Abstract
Background: Vision screening in infants is an important part of the medical care of children as some eye abnormalities, if not treated in the first few months or years of life, can lead to irreversible vision loss. Objective: The objective of this cross-sectional, descriptive study was to identify ocular anomalies among infants attending immunization clinics in Nigeria and refer promptly and appropriately. Methodology: Infants were screened across 6 immunization clinics. Screening activities included relevant ocular history, vision assessment, external ocular examination, ocular motility, Hirschberg’s test, pupil examination, and the red reflex test. Infants with abnormal findings were referred for comprehensive eye examination. Result: Of the 142 infants who underwent vision screening, 29 were referred. These referrals were either as a result of ocular abnormalities (n = 22) or presence of risk factors from history (n = 7). The prevalence of ocular abnormalities was 15.5% and neonatal conjunctivitis (38%), was the commonest ocular abnormality found. Others were bacterial conjunctivitis (14%), nasolacrimal duct obstruction (14%), strabismus (14%), capillary hemangiomas (10%), iris nevi (5%), and vernal keratoconjunctivitis (5%). Of the 7 infants referred based on history alone, 6 (85.7%) had a history of prematurity. Conclusion: Conjunctivitis, strabismus, congenital nasolacrimal duct obstruction, and capillary hemangioma are some of the prevalent disorders seen in infants at immunization clinics in Nigeria. Babies at risk of retinopathy of prematurity (preterm birth and oxygen therapy) can be identified. Immunization clinics can serve as good points of vision screening for infants in developing countries to facilitate prompt referral and treatment.
Keywords: vision screening, infants, immunization clinics
Introduction
Vision screening is an evaluation to detect reduced visual acuity or risk factors that threaten the healthy growth and development of the eye and visual system.1 It is an important part of the medical care of children as some eye abnormalities, if not treated in the first few months or years of life, can lead to irreversible vision loss; thereby increasing the magnitude of childhood blindness.2,3
Children are born with an immature visual system and need clear, focused images for normal visual development to occur.4 Amblyopia following failure of normal visual maturation cannot be corrected in adult life. Early recognition and treatment of childhood eye diseases, such as cataract, congenital glaucoma, corneal opacities, hereditary retinal dystrophies, lesions of the optic nerve, and retinopathy of prematurity,5,6 is therefore crucial to the prevention of blindness.4,7 Visual loss may also be an early indication of serious or life-threatening diseases, such as retinoblastoma or lipid storage disorders.2
The American Academy of Ophthalmology (AAO)1 and the American Academy of Pediatrics (AAP)3,8 recommend visual assessment from birth and during all routine health supervisory visits. The AAP guidelines include screening from the newborn period to age 3 years, by using the following components: ocular history, vision assessment, external examination, ocular motility, pupil examination, and red reflex examination. Infants with a known risk (retinopathy of prematurity, Down’s syndrome, etc) or significant family history (congenital glaucoma, strabismus) should be referred for further evaluation.8
Many strategies and suggestions have been put forward regarding the effective vision screening of infants and young children worldwide.9-14 Vision screening programs have been stratified by age; and several studies support the screening of infant/preschool children, highlighting its importance in the prevention of amblyopia and blindness.15-17 In developed countries18 and in Africa,19,20 such screening exercises have been conducted in schools at various levels but targeting well-child clinics will facilitate assessing children’s eyes at an earlier age. The Minnesota Expert Panel on Childhood Vision Screening21 therefore advocates the screening of infants for ocular anomalies at every well-child visit, following the usual schedule. The well-child clinics of the Western world are analogous to our immunization clinics in Nigeria.22
Immunization clinics are not just a tool to combat infectious diseases but also an avenue for health education and routine health examination. The National Program on Immunization (NPI),23 formerly Expanded Program for Immunization, has been in existence in Nigeria since 1979 and its immunization schedule describes vaccination of children from birth to 12 months of age. Over the years, the NPI has adopted and implemented strategies that aim to improve coverage and deliver other relevant child health interventions such as distribution of insecticide-treated nets, vitamin A supplementation, antihelminthics distribution, and so on.23,24 This provides a potential avenue for the incorporation of eye screening exercises into the NPI which, because of good coverage, will have a significant impact.
