Short abstract
Diabetic foot is a serious complication in patients with diabetes. It is caused by diabetes combined with lower extremity vascular lesions and neuropathy so that a wound does not heal for a long time. In severe cases, it may lead to bone marrow infection and bone destruction, with a high disability and fatality rate. This report describes the case of a patient with diabetic hallux gangrene with lower extremity vascular disease, which was treated by surgical debridement, ozone therapy, and vascular interventional surgery. Using this treatment, the diabetic foot can be cured better and faster, and a satisfactory effect can be achieved.
Keywords: Diabetic foot, lower extremity vascular disease, ozone therapy, vascular interventional surgery, medical footwear, diabetic hallux gangrene, diabetic neuropathy, wound, wound healing
Introduction
Concerns for patients with diabetic foot include ulceration, amputation, and death. Comprehensive treatment aims to avoid amputation. For diabetic ischemic foot with gangrene, one-stage surgical debridement is used to control the local infection symptoms and improve the general condition. After surgery, controlling blood sugar, preventing infection, reducing blood lipid levels, and improving micro-circulation and nutrient supply to the nerve are important, and ozone therapy can be applied to further control wound infection and promote granulation tissue growth. For ischemic lesions, secondary vascular reconstruction is particularly important.
Case report
A 67-year-old woman was admitted as a diabetic foot outpatient. She had gangrene of the right hallux with pain for 1 month and ulceration with purulence for 2 weeks. The patient’s spirit, diet, sleep, and weight had not changed substantially. She had a history of diabetes mellitus for more than 10 years and coronary heart disease for more than 10 years. She visited the orthopedic clinic at Beijing Shijitan Hospital CCMU on April 2, 2018.
