Abstract
Introduction
Nursing home residents represent a particularly vulnerable population experiencing high risk of unplanned hospital admissions, but few interventions have proved effective in reducing this risk. The aim of this research will be to verify the effects of a hospital-based multidisciplinary mobile unit (MMU) team intervention delivering urgent care to nursing home residents directly at their bedside.
Methods and analysis
Four nursing homes based in the Parma province, in Northern Italy, will be involved in this prospective, pragmatic, multicentre, 18-month quasiexperimental study (sequential design with two cohorts). The residents of two nursing homes will receive the MMU team care intervention. In case of urgent care needs, the nursing home physician will contact the hospital physician responsible for the MMU team by phone. The case will be triaged as (a) manageable by phone advice, (b) requiring urgent assessment by the MMU team or (c) requiring immediate emergency department (ED) referral. MMU team is composed of one senior physician and one emergency-medicine resident chosen within the staff of Internal Medicine and Critical Subacute Care Unit of Parma University-Hospital, usually with different specialty background, and equipped with portable ultrasound, set of drugs and devices useful in urgency. The MMU visits patients in nursing homes, with the mission to stabilise clinical conditions and avoid hospital admission. Residents of the other two nursing homes will receive usual care, that is, ED referral in every case of urgency. Study endpoints include unplanned hospital admissions (primary), crude all-cause mortality, hospital mortality, length of stay and healthcare-related costs (secondary).
Ethics and dissemination
The study protocol was approved by the Ethics Committee of Area Vasta Emilia Nord (Emilia-Romagna region). Informed consent will be collected from patients or legal representatives. The results will be actively disseminated through peer-reviewed journals and conference presentations, in compliance with the Italian law.
Trial registration number
ClinicalTrials.gov Registry (NCT 04085679); Pre-results.
Keywords: geriatric medicine, organisation of health services, quality in health care
Strengths and limitations of this study.
This study will explore the effectiveness of a complex intervention focused on the avoidance of hospital admissions for nursing home residents, with a strong hospital-community partnership.
The study intervention consists in bringing specialist hospital care directly at the bedside of nursing home residents, an innovative approach not previously described in the scientific literature.
The intervention has been developed considering the organisation of the Italian healthcare system but is reproducible and applicable in other settings.
Due to ethical concerns and the complex nature of the intervention, individual randomisation of participants is not possible.
The quasiexperimental design of the study allows an optimal compromise between soundness and feasibility, facilitating the transferability of results into clinical practice.
Introduction
The increasing clinical complexity of older medical patients, due to multimorbidity, polypharmacy, frailty, disability and social hardship, is challenging for healthcare systems.1 2 These characteristics are emphasised in nursing home residents, who experience a particularly high risk of emergency department (ED) visits and hospitalisation (greater than 20% per year).3–8 In the ED, these patients may experience misdiagnoses and undertreatment due to their complexity and atypical presentation of acute illness and contribute to the overcrowding phenomenon.4 5 9–11 Once admitted to wards, they are also more likely to have long stays (>2 weeks)9 and experience hospital-related complications.12 Additionally, when they are discharged back to nursing homes, they may experience further adverse events related to care transitions.6 12
In the light of these considerations, confirmed by large cohort studies conducted in the USA and Canada,7 8 a number of approaches have been developed to reduce the risk of hospitalisation in nursing home residents. These are summarised in the systematic review by Santosaputri et al,13 which includes quantitative comparative studies of all designs aiming to determine the efficacy of interventions provided by geriatric health professionals. Sixteen studies were eligible, of which six randomised controlled trials, involving an estimated total of over 7400 patients. The authors of the review categorised 14 intervention programme into three primary approaches (two did not fit in any category):
Prevention approach (nine studies): interventions (such as direct review of patients, telemedicine, comprehensive geriatric assessment) delivered in the nursing home by nurses, physicians and sometimes allied health personnel to prevent hospitalisation of residents.
ED‐based hospital avoidance (three studies): interventions provided by nursing staff (such as wound care or catheter management) targeting nursing home residents during ED visits.
Posthospital supported discharge (two studies): interventions designed to support residents in the care transition from the hospital to nursing home, including geriatrician and nurse review in the facility and standardised rehabilitation programme.
