.09 to 1.68) |
| Ptrend | 0.010 | 0.030 | 0.041 | 0.014 |
| Smoking | ||||
| Never | 1.00 | 1.00 | 1.00 | 1.00 |
| Light | 1.21 (0.94 to 1.56) | 1.12 (0.72 to 1.73) | 1.59 (0.26 to 9.86) | 2.65 (0.37 to 19.00) |
| Moderate/heavy | 1.14 (0.96 to 1.36) | 1.16 (0.87 to 1.54) | 0.94 (0.14 to 6.38) | 1.26 (0.10 to 15.82) |
| Ptrend | 0.068 | 0.204 | 0.860 | 0.574 |
| Drinking | ||||
| Never | 1.00 | 1.00 | 1.00 | 1.00 |
| Light | 1.074 (0.90 to 1.29) | 1.25 (0.93 to 1.68) | 1.01 (0.65 to 1.58) | 0.78 (0.42 to 1.47) |
| Moderate/heavy | 1.047 (0.85 to 1.29) | 1.40 (0.99 to 1.95) | 2.15 (0.74 to 6.21) | 3.95 (1.24 to 12.63) |
| Ptrend | 0.699 | 0.073 | 0.269 | 0.210 |
| Physical activity | ||||
| Low | 1.00 | 1.00 | 1.00 | 1.00 |
| Moderate | 1.14 (0.94 to 1.38) | 1.26 (0.92 to 1.74) | 1.42 (1.21 to 1.66) | 1.33 (1.06 to 1.65) |
| High | 1.54 (1.28 to 1.84) | 1.56 (1.17 to 2.10) | 2.00 (1.68 to 2.38) | 2.45 (1.95 to 3.09) |
| Ptrend | <0.001 | 0.005 | <0.001 | <0.001 |
| High-fat diet | 1.18 (0.99 to 1.42) | 1.01 (0.74 to 1.37) | 1.11 (0.92 to 1.33) | 0.95 (0.73 to 1.23) |
| More vegetables and fruits intake | 1.17 (1.01 to 1.36) | 0.94 (0.74 to 1.21) | 1.19 (1.04 to 1.36) | 0.84 (0.71 to 1.01) |
| BMI group | ||||
| Underweight | 2.01 (1.13 to 3.58) | 3.18 (1.63 to 6.21) | 2.31 (1.31 to 4.07) | 2.19 (1.12 to 4.30) |
| Normal | 1.00 | 1.00 | 1.00 | 1.00 |
| Overweight | 0.72 (0.61 to 0.85) | 0.40 (0.30 to 0.53) | 0.70 (0.60 to 0.81) | 0.48 (0.40 to 0.59) |
| Obesity | 0.71 (0.56 to 0.88) | 0.31 (0.20 to 0.49) | 0.57 (0.47 to 0.69) | 0.36 (0.28 to 0.46) |
| Ptrend | <0.001 | <0.001 | <0.001 | <0.001 |
BMI, body mass index.
Discussion
To the best of our knowledge, this is the first study that combined meta-analysis with cross-sectional study to report the prevalence rate of osteopenia and osteoporosis in Chinese rural population. The major findings are as follows: first, about a half of the adult population had osteopenia, while one-sixth of the rural adult population in China had osteoporosis. Second, the crude prevalence of osteopenia in men was significantly higher than that in women (p<0.001), on the contrary the crude prevalence of osteoporosis in men was lower than women (p<0.001). In addition, the crude prevalence rates of osteoporosis were slightly lower than the results of the meta-analysis except for that in men. Subjects who were much older, low level of education, low average monthly individual income and low BMI had a higher risk of osteopenia and osteoporosis.
This large study provides important new evidence about the current prevalence and burden of osteoporosis in the rural area of China. A study conducted in Jiangxi urban population among participants aged 16–93 reported the prevalence of osteoporosis as 16.1% in men and 20.8% in women in 2014,27 which is consistent with our findings. The prevalence rate of osteoporosis reported in previous studies about Italian general population was 18.1%,28 which is a little bit higher than the present results. However, a higher prevalence of osteoporosis and osteopenia among postmenopausal women has been observed in Jordan which was 37.5% and 44.6%, respectively.29 Geographic setting, socioeconomic level and lifestyle might partly contribute to this phenomenon. In addition, differences in the prevalence of osteoporosis of total sample (16.24% vs 18.0%), men (11.51% vs 7.7%) and women (19.44% vs 22.4%) were found between the present study and meta-analysis. There might be some potential reasons for the phenomenon, such as age structure and economic level of participants. The age range of participants was 18–79 years in the Henan Rural Cohort study, while the age of participants in studies included in the meta-analysis was mostly above 40 years old. In addition, the samples of the Henan Rural Cohort study were from five counties with higher economic level and living standard.