This study, therefore, aims to carry out vision screening on infants attending immunization clinics in Enugu North Local Government Area, Enugu State, Nigeria. This would provide an avenue for prompt referral of previously unidentified ocular anomalies for specialist care, thus contributing to the prevention of childhood blindness.
Methods
This is a prospective cross-sectional descriptive study in which infants attending randomly selected immunization clinics in Enugu North Local Government Area (LGA), Enugu State, Nigeria, underwent eye screening. Enugu state in southeast Nigeria is made up of 17 LGAs. The sample size was calculated using the Cochran formula for qualitative cross-sectional studies of infinite populations.25 A multistage sampling method was used. First, the 17 wards in Enugu-North LGA with health facilities offering immunization services were grouped into 6 clusters (A-F) based on location. From each of these groups, an immunization center was selected by simple random sampling method, using the balloting technique.
Subsequently, the children to be screened in each immunization center were selected. Based on the calculated minimum sample size, a target of 21 infants per center was set. A systematic sampling method was applied in which every second infant from an attendance list, whose parents or guardians had given consent, was screened. Ethical approval for this study was obtained from the Health Research Ethics Committee of University of Nigeria Teaching Hospital, Enugu (NHREC/05/01/2008B-FWA00002458-1RB00002323).
An interviewer-administered structured questionnaire was used to generate information on the sociodemographic and socioeconomic characteristics of the patient. The relevant ocular history included questions on the parents’ observation (Have you observed any problem with your child’s eye?) and infant visual behavioral patterns for certain age groups. Family history as regarding risk factors for ocular morbidity and blindness included first-degree relatives with congenital cataracts, congenital glaucoma, squint in childhood, or retinoblastoma. These questions were aided by picture representations of these conditions. Participants then underwent vision screening as recommended by the AAO, American Association for Pediatric Ophthalmology and Strabismus (AAPOS), and AAP for different age groups.1,8 (See summary tables in Supplementary Files 1 and 2.)
Visual acuity was assessed by the blink response to bright light in infants less than 3 months, and binocular fix and follow response in infants 3 months and above. The external structures of the eye were examined with a pen torch and a head loupe. Then, the corneal light reflex was assessed for proper alignment using the Hirschberg’s method. Ocular motility was assessed with a light source or a bright object/toy moving in the directions of gaze, for infants who could fix and follow (from 3 months). The red reflex was assessed using the direct ophthalmoscope to view both eyes simultaneously. This was done from approximately 60 cm away, with a broad beam directed so that both eyes were illuminated at the same time.
On completion of the screening examinations for each infant, a provisional diagnosis was made where applicable and the duration of the examination was documented. Each child in whom an abnormality was detected was promptly referred to the nearest specialist center for a comprehensive eye evaluation and treatment. All infants with no relevant ocular history or normal findings on examination were considered to have passed the screening.
Data management was done using the IBM SPSS Statistics for Windows (version 23.0; IBM Corp, Armonk, NY).
Results
A total of 142 infants were screened, across 6 NPI centers. Seventy-six (53.5%) were male and 66 (46.5%) were female, giving a male:female ratio of 1.15:1. The age range was from a day (0.03 months) old to 363 days (11.93 months) with a mean age of 91.63 ± 7.10 days (3.05± 0.24 months). The demographics of the infants screened is shown in Table 1.
Table 1.
Demographics of Infants Screened.
