Abstract
Background
Specialist parenting intervention could improve coexistent parenting and child mental health difficulties of parents affected by severe personality difficulties.
Objective
Conduct a feasibility trial of Helping Families Programme-Modified (HFP-M), a specialist parenting intervention.
Design
Pragmatic, mixed-methods trial, 1:1 random allocation, assessing feasibility, intervention acceptability and outcome estimates.
Settings
Two National Health Service health trusts and local authority children’s social care.
Participants
Parents: (i) primary caregiver, (ii) 18 to 65 years, (iii) severe personality difficulties, (iv) proficient English and (v) capacity for consent. Child: (i) 3 to 11 years, (ii) living with index parent and (iii) significant emotional/behavioural difficulties.
Intervention
HFP-M: 16-session home-based intervention using parenting and therapeutic engagement strategies. Usual care: standard care augmented by single psychoeducational parenting session.
Outcomes
Primary feasibility outcome: participant retention rate. Secondary outcomes: (i) rates of recruitment, eligibility and data completion, and (ii) rates of intervention acceptance, completion and alliance (Working Alliance Inventory-Short Revised). Primary clinical outcome: child behaviour (Eyberg Child Behaviour Inventory). Secondary outcomes: child mental health (Concerns About My Child, Child Behaviour Checklist-Internalising Scale), parenting (Arnold-O’Leary Parenting Scale, Kansas Parental Satisfaction Scale) and parent mental health (Symptom-Checklist-27). Quantitative data were collected blind to allocation.
Results
Findings broadly supported non-diagnostic selection criterion. Of 48 participants recruited, 32 completed post-intervention measures at mean 42 weeks later. Participant retention exceeded a priori rate (HFP-M=18; Usual care=14; 66.7%, 95% CI 51.6% to 79.6%). HFP-M was acceptable, with delivery longer than planned. Usual care had lower alliance rating. Child and parenting outcome effects detected across trial arms with potential HFP-M advantage (effect size range: 0.0 to 1.3).
Conclusion
HFP-M is an acceptable and potentially effective specialist parenting intervention. A definitive trial is feasible, subject to consideration of recruitment and retention methods, intervention efficiency and comparator condition. Caution is required in interpretation of results due to reduced sample size. No serious adverse events reported.
Trial registration number
Keywords: personality disorders, parenting, child behaviour, child & adolescent psychiatry
Strengths and limitations of this study.
This randomised trial assessed the feasibility of a specialist parenting intervention for coexistent mental health problems of parents affected by severe personality difficulties and their children.
Findings provide useful evidence to support further evaluation of this specialist parenting intervention within a definitive trial, with modifications required to improve intervention efficiency, augmented usual care condition acceptability and participant enrolment and retention.
Caution is required in interpretation of results due to reduced sample size.
The trial population’s complex personality difficulties underline the importance of effective and sensitive management of trial consent procedures, random allocation and ongoing engagement of participants, particularly for those allocated to the usual care condition.
Introduction
Mental ill health is the largest cause of disability, with three-quarters of lifetime disorders starting during childhood.1 Children of parents affected by severe personality difficulties are at particular risk due to the impact of parents’ symptoms and associated impairment on parenting capacity.2–4 Lack of evidence-based treatments, underdeveloped care pathways and stigma result in poorer immediate and longer-term child outcomes, increase intergenerational transmission of mental health difficulties and perpetuate social disadvantage.5 6
Severe personality difficulties, including personality disorders, affect over 4% of UK adults and 40% of mental health service users, at least one-quarter of whom are parents.7 8 Per annum UK treatment costs exceed £70 million, with wider societal costs estimated at £8 billion per year.9 Characterised by problematic interpersonal relationships, emotional dysregulation and poor impulse control, severe personality difficulties are associated with insensitive and intrusive interactions with offspring, family hostility, inconsistent and unpredictable family routines that undermine affectionate, stable and responsive parenting required for healthy child development.2–4 Affected parents are likely to suffer higher parenting stress and lower satisfaction, exacerbating underlying mental health difficulties.10 11
One in 10 UK children suffer mental health disorders, with children of parents with severe personality difficulties at substantially higher risk of intergenerational transmission, most commonly behavioural disorders.12 13 These childhood disorders are associated with academic failure, school exclusion, maltreatment, self-harm and gang affiliation, with increased life-time risk of comorbid mental and physical health conditions, drug misuse, offending and worklessness.1 12 13 Annual UK public service costs for severe behavioural problems are estimated at £5000 per child including £1400 health costs. Lifetime estimated costs range from £85 000 (moderate case) to £260 000 (severe case).14 15
Concerted preventative and early intervention during pregnancy, infancy and childhood is warranted.16 Effective care models for co-occurring child and parental mental health problems are significant health policy and research priorities.17–19 Nevertheless, routine care is highly variable, generally focussed on the needs of either the adult or the child,17 resulting in under-identification, poor understanding of the interrelationship between child and parent difficulties and misattribution of parenting difficulties to adult mental health symptoms per se.20 Affected parents can be reluctant to engage due to stigma, treatment scepticism and the interpersonal difficulties and adverse life circumstances associated with personality difficulties.21
Parenting and parent factors are central to much effective child mental health treatment and problem remediation. Parenting programmes are the recommended cost-effective treatment for child behaviour problems.22 23 However, non-specialised parenting programmes, not specifically designed for parents affected by mental health difficulties, often result in poorer engagement, acceptability and outcomes.24 25 Specialist interventions for some parental mental health conditions, such as depression, substance misuse and eating disorders, have demonstrated improved outcomes and reduced intergenerational transmission, by up to 40%.26 27 Specialist programmes for parents affected by personality difficulties are at an earlier stage of evidence production.
Helping Families Programme-Modified (HFP-M) was developed as a specialist, intensive parenting intervention to address this need and service gap. It aims to improve immediate child and parenting outcomes with longer-term potential to reduce intergenerational transmission and psychosocial adversity within affected families.4 Guided by recommended frameworks, HFP-M development synthesised two existing evidence-based interventions, incorporating relevant clinical practice recommendations and service user consultation.22 28–33 Consistent with other promising programmes aiming to improve parenting and child outcomes in high risk groups, HFP-M is based on a transtheoretical model of parenting drawing on attachment, social learning and cognitive-affective theories and methods.34 35 HFP-M does not target personality difficulties per se but aims to improve the ways that these characteristics affect parenting behaviour, emotional regulation, parent-child relationships and lead to adverse child outcomes.
HFP-M has three structured components:36 (i) Core Therapeutic Process: including partnership and goal-based methods to promote collaborative relational engagement, shared formulation, empathic parent validation and crisis management;36 (ii) Parent Groundwork: including emotion-focussed, cognitive, behavioural and interpersonal strategies to manage parental emotional dysregulation and hostility while relating to their children and undertaking parenting tasks and (iii) Parenting Strategies: including consistent use of positive parenting skills, such as, praise, consequences and limit setting, and relational and affective parenting methods such as emotionally responsive, warm care-giving and reflective function.