In general, the mean values of BMD declined significantly along with increase of age in both genders. A previous study has declared that the prevalence of osteoporosis was higher in women than men.30 Similar results were found in our study. The crude prevalence of osteopenia and osteoporosis in men and women were 48.14% vs 42.20% and 11.51% vs 19.44%, respectively. Further study showed that there were different trend changes in the prevalence of osteopenia and osteoporosis in men and women. In general, the age-standardised prevalence of osteoporosis among men and women increased with age groups, particularly after the age of 40 years in women and 60 years in men, and women had higher prevalence than men did in all age ranges. Men had obviously higher age-standardised prevalence of osteopenia than women at age 40–59 group, but lower prevalence in younger and older age group. That is to say, women, especially older women, are more likely to develop osteoporosis.
Our research demonstrated that higher education level and average monthly individual income could decrease the odds of osteoporosis and osteopenia in both genders. The association between education level, income and osteoporosis had also been found consistent with previous research.31 High education level and income might indicate higher socioeconomic status that demonstrated less probability of osteoporosis.32 Furthermore, the present study indicated that participants with higher BMI were less likely to have osteoporosis (obesity was negatively correlated with osteoporosis), and similar results were also reported in previous studies.33–36 It should be noted that a previous study has shown that the beneficial effect on BMD of increasing BMI exists up to 35 kg/m2, and a BMI higher than 35 kg/m2 is not associated with further increase in BMD.37 Differences in prevalence of osteoporosis and osteopenia between men and women may be attributed to difference in hormone levels: increased bone loss in women with sudden changes in hormone levels before and after menopause. Moreover, a multiple logistic regression analysis showed that moderate/heavy drinking in women also increased the risk of osteoporosis. By altering the structure of cell membranes, ethanol may non-selectively disrupt a multitude of regulatory pathways in bone cells; chronic heavy alcohol consumption is associated with decreased BMD.38 In addition, higher physical activity showed a higher risk of osteoporosis and in women adequate vegetable and fruit intake showed a higher risk of osteopenia, which was inconsistent with previous studies.39–41 This may be due to limitation of cross-sectional design, so further studies are needed.
This is the first study combining epidemiological survey and meta-analysis to analyse the prevalence of osteopenia and osteoporosis in Chinese rural area, and furthermore exploring related influencing factors. What is more, a wide range of covariables were controlled to guarantee the reliability of the analysis. We believe that our conclusions can provide the latest evidence for the development of effective national prevention and control programmes for osteoporosis and osteopenia management to reduce the development of osteoporosis-related fracture in areas with limited resources. Nevertheless, several limitations also warrant consideration. First, since the present study was a cross-sectional design, a causal relationship between osteoporosis and risk factors cannot be made. Second, the BMD of the calcaneus was measured using an ultrasonic bone density apparatus (Hologic Sahara, America). Although the accuracy of ultrasonic measurement is limited, it can reflect the BMD of the study subjects to some extent, which is acceptable in the epidemiological investigation of large samples and can be used for the screening of osteoporosis. Furthermore, previous study indicated that there was no significant difference between the QUS and X-ray densitometric BMD methods in separating normal from osteoporotic subjects when using receiver operating characteristic analysis.42 In addition, other studies43–45 have also clarified that the ability of low bone mass (measured by calcaneal ultrasound) to predict future fracture risk is equivalent to dual energy X-ray absorptiometry. Besides, the same method has been applied in an elderly Chinese population46 and in some large studies.47 48 Therefore, diagnostic cut-off points of −1.0 and −2.5 may be applicative. Moreover, in the studies included in the meta-analysis, the BMD measurement sites and the measurement methods were different. However, because of the insufficient number of studies included, subgroup analysis was not performed. We just combined multiple research results by performing a random-effects model. This is also a limitation of this study.
In conclusion, about half of the participants had osteopenia and one-sixth of the participants had osteoporosis in the general population living in rural area of China. The prevalence of osteoporosis in women was higher than men. Although the results were lower than that of meta-analysis, osteoporosis still accounts for huge burden of disease in rural population due to limited medical service and lack of health risk awareness rather than urban area. Therefore, effective measures are needed to prevent and control high risk factors in the population, particularly in older females in rural areas of China.