Although the majority of the studies reported reductions in hospitalisations, only six, with different designs and interventions, obtained statistically significant findings.14–19 Two of these studies, with retrospective design, involved delivery of routine care to nursing home residents by hospital-based nursing staff, with the possibility of obtaining support from a geriatrician in case of urgent situations.14 15 In another prospective quasiexperimental study, a team including a geriatrician and specialised nurses supported the nursing home physician in delivering routine care and in managing urgent clinical situations.16 The remaining three studies, all with prospective quasiexperimental design, were more focused on selected clinical scenarios, involving advice and education by ED staff to nursing home personnel after ED admission of residents,17 hospital nurse visits in the nursing home to implement strategies of delirium prevention18 and rehabilitation intervention delivered by a geriatric orthopaedic team to residents with hip fracture.19
Unfortunately, the quality of evidence was considered low to moderate, therefore further, well-designed studies are needed to identify which interventions are effective in reducing hospitalisation in the older residents.13 The interventions performed in the existing studies were also mainly focused on routine care, while a prompt and correct management of urgent situations and acute/subacute conditions may be fundamental for avoiding ED admissions in nursing home residents.7 20 Namely, interventions delivering urgent care with a multidisciplinary approach, based on geriatric expertise and on the capacity of performing first-line diagnostic examinations, such as ultrasonography, and basic invasive procedures, such as central venous line or nasogastric tube insertion, have a great potential of being successful in reducing ED visits, but have not been adequately investigated to date.7 20
At our institution, different projects have been carried out for many years to improve care of the elderly, primarily targeting hospital organisation, with the main objective to reduce unnecessary, avoidable length of stay (LOS).21–23 These efforts benefit inhospital patients but are not designed to prevent hospitalisations. In this framework, based on literature evidence, best current knowledge and long-time experience with elderly care developed at our university hospital, we hypothesise that a complex intervention delivered in nursing homes, where vulnerable high-risk patients live, involving direct patient care by hospital medical staff with multidisciplinary approach grounded on geriatric expertise, may reduce hospitalisation of residents.
Methods and analysis
Study setting
The study is based in the University Hospital of Parma, which has a catchment area of more than 400 000 inhabitants, of whom 22.3% is over 65 years old. It provides the only emergency service of the district, and it ranks fourth in Italy by number of ED visits (yearly average of over 110 000). The average admission rate of the adult ED population is 18%, of which 65% concern people older than 65.
In the last two decades, the University Hospital of Parma has implemented several innovative initiatives to manage the hospital flow of frail multimorbid patients and their complex needs. These initiatives included bed management to avoid ‘bed-blockers’,21 physician accountability for the discharge process22 and creation of a dedicated hospital unit, organised by intensity of care to anticipate the needs of these patients preserving high-performance indices.23 The multidisciplinary mobile unit (MMU) team will be based in this unit, called Internal Medicine and Critical Subacute Care.
Nursing homes participating in the study are public facilities of similar size (90–100 residents) which ensure the presence of nursing staff 24 hours a day and a physician at least 4 hours a day (high-intensity care facilities), in compliance with the care standards set by the Local Health Authority. No staff member is shared among the participating nursing homes. The possible role of distance to the hospital is considered by including in each group one nursing home located next to the hospital and one located at a distance of >5 km.
The participating nursing homes are the following Case Residenza Anziani (CRAs):
CRA ‘I Tigli’ Parma (intervention group).
CRA ‘Casa degli Anziani’, Collecchio (intervention group).
CRA ‘Le Tamerici’ Parma (control group).
CRA ‘Ines Ubaldi’, Parma (control group).
This study follows a multimethod approach, based on the Medical Research Council framework for developing and evaluating complex interventions,24 including the development, feasibility assessment and evaluation phases.
Development of the intervention
First, the different types of approaches reported in the literature, described above, were considered.13 The ‘prevention approach’, interventions conducted in nursing homes, was chosen as the most suitable strategy to integrate the hospital’s organisational model already in place, as it can target both hospitalisation rates and ED overcrowding, allowing to intervene before the person accesses the hospital.
Available evidence also prompted us to opt for a multicomponent approach. In fact, the current literature, mainly based on qualitative interviews with nursing home staff members in different countries, suggests that the decision to transfer residents to hospital may be influenced by different factors, such as staffing and skill mix in the nursing homes, treatment options available in the facility, end‐of‐life decision‐making and communication and bureaucratic requirements.25 This multifactorial association means that a multicomponent intervention is likely to be more effective than a single‐component intervention.26
Based on the Schippinger et al 16 and Diaz-Gegundez et al 27 studies, that obtained significant reduction of hospital admissions, we created a mobile physician service. Unlike those studies, we did not involve a nurse, because the participating facilities have nursing staff available 24 hours a day, and we used medical hospital staff because routine clinical management and scheduled follow-up evaluations are already performed by nursing home physicians during their office hours.
