Abstract
Shlezinger et al. (Reports, 8 September 2017, p. 1037) report that the common fungus Aspergillus fumigatus, a cause of aspergillosis, undergoes caspase-dependent apoptosis-like cell death triggered by lung neutrophils. However, the technologies they used do not provide reliable evidence that fungal cells die via a protease signaling cascade thwarted by a fungal caspase inhibitor homologous to human survivin.
Shlezinger et al. (1) reported the existence of an “apoptosis-like” programmed death pathway in the opportunistic pathogen Aspergillus fumigatus, a multicellular fungus responsible for life-threatening infections. However, this conclusion is compromised by several technical problems with their methods. These arise from the use of mammalian apoptosis assays designed to detect biochemical events that are not present or molecularly defined in fungi. A related problem stems from the assumption that fungal proteins with limited sequence homology to mammalian apoptosis regulators will function analogously in fungal cells. In this study, a chemical sensor and a small-molecule inhibitor of mammalian apoptosis regulators [caspases and the IAP (inhibitor of apoptosis) family of proteins, respectively] were applied to fungal cells with the expectation of binding to distant fungal homologs but without direct evidence for such. Furthermore, the proposed fungal target proteins (metacaspases and BIR1) appear to lack the corresponding binding sites for these chemical reagents. Thus, the evolutionary divide between fungi and mammals appears to be too great for what might seem like a safe extrapolation regarding apoptosis—generally defined in mammals as the classic biochemical and morphological consequence of caspase-3 or −7 activation.
Using a transgenic strain of A. fumigatus with a dual fluorescent probe to distinguish dying cells from dead cells, Shlezinger et al. report that mold conidia exposed to oxidative stress in vitro, or engulfed by neutrophils in vivo, exhibit features of apoptotic mammalian cells prior to loss of viability. The authors measured fungal caspase activity by flow cytometry or fluorescence microscopy using fluorescein isothiocyanate (FITC)–conjugated tripeptide Val-Ala-Asp (VAD) fused to fluoro-methylketone (FMK). FITC-VAD-FMK is a mammalian caspase reporter that mimics the required Asp cleavage site found in natural substrates of mammalian caspases. The FMK moiety results in tight binding to the caspase active-site cysteine, potently inhibiting caspase activity. By binding to active caspases, the fluorescent FITC moiety is retained in animal cells for easy detection.
However, despite careful scrutiny, sequence-based bioinformatics approaches have failed to detect caspase homologs in fungal genomes, or more generally in nonmetazoan organisms (2). A. fumigatus encodes two metacaspases (CasA and CasB) (3), which are also cysteine proteases related to animal caspases. However, metacaspases cleave their substrates after Arg and Lys, rather than Asp (4), the key residue in FITC-VAD-FMK. This raises a critical question: What enzymatic activities are responsible for the FITC-VAD-FMK caspase reporter activity in dying fungi? One possibility is that peptide-FMK reporters are promiscuous. They have been reported to bind or inhibit other classes of cysteine proteases in mammalian cells including cathepsins (5), and for these reasons have fallen from favor for use in mammalian models (6). Similarly, FITC-VAD-FMK could potentially monitor vacuolar cathepsins in fungi, but it can also nonspecifically label living nonpermeabilized yeast cells (7). Given its promiscuity, FITC-VAD-FMK could theoretically bind fungal metacaspases. However, although a double knockout of both A. fumigatus metacaspases CasA and CasB exhibited cell growth abnormalities, it was not resistant to cell death induced by oxidative stress or other stimuli tested (3).
Shlezinger et al. took a different approach to address a causal role for fungal caspase-like activities, leading to the identification of a virulence mechanism. They found that fungal strains overexpressing A. fumigatus BIR1 (AfBIR1) are resistant to oxidative stress (H2O2) in vitro and are more virulent in mice. AfBIR1 shares amino acid sequence similarity to a family of mammalian IAP proteins that, like AfBIR1, contain baculovirus IAP repeat (BIR) domains. The authors’ proposed model suggests that AfBIR1 behaves similarly to the human IAP protein survivin, based on the assumption that survivin inhibits apoptotic caspases. However, survivin is not a caspase inhibitor and it lacks the sequences found in the BIR region of mammalian XIAP and Drosophila IAP1 that directly inhibit caspases (8, 9). To provide evidence that endogenous AfBIR1 regulates caspase-like activity while over-coming the lethality caused by AfBIR1 deletion, Shlezinger et al. sought to inhibit AfBIR1 by treating fungal conidia and mice with S12, a small molecule reported to inhibit survivin (10). S12 was originally identified through chemical and computational screens for compounds that target a cavity located near the survivin dimerization interface. However, residues critical for S12 binding to survivin are not well conserved in AfBIR1 (Fig. 1).Thus, studies to verify direct binding of S12 to AfBIR1 are needed, as their interaction cannot be inferred solely on the basis of multiple sequence alignments.
Fig. 1. Amino acid residues in the single BIR domain of human survivin (BIRC5) required for binding S12 are not well conserved in either of the BIR domains of AfBIR1.
