Abstract
Objective
In this study, we assess the performance of public hospitals in Saudi Arabia. We detect the sources of inefficiency and estimate the optimal levels of the resources that provide the current level of health services. We enrich our analysis by employing locations and capacities of the hospitals.
Design
We employ data envelopment analysis (DEA) to measure the technical efficiency of 91 public hospitals. We apply the input-oriented Charnes, Cooper and Rhodes, and Banker, Charne, Cooper models under Constant and Variable Returns-to-Scale. The assessment includes four inputs, and six output variables taken from the Ministry of Health databases for 2017. We conducted the assessment via PIM-DEA V.3.2 software.
Setting
Ministry of health-affiliated hospitals in the Kingdom of Saudi Arabia.
Results
Findings identified 75.8% (69 of 91) of public hospitals as technically inefficient. The average efficiency score was 0.76, indicating that hospitals could have reduced their inputs by 24% without reduction in health service provision. Small hospitals (efficiency score 0.79) were more efficient than medium-sized and large hospitals. Hospitals in the central region were more efficient (efficiency score 0.83), than those located in other geographical locations. More than half of the hospitals (62.6%) were operating suboptimally in terms of the scale efficiency, implying that to improve efficiency, they need to alter their production capacity. Performance analysis identified overuse of physician’s numbers and shortage of health services production, as major causes of inefficiency.
Conclusion
Most hospitals were technically inefficient and operating at suboptimal scale size and indicate that many hospitals may improve their performance through efficient utilisation of health resources to provide the current level of health services. Changes in the production capacity are required, to facilitate optimal use of medical capacity. The inefficient hospitals could benefit from these findings to benchmarking their system and performance in light of the efficient hospital within their capacity and geographical location.
Keywords: Technical efficiency, Data envelopment analysis, Saudi Arabia, Public hospitals, General hospitals efficiency
Strengths and limitations of this study.
The study challenged to find data on economic values, the severity of cases and the quality of services. We expanded the selection of the variables to cover a broad range of health services and resources in the hospitals.
The hospital mortality rate was included in output variables as a proxy of the service quality in the studied hospitals.
We did not apply output-oriented data envelopment analysis models, alternatively, we adopted input orientation, since we aimed to estimate the optimum levels of the resources without deteriorating the health services.
Further estimation of the optimal levels of resources is required, to examine the allocation of these resources among the hospitals.
This is the first performance assessment of public hospitals in Saudi Arabia that uses real data obtained directly from official databases of the Ministry of Health.
Introduction
Increasing demand for healthcare and the expenditure required to provide efficient, equitable and effective healthcare systems, are the global concerns. The Kingdom of Saudi Arabia (KSA) has experienced these recently, alongside substantial population growth, increased life expectancy and the proliferation of lifestyle-related disease. These have increased the demand for health services at a time of the scant resource.1–3
During 2015, KSA government spending on health was 71.3% of the country’s total health expenditure, which corresponds to 4.1% of GDP for that year.4 Healthcare expenditure in KSA increased by 24.7% between 2013 and 2017 (table 1).1 2 5 While public spending on health in KSA is remarkably high in comparison to many high-income countries (71.3% for KSA vs 61.2% for high-income countries), the number of hospital beds is considerably lower.3 4 In other words, the cost of each hospital bed in the KSA is remarkably higher than those in other high-income countries.
Table 1.
Budget appropriations for the ministry of health (MOH) with respect to government budget (SR=Saudi Riyal)
| Year | Government budget billion SR |
MOH budget billion SR | Percentage of MOH to the government budget | No of hospitals | No of beds |
| 2013 | 820 | 54.3 | 6.63 | 268 | 38 970 |
| 2014 | 855 | 59.9 | 7.02 | 270 | 40 300 |
| 2015 | 860 | 62.3 | 7.25 | 274 | 41 297 |
| 2016 | 840 | 58.9 | 7.01 | 274 | 41 835 |
| 2017 | 890 | 67.7 | 7.61 | 282 | 43 080 |
Source; MOH; Statistical yearbook, 2017.
Although much has been done to promote the efficient use of resources, this has proven insufficient to meet the rising health expenditure and demand for healthcare in KSA.6 7 Providers seem to find it very challenging to deliver adequate provision using current resources.8 There seems to be an imbalance between health service availability and health spending, so better use of resources is necessary if KSA is to have an efficient and appropriate health system.7 It is thus important to investigate how existing resources can be used more efficiently for meeting the demand for healthcare in the country.
Governments worldwide conduct performance assessments of their health sectors, to ensure that public funds are effectively used.9 Efficiency evaluation is carried out under different concepts, such as technical, allocative, cost and overall efficiency.9 Of these, the technical efficiency approach is most commonly used. This is based on Farrell’s theory of 1957, which introduced a measure of technical efficiency based on comparison of the inputs and outputs of set entities, called decision-making units (DMUs).10
Hospital efficiency is crucial to the efficiency of the health system generally, as hospitals are key consumers of health resources.11 12 Hanson et al found that public hospitals consume around 40% of the total health budget in many sub-Saharan African countries.11 Public hospitals used almost 44% of the health spending in the UK in 2012/2013.13
In general, there is a scarcity of studies and empirical works on the performance assessment of public hospitals, and this rarity is particularly acute in the context of KSA.14 Systematic review of public hospital efficiency studies in the Gulf region and similar countries has shown the number of studies to be limited, as efficiency analysis is a novel approach to research in the Gulf, including KSA.14 The review found only two studies based in KSA context; a study by Helal and Elimam in 2017,15 which assessed the efficiency of health services at districts level in KSA. Another efficiency analysis conducted in 2013 of 20 public hospitals, under private sector management, which found that 60% of the study sample had not achieved the efficient score.16
Hospital efficiency has hitherto been measured mainly by frontier analysis methods, either through non-parametric data envelopment analysis (DEA) or as parametric stochastic frontier analysis (SFA).9 These methods compare hospital performance with an estimated efficient frontier comprising the best-performing hospitals.17 18
DEA has for many years been the most commonly used technique for measuring the relative efficiency in healthcare.12 19 Systematic reviews of efficiency studies have often identified that DEA to be the predominant method of public hospital efficiency assessments among studies reviewed.12 14 19 Hollingsworth and Hollingsworth conducted systematic reviews of efficiency analysis internationally and noticed that DEA was used in around the half of studies, a further fifth used DEA in with some form of secondary regressions.12 19 Another review,18 of efficiency in Iranian hospitals, found DEA was applied in all reviewed studies; three of those studies also used SFA to estimate efficiency scores. A systematic review of health system efficiency studies in the organization for economic, co-operation and development (OECD) countries20 found that DEA was applied in 64% of them.