Definitive trials require successful recruitment, retention and intervention acceptability.30 37–41 Participant retention underpins trial validity. Lower rates reduce power, undermine interpretation of findings and increase costs. HFP-M retention, and initial recruitment was expected to be affected by: (i) participants’ core clinical features, (ii) greater exposure to family stress, negative life events, lower levels of social support and comorbid mental health conditions and (iii) under-identification of need within routine care, negative referrer expectancies, lower service engagement and attendance. These factors are reflected in evidence derived from 45 personality disorder treatments trials reported in two systematic reviews indicating a median participant non-completion rate of 35%.37 42 Pre-feasibility trial case series findings, consultation with service user, clinicians and research ethics indicated that initial plans for trial recruitment based on personality disorder research diagnosis was unlikely to be viable for practical, participant acceptability and ethical reasons.21
To be useful and effective in practice, interventions need to demonstrate both clinical efficacy and user acceptability. Acceptability refers to service user judgements across four inter-related domains of intervention satisfaction: (i) relevance, (ii) content and procedures, (iii) clinician/provider characteristics and (iv) outcome suitability.39 40
This study reports quantitative findings from a randomised feasibility trial of HFP-M, based on a published protocol.4 The trial aimed to assess research and clinical feasibility of HFP-M for a target population with coexisting parent personality difficulties and child mental health difficulties with findings being used to inform the design of a full-scale trial.
The primary feasibility outcome was a participant retention rate of at least 65% post-intervention. Secondary feasibility outcomes were rates of: (i) participant identification and recruitment, (ii) data collection and (iii) intervention use, uptake and acceptability. Primary clinical outcome was child behaviour. Secondary clinical outcomes included parental child concerns, child internalising difficulties, parenting behaviour, satisfaction and psychological well-being. The trial sought to produce effect sizes and variance estimates for child and parent outcomes necessary to power a full-scale trial.
The findings of a parallel qualitative process evaluation investigating the influence of contextual factors on trial and intervention implementation and outcome generation are published elsewhere, as are the full findings of preliminary intervention costs and estimates of cost-effectiveness.43
Method
Design
Mixed-method, two-arm, parallel feasibility trial with random allocation in a 1:1 ratio to either: (i) HFP-M, or (ii) Usual care.
Quantitative data were collected at pre-randomisation baseline (Time 1); post-intervention (Time 2), 6 months from baseline and follow-up (Time 3), 4 months and 10 months from baseline.
Eligibility criteria
Parent: (i) primary parental caregiver for index child, (ii) aged 18 to 65, (iii) experiencing severe personality difficulties, assessed by self-administered Standardised Assessment of Personality-Abbreviated Scale (SAPAS) score of ≥3, the optimal cut-point for the intended sample population,44 (iv) proficient written and spoken English and (v) capacity to provide informed consent.
Child: (i) aged 3 to 11, (ii) living with index parent and (iii) experiencing significant emotional/behavioural difficulties, assessed by Strengths and Difficulties Questionnaire Total Score of ≥17.45
Exclusion criteria
Parent: (i) coexisting psychosis, (ii) engagement in another structured parenting intervention, (iii) inpatient status or (iv) insufficient language/cognitive abilities.
Child: (i) pervasive developmental disorder, (ii) not residing with index parent or (iii) considered for/subject to child protection supervision.
Interventions
HFP-M intervention
Sixteen-session home-based 1:1 parenting intervention for parents with severe personality difficulties, including personality disorder. Session modules proceeded iteratively to (i) establish effective, validating collaborative partnership, (ii) develop shared understanding of severe parental personality difficulties’ impact on parenting, child functioning and family ecology, (iv) implement parent quick wins, parenting and child intervention goals, (v) use evidence-based parenting and parent self-care strategies to achieve agreed goals and (vi) recurrent review of goals and therapeutic partnership. Six trial therapists received eight, 3-hour, training sessions provided by HFP-M programme developers and clinical experts. Trial therapists completed structured checklists and received fortnightly supervision from experienced HFP-M clinicians to support clinical implementation and fidelity.
Usual care
No systematised parenting pathway was typically provided for the participant population. To provide consistent, low intensity support, participants could receive an additional home-based one-to-one parent information and support session. Derived from the evidence-based Empowering Parents Empowering Communities parenting programme,46 session content included: (i) brief exploration of parenting and child needs, family support, parent priorities and goals, and (ii) focus on one parent priority topic, selected from Being Good Enough, Listening to My Child, Praising My Child, Taking Care of Myself, Understanding My Child’s Behaviour, My Child’s Emotion or Playing Together. The additional session was delivered by three trained parent practitioners, who received ongoing supervision to support implementation and fidelity.
Concomitant interventions
Both HFP-M and the single Usual care parent support session were provided in addition to existing medical, psychosocial and educational support and treatment services used by participating parents and their families. A joint-working protocol specified procedures for care coordination and information sharing between trial therapists and routine services.
Measures
Participant characteristics
Descriptive data were collected on parent and child age, gender and ethnicity, family household composition, participant diagnostic status and family socioeconomic status. Data from EuroQol five dimension scale (EQ-5D),47 48 provided information about parent and child health and disability.
Feasibility evaluation
Structured record sheets, completed prospectively by research staff and trial therapists, documented: (i) participant identification and verbal consent, (ii) screening, eligibility, informed written consent, randomisation and reasons for non-participation, and (iii) data collection and missing data.
Clinical outcomes
Eyberg Child Behaviour Inventory (ECBI),49 a 36-item questionnaire assessing intensity and number of disruptive behaviour problems in 2 to 16 year-olds, providing a comprehensive measure of child behaviour difficulties. Intensity Scale score of ≥131 indicates significant severity. Problem Scale score of ≥15 indicates significant number of problems.
Concerns About My Child (CAMC),46 a Visual Analogue Scale (0 to 100) rating three parental concerns about their child. Concerns nominated at baseline were re-rated at each time point, providing a sensitive, individualised index of change.
Child Behaviour Checklist-Internalising Scale (CBCL-Int),50 a 32-item questionnaire assessing internalising problems in 6 to 18 year-olds, with an alternate 36-item version for children aged 1½ to 5 years. Standardised T-scores combine results from both versions. A score of ≥60 indicates clinical caseness.
Arnold-O’Leary Parenting Scale (PS),51 a 30-item questionnaire assessing dysfunctional parental discipline behaviour for children aged 2 to 16 years, which correlates with more time-consuming observational ratings. A score of ≥3.2 differentiates clinic and non-referred children.
Kansas Parental Satisfaction Scale (KPSS),52 a 3-item scale providing a brief measure of parenting stress and satisfaction.
Symptom-Checklist-27,53 a 27-item questionnaire assessing psychological symptoms in adults that provides a Global Severity Index of psychopathology.
Intervention acceptability
Working Alliance Inventory-Short Revised (WAI-SR),54 a parent completed 12-item questionnaire assessing therapeutic relationship quality consisting of three subscales: (i) Goals, measuring agreement on intervention goals and outcomes, (ii) Tasks, measuring agreement on behaviours and thoughts underpinning intervention process and (iii) Bond, measuring mutual trust, acceptance and confidence.
Structured worksheets recorded intervention uptake, attendance, retention, reasons for missed sessions and dropout.
Health economic
Sample size
The primary feasibility criterion was post-intervention retention rate of at least 65%.37 42 A CI approach was used to calculate a planned sample size of n=70.56 Using a 95% CI for the proportion of parents who completed treatment and an expected completion rate of 80% based on previous evaluations of HFP, it was determined that an HFP-M intervention sample size of n=35 would provide a sufficiently precise estimate (95% CI 0.67 to 0.93). A sample size of n=70 was also sufficient to obtain stable estimates of population variances for future power calculations.57
Recruitment and consent procedures
Settings
Recruitment took place in two large UK National Health Service (NHS) health services and concomitant local authority children’s social care service in London (Site 1 and 2), located in areas of high mental health morbidity.
Identification and consent
Clinical keyworkers undertook exploratory discussion and provided written information to potential participants. With consent, contact details were provided to researchers, who provided information about study aims, eligibility criteria, procedures and a Participant Information Sheet. One week later, parents were contacted to determine participation and obtain written informed consent.
