Abstract
Background
Persistent patent ductus arteriosus (PDA) is associated with mortality and morbidity in preterm infants. Prostaglandin synthetase inhibitors such as indomethacin promote PDA closure but also have potential side effects. The effect of the prophylactic use of indomethacin, where infants who may not have gone on to develop a symptomatic PDA would be exposed to indomethacin, warrants particular scrutiny.
Objectives
To determine the effect of prophylactic indomethacin on mortality and morbidity in preterm infants.
Search methods
The standard search strategy of the Cochrane Neonatal Review Group was used. This included searches of the Cochrane Central Register of Controlled Trials (CENTRAL, The Cochrane Library, Issue 5, 2010), MEDLINE, EMBASE and CINAHL (until April 2010), conference proceedings, and previous reviews.
Selection criteria
Randomised or quasi‐randomised controlled trials that compared prophylactic indomethacin versus placebo or no drug in preterm infants.
Data collection and analysis
The standard methods of the Cochrane Neonatal Review Group were used, with separate evaluation of trial quality and data extraction by two review authors.
Main results
Nineteen eligible trials in which 2872 infants participated were identified. Most participants were very low birth weight, but the largest single trial restricted participation to extremely low birth weight infants (N = 1202). The trials were generally of good quality.
The incidence of symptomatic PDA [typical relative risk (RR) 0.44, 95% confidence interval (CI) 0.38 to 0.50] and PDA surgical ligation (typical RR 0.51, 95% CI 0.37,0.71) was significantly lower in treated infants. Prophylactic indomethacin also significantly reduced the incidence of severe intraventricular haemorrhage (typical RR 0.66, 95% CI 0.53 to 0.82). Meta‐analyses found no evidence of an effect on mortality (typical RR 0.96, 95% CI 0.81 to 1.12) or on a composite of death or severe neurodevelopmental disability assessed at 18 to 36 months old (typical RR 1.02, 95% CI 0.90, 1.15).
Authors' conclusions
Prophylactic indomethacin has short‐term benefits for preterm infants including a reduction in the incidence of symptomatic PDA, PDA surgical ligation, and severe intraventricular haemorrhage. However, there is no evidence of effect on mortality or neurodevelopment.
Plain language summary
Prophylactic intravenous indomethacin for preventing mortality and morbidity in preterm infants
Patent ductus arteriosus (PDA) occurs when an artery near the heart and lungs, which should close off soon after birth, stays open. Babies born preterm (premature) who have a PDA are at higher risk of severe illness and death. Indomethacin, a drug more commonly used for muscle and bone pain in adults, when given to preterm infants can help close a PDA. This review found evidence that giving all preterm infants (especially very preterm infants) indomethacin on the first day after birth reduced their risk of developing a PDA and the complications associated with PDA (including brain damage due to bleeding into the brain). However, despite these short term effects, the trials found evidence that indomethacin does not increase survival or reduce disability in the longer term.
Background
Description of the condition
About one‐third of very preterm or very low birth weight (VLBW) (birth weight < 1500 grams) infants develop a haemodynamically‐important patent ductus arteriosus (PDA) during the first few days after birth (Evans 1990). The incidence of PDA is inversely related to weight and gestational age at birth and is higher in infants with severe respiratory distress syndrome. PDA is persistent in about one‐half of extremely preterm or extremely low birth weight (ELBW) (birth weight < 1000 grams) infants (Evans 1995).
Following the postnatal fall in pulmonary vascular pressures, infants with a haemodynamically‐important PDA experience shunting of blood from the aorta to the pulmonary arterial circulation (Evans 1996). This "left to right" shunt alters the blood flow distribution to the lungs and other organs and may contribute to a higher risk of severe and prolonged respiratory distress syndrome, intraventricular haemorrhage (IVH), necrotising enterocolitis (NEC), bronchopulmonary dysplasia (BPD), and death in infants with a PDA compared to similar infants whose PDA has closed (Brown 1979; Lipman 1982).
Description of the intervention
PDA closure may be achieved surgically, by transthoracic ligation or transcatheter occlusion, or pharmacologically using prostaglandin synthetase inhibitors such as indomethacin or ibuprofen (Heymann 1976). Current data are insufficient to determine if surgical or medical treatment is the better initial option for closing a PDA in preterm infants (Malviya 2008; Mosalli 2008). Currently, surgical ligation or transcatheter occlusion is usually reserved for instances in which pharmacological intervention has been unsuccessful.
Three broad strategies of pharmacological therapy for PDA can be considered (Knight 2001):
treatment only when the PDA is judged to be haemodynamically‐important based on clinical or echocardiographic assessments ("symptomatic treatment"): see Herrera 2007.
treatment following diagnosis of a PDA (usually by screening echocardiography in first 24 hours after birth) but prior to the development of "left to right" shunting of blood ("targeted treatment"): see Cooke 2003; Ohlsson 2008.
treatment of all at risk infants within the first 24 hours after birth ("prophylactic treatment").
This review focusses on prophylactic treatment of PDA in preterm infants using indomethacin. Another Cochrane review examines ibuprofen prophylaxis (Shah 2006).
How the intervention might work
Prophylactic treatment aims to achieve PDA closure prior to the development of shunting and haemodynamic disturbances that are associated with morbidity and mortality but without the need for screening or surveillance using echocardiography. However, universal prophylaxis exposes a substantial proportion of infants in whom PDA closure would have occurred spontaneously to a pharmacological intervention. This is important because, as well as having potential benefits, treatment with prophylactic indomethacin may have harms related to reducing perfusion of essential organs such as reduced cerebral blood flow which may oppose any neurodevelopmental benefits due to possible reduction in the incidence of IVH (Edwards 1990); reduced gastrointestinal perfusion that potentially limits any effect of PDA closure on reducing the risk of NEC (Coombs 1990); and reduced renal perfusion, glomerular filtration and urine output causing fluid and electrolyte disturbances in the early neonatal period (Cifuentes 1979). Indomethacin may also inhibit platelet function and disrupt haemostasis that may cause clinically‐important bleeding e.g. IVH (Friedman 1978).
Why it is important to do this review
Given the uncertainty that exists about the balance between the putative benefits and harms associated with prophylactic indomethacin in preterm neonates, and the potential for this intervention to affect several major outcomes in this population, an attempt to detect, appraise, and synthesise evidence from randomised controlled trials is justified.
Objectives
To determine the effect of prophylactic indomethacin on mortality and morbidity in preterm infants.
Methods
Criteria for considering studies for this review
Types of studies
Randomised or quasi‐randomised controlled trials.
Types of participants
Preterm neonates (less than 37 weeks' completed gestation).
Types of interventions
Prophylactic (not guided by knowledge of PDA status) treatment with indomethacin given within 24 hours of birth vs. placebo or no treatment. Specific dose regimens were not pre‐specified.
Types of outcome measures
PRIMARY OUTCOMES:
All‐cause mortality prior to hospital discharge and at most recent follow‐up.
Neurodevelopment: (i) Death or severe neurodevelopmental disability defined as any one or combination of the following: non‐ambulant cerebral palsy, developmental delay (developmental quotient less than 70), auditory and visual impairment. Each component will be analysed individually as well as part of the composite outcome, (ii) Neurodevelopmental scores in survivors aged > 12 months measured using validated assessment tools, (iii) Cognitive and educational outcomes measured using validated assessment tools including school examinations.
SECONDARY OUTCOMES:
PDA: (i) symptomatic (clinical signs of heart failure as assessed by individual caregivers and/or receiving anti‐failure therapy such as diuretics, and/or receiving non‐steroidal anti‐inflammatory treatment to close a suspected or confirmed PDA), (ii) all PDA confirmed by echocardiography regardless of other clinical signs (minimum duct dimension not pre‐specified), (iii) surgical ligation or transcatheter occlusion of PDA.
IVH: (i) IVH; all grades (grades I‐IV), and (ii) severe IVH ‐ grade III (ventricles distended with blood) or IV (parenchymal involvement) (Papile 1978), (iii) other cranial ultrasound abnormalities related to IVH including post‐haemorrhagic ventricular dilatation (hydrocephalus), periventricular leukomalacia (PVL), and cystic PVL defined as cysts detected in the periventricular area on ultrasound, computerised tomography or magnetic resonance imaging.
Respiratory outcomes: (i) need for mechanical ventilation, (ii) duration of mechanical ventilation, (iii) duration of supplemental oxygen therapy, (iv) incidence of pneumothorax or pneumopericardium, (v) incidence of bronchopulmonary dysplasia (oxygen requirement beyond (a) 28 postnatal days, (b) 36 weeks' post menstrual age), (vi) pulmonary haemorrhage.
Renal outcomes: (i) anuria or severe oliguria (< 0.5 ml/kg/day), (ii) raised plasma creatinine, (iii) acute electrolyte disturbances, (iv) long term renal impairment (glomerular filtration rate less than 50% of index population mean assessed at > 12 months of age).
Gastrointestinal outcomes: (i) NEC confirmed by at least two of the following features: abdominal radiograph showing pneumatosis intestinalis or gas in the portal venous system or free air in the abdomen; abdominal distension with abdominal radiograph showing gaseous distension or frothy appearance of bowel lumen (or both); blood in stool; lethargy, hypotonia, or apnoea (or combination of these); or a diagnosis confirmed at surgery or autopsy, (ii) isolated gastrointestinal perforation, (iii) feed intolerance: days to establish full enteral feeding independently of parenteral nutrition.
Haemostasis outcomes: (i) "excessive clinical bleeding" (investigator defined) (ii) thrombocytopaenia ‐ platelet count < 50,000 per microlitre, or 'clinically important as defined by clinical investigators'.
Retinopathy of prematurity: (i) all stages, (ii) > stage 3 (ICROP 1984).
Search methods for identification of studies
We used the standard search strategy of the Cochrane Neonatal Review Group.
Electronic searches
Searches were made of the Cochrane Central Register of Controlled Trials (CENTRAL, The Cochrane Library, Issue 5, 2010), MEDLINE (1966 to April 2010), EMBASE (1980 to April 2010), and CINAHL (1982 to April 2010) using combinations of the following text words and MeSH terms: [Infant, Newborn OR Infant, Premature OR Infant, Low Birth Weight OR infan* OR neonat*] AND ["Anti‐Inflammatory Agents, Non‐Steroidal" OR indomethacin OR indometacin OR indocid OR NSAID]. The search outputs were limited with the relevant search filters for clinical trials. No language restriction was applied.
The following web sites were searched for completed or ongoing trials:
ClinicalTrials.gov
Current Controlled Trials
Searching other resources
The references in studies identified as potentially relevant were examined.
The abstracts from the meetings of the Pediatric Academic Societies (1993 to 2009), the European Society for Pediatric Research (1995 to 2009), and the Royal College of Paediatrics and Child Health (2000 to 2009) were searched.
Trials reported only as abstracts were eligible if sufficient information was available from the report, or from contact with the authors, to fulfil the inclusion criteria.
Data collection and analysis
The standard methods of the Cochrane Neonatal Review Group were used.
Selection of studies
The title and abstract of all studies identified by the above search strategy were screened and the full articles for all potentially relevant trials obtained. The full text of any potentially eligible reports was reassessed and those studies that did not meet all of the inclusion criteria were excluded. Any disagreements were discussed until consensus was achieved.
Data extraction and management
A data collection form was used to aid extraction of relevant information from each included study. Two review authors extracted the data separately. Any disagreements were discussed until consensus was achieved. If data from the trial reports were insufficient, the investigators were contacted for further information.
Assessment of risk of bias in included studies
The criteria and standard methods of the Cochrane Neonatal Review Group were used to assess the methodological quality of any included trials in terms of allocation concealment, blinding of parents or caregivers and assessors to the intervention and completeness of assessment in all randomised individuals. Additional information from the trial authors was requested to clarify methodology and results as necessary. In addition, the following issues were evaluated and entered into the Risk of Bias table:
1. Sequence generation: Was the allocation sequence adequately generated?
2. Allocation concealment: Was allocation adequately concealed?
3. Blinding of participants, personnel and outcome assessors: Was knowledge of the allocated intervention adequately prevented during the study? At study entry? At the time of outcome assessment?
4. Incomplete outcome data: Were incomplete outcome data adequately addressed?
5. Selective outcome reporting: Are reports of the study free of suggestion of selective outcome reporting?
6. Other sources of bias: Was the study apparently free of other problems that could put it at a high risk of bias?
Measures of treatment effect
Relative risk (RR) and risk difference (RD) were calculated for dichotomous data and weighted mean difference (WMD) for continuous data, with respective 95% confidence intervals (CI). The number needed to treat for benefit (NNTB) or harm (NNTH) was determined for a statistically significant difference in the RD.
Unit of analysis issues
The unit on analysis is the participating infant in individually randomised trials and the neonatal unit (or sub‐unit) for cluster randomised trials.
Assessment of heterogeneity
If more than one trial was included in a meta‐analysis, the treatment effects of individual trials and heterogeneity between trial results were to be examined by inspecting the forest plots. The I² statistic was calculated for each analysis to quantify inconsistency across studies and describe the percentage of variability in effect estimates that may be due to heterogeneity rather than sampling error. If substantial (I² > 50%) heterogeneity was detected, the possible causes (for example, differences in study design, participants, interventions, or completeness of outcome assessments) were explored in sensitivity analyses.
Data synthesis
The fixed effects model was used using RevMan 5 for meta‐analysis.
Subgroup analysis and investigation of heterogeneity
The following subgroup analyses were planned:
VLBW (less than 1500 grams) or very preterm (less than 32 weeks' gestation at birth).
ELBW (less than 1000 grams) or extremely preterm (less than 28 weeks' gestation at birth).
Results
Description of studies
Nineteen trials were found to be eligible for inclusion in this review (see table Characteristics of included studies). Overall, the quality of the trials was good, and the results were consistent across trials.
Thirty‐two additional studies were excluded (see table Characteristics of excluded studies).
Participants
The size of the trials ranged from single centre studies enrolling less than 50 infants to a large international multi‐centre study in which 1202 infants participated (TIPP 2001). Thirteen trials were conducted within North America and the others in Latin America, Europe and Asia. The large international trial included centres in North America, Australasia and Asia (TIPP 2001).
In most trials, participants were very preterm or VLBW infants receiving standard intensive care interventions such as mechanical ventilation. The largest included trial restricted participation to ELBW infants (TIPP 2001). Surfactant was given either as prophylaxis or rescue therapy in seven trials (Couser 1996; Domanico 1994; Ment 1994a; Ment 1994b; Supapannachart 1999; TIPP 2001; Yaseen 1997).
Bada 1989, Hanigan 1988, Krueger 1987, Ment 1985, Ment 1988, Ment 1994b; Morales‐Suarez 1994 and Rennie 1986a performed cranial ultrasounds before study entry and excluded infants with IVH. In Ment 1994a, participants were infants with pre‐existing grade 1 IVH. The remaining studies enrolled infants without knowledge of pre‐existing IVH.
Interventions
All the studies used prophylactic intravenous indomethacin as treatment. The dosage schedules varied from a single dose of 0.2 mg/kg at 24 hours of age to a daily dose of 0.1 mg/kg given for six days. A placebo, typically saline, was used as control in all trials apart from Krueger 1987.
Outcomes
Most trials examined short‐term clinical outcomes prior to discharge from hospital. Many of the outcome definitions varied, in particular the definition of BPD. Several studies looked at a variety of measures of renal function including urine output and renal biochemistry but there was little consistency between studies as to which measures and which cut‐off points were used. The same issue arose when examining haemostasis when the platelet count, bleeding time and "clinical bleeding" were variably used in different studies.
Data on long‐term neurodevelopmental outcomes up to 36 months corrected age were available from five trials (Bandstra 1988; Couser 1996; Ment 1994b; TIPP 2001; Vincer 1987). One trial assessed school age neurodevelopmental outcomes at eight years of age (Ment 1994b).
Risk of bias in included studies
Quality assessments are included in the table, Characteristics of included studies.
The exact method of concealment of randomisation could be determined for twelve of the included studies (Bandstra 1988; Couser 1996; Gutierrez 1987; Hanigan 1988; Mahony 1985; Ment 1985; Ment 1988; Ment 1994a; Ment 1994b; TIPP 2001; Supapannachart 1999; Yaseen 1997). Methods included telephone randomisation, sealed envelopes and coded vials. In the remaining seven studies, it has not been possible to tell how well randomisation was concealed.
Blinding of the intervention to those caring for the infant was explicitly described in nine of the studies (Bandstra 1988; Couser 1996; Domanico 1994; Gutierrez 1987; Hanigan 1988; Mahony 1985; Ment 1985; Ment 1988; Vincer 1987 and TIPP 2001). In Krueger 1987, caregivers were not blinded to the intervention group. Blinding of the intervention is unclear in Puckett 1985 and Rennie 1986a.
In three studies, it is not possible to determine whether or not those responsible for assessing the outcomes of interest were blind to intervention group (Krueger 1987; Puckett 1985; Rennie 1986a). In all the other studies, blinding was adequate.
For all short‐term outcome measures prior to discharge, follow‐up was more than 90% complete for all the trials. Long‐term outcome assessment remained impressive at > 85% in the two trials contributing most data (Ment 1994b; TIPP 2001) and even in smaller trials was still greater than 75% (Couser 1996; Vincer 1987).
Effects of interventions
PROPHYLACTIC INTRAVENOUS INDOMETHACIN VS. PLACEBO OR NO DRUG (COMPARISON 1)
PRIMARY OUTCOMES
Mortality (1.1 ‐ 1.2)
Mortality before hospital discharge (17 trials): Meta‐analysis did not detect a statistically significant effect [typical RR 0.82 (95% CI 0.65, 1.03); RD ‐0.03 (95% CI ‐0.06, 0.00): (Figure 1)]
1.

