Abstract
Background: Despite recent widespread acceptance that unmet social needs are critically relevant to health, limited guidance exists about how best to address them in the context of women's health care delivery. We aimed to evaluate two interventions: enhanced screening and referral (ESR), a screening intervention with facilitated referral and follow-up calls, and personalized support for progress (PSP), a community health worker intervention tailored to women's priorities.
Materials and Methods: Women >18 years were screened for presence of elevated depressive symptoms in three women's health clinics serving primarily Medicaid-eligible patients. If eligible and interested, we enrolled and randomized women to ESR or PSP. Pre- and postintervention assessments were conducted. Primary outcomes were satisfaction, depression, and quality of life (QOL). Planned analyses of subgroup differences were also explored.
Results: A total of 235 participants were randomized; 54% identified as African American, 19% as White, and 15% as Latina. Participant mean age was 30 years; 77% reported annual incomes below US $20,000/year; and 30% were pregnant at enrollment. Participants in both arms found the interventions satisfactory and improved for depression (p < 0.001). There were no differences between groups for the primary outcomes. Subgroups reporting greater improvement in QOL in PSP compared with ESR included participants who at baseline reported anxiety (p = 0.05), lack of access to depression treatment (p = 0.02), pain (p = 0.04), and intimate partner violence (p = 0.02).
Conclusions: Clinics serving women with unmet social needs may benefit from offering PSP or ESR. Distinguishing how best to use these interventions in practice is the next step.
Keywords: depression, social needs, prioritization, social determinants of health, patient-centered care
Introduction
Many women with unmet social needs describe depression as due to life circumstances rather than a health condition to be treated.1–5 Moreover, evidence is mounting that we must address unmet social needs as part of health care to reduce inequities in health.6–8 Meanwhile, depression is a leading cause of disability in the United States, affecting women twice as often as men,9 is considered the most common complication of childbirth,10 and further doubled among women affected by poverty.11 We know the de facto site of depression care for many women living in poverty is women's health clinics.12–14
Yet women's health care tends to be delivered in a standardized way without incorporating individual-level differences.15,16 Addressing the individual needs of women with unmet social needs and depression in the context of their care is demanding because of the social and psychological barriers and health comorbidities many women face, such as poor housing conditions, lack of social support, trauma experience, and health difficulties.17–20
This trial evaluated two innovative and patient-centered approaches recommended by our community advisory board (CAB) to address the needs of women with social needs and depression by literally, and figuratively, meeting them where they were, providing additional support, and incorporating their priorities and lived contexts and experiences. Our goal was to determine if women with unmet social needs and depression would improve for two outcomes identified by our CAB, depression and quality of life (QOL), in the context of their women's health care delivery.
We conducted a comparative effectiveness trial of two interventions: personalized support for progress (PSP), a community health worker (CHW) intervention tailored to women's priorities and social context; and enhanced screening and referral (ESR), a lower intensity intervention providing a personalized resource list and modest social support.21 Both study arms offered patient-centered support, a focus on unmet social needs, and assistance reducing barriers related to depression treatment engagement. Our hypotheses were that both interventions would be satisfactory and effective, and that PSP would be more satisfactory and more effective for reducing depression and improving QOL than ESR. Planned exploratory hypotheses were that the relative higher intensity of PSP would be particularly helpful compared with ESR for specific high-risk subgroups of women, including those coping with intimate partner violence (IPV), anxiety, alcohol abuse, physical health function difficulties, pain, negative attitudes toward depression treatment, and low perceived competence.
Materials and Methods
Development of study protocol
Using community-based participatory-based research principles,22 this comparative effectiveness trial was designed with active participation of a CAB of stakeholders.23 Patient partners were women's health patients with life experiences such as unmet social needs, depression, and challenges such as IPV. Women's health clinician partners were physicians, nurses, and psychotherapists who worked directly with women who have depression and unmet social needs, as well as policy makers and insurers. The CAB aimed to establish patient-driven, effective, generalizable, and scalable interventions to reduce health and social inequities. The CAB met throughout the project to select study arms and outcomes, discuss study progress, recommend protocol changes, and advise on implementation and dissemination strategies.
Study design
Screening and assessment
Research assistants screened for depression in the waiting rooms of three urban women's health clinics that provide care to women, many of whom were from the poorest zip codes in Rochester, NY.24,25 We invited women with elevated depressive symptoms to be assessed for study eligibility, and if eligible and consented, to complete the remaining questionnaires. Enrolled participants completed measures pre- and postintervention. Research assistants were masked to intervention assignment. If there were missing data, scale scores were computed if 80% or more of the items were completed.
Patient Satisfaction was measured with the Client Satisfaction Questionnaire,26 an eight-item instrument assessing subjective satisfaction with the intervention (1 = excellent, 2 = good, 3 = fair, 4 = poor) completed at postintervention phase only. Depression was measured with the patient health questionnaire (PHQ)-9,27 a nine-item depression screening tool with good discriminant validity for major depressive disorder and sensitivity to change (total scores range from 0 to 27. Scores of PHQ-9 ≥ 10 suggest moderate-to-severe depression; baseline Cronbach's alpha = 0.54, although scores at baseline were truncated since all participants had to score greater than or equal to 10 to participate in the study; α = 0.88 at post).28,29 The PHQ-9 is validated in women's health settings, with pregnant30 and postpartum31 women, and with women of color.32 The abbreviated World Health Organization Quality of Life (WHOQOL)33 was used to assess overall QOL. It includes four summary scales: physical (baseline α = 0.79), psychological (baseline α = 0.80), social (baseline α = 0.63), and environmental (baseline α = 0.71), plus a total score (baseline α = 0.88). All scores are ranging 0–100 (the higher score, the better QOL), and the measure has been validated for women following childbirth.34
Moderators of intervention outcomes included self-reported IPV on the Feldhaus Partner Violence Screen (a three-item measure about past physical violence, and perceived personal safety in relationship; 0 = no partner violence; ≥1 = partner violence),35,36 general anxiety disorder (GAD) on the GAD-7 (a seven-item screening tool for GAD with scores ranging from 0 to 21; a score of ≥10 suggesting presence of GAD; baseline α = 0.88),37,38 alcohol abuse on the Alcohol Use Disorders Identification Test (AUDIT-C) (a three-item screen to identify possible alcohol use disorder, with maximum score of 12; in women a score of ≤3 might indicate problematic drinking; baseline α = 0.85),39–41 pain measured by the sum of pain intensity (0–10) and pain interference (0–10) in the past week (adapted from the Brief Pain Inventory42,43; baseline α = 0.92), physical health function on the World Health Organization Disability Assessment Schedule 2.0 (WHODAS) (12-item measure assessing six domains of disability: mobility, cognition, self-care, getting along, life activities, and participation. It generates a total score 0–100; 0 = no disability, 100 = full disability; baseline α = 0.87),44,45 attitudes toward depression treatment on the Patients Attitudes Toward and Ratings of Care for Depression (a 16-item measure generating six domains, four of which were used in the current study: treatment effectiveness [baseline α = 0.70]; treatment problems [baseline α = 0.60]; patients' need for education, information, and understanding regarding depression [baseline α = 0.67]; and financial access to services [baseline α = 0.54]),2,46 Perceived Competence Scale (four-item measure with scores ranging 4–28, where higher score indicates higher competence, baseline α = 0.87),47 assessing the competence component of self-determination theory, and the Social Needs Questionnaire (α = 0.68). The Social Needs Questionnaire was created for this study due to a lack of an existing well-validated measure in the literature at the time, and evaluated social needs identified as important in focus groups, including stable housing, food scarcity, clothing, transportation, and legal needs (e.g., I have enough food in the house: not at all true, somewhat true, mostly true, or very true).