Allocation and randomisation
Participants were allocated a unique, anonymised ID number and randomised to trial conditions between 11 May 2016 and 29 March 2017 by Clinical Trials Unit, King’s College, London. Allocation was communicated confidentially to the trial coordinator, other researchers remained blind to allocation.
Data collection
Screening and assessments
Following consent, parents completed screening measures, and, when eligible, baseline measures in a standard sequence. Any parent discomfort was addressed sensitively and supportively. Persistent, non-intrusive efforts were used to complete post-intervention and follow-up data collection. Participants were reimbursed £10 per hour for data completion at each point.
Analysis
Statistical analysis was mainly descriptive using means and SD for continuous data, or medians and range where data were skewed. Frequencies and proportions were used to describe categorical variables. Feasibility of trial retention was assessed using the proportion of a predetermined parameter and estimated 95% CIs. Clinical outcomes were analysed using analysis of covariance models to estimate likely range of intervention effect, by assessing 95% CI, at post-treatment, with pre-randomisation values as a covariate.58 Follow-up data were not included in these analyses due to a smaller sample than planned. Standardised effect sizes were calculated using Cohen’s d. Given the complexity of coexistent parent and child mental health difficulties, the smallest change in outcome identified as clinically important is equivalent to a small effect size. Population variances for future power calculations were determined using the upper 80th percentile of CIs around the estimated population variance.58
Patient and public involvement
A senior staff member of a national service user organisation was a co-applicant and contributed to research conception, planning and governance. A service user researcher was involved in the analysis, interpretation and dissemination of findings. A service user panel advised on trial planning, intervention methods, outcome selection and interpretation of findings.59
Independent NHS research and development approval
Research and development approvals were obtained from South London and Maudsley NHS Foundation Trust and Central and North-West London NHS Foundation Trust.
Serious adverse events
The chief investigator was responsible for reporting serious adverse events to the trial’s independent Data Monitoring and Ethics Committee and responsible research ethics committee. No serious adverse events were reported.
Results
Feasibility evaluation
Recruitment took 4 months longer than planned due to delays in Site 2, resulting in a revised sample size of 48. Obtaining keyworker information on service users approached about trial participation proved impractical.
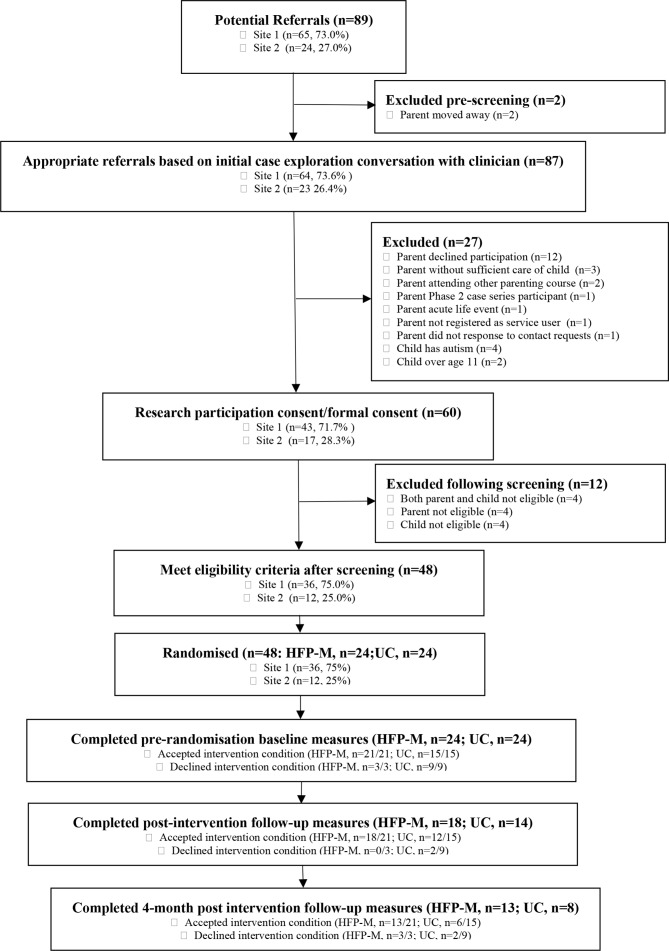
All referred service users (n=89, 100.0%) consented to research contact (see figure 1). Adult mental health services (AMHS) referred 30 (33.7%) parents, child and adolescent mental health services (CAMHS) 29 (32.6%) and children’s social care (CSS) 30 (33.7%). Site 1 referred 65 (73.0%) parents. Researchers made contact with 87 (97.7%) parents, requiring 1 to 13 communications per participant.
Figure 1.
Consolidated Standards of Reporting Trials diagram randomised feasibility trial recruitment and retention. HFP-M, Helping FamiliesProgramme-Modified; UC, usual care.
Sixty (69.7%) parents met initial criteria and completed screening. The most common reason for ineligibility was parents declining trial participation (n=12, 13.5%). Six parents were excluded due to child-related reasons, most commonly presence of child developmental disorder.
Forty-eight consenting participants met parent and child screening criteria, all of whom completed baseline measures, representing 80.0% of screened parents, 53.9% of referred parents and 68.8% of the planned sample. Five (8.3%) met neither parent nor child screening criteria, four (6.7%) did not meet SAPAS criterion and three (5.0%) did not meet Strengths and Difficulties Questionnaire (SDQ) criterion.
Thirty-six (75.0%) participants were from Site 1, exceeding the site recruitment target. Site 2 recruitment (n=12) was 34.3% of that planned, due to delayed recruitment and lower service engagement. Eighteen (37.5%) participants were referred by AMHS, 16 (33.3%) CAMHS and 14 (29.2%) CSS.
There was a significant difference in trial condition uptake (HFP-M: n=21, 87.5%; Usual care n=15, 62.5%; χ2=4.0, df=1 (48), p<0.05). Modal duration between randomisation and starting HFP-M was 2 weeks (range 1 to 23 weeks). Parents declined HFP-M because one gave birth, another was in couple conflict about participation and a third did not respond to persistent contact (see figure 1). The modal duration before Usual care parenting session receipt was 5.5 weeks (range 1 to 17 weeks). The most common reason for declining the additional Usual care parenting session was that participants hoped to be allocated to HFP-M.
Thirty-two (66.7%, 95% CI 51.6% to 79.6%) participants completed post-intervention measures. The majority of participants who did not take up the intervention offered, mainly in the Usual care condition, did not complete post-intervention measures.
Twenty-one (65.6%) parents completing post-intervention measures were also assessed at follow-up, representing 43.8% of all participants. Post-intervention measures were completed a mean of 42.0 weeks (SD 14.6) after baseline, due to HFP-M delivery being lengthier in duration than planned. Follow-up measures were completed a mean of 20 weeks (SD 8.9) later. Researchers required one to eight participant contacts to arrange post-intervention and follow-up data collection. Main reasons for non-completion included unable to contact participant, participant declining completion and participant health and life circumstances.
There were less than 0.1% missing data items across clinical measures at each time point.
Sample characteristics
Demographic characteristics
All 48 participants were the biological parent of the index child, one was a father (2.1%) (see table 1). The majority were lone parents (n=31, 67.4%), mean age 34.9 (SD 7.1) years. The majority (n=28, 61.0%) were White British/White, with fewer Black/Black British (n=9, 19.6%) and Dual Heritage (n=6, 13.5%) parents. English was the most common first language (n=44, 91.7%). Twenty-five (55.6%) participants completed education at 18 years or younger. Four participants (8.9%) were higher education graduates.
Table 1.