Forest plot of comparison: 1 Prophylactic indomethacin vs. control, outcome: 1.1 Death to hospital discharge.
Mortality at latest follow‐up (18 trials ‐ includesTIPP 2001): Meta‐analysis did not detect a statistically significant effect [typical RR 0.96 (95% CI 0.81, 1.12); RD ‐0.01 (95% CI ‐0.04, 0.02): (Figure 2)].
2.

Forest plot of comparison: 1 Prophylactic indomethacin vs. control, outcome: 1.2 Death at latest follow‐up.
There is no evidence of statistical heterogeneity in either of the meta‐analyses; I2= 0%.
Neurodevelopment (1.3 ‐ 1.7)
(i) Neurological assessments at 18 ‐ 36 months corrected age:
Death or severe neurodevelopmental disability (3 trials): Meta‐analysis did not detect a statistically significant effect [typical RR 1.02 (95% CI 0.90, 1.15); RD 0.01 (95% CI ‐0.04, 0.06): (Figure 3)].
3.

Forest plot of comparison: 1 Prophylactic indomethacin vs. control, outcome: 1.3 Death or severe neurosensory impairment.
Cerebral palsy (4 trials): Meta‐analysis did not detect a statistically significant effect [typical RR 1.04 (95% CI 0.77, 1.40); RD 0.00 (95% CI ‐0.03, 0.04): (Figure 4)].
4.

Forest plot of comparison: 1 Prophylactic indomethacin vs. control, outcome: 1.4 Cerebral palsy, visual impairment, hearing impairment and severe neurodevelopmental impairment.
Visual impairment (2 trials): Meta‐analysis did not detect a statistically significant effect [typical RR1.26 (95% CI 0.50, 3.18); RD 0.00 (95% CI ‐0.01, 0.02): (Figure 4)].
Hearing impairment (2 trials): Meta‐analysis did not detect a statistically significant effect [typical RR 1.02 (95% CI 0.45, 2.33); RD 0.00 (95% CI ‐0.01, 0.01): (Figure 4)].
Severe neurodevelopmental impairment (3 trials): The two trials using Bayley examinations at 24 months (TIPP 2001 and Bandstra 1988) found no difference in rates of severe impairment (Mental Developmental Index < 68‐70). Ment 1994b did not find a statistically significant difference in the WIPPSI‐R (full scale < 70) at 54 months.
Meta‐analysis of the three trials did not detect a statistically significant effect [typical RR 0.96 (95% CI 0.79, 1.17); RD ‐0.01 (95% CI ‐0.05, 0.04): (Figure 4)].
Cognitive outcomes (1 trial): Ment 1994b did not find a statistically significant difference in either Stanford‐Binet IQ scores [WMD 4.6 (95% CI ‐0.5, 9.7)] or Peabody Picture Vocabulary Test scores [WMD 4.7 (95% CI ‐0.5, 9.9) assessed at 36 months (Figure 5).
5.

Forest plot of comparison: 1 Prophylactic indomethacin vs. control, outcome: 1.10 Cognitive assessments (18‐36 months).
(ii) School‐age neurological and developmental assessments:
Ment 1994b did not detect any statistically significant effects on assessment of children aged eight years (Figure 6):
6.

Forest plot of comparison: 1 Prophylactic indomethacin vs. control, outcome: 1.6 School age neurological assessments.
Cerebral palsy: typical RR 1.24 (95% CI 0.59, 2.62); RD 0.02 (95% CI ‐0.04, 0.08).
Visual impairment: typical RR 0.13 (95% CI 0.01, 2.54); RD ‐0.02 (95% CI ‐0.05, 0.01).
Hearing impairment: typical RR 0.78 (95% CI 0.21, 2.86); RD ‐0.01 (95% CI ‐0.05, 0.03).
"Abnormal" neurological assessment: RR 1.14 (95% CI 0.59, 2.24); RD 0.01 (95% CI ‐0.05, 0.08).
Cognitive and educational outcomes: Ment 1994b did not detect statistically significant differences in the risk of scoring < 70 in Wechsler Intelligence Scale for Children ‐ Third Edition (WISC‐III) verbal IQ, performance IQ, or full‐scale IQ tests, or Peabody Individual Achievement Test‐Revised (PIAT‐R) assessments. The proportion of infants with a low Peabody Picture Vocabulary Test‐Revised (PPVT‐R) score (< 70) was statistically significantly lower in the indomethacin group: typical RR 0.54 (95% CI 0.31, 0.93); RD ‐0.09 (95% CI ‐0.17, ‐0.01); NNTB 11 (6, 100) (Figure 7).
7.

Forest plot of comparison: 1 Prophylactic indomethacin vs. control, outcome: 1.7 School age cognitive and educational outcomes.
SECONDARY OUTCOMES
Patent ductus arteriosus (Outcomes 1.8 ‐ 1.10):
All PDA, echocardiography confirmed (7 trials): Meta‐analysis found a statistically significant reduction [typical RR 0.29 (95% CI 0.22, 0.38), RD ‐0.27 (95% CI ‐0.32,‐0.21), NNTB 4 (95% CI 3, 5) (Figure 8)].
8.

Forest plot of comparison: 1 Prophylactic indomethacin vs. control, outcome: 1.12 All PDA (echo‐diagnosed, symptomatic or not).
Symptomatic PDA (14 trials): Meta‐analysis found a statistically significant reduction [typical RR 0.44 (95% CI 0.38, 0.50); RD ‐0.24 (95% CI ‐0.28, ‐0.21); NNTB 4 (95% CI 3, 5) (Figure 9)].
9.

Forest plot of comparison: 1 Prophylactic indomethacin vs. control, outcome: 1.11 Symptomatic PDA.
Surgical PDA ligation (8 trials): Meta‐analysis found a statistically significant reduction in risk [typical RR 0.51 (95% CI 0.37, 0.71), RD ‐0.05 (95% CI ‐0.08, ‐0.03), NNTB 20 (95% CI 12, 33) (Figure 10)].
10.

Forest plot of comparison: 1 Prophylactic indomethacin vs. control, outcome: 1.13 PDA ligation.
There is no evidence of statistical heterogeneity in any of the meta‐analyses; I2 = 0% ‐ 10%.
Intraventicular haemorrhage (1.11‐ 1.14)
Any IVH (14 trials): Meta‐analysis found a statistically significant reduction [typical RR 0.88 (95% CI 0.80, 0.98), RD ‐0.04 (95% CI ‐0.08, ‐0.01), NNTB 25 (95% CI 12, 100) (Figure 11)]. There is evidence that the treatment effect on this outcome is not consistent across all studies; I2 = 52%.
11.

Forest plot of comparison: 1 Prophylactic indomethacin vs. control, outcome: 1.14 All IVH.
Severe IVH ‐ grade >2 (14 trials): Meta‐analysis found a statistically significant reduction [typical RR 0.66 (95% CI 0.53, 0.82), RD ‐0.05 (95% CI ‐0.07, ‐0.02), NNTB 20 (95% CI 14, 50) (Figure 12)]. There is no evidence of statistical heterogeneity; I2 = 0%.
12.

Forest plot of comparison: 1 Prophylactic indomethacin vs. control, outcome: 1.15 Severe IVH: grades III ‐ IV.
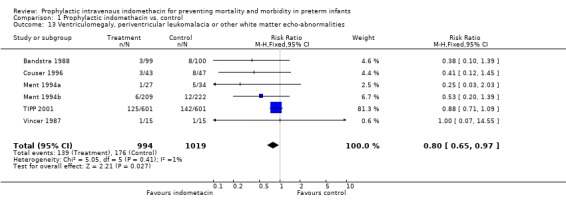
Ventriculomegaly, periventricular leukomalacia or other white matter echo‐abnormalities (6 trials): Meta‐analysis found a borderline statistically significant reduction [typical RR 0.80 (95% CI 0.65, 0.97), RD ‐0.04 (95% CI ‐0.07, 0.00), NNTB 25 (95% CI 14, infinity) (Figure 13)]. There is no evidence of statistical heterogeneity; I2 = 1%.
13.