Interventions
We randomized participants to either PSP or ESR. PSP builds on Self Determination Theory,48 and aims to facilitate women's experiences of autonomy, competence, and relatedness to empower them to meet their prioritized needs. To accomplish this, women partner with a CHW who provides tailored support and empowerment to address identified priorities. The CHW's first goal was to guide women through a computer-based card-sorting task to help the patient and CHW create a personalized care plan, outlining the steps that might be taken toward addressing the identified priorities. The CHW then provided up to 4 months of services to implement the plan. The frequency and type of contact were patient driven and ranged from monthly phone calls and texts to weekly home or community visits.
Initial PSP appointments, including completion of the card sort and plan, were video recorded. Two independent research assistants viewed and rated 30% (n = 30) of the appointments using our PSP Fidelity Checklist, created and piloted by our team. To ensure interrater reliability, the first 10 of these were independently rated by both research assistants. For the 10 tapes rated by both, interrater reliability was good for both adherence (intraclass correlation coefficient = 0.93; weighted kappa = 0.76) and competency (intraclass correlation coefficient = 0.89; weighted kappa = 0.72), so the remainder were reviewed by just one rater.
The participants assigned to ESR received a resource list with information specifying where they might obtain assistance based on their responses and assistance with connecting with these resources if desired. Participants then received monthly phone calls over the 4-month intervention period to provide support and see if they desired assistance connecting with any resources.
Data analysis plan
We randomized participants using a simple 1:1 randomized design to assign intervention arm using a random number generator, stratified on clinic and pregnancy status. The active intervention phase lasted 4 months. Participants completed follow-up assessments immediately postintervention, and at 3- and 6-months following the end of the intervention phase. Only results from the postintervention assessment are reported in this article. Institutional Human Subjects Review Board approval was obtained before implementation of the study. Poleshuck et al. provide further detail elsewhere.21
To assess the impact of PSP compared with ESR on the main outcomes, we used a general linear model approach (analysis of covariance). To improve precision and statistical power,49,50 we entered stratification (site, pregnancy status), characteristic differences found at baseline, and the baseline value of the dependent variable of interest as covariates in the models tested, when available. In this study, a full-information maximum likelihood approach was undertaken to account for missing covariate data. We considered impact estimates with p-values <0.05 (two-tailed tests) statistically significant.
We followed an intent-to-treat framework51,52 to estimate the average impact of PSP, relative to the ESR group, on patient satisfaction, depression, and QOL. We also examined moderators of intervention effects to determine which subgroups might better respond to either of the intervention approaches. Any and all heterogeneity of intervention effects were undertaken under an exploratory, hypothesis-generating approach to better understand which, if any, characteristics moderate intervention effects.53 We used procedures outlined by Aiken and West54 to minimize problems associated with multicollinearity. We computed multiplicative terms by first centering each continuous predictor variable and then forming the product term using the centered continuous predictor(s) of interest multiplied by experimental condition. Where significant interaction effects were noted, we graphically examined the results by plotting the continuous moderation variable at both high (+1 standard deviation [SD] from the mean) and low (−1 SD) values for each experimental condition (PSP/ESR).55 Effect sizes (ESs) were also examined, based on marginal means at both high (+1 SD from the mean for continuous moderator variables) and low (−1 SD from the mean) values of continuous moderation variables.
Study sample
Study inclusion criteria included being an active patient in one of three women's health clinics, ≥18 years, PHQ-9 score ≥10 indicating moderate or greater depressive symptoms, living within a prescribed geographic area, and speaking English. Exclusion criteria included current involvement with a CHW or case manager, significant cognitive impairment, active substance use disorder or active psychosis on the Mini-International Neuropsychiatric Interview,56 and imminent suicidal risk. Given the naturalistic approach to maximize generalizability of findings, women could be using antidepressants or engaged in psychotherapy, as long as they had elevated depressive symptoms suggesting inadequate response to treatment.
Based on power analysis, a sample size of 100 per group (n = 200) was planned to compare the two interventions for the primary outcomes. We were interested in the power of intervention status to detect differences in satisfaction, depression, and QOL. Within this regression framework, sample size must be specified (n = 200 completers), the total amount of variance must be specified, alpha must be specified (α = 0.05), and the variance explained without intervention status must be specific (i.e., variance explained by covariates). In our expected scenario for depression and QOL variables, we expected total variance explained to equal 35 and the variance explained by time 1 covariate(s) to equal 0.30, leaving 5% explained by intervention status which translates to a Cohen's d = 0.46,57,58 power = 0.97 to detect these differences. Reducing total variance explained to 0.23 and variance explained by time 1 covariates to 0.20 results in a power estimate of 0.79 (Cohen's d = 0.35). Because we exceeded recruitment goals, we attained sufficient power for the aims of the study.
