Abstract
Hotel housekeepers are exposed to stressors at work and outside of work. A minimal amount is known about these workers’ pathophysiological responses to those stressors. Allostatic load is a concept increasingly used to understand pathophysiologic manifestations of individuals’ bodily response to stress. The purpose of this study was to examine the associations between work and nonwork stressors, allostatic load, and health outcomes among hotel housekeepers. Work and nonwork stressors (e.g., the number of traumatic events, everyday discrimination, and job strain) and health outcomes (e.g., general health status, physical and mental health, and chronic diseases) were measured. Biometric and anthropometric measures and fasting blood specimens were collected. Blood biomarkers included CRP, HbA1c, HDL, and cortisol. Descriptive analyses, correlations, regressions, and t-tests were conducted. Forty-nine women hotel housekeepers participated, with a mean age of 40 years. One-fifth reported high job strain and more than 40% had at least one traumatic event. Chronic conditions were commonly reported, with about 78%, 55%, and 35% reporting one, two, and three chronic conditions, respectively. Correlation analyses showed that reports of high job strain and everyday discrimination were significantly associated with high ALI quartile score (r=0.39, p=0.011; r=0.41, p=0.004). Job strain and everyday discrimination had medium to large effect sizes on ALI quartile scores. High ALI quartile score was significantly associated with having at least one chronic disease (r=0.40, p=0.005), and it had a large effect size on chronic diseases. To our knowledge, this is the first study to explore allostatic load among hotel housekeepers. Hotel housekeepers have high exposure to stressors within and outside of their work and experience poor chronic conditions. Allostatic load had strong associations with both stressors and health outcomes. Despite this worker group being a hard-to-reach worker group to participate in research studies, this study demonstrates the feasibility of accessing, recruiting and collecting survey data and blood samples among them to determine health risks and guide future targeted interventions.
Keywords: Chronic conditions, hotel industry, immigrant workers, low-wage workers, maids, manual workers, Total Worker Health, travel accommodation, working population
Introduction
Hotel housekeepers (also referred to as hotel room cleaners or maids) are examples of low wage workers exposed to multiple stressors of undefined magnitude which increase their risk for poor health outcomes.[1] Among hotel housekeepers, immigrant women and women of color are overrepresented and exposed to physical, chemical, biological, and psychological hazards.[2-7] Hotel housekeepers have the highest injury rate (7.9 per 100) of all workers in the hospitality industry. They experience musculoskeletal disorders (3.2 per 100), low physical function, high levels of pain, and sprains and chronic diseases such as hypertension.[6,8,9] Moreover, data show increasing reports of illnesses and injuries among these workers (e.g., 897 more claims per year from 2010 to 2014).[10] A 2006 report of Workers Compensation data analysis identified an annual cost of more than $4.7 million from housekeepers alone.[11]
Constituting the majority of the 1.8 million workers in the hospitality industry, hotel housekeepers experience irregular work schedules, time pressure, hazardous physical conditions, few opportunities for professional growth, and lack of autonomy over their tasks.[12-16] This understudied population is part of a large and growing economic sector, thus meriting public health attention. Studies among this low wage worker group mainly focused on work hazards (e.g., musculoskeletal/ergonomic), with little emphasis on factors outside of work that can affect health. More importantly, manifestations of physiological responses to stressors within and outside of work remain unexplored among this at-risk worker group. Currently, it is a clinical challenge to identify who is most in need of interventions to remediate stress-related physiological dysregulations in time to prevent disease.
Concept of Allostatic Load
In 1998, McEwen proposed the concept of Allostatic Load (AL).[17] AL is defined as the accumulative physiological dysregulations across multiple body systems (i.e., cardiovascular, immune, neuroendocrine, and metabolic) in response to chronic or severe stressors.[18,19] AL is a near-term proxy outcome and can be considered as an early sign for developing clinical symptoms. AL has significant clinical value because it allows us to identify early signs of health risks at a subclinical level and thus can inform interventions geared at preventing further deterioration of health (i.e., health promotion and disease prevention). Although well-studied in the field of stress biology as an outcome, AL has been less studied in its role as a mechanism of adverse health outcomes and has only begun to be studied in occupational health science.[20-24]
Specifically, no studies have explored the AL levels among hotel workers who may experience elevated levels of work and nonwork stressors. Quantifying the physiological responses that manifest in relation to work and nonwork stressors would assist in identifying workers who are at high-risk for developing clinical conditions such as hypertension, diabetes and autoimmune disorders. Having a reliable, valid biological indicator of dysregulation that is sensitive to stress and stress reduction could aid in developing and testing interventions aimed at promoting worker health and safety and addressing occupational health disparities.
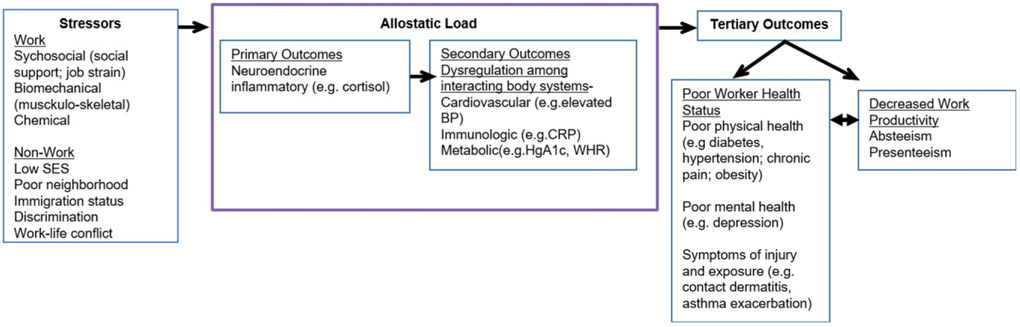
There are debates about inconsistences in the use of indicators to operationalize Allostatic Loads.[25-27] Yet there has been no report of an ideal set of indicators. Regardless of these inconsistences, AL remains a robust approach to determine pathophysiologic functioning and is increasingly being used to understand various eco-social gradients and how they relate to health disparities.[21,28-30] In fact, AL experts urge researchers to select their indicators based on their interested associated morbidity. McEwen stated, “biomarkers must be chosen and evaluated in terms of their functional significance in biological pathways, including both primary and secondary mediators and the secondary and tertiary consequences of their actions.”[31] For this study (Figure 1), our primary mediator was cortisol (indicator of the function of the neuroendocrine system). Our secondary consequences include blood pressure, heart rate, peak flow, BMI, waist-hip ratio, cholesterol, C-reactive protein (CRP), hemoglobin A1c, and triglycerides, all of which together indicate functioning of the cardiovascular, respiratory, immunologic, metabolic, and anthropometric systems. The AL score will indicate risks for the tertiary outcomes that are the chronic diseases.