Finally, medical hospital staff was preferred to community geriatricians, on the assumption that older patients may feel more comfortable being handled by physicians who may have already cared for them at the hospital. Moreover, hospital staff enables direct patient referral to the ward. Finally, this allows the use of diagnostic technologies available at the hospital, which can be used immediately without the need for hospital admission.
Description of the intervention
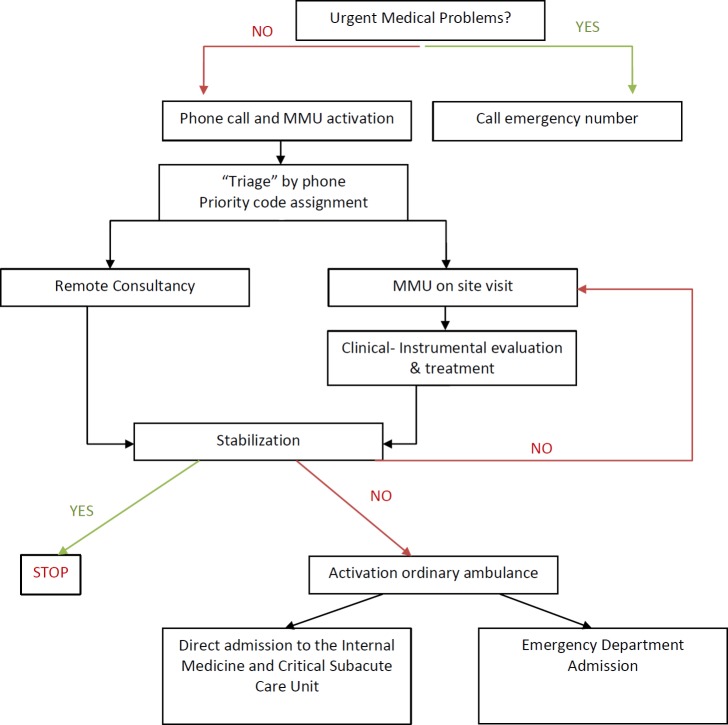
The model hinges on the strong collaboration between hospital and nursing home staff to provide residents with patient-centred care. It entails a multicomponent intervention which is integrated in standard care and comprises three steps: (1) MMU team activation, (2) on site visit by a team of physicians with geriatric expertise, (3) interdisciplinary care planning (figure 1).
Figure 1.
Description of the intervention of MMU team. MMU, multidisciplinary mobile unit.
Step 1: MMU team activation
Patient selection is necessary to ensure that available resources are used for patients who may really benefit. To this end, in case of need, the nursing home physician contacts by phone the ‘flow manager’, a skilled internist with strong clinical expertise, organisational attitude and managerial training, during the 08:00–18:00 time frame, Monday–Friday. The phone consultation is reported on a form containing the description of the patient’s clinical condition and a summary of the conversation. The form also indicates which decision was reached among the following six not mutually exclusive options:
The patient can be managed by nursing home staff, therapeutic advice is provided by phone.
Remote reassessment is scheduled after a number of hours agreed on by the team.
The MMU team is dispatched for evaluation, treatment and stabilisation on site.
A significant change in vital parameters is observed which requires immediate activation of emergency services.
Direct hospital admission is considered necessary.
Ambulatory outpatient visits or tests are planned.
Step 2: on site visit by a team of physicians with geriatric expertise
Visits at the nursing home are performed by two members of the MMU team: an expert hospital physician chosen on a case-by-case basis among the clinical staff of the Internal Medicine and Critical Subacute Care Unit, depending on the disease or clinical problem that must be treated and a specifically trained resident in Emergency Medicine. The physicians that may be involved in MMU activation include specialists in internal medicine, clinical ultrasonography, gastroenterology, geriatrics or clinical nutrition.
The team is provided with a car to reach the nursing homes, a portable ultrasound system and an essential set of drugs and medical devices useful in an emergency setting. The ultrasound system is equipped with three probes (convex, linear and phased array) for performing thoracopulmonary, cardiac, vascular, abdominal and soft tissue ultrasound when required. Available drugs include those that can be administered intravenously for treating urgent conditions (eg, loop diuretics, steroids, fluids, antibiotics). Devices include central and peripheral venous lines, nasogastric and rectal tubes and bladder catheters. Blood tests can also be performed.
Table 1 shows possible clinical scenarios which may require MMU team activation and possible decisions.
Table 1.