| Demographic Parameters | n (%) |
|---|---|
| Gender | |
| Male | 76 (53.5) |
| Female | 66 (46.5) |
| Age group (months) | |
| ≤1 | 30 (21.1) |
| >1-3 | 60 (42.3) |
| >3-6 | 27 (19.0) |
| >6-9 | 13 (9.2) |
| >9-12 | 12 (8.5) |
| Tribe | |
| Igbo | 134 (94.4) |
| Non-Igbo | 8 (5.6) |
| Highest educational qualification of mothers | |
| Primary | 8 (5.6) |
| Secondary | 66 (46.5) |
| Tertiary | 68 (47.9) |
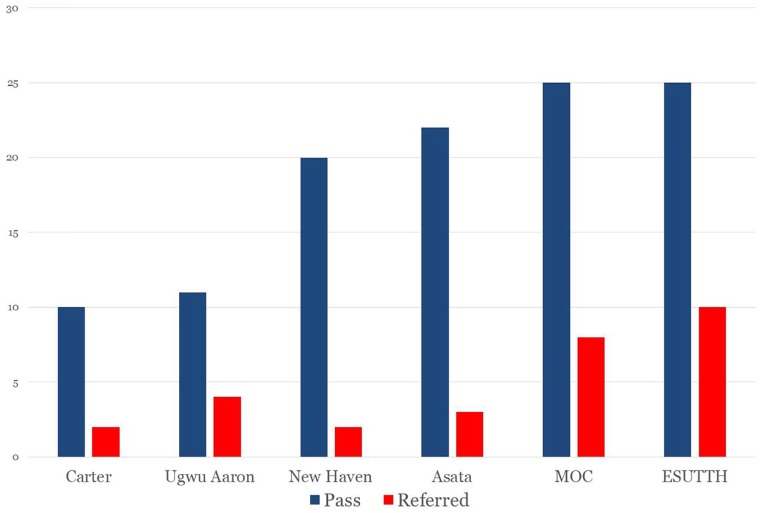
The majority of infants (42.3%) were aged >1 to 3 months. Of the 142 infants screened, 113 (79.6%) passed the test and 29 were referred (20.4%). The distribution of infants who passed the screening and those referred across the 6 screening centers is illustrated in Figure 1. The infants referred were either as a result of ocular abnormalities (n = 22) or the of risk factors from history (n = 7). Thus, the prevalence of ocular abnormalities was 15.5%. The screening findings are summarized in Table 2.
Figure 1.
Distribution of infants across screening centers.
Table 2.
Summary of Screening Findings.
| Reason for Referrala | n (%) |
|---|---|
| Relevant ocular history | 7 (20.7) |
| Abnormal vision assessment | 1 (2.9) |
| Abnormal external ocular exam | 18 (52.9) |
| Abnormal ocular motility | 0 (0) |
| Abnormal corneal light reflex | 3 (8.8) |
| Abnormal pupillary examination | 0 (0) |
| Abnormal red reflex examination | 5 (14.7) |
Some infants had more than 1 abnormal finding.
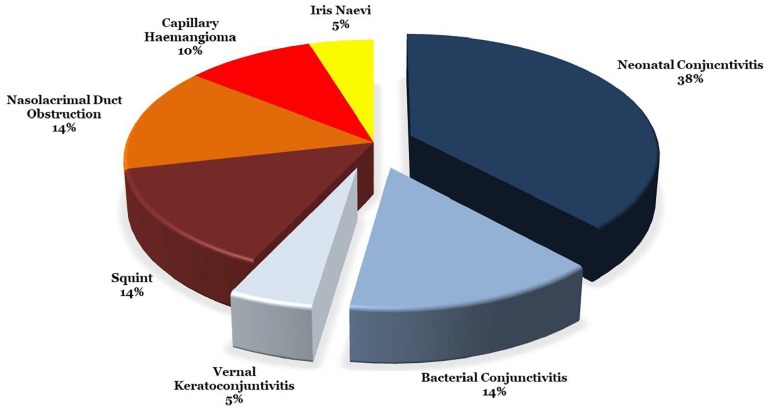
Of those referred, 11 were males and 18 females (male:female 1:1.64). While conjunctivitis was the most frequent reason for referral overall (n = 12), the risk of retinopathy of prematurity was the most frequently occurring history (n = 6). Provisional diagnoses were made on 21 infants and included conditions such as neonatal conjunctivitis, bacterial conjunctivitis, nasolacrimal duct obstruction, vernal keratoconjunctivitis, strabismus, iris nevi, and capillary hemangiomas as illustrated in Figure 2. No infants with congenital cataract, congenital glaucoma, corneal opacities or ptosis were seen.