Forest plot of comparison: 1 Prophylactic indomethacin vs. control, outcome: 1.16 Ventriculomegaly, periventricular leukomalacia or other white matter echo‐abnormalities.
IVH that progresses (2 trials): Meta‐analysis did not detect a statistically significant effect [typical RR 0.80 (95% CI 0.44, 1.47), RD ‐0.08 (95% CI ‐0.29, 0.13), (Figure 14).There is no evidence of statistical heterogeneity; I2 = 10%.
14.

Forest plot of comparison: 1 Prophylactic indomethacin vs. control, outcome: 1.17 IVH that progresses.
Respiratory outcomes (1.15 ‐ 1.20)
Duration of assisted ventilation (4 trials): Meta‐analysis did not detect a statistically significant effect [WMD ‐1.83 days (95% CI ‐5.53, 1.87) (Figure 15)].
15.

Forest plot of comparison: 1 Prophylactic indomethacin vs. control, outcome: 1.17 Duration of assisted ventilation.
Pneumothorax or pneumopericardium (6 trials): Meta‐analysis did not detect a statistically significant effect [typical RR 0.75 (95% CI 0.50, 1.13), RD ‐0.04 (95% CI ‐0.10, 0.02) (Figure 16)].
16.

Forest plot of comparison: 1 Prophylactic indomethacin vs. control, outcome: 1.18 Pneumothorax and/or pneumopericardium.
Bronchopulmonary dysplasia ‐ oxygen requirement at 28 days (9 trials): Meta‐analysis did not detect a statistically significant effect [typical RR 1.08 (95% CI 0.92, 1.26), RD 0.03 (95% CI ‐0.03, 0.08) (Figure 17)].
17.

Forest plot of comparison: 1 Prophylactic indomethacin vs. control, outcome: 1.19 Bronchopulmonary dysplasia (28 days).
Bronchopulmonary dysplasia ‐ oxygen requirement at 36 weeks' postmenstrual age (1 trial): TIPP 2001 did not detect a statistically significant effect [typical RR 1.06 (95% CI 0.92, 1.22), RD 0.03 (95% CI ‐0.04, 0.09) (Figure 18)].
18.

Forest plot of comparison: 1 Prophylactic indomethacin vs. control, outcome: 1.20 Bronchopulmonary dysplasia (36 weeks' PMA).
Duration of supplemental oxygen (4 trials): Meta‐analysis did not detect a statistically significant effect [WMD 3.76 days (95% CI ‐4.23, 11.74) (Figure 19)].
19.

Forest plot of comparison: 1 Prophylactic indomethacin vs. control, outcome: 1.21 Duration of supplementary oxygen requirement.
Pulmonary haemorrhage (4 trials): Meta‐analysis did not detect a statistically significant effect [typical RR 0.84 (95% CI 0.66, 1.07), RD ‐0.02 (95% CI ‐0.06, 0.01) (Figure 20)].
20.

Forest plot of comparison: 1 Prophylactic indomethacin vs. control, outcome: 1.22 Pulmonary haemorrhage.
There is no evidence of statistical heterogeneity in any of the meta‐analyses; I2 = 0%.
Renal outcomes (1.21 ‐ 1.22).
Oliguria/anuria (8 trials): Meta‐analysis showed a statistically significantly higher incidence in infants who receive prophylactic indomethacin [typical RR 1.90 (95% CI 1.45, 2.47), RD 0.06 (0.04, 0.08), NNTH 16 (Figure 21)].
21.

Forest plot of comparison: 1 Prophylactic indomethacin vs. control, outcome: 1.23 Oliguria/anuria.
Elevated serum creatinine (4 trials): Meta‐analysis did not detect a statistically significant difference [typical RR 1.09 (95% CI 0.47, 2.51), RD 0.00 (95% CI ‐0.03, 0.03) (Figure 22)].
22.

Forest plot of comparison: 1 Prophylactic indomethacin vs. control, outcome: 1.24 Elevated serum creatinine.
There is no evidence of statistical heterogeneity in either of these meta‐analyses; I2 = 0%.
Electrolyte disturbances (3 trials): Mahony 1985 reported no statistically significant differences in mean plasma sodium, potassium and creatinine levels on day three. Vincer 1987 reported significantly higher mean plasma sodium levels in the treatment group on days three and four. Rennie 1986a reported no significant differences in mean plasma sodium levels on days one and two following treatment. Data synthesis was not possible because of the differences in the methods of defining these outcomes.
Gastrointestinal outcomes (1.23 ‐ 1.24).
Necrotising enterocolitis (12 trials): Meta‐analysis did not detect a statistically significant difference [typical RR 1.09 (95% CI 0.82,1.46), RD 0.01 (95% CI ‐0.01, 0.03) (Figure 23)].There is no evidence of statistical heterogeneity in the meta‐analysis; I2 = 0%.
23.

Forest plot of comparison: 1 Prophylactic indomethacin vs. control, outcome: 1.26 Necrotizing enterocolitis.
Gastrointestinal perforation (1 trial): TIPP 2001 did not find a statistically significant difference [typical RR 1.12 (0.71,1.79), RD 0.01 (95% CI ‐0.02, 0.03) (Figure 24)].
24.

Forest plot of comparison: 1 Prophylactic indomethacin vs. control, outcome: 1.28 Gastointestinal perforation.
Enteral feeds intolerance: Not reported in any of the trials.
Haemostasis outcomes (1.25 ‐ 1.26)
Excessive bleeding (5 trials): Meta‐analysis did not detect a statistically significant difference [typical RR 0.74 (95% CI 0.40, 1.38), RD ‐0.01 (95% CI ‐0.02, 0.01) (Figure 25)]
25.

Forest plot of comparison: 1 Prophylactic indomethacin vs. control, outcome: 1.28 Excessive clinical bleeding.
Thrombocytopaenia (4 trials): Meta‐analysis did not detect a statistically significant difference [typical RR 0.50 (95% CI 0.11, 2.22), RD ‐0.01 (95%CI ‐0.03, 0.01) (Figure 26)].
26.

Forest plot of comparison: 1 Prophylactic indomethacin vs. control, outcome: 1.29 Thrombocytopaenia (investigator defined).
There is no evidence of statistical heterogeneity in either of the meta‐analyses; I2 = 0%.
Retinopathy of prematurity (1.27 ‐ 1.28)
Any ROP (5 trials): Meta‐analysis did not detect a statistically significant difference [typical RR 1.02 (95% CI 0.92, 1.12) (Figure 27)]
27.

Forest plot of comparison: 1 Prophylactic indomethacin vs. control, outcome: 1.30 Any retinopathy of prematurity.
Severe ROP (2 trials): Meta‐analysis did not detect a statistically significant difference [typical RR 1.75 (95% CI 0.92, 3.34) (Figure 28)].
28.

Forest plot of comparison: 1 Prophylactic indomethacin vs. control, outcome: 1.31 Severe retinopathy of prematurity (stage 3 or more).
There is no evidence of statistical heterogeneity in either of the meta‐analyses; I2= 0% ‐ 8%.
SUBGROUP ANALYSES
1. Very preterm or VLBW infants: Most trials restricted participation to VLBW infants. Only four small trials allowed infants of higher birth weight (< 1750 grams) to participate. Subgroup analysis excluding only the small number of infants with birth weight 1500 to 1750 grams was not possible.
2. Extremely preterm or ELBW infants: The largest single trial restricted participation to ELBW infants (TIPP 2001). The other trials had upper birth weight bounds between 1250 and 1500 grams (and up to 1750 grams in four small trials). Subgroup analysis of only ELBW infants was not possible for these trials.
Forest plot inspection comparing effect size estimates of TIPP 2001 alone versus the pooled effect sizes of the meta‐analyses did not generally reveal major differences in direction or size of effects apart from for the following outcomes related to IVH:
Any IVH (Figure 11): Meta‐analysis (14 trials) found a statistically significant reduction: typical RR 0.88 (95% CI 0.80, 0.98), RD ‐0.04 (95% CI ‐0.08, ‐0.01), NNTB 25 (95% CI 12, 100). In comparison, TIPP 2001 did not detect a statistically significant difference: RR 1.01 (95% CI 0.88, 1.16), RD 0.00 (95% CI ‐0.05, 0.06).
Ventriculomegaly, periventricular leukomalacia or other white matter echo‐abnormalities (Figure 13): Meta‐analysis (6 trials) found a borderline statistically significant reduction: typical RR 0.80 (95% CI 0.65, 0.97), RD ‐0.04 (95% CI ‐0.07, 0.00) NNTB 25 (95% CI 14, infinity). In comparison, TIPP 2001 did not detect a statistically significant difference: RR 0.88 (95% CI 0.71, 1.09), RD ‐0.03 (95% CI ‐0.08, 0.02).
Discussion
Summary of main results
This systematic review of 19 randomised controlled trials in which more than 2800 preterm infants participated found evidence that prophylactic indomethacin does not have a substantial effect on mortality or neurodevelopmental outcomes. The homogeneity in the meta‐analyses and the narrow confidence intervals around the estimates of effect suggest that small but potentially important effects are unlikely to exist and that further trials of this intervention are not a research priority.
With regard to secondary outcomes, the available evidence indicates that prophylactic administration of indomethacin has short term benefits including a reduction in the incidence of symptomatic PDA, the need for surgical PDA closure, and the incidence of severe IVH. Safety concerns have largely been allayed. The available data indicate that any indomethacin‐associated renal impairment is transient and there is no evidence that prophylactic indomethacin affects the risk of NEC or clinically‐important bleeding.
Overall completeness and applicability of evidence
The trials were generally of good methodological quality and the effect size estimates consistent between trials suggesting that the meta‐analyses were valid. The participants in the included trials reflect the population for which this intervention is currently considered, that is VLBW and particularly ELBW infants. On post hoc inspection of forest plots, the findings appear consistent across trials conducted before surfactant replacement and antenatal corticosteroid therapy were established as standards of care compared with trials undertaken during the later 1990s.
Potential biases in the review process
Most of the trials included in the review were relatively small. Two large multi‐centre studies contributed about 60% of the total number of participants (Ment 1994b; TIPP 2001). There is some variation in study design, particularly with regard to birth weight eligibility criteria and the indomethacin dosage regimens used but the meta‐analyses did not reveal statistical heterogeneity. The validity of the long term assessment data is enhanced by the impressive completeness of follow‐up in the largest trials. TIPP 2001 provided data on more than 95% of survivors at 18 months and showed no statistically significant differences in a variety of neurodevelopmental outcomes. Longer term assessments have not been performed in TIPP 2001 and some caution should perhaps be exercised in applying these findings at 18 months since it has been suggested that assessments done at a relatively young age may be insufficiently predictive of longer term neurodevelopmental outcomes, particularly with regard to cognitive functioning (Roberts 2009). However, Ment 1994b provided data on 85% of survivors at eight years and also failed to detect any statistically significant differences in a range of neurodevelopmental outcomes including educational and cognitive performance.
Authors' conclusions
Implications for practice.
Given the lack of evidence of effect on long term outcomes, the decision to use prophylactic indomethacin will depend on the values that families and clinicians attach to the short term benefits. In neonatal units without ready access to cardiac diagnostic and therapeutic services, a reduction in symptomatic PDA and a reduction in the need for surgical closure may be considered a greater benefit than in other units with ready access to these services. Cost implications may need to be considered although economic evaluation of this intervention has been limited to date (TIPP 2001).
Implications for research.
Further randomised controlled trials of prophylactic indomethacin versus placebo are unlikely to be considered a research priority. Exploring and evaluating parental perceptions and concerns regarding the use of prophylactic indomethacin may help guide policy and practice development. Although data are available on long term neurodevelopmental outcomes at the age of 18 months to five years in many children and at eight years in a smaller cohort, continuing follow‐up of these children would be justified as more subtle differences in later childhood and adulthood may become apparent (Roberts 2009).
What's new
| Date | Event | Description |
|---|---|---|
| 20 May 2010 | New search has been performed | This updates the review "Prophylactic intravenous indomethacin for preventing mortality and morbidity in preterm infants" published in the Cochrane Database of Systematic Reviews (Fowlie 2002). No new trials were identified in updated search May 2010. School‐age outcomes data from Ment 1994b have been included in this update. |
| 20 May 2010 | New citation required but conclusions have not changed | New co‐author William McGuire. |
History
Protocol first published: Issue 3, 1997 Review first published: Issue 3, 1997
| Date | Event | Description |
|---|---|---|
| 3 November 2008 | Amended | Converted to new review format. |
| 26 April 2002 | New citation required and conclusions have changed | Substantive amendment An initial literature search (English only) was undertaken in October 1994 in three databases: MEDLINE at NLM (1980 ‐ September 1994); EMBASE (1974 ‐ 1994) in DIALOG; and the Oxford Database of Perinatal Trials (ODPT) (Version 1.3, Disk issue 7, Spring 1992). A search by first author of any abstracts was done in the Science Citation Index to try and identify any corresponding full manuscripts published. None were identified. The literature search was updated in February 1997 by assessing a trials list supplied by the Cochrane Collaboration Neonatal Review Group and by searching in MEDLINE (September 1994 ‐ January 1997) using a similar strategy to the original search. EMBASE was not searched again as the original search in this database failed to identify any appropriate trials not identified by searching MEDLINE. The search was updated a third time in October 2001, searching in MEDLINE ["indomethacin AND infant AND (prophylactic OR prophylaxis OR prevention)"], and the Cochrane Controlled Trials Register, The Cochrane Library, Issue 3, 2001 ["indomethacin AND (infant OR newborn)"]. |
Acknowledgements
The Cochrane Neonatal Review Group has been funded in part with Federal funds from the Eunice Kennedy Shriver National Institute of Child Health and Human Development National Institutes of Health, Department of Health and Human Services, USA, under Contract No. HHSN267200603418C.
Data and analyses
Comparison 1. Prophylactic indomethacin vs. control.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Death to hospital discharge | 17 | 1567 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.82 [0.65, 1.03] |
| 2 Death at latest follow‐up | 18 | 2769 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.96 [0.81, 1.12] |
| 3 Death or severe neurosensory impairment | 3 | 1491 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.90, 1.15] |
| 4 Neurological assessments (18‐54 months) | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 4.1 Cerebral palsy | 4 | 1372 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.04 [0.77, 1.40] |
| 4.2 Visual impairment | 2 | 1274 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.26 [0.50, 3.18] |
| 4.3 Hearing impairment | 2 | 1259 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.45, 2.33] |
| 4.4 Severe neurodevelopmental impairment | 3 | 1286 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.96 [0.79, 1.17] |
| 5 Cognitive assessments (18‐36 months) | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 5.1 Stanford‐Binet IQ score | 1 | 233 | Mean Difference (IV, Fixed, 95% CI) | 4.60 [‐0.51, 9.71] |
| 5.2 Peabody Picture Vocabulary Test scores | 1 | 233 | Mean Difference (IV, Fixed, 95% CI) | 4.70 [‐0.54, 9.94] |
| 6 School age neurological assessments | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 6.1 Cerebral palsy aged 8 years | 1 | 304 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.24 [0.59, 2.62] |
| 6.2 Blind (receipt of services) aged 8 years | 1 | 306 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.13 [0.01, 2.54] |
| 6.3 Hearing impairment (requiring amplification) aged 8 years | 1 | 295 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.78 [0.21, 2.86] |
| 6.4 Abnormal neurological examination aged 8 years | 1 | 305 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.14 [0.59, 2.24] |
| 7 School age cognitive and educational outcomes | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 7.1 WISC‐III verbal IQ (<70) | 1 | 328 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.92 [0.46, 1.85] |
| 7.2 WISC‐III performance IQ (<70) | 1 | 328 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.99 [0.58, 1.69] |
| 7.3 WISC‐III full‐scale IQ (<70) | 1 | 328 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.16 [0.63, 2.14] |
| 7.4 PPVT‐R (<70) | 1 | 321 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.54 [0.31, 0.93] |
| 7.5 PIAT‐R reading recognition (<70) | 1 | 314 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.84 [0.39, 1.81] |
| 7.6 PIAT‐R reading comprehension (<70) | 1 | 315 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.52, 1.70] |
| 7.7 PIAT‐R mathematics (<70) | 1 | 313 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.56, 1.48] |
| 8 All PDA (echo‐diagnosed, symptomatic or not) | 7 | 965 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.29 [0.22, 0.38] |
| 9 Symptomatic PDA | 14 | 2193 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.44 [0.38, 0.50] |
| 10 PDA ligation | 8 | 1791 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.51 [0.37, 0.71] |
| 11 All IVH | 14 | 2532 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.80, 0.98] |
| 12 Severe IVH (grades III ‐ IV) | 14 | 2588 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.66 [0.53, 0.82] |
| 13 Ventriculomegaly, periventricular leukomalacia or other white matter echo‐abnormalities | 6 | 2013 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.80 [0.65, 0.97] |
| 14 IVH that progresses | 2 | 83 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.80 [0.44, 1.47] |
| 15 Duration of assisted ventilation | 4 | 417 | Mean Difference (IV, Fixed, 95% CI) | ‐1.83 [‐5.53, 1.87] |
| 16 Pneumothorax and pneumopericardium | 6 | 524 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.75 [0.50, 1.13] |
| 17 Bronchopulmonary dysplasia (28 days) | 9 | 1022 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.08 [0.92, 1.26] |
| 18 Bronchopulmonary dysplasia (36 weeks' PMA) | 1 | 999 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.06 [0.92, 1.22] |
| 19 Duration of supplementary oxygen requirement | 4 | 342 | Mean Difference (IV, Fixed, 95% CI) | 3.76 [‐4.23, 11.74] |
| 20 Pulmonary haemorrhage | 4 | 1591 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.84 [0.66, 1.07] |
| 21 Oliguria/anuria | 8 | 2115 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.90 [1.45, 2.47] |
| 22 Elevated serum creatinine | 4 | 618 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.09 [0.47, 2.51] |
| 23 Necrotising enterocolitis | 12 | 2401 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.09 [0.82, 1.46] |
| 24 Gastointestinal perforation | 1 | 1202 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.13 [0.71, 1.79] |
| 25 Excessive clinical bleeding (investigator defined) | 5 | 1776 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.74 [0.40, 1.38] |
| 26 Thrombocytopaenia (investigator defined) | 4 | 618 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.50 [0.11, 2.22] |
| 27 Any retinopathy of prematurity | 5 | 1571 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.92, 1.12] |
| 28 Severe retinopathy of prematurity (stage 3 or more) | 2 | 289 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.75 [0.92, 3.34] |
1.1. Analysis.