Overview of possible expected clinical situations for which a multidisciplinary mobile unit consultation may be activated and possible management
| Clinical situation | Clinical question | Mobile unit intervention | Disposition |
| Dyspnoea of unknown origin | Pulmonary? Cardiac? Embolism? Other causes? | Chest and abdomen ultrasound. Arterial gas sample, ECG, intravenous antibiotic administration. | Appropriate diagnosis and treatment on site. Immediate or scheduled admission whenever appropriate. |
| Abdominal pain | Gallbladder stones? Cholecystitis? Renal colic? Diverticular disease? Urinary retention? Faecal impaction? Peritonitis? Ascites? Acute/subacute Hernia? | Abdomen ultrasound, basic blood tests, intravenous antibiotic administration. | Appropriate diagnosis and treatment on site. Immediate or scheduled admission whenever appropriate. |
| Haematuria | UTI? Catheter dysfunction? Bladder polyps? Stones? | Abdomen ultrasound, bladder lavage, catheter (re-)positioning, intravenous antibiotic administration. | Appropriate diagnosis and treatment on site. Immediate or scheduled admission whenever appropriate. |
| Psychomotor agitation in previously stable dementia | Inadequate therapy? Emerging internistic problem? Other | CGA, neurogeriatric visit, exclusion of internistic emerging problem, ECG, thoracic and abdominal ultrasound. | Appropriate diagnosis and treatment on site. |
| Fever | Origin? | Thoracic and abdominal ultrasound, basic blood test. | Excluding common differential diagnosis. |
| Absence of peripheral veins for drugs or nutrients infusion | How to find adequate venous access | Ultrasound-guided central venous catheter or PICC or peripheral access. | Securing patient. |
| Monolateral leg oedema | DVT? Erysipelas? Trauma? | Venous and soft tissues ultrasound. | Appropriate diagnosis and treatment on site. |
| Terminal illness | Palliation strategy? How to get symptoms relief? | CGA. Multidisciplinary assessment. Positioning of drains (eg, abdominal drainage for ascites). Interview with relatives/caregivers and GP for sharing strategies. | Appropriate management. |
| Ultrasound examination in a patient who can be transported with difficulty | GP’s question | Abdominal, cardiac, arterial, thyroid, neck ultrasound. | Appropriate assessment. |
CGA, Comprehensive Geriatric Assessment; DVT, deep vein thrombosis; GP, general practitioner; PICC, peripherally inserted central venous catheter; UTI, urinary tract infection.
Step 3: interdisciplinary care planning
Based on the results of the visit and of any performed investigations, the MMU team formulates personalised advice and referrals and discusses these with the nursing home physician. If stabilisation on site is not deemed possible, the MMU team plans a direct admission to the Internal Medicine and Critical Subacute Care Unit, thus avoiding ED access. The planning and the final outcome of the intervention are recorded in the second part of the form.
Feasibility assessment
A pilot phase of 5 months (December 2018–April 2019) was conducted in the two nursing homes participating to the study as intervention group to look at feasibility of the MMU care model described above. Before the intervention was introduced, meetings were held with nursing home staff to agree on activation modalities.
In this period, 99 phone calls were received, of which 84 required MMU team onsite visits, and 15 were managed with remote consultancy. Of the latter, three required direct admission after remote phone consultancy. Only 4 of the 84 patients visited onsite required direct admission. One patient was sent to the ED for massive intestinal bleeding (figure 2).
Figure 2.
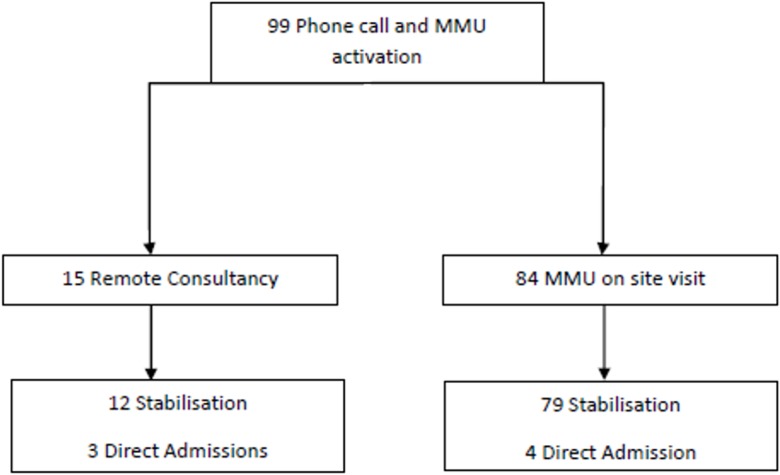
Results of pilot phase. MMU, multidisciplinary mobile unit.
This phase demonstrated the feasibility of the intervention and did not highlight any need for modifications.
