Abstract
Objectives
To study the implementation, effects and costs of Break the Chains, a community-based HIV prevention campaign for men who have sex with men (MSM) in Switzerland, from March to May 2015, which aimed to reduce early HIV transmission by promoting the campaign message to adopt short-term risk reduction followed by HIV testing.
Design
Non-randomised evaluation and cost analysis.
Setting
Gay venues in 11 of 26 cantons in Switzerland and national online media campaign.
Participants
MSM in online surveys (precampaign n=834, postcampaign n=688) or attending HIV testing centres (n=885); campaign managers (n=9); and campaign staff (n=38) or further intermediaries (n=80) in an online survey.
Primary and secondary outcome measures
The primary outcome measure was the proportion of MSM at risk of HIV acquisition or transmission who adhered to the campaign message. Secondary outcomes were postcampaign test uptake, knowledge about HIV primary infection and sense of belonging to the gay community.
Results
Campaign staff estimated that they contacted 17 145 MSM in 11 cantons. Among 688 respondents to the postcampaign survey, 311 (45.2%) were categorised as MSM at risk. Of 402/688 (58.5%) MSM who had heard about Break the Chains 2015, MSM categorised as being at risk were less likely to report adherence to the campaign message than MSM not at risk (adjusted OR 0.24; 95% CI 0.14 to 0.42). Twenty per cent of MSM with a defined risk of HIV acquisition or transmission who adopted risk reduction declared having done so because of the campaign. Costs for one MSM at risk to adhere to the campaign message were estimated at USD purchasing power parity 36–55. The number of HIV tests in the month after the campaign was twice the monthly average.
Conclusion
Break the Chains increased HIV testing, implying that community-based campaigns are useful HIV prevention strategies for MSM. Additional interventions are needed to reach MSM at the highest risk of infection more effectively.
Keywords: HIV infection, men having sex with men, prevention, community-based campaign, cost analysis
Strengths and limitations of this study.
This study adds to a limited body of literature evaluating implementation, effects and costs of multicomponent, community-based campaigns to prevent HIV in men who have sex with men (MSM).
The study is interdisciplinary and uses data on campaign implementation and costs, as well as outcome data from three surveys in MSM.
The study design did not include a control group.
The primary study outcome measurement is based on self-reported data collected from a non-random sample of respondents.
Introduction
The number of new HIV diagnoses among men who have sex with men (MSM) remains high, even in countries that have high levels of use of antiretroviral treatment (ART).1–5 Several modelling studies and studies of genetic sequence data suggest that a high proportion of new HIV infections results from MSM with undiagnosed early (primary) HIV infection.3 4 6–8 Interventions that increase HIV testing and prevent transmission early on, when viral load is highest, could have a particularly powerful effect in reducing the incidence of HIV in MSM.3 7 8
Switzerland has a history of innovative HIV health promotion, including the ‘Stop AIDS’ and ‘Love life’ information campaigns and the ‘Swiss statement’, which emphasised the low risk of sexual transmission of HIV during effective ART 10 years before ‘U=U’ (undetectable equals untransmittable) was broadly promoted.9 However, the population benefits of ART can only be realised if HIV infection is diagnosed, and reaching MSM with high-risk sexual behaviours who are unaware of their HIV status is challenging. A mathematical modelling study in Switzerland estimated that in 2012 about 14% of HIV-infected MSM with undiagnosed infection were the source of more than 80% of new HIV infections in MSM.8 Those with undiagnosed HIV infection are among about 20% of MSM in Switzerland who report never having had an HIV test during their life or among the 60% who have not had a test in the last year.10 We estimate that in 2012, 6300 MSM (8%) were living with HIV both diagnosed and undiagnosed, and 1700 (or 2.2%) had non-suppressed HIV infection.11 In addition, an increasing proportion of MSM report condomless anal intercourse with one or more casual sex partners.10
The Swiss Federal Office of Public Health developed an innovative community-based campaign, Break the Chains, to reduce HIV transmission during primary HIV infection.12 13 The rationale for the campaign is that intensive mobilisation by the MSM community will encourage those at high risk of HIV acquisition and transmission to adopt short-term risk reduction practices, followed by HIV testing.12 The risk reduction period should allow recently acquired HIV infections to become detectable using routine HIV testing methods.14 MSM with newly detected infections can be linked to care services and start immediate ART to reduce viral load and to reduce further HIV transmission.15 The campaign has been implemented every year in spring since 2012. While several individual components of the Break the Chains campaign are theory driven and effective, such as peer outreach activities, social marketing to promote HIV testing and voluntary counselling and testing (VCT),16–20 evaluations of multicomponent campaigns are rare. The objectives of this study were to evaluate the implementation, the effects and the costs of the Break the Chains 2015 campaign.
Methods
Participants
The Break the Chains 2015 campaign target population was MSM at risk of HIV acquisition or transmission (table 1). We define MSM as men who are attracted to other men or who have sex with men, regardless of whether they identify themselves as gay. The population of MSM aged 15–65 in Switzerland (2012) is estimated to be 80 000 (Bayesian 95% credibility interval 64 000 to 96 000) of whom about half live in the five largest cities (Zurich, Geneva, Basel, Lausanne and Bern).11
Table 1.
Definition of men who have sex with men (MSM) at risk, or not at risk of HIV acquisition or transmission, based on the theory of the 2015 Break the Chains campaign, Switzerland, March–May 2015
| MSM with specified HIV risks (MSMwr)* | MSM with no specified HIV risks (MSMnr)* |
| CAI with a partner of unknown or different HIV status (steady and/or casual partners) over the last 12 months | Did not report any of the criteria for MSMwr; considered to have avoided any risk of HIV transmission† |
| CAI with casual partners over the last 12 months | |
| Unknown HIV status within a steady partnership over the last 12 months | |
| HIV negative with steady partner who is HIV positive but does not receive antiretroviral therapy and/or has a detectable viral load | |
| HIV positive with detectable viral load‡ |
*MSMwr and MSMnr are mutually exclusive categories.
†MSM in this category are assumed to continue to avoid any risk of HIV transmission during the campaign and follow-up period.