Results
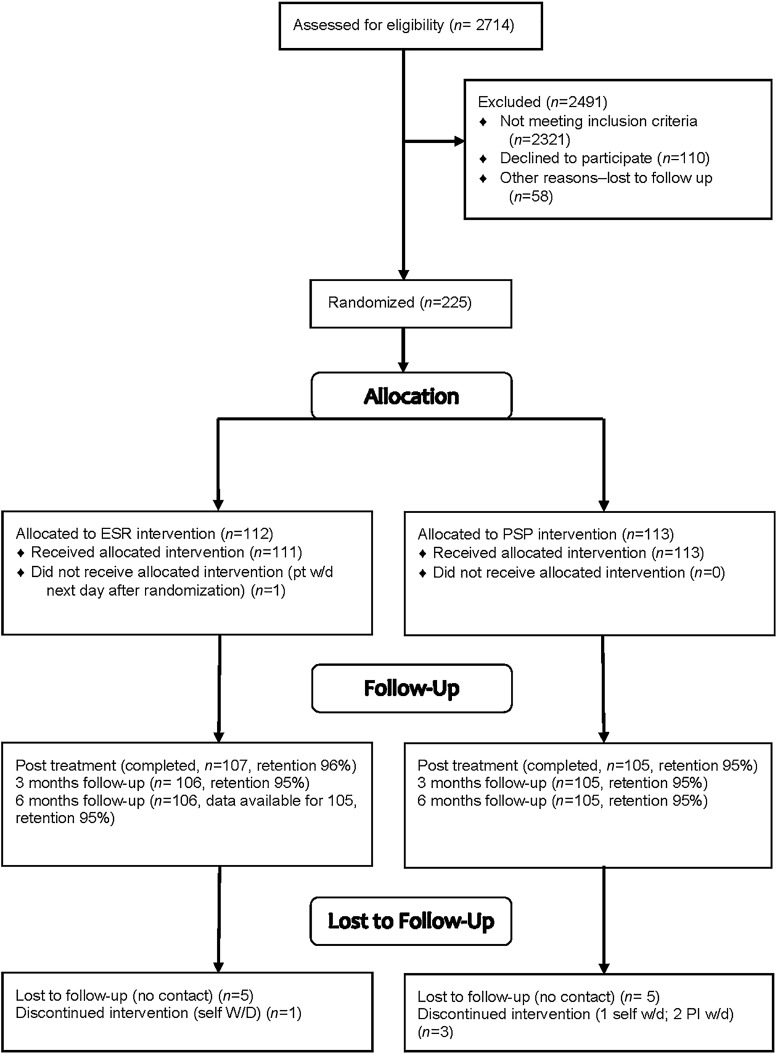
In 22 months (from January 2014 to October 2015), we approached women in clinic waiting rooms 9,562 times with a request to complete screening. In total, we initiated 4,035 (42% of approaches) screens, and 2,714 (67%) screens were sufficiently completed (defined as completing at least PHQ-9) before women were called back for their appointments. Of those screened, 423 (15.6%) had elevated depressive symptoms and 322 (76.1%) of those participants signed informed consent. Of those consented, we lost 58 to follow-up before baseline assessment/randomization, 30 did not meet final eligibility criteria based on further screening due to not being patient at the clinic (n = 5), reporting active psychotic symptoms (n = 8), active alcohol, or substance dependence (n = 5) or current involvement with case management or CHW (n = 12), and 9 withdrew. We randomized 225 women. For analyses, we combined the randomization by two of the clinics to one site because they were in the same site, and the number of participants at each of these clinics was small (13 for one clinic and 22 for the second). We withdrew two women from the final analyses due to later discovering they did not in fact meet eligibility criteria at baseline (one for active psychosis and one for already working with a CHW), leaving a total of 223 women in the final sample (Fig. 1). Retention at the postintervention follow-up was 212 (95%). Measures were completed independently in the office, unless a participant needed them read aloud.
FIG. 1.
Consort chart.
Our sample of 223 women included 137 (61.4%) Black/African American, 53 (23.8%) White/Caucasian, 43 (19.3%) Latina/Hispanic, and 12 (5.3%) reporting other race (Native American, Asian, Pacific Islander, and other) on self-reported Race/Ethnicity (women selected all that applied, thus totals are >100%). Mean age was 30.1 years (SD = 9.50), with an average of 1.3 children under the age of 18 living with them (range 0–5; SD = 1.3); 67 (30.0%) were pregnant at the time of enrollment. In terms of marital status, 159 (71.3%) were single, divorced, or widowed and 64 (28.7%) were married/living with a partner. Most women (163; 73.1%) reported a total household income of <$20,000. Rates of unmet social needs were as follows: 107 (48%) food scarcity; 109 (48.9%) lack of transportation; 112 (50.2%) insufficient clothing; 77 (34.5%) unsafe housing; 103 (46.2%) unstable housing; and 55 (24.7%) lack of access to a working phone; totaling 168 (75.3%) reporting ≥1 social need. A total of 149 (66.8%) reported elevated anxiety (GAD-7 ≥ 10), 56 (25.8%) reported IPV in the past year, and 42 (18.9%) reported problematic alcohol use.
We assessed randomization balance for demographics and baseline variables, using a conservative p-value of ≤0.20 given our interest was in establishing similarity as opposed to differences. We found no group differences in the categorical variables of site, pregnancy status, race/ethnicity, marital status, insurance status, illicit substance use, behavioral health treatment engagement (psychotherapy and/or antidepressants), presence of unmet social needs, or IPV. There were, however, significant differences in full-time employment status across the groups (χ2 = 10.53, p = 0.001) with more PSP women working full time. In terms of continuous variables, we noted baseline differences in social QOL (t = 2.15, p = 0.033) and disability (t = −2.01, p = 0.039) with ESR having a lower social QOL and being more disabled. Finally, number of children (t = −1.79, p = 0.074), depression (t = −1.52, p = 0.131), physical QOL (t = 1.29, p = 0.198), psychological QOL (t = 1.58, p = 0.116), and the total QOL score (t = 1.41, p = 0.160), each met the criterion of a p-value <0.2. The ESR group had more children, reported higher depression scores and lower QOL in all domains. We used the QOL total score at baseline as a covariate in all subsequent analyses, as well as the baseline number of children, depression, disability score, and full-time employment indicator. Stratification indicator variables (site and pregnancy status) were also included as covariates.
We examined intervention effects on our three main outcomes: satisfaction, depression, and QOL. Participants in both intervention groups described the interventions as highly satisfactory across the four questions asked with no between-group differences in satisfaction (Table 1). Most women were satisfied with the ESR and PSP interventions (>75% responded good or excellent to each question). Women in both intervention groups showed improvement for depression (PSP change on PHQ-9 = −3.33 points, n = 105, t = −5.24, p < 0.001, d = −0.50; ESR change = −2.33, n = 107, t = −3.93, p < 0.001, d = −0.38). There were no significant pre–post changes for QOL in either group. We did not find significant intervention effects between groups for either depression or QOL.
Table 1.