Participant demographic characteristics
| Demographic characteristics | Baseline (Time 1) | ||
| Total | Intervention | Usual care | |
| Parent gender (female) (n, %) | 47 (97.9) | 24 (100.0) | 23 (95.8) |
| Parent age (yrs.) (mean, SD) | 34.9 (7.1) | 34.7 (7.5) | 35.0 (6.9) |
| Received psychiatric diagnosis (n, %) | 25 (86.2) | 16 (88.9) | 9 (81.8) |
| Psychiatric diagnosis duration (yrs.) (mean, SD) | 9.7 (7.4) | 8.6 (7.0) | 10.9 (8.1) |
| Parent relationship to index child (biological parent) (n, %) | 46 (100.0) | 24 (100.0) | 22 (100.0) |
| Index child gender (male) (n, %) | 26 (55.3) | 12 (50.0) | 14 (60.9) |
| Index child age (mean, SD) | 7.8 (2.2) | 7.7 (2.0) | 7.9 (2.2) |
| Number of children at home (median, range) | 2 (1–5) | 2 (1–5) | 2 (1–5) |
| Not in paid employment (n, %) | 37 (80.4) | 19 (79.2) | 18 (81.8) |
| Lone parent (n, %) | 31 (67.4) | 14 (58.3) | 17 (77.3) |
| Partner in employment (n, %) | 9 (19.5) | 6 (25.0) | 3 (12.5) |
| Parent education (n, %) | |||
| Graduate | 4 (8.9) | 2 (8.3) | 2 (9.5) |
| University not completed | 3 (6.7) | 3 (12.5) | 0 (0.0) |
| Other for example, NVQ | 13 (28.9) | 6 (25.0) | 7 (33.3) |
| Left school 18 years | 9 (20.0) | 4 (16.7) | 5 (23.8) |
| Left school 16 years | 7 (15.6) | 4 (16.7) | 3 (14.3) |
| Left school under 16 | 9 (20.0) | 5 (20.9) | 4 (19.0) |
| Ethnicity (n, %) | |||
| White UK/White other | 28 (61.0) | 13 (54.2) | 15 (68.2) |
| Black UK/African Caribbean | 9 (19.6) | 7 (29.2) | 2 (9.1) |
| Dual heritage | 6 (13.0) | 3 (12.5) | 3 (13.6) |
| Black UK/African | 2 (4.3) | 0 (0.0) | 2 (9.1) |
| Other | 1 (2.2) | 1 (4.2) | 0 (0.0) |
| Parent health status* (n, %) | |||
| Mobility problems | 9 (25.0) | 4 (23.5) | 5 (26.4) |
| Problems in self-care washing and dressing | 3 (8.3) | 1 (5.9) | 2 (10.5) |
| Difficulties in undertaking usual activities | 13 (36.1) | 7 (41.1) | 6 (31.6) |
| Suffered pain/discomfort | 17 (47.2) | 6 (35.3) | 11 (57.9) |
*EQ-5D-5L health moderate/severe status.
NVQ, National Vocational Qualification; yrs., years.
Most participants (n=37, 80.4%) were not in paid employment. Nine (19.5%) had partners in paid employment, predominantly part-time (n=7, 15.2%). No parent was in paid employment in 30 (65.2%) households. Twenty-five (86.2%) parents had received a formal psychiatric diagnosis, mean time since initial diagnosis was 9.7 (7.4) years.
Twenty-six (54.2%) children were male, mean age of 7.8 (SD 2.2) years. Median number of children in the home was 2, range 1 to 5 (see table 1). Participants reported significant difficulties with anxiety/depression, pain/discomfort, with a smaller proportion experiencing difficulties in undertaking everyday activities (see table 1).
Clinical characteristics
Over 80 per cent of ECBI Problem and Intensity scores at baseline exceeded the clinical caseness cut-off, with similar caseness rates for CBCL-Int and PS (see table 2). The most common baseline CAMC child-related parent concerns were conduct, self-regulation, parent-child relationships and emotional distress (see table 3).
Table 2.
Participant baseline clinical caseness
| Measure | Baseline | ||
| Total | Intervention | Usual care | |
| ECBI problem caseness (≥15) (n, %) | 41 (89.1) | 21 (87.5) | 20 (90.9) |
| ECBI intensity caseness (≥131) (n, %) | 39 (83.0) | 19 (79.2) | 20 (83.3) |
| CBCL-Int (t-score) caseness (≥60) (n, %) | 45 (95.8) | 23 (95.8) | 22 (95.7) |
| PS caseness (≥3.2) (n, %) | 35 (74.5) | 18 (75.0) | 17 (73.9) |
CBCL-Int, Child Behaviour Checklist-Internalising Scale; ECBI, Eyberg Child Behaviour Inventory; PS, Arnold-O’Leary Parenting Scale.
Table 3.
Parent-reported concerns about index child
| Concern category | Primary | Secondary | Tertiary | Total |
| Conduct problems* (n, %) | 18 (38.3) | 27 (58.7) | 24 (53.3) | 69 (50.0) |
| Parent-child relationship and communication (n, %) | 16 (34.0) | 2 (4.4) | 4 (8.9) | 22 (15.9) |
| Child self-regulation† (n, %) | 4 (8.5) | 11 (23.9) | 7 (15.6) | 22 (15.9) |
| Emotional distress‡ (n, %) | 8 (17.0) | 4 (8.8) | 7 (15.6) | 19 (13.8) |
| Other§ (n, %) | 1 (2.1) | 2 (4.4) | 1 (2.2) | 4 (2.9) |
| School (n, %) | 0 (0.0) | 0 (0.0) | 2 (4.4) | 2 (1.5) |
| Total (n, %) | 47 | 46 | 45 | 138 |
*including anger, tantrums, defiance, non-compliance, aggression, running away and lying.
†including overactivity, poor concentration, overeating and wetting.
‡including low mood, anxiety, low self-esteem.
§including risk behaviours.
Trial interventions acceptability
HFP-M attendance
Of 21 participants who accepted HFP-M, 13 (61.9%, 95% CI 38.4% to 81.9%) completed HFP-M within the trial period. Six (28.6%, 95% CI 11.3% to 52.2%) withdrew before completion due to acute adult mental health crisis and complex family circumstances unrelated to HFP-M receipt. Recruitment delay and longer than anticipated intervention duration resulted in two (9.5%, 95% CI. 1.2% to 30.4%) participants not fully completing HFP-M before trial conclusion. The mean number of HFP-M appointments offered was 15.8 (SD 7.7) and mean number attended was 11.2 (SD 6.3). HFP-M appointment attendance was 70.2%. Mean duration of HFP-M delivery was 28.4 (SD 21.7) weeks.
HFP-M therapeutic alliance acceptability
Eighteen (85.3%) HFP-M participants completed post-intervention WAI-SR (mean total score=73.8, SD 10.4). Mean subscale scores were consistently in the upper end of the scale (Mean Tasks Subscale score=24.9, SD 3.5; Bond Subscale score=24.9, SD 3.9; Goals Subscale score=23.9, SD 4.1).
Usual care
All 15 participants accepting the additional parenting session completed. Due to lower retention, only six participants provided post-intervention WAI-SR data (mean total score=56.2, SD 18.8). Mean subscales scores were consistently lower than the HFP-M condition (Mean Tasks Subscale score=17.4, SD 7.2; Bond Subscale score=19.8, SD 7.1; Goals Subscale score=19.0, SD 7.6).
There appeared to be a substantial difference in WAI-SR scores between the two conditions but there was insufficient Usual care data to test for a statistical difference.
No adverse events were reported during the trial. Participant intervention withdrawal most frequently occurred due to deterioration in participant mental health and life circumstances, unrelated to trial participation.