‡MSM with HIV infection and a detectable viral load are at risk of transmitting HIV. They were not included in the calculation of those adopting the campaign message because they would not be expected to have another HIV test.
CAI, condomless anal intercourse.
Intervention
Break the Chains is a community-based multicomponent information and action campaign that involves: a media information campaign; local HIV prevention organisation professionals and volunteers who deliver peer outreach activities; an incentive (reduced cost of testing) to increase the uptake of HIV testing; and evaluation. The campaign message of Break the Chains 2015 (online supplementary figure S1) was: “It’s simple: In order to prevent new HIV infections, avoid taking any risks for the month of April and then take an HIV test for 10 Swiss francs in May. The more men who take part in this campaign, the more successful we will be in our efforts to combat HIV. So tell your friends about Break the Chains and join us”. The strategies to avoid taking risks were: safer sex practices (ie, condom use for penetrative sex, no sperm or blood in the mouth), and strategies adapted to the personal situation (eg, abstinence, only oral sex, sex exclusively with the steady partner who is either HIV negative or under treatment with an undetectable viral load). Pre-exposure prophylaxis (PrEP) has only been recommended in Switzerland since 2016.21
bmjopen-2019-032459supp001.pdf (758.7KB, pdf)
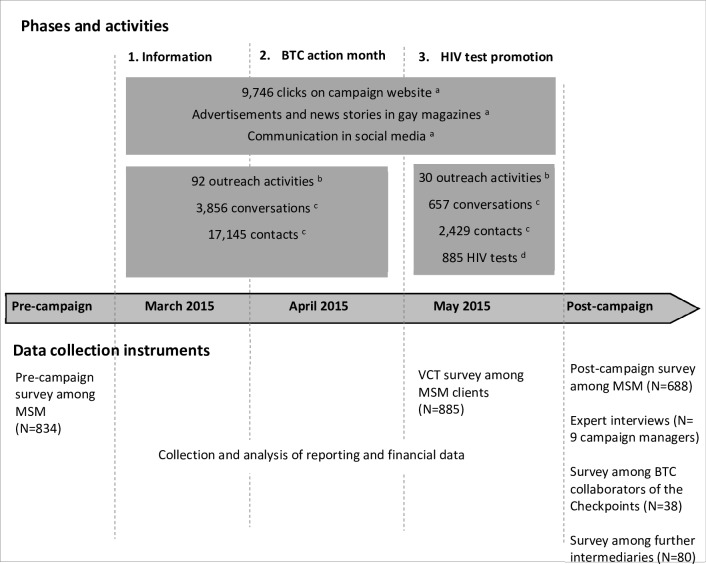
The Swiss Aids Federation implemented Break the Chains 2015 in three phases (figure 1): (1) Late February and March, mobilisation of MSM to follow the recommendations of Break the Chains and outreach activities to deliver the campaign message; (2) throughout April, Break the Chains action month, MSM avoid any risk of HIV transmission until they get tested for HIV; and (3) May, HIV test promotion at a reduced cost (USD purchasing power parity (PPP) 8 instead of USD PPP 48).
Figure 1.
Campaign phases, activities and data collection instruments, Break the Chains (BTC), Switzerland, March to May 2015. MSM, men who have sex with men; VCT, voluntary counselling and testing. aWeb clicks: no information available if web users are belonging to the target population; communication in gay magazines and social media: no data available on the audience size. Source: Swiss AIDS Federation, October 2015. bOutreach activities are visits to public gay venues by date of the activity and region. Data about outreach activities in May 2015 were missing for 3 out of 11 regions. Source: Swiss AIDS Federation, October 2015. cThe outreach worker responsible for each visit estimated the number of conversations and contacts; a ‘conversation’ involved a conversation of at least a few minutes and the dissemination of the core campaign messages; a ‘contact’ included handing out of leaflets or being seen, but with no conversation. Source: Swiss AIDS Federation, October 2015. dNumber of HIV tests among MSM clients of 34 VCT sites in May 2015, recorded by the Swiss Federal Office of Public Health.
The media information campaign was implemented across Switzerland with advertisements on websites, a Facebook page and a campaign website. Media included adverts and news stories in gay magazines, posters, flyers, condom catch covers and silicon bracelets. Local member organisations of the Swiss AIDS Federation delivered the campaign in 11 of 26 cantons in Switzerland. Intermediaries, such as gay community organisations and managers of gay bars, clubs and other venues gave permission for the prevention activities and put out the campaign materials. Community workers and volunteers visited gay venues in the main city in the five cantons most affected by HIV, and to a lesser extent in another six cantons from February to May 2015. They conducted peer outreach to engage MSM in conversation to inform them about the campaign, its message and the availability of HIV testing. In May 2015, 34 VCT centres across Switzerland, including ‘Checkpoints’, that is, dedicated health centres for MSM, offered low-cost HIV tests for MSM.
Data collection and outcome measures
We developed a detailed programme theory and evaluation plan (online supplementary figure S2) before the campaign started.22 The evaluation plan specified outcome measures based on the theory of how the programme should work to prevent HIV transmission during early infection. Outcomes for implementation, effects and costs were defined (online supplementary table S1) and measured as follows.
Implementation fidelity: this was measured as the intensity of the campaign activities, coherence between the campaign concept and delivery, and support for the campaign by intermediaries. We used three data sources (figure 1, online supplementary table S1). First, Swiss AIDS Federation staff collected campaign monitoring data, including frequencies of outreach activities and estimates of the numbers of contacts made. Second, we conducted qualitative face-to-face interviews with campaign managers at the national and local level. Third, we set up an online questionnaire for staff involved in the campaign delivery, bar and club managers, community activists and managers of HIV testing and prevention sites. The interviews and the online survey, completed in June 2015 after the campaign, included questions about the campaign’s concept, the delivery and the support for the campaign.
Intervention effect: the primary outcome was the proportion of MSM at risk of HIV acquisition or transmission who used one of the promoted HIV risk reduction strategies in April, and maintained it until HIV testing in May. Secondary outcomes were: test uptake in May, compared with the 12 preceding months; knowledge about primary HIV infection; and the sense of belonging to the gay community.