Specialist examination
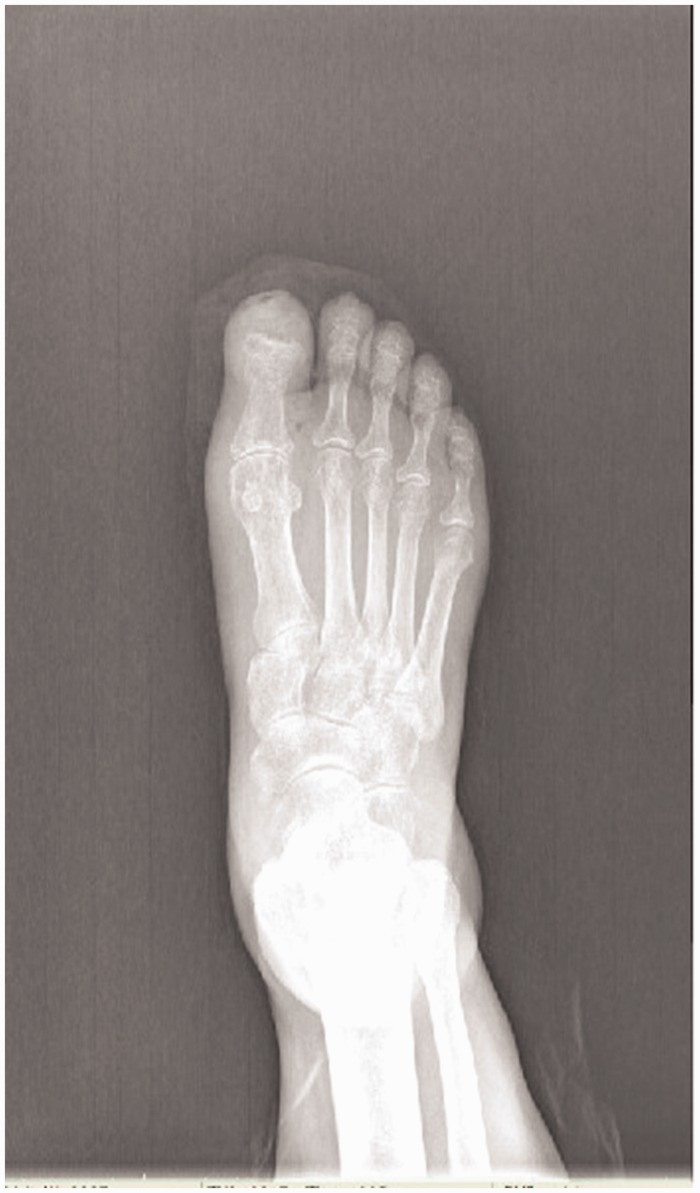
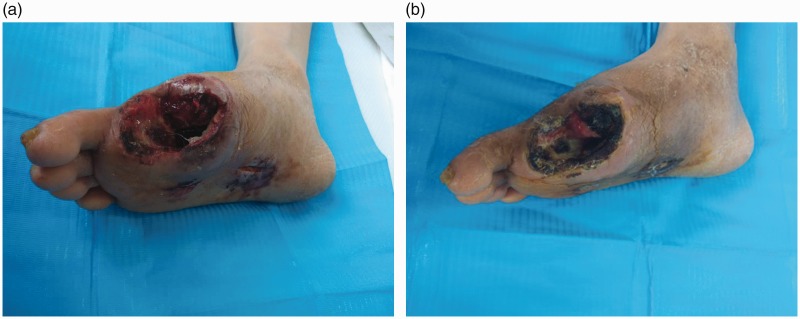
Examination showed that the right foot was red and swollen, and the distal hallux had a wound that was 1 cm × 0.5 cm × 0.5 cm, with a large amount of exudation. The distal skin margin showed black gangrene, high sensitivity in the area, bone test results were positive, and there was a weak pulsation of the dorsalis pedis. Additionally, 2–4 toes could undergo flexion and extension, and the ankle joint activity was normal (Figure 1).
Figure 1.
Right hallux condition at admission.
Routine laboratory examination results
The laboratory results including the biochemical and blood test results are presented in Table 1.
Table 1.
Routine laboratory examination results.
| Reference range | ||
|---|---|---|
| Biochemical examination results | ||
| Alanine aminotransferase (U/L) | 8 | 0.0–38.0 |
| Aspartate aminotransferase (U/L) | 9 | 0.0–38.0 |
| Total bilirubin (µmol/L) | 8.5 | 0.0–17.0 |
| Direct bilirubin (µmol/L) | 3.3 | 0.0–3.4 |
| Indirect bilirubin (µmol/L) | 5.1 | 0.0–14.4 |
| Total protein(g/L) | 63.8 | 65.0–85.0 |
| Na+ (mmol/L) | 138 | 137.0–147.0 |
| Cl− (mmol/L) | 103 | 99.0–110.0 |
| Ca2+ (mmol/L) | 2.26 | 2.10–2.75 |
| P3+ (mmol/L) | 1.1 | 0.97–1.62 |
| Fe2+ (µmol/L) | 8.8 | 7.0–32.0 |
| Mg2+ (mmol/L) | 0.87 | 0.66–1.20 |
| K+ (mmol/L) | 3.73 | 3.5–5.3 |
| Creatinine (µmol/L) | 52 | 44.0–80.0 |
| Uric acid (µmol/L) | 154 | 142.0–339.0 |
| Blood glucose (mmol/L) | 12.8 | 3.9–6.1 |
| Creatine kinase (U/L) | 29 | 20.0–190.0 |
| Lactate dehydrogenase (U/L) | 141 | 40.0–240.0 |
| Albumin (g/L) | 32.7 | 40.0–55.0 |
| Alkaline phosphatase (U/L) | 129 | 45–125 |
| Urea nitrogen (mmol/L) | 3.98 | 2.1–7.9 |