Clinical outcomes
There were estimated mean improvements from baseline scores across a number of outcomes within both trial conditions (see table 4). HFP-M mean differences exceeded those in Usual care on several outcomes. These findings should be treated with caution given the wide CIs.
Table 4.
Parent reported child, parenting and parent clinical outcomes (intention to treat analysis)
| Measure | Group | Baseline mean (SD) (n) |
Post-intervention mean (SD) (n) |
Follow-up mean (SD) (n) |
Baseline/post-intervention estimated mean difference (CI) | P value | Effect size |
| CAMC | |||||||
| Problem 1 | Intervention | 84.6 (16.0) (n=24) |
45.2 (27.2) (n=18) |
58.2 (29.5) (n=13) |
18.633 (-40.177 to 2.910) |
0.087 | 1.2 (0.4–2.0) |
| Usual care | 85.9 (14.7) (n=22) |
63.1 (31.1) (n=14) |
53.3 (34.4) (n=8) |
||||
| Problem 2 | Intervention | 85.0 (19.1) (n=24) |
51.1 (31.9) (n=18) |
56.4 (35.5) (n=13) |
22.486 (−44.318 to −0.654) |
0.044 | 1.3 (0.5–2.1) |
| Usual care | 82.9 (15.7) (n=22) |
72.5 (26.0) (n=14) |
66.5 (35.5) (n=8) |
||||
| Problem 3 | Intervention | 81.0 (17.0) (n=24) |
54.4 (33.8) (n=17) |
42.8 (35.4) (n=13) |
2.909 (-28.349 to 22.530) |
0.816 | 0.0 (-0.7–0.7) |
| Usual care | 78.9 (18.5) (n=22) |
57.3 (34.1) (n=14) |
39.6 (24.3) (n=8) |
||||
| ECBI | |||||||
| Problem score | Intervention | 22.1 (7.4) (n=24) |
17.9 (8.5) (n=15) |
15.3 (9.4) (n=13) |
1.559 (−4.24=55 to 7.374) |
0.585 | 0.1 (-0.7–0.88) |
| Usual care | 22.43 (6.2) (n=21) |
18.0 (11.5) (n=14) |
18.8 (12.3) (n=8) |
||||
| Intensity score | Intervention | 168.2 (35.9) (n=24) |
142.4 (39.3) (n=24) |
131.7 (43.0) (n=18) |
12.866 (−4.24=55 to 7.374) |
0.233 | 0.4 (-0.3–1.1) |
| Usual care | 169.5 (31.8) (n=23) |
155.7 (49.6) (n=14) |
148.9 (58.4) (n=8) |
||||
| CBCL-Int (t-score) |
Intervention | 72.9 (9.7) (n=24) |
69.6 (10.4) (n=18) |
68.2 (8.3) (n=13) |
1.853 (-9.023 to 5.317) |
0.601 | 0.2 (-0.5–0.9) |
| Usual care | 70.9 (11.9) (n=23) |
70.9 (9.3) (n=14) |
69.6 (8.6) (n=8) |
||||
| KPSS | Intervention | 10.1 (3.1) (n=24) |
12.9 (3.5) (n=18) |
14.9 (3.8) (n=13) |
1.177 (-1.260 to 3.615) |
0.331 | 0.4 (-0.3–1.1) |
| Usual care | 10.9 (2.8) (n=23) |
12.4 (3.9) (n=14) |
13.6 (3.9) (n=7) |
||||
| PS | Intervention | 111.0 (19.6) (n=24) |
108.7 (16.5) (n=18) |
98.3 (27.2) (n=13) |
0.210 (-14.776 to −15.196) |
0.977 | 0.0 (-0.7–0.7) |
| Usual care | 113.5 (24.8) (n=23) |
108.7 (28.9) (n=14) |
98.1 (26.9) (n=7) |
||||
| SCL-27 Global Severity Index | Intervention | 1.8 (1.1) (n=24 |
1.6 (0.8) (n=18) |
1.9 (0.8) (n=13) |
−0.105 (−0.599 to 0.389) |
0.666 | −0.1 (-0.8–0.6) |
| Usual care | 1.7 (0.8) (n=22) |
1.7 (0.9) (n=14) |
1.3 (1.0) (n=8) |
CAMC, Concerns About My Child; CBCL-Int, Child Behaviour Checklist-Internalising Scale; ECBI, Eyberg Child Behaviour Inventory; KPSS, Kansas Parental Satisfaction Scale; PS, Arnold-O’Leary Parenting Scale; SCL-27, Symptom-Checklist-27.
Estimated effect sizes showed a general post-intervention advantage for HFP-M on a range of outcomes. Medium effects for child behavioural problem severity (ECBI Intensity, effect size (ES) 0.4, CI −0.3 to 1.1), and parenting satisfaction (KPSS, ES 0.4, CI −0.3 to 1.1) were detected and a large effect for parent-reported reductions in concerns about their child (CAMC Problem 1, ES 1.2, CI 0.4 to 2.0, CAMC Problem 2, ES 1.3, CI 0.5 to 2.1). No effects were detected for parenting behaviour and adult mental health. Descriptive scrutiny of follow-up findings showed that outcome scores across both groups were generally maintained or continued to improve.
Estimates of SD and upper CIs (u80% CI) for future power calculations of main clinical outcomes are: ECBI Problem: SD 6.7 (u80% CI: 7.6), ECBI Intensity: SD 33.6 (u80% CI: 37.1), CAMC Problem 1: SD 15.3 (u80% CI: 17.4) and KPSS: 3.0 (u80% CI: 3.3).
Health economic findings
Details of the health economic analyses are provided in full in Day et al. At Time 2 CSRI data were available for 26 cases and 19 cases at Time 3. CSRI Time 2 data revealed that the services most used by caregivers included general practitioners (GPs), psychiatrists, other medics and social workers. Caregivers were often in receipt of medication. Children were frequently in contact with school nurses, dentists, opticians and GPs. EQ-5D-5L data were available for 36 caregivers at Time 1, 32 at Time 2 and 21 at Time 3. EQ-5D-Y data were available for 38, 31 and 20 children at each of the respective time points.
Conclusion
This study assessed feasibility, potential challenges and decision-making for a definitive HFP-M trial.28–30 39 Participant identification methods were successful across a wide range of mental health and CSS teams, over 90% of referred parents met dual child and parent screening criteria. Non-diagnostic eligibility criteria were acceptable and effective in recruiting an appropriate, multimorbid sample.60 61 Negative life events and disrupted family functioning, characteristic of the sample population, commonly delayed screening, data collection and intervention delivery.7 Nevertheless, participant retention exceeded the a priori primary feasibility criterion of 65%. Participants declining intervention conditions were less likely to be retained at follow-up. Participant recruitment was slower than planned, mainly due to operational difficulties in one site.
Participants’ multimorbid characteristics are commonly associated with poorer treatment engagement and outcomes.62 63 Intervention uptake differed substantially between trial conditions. HFP-M was largely acceptable to participants but delivery was less efficient than planned, often due to parents’ life circumstances. The augmented Usual care condition appeared to be less acceptable, and potentially affected participant retention. Lower Usual care retention and acceptability rates may reflect common dissatisfaction associated with control condition allocation.64 65
Clinical effects were detected across trial conditions, with potential advantage for child behaviour, parental child concerns and parenting satisfaction for HFP-M. These are welcome given the population’s complex parenting impairments and negative treatment expectancies.2 63 The final sample size limited trial power and consequently affected interpretation of results. A definitive trial could potentially narrow child selection criteria to include only behaviour problems as parenting programmes have a stronger evidence base for this condition. Alternatively, HFP-M content may require strengthening specifically in relation to child internalising difficulties. Economic findings indicated potential cost advantages for HFP-M over usual care.43 However, CSRI completion rates were not high and a simpler version may be required in a larger trial.