Figure 2.
Provisional diagnoses of referred infants.
Out of the 22 infants with abnormalities, 12 (54.5%) parents suspected something was wrong with their child’s eyes. Of the 7 infants referred based on history, 1 had a positive first-degree family history of childhood squint. Six had a history of prematurity, 5 of whom had oxygen therapy.
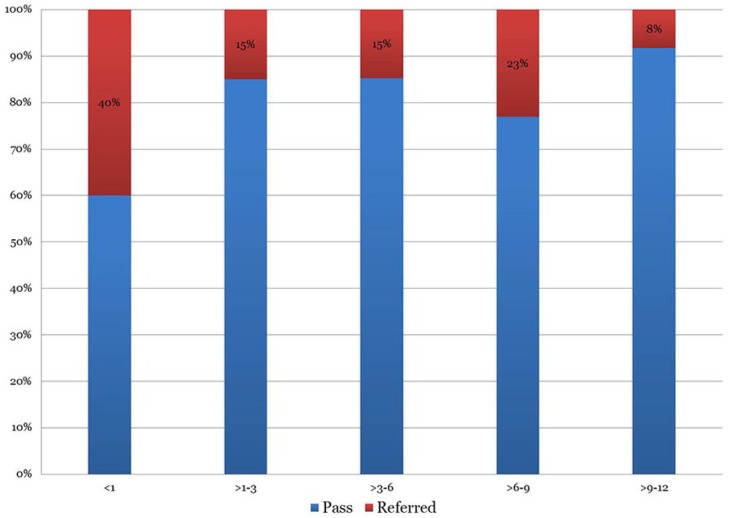
Neonates accounted for most of the referrals (n = 11, 38%) and only 1 (3%) infant in the >9- to 12-month age group was referred as shown in Figure 3.
Figure 3.
Proportion of referrals across the age groups (months).
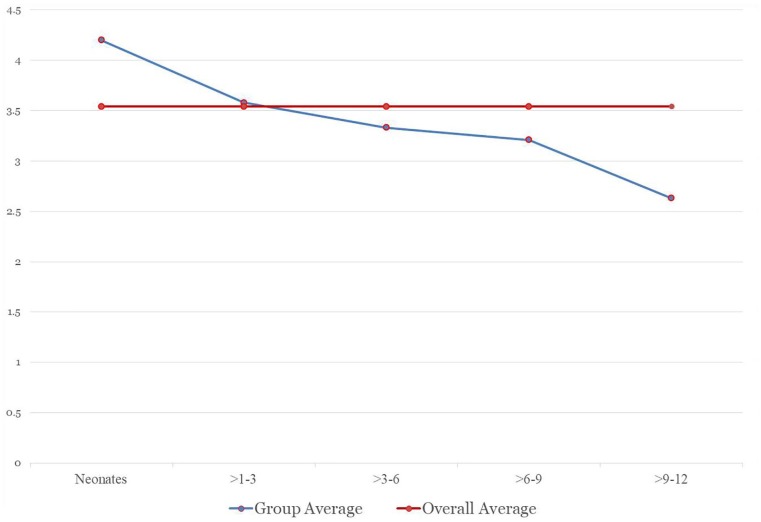
The time for examination ranged from 1.10 to 6.53 minutes per infant, with an overall average of 3.54 ± 0.10 minutes for infants who passed, and 4.37 ± 1.2 minutes for those who were referred. This is further illustrated in Figure 4.
Figure 4.
Average time for examination across the age groups (months).
Discussion
The largest proportion of the infants screened were less than 3 months of age. This could be due to a greater compliance with NPI appointments among parents with younger infants, as expected. The highest number of referrals was found in infants aged 1 month and below. The prevalence of neonatal/bacterial conjunctivitis and history of prematurity among them could account for this; as these were the most frequently occurring reasons for referral. Also, there were a decreasing number of infants attending NPI clinic after 6 months of age. These findings may support the screening of infants during their immunization visits at 6 weeks and 6 months.