In this study, we conduct a performance assessment of the Ministry of Health (MOH)-administered general hospitals in KSA. We measure the technical efficiency of public hospitals and identify the sources of inefficiency and estimate the optimal levels of the resources. We also provide subscriptions for improvements so as the inefficient hospitals to be rendered efficient. At a post-optimality phase, we enrich our analysis by employing information about the geographical location and the capacity (number of beds) of the hospitals. Thus, this performance assessment provides useful information to the decision-makers, which can be employed for policy reforms, to optimise the use of health resources in public hospitals and consequently improve the efficiency of healthcare systems.
Public health system in KSA
Under article 31 of the national constitution, the KSA government guarantees free medical care to all citizens.8 The government finances the public sector annually, largely from revenue derived from oil and gas production.21 Table 1 shows the proportion of national budget allocated to the KSA’s MOH.5 Thus, the available resources should be used optimally.
The MOH is the primary provider of healthcare services in KSA, administering 60% of all provision.22 It is the dominant provider of health services in the public sector.22 23 Other government agencies, including the Ministry of Defence, the national guard and universities, share the remaining of healthcare provision, as does the private sector.21 The MOH delivers primary, secondary and tertiary healthcare through 2361 primary healthcare centres and 282 hospitals, administering 43 080 beds throughout the country.5 Other MOH functions include strategic planning, formulation of health policy, supervision of all health service delivery programmes and the monitoring and management of all other health-related activities.22 Public (MOH-affiliated) hospitals in KSA can be broadly classified into two groups, general hospitals with different capacities (number of beds) and specialised hospitals. General hospitals provide a wide range of health services, while specialised hospitals deliver health services for a specific health condition or to a particular group of beneficiaries. General hospitals in KSA are located in various geographical locations and serve populations of different demographic characteristics and needs, which may affect the hospital performance, as observed in other studies.8 24
Methods
Population and selection of sample
As the application of DEA is based on a homogeneous (comparative) sample that use similar inputs to produce similar outputs, we focused on examining the technical efficiency for general hospitals.9
Hollingsworth, and Varabyova and Müller argued that the hospitals under evaluation should be of same type and provide the same services and health activities.19 20 Since the inclusion of divergent specialist units in the same sample will confound the results—frontier techniques are susceptible to outliers.19 20 Specialised hospitals often lack types of secondary service, for example, surgical operations rarely occur in psychiatric hospitals, and such hospitals, if included, will appear as inefficient while surgery is a considered as one of the outputs.18 19 25 Specialised hospitals were, therefore, excluded from this analysis. Similarly, small hospitals (with 50 beds or fewer) provide primary care services while lacking secondary and tertiary health services, and consequently miss a significant number of output variables (eg, inpatient services, patient discharge, surgical operations, laboratory testing) compared with bigger hospitals. In this study, we excluded also the smaller hospitals, to ensure greater homogeneity in performance evaluation across the units.9 26
Ultimately, the homogeneous sample used in the analysis included 21 528 out of 39 868 (54%) of the total active hospital beds provided by the MOH in KSA. We included in the assessment 97 general hospitals and removed six of them, due to missing data. The data of hospital inputs and outputs for 2017 were collected by the lead author from official statistical, informational and research databases of Administration of Statistics and Information and Administration of Research and Studies, which affiliated of the MOH, following approval from the designated authority. Data collection took place from May to July 2018.
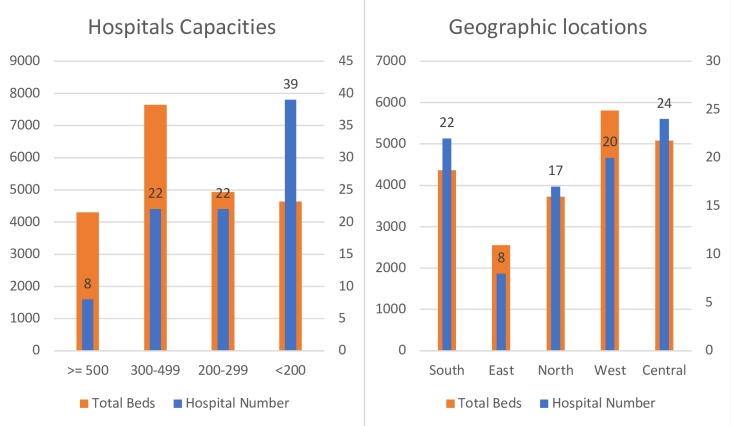
The sample hospitals are in 64 cities, affiliated to 20 administrative districts, located in five geographical regions, namely central, west, east, south and north regions. The general hospitals in the sample are classified into four groups based on their capacity (number of beds): small (fewer than 200 beds), lower-medium (200–299 beds), upper-medium (300–499 beds) and large (500 or more beds) hospitals, following Gok and Sezen’s27 categorisation. However, these hospitals are affiliated, organised and funded by the MOH, and have not autonomy in term of funding or organising structure by themselves or other agents. Thus, we applied the DEA model for all 91 hospitals. Then, we presented the efficiency scores in each capacity and each geographical location. Figure 1 illustrates number of hospitals and hospital beds in each category of capacity and location.
Figure 1.
Number of hospitals and hospital beds in each capacity and geographical location, 2017
Inputs and outputs
The selection of input and output variables is a crucial step in performance measurement, because the results of any efficiency assessment depend significantly on the variables used in the estimation models.28 The literature has focused on labour (eg, health professionals) and capital (eg, number of beds), as input variables, while some studies included consumable resources.9 28 The main categories of output used in healthcare-related efficiency studies were healthcare activities (eg, number of outpatient visits, inpatient services, number of surgeries) and health outcomes (eg, mortality rate).9 18 20
In our study, we selected the hospital outputs that dependent on the selected inputs, which cover a broad range of health services provided and health resources used by public hospitals in KSA. In particular, four inputs and six outputs were chosen based on the availability of the data in KSA context, which were rationally approved in previous theoretical and empirical studies.9 12 19
The input variables chosen are: (1) number of hospital beds; (2) number of full-time physicians; (3) number of full-time nurses and (4) number of full-time allied health personnel (ie, pharmacists, midwives, medical technicians, medical radiologists, physiotherapists) employed in the hospital. The output variables used in this study are: (1) outpatient visits (number of patients receiving outpatient treatment within a year); (2) discharged patients (number of patients receiving inpatient treatment within a year); (3) total number of surgical operations during the year; (4) number of radiological investigations conducted in hospital during the year; (5) number of laboratory tests during the year; (6) hospital mortality rate (ratio of inpatient deaths during hospitalisation to the total number of inpatients that year). The last output variable is an indicator of health service quality and health outcomes in hospital, as argued by Sahin and Ozcan.29 Reduction in the mortality rate and increase quantity of life signify an improvement in the health outcomes of the public hospital of investigation. Therefore, mortality rate could be a proxy for a weighted health quality measure in our assessment.30 The inverse value for the mortality rate (one divided by mortality rate) is included as an output value in the assessment, meaning that hospitals with higher mortality rate would have a smaller ratio as output values.29 As the model assumes that output and input variables are isotonic, (ie, increased input reduces efficiency as well as increased output increases efficiency). We had to apply this correction, otherwise, a higher mortality rate would incorrectly contribute to a better hospital outcome.30
The number of hospitals (DMUs in DEA context) should be at least two times larger than the sum of inputs and outputs.31 However, Hollingsworth32 suggested that the number of units used in efficiency assessment should be at least three times the sum of inputs and outputs. In accordance to the above-mentioned rule of thumb, in this study, we include 91 hospitals, more than three times the combined number of input and output variables.