We collected data between October 2014 and September 2015 in three anonymous online surveys (figure 1). The surveys were advertised on gay community, dating and social networking websites before and after the campaign period. Respondents to the survey were therefore self-selected and only account for a small proportion of all those who were approached during the campaign (figure 1, online supplementary table S1). All three surveys included questions about self-reported HIV infection status, HIV-related sexual risk behaviours and sociodemographic variables and connectedness to the lesbian, gay, bisexual, and transgender (LGBT) community.23 We defined MSM with risk of HIV infection (MSMwr) as having at least one of five indicators of HIV transmission risk in the last year (table 1). Survey respondents with none of the five indicators were defined as MSM with no risk of HIV infection (MSMnr).
The precampaign survey elicited intentions of MSM to take part in the campaign. We added specific questions to the 2014 edition of Gaysurvey, a structured questionnaire that has been conducted since 1987 as part of routine monitoring of sexual and preventive behaviours related to HIV risk among MSM in Switzerland (as an online survey since 2004).10 Participants were recruited through banner advertisements posted on relevant websites in October 2014. They completed an internet-based self-administered questionnaire and indicated whether they intended to take part in the 2015 Break the Chains campaign.
An online postcampaign survey was conducted 2 months after the campaign using the same recruitment strategy as the GaySurvey. In addition to topics covered in the precampaign survey, the postcampaign survey asked about awareness of the campaign, sexual behaviours during the campaign period and, for those who adopted an HIV risk reduction strategy during April 2015, whether they did it because of the campaign (online supplementary table S2).
In addition, MSM who visited any of the 34 VCT centres that offered reduced cost HIV tests in May 2015 were invited to fill in a questionnaire. This VCT survey asked about campaign exposure. Additionally, we collected data on the numbers of HIV tests taken by MSM in VCT centres between March 2014 and September 2015.
Costs of Break the Chains 2015: we used a full costing approach, including direct costs (irrespective of payer) and costs of non-market items.24 Costs were recorded in 2015 Swiss francs (CHF). Considering PPP for the same year, they were converted to United States Dollars (USD PPP). The direct cost components were personnel and other expenses such as travel, overheads of the involved organisations, campaign materials and services provided by third parties (eg, advertisements, translations), subsidies for HIV tests and the evaluation. The Swiss Federal Office of Public Health and Swiss AIDS Federation provided financial statements and time sheets on the numbers of paid and unpaid working hours by the staff and volunteers who implemented Break the Chains 2015 (figure 1, online supplementary table S3). The non-market cost component was unpaid volunteer work, estimated based on the human capital approach that assumed an hourly rate corresponding to the opportunity costs of a lost working hour in Switzerland (ie, USD PPP 26 per hour). Cost results are reported as programme costs and as cost per outcome achieved.
Analyses
Qualitative interviews were conducted by a member of the evaluation team, using an interview guide. The interviews were digitally recorded and then transcribed. A trained researcher used qualitative content analysis to analyse data about the implementation of the campaign.25 Descriptive statistics were used to report the precampaign intentions, intervention fidelity, uptake of the intervention and of HIV testing, as well as secondary outcomes.
We calculated the uptake of the primary outcome, use of a risk reduction strategy during April until HIV testing in May, among the sample of MSM who completed the postcampaign survey and had heard about the campaign. HIV-positive MSMwr (n=7/688) were excluded from these analyses as they were not supposed to take an HIV test in May. We used logistic regression to compare the primary outcome between the target group, MSMwr and MSM not in the target group (MSMnr) according to campaign-related, demographic, community and behavioural factors using univariable OR with 95% CI. We constructed a multivariable model to compare the outcome in MSMwr and MSMnr, adjusting for all factors in the univariable analysis, including the secondary outcome of sense of belonging to the gay community. Other secondary outcomes were described using frequencies (postcampaign test uptake) and χ2 tests (knowledge of primary HIV infection).
The cost estimates used full data obtained from all involved organisations so they are presented without measures of statistical uncertainty. We estimated the campaign cots per outcome by extrapolating the campaign effects measured among survey respondents to the entire estimated population of MSM in Switzerland, with uncertainty derived from the 95% credibility intervals (64 000 to 96 000).20
All quantitative data were processed in Excel (V.2016, Microsoft) and analysed using SPSS (V.23, IBM) and Stata (V.14, Stata Corp.).
Ethical committee
The overall study was conducted in accordance with the Ethics Committee of the Faculty of Arts and Sciences at University of Zurich. The protocol of the online surveys among MSM was submitted to the Ethics Commission of the canton of Vaud, who considered it exempt from ethical committee review because it used anonymous data (art. 2, al.2, Letter c, LRH).
Patient and public involvement
A representative of the community organisation responsible for the campaign (the Swiss Aids Federation) participated in study design as well as elaboration of survey instruments, and is a coauthor of this article.
Results
Precampaign intentions
In October 2014, a sample of 834 MSM responded to the online invitations to take part in the precampaign GaySurvey. Of these, 395 (47.4% (95% CI 43.9% to 50.8%)) said that they would be ready to take part in the Break the Chains 2015 campaign. Among these, there were 111 MSMwr (28.1% (95% CI 23.8% to 67.2%)) and 284 MSMnr (71.8% (95%CI 67.2% to 76.1%)).
Implementation fidelity
Outreach workers and volunteers from local organisations attended venues on 92 evenings in March and April 2015. They estimated that they had contacted a total of 17 145 MSM in 11 regions during this period and conducted 3856 conversations of a few minutes each to deliver the Break the Chains 2015 campaign message (figure 1, online supplementary table S1). Of these, 10 584 (61.7%) contacts and 3169 (82.2%) conversations were in the five cities most affected by HIV. Among venue managers, community activists and managers of HIV testing and prevention sites, 86.3% (69/80) reported having received the campaign posters and/or flyers and 87.0% (60/69) of those who received the materials said they had displayed them.