Supplementary Material
Acknowledgments
The authors thank all of the participants, coordinators and administrators for their support and help during the research. In addition, the authors would like to thank Tanko Abdulai for his critical reading of the manuscript.
Footnotes
Contributors: CW and JP conceived and designed the experiments. DQ, XTL, RT, XZ and XQ performed and conducted the experiments. DQ, HZ, JJ, ZT and GZ analysed the data and took responsibility for the integrity and accuracy of the information. YW, XD, ZL, XL, HT and GZ contributed to the reagents/materials/analysis tools. DQ and XZ drafted and revised the manuscript. All authors have approved the final manuscript.
Funding: This research was supported by the National Key Research and Development Program of China (Grant No: 2016YFC0900803), National Natural Science Foundation of China (Grant No: 81573243, 81602925), Henan Provincial Science Fund for Distinguished Young Scholars (Grant No: 164100510021), Science and Technology Innovation Talents Support Plan of Henan Province Colleges and Universities (Grant No: 14HASTIT035), High-level Personnel Special Support Project of Zhengzhou University (Grant No: ZDGD13001). The funders had no role in the study design, data collection and analysis, decision to publish or preparation of the manuscript.
Competing interests: None declared.
Patient consent for publication: Not required.
Ethics approval: Ethics approval was obtained from the
‘Zhengzhou University Life Science Ethics Committee’, and written informed consent was obtained for all participants. Ethic approval code: [2015] MEC (S128).
The present study was conducted according to the Declaration of Helsinki on research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data are available upon reasonable request. The data sets used and analysed during the current study are available from the corresponding author on reasonable request.
References
- 1. Johnell O, Kanis J. Epidemiology of osteoporotic fractures. Osteoporos Int 2005;16:S3–7 https://doi.org/ 10.1007/s00198-004-1702-6 [DOI] [PubMed] [Google Scholar]
- 2. Looker AC, Sarafrazi Isfahani N, Fan B, et al. Trends in osteoporosis and low bone mass in older US adults, 2005–2006 through 2013–2014. Osteoporos Int 2017;28:1979–88 https://doi.org/ 10.1007/s00198-017-3996-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. LY H, Sun Y, Yao WJ, et al. The prevalence rate of osteoporosis in the elderly in China between 2010 and 2016: a meta-analysis of single rate. Chin J Osteoporos 2016;22:1590–6. [Google Scholar]
- 4. Ballane G, Cauley JA, Luckey MM, et al. Worldwide prevalence and incidence of osteoporotic vertebral fractures. Osteoporos Int 2017;28:1531–42 https://doi.org/ 10.1007/s00198-017-3909-3 [DOI] [PubMed] [Google Scholar]
- 5. Si L, Winzenberg TM, Jiang Q, et al. Projection of osteoporosis-related fractures and costs in China: 2010–2050. Osteoporos Int 2015;26:1929–37 https://doi.org/ 10.1007/s00198-015-3093-2 [DOI] [PubMed] [Google Scholar]
- 6. Cosman F, de Beur SJ, LeBoff MS, et al. Clinician’s Guide to Prevention and Treatment of Osteoporosis. Osteoporos Int 2014;25:2359–81 https://doi.org/ 10.1007/s00198-014-2794-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kling JM, Clarke BL, Sandhu NP. Osteoporosis prevention, screening, and treatment: a review. Journal of Women's Health 2014;23:563–72. 10.1089/jwh.2013.4611 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Leslie WD, Morin SN. Osteoporosis epidemiology 2013: implications for diagnosis, risk assessment, and treatment. Curr Opin Rheumatol 2014;26:440–6. 10.1097/BOR.0000000000000064 [DOI] [PubMed] [Google Scholar]
- 9. Wang C-Y, Fu S-H, Yang R-S, et al. Age- and gender-specific epidemiology, treatment patterns, and economic burden of osteoporosis and associated fracture in Taiwan between 2009 and 2013. Arch Osteoporos 2017;12:92 10.1007/s11657-017-0385-5 [DOI] [PubMed] [Google Scholar]
- 10. Njeh CF, Boivin CM, Langton CM. The role of ultrasound in the assessment of osteoporosis: a review. Osteoporosis Int 1997;7:7–22 http://doi.org/ 10.1007/BF01623454 [DOI] [PubMed] [Google Scholar]
- 11. World Health Organization Assessment of fracture risk and its application to screening for postmenopausal osteoporosis. World Health Organ Tech Rep Ser 1994;843:1–129. [PubMed] [Google Scholar]
- 12. Ediriweera BR TS, Sir RD, Robin R. International guide for monitoring alcohol consumption and related harm (ed. World Health organization), Geneva 2000;51. [Google Scholar]
- 13. Chinese Nutrition Society The dietary guidelines for Chinese residents. Lhasa: The Tibet people's Publishing House, 2011: 198. [Google Scholar]
- 14. International physical activity questionnaire: short last 7 days self-administered format, 2005. Available: http://www.ipaq.ki.se/downloads.htm [Accessed 26 October 2015].