| Blood routine test results | ||
| White blood cell count (109/L) | 12.73 | 3.5–9.5 |
| Percentage of neutrophils (%) | 82.4 | 40–75 |
| Platelets count (109/L) | 410 | 125–350 |
| Hemoglobin (g/L) | 144 | 130–175 |
| C-reactive protein (CRP) (mg/L) | 60.14 | 0.0–5.0 |
| Procalcitonin (PCT) (ng/mL) | 0.06 | 0.0–0.05 |
Imaging examination
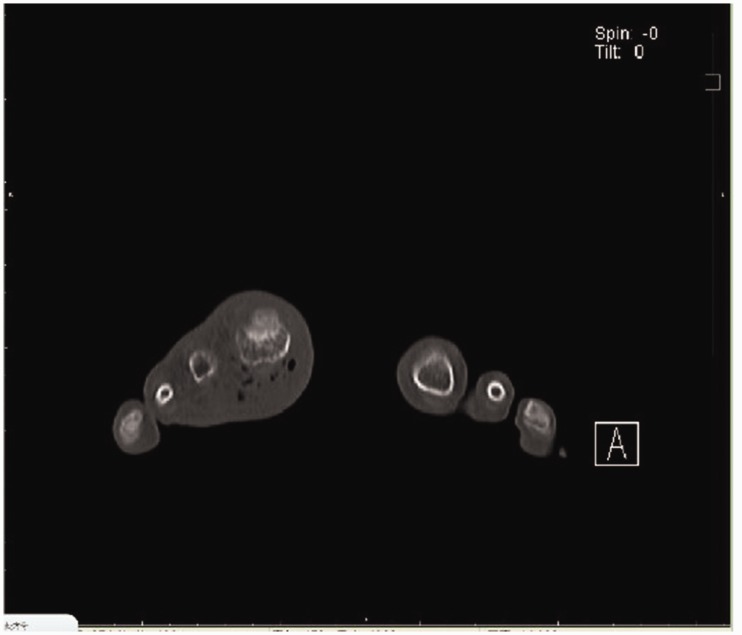
The imaging examination results were as follows: 1) X-ray of the right foot showed that the bone cortex of the distal phalanx of the hallux was increased slightly, the was density decreased, and it was not uniform, which was in agreement with the changes in a patient with diabetic foot and the regression of the first metatarsophalangeal joint of the right foot (Figure 2); and 2) CT scan of the right foot showed multiple gas density images in the soft tissue around the right hallux and the first metatarsophalangeal joint, which was consistent with gangrene. No obvious bone abnormalities were found in the other bones (Figure 3).
Figure 2.
Positive X-ray of the right foot.
Figure 3.
Bone destruction in the right hallux and gas detected in the image of the soft tissue around the first metatarsophalangeal joint in the right foot.
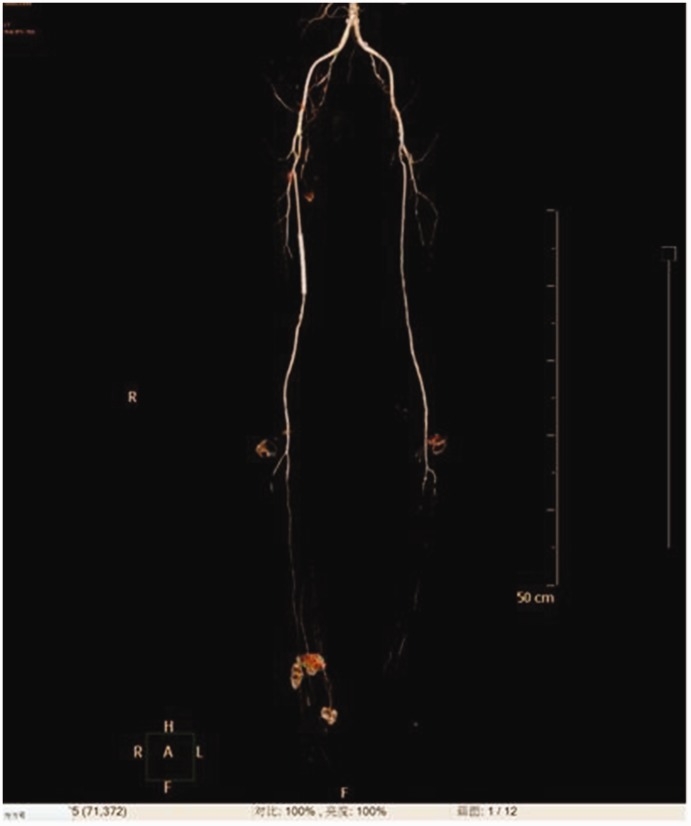
Blood vessel examination
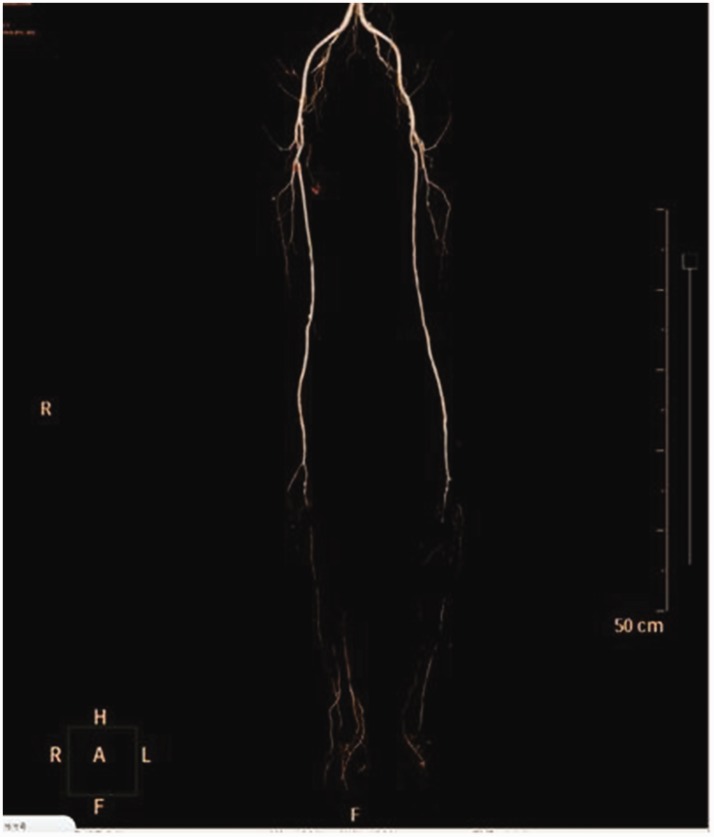
CT angiography (CTA) of both the lower extremities showed that at the end of the abdominal aorta, bilateral common iliac artery, external iliac artery, and internal iliac artery, there was slight arteriostenosis of the lumen (local thickening and calcification of vascular wall). The arteriostenosis of bilateral internal iliac arteries was more severe, with local arteriostenosis of 40%, and the bilateral femoral profound artery, superficial femoral artery, and popliteal artery (which showed local thickening and calcification