Interviews with Break the Chains 2015 campaign managers and data from the survey among staff revealed that they found it difficult to convey the full campaign message in their outreach communications. Interviewees stated that public gay venues, such as crowded parties or bars, did not allow detailed communication about the rationale for reducing risk behaviours, the relevance of sexual networks and primary infection. Campaign staff reported that ‘take a test in May’ was the message most frequently addressed in outreach conversations (on average in 9 out of 10 conversations), followed by ‘take part in Break the Chains and avoid any HIV transmission risk in April’ (on average in 8 out of 10 conversations). Thus, the message that was delivered put more emphasis on HIV test promotion rather than equal emphasis on risk reduction and HIV testing.
Exposure to, and effects of, the Break the Chains campaign
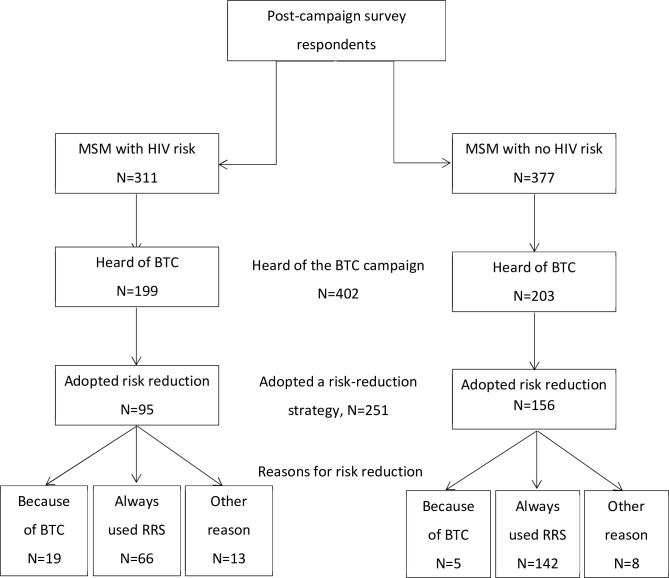
Of the 688 respondents to the online invitations to take part in the postcampaign survey, 311 (45.2%) were categorised as MSMwr and 377 as MSMnr (figure 2). Of 402/688 (58.5%) MSM who reported that they had heard about Break the Chains 2015, 199 (49.5%) were MSMwr. MSMwr (64.0%; 199/311) were more likely to have heard of the campaign than MSMnr (53.8%; 203/377; difference in proportions 10.1%, 95% CI 2.8% to 17.5%, p=0.007). Similar proportions of MSMwr and MSMnr were able to identify the main campaign message (overall, 65.4%; 95% CI 60.5% to 70.1%; 263/402) or felt personally concerned by the campaign (overall, 37.8%; 95% CI 33.1% to 42.8%; 152/402).
Figure 2.
Outcome of campaign among respondents to the postcampaign online survey, Break the Chains (BTC), Switzerland, March to May 2015. MSM, men who have sex with men; RRS, risk reduction strategy.
Risk reduction behaviour: of the 402 respondents to the postcampaign survey who had heard about the Break the Chains campaign, MSMwr (47.7%; 95/199) were less likely to report having consistently used a risk reduction strategy during April 2015 and maintained it until they got tested in May than MSMnr (76.8%; 156/203). The lower odds for MSMwr, compared with MSMnr, to use a risk reduction strategy (table 2) remained in multivariable analysis, after controlling for campaign-related, demographic and behavioural factors (adjusted OR (aOR) 0.24; 95% CI 0.14 to 0.42). Participation in a previous Break the Chains campaign was associated with an increased odds of using a risk reduction strategy (aOR 2.62; 95% CI 1.41 to 4.85). Regular use of sex-on-premises venues and use of the internet to find sexual partners were associated with reduced odds of using a risk reduction strategy (table 2).
Table 2.
Factors associated with the uptake of the campaign message, according to HIV risk status, Break the Chains (BTC), Switzerland, March to May 2015, postcampaign survey (among respondents who reported having heard of the campaign: n=402/688)
| All respondents | Risk reduction in April until tested* | Risk reduction in April until tested | ||||||||||
| n=402 | Column % | Yes, n=251 | No, n=151 | OR | 95% CI | P value from LR test | aOR | 95% CI | P value from LR test | |||
| N | Column% | N | Column% | |||||||||
| BTC target group | <0.001 | <0.001 | ||||||||||
| MSMwr | 199 | 49.5 | 95 | 37.9 | 104 | 68.9 | 0.28 | 0.18 to 0.42 | 0.24 | 0.14 to 0.42 | ||
| MSMnr | 203 | 50.5 | 156 | 62.1 | 47 | 31.3 | Ref. | |||||
| Felt personally concerned by BTC | 0.005 | 0.066 | ||||||||||
| Yes | 152 | 37.8 | 109 | 43.4 | 43 | 28.5 | 1.84 | 1.19 to 2.84 | 1.70 | 0.96 to 3.00 | ||
| No | 245 | 61.0 | 142 | 56.6 | 103 | 68.2 | Ref. | Ref. | ||||
| No response | 5 | 1.2 | 0 | 0.0 | 5 | 3.3 | ||||||
| Understand the message of BTC | 0.011 | 0.224 | ||||||||||
| Yes | 263 | 65.4 | 176 | 70.1 | 87 | 57.6 | 1.73 | 1.13 to 2.63 | 1.42 | 0.81 to 2.51 | ||
| No | 139 | 34.6 | 75 | 29.9 | 64 | 42.4 | Ref. | Ref. | ||||
| Participation in previous BTC campaign | <0.001 | 0.002 | ||||||||||
| Yes | 123 | 30.6 | 96 | 38.3 | 27 | 17.9 | 2.84 | 1.75 to 4.63 | 2.62 | 1.41 to 4.85 | ||
| No | 279 | 69.4 | 155 | 61.8 | 124 | 82.1 | Ref. | Ref. | ||||
| Age | 0.508 | 0.270 | ||||||||||
| <25 year. | 19 | 4.7 | 13 | 5.2 | 6 | 4.0 | 1.55 | 0.55 to 4.34 | 2.76 | 0.75 to 10.12 | ||
| 25–49 year. | 215 | 53.5 | 137 | 54.6 | 78 | 51.7 | 1.26 | 0.80 to 1.97 | 1.06 | 0.59 to 1.90 | ||