Trial conditions may have differed in duration, location and therapeutic intensity, potentially accounting for outcome and acceptability differences. Data collection relied on parent self-report, which is conventional given poor reliability of child-report across the age group and costs associated with independent ratings. Trial therapists provided self-report intervention fidelity data and supervision examined therapist HFP-M skills and implementation. Independent methods could strengthen validity of fidelity monitoring in a definitive trial, including observational and video methods.
A definitive trial is potentially feasible and should be based on the assumption of a medium effect size for the primary outcome of child behaviour. Site engagement, resource allocation and keyworker training in participant identification and recruitment will be crucial to enrolment of the larger sample required in a future trial. Embedded researchers assisting in caseload identification and direct parent recruitment, not possible in this feasibility study, may promote enrolment. Participant retention, particularly parents allocated to a usual care condition, will continue to be challenging for a full trial. The population’s complex personality difficulties and, typically, heightened sensitivity to rejection, underline the importance of managing sensitively and effectively trial consent procedures, the emotional and practical consequences of random allocation and proactively maintaining communication and validating relationships with participants throughout trial duration, particularly for those allocated to usual care. Though not routinely available, the usual care condition could be augmented with an ongoing parent support group to potentially increase equipoise, face validity and uptake, which may also benefit trial retention.
HFP-M clinical and trial efficiency may be improved with more explicit, validating discussion with participants about the potential impact of life and personal circumstances on attendance, use of pre-emptive cancellation plans and inclusion of inter-session contact using digital technology.31 63 66
Supplementary Material
Acknowledgments
We are indebted to the parents, practitioners, clinicians and service managers who worked with us on this trial, particularly Ruth Wilson. We would particularly like to thank Sarah Inkpen, Bethan Stevenson and Chelsea McCorry for their help with trial findings and Peter Fonagy and Philip Graham for overseeing the governance of the trial.
Footnotes
Contributors: CD, Head, Centre for Parent and Child Support, South London, and Maudsley NHS Foundation Trust and Head, CAMHS Research Unit, King’s College, London, was the chief investigator and responsible for the overall conception, design, data acquisition, analysis, interpretation of findings at each phase of this research. He is responsible for the overall content of this report. JB, Department of Psychology, King’s College, London, was the senior research trial coordinator and was responsible for data acquisition, analysis, interpretation, drafting findings and revising this report. MJC, Professor in Mental Health Research, Centre for Psychiatry, Imperial College, London, was a co-applicant and contributed to the overall conception, design and interpretation of findings at each phase of this research. He provided an expert contribution about personality disorder. He contributed to critically revising this report. LF, McPin Foundation, was a service user researcher and representative in this research. She contributed to the design, data acquisition, analysis, interpretation and drafting of findings. She contributed to critically revising this report. LH, Deputy Head, Centre for Parent and Child Support, South London and Maudsley NHS Foundation Trust, was responsible for the development and revision of Helping Families Programme-Modified and supervised trial therapists. She contributed to critically revising this report. JB is a researcher at King’s Health Economics, King’s College, London, co-conducted the health economic analysis and drafted findings for this report. PM, Professor of Health Economics and Director of King’s Health Economics, King’s College, London, was a co-applicant and contributed to the overall conception, design and interpretation of findings at each phase of this research. He led the health economic component of the research and contributed to critically revising this report. MM, Professor at the Institute of Mental Health, University of Nottingham, was a co-applicant and contributed to the overall conception, design and interpretation of findings at each phase of this research. She provided an expert contribution about personality disorder. She was a member of the Manualisation Working Group, contributed to research therapist training and contributed to critically revising this report. DM, Senior Lecturer in Clinical Psychology, School of Psychology, University of Sussex, was a co-applicant and worked closely with the chief investigator on the overall conception and design of this research. He was senior research coordinator during the intervention development phase leading up to this trial and contributed to critically revising this report. PM, Professor of Psychiatry, Population Health Sciences, University of Bristol, was a co-applicant and contributed to the overall conception, design and interpretation of findings at each phase of this research. He provided an expert contribution about personality disorder. He contributed to research therapist raining and critically revised this report. LM, CAMHS Research Unit, King’s College, London, was a researcher worker on this study. She was responsible for Phase 3 data acquisition, analysis and interpretation of findings. She completed the majority of qualitative data acquisition and led its analysis under the direction of the chief investigator. She contributed to critically revising this report. SS, Professor of Child Health and Behaviour, King’s College, London, was a co-applicant and contributed to the overall conception, design and interpretation of findings at each phase of this research. He provided an expert contribution about parenting and parenting programmes. He contributed to critically revising this report. DS, Reader in Biostatistics, Biostatistics and Health Informatics, King’s College, London, was a co-applicant and contributed to the overall conception, design and interpretation of findings at each phase of this research. He provided an expert contribution to the design, analysis and interpretation of quantitative components of the research. He contributed to critically revising this report. PR, LEGO Professor of Play in Education, Development and Learning, Faculty of Education, University of Cambridge, was a co-applicant and contributed to the overall conception, design and interpretation of findings at each phase of this research. He provided an expert contribution about child mental health and co-ordinated the research in CNWL. He contributed to critically revising this report. TW, Associate Professor in Mental Health, Mental Health Social Work and Interprofessional Learning, Middlesex University, London, was a co-applicant and contributed to the overall conception, design and interpretation of findings at each phase of this research. He provided an expert contribution about qualitative design, data acquisition and interpretation. He contributed to critically revising this report.
Funding: This work was supported by National Institute of Health Research, Health Technology Assessment, Project Reference Number: 12/194/01.
Competing interests: CD is the lead developer of two parenting programmes used in this report: Helping Families Programme and Empowering Parents Empowering Communities. MJC has previously received research grant funding on behalf of Imperial College London from the National Institute for Health Research. LH is a co-developer of the Helping Families Programme. MM was an author of the Psychoeducation plus Problems Solving (PEPS) intervention for adults with personality disorder. PEPS helped to inform the modified HFP. PM reports personal fees from a talk given at Fourth Bergen International Conference on Forensic Psychiatry 2016, Outside of the submitted work. PM led the development of the SAPAS, the personality disorder screen used in this study.
Patient consent for publication: Not required.
Ethics approval: Ethics approval was obtained from Health Research Authority South East Coast - Brighton and Sussex Research Ethics Committee (reference: 16/LO/0199).
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data are available upon reasonable request. All manuals can be obtained from the corresponding author. All data requests should be submitted to the corresponding author for consideration. Access to anonymised data may be granted following review.
