Short abstract
Objective
To investigate the characteristics of labor in Chinese women who successfully have vaginal birth after cesarean section (VBAC).
Methods
A retrospective cohort study was conducted in a hospital with 1000 beds between January 1 2015 and December 31 2017. A total 657 parturients with VBAC were selected. Women were divided into two groups according to previous cesarean section with or without trial of labor. Labor curves were analyzed and interval-censored regression was used to estimate the duration of labor.
Results
The 95th percentile for the first stage of labor in VBAC was 13.03 hours, and labor accelerated after 4 cm of cervical dilation in both groups. The dilation rate in the trial of labor group was superior to that in the non-trial of labor group at 6–10 cm of dilation. After 6 cm, labor accelerated much faster in the trial of labor group than in the non-trial of labor group.
Conclusions
Management of labor in parturients with VBAC whose cervical dilation is >6 cm should be treated differently according to previous cesarean section with or without trial of labor. If there is trial of labor in a previous delivery, the duration of labor should be shortened.
Keywords: Vaginal birth after cesarean section, vaginal delivery, labor duration, labor curve, cervical dilation, trial of labor
Introduction
Childbirth is a complex physiological process. The purpose of a partograph is to reduce maternal and fetal morbidity and mortality. However, most of the participants selected in previous studies on labor were women who were pregnant without uterine scarring.1–3 At present, a trial of labor after cesarean section (TOLAC) can only be managed according to the labor management model of parturients without a history of cesarean section. In China, with the development of the two-child-policy, the rate of cesarean section with a uterine scar as a surgical indication is increasing.4,5 However, for the population with pregnancy after cesarean delivery, vaginal birth after cesarean section (VBAC) has a lower incidence of postpartum hemorrhage, embolism disease, infection, and a shorter postpartum recovery time compared with those who have repeated cesarean delivery.6 Additionally, VBAC reduces the risk associated with multiple cesarean and fetal complications.7–9 Standardized management of labor is important for planned VBAC. In this situation, labor should be conducted in a suitably staffed and equipped delivery suite with continuous intrapartum care and monitoring with resources available for immediate cesarean delivery and advanced neonatal resuscitation.
This study aimed to investigate the characteristics of labor in Chinese women who successfully had VBAC.
Materials and methods
Study design and setting
We performed a retrospective cohort study. The study was conducted in Fujian Provincial Maternity and Children’s Hospital with 1000 beds.
Ethics and consent statements
We received exemption from the Ethics Committee of Fujian Provincial Maternity and Children’s Hospital because this was a retrospective cohort study. Signed patient consent was not applicable.
Women
A total of 1231 pregnant Chinese women with a history of lower uterine segment cesarean section, a single pregnancy, cephalic presentation and spontaneous onset of labor, successful vaginal delivery, and good outcomes of mothers and newborns, with a gestational age between 37 weeks, 0 days and 41 weeks, 6 days, were selected. Women were excluded for the following reasons: their previous indications of cesarean were unclear; this pregnancy was a multiple pregnancy; breech position; terminated pregnancy, placental abruption; premature birth; use of oxytocin or analgesia in labor; uterine rupture or neonatal asphyxia; instrumented delivery, and with a history of vaginal delivery. Finally, parturients with VBAC were included in the study.
These women were divided into the following two groups according to previous cesarean section with or without trial of labor: the trial of labor group (n = 170) and the non-trial of labor group (n = 487). In the trial of labor group, the previous delivery was cesarean in labor, and the indications of cesarean section were dystocia, cephalopelvic disproportion, fetal distress, umbilical cord prolapse, or placental abruption. In the non-trial of labor group, the previous delivery was elective cesarean section. In this group, the indications of cesarean were fetal macrosomia, breech presentation, transverse lie, oligoamnios, placenta previa, placental abruption, fetal distress, failure in induced labor, preeclampsia, umbilical cord factors, and the pregnant woman and her family requested cesarean section.
Variables
The main outcome was progression of cervical dilation during labor. This was recorded as zero (the start point) at the time of admission. Data on the times between each cervical examination and the start point were collected. Other variables included characteristics of the women, labor and delivery data, and information on the newborns.