Patient and public involvement
No patients were involved in this study, and we used anonymous data from MOH databases.
Data envelopment analysis
DEA is a powerful technique that is based on linear programming. It was developed for measuring the performance of a set of comparable entities, called DMUs, which convert multiple inputs into multiple outputs.26 32 In this method, each hospital is compared against the estimated efficient frontier comprising the best-performing hospitals.17 18
DEA has been already the most commonly used technique for measuring the relative efficiency in healthcare.12 19 In systematic reviews, we can observe that DEA is the predominant method of public hospital efficiency assessment.12 14 19 DEA is widely applicable since does not require any a priori specification of the underlying functional form that relates the inputs with the outputs.9 In addition, use of DEA is justified by its ability to incorporate multiple inputs and outputs in different units of assessment.9 32
Several DEA models have been developed to analyse the efficiency based on Farrell’s concept.10 The most well known and basis for the rest DEA models is the Charnes, Cooper and Rhodes (CCR) model developed by Charnes et al,33 which assumes that production has Constant Returns to Scale (CRS) and the Banker, Charne, Cooper (BCC) model developed by Banker et al,34 under the assumption of Variable Returns to Scale (VRS).9 12 The choice of CCR or BCC model depends on the context of the problem under examination, that is, the technology linking the inputs to outputs in the transformation process.9
Generally, the CCR model— whereby the efficiency frontier has a constant slope (CRS), which means that any change in the inputs results to a proportional change in the outputs.26 CRS may be adopted when machines are involved in the process, which roughly means that the production can be doubled by doubling the levels of inputs. However, when employees (human factor) participate in the production process, then it is naive to expect that they could work at a constant rate. The CCR efficiency assessment by the may be affected if the DMUs are not operating on the optimal scale, since CRS does not distinguish between the scale and pure (managerial) technical efficiency.35 If the efficiency analysis considers a managerial perspective, a BCC technology assumption will be appropriate to understand if a scale of operations or provider’s practice affects productivity.27 36 Scale efficiency (SE) is defined as a ratio of CRS to VRS efficiency scores and provides evidence whether the DMU is operating on the optimal scale size.12 20 Furthermore, the efficiencies of DMUs can be comprehensively analysed using both CRS and VRS assumption for more realistic changes in production process, and implications in the real world.9 26 Other systematic reviews20 25 have reported similar findings where studies used both CRS and VRS assumptions in efficiency measurements.
Rationally, the commonly used orientations in DEA analysis are input orientation (ie, minimisation of inputs with the given amount of outputs) and output orientation (ie, inputs are held constant and outputs are proportionally increased).26 Previous empirical studies35 have argued that hospitals have relatively little control over their outputs (eg, expanding surgical operations), but more control over the inputs (eg, medical devices), where they have the social responsibility to provide medical treatment through the public hospitals in general. Thus, most studies adopt input orientation for efficiency assessment of the hospitals.20 25 37 In a few studies, output orientation is adopted in response to the strategic health plans of the countries aiming to expand healthcare provision during a specific period.38 39 However, in our study, we aim to estimate the optimal levels of the resources without deteriorating the levels of the health services that the hospitals provide. In this way, we provide the central authorities with the potential savings that could be made in the health sector.
The efficiency of a hospital is defined as the ratio of the weighted sum of outputs (total virtual output) to the weighted sum of inputs (total virtual input), with the weights being obtained in favour of each evaluated unit by the optimisation process. Assume n DMUs, each using m inputs to produce s outputs. We denote the vector of inputs for DMU j is and the vector of outputs is . The model (1) is formulated and solved for each hospital in order to obtain its efficiency score. The variables η=(η1,…,ηm) and ω=(ω1,…,ωs) are the weights associated with the inputs and the outputs respectively. These weights are calculated in a manner that they provide the highest possible efficiency score for each hospital jo under evaluation.
The input-oriented BCC model that provides the efficiency for the hospital jo under VRS assumption is given below:
| (1) |
Notice that by excluding the free of sign variable ωο from model (1), the CCR model is obtained. The fractional model (1) can be transformed to a linear programme by applying the Charnes and Cooper transformation (C-C transformation hereafter).40 The transformation is carried out by considering a scalar such as and multiplying all terms of model (1) with t> 0 so that v=tη, u=t ω, uο=tωο. The linear equivalent of model (1) is formulated as:
| (2) |
Once an optimal solution v*, u*, uο* of model (2) is derived, the input-oriented BCC-efficiency for the hospitaljo under evaluation is obtained directly from the objective function.
Banker et al determined the Returns to Scale (RTS) using the optimal value of the free variable uo in the multiplier model (2).34 Given the point that lies on the efficient frontier, the RTS at this point are identified by the following three conditions:
Increasing Returns to Scale (IRS) prevail at if and only if for all optimal solutions. Meaning the increase in all production factors (inputs) resulted in more production (outputs).
Decreasing Returns to Scale (DRS) prevail at if and only if for all optimal solutions, meaning an equal increase in all production factors led to less production.
CRS prevail at if and only if in any optimal solutions, where equal increase in all production factors led to the same amount of increase in production.
Improvement management software (PIM-DEA V.3.2) was used for DEA analysis.41
Results
Descriptive statistics, concerning the inputs and outputs of 91 general hospitals during 2017, are presented in table 2. The average hospital size is 236.57 beds, with a range of 100–711 beds. Full-time physicians ranged from 38 to 894, with a mean of 212. The number of nurses is on average 495 but ranged from 74 to 1930. Full-time allied health personnel ranged from 37 to 1149, with an average of 280.