Evaluation phase (current study)
Aim and objectives
The study aim is to verify the effects of the implementation of the MMU care model tested in the pilot phase.
Primary objective is to verify reduction of unplanned hospitalisation rates in the nursing homes of the intervention group compared with the nursing homes in the control group. Secondary objectives are to measure the effects of the intervention in terms of crude all-cause mortality, hospital mortality, length of stay and healthcare-related costs.
Study design
This study is a prospective, pragmatic, cluster-multicentre, quasiexperimental study (sequential design with two cohorts), in which usual nursing home care is compared with care provided by applying the MMU model.
The cluster design was selected because the intervention is organisational and requires high involvement of all centre staff; therefore, randomising individual clinicians or patients would entail a high risk of contamination bias. A quasirandomised design was chosen as it prevents the need to discontinue the intervention conducted in two nursing homes which had participated in the pilot phase and would thus be more acceptable by staff. Furthermore, quasiexperiments do not imply the selection effects and ‘artificiality’ of randomised trials and are thus more suitable for studies on intervention implementation in real life, enabling a high degree of external validity.28
Study population
All residents staying in the participating nursing homes at the moment of study initiation or admitted afterwards are eligible for inclusion, regardless of their clinical status. Informed consent will be collected from patients or their proxies/legal representatives, according to the European Union law. Refusal to provide informed consent, either by patients or legal representatives, will imply study exclusion.
Usual care
Patients in the control cohort receive usual care, which means the actions to take are decided by the nursing home staff. Generally, this implies that patients who are clinically unstable, or require urgent instrumental tests, will be sent to the ED.
Measures: baseline variables
Demographic data on gender and age are collected by chart review.
Measures: outcome variables
The primary outcome is hospitalisation rate, considering at the numerator all unplanned admissions occurred during a 1-year period and at the denominator the sum of the person-time of the at risk population (days of stay at the nursing home). For the intervention group, the numerator corresponds to options (d) and (e) defined in ‘Step 1: MMU team activation’ (activation of emergency services and direct hospital admission).
The secondary outcomes are the following:
Crude all-cause death rate (CDR): the number of deaths during 1-year period on person-time of the at risk population.
Hospital mortality rate: the frequency of patients who die while in the hospital (death rate/1000).
Length of stay (LOS): the duration of a single episode of hospitalisation. Inpatient days are calculated by subtracting day of admission from day of discharge.
Adverse events or complications: frequency of events with novel unexpected worsening of clinical conditions, defined as alterations of vital signs, occurring within 48 hours from MMU team activation, for which hospital access becomes necessary.
Costs analysis, comparing the cost differences in the two groups.
Data collection
Patient demographic and clinical characteristics will be collected at baseline from nursing home clinical records to describe the study population and determine hospital admission rate. For participants in the control group, only data on age, sex, timing of admission and discharge in nursing home will be collected. For those in the intervention group, additional data on any MMU activation (reasons, timing, intervention, procedures and outcomes) will be collected with a specific case report form (CRF).
Participants’ files and electronic data will be stored securely at the study site (eg, locked area, password-protected hardware and software). Data integrity will be scrutinised with several strategies (eg, valid values, range checks, consistency checks). Patient data will be only identifiable with the unique participant’s number. Personal information will be collected and saved in a separate file (on a different server) which can only be accessed by the principal investigator. For the primary outcome, information will be obtained using administrative databases of the hospital and nursing homes. For secondary outcomes, the following data sources will be used: validated regional death registry to determine CDR; electronic discharge summaries to calculate hospital mortality rate and LOS; electronic ED registry to detect adverse events or complications; hospital administrative database and CRF for the cost analysis. Residents’ identification data will be deleted once the study is completed, making the dataset anonymous. All study protocol authors will have access to the anonymous dataset.
Study duration
Overall expected duration is 18 months, with study initiation presumably in January 2020 and completion in June 2021.
Statistical methodology
Sample size calculation
The number of subjects to include was estimated using the findings of Diaz-Gegundez et al, who performed a large quasiexperimental trial.27 Thus, considering 56 cases versus 32 cases per 100 residents and using a two-sided, large-samples z-test of the Poisson incidence rate difference at a significance level of 0.05, and with a power of 0.90, overall 338 residents should be enrolled. Since each of the participating nursing homes has between 90 and 100 residents, the study appears as feasible.
Statistical analysis plan
Descriptive statistics will be used to summarise patient populations and will be presented as means and SDs when normally distributed or as medians and IQRs.
For the primary analysis, we will used Poisson regression with robust SEs to evaluate relative differences in hospital rates among our two cohorts while adjusting for demographic characteristics.