Data sources
Measurements of cervical dilation and the state of fetal presentation were performed during pauses between uterine contractions by two midwifes who were properly trained and experienced. Usually, when the diameter was <3cm, measurement was carried out every 4 hours. When cervical dilation was 3–7 cm, measurement was carried out every 2 hours. When cervical dilation was >7 cm, measurement was carried out every hour. However, when there was rupture of the membranes, intensive contraction, the urge to push, and increased vaginal secretions occurred, the number of measurements was increased.
Statistical analysis
All statistical analyses were performed using SAS 9.2 (SAS Institute, Cary, NC, USA). We used the multinomial model to repeat measures and analysis and depict the average labor curves. We followed the same approach undertaken by Zhang et al.2 In brief, we estimated the distribution of times for progression from one integer centimeter of dilation to the next, and depicted the 95th percentiles of cumulative duration of labor. Regression analysis of interval-censored data was performed. The independent sample t-test or paired t test was used for comparison among groups. Data that were not normally distributed are presented as the median (5th percentile, 95th percentile). The Mann–Whitney test was used for comparison of these data among groups. Qualitative data are shown as frequency and percentage. The χ2 test was used for comparison of these data among groups. P < 0.05 was used for all comparisons.
Results
A total of 657 pregnant Chinese women with VBAC were studied. Baseline characteristics of the two groups are shown in Table 1. Mean maternal weight at delivery in the non-trial of labor group was significantly heavier than that in the trial of labor group (P < 0.001). The mean Bishop score at admission in the trial of labor group was significantly higher than that in the non-trial of labor group (P < 0.001).
Table 1.
Characteristics of parturients in the two groups.
|
Groups |
||||
|---|---|---|---|---|
| Trial of labor | Non-trial of labor | t/χ2 | P | |
| Number of women studied | 170 | 487 | ||
| Maternal age (mean ± SD, years) | 31.14 ± 3.81 | 31.16 ± 3.60 | 0.04 | 0.97 |
| Maternal stature (mean ± SD, m) | 1.59 ± 0.05 | 1.60 ± 0.05 | 4.12 | <0.001 |
| Maternal weight before pregnancy (mean ± SD, kg) | 51.88 ± 5.96 | 53.80 ± 8.48 | 2.54 | 0.01 |
| Maternal weight at delivery (mean ± SD, kg) | 64.85 ± 7.29 | 67.12 ± 7.88 | 3.09 | <0.001 |
| BMI before pregnancy (mean ± SD, kg/m2) | 20.63 ± 2.20 | 20.88 ± 3.10 | 0.92 | 0.36 |
| BMI at delivery (mean ± SD, kg/m2) | 25.77 ± 2.54 | 26.06 ± 2.70 | 1.12 | 0.26 |
| Gravidity | 2.88 ± 1.04 | 2.72 ±0.91 | 1.68 | 0.09 |
| Parity | 1.02 ± 0.16 | 1.02 ± 0.14 | −0.31 | 0.76 |
| Gestational weeks | 38.90 ± 1.02 | 39.02 ± 1.38 | 1.04 | 0.30 |
| Maternal abdominal circle | 97.05 ± 7.09 | 98.59 ± 5.12 | 2.84 | 0.01 |
| Uterine height | 34.05 ± 5.65 | 33.79 ± 1.63 | −0.85 | 0.39 |
| Bishop score | ||||
| At admission | 6.07 ± 2.30 | 5.19 ± 1.97 | 4.425 | <0.001 |
| Entering the delivery room | 7.91 ± 1.43 | 7.82 ± 1.20 | 0.736 | 0.46 |
| Birth weight | 3200 ± 340 | 3250 ± 340 | 1.62 | 0.11 |
| Days of hospital stay (days) | 3.76 ± 1.41 | 4.09 ± 1.63 | 2.17 | 0.03 |
| Duration interval of two deliveries (years)* | 5 (2, 10) | 5 (2, 11) | 1.24 | 0.22 |
*Data are median (5th, 95th percentiles). SD: standard deviation; BMI: body mass index.
The duration of labor in the two groups is shown in Table 2. The 95th percentile for the first stage of labor in VBAC was 13.03 hours. The 95th percentile for the total stage of labor in VBAC was 14.15 hours. There were no significant differences in the duration of labor in the first, second, and total stages of labor between the groups.
Table 2.