Table 2.
Descriptive statistics of the inputs and outputs of the 91 hospitals
| Mean | SD | Min | Max | |
| Inputs | ||||
| Hospital beds | 236.6 | 137.6 | 100 | 711 |
| Physicians | 212.3 | 168.7 | 38 | 894 |
| Nurses | 495.2 | 403.6 | 74 | 1930 |
| Allied health personnel | 280.1 | 219.1 | 37 | 1149 |
| Outputs | ||||
| Outpatient visits | 72 986.5 | 72 475.3 | 1785 | 466 608 |
| Discharged patients | 26 016.4 | 55 856.4 | 19 | 503 216 |
| Surgical operations | 2638.4 | 2151.2 | 172 | 9464 |
| Laboratory tests | 965 840.8 | 1 095 415.6 | 794 | 5 512 774 |
| Radiology investigations | 53 531.4 | 46 788.7 | 107 | 221 980 |
| Hospital mortality rate | 0.0224 | 0.0212 | 0.0003 | 0.125 |
Concerning the outputs, the average number of patient visits to outpatient departments is 72 986 and ranged from 1785 to 466 608 visits. Discharged patients receiving inpatient services during 2017 averaged 26 016, ranging from 19 to 503 216. Surgical operations ranged from 172 to 9464 with a mean of 2638 surgeries per hospital. Means for laboratory and radiology tests are 965 840 and 53 531, respectively, during 2017. Average mortality rate is 2.24%.
Table 3 presents the results of DEA models, summary statistics of average technical (CRS and VRS) efficiency, and SE scores, as well as concerning the return to scale.
Table 3.
Technical efficiency scores and returns to the scale of the public hospitals in KSA
| CRS technical efficiency | VRS technical efficiency | Scale efficiency | CRS (N (%)) | IRS (N (%)) | DRS (N (%)) | |
| All hospitals (n=91) | ||||||
| Mean | 0.76 | 0.87 | 0.87 | 34 (37.4) | 40 (44) | 17 (18.6) |
| SD | 0.23 | 0.18 | 0.18 | |||
| Min | 0.11 | 0.30 | 0.19 | |||
| No full score | 22 (24.2%) | 47 | 25 | |||
| Large hospitals: ≥500 beds (n=8) | ||||||
| Mean | 0.65 | 0.75 | 0.87 | 2 (25) | 1 (12.5) | 5 (62.5) |
| SD | 0.27 | 0.30 | 0.13 | |||
| Min | 0.28 | 0.30 | 0.59 | |||
| No full score | 1 (12.5%) | 4 | 1 | |||
| Upper-medium hospitals: 300–499 beds (n=22) | ||||||
| Mean | 0.76 | 0.80 | 0.94 | 7 (31.8) | 5 (22.7) | 10 (45.5) |
| SD | 0.19 | 0.19 | 0.07 | |||
| Min | 0.39 | 0.41 | 0.76 | |||
| No full score | 3 (13.6%) | 7 | 3 | |||
| Lower-medium hospitals: 200–299 beds (n=22) | ||||||
| Mean | 0.73 | 0.79 | 0.90 | 10 (45.5) | 10 (45.5) | 2 (9.1) |
| SD | 0.25 | 0.19 | 0.18 | |||
| Min | 0.11 | 0.50 | 0.22 | |||
| No full score | 4 (18.2%) | 4 | 4 | |||
| Small hospitals: <200 beds (n=39) | ||||||
| Mean | 0.79 | 0.96 | 0.82 | 15 (38.5) | 24 (61.5) | 0 (0) |
| SD | 0.23 | 0.09 | 0.22 | |||
| Min | 0.19 | 0.67 | 0.19 | |||
| No full score | 13 (33.3%) | 31 | 13 | |||
CRS, Constant Returns to Scale; DRS, Decreasing Return to Scale; IRS, Increasing Returns to Scale; KSA, Kingdom of Saudi Arabia; SD, standard deviation; VRS, Variable Returns to Scale.
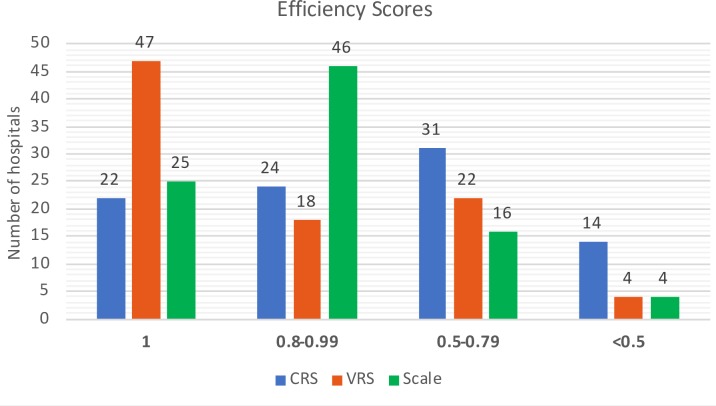
The average CRS technical efficiency score for MOH general hospitals is 0.76, with an SD of 0.23, which indicates that these hospitals could reduce use of all their inputs on average by 24% without any reduction in the number of services provided. Also, the VRS technical score on average is 0.87 (SD 0.18). The distribution of technical, pure technical and SE scores is given in figure 2.
Figure 2.
Distribution of technical efficiency scores of the hospitals on technical (CRS), pure technical (VRS) and scale efficiencies. CRS, Constant Returns to Scale; VRS, Variable Returns to Scale.
The lowest technical efficiency score reported is 0.11, but 22 hospitals out of 91 (24.2%) are both technically and scale efficient, which indicates that these hospitals use optimally their inputs. Among the inefficient hospitals 55 hospitals (60.4%) achieved efficiency scores of at least 0.50 efficiency level (figure 2) and 14 hospitals (15.4%) reported efficiency scores below 0.50. Average SE scores are 0.87, with (SD 0.18). Although 47 hospitals (52%) reported an efficient score on VRS (pure efficiency), only 25 (27%) hospitals are efficient on the scale.
Concerning the RTS, we have found that 34 hospitals (37.4%) operate under CRS; while 40 hospitals (44%) operate under IRS, and 17 hospitals (18.6%) DRS, However, hospitals that were operating on either IRS or DRS needed to alter their capacity to operate on the optimal scale size, that is, at the CRS, which would be required to achieve technical efficiency.