of vascular wall) showed local narrowing with arteriostenosis of less than 50%. Additionally, there were bilateral superficial femoral artery proximal local low-density plaques and local arteriostenosis of the lumen was approximately 30%–40%. The lumen of the bilateral anterior tibial artery, posterior tibial artery, and peroneal artery did not contain much blood. Multiple branches of the small arteries could be seen in the calf and plaques were visible in these arteries. Gas density was high in the soft tissue of the right foot (Figure 4).
Figure 4.
Arterial angiography of both lower extremities.
Treatment process
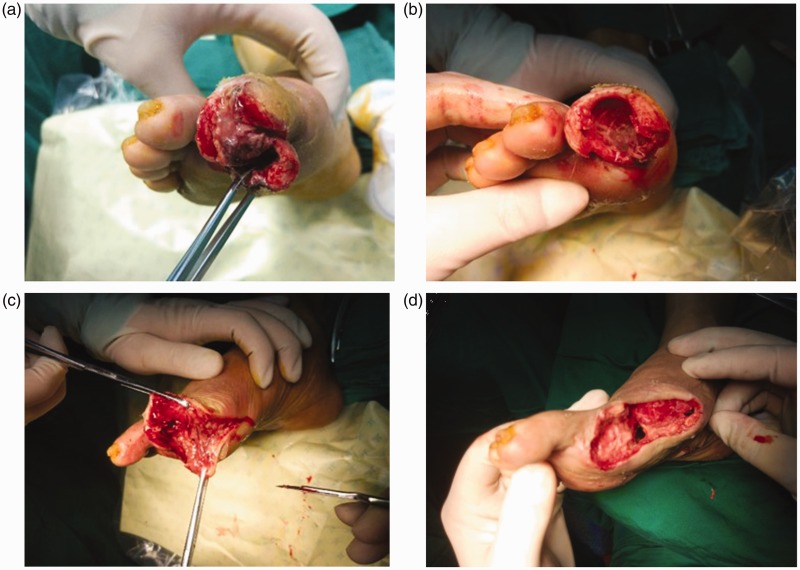
After admission, the patient was given symptomatic treatment including anti-inflammatory medication, detumescence, improvement of circulation and nutrients to the nerves, and anticoagulant medications. On April 3, 2018, under spinal anesthesia, right hallux amputation including necrotic tissue debridement and neurovascular tendon exploration was performed (Figure 5). After surgery, the wound was treated with ozone therapy (Figure 6). After the first stage of hallux amputation and necrotic tissue debridement, ozone bagging therapy was applied. The wound was cleaned with saline before changing the dressing, and a disposable plastic bag was then placed onto the skin lesion. The bag was then filled with ozone at the given concentration, and the bag was left on the patient’s foot for 20 minutes. The patient started with an ozone concentration of 30 µg/mL. After two consecutive treatments, the ozone concentration increased gradually by 5 µg/mL. After the treatment, the ozone was removed from the bag and the bag was removed from the patient’s foot. The wound that was treated by ozone showed good growth of granulation tissue and maintained a relatively clean wound environment.