Comparison 1 Prophylactic indomethacin vs. control, Outcome 1 Death to hospital discharge.
1.2. Analysis.

Comparison 1 Prophylactic indomethacin vs. control, Outcome 2 Death at latest follow‐up.
1.3. Analysis.

Comparison 1 Prophylactic indomethacin vs. control, Outcome 3 Death or severe neurosensory impairment.
1.4. Analysis.

Comparison 1 Prophylactic indomethacin vs. control, Outcome 4 Neurological assessments (18‐54 months).
1.5. Analysis.

Comparison 1 Prophylactic indomethacin vs. control, Outcome 5 Cognitive assessments (18‐36 months).
1.6. Analysis.

Comparison 1 Prophylactic indomethacin vs. control, Outcome 6 School age neurological assessments.
1.7. Analysis.

Comparison 1 Prophylactic indomethacin vs. control, Outcome 7 School age cognitive and educational outcomes.
1.8. Analysis.

Comparison 1 Prophylactic indomethacin vs. control, Outcome 8 All PDA (echo‐diagnosed, symptomatic or not).
1.9. Analysis.

Comparison 1 Prophylactic indomethacin vs. control, Outcome 9 Symptomatic PDA.
1.10. Analysis.

Comparison 1 Prophylactic indomethacin vs. control, Outcome 10 PDA ligation.
1.11. Analysis.

Comparison 1 Prophylactic indomethacin vs. control, Outcome 11 All IVH.
1.12. Analysis.

Comparison 1 Prophylactic indomethacin vs. control, Outcome 12 Severe IVH (grades III ‐ IV).
1.13. Analysis.
Comparison 1 Prophylactic indomethacin vs. control, Outcome 13 Ventriculomegaly, periventricular leukomalacia or other white matter echo‐abnormalities.
1.14. Analysis.

Comparison 1 Prophylactic indomethacin vs. control, Outcome 14 IVH that progresses.
1.15. Analysis.

Comparison 1 Prophylactic indomethacin vs. control, Outcome 15 Duration of assisted ventilation.
1.16. Analysis.

Comparison 1 Prophylactic indomethacin vs. control, Outcome 16 Pneumothorax and pneumopericardium.
1.17. Analysis.

Comparison 1 Prophylactic indomethacin vs. control, Outcome 17 Bronchopulmonary dysplasia (28 days).
1.18. Analysis.

Comparison 1 Prophylactic indomethacin vs. control, Outcome 18 Bronchopulmonary dysplasia (36 weeks' PMA).
1.19. Analysis.

Comparison 1 Prophylactic indomethacin vs. control, Outcome 19 Duration of supplementary oxygen requirement.
1.20. Analysis.

Comparison 1 Prophylactic indomethacin vs. control, Outcome 20 Pulmonary haemorrhage.
1.21. Analysis.

Comparison 1 Prophylactic indomethacin vs. control, Outcome 21 Oliguria/anuria.
1.22. Analysis.

Comparison 1 Prophylactic indomethacin vs. control, Outcome 22 Elevated serum creatinine.
1.23. Analysis.

Comparison 1 Prophylactic indomethacin vs. control, Outcome 23 Necrotising enterocolitis.
1.24. Analysis.

Comparison 1 Prophylactic indomethacin vs. control, Outcome 24 Gastointestinal perforation.
1.25. Analysis.

Comparison 1 Prophylactic indomethacin vs. control, Outcome 25 Excessive clinical bleeding (investigator defined).
1.26. Analysis.

Comparison 1 Prophylactic indomethacin vs. control, Outcome 26 Thrombocytopaenia (investigator defined).
1.27. Analysis.

Comparison 1 Prophylactic indomethacin vs. control, Outcome 27 Any retinopathy of prematurity.
1.28. Analysis.