Table of Primary Outcomes
| Primary outcomes | PSP |
ESR |
|
|
|
||||
|---|---|---|---|---|---|---|---|---|---|
| N | Mean | SD | N | Mean | SD | t | p | ES | |
| Depression (PHQ-9) | |||||||||
| Baseline | 111 | 13.92 | 3.78 | 112 | 14.74 | 4.21 | −1.517 | 0.131 | −0.203 |
| Posttreatment | 105 | 10.61 | 6.43 | 107 | 12.58 | 6.56 | −1.192 | 0.233 | −0.136 |
| Quality of life—physical | |||||||||
| Baseline | 111 | 49.24 | 20.39 | 112 | 45.70 | 20.64 | 1.291 | 0.198 | 0.173 |
| Posttreatment | 105 | 52.72 | 20.39 | 107 | 49.13 | 19.509 | −0.076 | 0.939 | −0.008 |
| Quality of life—psychological | |||||||||
| Baseline | 111 | 50.94 | 17.98 | 112 | 46.99 | 19.29 | 1.580 | 0.116 | 0.212 |
| Posttreatment | 105 | 55.14 | 18.86 | 107 | 50.20 | 21.69 | 0.107 | 0.915 | 0.010 |
| Quality of life—social | |||||||||
| Baseline | 111 | 56.41 | 22.21 | 112 | 49.87 | 23.30 | 2.148 | 0.033 | 0.288 |
| Posttreatment | 105 | 57.42 | 23.28 | 107 | 50.18 | 23.52 | 0.608 | 0.543 | 0.071 |
| Quality of life—environmental | |||||||||
| Baseline | 111 | 56.64 | 15.98 | 112 | 55.30 | 15.24 | 0.639 | 0.052 | 0.086 |
| Posttreatment | 105 | 59.43 | 15.82 | 107 | 56.80 | 18.05 | −0.074 | 0.941 | −0.008 |
| Quality of life—total | |||||||||
| Baseline | 111 | 79.51 | 13.82 | 112 | 76.91 | 13.70 | 1.411 | 0.160 | 0.189 |
| Posttreatment | 105 | 82.70 | 14.14 | 107 | 78.85 | 15.57 | 0.499 | 0.618 | 0.049 |
| Client satisfaction (at posttreatment only) | |||||||||
| How would you rate the quality of services you have received?a | 105 | 1.43 | 0.65 | 106 | 1.57 | 0.65 | −1.396 | 0.163 | −0.195 |
| To what extent has our program met your needs?b | 105 | 1.88 | 0.87 | 107 | 2.00 | 0.88 | −0.494 | 0.621 | −0.067 |
| Have the services you received helped you to deal more effectively with your problems?c | 105 | 1.71 | 0.74 | 107 | 1.80 | 0.64 | −0.121 | 0.904 | −0.016 |
| In an overall, general sense, how satisfied are you with the service you have received?d | 105 | 1.61 | 0.77 | 107 | 1.71 | 0.76 | −0.209 | 0.834 | −0.028 |
All models statistically control for baseline value of the dependent variable as well as number of children in household, full-time employment status, baseline depression (PHQ9), disability (WHODAS), and quality of life (WHOQOL-Total) as well as stratification variables (site and pregnancy status). All heterogeneity of treatment effects analyses were examined at the posttreatment assessment only.
Scored 1 = excellent; 2 = good; 3 = fair; 4 = poor.
Scored 1 = almost all of my needs have been met; 2 = most of my needs have been met; 3 = only a few of my needs have been met; 4 = none of my needs has been met.
Scored 1 = yes, they helped a great deal; 2 = yes, they helped somewhat; 3 = no, they did not really help; 4 = no, they seemed to make things worse.
Scored 1 = very satisfied; 2 = mostly satisfied; 3 = indifferent, or mildly dissatisfied; 4 = quite dissatisfied.
ESR, enhanced screening and referral; PSP, personalized support for progress; M, mean; SD, standard deviation; ES, effect size (Cohen's d); PHQ, patient health questionnaire.
In planned exploratory moderator analysis, we determined if the following moderated intervention effects: (i) baseline social barriers (IPV, social needs, available financial resources for treatment), (ii) baseline psychological barriers (perceptions of depression treatment effectiveness, perceived competence), and (iii) baseline health comorbidities (disability, anxiety, pain, alcohol use).
Heterogeneity and social barriers
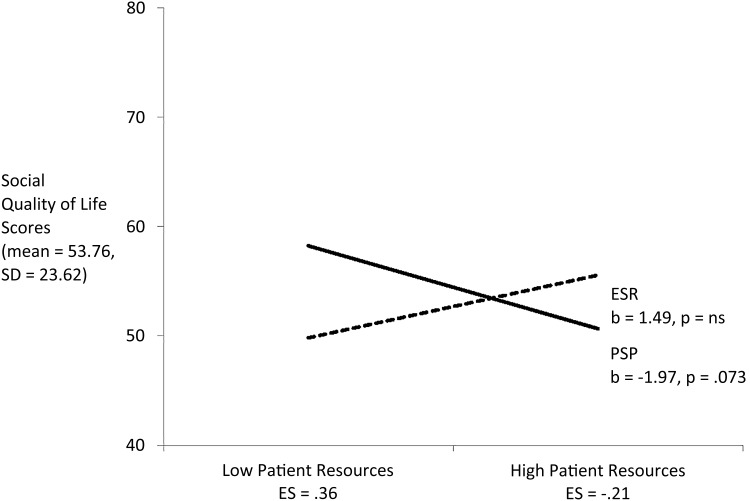
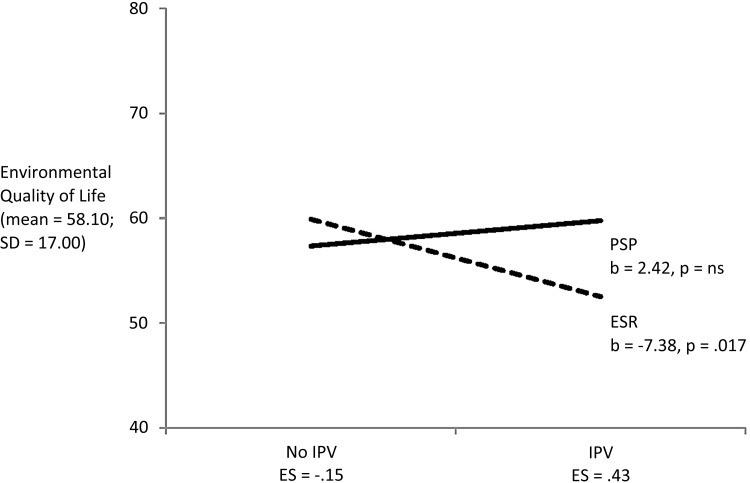
Findings suggested those with greater baseline social barriers, such as IPV and lack of financial resources to engage in depression treatment, had better outcomes with PSP compared with ESR. Baseline perceived lack of financial resources to afford depression treatment moderated the effect of PSP on postintervention Social QOL (t = −2.431, p = 0.015; Fig. 2). Women with high perceived financial resources for depression treatment had better response with ESR (ES = 0.36), whereas women with low baseline levels of perceived financial resources had better response with PSP women (ES = −0.21). Baseline IPV status moderated the effect of the interventions for Environmental QOL (t = 2.35, p = 0.019; Fig. 3). Effects of PSP were minimal for those not reporting IPV at baseline (n = 161; ES = −0.15) and more robust for those reporting IPV at baseline (n = 56; ES = 0.43). No subgroup differences were found based on baseline social needs.