Figure 5.
Right hallux amputation with necrotic tissue debridement and neurovascular tendon exploration under spinal anesthesia. (a) Bone necrosis of the distal hallux and a dim color were observed during surgery; (b) Complete disruption of the distal hallux phalanx bone, insufficient blood supply to the proximal phalanx bone and dim color of the phalanx bone; (c) Disruption of the proximal phalanx bone along the articular surface of metatarsophalangeal bone, removal of distal metatarsal joint surface, and presence of purulent secretion into the plantar lacuna; (d) Debridement of the necrotic tissue to the fresh wound surface, small incision drainage on the plantar surface.
Figure 6.
The wound dressing was changed after surgery. (a) Three days after surgery and (b) 14 days after surgery, the wound was ischemic with necrosis.
To improve the condition of the blood vessels in the right lower extremity and promote wound healing, vascular interventional surgery was performed. Balloon dilatation and stent implantation into the femoral artery in the right lower extremity was performed under local anesthesia on April 18, 2018. Postoperative lower extremity angiography was performed. The stent image was visible in the right femoral artery, and the stent shape was acceptable. Contrast medium filled evenly throughout in the stent, and no obvious filling defect was found. Filling of the bilateral calf arteries was better compared with before surgery. The multiple small vessels in the calf artery were not visible in the later image (Figure 7).
Figure 7.
Lower extremity angiography after balloon dilatation and stent implantation into the femoral artery in the right lower extremity.
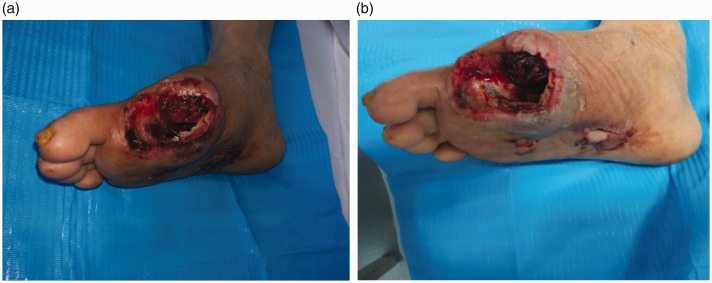
After surgery, the wound was treated with ozone therapy, and granulation tissue was observed because the blood supply was restored (Figure 8a,b). The right foot was examined using magnetic resonance imaging (Figure 9). To close the wound, a third operation was performed under spinal anesthesia on May 4, 2018 (Figure 10). The patient was discharged on May 6, 2018, and was re-examined 1 month after discharge (Figure 11).
Figure 8.
(a,b) Granulation tissue resulting from restoration of the blood supply.
Figure 9.
No osteomyelitis was found in the first metatarsal bone or in the surrounding bone of the right foot.
Figure 10.
Right foot wound debridement and suturing.
Figure 11.
Follow-up of the patient’s wounds 1 month after discharge on June 6, 2018.