| ≥50 year. | 127 | 31.6 | 74 | 29.5 | 53 | 35.1 | Ref. | Ref. | ||||
| No response | 41 | 10.2 | 27 | 10.8 | 14 | 9.3 | ||||||
| University degree | 0.011 | 0.053 | ||||||||||
| Yes | 250 | 62.2 | 168 | 66.9 | 82 | 54.3 | 1.72 | 1.13 to 2.61 | 1.74 | 0.99 to 3.06 | ||
| No | 149 | 37.1 | 81 | 32.3 | 68 | 45.0 | Ref. | Ref. | ||||
| No response | 3 | 0.8 | 2 | 0.8 | 1 | 0.7 | ||||||
| Live in area with >100 000 inhabitants | 0.416 | 0.587 | ||||||||||
| Yes | 165 | 41.0 | 107 | 42.6 | 58 | 38.4 | 1.19 | 0.79 to 1.79 | 1.17 | 0.67 to 2.03 | ||
| No | 235 | 58.5 | 143 | 57.0 | 92 | 60.9 | Ref. | Ref. | ||||
| No response | 2 | 0.5 | 1 | 0.4 | 1 | 0.7 | ||||||
| Community connectedness | 0.017 | 0.475 | ||||||||||
| Mean | 2.47 | 2.54 | 2.36 | |||||||||
| Score 1–2.5 | 195 | 54.5 | 110 | 49.6 | 85 | 62.5 | Ref. | Ref. | ||||
| Score 2.6–4 | 163 | 45.5 | 112 | 50.5 | 51 | 37.5 | 1.70 | 1.10 to 2.62 | 1.23 | 0.70 to 2.14 | ||
| Regularly visit sex-on-premises venues† | 0.009 | 0.032 | ||||||||||
| Yes (frequently) | 66 | 16.4 | 31 | 12.4 | 35 | 23.2 | 0.50 | 0.29 to 0.84 | 0.46 | 0.22 to 0.94 | ||
| No (sometimes/never) | 324 | 80.6 | 213 | 84.9 | 111 | 73.5 | Ref. | Ref. | ||||
| No response | 12 | 3.0 | 7 | 2.8 | 5 | 3.3 | ||||||
| Frequent use of the internet for sexual encounters† | <0.001 | 0.024 | ||||||||||
| Yes (frequently) | 178 | 44.3 | 88 | 35.1 | 90 | 59.6 | 0.36 | 0.24 to 0.55 | 0.52 | 0.30 to 0.92 | ||
| No (sometimes/never) | 221 | 55.0 | 161 | 64.1 | 60 | 39.7 | Ref. | Ref. | ||||
| No response | 3 | 0.8 | 2 | 0.8 | 1 | 0.7 | ||||||
*Respondents were categorised as having adopted an risk reduction strategy if they reported ‘always’ to either of two questions asking whether they had followed one of the two strategies promoted by the campaign (ie, followed safer sex practices (151 respondents), or a risk reduction strategy adapted to their personal situation (232 respondents)). Other answer categories were ‘sometimes’, ‘never’ and ‘no answer’. (For exact question wording, see online supplementary table S2.)
†In the last 12 months.
aOR, adjusted OR, adjusted for all variables in the table; LR, likelihood ratio; MSM, men who have sex with men; MSMnr, MSM with no HIV risk; MSMwr, MSM with HIV risk; Ref., reference category.
Among the 251 respondents to the postcampaign survey who consistently used a risk reduction strategy in April, 91.0% (142/165) of MSMnr and 69.5% (66/95) of MSMwr reported that they always use a risk reduction strategy. Nineteen of the 95 (20.0%) MSMwr who reported they had used a risk reduction strategy in April 2015 did it in order to comply with the key message of the Break the Chains campaign (figure 2, multiple answers allowed).
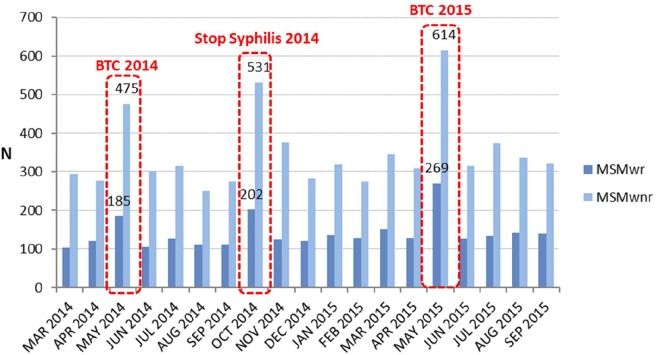
Test uptake: 707 MSM who were tested in the VCT centres during May 2015 reported their reason for getting a test (online supplementary figure S3, multiple answers were allowed): 65 (9.2%) came to test as part of the campaign, having avoided HIV transmission risks in April; 342 (48.4%) were being tested because of the reduced cost; 30 (4.2%) said the campaign made them aware of transmission risks, but they did not follow the recommendations, for 300 (42.4%) the reason was unrelated to the campaign, and 34 (4.8%) did not answer the question. Overall, 373 of 707 respondents (52.8%) mentioned a least one reason that was linked to the campaign, of which reduced cost was the most common (online supplementary figure S3). A plot of monthly HIV test numbers from March 2014 to September 2015 (figure 3) shows that the number of tests during May 2015 (n=883) was twice as high as the average (n=436) for months when there was no HIV test promotion. MSMnr accounted for about 70% of HIV tests both during months with HIV test promotion and all other months.
Figure 3.
HIV test uptake at voluntary counselling and testing sites in Switzerland by month of consultation and risk behaviour, Break the Chains (BTC) campaign, Switzerland, March to May 2015. MSMwnr, men who have sex with men with none of the specified risks of HIV transmission; MSMwr, men who have sex with men with a specified risk of HIV transmission; n, number of tests; Stop Syphilis, health promotion campaign that offered free tests for syphilis. Red-dashed lines indicate that months in which HIV or syphilis tests were available at reduced or no cost.