References
- 1. Fergusson DM, Horwood LJ, Ridder EM. Show me the child at seven: the consequences of conduct problems in childhood for psychosocial functioning in adulthood. J Child Psychol Psychiatry 2005;46:837–49. 10.1111/j.1469-7610.2004.00387.x [DOI] [PubMed] [Google Scholar]
- 2. Petfield L, Startup H, Droscher H, et al. . Parenting in mothers with borderline personality disorder and impact on child outcomes. Evid Based Ment Health 2015;18:67–75. 10.1136/eb-2015-102163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Eyden J, Winsper C, Wolke D, et al. . A systematic review of the parenting and outcomes experienced by offspring of mothers with borderline personality pathology: potential mechanisms and clinical implications. Clin Psychol Rev 2016;47:85–105. 10.1016/j.cpr.2016.04.002 [DOI] [PubMed] [Google Scholar]
- 4. Day C, Briskman J, Crawford MJ, et al. . Feasibility trial of a psychoeducational intervention for parents with personality difficulties: the helping families programme. Contemp Clin Trials Commun 2017;8:67–74. 10.1016/j.conctc.2017.08.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ackerson BJ. Coping with the dual demands of severe mental illness and parenting: the parents' perspective. Families in Society 2003;84:109–18. 10.1606/1044-3894.69 [DOI] [Google Scholar]
- 6. Newton-Howes G, Weaver T, Tyrer P. Attitudes of staff towards patients with personality disorder in community mental health teams. Aust N Z J Psychiatry 2008;42:572–7. 10.1080/00048670802119739 [DOI] [PubMed] [Google Scholar]
- 7. Coid J, Yang M, Tyrer P, et al. . Prevalence and correlates of personality disorder in Great Britain. Br J Psychiatry 2006;188:423–31. 10.1192/bjp.188.5.423 [DOI] [PubMed] [Google Scholar]
- 8. Newton-Howes G, Tyrer P, Anagnostakis K, et al. . The prevalence of personality disorder, its comorbidity with mental state disorders, and its clinical significance in community mental health teams. Soc Psychiatry Psychiatr Epidemiol 2010;45:453–60. 10.1007/s00127-009-0084-7 [DOI] [PubMed] [Google Scholar]
- 9. McCrone P, Patel A, Knapp M, et al. . Paying the price: the cost of mental health care in England to 2026. London: King's Fund, 2008. http://www.kingsfund.org.uk/sites/files/kf/Paying-the-Price-the-cost-of-mental-health-care-England-2026-McCrone-Dhanasiri-Patel-Knapp-Lawton-Smith-Kings-Fund-May-2008_0.pdf [Google Scholar]
- 10. Johnson JG, Cohen P, Kasen S, et al. . Associations of parental personality disorders and axis I disorders with childrearing behavior. Psychiatry 2006;69:336–50. 10.1521/psyc.2006.69.4.336 [DOI] [PubMed] [Google Scholar]
- 11. Newman LK, Stevenson CS, Bergman LR, et al. . Borderline personality disorder, Mother–Infant interaction and parenting perceptions: preliminary findings. Aust N Z J Psychiatry 2007;41:598–605. 10.1080/00048670701392833 [DOI] [PubMed] [Google Scholar]
- 12. Green H, McGinnity A, Meltzer H, et al. . Mental health of children and young people in Great Britain, 2004. Basingstoke: Palgrave Macmillan, 2005. http://www.esds.ac.uk/doc/5269/mrdoc/pdf/5269technicalreport.pdf [Google Scholar]
- 13. Davis H, Day C, Cox A, et al. . Child and adolescent mental health needs assessment and service implications in an inner City area. Clin Child Psychol Psychiatry 2000;5:169–88. 10.1177/1359104500005002003 [DOI] [Google Scholar]
- 14. Romeo R, Knapp M, Scott S. Economic cost of severe antisocial behaviour in children - and who pays it. Br J Psychiatry 2006;188:547–53. 10.1192/bjp.bp.104.007625 [DOI] [PubMed] [Google Scholar]
- 15. Parsonage M, Khan L, Saunders . Building a better future: the lifetime costs of childhood behavioural problems and the benefits of early intervention. Lond Cent Ment Health, 2014. [Google Scholar]
- 16. Sved Williams AE, Yelland C, Hollamby S, et al. . A new therapeutic group to help women with borderline personality disorder and their infants. J Psychiatr Pract 2018;24:331–40. 10.1097/PRA.0000000000000330 [DOI] [PubMed] [Google Scholar]
- 17. Department of Health,, Department for Education . Transforming Children and Young People’s Mental Health Provision: A Green Paper. London: DoH/DfE, 2017. [Google Scholar]
- 18. Social Care Institute for Excellence Think child, think parent, think family: a guide to parental mental health and child welfare, 2011. Available: https://www.scie.org.uk/publications/guides/guide30/summary.asp [Accessed 31 May 18].
- 19. Mental Health Taskforce The five year forward view of mental health. mental health Taskforce, 2016. Available: www.england.nhs.uk/mentalhealth/taskforce [Accessed 2 Nov 18].
- 20. Parker G, Beresford B, Clarke S. Technical report for SCIE research review on theprevalence and incidence of parental mental healthproblems and the detection, screening and reporting ofparental mental health problems. University of York, 2008. [Google Scholar]
- 21. Wilson R, Weaver T, Michelson D, et al. . Experiences of parenting and clinical intervention for mothers affected by personality disorder: a pilot qualitative study combining parent and clinician perspectives. BMC Psychiatry 2018;18 10.1186/s12888-018-1733-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. National Institute for Health and Clinical Excellence Antisocial behaviour and conduct disorders in children and young people: recognition, intervention and management. London: NICE, 2013. [PubMed] [Google Scholar]
- 23. Michelson D, Davenport C, Dretzke J, et al. . Do evidence-based interventions work when tested in the "real world?" A systematic review and meta-analysis of parent management training for the treatment of child disruptive behavior. Clin Child Fam Psychol Rev 2013;16:18–34. 10.1007/s10567-013-0128-0 [DOI] [PubMed] [Google Scholar]
- 24. Reyno SM, McGrath PJ. Predictors of parent training efficacy for child externalizing behavior problems--a meta-analytic review. J Child Psychol Psychiatry 2006;47:99–111. 10.1111/j.1469-7610.2005.01544.x [DOI] [PubMed] [Google Scholar]
- 25. Lundahl B, Risser HJ, Lovejoy MC. A meta-analysis of parent training: moderators and follow-up effects. Clin Psychol Rev 2006;26:86–104. 10.1016/j.cpr.2005.07.004 [DOI] [PubMed] [Google Scholar]
- 26. Dawe S, Harnett P. Improving family functioning in methadone maintained families: results from a randomised controlled trial. J Subst Abuse Treat 2007;32:381–90. [DOI] [PubMed] [Google Scholar]
- 27. Thanhäuser M, Lemmer G, de Girolamo G, et al. . Do preventive interventions for children of mentally ill parents work? results of a systematic review and meta-analysis. Curr Opin Psychiatry 2017;30:283–99. 10.1097/YCO.0000000000000342 [DOI] [PubMed] [Google Scholar]
- 28. Craig P, Dieppe P, Macintyre S, et al. . Developing and evaluating complex interventions: new guidance. London: Medical Research Council, 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Hoffmann TC, Glasziou PP, Boutron I, et al. . Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ 2014;348:g1687 10.1136/bmj.g1687 [DOI] [PubMed] [Google Scholar]
- 30. Eldridge SM, Chan CL, Campbell MJ, et al. . Consort 2010 statement: extension to randomised pilot and feasibility trials. Pilot Feasibility Stud 2016;2:64 10.1186/s40814-016-0105-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Bateman AW, Fonagy P. Effectiveness of psychotherapeutic treatment of personality disorder. Br J Psychiatry 2000;177:138–43. 10.1192/bjp.177.2.138 [DOI] [PubMed] [Google Scholar]