The prevalence of ocular anomalies in this study was 15.5%, which was surprisingly high for a study with its sample size. Similar figures (14.93%) were obtained by Goyal et al.26 However, this26 study included posterior segment examination. The study done in Hawaii,14 though the sample size was similar to that of the index study (137), had a prevalence of 8%. This discrepancy may be attributed to the fact that diagnoses, in the index study, were provisional and on confirmation, may reduce in number.
The study had 29 referrals; 22 (15.5%) had ocular abnormalities and 7 (4.9%) referrals were due to presence of risk factors for ocular morbidities. All infants in this study with a history of prematurity were referred for comprehensive ocular examination to rule out retinopathy of prematurity. Nie et al27 similarly referred all 27 infants with a history of prematurity; however, an immediate comprehensive ocular examination was carried out in the field with handheld slit lamps and mydriatic examination.
All screened infants passed the pupil examination and no defective ocular motility was documented. This may be as a result of the rarity of optic neuropathies and restrictive motility syndromes, as was found by other authors.26 One participant was referred on account of a defective red reflex test alone and no provisional diagnosis was made. Most anomalies were detected on external ocular examination and ocular discharge was the most common feature. Neonatal conjunctivitis has been documented as the commonest acquired ocular abnormality in a neonatal ocular screening study27 and this was similar to the findings in this study. Other studies26,28 found retinal hemorrhages to be the major abnormality detected on screening. However, these authors26,28 also performed dilated fundus examination with the RetCam wide-field digital imaging system, which was not used in this study. Three infants with neonatal jaundice were encountered and referred for pediatric evaluation.
Congenital ocular anomalies such as ptosis, corneal opacity, congenital cataract, and congenital glaucoma were not noted in this study. This may be attributable to the low incidence of these congenital disorders.29 Li et al28 screened 3573 infants within their first 42 days and found 7 cases of optic nerve dysplasia, 2 cases of congenital cataracts, 2 cases of persistent fetal vasculature, and 1 corneal leucoma. Nie et al27 screened 15 398 neonates and identified congenital ptosis in 2 cases (0.013%), congenital corneal opacity in 6 cases (0.039%), congenital cataract in 15 cases (0.097%), and no congenital glaucoma. This shows that these conditions could be identified when screening a large number of infants; as will be the case with the inclusion of regular eye screening into the NPI.
Though the examinations in this screening exercise were performed by ophthalmologists-in-training, these examinations can easily be carried out by nurses or community health workers who have had adequate training.
The average duration of examination per infant was 3.54 minutes. This was determined in order to establish the additional time required to attend to an infant in the immunization clinic, if vision screening is incorporated. The longest duration of examination was 6.53 minutes which suggests that the benefits of additional eye screening will far outweigh the additional time spent in the immunization clinic.
Most of the studies regarding the screening of infants for eye abnormalities were carried out in Europe, America, or Asia. The previous reports from Africa and Nigeria in particular, generally address vision screening in children of preschool, primary school, and secondary school age.
The lack of eye screening in neonates and infants is attributable to the misconception that vision screening in this age group must be expensive, time-consuming, and cumbersome, and hence unacceptable to both health care providers and recipients. This article has illustrated that there are quick, easy and efficient screening tests to detect eye abnormalities in infants on a large scale, with subsequent adequate referral. It has also shown that, through a government-endorsed partnership, the national immunization program can be maximized to ensure extensive coverage of primary eye care in children nationwide, beginning at infancy.
Limitations
Almost all the parents and caregivers gave negative responses about the family history of ocular diseases. This could have been a reflection of their poor knowledge of the disease conditions rather than a true absence of such history.
Several studies13,14,30 have been done on the efficacy, sensitivity and specificity of photo-screening devices. The use of these devices would have permitted screening of larger number of infants in less time and definitive diagnosis such as refractive error made on field.
Conclusion
Conjunctivitis, strabismus, congenital nasolacrimal duct obstruction, and capillary hemangioma are some of the prevalent disorders seen in infants at immunization clinics. Babies at risk, such as those with a history of prematurity and oxygen therapy or those with positive relevant family ocular history, can be identified at immunization clinics and referred for comprehensive eye evaluation. This study has also shown that vision screening can be effectively carried out on infants attending immunization clinics, which makes a strong case for the incorporation of regular infant vision screening into the Immunization program of developing countries.