Duration of labor of pregnant women in the two groups
|
Groups |
|||
|---|---|---|---|
| Duration of labor | Trial of labor | Non-trial of labor | P |
| Total stage (hours) | 5.94 (2.76, 13.18) | 5.93 (2.13, 14.15) | 0.57 |
| First stage (hours) | 5.29 (2.17,12.50) | 5.50 (1.75,13.03) | 0.52 |
| Second stage (hours) | 0.40 (0.17, 1.06) | 0.37 (0.10, 1.20) | 0.22 |
Data are median (5th, 95th percentiles).
Table 3 shows the 95th percentiles of progress in the duration of labor from 3–10 cm in the two groups. Labor accelerated after 4 cm of cervical dilation in both groups. There was no significant difference in the dilation rate at 3–6 cm between the two groups. The dilation rate in the trial of labor group was superior to that in non-trial of labor group at 6–10 cm, with significant differences between the groups (all P < 0.05).
Table 3.
Cumulative duration required for each 1-cm expansion of cervical dilation in the two groups.
|
Groups |
|||||
|---|---|---|---|---|---|
|
Trial of labor |
Non-trial of labor |
||||
| Cervical dilation (cm) | Number of women | Duration (hours) | Number of women | Duration (hours) | P |
| 3–4 | 82 | 0.74 (1.27) | 118 | 1.02 (1.62) | 0.14 |
| 4–5 | 39 | 0.49 (1.91) | 66 | 0.57 (1.45) | 0.61 |
| 5–6 | 34 | 0.33 (1.89) | 52 | 0.36 (2.76) | 0.69 |
| 6–7 | 24 | 0.29 (1.81) | 51 | 0.32 (2.63) | 0.03 |
| 7–8 | 39 | 0.25 (0.74) | 63 | 0.28 (2.07) | 0.00 |
| 8–9 | 81 | 0.22 (0.56) | 95 | 0.27 (1.27) | 0.00 |
| 9–10 | 96 | 0.21 (0.46) | 127 | 0.26 (1.26) | 0.00 |
Note: data that exceeded 1 cm of expansion between examinations were not included in the analysis. Data are median (95th percentile).
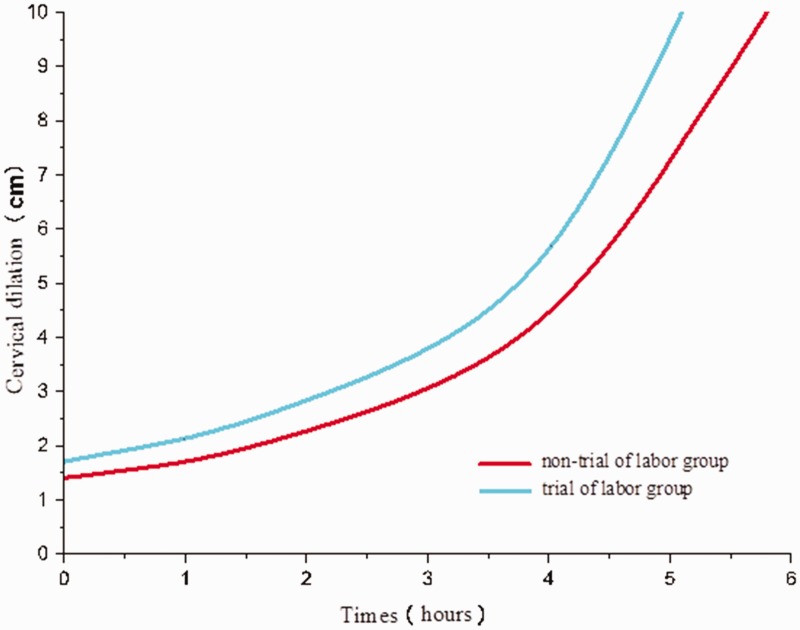
Figure 1 shows the labor curves in the two groups. The two groups showed a similar trend, with the absence of a deceleration phase. Before cervical dilation at 4cm, the slope of the curve was gradual. Labor appeared to accelerate after 4cm and the slope was greatest after 6 cm. The slope in the trial of labor group was increased earlier than that in the non-trial of labor group.
Figure 1.
Average labor curves of women in the two groups.