Discussion
Diabetic foot disease comprises foot infection, ulcers, and/or deep tissue damage that is caused by abnormal nerves in the distal lower extremities and vascular disease in diabetic patients. It is one of the most serious chronic complications of patients with diabetes mellitus and the cost of treating patients with diabetic foot is high. Diabetic foot in obese people can lead to amputation and death.1 Globally, the prevalence rate of diabetic foot is more than 6%, and the average prevalence rate of diabetic foot in China is 5.7%.2 Among diabetic patients who are over 50 years old in China, the annual incidence of foot ulcer was 8.1% and the re-incidence rate after cure was 31.6%.3 Treatment of this disease should involve an interdisciplinary diabetic foot treatment center that includes a registered dietitian, diabetes specialist, orthopedic and/or vascular surgeon, wound manager, foot orthopedic specialist, and podiatrist.4
Diabetic ischemic foot gangrene can occur suddenly, and the pain is intense. Gangrene occurs slowly in most patients, and while there is serious nerve damage, the pain can be mild or severe. There can be local mild injury and small blisters localized in the skin. This is followed by the subcutaneous tissue that turns dark red or black, ulceration, and necrosis, with dry and black skin, and purulent infection. The patient was hospitalized with gangrene of the right hallux with pain for 1 month and ulceration with purulent discharge for 2 weeks, and the diagnosis of diabetic ischemic foot gangrene was made. The results of arteriography of both lower limbs confirmed that the patient’s main blood vessels in her foot were occluded. After hallux amputation, the pain persisted, and it was caused by ischemic lesions. Therefore, it was particularly important to recanalize the main blood vessels of the lower limbs after hallux amputation. The microcirculation can also be reconstructed around the wound to promote wound healing.5–6
Diabetic foot patients often have occlusion of the lower limb main circulation, so minimally invasive interventional therapy is widely used in the clinic. It is a less traumatic operation. It can restore long-term ischemic limb blood perfusion through intraluminal vascular recanalization, so that the blood supply around the foot wound can be restored and promote wound healing. The methods of revascularization under interventional conditions include percutaneous transluminal angioplasty, endovascular circumcision based on balloon dilation, thrombolysis, and stent implantation. In this patient, the blood supply to the lower limb artery was improved after balloon dilatation and stent implantation in the right lower limb femoral artery, which increased the blood perfusion at the edge of the wound and created conditions to allow the growth of granulation tissue on the wound surface.7–8 For patients with diabetic foot that is in the acute infection stage, advanced debridement is needed to avoid toxins entering the blood after the blood vessels are opened during the first stage, which could result in sepsis.
The special feature of this case was that the patient’s foot was in the acute infection stage at the time of admission (laboratory indicators and imaging examination indicate that the infection was more serious). The debridement procedure is performed in the first stage, and the vascular opening procedure is performed after the local infection is controlled. However, it should be emphasized that for a severe infection or foot ulcers in the acute infection period, if the ischemia is resolved first after debridement, the infection could worsen after the ischemia resolves, and sepsis could appear.
Ozone is a strong oxidizing gas with a half-life of about 30 minutes at room temperature. Ozone is currently used to treat infectious wounds such as chronic ulcers in diabetic foot because it can kill many kinds of microorganisms quickly in vitro and in water.9 The patient’s wound that was treated by ozone showed good growth of granulation tissue and maintained a relatively clean wound environment; this provided the required conditions for secondary surgical suture of the wound.10 Local application of ozone has a strong bactericidal ability, which can clean the wound and promote the growth of granulation tissue in the later stage of skin grafting and skin flap transplantation to repair the wound. However, we will design a case-control study of ozone therapy for diabetic foot ulcers to confirm the significance of ozone therapy in promoting wound treatment. In this case, we only used ozone therapy to accelerate wound healing, but more case studies are needed to confirm the effect of this therapy.