Comparison 1 Prophylactic indomethacin vs. control, Outcome 28 Severe retinopathy of prematurity (stage 3 or more).
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Bada 1989.
| Methods | Blinding of randomisation: can't tell Blinding of intervention: yes Blinding of outcome measurement: yes Complete (> 90%) follow‐up: yes | |
| Participants | 141 VLBW infants. Excluded: IVH > grade 2. |
|
| Interventions | Indomethacin (3 iv doses ‐ 0.2; 0.1; 0.1 mg/kg); first dose at 6 hours of age, then 12 hourly thereafter versus placebo (not described). | |
| Outcomes | Death before hospital discharge IVH BPD (oxygen supplementation beyond 28 days) Pulmonary haemorrhage (blood up tube, consistent radiological findings, ventilation required) NEC (Bell stage 2 or 3 disease) Renal dysfunction (low urine output, elevated creatinine and urea) | |
| Notes | Published in abstract form only. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Blinding? All outcomes | Low risk | Blinding of intervention ‐ yes Blinding of outcome measurement(s) ‐ yes |
| Incomplete outcome data addressed? All outcomes | Low risk | Complete (> 90%) follow‐up ‐ yes |
Bandstra 1988.
| Methods | Blinding of randomisation: yes Blinding of intervention: yes Blinding of outcome measurement: yes Complete (> 90%) follow‐up: Short term outcomes ‐ yes; Long‐term neurodevelopmental outcomes ‐ no (76%). | |
| Participants | 199 infants with birthweight <1300 grams. No cranial ultrasound screening before study entry. |
|
| Interventions | Indomethacin (3 iv doses ‐ 0.2; 0.1; 0.1 mg/kg), first dose at less than 12 hours of age, 12 hourly thereafter vs. an equal volume of saline placebo. | |
| Outcomes | Death before hospital discharge and death (up to 24 months) IVH Clinically significant PDA; PDA ligation Duration of supplemental oxygen Duration of ventilation Chronic lung disease Pneumothorax Episodes of sepsis NEC ROP: any and severe Renal function (oliguria < 1 ml/kg/hour) IVH grade II ‐ IV; PVL; Long‐term outcome assessed as the latest of 6, 12, 18, 24 months visits (numbers not specified). Bayley Mental Development Index (MDI) ‐ Abnormal < 68; Bayley Physical Developmental Index (PDI) ‐ Abnormal < 68; Death or neurosensory impairment (death or Bayley MDI <68); Heamostasis ‐ bleeding time and platelet count | |
| Notes | Data on 149 infants available for long‐term follow‐up. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | Adequate |
| Blinding? All outcomes | Low risk | Blinding of intervention ‐ yes Blinding of outcome measurement(s) ‐ yes |
| Incomplete outcome data addressed? All outcomes | Low risk | Complete (> 90%) follow‐up: yes |
Couser 1996.
| Methods | Blinding of randomisation: yes Blinding of intervention: yes Blinding of outcome measurement: yes Complete (> 90%) follow‐up: yes for short term outcomes but 77% for long term outcomes. | |
| Participants | 90 (of 93 randomised) newborn infants 23 ‐ 29 weeks gestation, birth weight 600 ‐ 1250 grams. No cranial ultrasound screening before study entry. All infants received prophylactic surfactant at initial resuscitation. Follow‐up data available on 68 of 88 surviving infants. | |
| Interventions | Indomethacin vs. normal saline placebo. Indomethacin dosage: 0.1 mg/kg, within 24 hours of birth followed by same dose every 24 hours thereafter for a total of 6 doses. | |
| Outcomes | Neurodevelopmental impairment including cerebral palsy at 36 months corrected age Clinically significant PDA IVH grade 3 or 4 Mortality Duration of supplementary oxygen requirement NEC ROP stage 3 Chronic lung disease (supplementary oxygen at 28 days plus chest Xray changes) Urine output reduced to < 1.0 ml/kg/hour at any time during first 7 days | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Adequate |
| Allocation concealment? | Low risk | Adequate (pharmacy prepared vials) |
| Blinding? All outcomes | Low risk | Blinding of intervention ‐ yes Blinding of outcome measurement(s) ‐ yes |
| Incomplete outcome data addressed? All outcomes | Low risk | Complete (> 90%) follow‐up: yes |
Domanico 1994.
| Methods | Blinding of randomisation: can't tell Blinding of intervention: yes Blinding of outcome measurement: Yes Complete (> 90%) follow‐up: yes | |
| Participants | 100 preterm infants, birth weight < 1250 grams | |
| Interventions | Indomethacin vs. equal volume of placebo (saline). Indomethacin dosage: 3 doses 0.2, 0.1, 0.1 mg/kg; first dose < 12 hours, second dose 12 hours later, final dose 36 hours after first dose | |
| Outcomes | PDA (Diagnosed by echocardiography on day 3‐5) Pulmonary haemorrhage IVH grade 3 or 4 Incomplete data on duration of ventilation and duration of supplementary oxygen requirement | |
| Notes | Published in abstract form only. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Blinding? All outcomes | Low risk | Blinding of intervention ‐ yes Blinding of outcome measurement(s) ‐ yes |
| Incomplete outcome data addressed? All outcomes | Low risk | Complete (> 90%) follow‐up: yes |
Gutierrez 1987.
| Methods | Blinding of randomisation: yes Blinding of intervention: yes Blinding of outcome measurement: yes Complete (>90%) follow‐up: yes | |
| Participants | 59 newborn infants less than 34 weeks gestation and less than 1751 grams birth weight | |
| Interventions | IV indomethacin vs. placebo (saline). Indomethacin dosage: 3 doses, 0.2, 0.1, 0.1 mg/kg first dose less than 24 hours of age, then 12 hourly thereafter | |
| Outcomes | Death Symptomatic PDA (Cabal‐Siassi score > 3) | |
| Notes | Details were obtained from the trial registration with the Oxford Database of Perinatal Trials. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Adequate |
| Allocation concealment? | Low risk | Adequate (sealed envelopes) |
| Blinding? All outcomes | Low risk | Blinding of intervention ‐ yes Blinding of outcome measurement(s) ‐ yes |
| Incomplete outcome data addressed? All outcomes | Low risk | Complete (> 90%) follow‐up: yes |
Hanigan 1988.
| Methods | Blinding of randomisation: yes Blinding of intervention: yes Blinding of outcome measurement: yes Complete (> 90%) follow‐up: yes | |
| Participants | 111 VLBW infants. All had normal cranial ultrasound examination before study entry. |
|
| Interventions | IV prophylactic indomethacin versus saline placebo. Dose of study drug given before 12 hours of age and then at 24, 48 and 72 hours of age. Indomethacin dosage: 0.1 mg/kg. | |
| Outcomes | Death IVH (Krishnamoorthy classification) PDA Duration of ventilation Pneumothorax | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Adequate |
| Allocation concealment? | Low risk | Adequate (sealed envelopes) |
| Blinding? All outcomes | Low risk | Blinding of intervention ‐ yes Blinding of outcome measurement(s) ‐ yes |
| Incomplete outcome data addressed? All outcomes | Low risk | Complete (> 90%) follow‐up: yes |
Krueger 1987.
| Methods | Blinding of randomisation: can't tell Blinding of intervention: no Blinding of outcome measurement: no Complete (> 90%) follow‐up: yes | |
| Participants | 32 VLBW infants who were ventilator dependent at 24 hours of age with a diagnosis of RDS. Excluded infants with US or clinical evidence of IVH. |
|
| Interventions | IV prophylactic indomethacin, single dose (0.2 mg/kg) at 24 hours of age versus nothing (no placebo used). | |
| Outcomes | Death Symptomatic PDA IVH Duration of ventilation Chronic lung disease NEC Renal insufficiency (Input/output ratio in fixed time period following treatment ‐ 0‐24 hour & 25 ‐ 48 hours; serum creatinine) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Blinding? All outcomes | High risk | Blinding of intervention ‐ no Blinding of outcome measurement(s) ‐ no |
| Incomplete outcome data addressed? All outcomes | Low risk | Complete (> 90%) follow‐up: yes |
Mahony 1985.
| Methods | Blinding of randomisation: yes Blinding of intervention: yes Blinding of outcome measurement: yes Complete (> 90%) follow‐up: yes | |
| Participants | 110 infants, birthweight <1300 grams | |
| Interventions | IV prophylactic indomethacin, 3 doses (0.2, 0.1, 0.1 mg/kg), first dose at 12 ‐18 hours of age, second dose 12 hours after the first and third dose 24 hours after the second versus placebo (unspecified) | |
| Outcomes | Mortality Symptomatic PDA and all PDA IVH Duration of oxygen dependence Duration of mechanical endotracheal ventilation Incidence of sepsis Incidence of NEC Incidence of ROP Parameters of renal function (serum creatinine and electrolytes) | |
| Notes | Six early deaths (3 in each group) which were not included in the denominators of any study outcome in the original article have been included for the purposes of this review. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Adequate |
| Allocation concealment? | Low risk | Adequate |
| Blinding? All outcomes | Low risk | Blinding of intervention ‐ yes Blinding of outcome measurement(s) ‐ yes |
| Incomplete outcome data addressed? All outcomes | Low risk | Complete (> 90%) follow‐up: yes |
Ment 1985.
| Methods | Blinding of randomisation: yes Blinding of intervention: yes Blinding of outcome measurement: yes Complete (> 90%) follow‐up: yes | |
| Participants | 48 newborn infants, birthweight < 1250 grams. Excluded any IVH on pre‐study ultrasound examination. |
|
| Interventions | Indomethacin, 5 doses (0.2; 0.1 x 4 mg/kg), first dose at 6 hours, then 12 hourly thereafter versus saline placebo. Study medication stopped if IVH detected, abnormal bleeding, thrombocytopaenia, elevated plasma urea, or urine output <0.5 ml/kg/hr. | |
| Outcomes | Mortality IVH All PDA Parameters of renal function; urine output and serum electrolytes Parameters of haemostasis; platelet abnormalities and bleeding problems | |
| Notes | Dosage schedule changed to 0.1 mg/kg x 5 in trial after concern expressed at diminished urine output in infants receiving indomethacin. On the advice of an advisory committee "the study was terminated when statistical significance was achieved". | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Adequate |
| Allocation concealment? | Low risk | Adequate |
| Blinding? All outcomes | Low risk | Blinding of intervention ‐ yes Blinding of outcome measurement(s) ‐ yes |
| Incomplete outcome data addressed? All outcomes | Low risk | Complete (> 90%) follow‐up: yes |
Ment 1988.
| Methods | Blinding of randomisation: yes Blinding of intervention: yes Blinding of outcome measurement: yes Complete (> 90%) follow‐up: yes | |
| Participants | 36 newborn infants, birthweight < 1250 grams. Excluded infant with IVH on pre‐study ultrasound examination. |
|
| Interventions | Indomethacin versus saline placebo. Indomethacin dosage: 3 doses (3 x 0.1 mg/kg), first dose 6 ‐ 12 hours of age, 24 hourly thereafter. Study medication stopped if IVH detected, abnormal bleeding, thrombocytopaenia, elevated plasma urea, or urine output <0.5 ml/kg/hr. | |
| Outcomes | Death IVH PDA Renal function (electrolyte abnormality, urine output) Haemostasis (Platelet count, clinical bleeding) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Adequate |
| Allocation concealment? | Low risk | Adequate |
| Blinding? All outcomes | Low risk | Blinding of intervention ‐ yes Blinding of outcome measurement(s) ‐ yes |
| Incomplete outcome data addressed? All outcomes | Low risk | Complete (> 90%) follow‐up: yes |
Ment 1994a.
| Methods | Blinding of randomisation: yes Blinding of intervention: yes Blinding of outcome measurement: yes Complete (> 90%) follow‐up: yes | |
| Participants | 61 newborn infants all with non‐severe IVH (grade 1) at time of enrolment. Birthweight < 1250 grams | |
| Interventions | Indomethacin versus saline placebo. Indomethacin dosage: 3 doses (3 x 0.1 mg/kg), first dose at 6 ‐ 12 hours of age, 24 hourly thereafter | |
| Outcomes | Death Extension of IVH Closure of PDA NEC Renal function (urine output < 0.5 ml/kg/hour, serum creatinine > 159 micromol/L) Haemostasis (platelet count <50000/mm, clinical bleeding) |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Adequate |
| Allocation concealment? | Low risk | Adequate |
| Blinding? All outcomes | Low risk | Blinding of intervention ‐ yes Blinding of outcome measurement(s) ‐ yes |
| Incomplete outcome data addressed? All outcomes | Low risk | Complete (> 90%) follow‐up ‐ yes for in hospital outcomes, no for longer term neurodevelopmental outcomes |
Ment 1994b.
| Methods | Blinding of randomisation: yes Blinding of intervention: yes Blinding of outcome measurement: yes Complete (> 90%) follow‐up: Outcomes prior to hospital discharge ‐ yes; long‐term neurodevelopmental outcomes ‐ no. | |
| Participants | 431 newborn infants, birthweight < 1250 grams. Excluded infants with any IVH on pre‐study cranial ultrasound. | |
| Interventions | IV prophylactic indomethacin versus saline placebo. Indomethacin dosage: 3 doses (3 x 0.1 mg/kg), first dose at 6 ‐ 12 hours of age, 24 hourly thereafter by slow infusion (5 ‐ 10 minutes) | |