- 15. The WHO MONICA Project World health STAT quarterly Rapp trimest STAT sanit mond geographical variation in the major risk factors of coronary heart disease in men and women aged 35-64 year 1998:115–40. [PubMed]
- 16. Working Group on Obesity in China. The guidelines for prevention and control of overweight and obesity in Chinese adults. Acta nutrimenta sinica 2004;26:1–4. [Google Scholar]
- 17. Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol 2009;62:e1–34. 10.1016/j.jclinepi.2009.06.006 [DOI] [PubMed] [Google Scholar]
- 18. Higgins JPT, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med 2002;21:1539–58. 10.1002/sim.1186 [DOI] [PubMed] [Google Scholar]
- 19. Luo WD, Zhao G, Shu J, et al. Prevalence and correlation factors of osteoporosis in middle-aged and elderly people of Zhuang nationality in Yunnan based on a survey. Chinese General Practice 2017;20:912–7. [Google Scholar]
- 20. Zhang CC, XF J. Investigation of bone loss and osteoporosis in middle and old people. Clinical practice of integrated traditional Chinese and Western Medicine 2017;17:69–71. [Google Scholar]
- 21. Tian L, Yang R, Wei L, et al. Prevalence of osteoporosis and related lifestyle and metabolic factors of postmenopausal women and elderly men: a cross-sectional study in Gansu Province, northwestern of China. Medicine 2017;96:e8294 10.1097/MD.0000000000008294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. ZQ W, YF W, BJ H, et al. Prevalence rate of primary osteoporosis and related factors in 1263 middle aged and elderly people in Zhongshan area of Guangdong Province. Journal of New Chinese Medicine 2013;45:51–3. [Google Scholar]
- 23. Guo L. Survey on influential factors of bone mineral density in middle and elder persons living in Yi ethnic area of Liangshan. Clinical Focus 2012;27:474–6. [Google Scholar]
- 24. NH L, Zhang DX, Li E, et al. Study on prevalence rate of osteoporosis in middle-aged and elderly population in some parts of Huabei area in China. Chin Prev Med 2001;02:19–21. [Google Scholar]
- 25. Wang LR, Sun XY, Zhu RX, et al. Epidemiological investigation and analysis of women aged 40–55 years old with osteoporosis in Gansu Province. J Development Med 2017;5:164–7. [Google Scholar]
- 26. Yang TY. Prevalence and influencing factors of osteoporosis among rural women in minority regions of Guizhou Province. Chin J Public Health 2016;32:266–9. [Google Scholar]
- 27. Hu Y. Epidemiological study of bone mineral density in 4515 residents in Jinxian area of Jiangxi.. Jiangxi Medical Journal 2016;51:1013–5. [Google Scholar]
- 28. Cavalli L, Guazzini A, Cianferotti L, et al. Prevalence of osteoporosis in the Italian population and main risk factors: results of BoneTour campaign. BMC Musculoskelet Disord 2016;17:396 https://doi.org/ 10.1186/s12891-016-1248-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Hyassat D, Alyan T, Jaddou H, et al. Prevalence and risk factors of osteoporosis among Jordanian postmenopausal women attending the National center for diabetes, endocrinology and genetics in Jordan. Biores Open Access 2017;6:85–93. 10.1089/biores.2016.0045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Mengmeng Z, Yagang L, Ying L, et al. A study of bone mineral density and prevalence of osteoporosis in Chinese people of Han nationality from Changchun. Arch Osteoporos 2012;7:31–6 https://doi.org/ 10.1007/s11657-011-0066-8 [DOI] [PubMed] [Google Scholar]
- 31. Kim KH, Lee K, Ko Y-J, et al. Prevalence, awareness, and treatment of osteoporosis among Korean women: the fourth Korea National health and nutrition examination survey. Bone 2012;50:1039–47. 10.1016/j.bone.2012.02.007 [DOI] [PubMed] [Google Scholar]
- 32. Yoo JE, Park HS. Prevalence and associated risk factors for osteoporosis in Korean men. Arch Osteoporos 2018;;;13:88 20 https://doi.org/ 10.1007/s11657-018-0506-9 [DOI] [PubMed] [Google Scholar]