Figure 1.
Model illustrating the stressor-stress-strain process for a low wage worker.
Applying a model of AL to address low wage workers’ health
Figure 1 depicts a model to explore stressors, AL, and outcomes among low wage workers. The model is aligned with the current National Institute for Occupational Safety and Health (NIOSH) Total Worker Health Initiative that emphasizes the need for a comprehensive approach that includes consideration of stressors both within (including the psychosocial work environment: i.e., job strain) and outside (including work-life balance, life stressors, health-related behaviors, and other socio-determinants) of the workplace to promote health and prevent injuries and illnesses among the 21st century workforce.[32-35] It also is consistent with conceptual models of AL.[18] Based on this model, stressors (work and nonwork) initiate responses (neuroendocrine, inflammatory), which, when chronic, lead to dysregulations in cardiorespiratory, immune, and metabolic systems that interact. These dysregulations then cause “wear and tear” seen as early stages of morbidity and, ultimately, manifest in premature disease, decreased work productivity, and untimely death.
AL is commonly operationalized as an index of an aggregated set of component indicators—biometric and anthropometric measures and biomarkers (e.g., cortisol, blood pressure, CRP, hemoglobin A1c, BMI). One issue to resolve is which indicators to include in the allostatic load index, given that the choice of indicators has varied across studies.[26] Some consensus is beginning to emerge for using a set of approximately 10 components that have strong utility as risk markers for disease in one or more of the body systems. Another issue to resolve is the scoring method. The most common method in research to date uses the high-risk quartile as a cut-point and sums the number of components for which the person’s levels are in that risk quartile. This method evidences a weakness of being “sample-specific” (i.e., top quartile among professional athletes vs. among their television watching fans); however, population norms have not yet been established. An alternative that may better serve clinical purposes would use established clinical cut-points on each indicator, which would be a step toward comparing individual risk based on a norm. In the absence of definitive index components and scoring recommendations, attention to these issues in pilot work remains important.
Measuring stressors
The Total Worker Health initiative calls for measuring both work and nonwork stressors from psychosocial as well as biomechanical and chemical sources. Measures for psychosocial stressors ideally should be assessed across eco-sociological levels, including intra- and inter-personal, contextual, and social determinant factors, such as trauma exposure. It is not known which stressors are most predictive of AL. These factors warrant comprehensive measurement and analysis, but the burdens associated with such comprehensive measurement on low wage workers is a concern, along with literacy level and concerns about acceptability of answering sensitive questions about trauma, or experiences of discrimination, for example. Preliminary studies are needed to continue testing the concept and estimating the effect size of the relationship between stressors and AL.
Feasibility
Low-wage workers are a challenging group to study. The stressors that may make them vulnerable to poor health outcomes could also deter participation, including immigration status, language and literacy barriers, and irregular shifts or multiple jobs that may make scheduling participation difficult. Pilot work is needed to verify that these workers can be recruited to participate in research studies involving survey, biometric and anthropometric measurements, and fasting blood collection. To assess feasibility, the ability to reach study participants was explored, and participant recruitment approaches were examined for effectiveness. In addition, the willingness of participants to allow blood draws and both willingness and ability of participants to complete the survey booklet were examined.
AL is a promising concept to use in occupational health; however, pilot research is needed. The purposes of this study were to assess feasibility, consider technical issues about measurement of stressors and creation and scoring of an AL index, show test-of-concept, and gather preliminary data.
Method
Recruitment and eligibility
Recruitment flyers were distributed through a local housekeepers’ union and augmented by the efforts of a bilingual (English-Spanish) cultural broker who had the trust of the community. The cultural broker along with other members of the research team distributed flyers in local hotels. Either they were instructed to leave the flyers at the front desk or a manager took the flyer and informed the research team that they would post the flyers in the breakrooms. The flyers had contact information, and individuals who were interested in participating reached out individually. Furthermore, snowball technique and collaboration with interested hotel housekeeping managers offered additional recruitment opportunities. To participate, individuals had to: (1) identify as female; (2) be currently employed as a hotel housekeeper; (3) be of age 18+ years; and (4) be able to provide verbal and written consent in English or Spanish. Exclusion criteria included: (1) private housekeepers and hotel housemen (because their working conditions and workload differ from that of female hotel housekeepers); and (2) those with bleeding disorders or unwillingness to provide a blood specimen.
Design, setting, and protocol
The study used a cross-sectional design. The study protocol was approved by the authors’ affiliating university Institutional Review Board.
Data were collected in home, workplace, or at an urban university site, based on study participants’ preference. Once individuals expressed their interest in participating in the study, research team members set up an appointment with them. Two to three days prior to the data collection, research team members contacted the individual to remind them not eat or drink prior to the data collection time. Thus, all the data were collected early in the morning before participants started their day or headed to work. On the morning of data collection, research team members answered participants’ questions about the study and obtained written consent. Biometric and anthropometric measures were then completed, followed by blood specimen collection, after which refreshments were provided. The protocol finished with completion of the questionnaire booklet containing the study surveys. Participants received $30 for their participation.
Biometric and anthropometric measures
The five biometric and anthropometric measures included systolic blood pressure (SBP), diastolic blood pressure (DBP), heart rate (HR), waist/hip ratio (WHR), and BMI. SBP, DBP, and HR were measured twice using the left arm, at least 5 min apart, with the participant in a seated position, both feet uncrossed and flat on the floor, using an OMRON Series 5 automated blood pressure device (Lake Forest, IL), following guidelines of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure.[36] A measurement tape was used to measure participants’ waists and hips. The iliac crest was located by placing hands around their waist, squeezing slightly and then moving fingers downward until the top curve of the hips was felt. A tape measure was placed just above the upper hip bone. Height in feet and inches and weight in pounds were measured to calculate BMI.
Blood specimen collection
Participants were instructed not to eat for at least 8 hr prior to blood specimen collection. A phlebotomist collected 10mL of blood to measure four biomarkers: high density lipoprotein (HDL), hemoglobin A1c (HbA1c), CRP, and cortisol. Blood specimens were transported (either at room temperature or on ice, depending on the distance traveled from the data collection location to the lab) to the laboratory for processing.
Blood specimen assays for indicators
Cortisol.