| Outcomes | Death IVH PDA NEC Renal impairment (serum creatinine > 1.8 mg/dL) Impaired haemostasis (platelet count < 50000/mm, clinical bleeding) Stanford‐Binet Intelligence Scale Peabody Picture Vocabulary Test‐ Revised Cerebral palsy on clinical examination ‐ spastic diplegia, tetraplegia, hemiplegia Blindness (not further defined) Deafness (not further defined) | |
| Notes | 431 infants were randomised. 45 died before hospital discharge and their group of allocation is known. At 36 months follow‐up, 343 (89% of survivors) were assessed for the presence or absence of cerebral palsy. Fewer were formally assessed for hearing impairment (135) and visual impairment (158). 251 infants underwent objective cognitive function testing. Cognitive function testing was limited to children who spoke English as their first and only language because of concerns that the instruments used were not valid in non‐English speaking or multilingual children. The proportions of survivors who were tested for cognitive function at follow‐up were similar for the indomethacin and placebo groups. However, no data were provided on those children not assessed. At 54‐months follow‐up, vision and hearing were assessed in 337 infants, presence or absence of cerebral palsy in 323 and cognitive testing in 233. For the purposes of this review, we used the 54‐month outcomes for vision and hearing and the 36‐month outcome for cerebral palsy to minimise loss to follow‐up. Follow‐up neurodevelopmental and/or educational outcomes assessments at aged 8 years were reported for 328 of 384 surviving children (85%). |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Adequate |
| Allocation concealment? | Low risk | Adequate |
| Blinding? All outcomes | Low risk | Blinding of intervention ‐ yes Blinding of outcome measurement(s) ‐ yes |
| Incomplete outcome data addressed? All outcomes | Low risk | Complete (> 90%) follow‐up ‐ yes for in hospital outcomes, no for longer term neurodevelopmental outcomes |
Morales‐Suarez 1994.
| Methods | Blinding of randomisation: can't tell Blinding of intervention: yes Complete follow‐up: yes Blind outcome assessment: yes | |
| Participants | 80 preterm infants with gestational ages between 28 and 36 weeks, intubated in the delivery room and requiring ventilation in ICU. Excluded those with IVH on admission US, platelet count < 50,000, oliguria and pneumothorax | |
| Interventions | IV prophylactic indomethacin 0.1 mg/kg in first 12 hours then 2 further doses 12 hours apart versus equal volume of normal saline placebo. | |
| Outcomes | Death to hospital discharge IVH ‐ all and severe Symptomatic PDA Pneumothorax |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Blinding? All outcomes | Low risk | Blinding of intervention ‐ yes Blinding of outcome measurement(s) ‐ yes |
| Incomplete outcome data addressed? All outcomes | Low risk | Complete follow‐up: yes |
Puckett 1985.
| Methods | Blinding of randomisation: can't tell Blinding of intervention: can't tell Blinding of outcome measurement: can't tell Complete (> 90%) follow‐up: no | |
| Participants | 32 newborn infants, birthweight < 1400 grams | |
| Interventions | Indomethacin vs. placebo (unspecified). Indomethacin dosage: 3 doses (3 x 0.2 mg/kg), first dose at less than 24 hours, 12 hourly thereafter | |
| Outcomes | Death PDA IVH Duration of mechanical ventilation Duration of supplemental oxygen requirement | |
| Notes | Details of this study are available in abstract only. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Blinding? All outcomes | Unclear risk | Blinding of intervention ‐ unclear Blinding of outcome measurement(s) ‐ unclear |
| Incomplete outcome data addressed? All outcomes | High risk | Complete follow‐up: no |
Rennie 1986a.
| Methods | Blinding of randomisation: can't tell Blinding of intervention: can't tell Blinding of outcome measurement: can't tell. Complete (> 90%) follow‐up: yes | |
| Participants | 50 newborn infants, birthweight < 1750 grams. Excluded infants with IVH on pre‐study US. | |
| Interventions | Indomethacin versus an equal volume of saline placebo. Indomethacin dosage: 3 doses (3 x 0.2 mg/kg), first dose at less than 24 hours, 24 hourly thereafter | |
| Outcomes | Death Clinical PDA requiring treatment IVH Duration of ventilation Duration of oxygen supplementation Chronic lung disease Pneumothorax Renal impairment (peak serum creatinine, "renal impairment", serum sodium on days 1 and 2) Impaired haemostasis ("GI bleed", bleeding time) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Blinding? All outcomes | Unclear risk | Blinding of intervention ‐ unclear
Blinding of outcome measurement(s) ‐ unclear (one member of nursing staff prepared study drug vials) |
| Incomplete outcome data addressed? All outcomes | Low risk | Complete (> 90%) follow‐up: yes |
Supapannachart 1999.
| Methods | Blinding of randomisation: yes (sealed envelopes) Blinding of intervention: yes Complete follow‐up: yes Blind outcome assessment: yes. | |
| Participants | 30 newborn infants with birth weights < 1250g and <24 hours old. Excluded: thrombocytopenia, elevated creatinine, overt bleeding, poor urine output and major congenital anomalies. | |
| Interventions | IV prophylactic indomethacin 0.2 mg/kg initially, then 0.1 mg/kg x 2 doses, 12 hours apart versus an equal volume of saline placebo. | |
| Outcomes | Death Symptomatic PDA PDA ligation BPD IVH: all and severe NEC Diminished urine output Any ROP |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Adequate |
| Allocation concealment? | Low risk | Adequate |
| Blinding? All outcomes | Low risk | Blinding of intervention ‐ yes Blinding of outcome measurement(s) ‐ yes |
| Incomplete outcome data addressed? All outcomes | Low risk | Complete (> 90%) follow‐up: yes |
TIPP 2001.
| Methods | Blinding of randomisation: yes Blinding of intervention: yes Blind outcome assessment: yes Complete follow‐up (>90%): yes | |
| Participants | 1202 ELBW infants, birthweight 500‐999 grams between 2 and 6 hours of age. Excluded known cardiac or renal disease, dysmorphic features, platelet count < 50,000/ml, maternal indomethacin therapy or overt bleeding. No screening for IVH before study entry. | |
| Interventions | Indomethacin versus an equal volume of normal saline placebo (both masked using yellow tape). Indomethacin dose: 0.1 mg/kg every 24 hours for 3 doses starting between 2 and 6 hours of age. | |
| Outcomes | Death PDA PDA ligation BPD (36 weeks) IVH White matter injury on cranial ultrasound Bayley Mental Developmental Index Blindness Deafness Cerebral palsy Death or major impairment NEC and gastrointestinal perforation Diminished urine output Excessive clinical bleeding Pulmonary haemorrhage ROP (any and grade 3 or worse) | |
| Notes | Follow‐up outcomes assessed at 18 months. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Adequate |
| Allocation concealment? | Low risk | Adequate |
| Blinding? All outcomes | Low risk | Blinding of intervention ‐ yes Blinding of outcome measurement(s) ‐ yes |
| Incomplete outcome data addressed? All outcomes | Low risk | Complete follow‐up (>90%): yes |
Vincer 1987.
| Methods | Blinding of randomisation: can't tell Blinding of intervention: yes Blinding of outcome measurement: yes Complete (> 90%) follow‐up: yes | |
| Participants | 30 newborn infants, birthweight < 1500 grams | |
| Interventions | IV prophylactic indomethacin vs. an equal volume of normal saline. Indomethacin dosage: 3 doses (3 x 0.2 mg/kg), first dose at 12 hours of age, 12 hourly thereafter | |
| Outcomes | Cerebral palsy at 2 years corrected age Death IVH Symptomatic PDA Evolving chronic lung disease (clinical signs, pCO2 > 60 mm Hg at 2 weeks of age) NEC ROP Renal impairment | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Blinding? All outcomes | Low risk | Blinding of intervention ‐ yes Blinding of outcome measurement(s) ‐ yes |
| Incomplete outcome data addressed? All outcomes | Low risk | Complete (> 90%) follow‐up: yes |
Yaseen 1997.
| Methods | Blinding of randomisation: yes ‐ sealed, sequentially numbered and coded envelopes Blinding of intervention: yes Blind outcome assessment: yes Complete follow‐up (>90%): yes | |
| Participants | 27 preterm infants, birthweight <1750g, RDS requiring ventilation with > 30% oxygen. Excluded if platelets < 75,000/ml, creatinine >180 micromol/L, serum bilirubin > 90 micromol/L in first 8 hours | |
| Interventions | IV prophylactic indomethacin versus an equal volume of saline. First dose 0.2 mg/kg at 12 hours then repeated twice at 24 hour intervals. | |
| Outcomes | Death before hospital discharge; IVH grades 3 and 4: BPD at 28 days; duration of supplemental oxygen; NEC; duration of hospital stay. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Adequate |
| Allocation concealment? | Low risk | Adequate |
| Blinding? All outcomes | Low risk | Blinding of intervention ‐ yes Blinding of outcome measurement(s) ‐ yes |
| Incomplete outcome data addressed? All outcomes | Low risk | Complete (> 90%) follow‐up: yes |
ROP=retinopathy of prematurity CP=cerebral palsy BPD=bronchopulmonary dysplasia NEC=necrotising enterocolitis PDA=patent ductus arteriosus
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Bada 1996 | These data are presented in abstract only. From the limited published information, it is not possible to determine if this is follow‐up of an RCT or not, hence the data are not included in the review. However, it seems likely it may relate to the study listed in the "included studies" ‐ Bada 1989. |
| Cotton 1980 | Not a study of indomethacin given prophylactically. |
| Cotton 1983 | No original data on prophylactic indomethacin. |
| Gersony 1983 | Not a study of indomethacin given prophylactically. |
| Hammerman 1986 | Not an RCT. |
| Hammerman 1987 | Not a study of indomethacin used prophylactically. All the infants enrolled had echocardiographic evidence of a PDA at 48‐72 hours of life. |
| Hammerman 1990 | Not a study of indomethacin used prophylactically. |
| Hammerman 1995 | Not an RCT. |
| Kaapa 1983 | Not a study of indomethacin used prophylactically. |
| Krauss 1989 | Not a study of indomethacin used prophylactically. |
| Lai 1990 | This is an RCT of ORAL indomethacin used prophylactically. |
| Mahony 1982 | Not a study of prophylactic indomethacin ‐ all infants had "subclinical PDA". |
| Mardoum 1991 | Not an RCT of indomethacin given prophylactically. |
| Ment 1987 | This is probably the same study as Ment 1994b. Because it is not possible to determine this with certainty from the published information it has been labelled as a separate study. However, it probably reports interim analyses of the data included in this review taken from Ment 1994b and would not contribute any unique data. |
| Ment 1993 | From the published information, it is unclear if this was truly prophylactic indomethacin so the data presented cannot be included in this review. In fact, this might well be an analysis of a selected population from two studies that are included in this review ‐ Ment 1994a and Ment 1994b. It is therefore likely that the findings are already incorporated into the review. |
| Merritt 1981 | Not a study of indomethacin used prophylactically. |
| Monset‐Couchard 1983 | Not a trial of indomethacin used prophylactically: all infants had symptomatic PDA. |
| Mullett 1982 | This is an RCT of oral indomethacin and the treatment is not used prophylactically: all infants had clinical evidence of a PDA. |
| Nestrud 1980 | Not a trial of indomethacin given prophylactically: all the infants had PDA. |
| Neu 1980 | Not a study of indomethacin given prophylactically. |
| Rennie 1991 | Intervention was not indomethacin given prophylactically. |
| Rhodes 1988 | Not a trial of indomethacin used prophylactically. |
| Rudd 1983 | Not a study of indomethacin used prophylactically. |
| Valaes 1980 | Not a study of indomethacin used prophylactically. |
| van Overmeire 1995 | Not an RCT of indomethacin used prophylactically. |
| Vogtmann 1988 | This is a trial of oral prophylactic indomethacin. |
| Wagner 1984 | Not an RCT of prophylactic indomethacin. |
| Weesner 1987 | Not a study of prophylactic therapy ‐ all infants enrolled had an asymptomatic PDA. |
| Wurtzel 1990 | This is a trial examining the effects of maternal antenatal indomethacin on the renal function of the newborn infant. |
| Yanagi 1981 | Not a study of indomethacin used prophylactically. |
| Yeh 1981 | Not an RCT of indomethacin given prophylactically ‐ all infants had a documented PDA at entry to the trial. |
| Zamboni 1993 | Not an RCT of indomethacin. |
Contributions of authors
Peter Fowlie developed the original protocol and undertook the inception review (Fowlie 1997). Peter Fowlie and Peter Davis updated the review in 2002 (Fowlie 2002). William McGuire and Peter Fowlie undertook the May 2010 revision and update .
Sources of support
Internal sources
Murdoch Children's Research Institute, Melbourne, Australia.
Royal Women's Hospital, Melbourne, Australia.
Ninewells Hospital and Medical School, Dundee, UK.
Centre for Reviews and Dissemination, University of York, UK.