FIG. 2.
Patient financial resources by condition predicting social quality of life.
FIG. 3.
History of interpersonal violence by condition predicting environmental quality of life.
Heterogeneity and psychological barriers
There were no significant moderation effects associated with Psychological QOL.
Heterogeneity and health comorbidities
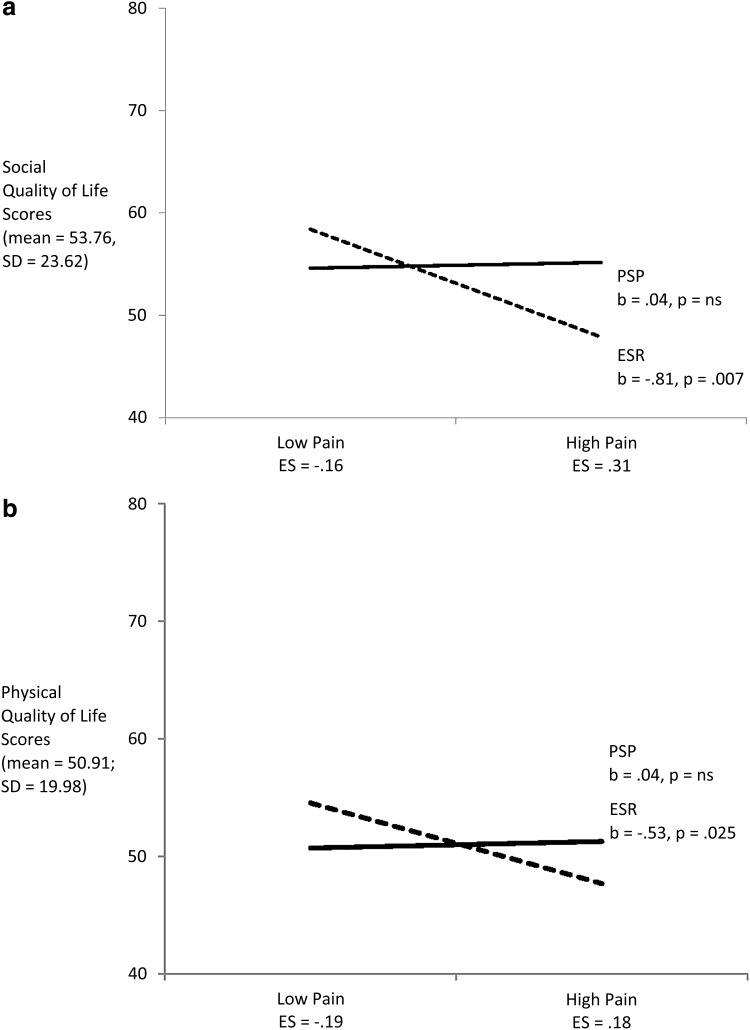
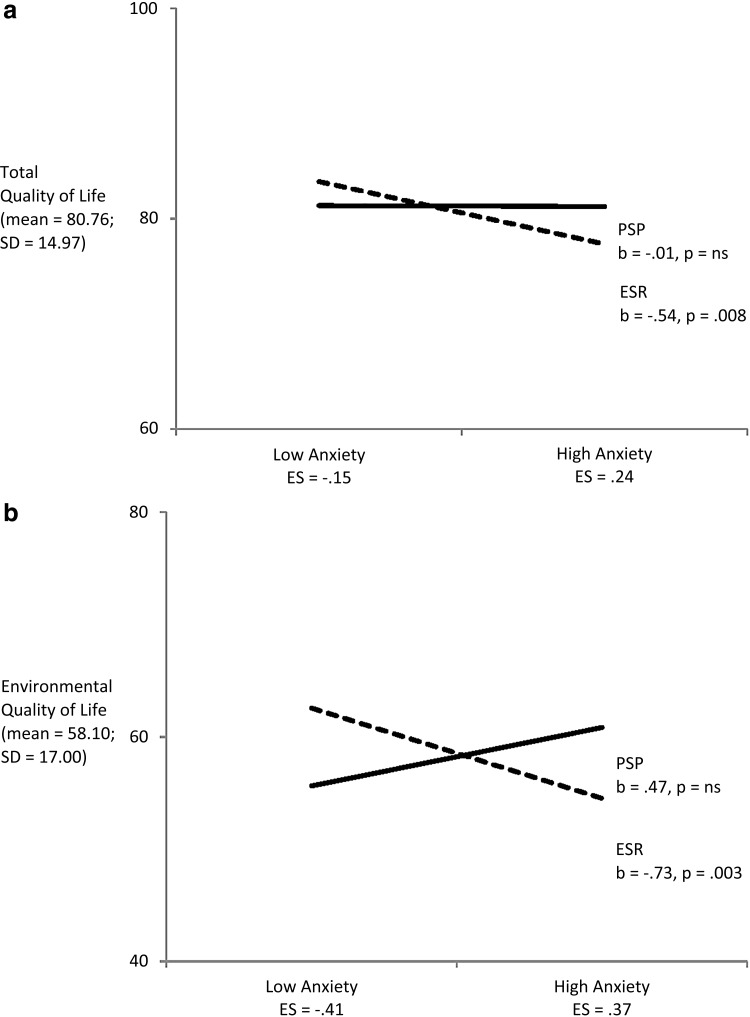
Baseline pain, anxiety, and disability each moderated the effect of PSP on QOL. Specifically, baseline level of pain significantly moderated the intervention effect on postintervention Social QOL (t = 2.07, p = 0.038; Fig. 4a). The effect was minimal for those with low levels of baseline pain, favoring ESR (ES = −0.16) and larger for women with high levels of baseline pain, favoring PSP (ES = 0.31). Baseline levels of pain moderated the effect of PSP on Physical QOL, although marginally (t = 1.92, p = 0.056; Fig. 4b). ESs at both ends of the pain distribution were small (i.e., low level of baseline pain, ES = −0.19 favoring ESR; high levels of baseline pain, ES = 0.18 favoring PSP). Baseline levels of anxiety also moderated the effect of the PSP condition on Total QOL (t = 2.01, p = 0.045; Fig. 5a). Again, moderating effects were minimal under conditions of low baseline anxiety (ES = −0.15); under conditions of high levels of baseline anxiety effects were small, but potentially meaningful (ES = 0.24) favoring PSP. There was a significant moderating effect of anxiety on the effect of PSP on Environmental QOL (t = 3.71, p < 0.001; Fig. 5b). Here, under low levels of baseline anxiety, moderating effects favored the ESR participants (ES = −0.41). Under high levels of baseline anxiety, effects favored the PSP participants (ES = 0.37). There were no significant moderating effects on QOL for baseline depression or alcohol use.