The human cortisol (ALPCo, 11-CORHU-E01) assay employs the quantitative competitive enzyme immunoassay technique. An antibody specific for cortisol has been precoated onto a microplate. Standards and samples are pipetted into the wells and cortisol present is bound by the immobilized antibody. This competes with enzyme-labeled cortisol for available binding sites. Following a wash to remove any unbound enzyme reagent, a substrate solution is added to the wells and color develops. The color development is stopped and the intensity of the color is measured. Absorbance at 450nm is inversely proportional to the amount of cortisol bound in the initial step. The assay has a range (standard curve) of 0.5–60 ug/dL. The following coefficients of variation were observed: inter-assay CV: 2.9% at 39.6 ug/dL, 6.1% at 16.2 ug/dL; intra-assay CV: 2.6% at 39.6 ug/dL, and 4.4% at 16.2 ug/dL.
High density lipoprotein (HDL).
The HDL assay was performed on the Alfa-Wasserman ACE analyzer and utilized a detergent to solubilize only the HDL particles, releasing HDL to react with cholesterol oxidase in the presence of chromogen (N, N-bis (4-sulfobutyl)-m-touidine) to produce a chromophor that absorbs at 592/692 nm. HDL concentration in serum is directly proportional to the amount of chromophor produced. The ACE HDL assay is linear from 2 to 125 mg/dL. The MDL is 2 mg/dL (2 SD greater than the 0 standard). The following coefficients of variation were reported: inter-assay CV: 9.9% at 23.8 mg/dL, 1.7% at 64.8 mg/dL; intra-assay CV: 2.4% at 23.8 mg/dL, and 2.0% at 64.8 mg/dL.
C-reactive protein (hsCRP).
CRP was performed on the Alfa-Wasserman ACE analyzer. CRP in the sample reacted with the anti-CRP sensitized latex particles in the hs-CRP antibody reagent to form antigen-antibody complexes that agglutinate the latex particles. The increase in absorbance, measured monochromatically at 592 nm, during a fixed time interval, is directly proportional to the amount of CRP in the sample. The ACE hs-CRP assay is linear from 0.25 to 10.0 mg/L. The MDL is 0.1 mg/dL (2 SD greater than the 0 standard). The following Intra-assay precision expressed as CV: 5.7% (0.5 mg/L), 2.0% (2.3 mg/L), and 1.2% (9.8 mg/L). The following inter-assay precisions are expressed as CV: 7.0% (0.5 mg/L), 3.3% (2.2 mg/L), and 1.2% (9.8 mg/L).
Hemoglobin A1c (HbA1c).
The human glycated hemoglobin A1c (HbA1c) assay (Antibodies On Line ABIN1570251, Supplied by Cloud Clone) is designed to quantitative measurement of HbA1c in human serum, plasma, and erythrocyte lysates. This assay employs the competitive inhibition enzyme immunoassay technique. A monoclonal antibody specific to HbA1c was precoated onto a microplate. A competitive inhibition reaction was launched between biotin labeled HbA1c and unlabeled HbA1c (standards or samples) with the precoated antibody specific to HbA1c. After incubation the unbound conjugate was washed off. Next, avidin conjugated to Horseradish Peroxidase (HRP) was added to each microplate well and incubated. The amount of bound HRP conjugate is inversely proportional to the concentration of HbA1c in the sample. After addition of the substrate solution, absorbance at 450nm is inversely proportional to the amount of HbA1c bound in the initial step. The assay has a range (standard curve) of 12.35–3000 μg/mL with a minimum detection limit of 4.95 μg/mL. The following Intra-assay precisions are reported expressed as CV: 3.7% (966 μg/mL). The following inter-assay precision are reported expressed as CV: 4.5% (966 μg/mL).
Questionnaire booklet
Participants completed a questionnaire booklet that contained questions that assessed work and nonwork related stressors. The questionnaire booklet had both English and Spanish version.
Work-related stressors.
A shortened version of the job content questionnaire (JCQ) was used to measure job strain.[37,38] The item score is based on a 4-point Likert scale ranging from “strongly disagree” to “strongly agree.” According to the scoring method of the JCQ, five items were included to compute the job demands score and nine items were included to calculate the job decision latitude score. The medians of the job demands and job decision latitude scores for the overall sample were also calculated. If the subject’s job demands score was more than the median and at the same time her job decision latitude score was less than the median, then the subject had high job strain. Otherwise, the subject had low job strain. The reliability (Cronbach’s alpha) of the JCQ in our sample was 0.88, indicating a good reliability of the JCQ in the hotel housekeeper sample. Except for job strain as a work-related stressor, the number of rooms cleaned on a normal shift was also inquired to reflect hotel housekeeper’s workload.
Nonwork stressors.
The nine-item Everyday Discrimination Scale (EDS) was used.[39] This scale measures everyday experiences of discrimination. Answers are based on a 6-point Likert scale ranging from “almost every day” to “never.” According to the scoring method of the EDS, subjects experiencing any of the items a few times a year or more were coded as high levels of discrimination (score of 1) compared with those who reported never or less than once a year (score of 0). The total score was the sum of the dichotomized item scores. A higher score indicated heightened discrimination in everyday life. High everyday discrimination was defined as experiencing any of the nine items a few times a year or more. The reliability (Cronbach’s alpha) of the EDS in our sample was 0.93, indicating an excellent reliability of the EDS in the hotel housekeeper sample. The Life Event Checklist was used, which queries lifetime history of 17 traumatic events (e.g., exposures to disaster, accidents, crime victimization, and not having money for food).[40] The six experience responses are “happened to me,” “witnessed it,” “learned about it,” “part of my job,” “not sure,” and “doesn’t apply to me.” According to the scoring method of the checklist, for each item, a score of one is given if the subject directly experienced the traumatic event (“happened to me”) and zero for all other of the remaining five responses. The number of traumatic events is the sum of the dichotomized item scores. In this study, trauma exposure was coded as having at least one traumatic event for which subjects answered “happened to me.”
Measures of health outcomes.