External sources
MRC (UK), UK.
Department of Clinical Epidemiology and Biostatistics, McMaster University, Canada.
Declarations of interest
None.
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
Bada 1989 {published data only}
- *Bada HS, Green RS, Pourcyrous M, et al. Indomethacin reduces the risks of severe intraventricular hemorrhage. Journal of Pediatrics 1989;115:631‐7. [DOI] [PubMed] [Google Scholar]
- Bada HS, Green RS, Pourcyrous M, Leffler CW, Korones SB, Arheart K. Indomethacin reduces relative risks of severe intraventricular hemorrhage [Abstract]. Pediatric Research 1989;25:353A. [DOI] [PubMed] [Google Scholar]
- Pourcyrous M, Bada HS, Green RS, Korones SB. Safety of indomethacin use for newborn infants [Abstract]. Pediatric Research 1988;23:422A. [Google Scholar]
Bandstra 1988 {published data only}
- *Bandstra ES, Montalvo BM, Goldberg RN, et al. Prophylactic indomethacin for prevention of intraventricular hemorrhage in premature infants. Pediatrics 1988;82:533‐542. [PubMed] [Google Scholar]
- Bandstra ES, Bauer CR, Duenas ML, Chao H, Montalvo BM, Bancalari E. Prophylactic indomethacin for prevention of intraventricular hemorrhage: neurodevelopmental follow‐up [Abstract]. Annals of Neurology 1987;22:427A. [Google Scholar]
- Bandstra ES, Duenas ML, Rodriguez I, et al. Prophylactic indomethacin for the prevention of intraventricular hemorrhage (IVH): neurodevelopmental follow‐up [Abstract]. Pediatric Research 1987;21:391. [Google Scholar]
- Setzer ES, Morse BM, Goldberg RN, Smith M, Bancalari E. Prophylactic indomethacin and intraventricular hemorrhage in the premature [Abstract]. Pediatric Research 1984;18:345A. [Google Scholar]
- Setzer ES, Smith M, Goulding PJ, Bandstra TE. Severity of platelet dysfunction induced by prophylactic indomethacin in the premature [Abstract]. Pediatric Research 1984;18:346A. [Google Scholar]
- Setzer ES, Torres‐Arraut E, Gomez‐del‐Rio M, Young ML, Pacheco I, Ferrer PL, et al. Cardiopulmonary effects of prophylactic indomethacin in the very low birth weight infant [Abstract]. Pediatric Research 1984;18:346A. [Google Scholar]
Couser 1996 {published data only}
- *Couser RJ, Ferrara TB, Wright GB, Cabalka AK, Schilling CG, et al. Prophylactic indomethacin therapy in the first 24 hours of life for the prevention of patent ductus arteriosus in preterm infants treated prophylactically with surfactant in the delivery room. Journal of Pediaitrcs 1996;128:631‐7. [DOI] [PubMed] [Google Scholar]
- Couser RJ, Hoekstra RE, Ferrara B, Wright GB, Cabalka AK, Connet JE. Neurodevelopmental follow‐up at 36 months' corrected age of preterm infants treated with prophylactic indomethacin. Archives of Pediatric and Adolescent Medicine 2000;154:598‐602. [DOI] [PubMed] [Google Scholar]
Domanico 1994 {published data only}
- Domanico RS, Waldman JD, Lester LA, McPhillips HA, Catrambone JE, Covert RF. Prophylactic indomethacin reduces the incidence of pulmonary hemorrhage and patent ductus arteriosus in surfactant‐treated infants < 1250 grams. Pediatric Research 1994;35:331A. [Google Scholar]
Gutierrez 1987 {published data only}
- Gutierrez NG, Lapasset M. Prophylactic indomethacin and the incidence of patent ductus arteriosus in preterm neonates. Proceedings of the 3rd Argentinian Congress of Perinatology, Buenos Aires. 1987; Vol. 62.
Hanigan 1988 {published data only}
- Hanigan WC, Kennedy G, Roemisch F, et al. Administration of indomethacin for the prevention of periventricular haemorrhage in high‐risk neonates. Journal of Pediatrics 1988;112:941‐7. [DOI] [PubMed] [Google Scholar]
Krueger 1987 {published data only}
- Krueger E, Mellander M, Bratton D, Cotton R. Prevention of symptomatic patent ductus arteriosus with a single dose of indomethacin. Journal of Pediatrics 1987;111:749‐54. [DOI] [PubMed] [Google Scholar]
Mahony 1985 {published data only}
- Mahony L, Caldwell RL, Girod DA, et al. Indomethacin therapy on the first day of life in infants with very low birth weight. Journal of Pediatrics 1985;106:801‐5. [DOI] [PubMed] [Google Scholar]
Ment 1985 {published data only}
- Ment LR, Duncan CC, Ehrenkranz RA, et al. Randomized indomethacin trial for prevention of intraventricular hemorrhage in very low birth weight infants. Journal of Pediatrics 1985;107:937‐43. [DOI] [PubMed] [Google Scholar]
Ment 1988 {published data only}
- Ment LR, Duncan CC, Ehrenkranz RA, et al. Randomized low‐dose indomethacin trial for prevention of intraventricular hemorrhage in very low birth weight neonates. Journal of Pediatrics 1988;112:948‐55. [DOI] [PubMed] [Google Scholar]
Ment 1994a {published data only}
- Ment LR, Oh W, Ehrenkranz, Phillip AGS, et al. Low‐dose indomethacin therapy and extension of intraventricular hemorrhage: a multicenter randomized trial. Journal of Pediatrics 1994;124:951‐5. [DOI] [PubMed] [Google Scholar]
Ment 1994b {published data only}
- Ment LR, Duncan CC, Ehrenkranz RA, Kleinman CS, Taylor KJW, Scott DT. Randomized low‐dose indomethacin trial for the prevention of intraventricular hemorrhage in very low birth weight neonates [Abstract]. Annals of Neurology 1987;22:406‐7. [Google Scholar]
- Ment LR, Oh W, Ehrenkranz RA, Phillip AG, Vohr B, Allan W, et al. Low‐dose indomethacin and prevention of intraventricular hemorrhage: a multicenter randomized trial. Pediatrics 1994;93:543‐50. [PubMed] [Google Scholar]
- Ment LR, Peterson BS, Meltzer JA, Vohr B, Allan W, Katz KH. A functional magnetic resonance imaging study of the long‐term influences of early indomethacin exposure on language processing in the brains of prematurely born children. Pediatrics 2006;118:961‐70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ment LR, Vohr B, Allan W, Westerveld M, Sparrow SS, Schneider KC, et al. Outcome of children in the indomethacin intraventricular hemorrhage prevention trial. Pediatrics 2000;105:485‐91. [DOI] [PubMed] [Google Scholar]
- Ment LR, Vohr B, Oh W, Scott DT, Allen WC, Westerveld M, et al. Neurodevelopmental outcome at 36 months corrected age of preterm infants in the Multicenter Indomethacin Intraventricular Hemorrhage Prevention Trial. Pediatrics 1996;98:714‐8. [PubMed] [Google Scholar]
- Vohr BR, Allan WC, Westerveld M, et al. School‐age outcomes of very low birth weight infants in the indomethacin intraventricular hemorrhage prevention trial. Pediatrics 2003;111:e340‐6. [DOI] [PubMed] [Google Scholar]
Morales‐Suarez 1994 {published data only}
- Morales‐Suarez M, Lemus‐Varella L, Udaeta‐Mora E, Cardiel‐Marmolejo L, Rodriguez‐Balderrama I, Liz‐Cedilla RE. Indomethacin in the prevention of subependymal‐intraventricular hemorrhage in preterm newborns with conventional mechanical ventilation. Boletin Medico del Hospital Infantil de Mexico 1992;49:217‐24. [PubMed] [Google Scholar]
- Morales‐Suarez M, Sanchez‐Gil T, Lemus‐Varela L. Low dose indomethacin for prevention of intraventricular hemorrhage in the preterm infant with mechanical ventilation: Final report of a randomized study [Estudio comparavito de dosis baja de indometacina profilactica para hemorragia subependimaria/intraventricular en neonatos pretermino con ventilation mecanica]. Boletin Medico del Hospital Infantil de Mexico 1994;51:389‐394. [Google Scholar]
Puckett 1985 {published data only}
- Puckett CG, Cox MA, Haskins KS, Fisher DJ. Prophylactic indomethacin (I) for the prevention of patent ductus arteriosus (PDA) [Abstract]. Pediatric Research 1985;19:358. [Google Scholar]
Rennie 1986a {published data only}
- Rennie JM, Doyle J, Cooke RWI. Early administration of indomethacin to preterm infants. Archives of Disease in Childhood 1986;61:233‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Supapannachart 1999 {published data only}
- Supapannachart S, Khowsathit P, Patchakapati B. Indomethacin prophylaxis for patent ductus arteriosus (PDA) in infants with a birth weight of less than 1250 grams. Journal of the Medical Associaition of Thailand 1999;82:S87‐S91. [PubMed] [Google Scholar]
TIPP 2001 {published data only}
- Ohlsson A, Roberts RS, Schmidt B, Davis P, Moddeman D, Saigal S, et al. Male/female differences in indomethacin effects in preterm infants. Journal of Pediatrics 2005;147:860‐2. [PUBMED: 16356449] [DOI] [PubMed] [Google Scholar]
- Schmidt B, Davis P, Moddemann D, Ohlsson A, Roberts RS, Saigal S, et al. Long‐term effects of indomethacin prophylaxis in extremely‐low‐birth‐weight infants. New England Journal of Medicine 2001;344:1966‐72. [DOI] [PubMed] [Google Scholar]
- Schmidt B, Roberts RS, Fanaroff A, Davis P, Kirpalani HM, Nwaesei C, et al. Indomethacin prophylaxis, patent ductus arteriosus, and the risk of bronchopulmonary dysplasia: further analyses from the Trial of Indomethacin Prophylaxis in Preterms (TIPP). Journal of Pediatrics 2006;148:730‐4. [DOI] [PubMed] [Google Scholar]
- Zupancic JA, Richardson DK, O'Brien BJ, Cronin CG, Schmidt B, Roberts R, et al. Retrospective economic evaluation of a controlled trial of indomethacin prophylaxis for patent ductus arteriosus in premature infants. Early Human Development 2006;82:97‐103. [DOI] [PubMed] [Google Scholar]
Vincer 1987 {published data only}
- Vincer M, Allen A. Does prophylactic indomethacin in VLBW (<1500 grams birth weight) infants cause cerebral palsy (CP)?. Pediatric Research 1998;43:232. [Google Scholar]
- Vincer M, Allen A, Evans J, Nwaesei C, Stinson D, Rees E, et al. Early intravenous indomethacin prolongs respiratory support in very low birth weight infants. Acta Paediatrica Scandinavica 1987;76:894‐7. [DOI] [PubMed] [Google Scholar]
Yaseen 1997 {published data only}
- Yaseen H, al Umran K, Ali H, Rustum M, Darwich M, al‐Faraidy A. Effects of early indomethacin administration on oxygenation and surfactant requirement in low birth weight infants. Journal of Tropical Pediatrics 1997;43:42‐6. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Bada 1996 {published data only}
- Bada HS, Yolton KA, Duncan C, Wong SP, Pourcyrous M, Korones SB. Indomethacin (INDO) prophylaxis and outcome at school age [abstract]. Pediatric Research 1996;39:373A. [Google Scholar]
Cotton 1980 {published data only}
- Cotton RB, Hickey DE, Graham TP, Stahlman MT. Effects of early indomethacin (I) on ventilatory status of preterm infants with symptomatic patent ductus arteriosus (sPDA) [abstract]. Pediatric Research 1980;14:442A. [Google Scholar]
Cotton 1983 {published data only}
- Cotton L, Hickey D, Stahlman MT. Management of premature infants with symptomatic patent ductus arteriosus Intensive. In: Stern L editor(s). Care in the Newborn. IV. New York: Masson Publishing Co, 1983:225‐31. [Google Scholar]
Gersony 1983 {published data only}
- Gersony WM, Peckham GJ, Ellison RC, Miettinen OS, Nadas AS. Effects of indomethacin in premature infants with patent ductus arteriosus: results of a national collaborative study. Journal of Pediatrics 1983;102:895‐906. [DOI] [PubMed] [Google Scholar]
- Peckham GJ, Miettinen OS, Ellison RC, Kraybill EN, Gersony WM, Zeirler S, Nadas AS. Clinical course to 1 year if age in premature infants with patent ductus arteriosus: results of a multicenter randomized trial of indomethacin. Journal of Pediatrics 1984;104:285‐91. [DOI] [PubMed] [Google Scholar]
Hammerman 1986 {published data only}
- Hammerman C, Strates E, Valaitis S. The silent ductus: its precursors and its aftermath. Pediatric Cardiology 1986;7:121‐7. [DOI] [PubMed] [Google Scholar]
Hammerman 1987 {published data only}
- Hammerman C, Strates E, Komar K, Bui K. Failure of prophylactic indomethacin to improve the outcome of the very low birth weight infant. Developmental Pharmacology and Therapeutics 1987;10:393‐404. [DOI] [PubMed] [Google Scholar]
Hammerman 1990 {published data only}
- Hammerman C, Aramburo MJ. Prolonged indomethacin therapy for the prevention of recurrences of patent ductus arteriosus. Journal of Pediatrics 1990;117:771‐6. [DOI] [PubMed] [Google Scholar]
Hammerman 1995 {published data only}
- Hammerman C, Glaser J, Schimmel MS, Ferber B, Kaplan M, Eidelman AI. Continuous versus multiple rapid infusions of indomethacin: effects on cerebral blood flow velocity. Pediatrics 1995;95:244‐8. [PubMed] [Google Scholar]
Kaapa 1983 {published data only}
- Kaapa P, Lanning P, Koivisto M. Early closure of patent ductus arteriosus with indomethacin in preterm infants with idiopathic respiratory distress syndrome. Acta Paediatrica Scandanavia 1983;72:179‐84. [DOI] [PubMed] [Google Scholar]
Krauss 1989 {published data only}
- Krauss AN, Fatica N, Lewis BS, Cooper R, Thaler HT, Cirrincione C, O'Loughlin J, Levin A, Engle MA, Auld PAM. Pulmonary function in preterm infants following treatment with intravenous indomethacin. American Journal of Diseases of Children 1989;143:78‐81. [DOI] [PubMed] [Google Scholar]
Lai 1990 {published data only}
- Lai TH, Soong WJ, Hwang B. Indomethacin for the prevention of symptomatic patent ductus arteriosus in very low birth weight infants. Acta Paediatrica Sinica 1990;31:17‐23. [PubMed] [Google Scholar]
Mahony 1982 {published data only}