Post-surgery, the patient was fitted for medical grade footwear and orthotics using a three-dimensional (3D) scanner. The orthotics incorporated an artificial toe to fill the space where the hallux had been and to support in the rear of the foot. Materials that can be used for the orthotics are ethylene vinyl acetate copolymer (EVA) and memory foam (PU) that is milled out of a single block of material. The orthotics should not be covered on the top because the patient should have as much sensory feedback as possible from the texture of the materials that are used. The medical grade footwear is constructed over the cast that is milled from the information taken from the 3D scan. This footwear is light-weight but functional and rigid where it is needed to give support, and flexible where the foot needs to move freely.11
In conclusion, debridement of local necrotic tissue is particularly important; it can reduce systemic infection symptoms and foot ulcer symptoms in diabetic patients. The main reason for this difficulty in healing is a reduction in the body’s resistance and local wound infection. The local application of medical ozone has strong bactericidal ability, and it can clean wounds and promote the growth of wound granulation tissue to prepare for post-skin grafting and flap transplantation to repair the wounds. There are two main methods that are used for interventional treatment of diabetic foot, including placing a balloon or a stent, and these treatments should be used based on the patient’s individual condition. Generally, for patients with segmental stenosis of the lower extremity, the balloon can be used to expand the blood vessel. For patients with severe stenosis, a stent can be placed to keep the blood vessel open. During treatment, attention should also be paid to glycemic control. Thus, the diabetic foot can be cured better and faster, and a satisfactory effect can be achieved. Each new or old diabetic patient who attends a clinic should have a podiatry assessment. To protect the foot from further injury, orthotics and footwear comprise the next step for each patient who loses part of a limb.
Acknowledgements
The authors thank all the people who helped during the writing of this paper.
Declaration of conflicting interest
The authors declare that there is no conflict of interest.
Ethics approval
This article was approved by the Ethics Committee at the Capital Medical University Affiliated Beijing Shijitan Hospital.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Informed Consent
Written consent was obtained from the patient to publish the details of this case.
ORCID iD
References
- 1.Chinese Diabetes Society. Guidelines for the prevention and control of type 2 diabetes in China (2017 Edition)[J]. Chinese J Practical Intl Med 2018; 10: 4–67. [Google Scholar]
- 2.Zhang P, Lu J, Jing Y, et al. Global epidemiology of diabetic foot ulceration: a systematic review and meta-analysis [J]. Ann Med 2017; 49: 106–116. [DOI] [PubMed] [Google Scholar]
- 3.Jiang Y, Wang X, Xia L, et al. A cohort study of diabetic patients and diabetic foot ulceration patients in China [J]. Wound Repair Regen 2015; 23: 222–230. [DOI] [PubMed] [Google Scholar]
- 4.Wang J and Gao L. New progress in the treatment of chronic wound of diabetic foot [J]. Chinese J Repar Reconstructive Surg 2018; 32: 832–837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Barwick A, Tessier J, Mirow J, et al. Computed tomography derived bone density measurement in the diabetic foot. J Foot Ankle Res 2017; 10: 1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Uzun G, Mutluoğlu M, Karagöz H, et al. Pitfalls of intralesional ozone injection in diabetic foot ulcers: a case study, J Am Coll Clin Wound Spec 2014; 4: 81–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Weaver ML, Hicks CW, Canner JK, et al. The Society for Vascular Surgery Wound, Ischemia, and foot Infection (WIfI) classification system predicts wound healing better than direct angiosome perfusion in diabetic foot wounds. J Vasc Surg 2018; 68: 1473–1481. [DOI] [PubMed] [Google Scholar]
- 8.Ali SR, Ozdemir BA, Hinchliffe RJ. Critical appraisal of the quality of evidence addressing the diagnosis, prognosis, and management of peripheral artery disease in patients with diabetic foot ulceration. Eur J Vasc Endovasc Surg 2018; 56: 401–408. [DOI] [PubMed] [Google Scholar]
- 9.Izadi M, Kheirjou R, Mohammadpour R, et al. Efficacy of comprehensive ozone therapy in diabetic foot ulcer healing [J]. Diabetes Metab Syndr 2019; 1 3(1): 822–825. [DOI] [PubMed] [Google Scholar]
- 10.Bocci V, Zanardi I, Huijberts MS, et al. Diabetes and chronic oxidative stress. A perspective based on the possible usefulness of ozone therapy. Diabetes Metab Syndr 2011; 5: 45–49. [DOI] [PubMed] [Google Scholar]
- 11.Jeffcoate WJ, Vileikyte L, Boyko EJ, et al. current challenges and opportunities in the prevention and management of diabetic foot ulcers. Diabetes Care 2018; 41: 645–652. [DOI] [PubMed] [Google Scholar]