Participants’ health outcomes were assessed through the 12-item Short Form Health Survey (SF-12).[41,42] The SF-12 is a gold standard measure with 12 items that assess an individual’s overall general health with further details regarding physical and mental well-being. The specialized computer software – SF-12v2TM health survey was used to compute SF-12 physical and mental health scores and provide individual and aggregate reports of health status,[43] with higher score indicating better health. The one-item self-rated general health status instrument with five response options (1 = “excellent,” 2 = “very good,” 3 = “good,” 4 = “fair,” 5 = “poor”) was included. General health status was considered as a discrete variable for analysis. In addition, participants were asked if they had any of 13 types of chronic diseases (i.e., arthritis, chronic back pain, chronic neck pain, migraine headache, other frequent or severe headache, other chronic pain, hypertension, diabetes, asthma, high cholesterol, congestive heart failure, chronic sleeping problems, and chronic fatigue or low energy). The number of chronic diseases was computed. The chronic disease item was coded as present/not present.
Sociodemographic characteristics.
The questionnaire queried about age, race, ethnicity, education level, marital status, hourly wage, insurance, smoking status, and alcohol use.
Statistical Analysis
Feasibility was analyzed in relation to problems with procedures and amount and pattern of missing data. Feasibility was also determined based on the length of time it took to recruit study participants, any issues or concerns that arose during recruitment, and data collection. The most effective pathways to recruitment were also explored: the in-person flyer distribution at local hotels, use of the cultural broker, and word of mouths.
The allostatic load index (ALI) consisted of nine biomarkers: SBP, DBP, HR, WHR, BMI, HDL, HbA1c, CRP, and cortisol. Medication use was adjusted for in the preliminary analysis. Participants taking medications for hypertension at the time of assessment had 10mmHg and 5mmHg added to their respective SBP and DBP. Medication was adjusted. We dichotomized each biomarker into high- and low-risk two ways. To construct an ALI based on clinical risk parameters established for adult women (ALI-Clinical), we used clinical risk cut-points and summed the number of high-risk biomarkers for each person. The common method of summing the number of high-risk quartiles for each person (ALI-Quartile) was used.(30) Both ALI-Clinical and ALI-Quartile scores range from 0–9.
Frequencies, percentages, means and standard deviations were computed for sociodemographic characteristics, stressors, and health outcomes. Pearson correlation analyses were conducted to examine the correlations between ALI-Clinical and ALI-Quartile with general health status, SF-12 physical health, SF-12 mental health, everyday discrimination, and the number of rooms cleaned. Spearman correlation analyses were conducted to examine the correlations between ALI-Clinical and ALI-Quartile with job strain, trauma exposure, and chronic diseases. Multiple linear regressions were conducted to test the associations between stressors (e.g., job strain, the number of rooms cleaned on a normal day, everyday discrimination, and trauma exposure) with ALI-Clinical and ALI-Quartile. Dependent variables were ALI-Clinical and ALI-Quartile, while independent variables were job strain, the number of rooms cleaned on a normal day, everyday discrimination, and trauma exposure. Regressions were conducted to test the associations between ALI-Clinical and ALI-Quartile with health outcomes (e.g., general health status, SF-12 physical health, SF-12 mental health, and chronic diseases). Linear regressions were conducted with general health status, SF-12 physical health, and SF-12 mental health as the dependent variable respectively and ALI-Clinical and ALI-Quartile as the independent variable, respectively. Binomial logistic regressions were conducted with chronic diseases as the dependent variable and ALI-Clinical and ALI-Quartile as the independent variable, respectively. We also conducted regressions controlling for socio-demographic variables (e.g., age, education, income, hourly wage, and insurance). Lastly, we conducted t-tests to compare ALI-Clinical and ALI-Quartile scores between hotel housekeepers with high and low stressors and between those with chronic diseases or not. Cohen’s d was also calculated to estimate the effect size. All analyses were conducted using the SPSS software (Version 22.0, IBM, Inc., Armonk, NY).
Results
Feasibility
Study participants were recruited within a period of 6 months. Accessing and recruiting the workers and data collection were successful. The main initial concerns for the participants were related to the blood sample collections. However, given the skills of the research team members, there were no adverse events with blood sample collection. Participants were really pleased to receive their blood test results in the mail, accompanied by a list of local clinics that provided free or sliding scale services. The list also indicated the presence of Spanish-speaking staff. Data collection in participants’ homes and their workplace (when allowed by the manager) were preferred by participants over using the university site location. For example, only three individuals opted to meet at the university satellite option for data collection. Receipt of refreshments after blood specimen collection was also well received.
Socio-demographic characteristics
A total of 49 female hotel housekeepers participated in the study (Table 1). The mean age was 40 years (SD = 11; range = 21–59). The majority (56.3%) reported being Hispanic Latino followed by Black or African American (29.2%). Most (60.4%) were married or partnered. Around 63% were foreign born. More than half of the sample (55%) reported less than high school education. About 37% reported an hourly wage of $10 or less, and about 41% reported an hourly wage of up to $12. More than three-fourths (77%) reported no or partial health benefits from their employer. Around 33% reported experience with smoking and nearly 53% drank alcohol.
Table 1.
Sample characteristics (N = 49).