- 32. McMurran M, Crawford MJ, Reilly JG, et al. . Psycho-education with problem solving (PEPs) therapy for adults with personality disorder: a pragmatic multi-site community-based randomised clinical trial. Trials 2011;12:198 10.1186/1745-6215-12-198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Day C, Kowalenko S, Ellis M, et al. . The helping families programme: a new parenting intervention for children with severe and persistent conduct problems. Child Adolesc Ment Health 2011;16:167–71. 10.1111/j.1475-3588.2010.00588.x [DOI] [PubMed] [Google Scholar]
- 34. Harnett PH, Dawe S. Reducing child abuse potential in families identified by social services: implications for assessment and treatment. Brief Treat Crisis Interv 2008;8:226–35. 10.1093/brief-treatment/mhn010 [DOI] [Google Scholar]
- 35. Gray AS, Townsend ML, Bourke ME, et al. . Effectiveness of a brief parenting intervention for people with borderline personality disorder: a 12-month follow-up study of clinician implementation in practice. Advances in Mental Health 2019;17:33–43. 10.1080/18387357.2018.1464887 [DOI] [Google Scholar]
- 36. Day C, Ellis. M, Harris . Family partnership model reflective practice Handbook. 2nd Edn South London: Maudsley NHS Foundation Trust/King’s College, London, 2015. [Google Scholar]
- 37. McMurran M, Huband N, Overton E. Non-completion of personality disorder treatments: a systematic review of correlates, consequences, and interventions. Clin Psychol Rev 2010;30:277–87. 10.1016/j.cpr.2009.12.002 [DOI] [PubMed] [Google Scholar]
- 38. Tetley A, Jinks M, Huband N, et al. . Barriers to and facilitators of treatment engagement for clients with personality disorder: a Delphi survey. Personal Ment Health 2012;6:97–110. 10.1002/pmh.1176 [DOI] [Google Scholar]
- 39. Kazdin AE. Acceptability of alternative treatments for deviant child behavior. J Appl Behav Anal 1980;13:259–73. 10.1901/jaba.1980.13-259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Foster SL, Mash EJ. Assessing social validity in clinical treatment research: issues and procedures. J Consult Clin Psychol 1999;67:308–19. 10.1037/0022-006X.67.3.308 [DOI] [PubMed] [Google Scholar]
- 41. Bugge C, Williams B, Hagen S, et al. . A process for decision-making after pilot and feasibility trials (ADEPT): development following a feasibility study of a complex intervention for pelvic organ prolapse. Trials 2013;14:353 10.1186/1745-6215-14-353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Oud M, Arntz A, Hermens MLM, et al. . Specialized psychotherapies for adults with borderline personality disorder: a systematic review and meta-analysis. Aust N Z J Psychiatry 2018;52:949–61. 10.1177/0004867418791257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Day C, Briskman J, Crawford MJ, et al. . Helping families Programme-Modified: development of a specialised parenting intervention for parents affected by severe personality difficulties and randomised feasibility trial. Health Technol Assess. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Moran P, Leese M, Lee T, et al. . Standardised Assessment of Personality - Abbreviated Scale (SAPAS): preliminary validation of a brief screen for personality disorder. Br J Psychiatry 2003;183:228–32. 10.1192/bjp.183.3.228 [DOI] [PubMed] [Google Scholar]
- 45. Goodman R, Ford T, Richards H, et al. . The development and well-being assessment: description and initial validation of an integrated assessment of child and adolescent psychopathology. J Child Psychol Psychiatry 2000;41:645–55. 10.1111/j.1469-7610.2000.tb02345.x [DOI] [PubMed] [Google Scholar]
- 46. Day C, Michelson D, Thomson S, et al. . Evaluation of a peer led parenting intervention for disruptive behaviour problems in children: community based randomised controlled trial. BMJ 2012;344:e1107 10.1136/bmj.e1107 [DOI] [PubMed] [Google Scholar]
- 47. van Reenen M, Janssen B. EQ-5D-5L user guide, 2015. Available: https://euroqol.org/wp-content/uploads/2016/09/EQ-5D-5L_UserGuide_2015.pdf [Accessed 29 May 2018].
- 48. Wille N, Badia X, Bonsel G, et al. . Development of the EQ-5D-Y: a child-friendly version of the EQ-5D. Qual Life Res 2010;19:875–86. 10.1007/s11136-010-9648-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Eyberg SM, Ross AW. Assessment of child behavior problems: the validation of a new inventory. J Clin Child Psychol 1978;7:113–6. 10.1080/15374417809532835 [DOI] [Google Scholar]
- 50. Achenbach T, Rescorla L. Manual for the ASEBA school-age forms and profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth & Families, 2001. [Google Scholar]
- 51. Arnold DS, O'Leary SG, Wolff LS, et al. . The parenting scale: a measure of dysfunctional parenting in discipline situations. Psychol Assess 1993;5:137–44. 10.1037/1040-3590.5.2.137 [DOI] [Google Scholar]
- 52. James DE, Schumm WR, Kennedy CE, et al. . Characteristics of the Kansas parental satisfaction scale among two samples of married parents. Psychol Rep 1985;57:163–9. 10.2466/pr0.1985.57.1.163 [DOI] [Google Scholar]
- 53. Müller JM, Postert C, Beyer T, et al. . Comparison of eleven short versions of the symptom checklist 90-Revised (SCL-90-R) for use in the assessment of general psychopathology. J Psychopathol Behav Assess 2010;32:246–54. 10.1007/s10862-009-9141-5 [DOI] [Google Scholar]
- 54. Hatcher RL, Gillaspy JA. Development and validation of a revised short version of the working alliance inventory. Psychotherapy Research 2006;16:12–25. 10.1080/10503300500352500 [DOI] [Google Scholar]
- 55. Beecham J, Knapp M. Thornicroft G, Costing psychiatric interventions. London, Gaskell: Measuring Mental Health Needs, 2001. [Google Scholar]
- 56. Hertzog MA. Considerations in determining sample size for pilot studies. Res Nurs Health 2008;31:180–91. 10.1002/nur.20247 [DOI] [PubMed] [Google Scholar]
- 57. Browne RH. On the use of a pilot sample for sample size determination. Stat Med 1995;14:1933–40. 10.1002/sim.4780141709 [DOI] [PubMed] [Google Scholar]
- 58. Brown H, R P. Applied mixed models in medicine. 2nd Edn New York: John Wiley & Sons, 2007. [Google Scholar]
- 59. Involve Payment for involvement: a guide for making payments to members of the public actively involved in NHS, public health and social care research. Eastleigh: INVOLVE, 2010. [Google Scholar]
- 60. McMurran M, Delport J, Wood K, et al. . Recruitment to personality disorder treatment trials. Mental Health Review Journal 2012;17:119–27. 10.1108/13619321211287166 [DOI] [Google Scholar]
- 61. Stines LR, Feeny NC. Unique ethical concerns in clinical trials comparing psychosocial and psychopharmalogical interventions. Ethics Behav 2008;18:234–46. 10.1080/10508420802064333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Cooper AA, Conklin LR. Dropout from individual psychotherapy for major depression: a meta-analysis of randomized clinical trials. Clin Psychol Rev 2015;40:57–65. 10.1016/j.cpr.2015.05.001 [DOI] [PubMed] [Google Scholar]
- 63. Barnicot K, Katsakou C, Marougka S, et al. . Treatment completion in psychotherapy for borderline personality disorder: a systematic review and meta-analysis. Acta Psychiatr Scand 2011;123:327–38. 10.1111/j.1600-0447.2010.01652.x [DOI] [PubMed] [Google Scholar]
- 64. Lindström D, Sundberg-Petersson I, Adami J, et al. . Disappointment and drop-out rate after being allocated to control group in a smoking cessation trial. Contemp Clin Trials 2010;31:22–6. 10.1016/j.cct.2009.09.003 [DOI] [PubMed] [Google Scholar]
- 65. Cook T, Campbell D. Quasi-experimentation: design and analysis issues for field settings. Chicago: Rand McNally, 1979. [Google Scholar]
- 66. McMain SF, Boritz TZ, Leybman MJ. Common strategies for cultivating a positive therapy relationship in the treatment of borderline personality disorder. J Psychother Integr 2015;25:20–9. 10.1037/a0038768 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.