- 33. Saarelainen J, Kiviniemi V, Kröger H, et al. Body mass index and bone loss among postmenopausal women: the 10-year follow-up of the OSTPRE cohort. J Bone Miner Metab 2012;30:208–16 https://doi.org/ 10.1007/s00774-011-0305-5 [DOI] [PubMed] [Google Scholar]
- 34. Salamat MR, Salamat AH, Janghorbani M. Association between obesity and bone mineral density by gender and menopausal status. Endocrinol Metab 2016;31:547–58 https://doi.org/ 10.3803/EnM.2016.31.4.547 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Lloyd JT, Alley DE, Hawkes WG, et al. Body mass index is positively associated with bone mineral density in US older adults. Arch Osteoporos 2014;9:175 https://doi.org/ 10.1007/s11657-014-0175-2 [DOI] [PubMed] [Google Scholar]
- 36. Wu DY, Qiao D, Zhang X, et al. Lipid profiles as potential mediators linking body mass index to osteoporosis among Chinese adults: the Henan rural cohort study. Osteoporos Int 2019;30:1413–22. 10.1007/s00198-019-04878-y [DOI] [PubMed] [Google Scholar]
- 37. WW G, Wang HB, Sun P, et al. The relationship between bone mineral density and higher body mass index in medium-elderly men. Public Medical Forum Magazine 2015;19:4334–6. [Google Scholar]
- 38. Gaddini GW, Turner RT, Grant KA, et al. Alcohol: a simple nutrient with complex actions on bone in the adult skeleton. Alcohol Clin Exp Res 2016;40:657–71 https://doi.org/ 10.1111/acer.13000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Holm JP, Hyldstrup L, Jensen J-EB. Time trends in osteoporosis risk factor profiles: a comparative analysis of risk factors, comorbidities, and medications over twelve years. Endocrine 2016;54:241–55 https://doi.org/ 10.1007/s12020-016-0987-5 [DOI] [PubMed] [Google Scholar]
- 40. Ford MA, Bass MA, Turner LW, et al. Past and recent physical activity and bone mineral density in college-aged women. J Strength Cond Res 2004;18:405–9. 10.1519/13343.1 [DOI] [PubMed] [Google Scholar]
- 41. Qiu R, Cao W-T, Tian H-Y, et al. Greater intake of fruit and vegetables is associated with greater bone mineral density and lower osteoporosis risk in middle-aged and elderly adults. PLoS One 2017;12:e0168906 10.1371/journal.pone.0168906 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Guglielmi G, de Terlizzi F. Quantitative ultrasound in the assessment of osteoporosis. Eur J Radiol 2009;71:425–31 https://doi.org/ 10.1016/j.ejrad.2008.04.060 [DOI] [PubMed] [Google Scholar]
- 43. Pluijm SM, Graafmans WC, Bouter LM, et al. Ultrasound measurements for the prediction of osteoporotic fractures in elderly people. Osteoporos Int 1999;9:550–6. 10.1007/s001980050275 [DOI] [PubMed] [Google Scholar]
- 44. Hans D, Dargent-Molina P, Schott AM, et al. Ultrasonographic heel measurements to predict hip fracture in elderly women: the EPIDOS prospective study. The Lancet 1996;348:511–4. 10.1016/S0140-6736(95)11456-4 [DOI] [PubMed] [Google Scholar]
- 45. Mazess RB. Quantitative heel ultrasound as a predictor for osteoporosis. Med J Aust 2000;172:245 10.5694/j.1326-5377.2000.tb123930.x [DOI] [PubMed] [Google Scholar]
- 46. Tian Y, Shen L, Wu J, et al. Sleep duration and timing in relation to osteoporosis in an elderly Chinese population: a cross-sectional analysis in the Dongfeng-Tongji cohort study. Osteoporos Int 2015;26:2641–8. 10.1007/s00198-015-3172-4 [DOI] [PubMed] [Google Scholar]
- 47. Stiles VH, Metcalf BS, Knapp KM, et al. A small amount of precisely measured high-intensity habitual physical activity predicts bone health in pre- and post-menopausal women in UK Biobank. Int J Epidemiol 2017;46:1847–56. 10.1093/ije/dyx080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Li X, Qiao Y, Yu C, et al. Tea consumption and bone health in Chinese adults: a population-based study. Osteoporos Int 2019;30:333–41. 10.1007/s00198-018-4767-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2018-028593supp001.pdf (61.1KB, pdf)