Supplemental Material
Supplemental material, Supporting_Tables_editable for Vision Screening in Infants Attending Immunization Clinics in a Developing Country by Chinwe Cynthia Jac-Okereke, Chukwunonso Azubuike Jac-Okereke, Ifeoma Regina Ezegwui and Obiekwe Okoye in Journal of Primary Care & Community Health
Acknowledgments
We wish to appreciate the management of the health institutions where the screening exercises were conducted; Asata Health Centre, Enugu State University of Science and Technology Teaching Hospital (ESUTTH), Ugwu Aaron Health Centre, Mother of Christ Specialist Hospital, New Haven Health Centre, and Carter Street Health Centre. Also, the following doctors were of great assistance; Chukwu Chinonso, Edoga Chima, Ehumadu Chioma, Ezike Chinenye, Nwaogwugu Ebuka, Nweke Adaobi, and Ogwuegbu Nonso,
Footnotes
Author Contributions: The authors listed have significant contributions, including conception and design, data collection, analysis and interpretation. All authors approved the final submitted version of this article.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Chinwe Cynthia Jac-Okereke  https://orcid.org/0000-0003-3665-480X
https://orcid.org/0000-0003-3665-480X
Supplemental Material: Supplemental material for this article is available online.
References
- 1. Wallace DK, Morse CL, Melia M, et al. Pediatric Eye Evaluations Preferred Practice Pattern®: I. Vision screening in the primary care and community setting; II. Comprehensive ophthalmic examination. Ophthalmology. 2018;125:P184-P227. doi: 10.1016/j.ophtha.2017.09.032 [DOI] [PubMed] [Google Scholar]
- 2. Coats DK, Paysse EA, Torchia MM. Visual development and vision assessment in infants and children. http://uptodate.dratef.net/contents/UTD.htm?23/59/24505?source=see_link. Accessed February 1, 2020.
- 3. Rogers GL, Jordan CO. Pediatric vision screening. Pediatr Rev. 2013;34:126-132. [DOI] [PubMed] [Google Scholar]
- 4. Gilbert C, Foster A. Childhood blindness in the context of VISION 2020—the right to sight. Bull World Health Organ. 2001;79:227-232. [PMC free article] [PubMed] [Google Scholar]
- 5. World Health Organization. Priority eye diseases. https://www.who.int/blindness/causes/priority/en/index1.html. Accessed February 1, 2020.
- 6. Gilbert C, Muhit M. Twenty years of childhood blindness: what have we learnt? Community Eye Health. 2008;21:46-47. [PMC free article] [PubMed] [Google Scholar]
- 7. Gogate P, Muhit M. Blindness and cataract in children in developing countries. Community Eye Health. 2009;22:4-5. [PMC free article] [PubMed] [Google Scholar]
- 8. Donahue SP, Nixon CN; Section on Opthamology, American Academy of Pediatrics; et al. Visual system assessment in infants, children, and young adults by pediatricians. Pediatrics. 2016;137:28-30. [DOI] [PubMed] [Google Scholar]
- 9. Amit M; Canadian Paediatric Society; Community Paediatrics Committee. Vision screening in infants, children and youth. Paediatr Child Health. 2009;14:246-248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Halegoua J, Schwartz RH. Vision photoscreening of infants and young children in a primary care pediatric office: can it identify asymptomatic treatable amblyopic risk factors? Clin Pediatr (Phila). 2015;54:33-39. [DOI] [PubMed] [Google Scholar]
- 11. Basch CE. Vision and the achievement gap among urban minority youth. J Sch Health. 2011;81:599-605. [DOI] [PubMed] [Google Scholar]
- 12. Zhao KX, Shi XF. Pay attention to abnormal vision screening for infants and young children [in Chinese]. Zhonghua Yan Ke Za Zhi. 2013;49:577-579. [PubMed] [Google Scholar]