FIG. 4.
(a) Pain by condition predicting social quality of life. (b) Pain by condition predicting physical quality of life.
FIG. 5.
(a) Anxiety by condition predicting total quality of life. (b) Anxiety by condition predicting environmental quality of life.
Discussion
Participants in both ESR and PSP groups reported high satisfaction and improved for depression but not QOL. Our hypotheses for main effects of PSP over ESR for satisfaction, depression, and QOL were not supported. Further subgroup analyses demonstrated improvement in QOL among PSP participants with additional complex challenges, such as those who endorsed believing mental health treatment was not an affordable option, and those with IPV, chronic pain, and anxiety.
Both interventions, a low-intensity, low-cost intervention and a higher intensity CHW intervention, were highly acceptable and beneficial for depression. Our high retention, high satisfaction, and improvement for depression across both groups, despite their relative low intensity, are notable. This is particularly true given that none was seeking out services for depression, most participants were women of color, and many were coping with multiple challenges such as poverty, unstable living situations, active IPV, and pain. These findings reflect the importance of partnering evidence-based interventions with stakeholder involvement. Our years of conversations with women and providers facilitated our understanding of the problem, ensured we offered intervention arms that were appealing to participants, minimized participant burden, captured outcomes that mattered, and improved outcomes.
As health care is evolving to acknowledge that social and structural factors influence health outcomes,55 it is important to understand we can intervene. We examined two patient-centered approaches that addressed unmet social needs; neither were depression treatments yet both were associated with decreased depression. We learned subgroups of women facing additional difficulties benefited from the additional support of a CHW offered by the PSP intervention, while others, primarily with less complex presentations, showed improvement in response to a personalized resource list and minimal support only. Our findings that many women can benefit from ESR are consistent with other research showing the impact of low-intensity interventions, such as a study that found mailing an outreach postcard dramatically reduced suicide and psychiatric admissions after 5 years.59
Strengths of our study include the involvement of community stakeholders; the use of innovative approaches to address unmet social needs; and the high retention rate.
Limitations include the lack of a true control condition, and the intervention phase was short, especially to see change in QOL, making it difficult to learn what the potential impact of PSP might be if duration was based on the time needed for each woman to attain her personal goals. The frequency and type of contact, as well as the content of the contacts received by PSP participants varied greatly, creating substantial heterogeneity. Requiring participants to be English speaking excluded some individuals at particular risk of unmet social needs; future studies plan to offer the intervention in Spanish as an initial step. Depression may not have been the best outcome to assess: only 38% of the women identified “emotional needs” as the problem they wanted to focus on with their CHWs. Social needs would have been a relevant outcome to consider but was not analyzed because it was not included in the initial hypotheses. Neither intervention was integrated into the actual delivery of the women's health care, but rather was implemented in parallel to their usual health care.
We hypothesize these interventions may prove most helpful as adjuncts for all women with unmet social needs and can be delivered in combination with depression treatments for women with depressive disorder diagnoses. These findings highlight the importance of supporting busy practices to implement universal screening for unmet social needs and offer additional interventions and determining further who may benefit from ESR and who may require the additional support of PSP.
Conclusions
Our results support that both PSP and ESR are effective, scalable interventions that are personalized, address unmet social needs, and can be used in busy, real-life women's health settings. Perhaps the interventions could benefit all women with unmet social needs, not just those with depression. The greater intensity and support provided by the PSP intervention was needed for women with multiple, complex, and competing unmet social needs and health comorbidities. Finally, additional research is needed as we continue to try to determine what approaches are required and for whom within the context of women's health practices to attain stronger outcomes among women facing significant social and health inequities. Our research continues seeking to understand how population health-based approaches can be enhanced by incorporating interventions to impact long-term health and service utilization.
Acknowledgments
All statements in this report, including its findings and conclusions, are solely those of the authors and do not necessarily represent the views of the Patient-Centered Outcomes Research Institute, its Board of Governors, or Methodology Committee. The content does not necessarily represent the official views of the Patient-Centered Outcomes Research Institute nor the National Institutes of Health. Study data were collected and managed using Research Electronic Data Capture (REDCap) electronic data capture tools hosted at the University of Rochester Medical Center. REDCap is a secure, web-based application designed to support data capture for research studies, providing (i) an intuitive interface for validated data entry; (ii) audit trails for tracking data manipulation and export procedures; (iii) automated export procedures for seamless data downloads to common statistical packages; and (iv) procedures for importing data from external sources. The authors are very grateful for the generous input provided by their study participants, clinic staff, and the study Community Advisory Board. This study could not have been completed without the dedication and effort of the following individuals: Emma Briggs, B.A.; Jenna Chaudari, BS; Ineabelle Geena Cruz, BA; Sarah Danzo, MA; Tara Gellasch, MD, MBA; Shaya Greathouse, MA; Nikki Haynesworth, MS, LMHC; Kim Hober, LMSW; Paige Iovine-Wong, BS; Allison Lobell, RN; Rachel Missell, MS; Shirley Morgan; Wanda Perez-Diaz, BA; Michelle ReQua, MS; Mardy Sandler, LMSW; Jennifer Thompson-Stone, MA; and Cassandra Uthman, BA.
Author Disclosure Statement
No competing financial interests exist.
Funding Information
This research was supported by Patient-Centered Outcomes Research Institute Program Award (AD-12-4261). The research also was supported by the University of Rochester CTSA award number UL1 TR000042 from the National Center for Advancing Translational Sciences of the National Institutes of Health.