| N | M± SD/% | Range | |
|---|---|---|---|
| Socio-demographics | |||
| Age | 47 | 40.4 ± 10.5 | 21–59 |
| Marital status | 48 | ||
| Married/Partnered | 29 | 60.4 | |
| Single/Divorced/Widowed | 19 | 39.6 | |
| Race/ethnicity | 48 | ||
| Black or African American | 14 | 29.2 | |
| White | 3 | 6.3 | |
| Hispanic, Latino, Mexican American, Mexican | 27 | 56.3 | |
| American Indian/Alaska Native/Asian | 2 | 4.2 | |
| More than one race | 2 | 4.2 | |
| Foreign born | 49 | ||
| Foreign born | 31 | 63.3 | |
| US born | 18 | 36.7 | |
| Education | 47 | ||
| Some high school but did not graduate or less | 26 | 55.3 | |
| High school graduate or more | 21 | 44.7 | |
| Hourly wage | 49 | ||
| 10 or less | 18 | 36.8 | |
| 10.01–12 | 20 | 40.8 | |
| 12.01–14 | 6 | 12.2 | |
| More than 14 | 5 | 10.0 | |
| Insurance | 48 | ||
| Full insurance | 11 | 28.9 | |
| Partial or no insurance | 37 | 77.1 | |
| Smoking status | 49 | ||
| Currently | 8 | 16.3 | |
| Ex-smoker | 6 | 12.2 | |
| Only smoked a few times | 2 | 4.1 | |
| Never | 33 | 67.3 | |
| Alcohol use | 49 | ||
| 1–2 days per week | 7 | 14.3 | |
| 1–3 days per month | 3 | 6.1 | |
| Less than once per month | 16 | 32.7 | |
| Never | 23 | 46.9 | |
| Stressors | |||
| Number of traumatic events | 49 | 0.9 ± 1.5 | 0–6 |
| At least one traumatic event | 21 | 42.9 | |
| None | 28 | 57.1 | |
| Everyday discrimination | 48 | 2.02 ± 2.59 | |
| High | 25 | 52.1 | |
| Low | 23 | 47.9 | |
| Job strain | 43 | ||
| High | 9 | 20.9 | |
| Low | 34 | 79.1 | |
| Number of rooms cleaned on a normal day | 45 | 14.6 ± 2.7 | 8–21 |
| Health outcomes | |||
| General health status | 49 | ||
| Excellent | 6 | 12.2 | |
| Very good | 7 | 14.3 | |
| Good | 32 | 65.3 | |
| Fair | 2 | 4.1 | |
| Poor | 2 | 4.1 | |
| SF-12 physical health | 49 | 49.3 ± 8.0 | 24.2–60.6 |
| SF-12 mental health | 49 | 48.4 ± 10.5 | 22.4–68.1 |
| Chronic diseases | 49 | 2.2 ± 2.1 | 0–9 |
| ≥1 | 38 | 77.6 | |
| None | 11 | 22.4 |
Health outcomes
Almost 92% of study participants rated their health as being excellent, very good, or good (Table 1). However, the SF-12 instrument indicated that 38% and 39% of the study participants scored below the US population for their physical and mental health, respectively. Chronic conditions were commonly reported, with about 78%, 55%, and 35% reporting one, two, and three chronic conditions, respectively. The chronic conditions included chronic back pain (38.1%), migraine headache (31.7%), diagnosed arthritis (31.7%), diagnosed hypertension (30.2%); frequent or severe headache (26.2%), chronic fatigue (22%), chronic sleeping difficulties (15%), diagnosed high cholesterol (15%), diagnosed asthma (14.6%), chronic neck pain (14.3%), diagnosed diabetes (10%); other chronic pain (9.8%), and congestive heart failure (2.5%).
Stressors
Stressors were categorized as work and nonwork stressors (Table 1). For the work-related stressors, around 21% of participants reported high job strain, and the average number of rooms cleaned on a normal day was 15 (SD = 3; range = 8–21). Regarding nonwork stressors, nearly 43% of participants experienced at least one traumatic event and the average everyday discrimination was 2.02 (SD = 2.59).
Allostatic Load Index (ALI)
For this study, the ALI was comprised of nine biomarkers. Means with standard deviations and the percentages of participants within the risk thresholds of each biomarker are displayed in Table 2. Compared to the high-risk quartile cut-off points, use of the clinical cut-off points resulted in more participants placed within the risk thresholds of CRP, HDL, WHR, and BMI, while fewer participants were within the risk threshold of HbA1c, cortisol, SBP, DBP, and HR. The distributions of the ALI-Clinical and ALI-Quartile scores are shown in Table 3. The mean ALI-Clinical score was 2.3 (SD = 1.3; range = 0-5); while the mean ALI-Quartile score was 2.1 (SD = 1.5; range = 0–7). Using the clinical cut-off points, most participants (34.7%) scored 2. Using the high-risk quartile cut-off points, the largest group (28.6%) also scored 2.
Table 2.
Biomarkers.
| N | M ± SD | Clinical cut-off points |
High risks, n (%) |
High-risk quartile cut-off points |
High risks, n (%) |
|
|---|---|---|---|---|---|---|
| CRP (mg/L) | 49 | 4.2 ± 4.7 | ≥3.0 | 22 (44.9) | >6.8 | 12 (24.5) |
| HDL (mg/dL) | 49 | 58.2 ± 11.9 | <50 | 15 (30.6) | <46.5 | 12 (24.5) |
| HbA1c (ug/mL) | 49 | 633.9 ± 208.6 | ≥1170 | 1 (2.0) | >789.0 | 12 (24.5) |
| Cortisol (ug/dL) | 49 | 15.3 ± 5.3 | >23 | 6 (12.2) | >19.1 | 12 (24.5) |
| SBP (mmHg) | 49 | 124.3 ± 17.9 | >140 | 5 (10.2) | >137.0 | 10 (20.4) |
| DBP (mmHg) | 49 | 77.2 ± 11.6 | >90 | 6 (12.2) | >85.5 | 10 (20.4) |
| HR | 49 | 74.2 ± 10.9 | >100 | 1 (2.0) | >80.5 | 12 (24.5) |
| WHR | 49 | 0.9 ± 0.1 | ≥0.85 | 40 (81.6) | >0.9 | 12 (24.5) |
| BMI | 44 | 29.5 ± 7.1 | ≥30 | 17 (34.7) | >33.4 | 11 (22.4) |
High levels of each biomarker except HDL indicate high risk.
CRP: Serum C-reactive protein; Serum HDL: high density lipoprotein; Serum HbA1c: hemoglobin A1c; Cortisol: Serum Cortisol; SBP: systolic blood pressure; DBP: diastolic blood pressure; HR: heart rate; WHR: waist/hip ratio; BMI: body mass index.
Table 3.
Allostatic load index scores using clinical and high-risk quartile cut-off points.
| ALI-Clinical | N (%) | ALI-Quartile | N (%) |
|---|---|---|---|
| 0 | 4 (8.2) | 0 | 6 (12.2) |
| 1 | 8 (16.3) | 1 | 13 (26.5) |
| 2 | 17 (34.7) | 2 | 14 (28.6) |
| 3 | 12 (24.5) | 3 | 8 (16.3) |
| 4 | 5 (10.2) | 4 | 4 (8.2) |
| 5 | 3 (6.1) | 5 | 3 (6.1) |
| 7 | 1 (2.0) |
ALI-Clinical: allostatic load index score using the clinical cut-off points; ALI-quartile: allostatic load index score using the high-risk quartile cut-off points.
Associations between ALI, stressors, and health outcomes
Correlation analyses (Table 4) showed that high job strain and everyday discrimination were significantly associated with high ALI-quartile score (r = 0.39; P = 0.011; r = 0.41; P = 0.004), while other stressors were not significantly associated with ALI-quartile score (Ps > 0.5). There were no significant correlations between all stressors and ALI-Clinical score (Ps > 0.05). High ALI-quartile score was significantly associated with having at least one chronic disease (r = 0.40; P = 0.005), while it was not related to general health status or SF-12 physical and mental health (Ps > 0.5). No significant correlations were found between ALI-Clinical score and all health outcomes (Ps > 0.05).