We present in table 3 the efficiency scores of the 91 hospitals for each capacity (size category). From the capacity perspective, small hospitals had higher levels of technical (CRS and VRS) efficiencies than medium-sized (both lower-medium and upper-medium) and large hospitals. Table 3 shows that small hospitals have on average technical efficiency of 0.79 (SD 0.23); one-third of the hospitals in this category are technically and the scale efficient. Average technical efficiency of lower-medium hospitals is 0.73 (SD 0.25), with a higher percentage of inefficient hospitals (81.8%), than for small hospitals. Although upper-medium-sized hospitals reported a slightly higher average technical efficiency score of 0.76 (SD 0.19), fewer hospitals in this category reported an efficient score, meaning a higher percentage of inefficiencies (86.4%). Large hospitals were the least efficient when compared with other categories. The average technical efficiency of large hospitals was 0.65 (SD 0.27), only one was technically efficient.
Regarding scale-efficiency scores, upper-medium (0.94) and lower-medium (0.90) sized hospitals operate at a more optimal scale than small (0.82) or large hospitals (0.87). Also, 45.5% of lower-medium hospitals operate on the CRS, followed by small hospitals (38.5%). However, most of the remaining hospitals in these categories, that is, lower-medium (45.5%) and small size (61.5%) hospitals are operating on IRS. In contrast, most large hospitals (62.5%) showed DRS, and two of them were on CRS, indicating a need to downsize these hospitals to improve technical efficiency. Similarly, 45.5% of upper-medium-sized hospitals operate on DRS and one-third of this category are operating (CRS).
Table 4 shows the average efficiency scores in five geographical regions, however, based on the analysis of all 91 hospitals together. Hospitals in the central region reported the highest average technical efficiency score of 0.83 (SD 0.18), followed by eastern hospitals with an average score of 0.80 (SD 0.28). Hospitals in western KSA reported the least average score, 0.68 (SD 0.20).
Table 4.
Technical efficiency scores and returns to the scale of the hospitals categorised by location
| CRS technical efficiency | VRS technical efficiency | Scale efficiency | CRS (N (%)) | IRS (N (%)) | DRS (N (%)) | |
| South region hospitals (n=22) | ||||||
| Mean | 0.75 | 0.89 | 0.83 | 9 (40.9) | 9 (40.9) | 4 (18.2) |
| SD | 0.25 | 0.18 | 0.23 | |||
| Min | 0.11 | 0.41 | 0.22 | |||
| No full score | 4 (18.2%) | 13 | 4 | |||
| East region hospitals (n=8) | ||||||
| Mean | 0.80 | 0.85 | 0.90 | 4 (50) | 1 (12.5) | 3 (37.5) |
| SD | 0.28 | 0.21 | 0.16 | |||
| Min | 0.27 | 0.50 | 0.54 | |||
| No full score | 1 (12.5%) | 4 | 1 | |||
| North region hospitals (n=17) | ||||||
| Mean | 0.75 | 0.84 | 0.90 | 7 (41.2) | 9 (52.9) | 1 (5.9) |
| SD | 0.28 | 0.23 | 0.20 | |||
| Min | 0.19 | 0.30 | 0.19 | |||
| No full score | 6 (35.3%) | 9 | 6 | |||
| Central region hospitals (n=24) | ||||||
| Mean | 0.83 | 0.89 | 0.93 | 10 (41.7) | 11 (45.8) | 3 (12.5) |
| SD | 0.18 | 0.16 | 0.10 | |||
| Min | 0.49 | 0.50 | 0.69 | |||
| No full score | 8 (33.3%) | 12 | 8 | |||
| West region hospitals (n=20) | ||||||
| Mean | 0.68 | 0.85 | 0.81 | 4 (20) | 10 (50) | 6 (30) |
| SD | 0.20 | 0.17 | 0.17 | |||
| Min | 0.37 | 0.42 | 0.46 | |||
| No full score | 3 (15%) | 9 | 3 | |||
CRS, Constant Returns to Scale; DRS, Decreasing Returns to Scale; IRS, Increasing Returns to Scale; SD, Standard Deviation; VRS, Variable Returns to Scale.
The percentage of efficient hospitals in the north (35.3%) and the central (33.3%) regions are higher than the other regions. The eastern, western and southern regions have a higher percentage of inefficient hospitals. Both central and southern regions reported relatively higher VRS efficiency score of 0.89. In terms of average SE scores, central region hospitals (0.93), and hospitals in the north and east (both 0.90) were operating at more optimal scale than those in the west (0.81) and south (0.83). Half of the sample hospitals in the east region operate on CRS, followed by hospitals in the central and north regions (both 41%). The findings also revealed that 52.9% of north region hospitals were operating on IRS, while 37.5% of east region hospitals were operating on DRS.
The performance analysis identified the slacks, which showed either excess input utilisation or shortages of output production. Table 5 shows the average amount of slack in hospitals deemed inefficient. These results represent the combined scores of slack for all inefficient hospitals, for each input and output. Table 5 also shows the percentage of change (slacks) in the number of inputs or outputs required to eliminate the inefficiencies and achieve target levels.
Table 5.
Slacks evaluation for inefficient hospitals
| Input slacks | Mean (SD) | Percentage of change |
| Hospital beds | 48.4 (76.6) | −20.4 |
| Physicians | 47.5 (72.6) | −22.4 |
| Nurses | 102.9 (173.1) | −20.8 |
| Allied health personnel | 58.38 (98.3) | −20.84 |
| Output slacks | ||
| Outpatient visits | 8866.1 (23712) | 12.2 |
| Discharged patients | 3700.6 (8214.2) | 14.2 |
| Surgical operations | 282.6 (730.9) | 10.7 |
| Laboratory tests | 66 105.6 (140332.4) | 6.8 |
| Radiology investigations | 2204.6 (6944.1) | 4.1 |
| Mortality rate | 0.006 (0.014) | 21.7 |
In terms of inputs, results show that an excess of physicians was the main cause of inefficiencies in public hospitals. A feasible, achievable reduction in the number of physicians was on average 22.38% of the current values (compared with the amounts given in table 2). The next most substantial slack was observed in allied health personnel, at 20.84%. Surpluses of hospital beds and nurses were also important causes of inefficiency and should be reduced on average by 20.44% and 20.77%, respectively. In addition to the input reduction, the average number of services should be increased to meet targets. Furthermore, the quality of health services in public hospitals would have improved with a decrease in the hospital mortality rate.