- *Mahony L, Carnero V, Brett C, Heymann MA, Clyman RI. Prophylactic indomethacin therapy for patent ductus arteriosus in very low birth weight infants. New England Journal of Medicine 1982;306:506‐10. [DOI] [PubMed] [Google Scholar]
- Mahony L, Heymann MA, Carnero V, Brett C, Clyman RI. When to treat the patent ductus arteriosus with indomethacin in very low birth weight infants. Advances in Prostaglandin, Thromboxane, and Leukotriene Research 1983;12:491‐4. [PubMed] [Google Scholar]
Mardoum 1991 {published data only}
- Mardoum R, Bejar R, McFeely E, Peterson B, Merritt TA. Controlled study of the effects of indomethacin (INDO) on the cerebral blood flow velocities in the newborn infant [Abstract]. Pediatric Research 1988;23:554. [Google Scholar]
- Mardoum R, Bejar R, Merritt A, Berry C. Controlled study of the effects of indomethacin on cerebral blood flow velocities in newborn infants. Journal of Pediatrics 1991;118:112‐5. [DOI] [PubMed] [Google Scholar]
Ment 1987 {published data only}
- Ment LR, Duncan CC, Ehrenkranz RA, Kleinman CS, Taylor KJW, Scott DT. Randomized low‐dose indomethacin trial for the prevention of intraventricular hemorrhage in very low birth weight neonates [Abstract]. Annals of Neurology 1987;22:406‐7. [Google Scholar]
Ment 1993 {published data only}
- Ment LR, Oh W, Ehrenkrantz RA, Philip AGS, Schneider K, Katz KH, Taylor KJW, Duncan CC, Makuch. Risk period for intraventricular hemorrhage of the preterm neonate is independent of gestational age. Seminars in Perinatology 1993;17:338‐41. [PubMed] [Google Scholar]
Merritt 1981 {published data only}
- Merritt TA, Harris JP, Roghmann K, Wood B, Campanella V, Alexzon C, Manning J, Shapiro DL. Early closure of patent ductus arteriosus in very low birth weight infants: a controlled trial. Journal of Pediatrics 1981;99:281‐6. [DOI] [PubMed] [Google Scholar]
Monset‐Couchard 1983 {published data only}
- Monset‐Couchard M, Dias‐Mancano D, Murat I, Relier JP. Controlled trial of intravenous lyophilized indomethacin in the treatment of persistent ductus arteriosus in premature infants [French]. Pediatrie 1983;38:365‐77. [PubMed] [Google Scholar]
Mullett 1982 {published data only}
- *Mullett MD, Croghan TW, Myerberg DZ, Krall JM, Neal WA. Indomethacin closure of patent ductus arteriosus in prematures. Clinica Pediatrica 1982;21:217‐20. [DOI] [PubMed] [Google Scholar]
- Mullett MD, Crogan TW, Myerberg DZ, Neal WA. Administration of oral indomethacin (I) to prematures with patent ductus arteriosus (PDA): a randomized double blind study [Abstract]. Pediatric Research 1980;14:606. [Google Scholar]
Nestrud 1980 {published data only}
- Nestrud RM, Hill DE, Arrington RW, Beard AG, Dungan WT, Norton JB, Radinger RI. Indomethacin treatment in patent ductus arteriosus. A double blind study utilizing indomethacin plasma levels. Developmental Pharmacology and Therapeutics 1980;1:125‐36. [PubMed] [Google Scholar]
Neu 1980 {published data only}
- Neu J, Ariagno RL, Johnson JD, Pitlick PT, Cohen JS, Beets CL. A double blind study of the effects of oral indomethacin (IN) in preterm infants with patent ductus arteriosus (PDA) who failed medical management [Abstract]. Pediatric Research 1980;14:607. [PubMed] [Google Scholar]
Rennie 1991 {published data only}
- Rennie JM, Cooke RWI. Prolonged low dose indomethacin for persistent ductus arteriosus of prematurity. Archives of Disease in Childhood 1991;66:55‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Rhodes 1988 {published data only}
- Rhodes PG, Ferguson MG, Reddy NS, Joransen JA, Gibson J. Effects of prolonged versus acute indomethacin therapy in very low birth weight infants with patent ductus arteriosus. European Journal of Paediatrics 1988;147:481‐4. [DOI] [PubMed] [Google Scholar]
Rudd 1983 {published data only}
- Rudd P, Montanez P, Hallidie‐Smith K, Silverman M. Indomethacin treatment for patent ductus arteriosus in very low birthweight infants: double blind trial. Archives of Disease in Childhood 1983;58:267‐70. [DOI] [PMC free article] [PubMed] [Google Scholar]
Valaes 1980 {published data only}
- Valaes T, Moylan FMB, Cohn H, Chung K, Nagpaul K, Chrenoff HL, Kreidberg MB. Incidence and significance of PDA in preterm infants (PTI) and controlled blind trial of indomethacin (IND) [Abstract]. Pediatric Research 1980;14:452. [Google Scholar]
van Overmeire 1995 {published data only}
- Overmeire B, Brus F, Acker KJ, et al. Aspirin versus indomethacin treatment of patent ductus arteriosus in preterm infants with respiratory distress syndrome. Pediatric Research 1995;38:886‐91. [DOI] [PubMed] [Google Scholar]
Vogtmann 1988 {published data only}
- Vogtmann C, Grubbe G, Ruckhaberle KE, Bottcher H, Ockert C. Effects of early therapy with indomethacin on the manifestation of a persistent ductus arteriosus in extremely underweight premature infants [German]. Monatsschrift Kinderheilkunde 1988;136:636‐9. [PubMed] [Google Scholar]
Wagner 1984 {published data only}
- Wagner HR, Ellison C, Zierler S, Lang P, Purohit DM, Behrendt D, Waldhausen JA. Surgical closure of patent ductus arteriosus in 268 preterm infants. Journal of Thoracic and Cardiovascular Surgery 1984;87:870‐5. [PubMed] [Google Scholar]
Weesner 1987 {published data only}
- Weesner KM, Dillard RG, Boyle RJ, Block SM. Prophylactic treatment of asymptomatic ductus arteriosus in premature infants with respiratory distress syndrome. Southern Medical Journal 1987;80:706‐8. [DOI] [PubMed] [Google Scholar]
Wurtzel 1990 {published data only}
- Wurtzel D. Prenatal administration of indomethacin as a tocolytic agent: effect on neonatal renal function. Obstetrics and Gynecology 1990;76:689‐92. [PubMed] [Google Scholar]
Yanagi 1981 {published data only}
- Yanagi RM, Wilson A, Newfeld EA, Aziz KU, Hubt CE. Indomethacin treatment for symptomatic patent ductus arteriosus: a double blind control study. Pediatrics 1981;67:647‐52. [PubMed] [Google Scholar]
Yeh 1981 {published data only}
- *Yeh TF, Luken JA, Thalji A, Raval D, Carr I, Pildes RS. Intravenous indomethacin therapy in premature infants with persistent ductus arteriosus ‐ a double blind controlled study. Journal of Pediatrics 1981;98:137‐45. [DOI] [PubMed] [Google Scholar]
- Betkerur MV, Yeh TF, Miller K, Glasser RJ, Pildes RS. Indomethacin and its effect on renal function and urinary kallikrein excretion in premature infants with patent ductus arteriosus. Pediatrics 1981;68:99‐102. [PubMed] [Google Scholar]
- Yeh TF, Goldbarg HR, Henek T, Thalji A, Pildes RS. Intravenous indomethacin therapy in premature infants with patent ductus arteriosus. Causes of death and one year follow‐up. American Journal of Diseases of Children 1982;136:803‐7. [DOI] [PubMed] [Google Scholar]
- Yeh TF, Raval D, Pyati S, Pildes RS. Retinopathy of prematurity (ROP) and indomethacin therapy in premature infants with patent ductus arteriosus (PDA). Prostaglandins 1983;25:385‐91. [DOI] [PubMed] [Google Scholar]
- Yeh TF, Thalji A, Luken L, Lilien L, Carr I, Pildes RS. Improved lung compliance following indomethacin therapy in premature infants with patent ductus arteriosus. Chest 1981;80:698‐700. [DOI] [PubMed] [Google Scholar]
- Yeh TF, Wilks A, Singh J, Betkerur M, Lilien L, Pildes RS. Furosemide prevents the renal side effects of indomethacin therapy in premature infants with patent ductus arteriosus. Journal of Pediatrics 1982;101:433‐7. [DOI] [PubMed] [Google Scholar]
Zamboni 1993 {published data only}
- Zamboni G, Piemonte G, Boner A, et al. Influence of dietary taurine on vitamin D absorption. Acta Paediatrica 1993;82:811‐5. [DOI] [PubMed] [Google Scholar]
Additional references
Brown 1979
- Brown ER. Increased risk of bronchopulmonary dysplasia in infants with patent ductus arteriosus. Journal of Pediatrics 1979;95:865. [DOI] [PubMed] [Google Scholar]
Cifuentes 1979
- Cifuentes RF, Olley PM, Balfe JW, et al. Indomethacin and renal function in premature infants with persistent patent ductus arteriosus. Journal of Pediatrics 1979;95:583‐7. [DOI] [PubMed] [Google Scholar]
Cooke 2003
- Cooke L, Steer P, Woodgate P. Indomethacin for asymptomatic patent ductus arteriosus in preterm infants. Cochrane Database of Systematic Reviews 2003, Issue 1. [DOI: 10.1002/14651858.CD003745] [DOI] [PMC free article] [PubMed] [Google Scholar]
Coombs 1990
- Coombs RC, Morgan MEI, Durbin GM, et al. Gut blood flow velocities in the newborn: effects of patent ductus arteriosus and parenteral indomethacin. Archives of Disease in Childhood 1990;65:1067‐71. [DOI] [PMC free article] [PubMed] [Google Scholar]
Edwards 1990
- Edwards AD, Wyatt JS, Richardson C, et al. Effects of indomethacin on cerebral haemodynamics in very preterm infants. Lancet 1990;335:1491‐5. [DOI] [PubMed] [Google Scholar]
Evans 1990
- Evans NJ, Archer LN. Postnatal circulatory adaptation in healthy term and preterm neonates. Archives of Disease in Childhood 1990;65:24‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Evans 1995
- Evans N, Iyer P. Longitudinal changes in the diameter of the ductus arteriosus in ventilated preterm infants: correlation with respiratory outcomes. Archives of Disease in Childhood. Fetal and Neonatal Edition 1995;72:F156‐61. [DOI] [PMC free article] [PubMed] [Google Scholar]
Evans 1996
- Evans N, Kluckow M. Early determinants of right and left ventricular output in ventilated preterm infants. Archives of Disease in Childhood. Fetal and Neonatal Edition 1996;74:F88‐94. [DOI] [PMC free article] [PubMed] [Google Scholar]
Fowlie 1996
- Fowlie PW. Prophylactic indomethacin: systematic review and meta‐analysis. Archives of Disease in Childhood 1996;74:F81‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Friedman 1978
- Friedman Z, Whitman V, Maisels MJ, et al. Indomethacin disposition and indomethacin‐induced platelet dysfunction in premature infants. Journal of Clinical Pharmacology 1978;18:272‐9. [DOI] [PubMed] [Google Scholar]
Herrera 2007
- Herrera C, Holberton J, Davis P. Prolonged versus short course of indomethacin for the treatment of patent ductus arteriosus in preterm infants. Cochrane Database of Systematic Reviews 2007, Issue 2. [DOI: 10.1002/14651858.CD003480.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Heymann 1976
- Heymann MA, Rudolph AM, Silverman NH. Closure of the ductus arteriosus in premature infants by inhibition of prostaglandin synthesis. New England Journal of Medicine 1976;295:530‐3. [DOI] [PubMed] [Google Scholar]
ICROP 1984
- ICROP. An International Classification of Retinopathy of Prematurity. Pediatrics 1984;74:127‐133. [PubMed] [Google Scholar]
Knight 2001
- Knight DB. The treatment of patent ductus arteriosus in preterm infants. A review and overview of randomized trials. Seminars in Neonatology 2001;6:63‐73. [DOI] [PubMed] [Google Scholar]
Lipman 1982
- Lipman B, Server GA, Brazy JE. Abnormal cerebral haemodynamics in preterm infants with patent ductus arteriosus. Pediatrics 1982;69:778‐781. [PubMed] [Google Scholar]
Malviya 2008
- Malviya M, Ohlsson A, Shah S. Surgical versus medical treatment with cyclooxygenase inhibitors for symptomatic patent ductus arteriosus in preterm infants. Cochrane Database of Systematic Reviews 2008, Issue 1. [DOI: 10.1002/14651858.CD003951.pub2] [DOI] [PubMed] [Google Scholar]
Mosalli 2008
- Mosalli R, Alfaleh K. Prophylactic surgical ligation of patent ductus arteriosus for prevention of mortality and morbidity in extremely low birth weight infants. Cochrane Database of Systematic Reviews 2008, Issue 1. [DOI: 10.1002/14651858.CD006181.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ohlsson 2008
- Ohlsson A, Walia R, Shah S. Ibuprofen for the treatment of patent ductus arteriosus in preterm and/or low birth weight infants. Cochrane Database of Systematic Reviews 2010, Issue 4. [DOI: 10.1002/14651858.CD003481.pub4] [DOI] [PubMed] [Google Scholar]
Papile 1978
- Papile LA, Burstein J, Burstein R, Koffler H. Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birthweights less than 1,500 grams. Journal of Pediatrics 1978;92:529‐34. [DOI] [PubMed] [Google Scholar]
Roberts 2009
- Roberts G, Doyle LW, Anderson PJ. The stability of the diagnosis of developmental disability between age 2 and 8 in a geographic cohort of very preterm children born In 1997. Archives of Disease in Childhood 2009;October 14:[Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
Shah 2006
- Ohlsson A, Shah SS. Ibuprofen for the prevention of patent ductus arteriosus in preterm and/or low birth weight infants. Cochrane Database of Systematic Reviews 2006, Issue 1. [DOI: 10.1002/14651858.CD004213.pub2] [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Fowlie 1997
- Fowlie PW. Intravenous indomethacin for preventing mortality and morbidity in very low birth weight infants. Cochrane Database of Systematic Reviews 1997, Issue 3. [DOI: 10.1002/14651858.CD000174] [DOI] [PubMed] [Google Scholar]
Fowlie 2002
- Fowlie PW, Davis PG. Prophylactic intravenous indomethacin for preventing mortality and morbidity in preterm infants. Cochrane Database of Systematic Reviews 2002, Issue 3. [DOI: 10.1002/14651858.CD000174] [DOI] [PubMed] [Google Scholar]