Concerning the secondary outcomes, the following analyses will be performed:
Rates will be compared considering the quotient between the intervention and control groups.
A log-normal model will be used to compare inhospital LOS.
χ2 tests will be conducted for categorical data as adverse events or complications.
The demographic and clinical variables which influence the outcome with a p value <0.20 in the univariate analysis will be included in the Poisson regression model.
Finally, cost analysis will be performed. We will identify the changes in net costs associated with 1-year exposure to the intervention, consisting in the induced costs due to incremental resource inputs for carrying out the intervention and hospital health service use costs. Staffing costs will be calculated considering the time spent by the professionals involved in the intervention. Non-staff running costs include expenses of MMU staff travelling to and from the nursing home. The health service use costs will be identified based on the standard regional tariffs assigned to each admission according to the Diagnosis Related Group system. We will use the following equations to summarise the annual net costs associated with the implementation of the intervention. Any costs with negative values mean ‘savings’ and any costs with positive values mean ‘losses’. Net costs = A (intervention costs)±B (costs for differences in hospital health service use) where: A=intervention: staffing costs+intervention: non-staff costs and B=costs for differences in inpatient care use. Therefore, the net costs arising from 1-year implementation of the intervention as compared with the current practice will be obtained, where a negative value of net costs represents ‘cost-saving’ and a positive value represents ‘not cost-saving’.
The analyses will be performed using SAS V.8.2 (SAS Institute) and STATA-SE V.11 (StataCorp LP).
Patient and public involvement
No patient involved.
Ethics and dissemination
All participants or their legal representatives will sign informed consent form. This study does not entail any experimental pharmacological treatment or changes in the diagnostic-therapeutic pathway. Eligible patients or their legal representatives will be also asked to give written consent to handling of their personal data. If a patient wishes to discontinue his/her participation in the study, it is the responsibility of the investigator to ensure that no further data regarding the person’s health condition shall be collected. All collected data will be used in the final analysis.
All data collected, handled and stored for the purpose of this study will be kept confidential at any time and will be securely stored, as required in Good Clinical Practice guidelines and in current privacy legislation.
Discussion
The MMU-1 study will represent one of the first attempts to prevent hospital admissions of nursing home residents by using a multicomponent complex intervention with a strong multidisciplinary approach. Most of previous studies in this field were in fact focused on geriatric routine care, nurse counselling and education but did not deliver diagnostic and therapeutic interventions at the bedside in case of urgent needs.13–19 27 The multidisciplinary skills of MMU-1 staff, that may involve expert physicians with different skills and background depending on the clinical problem of patients, represents a novelty at the current literature state of the art and has a great potential of being successful in preventing hospital admission, considering the high clinical complexity of nursing home residents. The use of bedside ultrasound equipment also represents a high value added to the care of these patients, allowing to reach a high diagnostic accuracy and to perform invasive procedures without moving patients to the hospital.29 30 The use of bedside ultrasonography in geriatrics is becoming increasingly popular but is generally unavailable in nursing homes.29 30 When integrated with an accurate physical examination, bedside ultrasonography can dramatically improve the diagnostic process,31 especially in geriatric multimorbid patients where severity of symptoms, cognitive impairment and mobility limitations may reduce the accuracy of traditional imaging.29 30
Finally, the MMU-1 intervention is not fixed into a rigid algorithm, but different kinds of consultancy can be made according to the clinical situation of each patient (figure 1). This circumstance represents an advancement with respect of other interventions previously described in the literature,13 and an effort towards personalisation of geriatric care. Even in the two studies by Schippinger et al 16 and Diaz-Gegundez et al 27 reporting a significant reduction of hospital admissions, the intervention was rather fixed, centred exclusively on comprehensive geriatric assessment and lacked technological support such as bedside ultrasound.
Some limitations of this study should be considered. First, we acknowledge that the stepped wedge cluster randomised design would represent the best design for testing the effects of a novel care model implemented in multiple nursing homes. However, this was not feasible due to practical and economic barriers. In fact, it entails a larger sample size and study duration, and the currently available technical and human resources would not be sufficient to sustain MMU intervention delivery in more than two nursing homes at the same time. It is also noteworthy that most of the existing studies included in the Santosaputri review13 adopted a quasiexperimental design, because, in research on complex care interventions, methodological soundness must always face practical considerations on feasibility.28
In conclusion, if the results of this study suggest benefits for patients and the healthcare system, future investigations with sounder methodology should be implemented to assess a large-scale application of the proposed care model.