Knowledge about primary infection: the proportion of survey respondents who felt well informed about primary HIV infection was higher in the postcampaign than the precampaign survey (58.0% vs 51.1%; p=0.019). Among respondents to the postcampaign survey, this proportion was higher among those who had heard about the campaign than those who had not (65.0% vs 36.3%; p<0.001).
Sense of belonging to the gay community: a higher score for connectedness to the LGBT community was associated with adoption of a risk reduction strategy in univariable but not multivariable analysis (table 2). The mean scores in respondents of the precampaign and postcampaign (2.39; SD=0.84 vs 2.37; SD=0.82, p=0.745) surveys were similar. Respondents to the postcampaign survey who reported having heard about Break the Chains had a higher score (2.47; SD=0.79) than the respondents who reported not having heard about the campaign (2.14; SD=0.84).
Costs of Break the Chains 2015
The total costs of the campaign were USD PPP 488 984, with direct costs of USD PPP 474 019 and costs of non-market items of USD PPP 14 965 (online supplementary table S3). Salaries accounted for 46.1% of the total costs, while 6.0% of the total costs (USD PPP 29 473) were spent on the reduction of the price for HIV tests in May 2015. The costs of the present evaluation amounted to 16.4% of the total campaign costs.
Table 3 shows the total costs in relation to the outcomes of the campaign. The cost per encounter (outreach contacts and conversations, clicks on the campaign website) is estimated at USD PPP 14. Based on the results of the postcampaign survey, an estimated 58.4% of the MSM population in Switzerland had heard of the campaign. Extrapolation of these costs to the estimated population of MSM in Switzerland resulted in an estimate of USD PPP 9–13 to reach one MSM, USD PPP 36–55 for one MSM at risk of HIV to adhere to a risk reduction strategy and USD PPP 181–272 for one MSM at risk of HIV to adhere to a risk reduction strategy because of the campaign.
Table 3.
Approximate costs of outcomes of the campaign, Break the Chains (BTC), Switzerland, March to May 2015
| Outcomes | Outcome measure (data source) | Estimated outcomes at the MSM population level | Campaign costs*/estimated outcome |
| Encounter | BTC 2015 outreach contacts/conversations with MSM, clicks on the campaign website† | 33 833 | USD PPP 14 |
| To reach one MSM | MSM who heard about BTC 2015 (58.4%, postcampaign survey) | 37 376–52 560‡ | USD PPP 9–13 |
| One MSMwr adopts a risk reduction strategy in April 2015 | MSM at risk who used a risk reduction strategy in April 2015 (13.8%, postcampaign survey§) | 8832–13 248‡ | USD PPP 36–55 |
| One MSMwr adopts an HIV risk reduction strategy because of the campaign | MSMwr who adopted an HIV risk reduction strategy in April and maintained it until HIV testing in May because of the BTC campaign (2.8%, postcampaign survey¶) | 1792–2688‡ | USD PPP 181–272 |
*Total campaign costs were USD PPP 488 984 (incl. direct USD PPP 474 019 and costs of non-market items USD PPP 14 965, as well as the costs for the HIV test price reduction USD PPP 29 473; CHF 603 896; purchasing power parity conversion rate for the year 2015: 1 CHF=1.235 USD PPP). See online supplementary table S3 for more detailed explanation.
†9746 (28.8%) of the 33 833 encounters are web clicks (no information available if web users are belonging to the target population), data from Swiss AIDS Federation.
‡Extrapolation of the outcome measure to the Swiss men who have sex with men (MSM) population (estimated size of the population of MSM between 15 and 64 years old: 64 000–96 000 men20).
§Of 402 (58.4%) respondents who heard of the campaign 95 MSM with HIV risk (MSMwr) respondents indicated that they adopted an HIV risk reduction strategy in April and maintained it until HIV testing in May (95/688=13.8%).
¶Of 402 (58.4%) respondents who heard of the campaign 19 MSMwr respondents indicated that they adopted their risk behaviour in order to comply with the key message of the campaign (19/688=2.8%).
Discussion
The multicomponent community participatory Break the Chains campaign delivered information to an estimated 17 145 MSM in a large number of gay venues in Switzerland from March to April 2015. The target group, MSMwr, was more likely to have heard of the campaign but less likely than MSMnr to have used a risk reduction strategy until being tested for HIV in May 2015 (aOR 0.24; 95% CI 0.14 to 0.42). Twenty per cent of MSMwr who used a HIV risk reduction strategy in April did it as a direct result of the campaign. HIV test uptake increased after the campaign, but most tests were taken by MSMnr. Self-reported level of knowledge about primary HIV infection and a sense of belonging to the LGBT community were higher in MSM who had heard about the campaign than those who had not. The campaign was estimated to have cost USD PPP 181–272 for each MSMwr who adhered to the campaign message.
Our results suggest that the Break the Chains campaign 2015 produced a substantial short-term increase in HIV testing among MSM, but not necessarily by those with sexual behaviours associated with higher risks of HIV. The information campaign achieved an exposure level that compares well with levels reported in the wider literature on HIV campaigns.18 19 26 The peer outreach workers were well organised and appeared to reach MSM who felt connected to the gay community. Their reports indicated, however, that the message to have an HIV test came across more clearly than advice to avoid exposure to HIV. The evaluation suggests that we underestimated the complexity of delivering the two-part message and its rationale in the outreach venues. Uptake of HIV testing might be higher with more emphasis on having an HIV test if one has had a potentially high-risk exposure in the previous month.