Table 4.
Correlations between allostatic load, stressors, and health outcomes.
| ALI-Clinical |
ALI-Quartile |
|||
|---|---|---|---|---|
| r | P | r | P | |
| Job strain | 0.230 | 0.147 | 0.390* | 0.011 |
| Rooms cleaned | 0.056 | 0.713 | −0.077 | 0.615 |
| Everyday discrimination | 0.220 | 0.146 | 0.410** | 0.004 |
| Trauma exposure | 0.140 | 0.332 | 0.140 | 0.341 |
| General health status | 0.055 | 0.708 | 0.250 | 0.082 |
| SF-12 physical health | −0.130 | 0.379 | −0.180 | 0.205 |
| SF-12 mental health | 0.120 | 0.433 | −0.170 | 0.251 |
| Chronic diseases | 0.270 | 0.063 | 0.400** | 0.005 |
ALI-Clinical: allostatic load index scores using the clinical cut-off points; ALI-Quartile: allostatic load index scores using the high-risk quartile cut-off points.
P < 0.05.
P < 0.01.
Linear regressions showed significant association between everyday discrimination with elevated ALI-quartile score (β = 0.36; P = 0.040), but the association became not significant after adjusting for age, foreign born, marital status, education, hourly wage, and insurance (β = 0.15; P = 0.368). The association between high job strain and ALI-quartile score was close to significant (β = 0.28; P = 0.072) and became significant after adjusting for socio-demographic factors (β = 0.30; P = 0.041). Binomial logistic regression showed high ALI-quartile score was associated with increased risk of having at least one chronic disease (OR = 2.73; P = 0.013). The associations remained significant when adjust for socio-demographic factors (P = 0.035). There were no significant associations between ALI-quartile score and any other stressors and health outcomes (Ps > 0.05). No associations were found between ALI-Clinical score and all stressors and health outcomes (Ps > 0.05).
As seen in Table 5, the t-tests showed that hotel housekeepers with high job strain or everyday discrimination had significantly higher ALI-Quartile scores compared with those with low job strain or everyday discrimination (t = 2.31, P = 0.026; t = 2.12, P = 0.040). Job strain and everyday discrimination had medium to large effect sizes on ALI-Quartile scores (Cohen’s d = 0.87; Cohen’s d = 0.61). Though no significant differences were found for ALI-Clinical scores between hotel housekeepers with high and low stressors (Ps > 0.05), job strain and everyday discrimination had small to medium effect sizes on ALI-Clinical scores (Cohen’s d = 0.61; Cohen’s d = 0.35). Hotel housekeepers who had at least one type of chronic diseases had higher ALI-Clinical and ALI-Quartile scores than those without chronic diseases (t = 2.04, P = 0.047; t = 2.64, P = 0.011). The effect sizes for ALI-Clinical and ALI-Quartile scores were medium to large (Cohen’s d = 0.69; Cohen’s d = 0.90).
Table 5.
Comparisons on allostatic load index scores in relation to job strain, everyday discrimination, and chronic diseases.
| Job strain |
Everyday discrimination |
Chronic diseases |
||||
|---|---|---|---|---|---|---|
| High (n = 9) |
Low (n = 34) |
High (n = 25) |
Low (n = 23) |
Yes (n = 38) |
No (n = 11) |
|
| ALI-Clinical | ||||||
| M ± SD | 2.89 ± 1.27 | 2.12 ± 1.27 | 2.56 ± 1.36 | 2.13 ± 1.10 | 2.50 ± 1.27 | 1.64 ± 1.12 |
| t | 1.62 | 1.20 | 2.04 | |||
| P | 0.114 | 0.237 | 0.047 | |||
| Cohen’s d | 0.61 | 0.35 | 0.69 | |||
| ALI-Quartile | ||||||
| M ± SD | 3.11 ± 1.27 | 1.88 ± 1.45 | 2.56 ± 1.71 | 1.65 ± 1.19 | 2.39 ± 1.53 | 1.09 ± 1.04 |
| t | 2.31 | 2.12 | 2.64 | |||
| P | 0.026 | 0.040 | 0.011 | |||
| Cohen’s d | 0.87 | 0.61 | 0.90 | |||
Discussion
Our purpose was to assess feasibility, consider technical issues about measurement of stressors and creation and scoring of an AL index, show test-of-concept, and gather preliminary data among hotel housekeepers. To our knowledge, this is the first study to use an Allostatic load index with biomarkers to explore health risks among this immigrant worker group. Results suggest that such a project is both needed and feasible. Frequent reports of work-related stressors, including high levels of job strain, were found.
These workers are a fairly young group (with a mean age of 40 years). Yet we found frequent reports of chronic conditions such as hypertension, diabetes, high cholesterol, pain, fatigue, and arthritis. Krause and colleagues recently reported high prevalence of hypertension among hotel housekeepers.[44] Previous studies have shown frequent reports of pain.[5,45,46] However, this is the first time that a study reported findings of self-reported history of high cholesterol and arthritis diagnoses among these workers.
Despite the small sample size in this feasibility study, significant associations were found between job strain and everyday discrimination with allostatic load, and between allostatic load with chronic diseases. Job strain and everyday discrimination have medium to large effect sizes on ALI-Quartile scores and small to medium effect sizes on ALI-Clinical scores. And the differences in mean ALI-Clinical and ALI-Quartile scores in hotel housekeepers with and without chronic conditions also reflected medium to large effect sizes. The findings suggested that those female hotel housekeepers with high work and nonwork stressors had elevated physiological dysregulations across multiple body systems. The accumulated multisystem physiological dysregulations could lead to increased risk for having chronic diseases. But the study did not demonstrate the mediating role of AL in the associations between stressors and health outcomes. Future research needs to explore other AL-related stressors that were strongly associated with this population’s poor health outcomes. Additionally, previous studies reported lower AL scores in foreign-born immigrants compared to U.S.-born counterparts and some immigration-related factors such as age upon arrival and length in U.S. residence were associated with AL scores.[47] Given the high proportion of hotel workers who are foreign-born in this study, future research is needed to examine the role of immigration-related factors (i.e., nativity, age upon arrival, time in U.S. residence, and acculturation) in the associations between work-related stressors, allostatic load, and health outcomes among immigrant hotel workers.