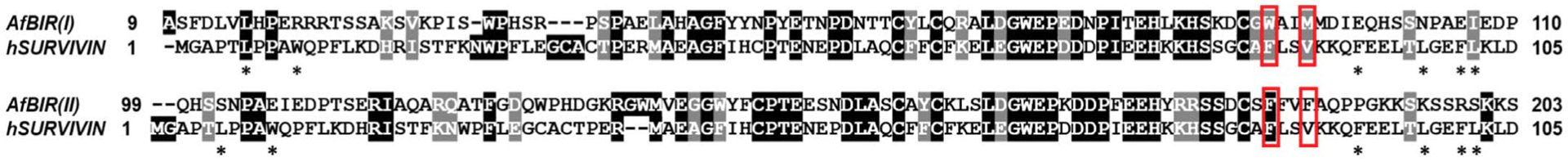
Human survivin (NP_001159) is aligned using ClustalW to both BIR domains of A. fumigatus BIR1 (XP_752777). Disruption of either Phe86 or Val89 (red frames) in survivin inhibits S12 binding; asterisks mark residues forming the interface between survivin dimers (10). Amino acid abbreviations: A, Ala; C, Cys; D, Asp; E, Glu; F, Phe; G, Gly; H, His; I, Ile; K, Lys; L, Leu; M, Met; N, Asn; P, Pro; Q, Gln; R, Arg; S, Ser; T, Thr; V, Val; W, Trp; Y, Tyr.
The other hallmark of mammalian apoptosis used throughout the Shlezinger et al. study is nuclear DNA fragmentation, which is quantified using TUNEL (terminal deoxynucleotidyl transferase–mediated deoxyuridine triphosphate nick end labeling) assays. The TUNEL assay is useful for labeling the new ends of nuclear DNA after caspase-dependent activation of the mammalian DNase CAD (caspase-activated deoxyribonuclease) (11). However, the TUNEL assay is not specific to apoptosis and detects DNA breaks resulting from nonapoptotic cell death (12). DNA fragmentation and many other features of dying mammalian cells have been observed in a diverse range of nonmetazoan taxa, including protists, microalgae, yeast, bacteria, and plants. However, the genes directly responsible are largely unknown. Thus, the central unanswered question is whether the fungal factors responsible for TUNEL reactivity, caspase-like activity, or other mammalian readouts play an active and causal role in fungal cell death, or whether they only serve to mark dead and dying cells with degrading DNA, vacuolar permeability, and depletion of ATP.
Shlezinger et al. provide convincing genetic arguments that host phagocyte NOX [reduced nicotinamide adenine dinucleotide phosphate (NADPH) oxidase] mediates the demise of ingested fungal conidia. The possibility that a NOX-derived reactive oxygen species induces a FITC-VAD-FMK–traceable signal modulated by AfBIR is also intriguing, but more evidence will be required to distinguish this model from other possibilities, including direct killing of the engulfed pathogens by neutrophils without pro-death contributions from fungal “caspase-like activities.” Some fungal species have orthologs of the mammalian necroptosis mediator MLKL or the mammalian pyroptosis mediator DNFA5/gasdermin (13, 14). Even if these pro-necrotic death factors also do not promote regulated death pathways in fungi, this does not deny the existence of genetically controlled fungal cell death, especially in fungi with elaborate morphological forms (15).
ACKNOWLEDGMENTS
Funding: Supported by the Fondation ARC and the Ligue Contre le Cancer Comité du Gard (A.A.); NIH grants RO1 NS083373, R21 NS096677, and RO1 GM077875 (J.M.H.); NIH grant R21 AI115016 (K.W.C.); and the CZ.1.05/1.1.00/02.0109 BIOCEV by ERDF and MEYS (Z.P. and L.V.).
Footnotes
Competing interests:
We declare no competing interests.
REFERENCES AND NOTES
- 1.Shlezinger N et al. , Science 357, 1037–1041 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bell RAV, Megeney LA, Cell Death Differ. 24, 1359–1368 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Richie DL et al. , Mol. Microbiol 63, 591–604 (2007). [DOI] [PubMed] [Google Scholar]
- 4.Bouvier LA, Niemirowicz GT, Salas-Sarduy E, Cazzulo JJ, Alvarez VE, FEBS J. 285, 1097–1110 (2018). [DOI] [PubMed] [Google Scholar]
- 5.Rozman-Pungerčar J et al. , Cell Death Differ. 10, 881–888 (2003). [DOI] [PubMed] [Google Scholar]
- 6.Poreba M, Strózyk A, Salvesen GS, Drag M, Cold Spring Harb. Perspect. Biol 5, a008680 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Váchová L, Palková Z, FEMS Yeast Res. 7, 12–21 (2007). [DOI] [PubMed] [Google Scholar]
- 8.Chai J et al. , Cell 104, 769–780 (2001). [DOI] [PubMed] [Google Scholar]
- 9.Riedl SJ et al. , Cell 104, 791–800 (2001). [DOI] [PubMed] [Google Scholar]
- 10.Berezov A et al. , Oncogene 31, 1938–1948 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Enari M et al. , Nature 391, 43–50 (1998). [DOI] [PubMed] [Google Scholar]
- 12.Grasl-Kraupp B et al. , Hepatology 21, 1465–1468 (1995). [DOI] [PubMed] [Google Scholar]
- 13.Daskalov A et al. , Proc. Natl. Acad. Sci. U.S.A 113, 2720–2725 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gregan J, Van Laer L, Lieto LD, Van Camp G, Kearsey SE, Biochim. Biophys. Acta 1638, 179–186 (2003). [DOI] [PubMed] [Google Scholar]
- 15.Gonçalves AP, Heller J, Daskalov A, Videira A, Glass NL, Front. Microbiol 8, 1837 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]