This comprehensive assessment of a complex community-based HIV prevention intervention at country level in Switzerland has several strengths. The campaign components were evidence based and the interdisciplinary and multimethod research design was theory driven, according to a programme theory of the way in which the intervention should work.22 The implementation and evaluation involved the main stakeholders in HIV prevention among MSM, allowed us to maximise the acceptability of data collection and to evaluate the campaign under real-world conditions.27 The online surveys were an efficient way to measure the precampaign intentions and campaign effects in independent samples of MSM across Switzerland and used a consistent way to define those at risk of HIV infection or transmission. The evaluation, however, also has weaknesses. First, we analysed campaign effects among all respondents who had heard of the campaign and did not differentiate between those who were contacted in outreach venues and those who had seen only the media information. We thus were unable to assess a possible dose–response effect. Second, self-administered online surveys might result in participation bias, limiting generalisability to the whole MSM population.28 29 Nevertheless, online surveys are widely used to conduct research with hard to reach groups and have been used in Switzerland to assess sexual and preventive behaviours related to HIV risk since 2009. Third, the primary outcome was self-reported so might be influenced by recall and social desirability biases. We tried to mitigate these concerns by using a brief recall period (2 months after the campaign) and self-administered, anonymous questionnaires. We acknowledge that respondents’ attribution of changes in their behaviours would not capture subconscious influences of social networks and other mechanisms. We also acknowledge that the association with reported sense of belonging to the gay community might have been either a motivation for, or a consequence of the campaign. Fourth, campaign collaborators and intermediaries might have overestimated their activities. The overall number of campaign encounters is likely to be an underestimate because it does not include contacts achieved through other channels such as gay media communications, posters and flyers. Fifth, the extrapolation of costs to the national level assumes that the costs for areas involved in the campaign can be simply multiplied. In a small country like Switzerland, we think this was a reasonable assumption. It remains unknown to what extent the unpaid volunteer work provided, conceptualised here as a non-market cost item, translated into a reduction of paid work and thus cost of lost productivity at the societal level.
Public health implications
The identification of people with undiagnosed HIV infection is the biggest challenge to the achievement of the UNAIDS 90-90-90 targets to end HIV/AIDS as a public health problem.20 30 Health promotion practitioners and policy-makers need interventions that increase HIV testing uptake in MSM and other populations at the highest risk of acquiring HIV infection and of transmitting it before diagnosis and the start of antiretroviral therapy. Since the Break the Chains 2015 campaign, pragmatic trials have shown the effectiveness of PrEP to prevent HIV infection in MSM with high levels of risk behaviours.31 32 Informing MSM at risk about PrEP as an additional risk reduction strategy should therefore become part of HIV prevention campaigns, as it is already in Switzerland.21 This evaluation showed that Break the Chains increased HIV testing, but campaign messages need to be simplified and additional interventions are needed to identify the target group more accurately. The development, improvement and evaluation of community-based campaigns identifying those at the highest risk of infection should remain a cornerstone in HIV prevention strategies for MSM.
Supplementary Material
Acknowledgments
The authors thank all persons who contributed to this study and participated in online surveys or interviews. They would like to acknowledge Christopher Goodman and Elodie Panoussopoulos for their valuable research assistance.
Footnotes
Twitter: @nicolamlow
KF and SL contributed equally.
RB, DK and NL contributed equally.
Contributors: KF, SL, RB, FD-A, RR, NL and DK conceived the study. KF was responsible for the coordination of the research activities of the overall project and did the analysis of the implementation of the campaign. SL, RB and NL did the statistical analysis. PB and MS did the cost analysis. AS provided data on the total number of MSM and with unsuppressed HIV in Switzerland. SD, RS and AL provided monitoring and cost data for the analyses. NL, RR, FD-A, AS and DK gave advice on analysis and interpretation. All authors contributed to the interpretation. KF wrote the first draft of the article. SL, RB, DK and NL revised the article. All authors reviewed and approved the final version.
Funding: This work was supported by the Swiss Federal Office of Public Health.
Disclaimer: The findings and conclusion in this report are those of the authors and do not necessarily represent the views of the Swiss Federal Office of Public Health or the Swiss Aids Federation.
Competing interests: At the time of the study, RS, AS and SD were with the Swiss Federal Office of Public Health. They were responsible for HIV prevention of the Swiss government and developed and implemented the ‘Break the Chains’ campaign. KF, SL and RB received salary support from the Swiss Federal Office of Public Health. AL is with the Swiss Aids Federation and was involved in the development and implementation of the ‘Break the Chains’ campaign.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Anonymised quantitative survey data used for the analyses in this article are available upon reasonable request from the corresponding author.
References
- 1. European Centre for Disease Prevention and Control, WHO Regional Office for Europe Hiv/Aids surveillance in Europe 2014. Stockholm, Sweden: European Centre for Disease Prevention and Control, 2015. [Google Scholar]
- 2. Sullivan PS, Jones JS, Baral SD. The global North: HIV epidemiology in high-income countries. Curr Opin HIV AIDS 2014;9:199–205. 10.1097/COH.0000000000000039 [DOI] [PubMed] [Google Scholar]
- 3. Ratmann O, van Sighem A, Bezemer D, et al. Sources of HIV infection among men having sex with men and implications for prevention. Sci Transl Med 2016;8:320ra2 10.1126/scitranslmed.aad1863 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Beyrer C. Strategies to manage the HIV epidemic in gay, bisexual, and other men who have sex with men. Curr Opin Infect Dis 2014;27:1–8. 10.1097/QCO.0000000000000037 [DOI] [PubMed] [Google Scholar]