References
- 1. Bell RA, Franks P, Duberstein PR, et al. Suffering in silence: Reasons for not disclosing depression in primary care. Ann Fam Med 2011;9:439–446 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Cooper LA, Gonzales JJ, Gallo JJ, et al. The acceptability of treatment for depression among African-American, Hispanic, and White primary care patients. Med Care 2003;41:479–489 [DOI] [PubMed] [Google Scholar]
- 3. Karasz A. Cultural differences in conceptual models of depression. Soc Sci Med 2005;60:1625–1635 [DOI] [PubMed] [Google Scholar]
- 4. Voigt I, Wrede J, Diederichs-Egidi H, Dierks M, Junius-Walker U. Priority setting in general practice: Health priorities of older patients differ from treatment priorities of their physicians. Croat Med J 2010;51:483–492 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Wittink MN, Joo JH, Lewis LM, Barg FK. Losing faith and using faith: Older African Americans discuss spirituality, religious activities, and depression. J Gen Intern Med 2009;24:402–407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. American College of Obstetricians and Gynecologists. ACOG committee opinion no. 729: Importance of social determinants of health and cultural awareness in the delivery of reproductive health care. Obstet Gynecol 2018;131:e43–e48 [DOI] [PubMed] [Google Scholar]
- 7. Blumenshine P, Egerter S, Barclay CJ, Cubbin C, Braveman PA. Socioeconomic disparities in adverse birth outcomes: A systematic review. Am J Prev Med 2010;39:263–272 [DOI] [PubMed] [Google Scholar]
- 8. Braslow JT, Messac L. Medicalization and demedicalization—a gravely disabled homeless man with psychiatric illness. N Engl J Med 2018;379:1885–1888 [DOI] [PubMed] [Google Scholar]
- 9. Kessler RC. Epidemiology of women and depression. J Affect Disord 2003;74:5–13 [DOI] [PubMed] [Google Scholar]
- 10. Stewart DE, Robertson E, Dennis C, Grace SL, Wallington T. Postpartum depression: Literature review of risk factors and interventions. Toronto, Canada: University Health Network Women's Health Program for Toronto Public Health, 2003. Available at: https://who.int/mental_health/prevention/suicide/lit_review_postpartum_depression.pdf Accessed March19, 2019 [Google Scholar]
- 11. Hobfoll SE, Ritter C, Lavin J, Hulsizer MR, Cameron RP. Depression prevalence and incidence among inner-city pregnant and postpartum women. J Consult Clin Psychol 1995;63:445–453 [DOI] [PubMed] [Google Scholar]
- 12. Coleman VH, Laube DW, Hale RW, Williams SB, Power ML, Schulkin J. Obstetrician–gynecologists and primary care: Training during obstetrics–gynecology residency and current practice patterns. Acad Med 2007;82:602–607 [DOI] [PubMed] [Google Scholar]
- 13. Scholle SH, Kelleher K. Assessing primary care performance in an obstetrics/gynecology clinic. Women Health 2003;37:15–30 [DOI] [PubMed] [Google Scholar]
- 14. Petterson SM, Bazemore AW, Phillips RL, Rayburn WF. Trends in office-based care for reproductive-aged women according to physician specialty: A ten-year study. J Womens Health (Larchmt) 2014;23:1021–1026 [DOI] [PubMed] [Google Scholar]
- 15. Braveman PA, Cubbin C, Egerter S, et al. Socioeconomic status in health research: One size does not fit all. JAMA 2005;294:2879–2888 [DOI] [PubMed] [Google Scholar]
- 16. Moos M. Prenatal care: Limitations and opportunities. J Obstet Gynecol Neonatal Nurs 2006;35:278–285 [DOI] [PubMed] [Google Scholar]
- 17. Cerimele JM, Vanderlip ER, Croicu CA, et al. Presenting symptoms of women with depression in an obstetrics and gynecology setting. Obstet Gynecol 2013;122:313–318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Bhat A, Reed SD, Unutzer J. The obstetrician-gynecologist's role in detecting, preventing, and treating depression. Obstet Gynecol 2017;129:157–163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Leddy MA, Lawrence H, Schulkin J. Obstetrician-gynecologists and women's mental health: Findings of the collaborative ambulatory research network 2005–2009. Obstet Gynecol Surv 2011;66:316–323 [DOI] [PubMed] [Google Scholar]
- 20. World Health Organization. Women and health: Today's evidence tomorrow's agenda. Geneva: World Health Organization, 2009 [Google Scholar]
- 21. Poleshuck E, Wittink M, Crean H, et al. Using patient engagement in the design and rationale of a trial for women with depression in obstetrics and gynecology practices. Contemp Clin Trials 2015;43:83–92 [DOI] [PubMed] [Google Scholar]
- 22. Israel BA, Parker EA, Rowe Z, et al. Community-based participatory research: Lessons learned from the centers for children's environmental health and disease prevention research. Environ Health Perspect 2005;113:1463–1471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Poleshuck E, Mazzotta C, Resch K, et al. Development of an innovative treatment paradigm for intimate partner violence victims with depression and pain using community-based participatory research. J Interpers Violence 2018;33:2704–2724 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. New York State Department of Health, Division of Information and Statistics Office of Quality and Patient Safety. Annual report of vital statistics in New York State, 2014. Available at: https://health.ny.gov/statistics/vital_statistics/docs/vital_statistics_annual_report_2014.pdf Accessed March19, 2019
- 25. New York State Department of Health. Socio-economic status and general heath indicators-Monroe County 2013–2015, 2017. Available at: https://health.ny.gov/statistics/chac/chai/docs/ses_26.htm Accessed August30, 2019
- 26. Attkisson CC, Greenfield TK. Client satisfaction questionnaire-8 and service satisfaction scale-30. In: Maruish ME, ed. The use of psychological testing for treatment planning and outcome assessment. Hillsdale, NJ: Lawrence Erlbaum Associates, Inc., 1994:402–420 [Google Scholar]
- 27. Kroenke K, Spitzer RL, Williams JBW. The PHQ-9. Validity of a brief depression severity measure. J Gen Intern Med 2001;16:606–613 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. University of Michigan. Quality department for ambulatory care. UMHS depression guideline update, August 2011. Depression 2011 update, 1998. Available at: http://med.umich.edu/1info/FHP/practiceguides/depress/depression.pdf Accessed March2019
- 29. Kroenke K, Spitzer RL, Williams JB, Löwe B. The patient health questionnaire somatic, anxiety, and depressive symptom scales: A systematic review. Gen Hosp Psychiatry 2010;32:345–359 [DOI] [PubMed] [Google Scholar]