Discussion
This study evaluated the technical efficiency of public hospitals affiliated to the KSA’s MOH, using DEA. Analysis showed 75% of sample hospitals could not use their intact resources to generate specified outputs. The average CRS technical efficiency score was 0.76, indicating that hospitals could produce their current level of outputs with 76% of inputs currently used, and thereby achieve efficiency. Efficiency scores ranged from 0.11 to 1.00 (figure 2), revealing considerable variations in efficiency scores among hospitals. Moreover, the average VRS technical efficiency and SE scores were both 0.87. This indicated that inefficiency might be due to administrative gaps to overcome external environmental factors, and limitations in managing internal operations in the hospitals. Notably, Helal and Elimam15, assessed the efficiency of health services at districts level in KSA based on MOH data 2014, found an average efficiency score of 0.92, and 45% of the districts achieved the technical efficiency score. An efficiency analysis of 20 public hospitals, under private sector management in KSA, found that 60% of the study sample had not achieved the efficient score, with an average score of 0.84.16
Results of the study presented here suggest that small hospitals were relatively more technically efficient than medium-sized and large hospitals (table 2). Other efficiency studies have reported similar findings: Gok and Sezen27 found that small hospitals achieved higher efficiency scores than medium-sized and large ones. This might be due to the differing locations and missions of small and large hospitals.27 36 In this study’s sample, small hospitals were mainly in peripheral cities and towns in KSA, which lacked other sources of public or private healthcare. Service provision in those hospitals might be relatively high compared with the health resources used. Large hospitals (500 or more beds) tended to be in larger cities in urban areas, where many other health providers shared the healthcare of much of the urban population, which might generate a relatively decreased level of health services production in respect of inputs used.
Regarding the different missions, large hospitals consumed a high amount of health resources to meet the various requirements of comprehensive care.27 Since some of these were teaching hospitals, however, teaching activities were not counted in the outcome measurements.27 28 In such large hospitals, treatment processes might be more complicated, and some of the productions of these hospitals could not be assessed in the hospital outcomes.42
This study found 57 hospitals (62.6%) operating on non-optimal scale size; 44% were operating on the IRS, while 18.6% showed DRS (table 3). This indicated that the efficiency of healthcare in KSA might be improved through downsizing of hospitals on DRS and reallocating these inputs to the hospitals operating in the IRS. Moreover, five out of eight large hospitals (500 or more beds) were operating on DRS, implying that to improve efficiency, they needed to reduce their production capacity. This is supported by other research findings.43
This study found that 61.5% of small hospitals had been operating on IRS, none was on DRS. It can, thus, be argued, like Kiadaliri et al, that the increase of capacity (inputs) of this category should be increased by reallocating resources from the larger hospitals for improving efficiency.43 The efficient scale of public hospitals was in medium-sized establishments (200–499 beds). Although half of the hospitals located in the east were operating on the most productive scale size (CRS), three were operating on DRS. Around 53% of the hospitals in the north were operating on IRS, whereas 30% of western region hospitals, which reported the lowest efficiency scores, were operating on DRS.
Our analysis found that hospitals located in the west region were relatively less efficient than hospitals located in other regions. The central region hospitals appeared to be the efficient. Atılgan24 reported in the same line as our findings, that is, location-specific differences in efficiency scores for general MOH hospitals in Turkey. Atılgan argued that this could be due to case mix and/or case severity differences between hospitals. We observed that five out of eight large hospitals in our sample are located in the west region. We can argue that hospitals in the west region might be treating more severe cases than hospitals in other regions in KSA, which might have led to different levels of efficiency scores in hospitals across regions.18 Another explanation could be that hospitals in this region consumed more inputs in anticipation of the annual pilgrimage season, for which government of KSA allocates more resources to such hospitals.
Regardless of the capacity or location-based performance variations, improving the SE of hospitals would require long-term effort, reflected in amendments to health policies, strategic plans and the autonomy of hospital managers.43 The prevailing ability of patients to access health services should not be compromised while reallocating the resources to the other hospitals until Pareto optimality is achieved.9
The use of DEA can identify sources of inefficiency, helping hospital managers and health policy-makers to reach informed decisions.36 The analysis showed that the number of full-time physicians was slightly larger notable reason for inefficiency than the other factors, with an average excess of 22.4%, from an input perspective. Other inputs among labour variables that showed a surplus in use were the number of nurses and the number of allied health personnel, in addition to excess number of hospital beds (capital variable). Analysis revealed a shortage of outputs production, for example, hospitals needed to increase the number of outpatients and hospitalised inpatient services on average by 12.2% and 14.2% respectively, to be efficient.
Given our findings, health policy-makers may consider redeploying their labour forces from inefficient hospitals to more efficient ones.36 43 Public hospitals can consider taking measures for using existing beds effectively to increase efficiency. For example, in this study, many large hospitals had been operating on DRS; however, most of the small hospitals were operating on IRS. Healthcare administrators should assess the legal conditions and regulations for the effective use of medical capacity in light of the findings of this slack analysis.
It had been argued by Afzali et al 28 and Hollingsworth12 that many hospital databases are compromised by insufficient data on a broad range of hospital functions and care, for example, preventive care, health promotion, staff development activities. Thus, improving hospital’s databases through high-quality data collection and processing techniques—including data from different health provision levels, capturing valid data that reflects the severity of cases and related health services, quality of care and pattern of activities—is very important.29 44 Such improvement would facilitate further efficiency research by indicating weaknesses in healthcare production processes and consequently would guide policy-makers in potential reforms of health policy and directives.
In recent years, KSA has been facing the global trends of rising healthcare costs in addition to high growth rate of population and high prevalence of chronic diseases. The government thus realised that the existing healthcare financing system with oil revenue is unsustainable.45 It, thus, can be argued that optimum use of existing health resources, which is a fundamental requirement for achieving universal health coverage as advised by WHO46 can appropriately be applied for KSA. An application of these findings is useful for high income, and Gulf countries in particular, which have the same health financing systems and comparable demand for health services.2 3 14 Our findings from this current analysis of KSA public hospitals indicated that there is large scope for improving efficiency in using healthcare resources. We recommend the policy-makers to consider the appropriate use of resources within hospitals as well as reallocate resources across hospitals, given the findings of this research. Thus, to meet the efficient use of health resources to ensure the maximum value for money, which is expected to contribute significantly towards achieving universal health coverage in KSA.
The study faced the challenges of finding data on economic values of the inputs, also severity of cases and quality of services of the outputs. We, however, could use the mortality rate as the proxy for quality of services. The performance assessment is devoted on how to use optimally the resources of the health sector in order to provide the given levels of health services. Thus, we rationally adopted input orientation in the assessment. However, DEA methodology also permits the assumption of output orientation. We did not apply output-oriented DEA models because outputs of different type than the ones used in the current study would need to be available.