Supplementary Material
Footnotes
Contributors: AN, BP, SL, PM, EB, MF and TM conceptualised the project and designed the intervention. FD, AT, PS, FP, BS and CC provided relevant contributions for study conception and design. EL gave statistical consult. AN, CC, FD and AT drafted the manuscript. All the authors read and approved the final manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Not required.
Ethics approval: The study was approved by the competent Ethics Committee (Comitato Etico Area Vasta Emilia Nord, Emilia-Romagna region) under the ID 846/2019/OSS/AOUPR. The study will be conducted in compliance with the principles of the revision of the Helsinki Declaration and by current legislation on scientific research.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Corazza GR, Formagnana P, Lenti MV. Bringing complexity into clinical practice: an internistic approach. Eur J Intern Med 2019;61:9–14. 10.1016/j.ejim.2018.11.009 [DOI] [PubMed] [Google Scholar]
- 2. Mannucci PM, Nobili A, Pasina L, et al. . Polypharmacy in older people: lessons from 10 years of experience with the REPOSI register. Intern Emerg Med 2018;13:1191–200. 10.1007/s11739-018-1941-8 [DOI] [PubMed] [Google Scholar]
- 3. Samaras N, Chevalley T, Samaras D, et al. . Older patients in the emergency department: a review. Ann Emerg Med 2010;56:261–9. 10.1016/j.annemergmed.2010.04.015 [DOI] [PubMed] [Google Scholar]
- 4. Aminzadeh F, Dalziel WB. Older adults in the emergency department: a systematic review of patterns of use, adverse outcomes, and effectiveness of interventions. Ann Emerg Med 2002;39:238–47. 10.1067/mem.2002.121523 [DOI] [PubMed] [Google Scholar]
- 5. Salvi F, Morichi V, Grilli A, et al. . The elderly in the emergency department: a critical review of problems and solutions. Intern Emerg Med 2007;2:292–301. 10.1007/s11739-007-0081-3 [DOI] [PubMed] [Google Scholar]
- 6. Wyman JF, Hazzard WR. Preventing avoidable hospitalizations of nursing home residents: a multipronged approach to a perennial problem. J Am Geriatr Soc 2010;58:760–1. 10.1111/j.1532-5415.2010.02775.x [DOI] [PubMed] [Google Scholar]
- 7. LaMantia MA, Lane KA, Tu W, et al. . Patterns of emergency department use among long-stay nursing home residents with differing levels of dementia severity. J Am Med Dir Assoc 2016;17:541–6. 10.1016/j.jamda.2016.02.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Gruneir A, Cigsar C, Wang X, et al. . Repeat emergency department visits by nursing home residents: a cohort study using health administrative data. BMC Geriatr 2018;18:157 10.1186/s12877-018-0854-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Jay S, Whittaker P, Mcintosh J, et al. . Can consultant geriatrician led comprehensive geriatric assessment in the emergency department reduce hospital admission rates? A systematic review. Age Ageing 2017;46:366–72. [DOI] [PubMed] [Google Scholar]
- 10. Limpawattana P, Phungoen P, Mitsungnern T, et al. . Atypical presentations of older adults at the emergency department and associated factors. Arch Gerontol Geriatr 2016;62:97–102. 10.1016/j.archger.2015.08.016 [DOI] [PubMed] [Google Scholar]
- 11. Roberts DC, McKay MP, Shaffer A. Increasing rates of emergency department visits for elderly patients in the United States, 1993 to 2003. Ann Emerg Med 2008;51:769–74. 10.1016/j.annemergmed.2007.09.011 [DOI] [PubMed] [Google Scholar]
- 12. Buurman BM, Hoogerduijn JG, van Gemert EA, et al. . Clinical characteristics and outcomes of hospitalized older patients with distinct risk profiles for functional decline: a prospective cohort study. PLoS One 2012;7:e29621 10.1371/journal.pone.0029621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Santosaputri E, Laver K, To T. Efficacy of interventions led by staff with geriatrics expertise in reducing hospitalisation in nursing home residents: a systematic review. Australas J Ageing 2019;38:5–14. 10.1111/ajag.12593 [DOI] [PubMed] [Google Scholar]
- 14. Street M, Considine J, Livingston P, et al. . In-reach nursing services improve older patient outcomes and access to emergency care. Australas J Ageing 2015;34:115–20. 10.1111/ajag.12137 [DOI] [PubMed] [Google Scholar]
- 15. Hutchinson AF, Parikh S, Tacey M, et al. . A longitudinal cohort study evaluating the impact of a geriatrician-led residential care outreach service on acute healthcare utilisation. Age Ageing 2015;44:365–70. 10.1093/ageing/afu196 [DOI] [PubMed] [Google Scholar]