- 30. Sidebottom AC, Harrison PA, Godecker A, Kim H. Validation of the patient health questionnaire (PHQ)-9 for prenatal depression screening. Arch Womens Ment Health 2012;15:367–374 [DOI] [PubMed] [Google Scholar]
- 31. Chaudron LH, Szilagyi PG, Tang W, et al. Accuracy of depression screening tools for identifying postpartum depression among urban mothers. Pediatr 2010;125:e609–e617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Huang F, Chung H, Kroenke K, Delucchi K, Spitzer R. Using the patient health questionnaire-9 to measure depression among racially and ethnically diverse primary care patients. J Gen Intern Med 2006;21:547–552 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Skevington SM, Lotfy M, O'Connell KA. The world health organization's WHOQOL-BREF quality of life assessment: Psychometric properties and results of the international field trial. A report from the WHOQOL group. Qual Life Res 2004;13:299–310 [DOI] [PubMed] [Google Scholar]
- 34. Webster J, Nicholas C, Velacott C, Cridland N, Fawcett L. Validation of the WHOQOL-BREF among women following childbirth. Aust N Z J Obstet Gynaecol 2010;50:132–137 [DOI] [PubMed] [Google Scholar]
- 35. Feldhaus KM, Koziol-McLain J, Amsbury HL, Norton IM, Lowenstein SR, Abbott JT. Accuracy of 3 brief screening questions for detecting partner violence in the emergency department. JAMA 1997;277:1357–1361 [PubMed] [Google Scholar]
- 36. Paterno MT, Draughon JE. Screening for intimate partner violence. J Midwifery Womens Health 2016;61:370–375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch Intern Med 2006;166:1092–1097 [DOI] [PubMed] [Google Scholar]
- 38. Löwe B, Decker O, Müller S, et al. Validation and standardization of the generalized anxiety disorder screener (GAD-7) in the general population. Med Care 2008;46:266–274 [DOI] [PubMed] [Google Scholar]
- 39. Bush K, Kivlahan DR, McDonell MB, Fihn SD, Bradley KA. The AUDIT alcohol consumption questions (AUDIT-C): An effective brief screening test for problem drinking. Arch Intern Med 1998;158:1789–1795 [DOI] [PubMed] [Google Scholar]
- 40. Dawson DA, Grant BF, Stinson FS, Zhou Y. Effectiveness of the derived alcohol use disorders identification test (AUDIT-C) in screening for alcohol use disorders and risk drinking in the US general population. Alcohol Clin Exp Res 2005;29:844–854 [DOI] [PubMed] [Google Scholar]
- 41. Khadjesari Z, White IR, McCambridge J, et al. Validation of the AUDIT-C in adults seeking help with their drinking online. Addict Sci Clin Pract 2017;12:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Cleeland CS, Ryan KM. Pain assessment: Global use of the brief pain inventory. Ann Acad Med Singapore 1994;23:129–138 [PubMed] [Google Scholar]
- 43. Tan G, Jensen MP, Thornby JI, Shanti BF. Validation of the brief pain inventory for chronic nonmalignant pain. J Pain 2004;5:133–137 [DOI] [PubMed] [Google Scholar]
- 44. Andrews G, Kemp A, Sunderland M, Von Korff M, Ustun TB. Normative data for the 12 item WHO disability assessment schedule 2.0. PLoS One 2009;4:e8343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Silveira C, Souza RT, Costa ML, et al. Validation of the WHO disability assessment schedule (WHODAS 2.0) 12-item tool against the 36-item version for measuring functioning and disability associated with pregnancy and history of severe maternal morbidity. Obstet Gynecol Int J 2018;141(Suppl 1):39–47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Cooper LA, Brown C, Vu HT, et al. Primary care patients' opinions regarding the importance of various aspects of care for depression. Gen Hosp Psychiatry 2000;22:163–173 [DOI] [PubMed] [Google Scholar]
- 47. Williams GC, Deci EL. Internalization of biopsychosocial values by medical students: A test of self-determination theory. J Pers Soc Psychol 1996;70:767–779 [DOI] [PubMed] [Google Scholar]
- 48. Ryan RM, Deci EL. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am Psychol 2000;55:68–78 [DOI] [PubMed] [Google Scholar]
- 49. Lipsey MW, Hurley SM. Design sensitivity: Statistical power for experimental research. In: Bickman L, Rog DJ, eds. The SAGE handbook of applied social research methods, 2nd ed. Thousand Oaks, CA: SAGE Publications, Inc., 2009:44–76 [Google Scholar]
- 50. Van Breukelen GJ. ANCOVA versus change from baseline: More power in randomized studies, more bias in nonrandomized studies [corrected]. J Clin Epidemiol 2006;59:920–925 [DOI] [PubMed] [Google Scholar]
- 51. Fisher LD, Dixon DO, Herson J, Frankowski RF, Hearron MS, Peace KE. Intention to treat in clinical trials. In: Peace KE, ed. Statistical issues in drug research and development (American statistical associations group). New York: Marcel Dekker, Inc., 1990:331–350 [Google Scholar]
- 52. Ten Have TR, Normand SLT, Marcus SM, Brown CH, Lavori P, Duan N. Intent-to-treat vs. non-intent-to-treat analyses under treatment non-adherence in mental health randomized trials. Psychiatr Ann 2008;38:772–783 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Varadhan R, Wang SJ. Chapter 3: Estimation and reporting of heterogeneous treatment effects. In: Velentgas P, Dreyer N, Nourjah P, Smith S, Torchia M, eds. Developing a protocol for observational comparative effectiveness research: A user's guide. Rockville, MD: Agency for Healthcare Research and Quality, 2013:35–45 [PubMed] [Google Scholar]
- 54. Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Thousand Oaks, CA: Sage Publications, Inc., 1991 [Google Scholar]
- 55. Metzl JM, Hansen H. Structural competency: Theorizing a new medical engagement with stigma and inequality. Soc Sci Med 2014;103:126–133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Sheehan DV, Lecrubier Y, Sheehan KH, et al. The mini-international neuropsychiatric interview (M.I.N.I.): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry 1998;59 Suppl 20:22–33, quiz 34–57 [PubMed] [Google Scholar]
- 57. Borenstein M, Hedges LV, Higgins JP, Rothstein HR. Introduction to meta-analysis. Chichester, United Kingdom: John Wiley and Sons, 2009 [Google Scholar]
- 58. Cohen J, Cohen P, West SG, Aiken LS. Applied multiple regression/correlation analysis for the behavioral sciences, 3rd ed. Mahwah, NJ: Lawrence Erlbaum Associates, Inc., 2003 [Google Scholar]
- 59. Carter GL, Clover K, Whyte IM, Dawson AH, D'este C. Postcards from the EDge: 5-Year outcomes of a randomised controlled trial for hospital-treated self-poisoning. Br J Pyschiatry 2013;202:372–380 [DOI] [PubMed] [Google Scholar]