In this study, we provide the optimal levels of resources that render efficient each hospital given the health services levels that each one of them provides. Further to estimating the optimal levels of resources, a different yet important assessment is to examine the allocation of these resources among the hospitals. This extension is left for future research. Despite a few limitations, the study site (KSA) and data sources might create strong interest among policy-makers, stakeholders, researchers and academics. This is the first research study of technical efficiency based on official data from KSA that has considered public hospital capacities and geographical locations.
Conclusions
Given the scarcity of resources, growing expenditure on health and demand for health services, more attention should be paid to improving the efficiency of healthcare by better utilisation of current resources. In this study, inefficiency existed in most public hospitals, and these could reduce their inputs by 24% without any reduction in service provision. Small hospitals and hospitals in the central region of KSA were relatively more efficient. A high proportion of hospitals were operating at non-optimal scale size, while an efficient scale of operation was observed in medium-sized hospitals. The finding suggests that it would be helpful to adjust production capacity by downsizing hospitals operating on DRS and reallocating the resources to hospitals on the IRS, as reflected in the scale analysis. Performance analysis shows the surplus of the health workers and a shortage of health services to be major causes of inefficiency, implying that health regulators might redeploy their labour forces for effective utilisation of medical capacity. A possible reallocation of resource must take place without compromising patients’ current access to public-funded health services.
Supplementary Material
Acknowledgments
We are grateful for the Ministry of Education and the government of Saudi Arabia for unlimited support. The authors would like to thank of the Administration of Statistics and Information and the Administration of Research and Studies in the Ministry of Health for providing access to the hospital’s databases. Special gratitude to Mr. Nabil A. Othman and Mrs. Nuwayyir Alshalawi at Administration of Statistics and Information for their contributions through permitting to use the administration’s access to the necessary databases to complete the data collection.
Footnotes
Twitter: @atawipd
Contributors: ADA, LWN and JAMK contributed to conceptualising the research question, study design and settings and literature search. ADA contributed to data collection and variable extraction. ADA and JAMK conducted the data analysis, interpretation and writing the manuscript. ADA, LWN and JAMK contributed to writing, reviewing and revising the manuscript. All authors finally reviewed the manuscript critically and approved the final version for submission.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Not required.
Ethics approval: Ethics approval was obtained from the Ethics Committee of Institutional Review Board (IRB) of King Fahad Medical City, the Ministry of Health in Saudi Arabia (IRB log No. 18-166E).
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data were extracted from the hospital databases at Administration of Statistics and Information in The Ministry of Health. Additional data are available if requested.
References
- 1. Khoja T, Rawaf S, Qidwai W, et al. Health care in Gulf cooperation Council countries: a review of challenges and opportunities. Cureus 2017;9:e1586 10.7759/cureus.1586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ardent Advisory & Accounting GCC healthcare sector report. A focus area for governments. Abu Dhabi, UAE, 2015. Available: http://www.ardentadvisory.com/files/GCC-Healthcare-Sector-Report.pdf [Accessed Jan 2018].
- 3. Ram P. Management of healthcare in the Gulf cooperation Council (GCC) countries with special reference to Saudi Arabia. International Journal of Academic Research in Business and Social Sciences 2014;4 10.6007/IJARBSS/v4-i12/1326 [DOI] [Google Scholar]
- 4. The World Bank Country data, 2019. Available: https://data.worldbank.org/country/saudi-arabia [Accessed Jan 2019].
- 5. MOH portal.com Annual statistical book, 2017. Available: https://www.moh.gov.sa/en/Ministry/Statistics/book/Documents/ANNUAL-STATISTICAL-BOOK-1438H.pdf [Accessed Oct 2018].
- 6. Mourshed M, Hediger V, Lambert T. Gulf cooperation Council healthcare: challenges and opportunities. 2007. Arab World Competitiveness Report (Part 5);55–64, World Economic Forum, Geneva, Switzerland 2007. http://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.183.7279&rep=rep1&type=pdf [Google Scholar]
- 7. MOH portal.com Ministry of health strategic plan 2010–2020. Available: https://www.moh.gov.sa/Portal/WhatsNew/Documents/OKIstragi260p.pdf [Accessed October 2018].
- 8. Albejaidi F. Healthcare system in Saudi Arabia: an analysis of structure, total quality management and future challenges. J Alternat Perspec Social Sci 2010;2:794–818. [Google Scholar]
- 9. Jacobs R, Smith P, Street A. Measuring efficiency in health care: Analytic techniques and health policy. Cambridge: Cambridge University, 2006: 3–39. [Google Scholar]
- 10. Farrell MJ. The measurement of productive efficiency. J R Stat Soc Ser A 1957;120:253–90. 10.2307/2343100 [DOI] [Google Scholar]
- 11. Hanson K, Atuyambe L, Kamwanga J, et al. Towards improving Hospital performance in Uganda and Zambia: reflections and opportunities for autonomy. Health Policy 2002;61:73–94. 10.1016/S0168-8510(01)00212-3 [DOI] [PubMed] [Google Scholar]
- 12. Hollingsworth B. Non-Parametric and parametric applications measuring efficiency in health care. Health Care Manag Sci 2003;6:203–18. 10.1023/A:1026255523228 [DOI] [PubMed] [Google Scholar]
- 13. Kelly E, Stoye G, Vera-Hernández M. Public hospital spending in England: evidence from national health service administrative records. Fisc Stud 2016;37:433–59. 10.1111/j.1475-5890.2016.12101 [DOI] [Google Scholar]
- 14. Alatawi A, Ahmed S, Niessen L, et al. Systematic review and meta-analysis of public hospital efficiency studies in Gulf region and selected countries in similar settings. Cost Eff Resour Alloc 2019;17:17 10.1186/s12962-019-0185-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Helal SMA, Elimam HA. Measuring the efficiency of health services areas in Kingdom of Saudi Arabia using data envelopment analysis (DEA): a comparative study between the years 2014 and 2006. Int J Econ Finance 2017;9:172–84. 10.5539/ijef.v9n4p172 [DOI] [Google Scholar]