- 16. Schippinger W, Hartinger G, Hierzer E, et al. . Mobile geriatric consultant services for rest homes: study of the effects of consultations by internal medicine specialists in the medical care of rest home residents. Z Gerontol Geriatr 2012;45:735–41. [DOI] [PubMed] [Google Scholar]
- 17. Fan L, Hou X-Y, Zhao J, et al. . Hospital in the nursing home program reduces emergency department presentations and hospital admissions from residential aged care facilities in Queensland, Australia: a quasi-experimental study. BMC Health Serv Res 2015;16:46 10.1186/s12913-016-1275-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Boockvar KS, Teresi JA, Inouye SK. Preliminary data: an adapted Hospital elder life program to prevent delirium and reduce complications of acute illness in long-term care delivered by certified nursing assistants. J Am Geriatr Soc 2016;64:1108–13. 10.1111/jgs.14091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Gregersen M, Zintchouk D, Borris LC, et al. . A geriatric multidisciplinary and tailor-made hospital-at-home method in nursing home residents with hip fracture. Geriatr Orthop Surg Rehabil 2011;2:148–54. 10.1177/2151458511421908 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kirsebom M, Hedström M, Wadensten B, et al. . The frequency of and reasons for acute Hospital transfers of older nursing home residents. Arch Gerontol Geriatr 2014;58:115–20. 10.1016/j.archger.2013.08.002 [DOI] [PubMed] [Google Scholar]
- 21. Meschi T, Nouvenne A, Maggio M, et al. . Bed-blockers: an 8 year experience of clinical management. Eur J Intern Med 2012;23:e73–4. 10.1016/j.ejim.2011.11.012 [DOI] [PubMed] [Google Scholar]
- 22. Caminiti C, Meschi T, Braglia L, et al. . Reducing unnecessary Hospital days to improve quality of care through physician accountability: a cluster randomised trial. BMC Health Serv Res 2013;13:14 10.1186/1472-6963-13-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Meschi T, Ticinesi A, Prati B, et al. . A novel organizational model to face the challenge of multimorbid elderly patients in an internal medicine setting: a case study from Parma Hospital, Italy. Intern Emerg Med 2016;11:667–76. 10.1007/s11739-016-1390-1 [DOI] [PubMed] [Google Scholar]
- 24. Craig P, Dieppe P, Macintyre S, et al. . Developing and evaluating complex interventions: the new medical Research Council guidance. BMJ 2008;337:a1655 10.1136/bmj.a1655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Trahan LM, Spiers JA, Cummings GG. Decisions to transfer nursing home residents to emergency departments: a scoping review of contributing factors and staff perspectives. J Am Med Dir Assoc 2016;17:994–1005. 10.1016/j.jamda.2016.05.012 [DOI] [PubMed] [Google Scholar]
- 26. Arendts G, Howard K. The interface between residential aged care and the emergency department: a systematic review. Age Ageing 2010;39:306–12. 10.1093/ageing/afq008 [DOI] [PubMed] [Google Scholar]
- 27. Dìaz-Gegundez M, Paluzie G, Sanz-Ballester C, et al. . Evaluation of an intervention program in nursing homes to reduce hospital attendance. Rev Esp Geriatr Gerontol 2011;46:261–4. [DOI] [PubMed] [Google Scholar]
- 28. Bärnighausen T, Tugwell P, Røttingen J-A, et al. . Quasi-Experimental study designs series—paper 4: uses and value. J Clin Epidemiol 2017;89:21–9. 10.1016/j.jclinepi.2017.03.012 [DOI] [PubMed] [Google Scholar]
- 29. Ticinesi A, Scarlata S, Nouvenne A, et al. . The geriatric patient: the ideal one for chest ultrasonography? A review from the chest ultrasound in the elderly Study Group (GRETA) of the Italian Society of gerontology and geriatrics (SIGG). J Am Med Dir Assoc 2019. 10.1016/j.jamda.2019.06.018 [DOI] [PubMed] [Google Scholar]
- 30. Fröhlich E, Beller K, Muller R, et al. . Point of care ultrasound in geriatric patients: prospective evaluation of a portable handheld ultrasound device. Ultraschall in Med 2019. 10.1055/a-0889-8070 [DOI] [PubMed] [Google Scholar]
- 31. Narula J, Chandrashekhar Y, Braunwald E. Time to add a fifth Pillar to bedside physical examination: inspection, palpation, percussion, auscultation, and Insonation. JAMA Cardiol 2018;3:346–50. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.