- 5. Kohler P, Schmidt AJ, Cavassini M, et al. The HIV care cascade in Switzerland: reaching the UNAIDS/WHO targets for patients diagnosed with HIV. AIDS 2015;29:2509–15. 10.1097/QAD.0000000000000878 [DOI] [PubMed] [Google Scholar]
- 6. Pinkerton SD. How many sexually-acquired HIV infections in the USA are due to acute-phase HIV transmission? AIDS 2007;21:1625–9. 10.1097/QAD.0b013e32826fb6a6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Marzel A, Shilaih M, Yang W-L, et al. Hiv-1 transmission during recent infection and during treatment interruptions as major drivers of new infections in the Swiss HIV cohort study. Clin Infect Dis 2016;62:115–22. 10.1093/cid/civ732 [DOI] [PubMed] [Google Scholar]
- 8. van Sighem A, Vidondo B, Glass TR, et al. Resurgence of HIV infection among men who have sex with men in Switzerland: mathematical modelling study. PLoS One 2012;7:e44819 10.1371/journal.pone.0044819 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Vernazza P, Hirschel B, Bernasconi E, et al. HIV-infizierte Menschen ohne andere STD sind unter wirksamer antiretroviraler therapie sexuell nicht infektiös. Schweizerische Ärztezeitung 2008;89:165–9. [Google Scholar]
- 10. Lociciro S, Bize R. Les comportements face Au VIH/Sida des hommes qui ONT des rapports sexuels avec des hommes. Enquête Gaysurvey 2014. Lausanne, Switzerland: Institut universitaire de médecine sociale et préventive; 2015. [Google Scholar]
- 11. Schmidt AJ, Altpeter E. The denominator problem: estimating the size of local populations of men-who-have-sex-with-men and rates of HIV and other STIs in Switzerland. Sex Transm Infect 2019;95:285–91. 10.1136/sextrans-2017-053363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Swiss Federal Office of Public Health Sex between men: towards a better sexual health 2012. Bern, Switzerland: Swiss Federal Office of Public Health, 2011. [Google Scholar]
- 13.Lociciro S, Jeannin A, Dubois-Arber F. Lausanne, Switzerland: Institut universitaire de médecine sociale et préventive; 2013. Evaluation de la campagne break the chain 2012. Raisons de santé 210, report. [Google Scholar]
- 14. Konrad BP, Taylor D, Conway JM, et al. On the duration of the period between exposure to HIV and detectable infection. Epidemics 2017;20:73–83. 10.1016/j.epidem.2017.03.002 [DOI] [PubMed] [Google Scholar]
- 15. Cohen MS, McCauley M, Gamble TR. Hiv treatment as prevention and HPTN 052. Curr Opin HIV AIDS 2012;7:99–105. 10.1097/COH.0b013e32834f5cf2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Strömdahl S, Hickson F, Pharris A, et al. A systematic review of evidence to inform HIV prevention interventions among men who have sex with men in Europe. Euro Surveill 2015;20:21096 10.2807/1560-7917.ES2015.20.15.21096 [DOI] [PubMed] [Google Scholar]
- 17. Berg R. The effectiveness of behavioural and psychosocial HIV/STI prevention interventions for MSM in Europe: a systematic review. Euro Surveill 2009;14. doi: 10.2807/ese.14.48.19430-en. [Epub ahead of print: 03 Dec 2009]. [DOI] [PubMed] [Google Scholar]
- 18. Lorimer K, Kidd L, Lawrence M, et al. Systematic review of reviews of behavioural HIV prevention interventions among men who have sex with men. AIDS Care 2013;25:133–50. 10.1080/09540121.2012.699672 [DOI] [PubMed] [Google Scholar]
- 19. Noar SM, Palmgreen P, Chabot M, et al. A 10-year systematic review of HIV/AIDS mass communication campaigns: have we made progress? J Health Commun 2009;14:15–42. 10.1080/10810730802592239 [DOI] [PubMed] [Google Scholar]
- 20. Martínez-Donate AP, Zellner JA, Sañudo F, et al. Hombres Sanos: evaluation of a social marketing campaign for heterosexually identified Latino men who have sex with men and women. Am J Public Health 2010;100:2532–40. 10.2105/AJPH.2009.179648 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Tarr P, Boffi El Amari E, Haerri D, et al. Hiv Prä-Expositionsprohylaxe (PreP). Schweiz Med Forum 2017;17:579–82. 10.4414/smf.2017.03004 [DOI] [Google Scholar]
- 22. Chen H-T. Practical program evaluation: assessing and improving planning, implementation, and effectiveness. Thousand Oaks, CA: Sage, 2005. [Google Scholar]
- 23. Frost DM, Meyer IH. Measuring community connectedness among diverse sexual minority populations. J Sex Res 2012;49:36–49. 10.1080/00224499.2011.565427 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Drummond MF, Sculpher MJ, Torrance GW, et al. Methods for the economic evaluation of heatlh care programmes. Oxford: Oxford University Press, 2005: 55–94. [Google Scholar]
- 25. Mayring P, Analysis QC. Qualitative Content Analysis : Flick U, von Kardoff E, Steinke I, A companion to qualitative research. London: Sage, 2004: 266–9. [Google Scholar]
- 26. Flowers P, McDaid LM, Knussen C. Exposure and impact of a mass media campaign targeting sexual health amongst Scottish men who have sex with men: an outcome evaluation. BMC Public Health 2013;13:737 10.1186/1471-2458-13-737 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Laga M, Rugg D, Peersman G, et al. Evaluating HIV prevention effectiveness: the perfect as the enemy of the good. AIDS 2012;26:779–83. 10.1097/QAD.0b013e328351e7fb [DOI] [PubMed] [Google Scholar]
- 28. Erens B, Burkill S, Couper MP, et al. Nonprobability web surveys to measure sexual behaviors and attitudes in the general population: a comparison with a probability sample interview survey. J Med Internet Res 2014;16:e276 10.2196/jmir.3382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Evans AR, Wiggins RD, Mercer CH, et al. Men who have sex with men in Great Britain: comparison of a self-selected Internet sample with a national probability sample. Sex Transm Infect 2007;83:200–5. 10.1136/sti.2006.023283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. UNAIDS 90–90–90 an ambitious treatment target to help end the AIDS epidemic, 2014. Available: http://www.unaids.org/en/resources/documents/2017/90-90-90
- 31. McCormack S, Dunn DT, Desai M, et al. Pre-Exposure prophylaxis to prevent the acquisition of HIV-1 infection (PROUD): effectiveness results from the pilot phase of a pragmatic open-label randomised trial. The Lancet 2016;387:53–60. 10.1016/S0140-6736(15)00056-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Molina J-M, Capitant C, Spire B, et al. On-Demand preexposure prophylaxis in men at high risk for HIV-1 infection. N Engl J Med Overseas Ed 2015;373:2237–46. 10.1056/NEJMoa1506273 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2019-032459supp001.pdf (758.7KB, pdf)