- 16. Abou El-Seoud M. Measuring efficiency of reformed public hospitals in Saudi Arabia: an application of data envelopment analysis. Int J Econ Manag Sci 2013;2:44–53. [Google Scholar]
- 17. Hussey PS, de Vries H, Romley J, et al. A systematic review of health care efficiency measures. Health Serv Res 2009;44:784–805. 10.1111/j.1475-6773.2008.00942.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kiadaliri AA, Jafari M, Gerdtham U-G. Frontier-based techniques in measuring Hospital efficiency in Iran: a systematic review and meta-regression analysis. BMC Health Serv Res 2013;13:312 10.1186/1472-6963-13-312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Hollingsworth B. The measurement of efficiency and productivity of health care delivery. Health Econ 2008;17:1107–28. 10.1002/hec.1391 [DOI] [PubMed] [Google Scholar]
- 20. Varabyova Y, Müller J-M. The efficiency of health care production in OECD countries: a systematic review and meta-analysis of cross-country comparisons. Health Policy 2016;120:252–63. 10.1016/j.healthpol.2015.12.005 [DOI] [PubMed] [Google Scholar]
- 21. Al-Homayan A, Shamsudin F, Subramaniam C, et al. Analysis of health care system — resources and nursing sector in Saudi Arabia. Advances in Environmental Biology 2013;7:2584–92. [Google Scholar]
- 22. Almalki M, Fitzgerald G, Clark M. Health care system in Saudi Arabia: an overview. East Mediterr Health J 2011;17:784–93. 10.26719/2011.17.10.784 [DOI] [PubMed] [Google Scholar]
- 23. MOH portal.com Annual statistical book, 2015. https://www.moh.gov.sa/en/Ministry/Statistics/book/Documents/StatisticalBook-1436.pdf [Google Scholar]
- 24. Atılgan E. The technical efficiency of hospital inpatient care services: an application for Turkish public hospitals. Business and Economics Research Journal 2016;7:203–14. 10.20409/berj.2016217537 [DOI] [Google Scholar]
- 25. Pelone F, Kringos DS, Romaniello A, et al. Primary care efficiency measurement using data envelopment analysis: a systematic review. J Med Syst 2015;39:156 10.1007/s10916-014-0156-4 [DOI] [PubMed] [Google Scholar]
- 26. Cooper W, Seiford L, Tone K. Data envelopment analysis: a comprehensive text with models, applications, references and DEA-solver software. New York: Springer, 2007: 1–85. [Google Scholar]
- 27. Gok MS, Sezen B. Analyzing the ambiguous relationship between efficiency, quality and patient satisfaction in healthcare services: the case of public hospitals in turkey. Health Policy 2013;111:290–300. 10.1016/j.healthpol.2013.05.010 [DOI] [PubMed] [Google Scholar]
- 28. Afzali HHA, Moss JR, Mahmood MA. A conceptual framework for selecting the most appropriate variables for measuring Hospital efficiency with a focus on Iranian public hospitals. Health Services Management Research 2009;22:81–91. 10.1258/hsmr.2008.008020 [DOI] [PubMed] [Google Scholar]
- 29. Sahin I, Ozcan YA. Public sector Hospital efficiency for provincial markets in turkey. J Med Syst 2000;24:307–20. 10.1023/A:1005576009257 [DOI] [PubMed] [Google Scholar]
- 30. Ahmed S, Hasan MZ, MacLennan M, et al. Measuring the efficiency of health systems in Asia: a data envelopment analysis. BMJ Open 2019;9:e022155 10.1136/bmjopen-2018-022155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Dyson RG, Allen R, Camanho AS, et al. Pitfalls and protocols in DEA. Eur J Oper Res 2001;132:245–59. 10.1016/S0377-2217(00)00149-1 [DOI] [Google Scholar]
- 32. Hollingsworth B. Evaluating efficiency of a health care system in the developed world. Encyclopedia of Health Economics 2014;1:292–9. [Google Scholar]
- 33. Charnes A, Cooper WW, Rhodes E. Measuring the efficiency of decision making units. Eur J Oper Res 1978;2:429–44. 10.1016/0377-2217(78)90138-8 [DOI] [Google Scholar]
- 34. Banker RD, Charnes A, Cooper WW. Some models for estimating technical and scale inefficiencies in data envelopment analysis. Manage Sci 1984;30:1078–92. 10.1287/mnsc.30.9.1078 [DOI] [Google Scholar]
- 35. Chuang C-L, Chang P-C, Lin R-H. An efficiency data envelopment analysis model reinforced by classification and regression tree for hospital performance evaluation. J Med Syst 2011;35:1075–83. 10.1007/s10916-010-9598-5 [DOI] [PubMed] [Google Scholar]
- 36.pp Gok MS, Altındağ E. Analysis of the cost and efficiency relationship: experience in the Turkish pay for performance system. Eur J Health Econ 2015;16:459–69. 10.1007/s10198-014-0584-6 [DOI] [PubMed] [Google Scholar]
- 37. O’Neill L, Rauner M, Heidenberger K, et al. A cross-national comparison and taxonomy of DEA-based Hospital efficiency studies. Socioecon Plann Sci 2008;42:158–89. 10.1016/j.seps.2007.03.001 [DOI] [Google Scholar]
- 38. Mahate A, Hamidi S. Frontier efficiency of hospitals in United Arab Emirates: an application of data envelopment analysis. J Hosp Admin 2016;5:pp7–16. [Google Scholar]
- 39. Ramanathan R. Operations assessment of hospitals in the Sultanate of Oman. Int Jrnl of Op & Prod Mnagemnt 2005;25:39–54. 10.1108/01443570510572231 [DOI] [Google Scholar]
- 40. Charnes A, Cooper WW. Programming with linear fractional functionals. Naval Research Logistics 1962;9:181–6. 10.1002/nav.3800090303 [DOI] [Google Scholar]
- 41. Emrouznejad A, Thanassoulis E. Performance improvement management software: PIM-DEAsoft-V3.0 user guide, 2011. Performance improvement management limited, UKISBN: 1-85449-412-2. www.DEAsoftware.co.uk Available: https://deazone.com/en/software
- 42. Shahhoseini R, Tofighi S, Jaafaripooyan E, et al. Efficiency measurement in developing countries: application of data envelopment analysis for Iranian hospitals. Health Serv Manage Res 2011;24:75–80. 10.1258/hsmr.2010.010017 [DOI] [PubMed] [Google Scholar]
- 43. Kiadaliri A, Haghparast-Bidgoli H, Zarei A. Measuring efficiency of general hospitals in the South of Iran. World Appl Sci J 2011;13:1310–6. [Google Scholar]
- 44. Afzali HHA, Moss JR, Mahmood MA. Exploring health professionals' perspectives on factors affecting Iranian Hospital efficiency and suggestions for improvement. Int J Health Plann Manage 2011;26:e17–29. 10.1002/hpm.1035 [DOI] [PubMed] [Google Scholar]
- 45. Al-Salem AA. Renovation of financing healthcare services in Kingdom of Saudi Arabia, by implementing National health insurance (NHI). Eur J Pharm Med Res 2018;5:439–48. [Google Scholar]
- 46. World Health Organization Health systems financing: the path to universal coverage, world health report 2010. Geneva 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.