- 13. Crescioni M, Miller JM, Harvey EM. Accuracy of the spot and plusoptix photoscreeners for detection of astigmatism. J AAPOS. 2015;19:435-440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Chang DA, Ede RC, Chow DC, et al. Early childhood vision screening in Hawaii utilizing a hand-held screener. Hawaii J Med Public Health. 2015;74:292-296. [PMC free article] [PubMed] [Google Scholar]
- 15. US Preventive Services Task Force. Vision screening for children 1 to 5 years of age: US Preventive Services Task Force recommendation statement. Pediatrics. 2011;127:340-346. [DOI] [PubMed] [Google Scholar]
- 16. Jonas DE, Amick HR, Wallace IF, et al. Vision screening in children aged 6 months to 5 years: evidence report and systematic review for the US Preventive Services Task Force. JAMA. 2017;318:845-858. [DOI] [PubMed] [Google Scholar]
- 17. Chang CH, Tsai RK, Sheu MM. Screening amblyopia of preschool children with uncorrected vision and stereopsis tests in Eastern Taiwan. Eye (Lond). 2007;21:1482-1488. [DOI] [PubMed] [Google Scholar]
- 18. Mathers M, Keyes M, Wright M. A review of the evidence on the effectiveness of children’s vision screening. Child Care Health Dev. 2010;36:756-780. [DOI] [PubMed] [Google Scholar]
- 19. Balarabe A, Adamu I, Abubakar A. Vision screening to detect refractive errors in three selected secondary schools in Birnin Kebbi, North West, Nigeria. Sahel Med J. 2015;18:61-65. [Google Scholar]
- 20. Adegbehingbe BO, Oladehinde MK, Majemgbasan TO, Onakpoya HO, Osagiede EO. Screening of adolescents for eye diseases in Nigerian high schools. Ghana Med J. 2005;39:138-142. [Google Scholar]
- 21. Minnesota Department of Health. Vision Screening Procedures for Infancy, Childhood and School Age Children. St Paul, MN: Minnesota Department of Health; 2017. [Google Scholar]
- 22. Abhulimhen-Iyoha B, Ibadin MO. Cord care education and its content given to mothers at antenatal clinics in various health facilities in Edo state, Nigeria. Sahel Med J. 2015;18:129-133. [Google Scholar]
- 23. Federal Ministry of Health Nigeria. Comprehensive EPI multi-year plan 2011-2015. http://www.nationalplanningcycles.org/sites/default/files/planning_cycle_repository/nigeria/cmyp_2011-2015_country_final.pdf. Accessed February 1, 2020.
- 24. Ophori EA, Tula MY, Azih AV, Okojie R, Ikpo PE. Current trends of immunization in Nigeria: prospect and challenges. Trop Med Health. 2014;42:67-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Machin D, Campbell MJ, Tan SB, Tan SH. Sample Size Tables for Clinical Studies. Oxford, England: Wiley-Blackwell; 2008. [Google Scholar]
- 26. Goyal P, Padhi TR, Das T, et al. Outcome of universal newborn eye screening with wide-field digital retinal image acquisition system: a pilot study. Eye (Lond). 2018;32:67-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Nie WY, Wu HR, Qi YS, et al. A pilot study of ocular diseases screening for neonates in China [in Chinese]. Zhonghua Yan Ke Za Zhi. 2008;44:497-502. [PubMed] [Google Scholar]
- 28. Li LH, Li N, Zhao JY, et al. Findings of perinatal ocular examination performed on 3573, healthy full-term newborns. Br J Ophthalmol. 2013;97:588-591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Mansoor N, Mansoor T, Ahmed M. Eye pathologies in neonates. Int J Ophthalmol. 2016;9:1832-1838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Mendez AM, Arguello L, Martinez J, et al. Evaluation of the Spot vision screener in young children in Costa Rica. J AAPOS. 2015;19:441-444. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, Supporting_Tables_editable for Vision Screening in Infants Attending Immunization Clinics in a Developing Country by Chinwe Cynthia Jac-Okereke, Chukwunonso Azubuike Jac-Okereke, Ifeoma Regina Ezegwui and Obiekwe Okoye in Journal of Primary Care & Community Health