The individual biomarkers in the Allostatic load index also showed high risk for disease development. For example, 44.9% of the individuals had CRP levels outside of the normal limits for the clinical cut off point. Also, about 30% indicated cholesterol levels outside of normal limits. Risks for obesity were also observed, with more than 80% outside of normal limit for waist-to-hip ratio, and more than 34% with BMI above that of the general population for the clinical cut point. Larger studies are needed to explore the relationship between stressors and allostatic load among these workers. In addition, no significant differences between the two approaches of allostatic load scoring were found: AL-Clinical and AL-Percentile. This may be due to the small sample size. A larger study is needed to determine differences between these two scoring methods.
Stressors to which these workers are exposed are complex. From a socioecological standpoint, hotel housekeepers may experience stressors across the individual, interpersonal, organizational, and structural/systemic levels. Therefore, it remains challenging to fully capture these stressors in their entirety and determine how they intersect to affect workers’ health. Thus, explorations of these stressors require careful consideration across all aspects of the research methodology (including recruitment, instrumentation, and interpretation). In addition, such complexity warrants the need for both quantitative and qualitative data to gauge the objective and subjective interpretation of stressors and how they affect health. Larger studies are needed to: (1) identify key stressors and comprehend their significant impact on the health of these workers; and (2) compare various factors (e.g., nativity, job description; industry) across different low-wage worker groups. In addition, qualitative inquiries are needed to explore the workers’ perception of stressors and to identify the protective factors that can be strengthened to buffer the effects of stressors.
Limitations
A limitation of this study was that it only focused on women; thus, the study finding cannot be generalized to hotel housemen. More studies are needed to include men, for use in comparisons. Another limitation of the study was our small sample size (N = 49), limiting our ability to make deductions about the relationships between stressors and allostatic load. Many of these limitations can be addressed with a larger sample size.
Acknowledgments
Funding
This study was supported by the Grant or Cooperative Agreement Number, T42 OH008455, funded by the Centers for Disease Control and Prevention. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the Centers for Disease Control and Prevention or the Department of Health and Human Services.
References
- [1].Occupational Safety and Health Administration: "Hotel Housekeeping Safety." Available at https://www.osha.gov/SLTC/etools/hospital/housekeeping/housekeeping.html (accessed 2015).
- [2].Buchanan S, Vossenas P, Krause N, et al. : Occupational injury disparities in the US hotel industry. Am. J. Ind. Med 53(2): 116–125 (2010). [DOI] [PubMed] [Google Scholar]
- [3].Bureau of Labor Statistics: "37-2012 maids and housekeeping cleaners." Available at http://www.bls.gov/oes/current/oes372012.htm (accessed 2017).
- [4].Bureau of Labor Statistics: "Occupational outlook handbook, 2014–15 edition: Maids and housekeeping cleaners." Available at http://www.bls.gov/ooh/building-and-grounds-cleaning/maids-and-housekeeping-cleaners.htm (accesssed 2015).
- [5].Krause N, Scherzer T, and Rugulies R: Physical workload, work intensification, and prevalence of pain in low wage workers: Results from a participatory research project with hotel room cleaners in Las Vegas. Am. J. Ind. Med 48(5): 326–337 (2005). [DOI] [PubMed] [Google Scholar]
- [6].Sanon MA: Hotel housekeeping work influences on hypertension management. Am. J. Ind. Med 56(12): 1402–1413 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Sanon MA: Agency-hired hotel housekeepers: An at-risk group for adverse health outcomes. Workplace Health Saf. 62(2): 81–85 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Krause N, Rugulies R, and Maslach C: Effort-reward imbalance at work and self-rated health of Las Vegas hotel room cleaners. Am. J. Ind. Med 53(4): 372–386 (2010). [DOI] [PubMed] [Google Scholar]
- [9].Rosemberg MA, Ghosh B, Shaver J, Militzer M, Seng J, and McCullagh M: Blood pressure and job domains among hotel housekeepers. J. Health Disp. Res. Pract 11(3): 101–115 (2018). [Google Scholar]
- [10].Department of Industrial Relations: "Issue brief: Workplace injuries in hotel housekeeping in California." 2016. [Google Scholar]
- [11].Frumin E, Moriarty J, Vossenas P, Orris P, Krause N: Workload-related musculoskeletal disorders among hotel housekeepers: Employer records reveal a growing national problem (2006). Available at: http://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.371.7091&rep=rep1&type=pdf. [Google Scholar]
- [12].Hsieh Y-C, Apostolopoulos Y, and Sönmez S: Work conditions and health and well-being of Latina hotel housekeepers. J. Immigr. Minor. Health 18(3): 568–581 (2016). [DOI] [PubMed] [Google Scholar]
- [13].Hsieh Y-CJ, Apostolopoulos Y, Hatzudis K, and Sönmez S: Occupational exposures and health outcomes among Latina hotel cleaners. Hisp. Health Care Int. 12(1): 6–15 (2014). [DOI] [PubMed] [Google Scholar]
- [14].Hsieh Y-CJ, Apostolopoulos Y, and Sönmez S: The world at work: Hotel cleaners. Occup. Environ. Med 70(5): 360–364 (2013). [DOI] [PubMed] [Google Scholar]
- [15].Seifert AM, and Messing K: Cleaning up after globalization: An ergonomic analysis of work activity of hotel cleaners. Antipode 38(3): 557–578 (2006). [Google Scholar]
- [16].Wial H, and Rickert J: US Hotels and Their Workers: Room for Improvement: Working for America Institute, 2002. Available at https://www.hotel-online.com/News/PR2002_3rd/Aug02_HotelJobs.html. [Google Scholar]
- [17].McEwen BS: Stress, adaptation, and disease: Allostasis and allostatic load. Ann. N. Y. Acad. Sci 840(1): 33–44 (1998). [DOI] [PubMed] [Google Scholar]
- [18].Read S, and Grundy E: Allostatic load-a challenge to measure multisystem physiological dysregulation. National Center for Research Methods (NCRM), 2012. Available at: http://eprints.ncrm.ac.uk/2879/1/NCRM_workingpaper_0412.pdf [Google Scholar]
- [19].Seeman TE, Singer BH, Rowe JW, Horwitz RI, and McEwen BS: Price of adaptation—Allostatic load and its health consequences: MacArthur studies of successful aging. Arch. Intern. Med 157(19): 2259–2268 (1997). [PubMed] [Google Scholar]
- [20].de Castro A, Voss JG, Ruppin A, Dominguez CF, and Seixas NS: Stressors among Latino day laborers A pilot study examining allostatic load. AAOHN 58(5): 185 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Schnorpfeil P, Noll A, Schulze R, Ehlert U, Frey K, and Fischer JE: Allostatic load and work conditions. Soc. Sci. Med 57(4): 647–656 (2003). [DOI] [PubMed] [Google Scholar]
- [22].Sun J, Wang S, Zhang J-Q, and Li W: Assessing the cumulative effects of stress: The association between job stress and allostatic load in a large sample of Chinese employees. Work Stress. 21(4): 333–347 (2007). [Google Scholar]
- [23].von Thiele U, Lindfors P, and Lundberg U: Self-rated recovery from work stress and allostatic load in women. J. Psychosom. Res 61(2): 237–242 (2006). [DOI] [PubMed] [Google Scholar]
- [24].Rosemberg MAS, Li Y, and Seng J: Allostatic load: A useful concept for advancing nursing research. J. Clin. Nurs. 26(23–24): 5191–5205 (2017). [DOI] [PubMed] [Google Scholar]
- [25].Beckie TM: A systematic review of allostatic load, health, and health disparities. Biol. Res. Nurs 14(4): 311–346 (2012). [DOI] [PubMed] [Google Scholar]
- [26].Juster RP, McEwen BS, and Lupien SJ: Allostatic load biomarkers of chronic stress and impact on health and cognition. Neurosci. Biobehav. Rev 35(1): 2–16 (2010). [DOI] [PubMed] [Google Scholar]
- [27].Johnson SC, Cavallaro FL, and Leon DA: A systematic review of allostatic load in relation to socioeconomic position: Poor fidelity and major inconsistencies in biomarkers employed. Soc. Sci. Med 192: 66–73 (2017). [DOI] [PubMed] [Google Scholar]
- [28].Seeman M, Merkin SS, Karlamangla A, Koretz B, and Seeman T: Social status and biological dysregulation: The “status syndrome” and allostatic load. Soc. Sci. Med 118: 143–151 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Seeman T, Epel E, Gruenewald T, Karlamangla A, and McEwen BS: Socio-economic differentials in peripheral biology: Cumulative allostatic load. Ann. N. Y. Acad. Sci 1186(1): 223–239 (2010). [DOI] [PubMed] [Google Scholar]
- [30].Seeman TE, Crimmins E, Huang MH, Singer B, Bucur A, Gruenewald T et al. : Cumulative biological risk and socio-economic differences in mortality: MacArthur studies of successful aging. Soc. Sci. Med 58(10): 1985–1997 (2004). [DOI] [PubMed] [Google Scholar]
- [31].McEwen BS: Biomarkers for assessing population and individual health and disease related to stress and adaptation. Metabolism 64(3): S2–S10 (2015). [DOI] [PubMed] [Google Scholar]
- [32].National Institute of Occupational Safety and Health: "Research compendium: The NIOSH Total Worker Health Program: Seminnal Research Papers 2012" U.S. Department of Health and Human Services, Public Health Services, Centers for Disease Control and Prevention, National Institute of Occupational Safety and Health and D. (NIOSH) (eds.). Washington DC, 2012. [Google Scholar]
- [33].National Institute of Occupational Safety and Health: "What is Total Worker Health?" Available at http://www.cdc.gov/niosh/twh/default.html (accessed 2016).
- [34].National Institute of Occupational Safety and Health (NIOSH): "National Occupational Research Agenda (NORA)/national Total Worker Health agenda (2016–2026): A national agenda to advance total worker health research, practice, policy and capacity": Department of Health and Human Services: Centers for Disease Control and Prevention National Institute of Occupational Safety and Health, 2016. [Google Scholar]
- [35].Schill A, and Chosewood C: Total Worker Health®. Workplace Health Safety 64(1): 4–5 (2016). [DOI] [PubMed] [Google Scholar]
- [36].Takahashi H, Yoshika M, and Yokoi T: Validation of two automatic devices for the self-measurement of blood pressure according to the ANSI/AAMI/ISO81060-2:2009 guidelines: The Omron BP765 (HEM-7311-ZSA) and the Omron BP760N (HEM-7320-Z). Vasc. Health Risk Manag 11: 49–53 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Karasek R, Brisson C, Kawakami N, Houtman I, Bongers P, and Amick B: The Job Content Questionnaire (JCQ): An instrument for internationally comparative assessments of psychosocial job characteristics. J. Occup. Health Psychol 3(4): 322 (1998). [DOI] [PubMed] [Google Scholar]
- [38].Siegrist J, Starke D, Chandola T, et al. : The measurement of effort-reward imbalance at work: European comparisons. Soc. Sci. Med 58(8): 1483–1499 (2004). [DOI] [PubMed] [Google Scholar]
- [39].Williams DR: Measuring discrimination resource. Psychology 2(3): 335–351 (1997). [DOI] [PubMed] [Google Scholar]
- [40].Gray MJ, Litz BT, Hsu JL, and Lombardo TW: Psychometric properties of the life events checklist. Assessment 11(4): 330–341 (2004). [DOI] [PubMed] [Google Scholar]
- [41].Brazier JE, and Roberts J: The estimation of a preference-based measure of health from the SF-12. Med. Care 42(9): 851–859 (2004). [DOI] [PubMed] [Google Scholar]
- [42].Ware JE, Kosinski M, and Keller SD: A 12-item short-form health survey: Construction of scales and preliminary tests of reliability and validity. Med. Care 34(3): 220–233 (1996). [DOI] [PubMed] [Google Scholar]
- [43].Ware JE: The SF-12v2TM how to score version 2 of the SF-12® health survey:(With a supplement documenting version 1): Quality Metric, 2002. [Google Scholar]
- [44].Krause N, and Arias OE: Disparities in prevalence, treatement, and control of hypertension among low wage immigrant workers beyond health insurance coverage: The Las Vegas hotel room cleaners blood pressure study. J. Hypertens. Manag 1: 003 (2015). [Google Scholar]
- [45].Burgel BJ, White MC, Gillen M, and Krause N: Psychosocial work factors and shoulder pain in hotel room cleaners. Am. J. Ind. Med 53(7): 743–756 (2010). [DOI] [PubMed] [Google Scholar]
- [46].Scherzer T, Rugulies R, and Krause N: Work-related pain and injury and barriers to workers’ compensation among Las Vegas hotel room cleaners. Am. J. Public Health 95(3): 483 (2005). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Doamekpor LA, and Dinwiddie GY: Allostatic load in foreign-born and US-born blacks: Evidence from the 2001-2010 National Health and Nutrition Examination Survey. Am. J. Public Health 105(3): 591–597 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]