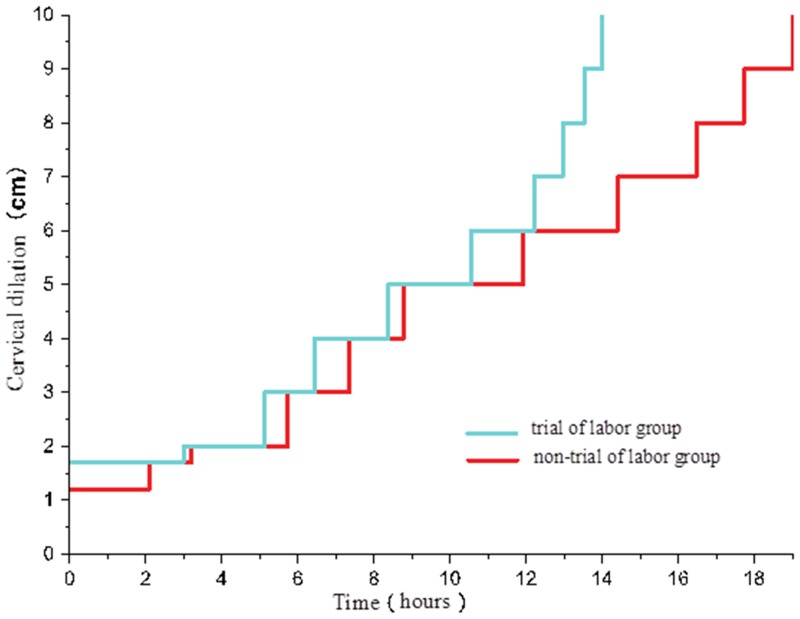
The 95th percentiles of cervical dilation are plotted as connected staircase lines in Figure 2.
Figure 2.
Comparison of the 95th percentiles of the cumulative duration of labor in the two groups.
Discussion
Duration of the first stage of labor
In 2010, Zhang et al.2 used interval-censored regression to estimate the duration of labor and found that the duration of the first stage of labor lasted for 20 hours. We used the same statistical methods as Zhang et al.2 We found that the duration of labor in the trial of labor and non-trial of labor groups lasted for 14 and 19 hours, respectively, which are shorter times than those reported by Zhang et al.2 (Figure 2). The study by Zhang et al.2 excluded women whose cervix was dilated >6 cm at admission, probably thus excluding many of the most rapid labors. In our study, all parturients with VBAC, regardless of how large the cervix was dilated at admission, were included. This may be the reason for the shorter duration in our study than in Zhang et al.’s study.2
Deceleration phase
Studies by Friedman1 and Incerti et al.10 found that the deceleration phase appeared when cervical dilation was 9–10 cm. Zhang et al.2 found that there was no significant deceleration phase in labor. No deceleration phase was observed in a study by Suzuki et al.11 regarding labor of Japanese primipara and in a study by Shi et al.3 regarding labor of Chinese primiparas.
In our study, we did not find any deceleration phase in labor of parturients with VBCA (Figure 1). Some previous studies showed that labor failed to show a deceleration phase,2,3,11 but they acknowledged that this phase was present in women who delivered by cesarean who were excluded from their analysis. Therefore, the absence of a deceleration phase in the average curves in these previous studies was a result of patient selection. This also explains why there was no deceleration phase in parturients with vaginal delivery and normal perinatal outcomes. If there is a deceleration phase in the labor, it may indicate dystocia.
Acceleration phase
Friedman1 found that the acceleration phase appeared when cervical dilation was 3–4 cm. A study by Zhang et al.2 suggested that there was no obvious acceleration phase in primiparas, and in multiparas, labor appeared to accelerate after 6 cm of cervical dilation. Shi et al.3 showed that the dilation speed was accelerated when cervical dilation was 5–6 cm in Chinese primiparas, but no accelerated inflection point was observed. We found that, in parturients with VBAC, labor was gradually accelerated when cervical dilation was 4–6 cm (Figure 1).
Duration of the active phase
Zhang et al.2 calculated the duration required for each 1-cm expansion of the parturients’ cervix. These authors proposed to set the duration of no significant expansion at 4, 5, and 6 cm as 6, 3, and 2 hours, respectively. In 2014, the Obstetric Group of the Obstetrics and Gynecology Branch of the Chinese Medical Association suggested the diagnostic criteria of arrest of labor as follows: rupture of the membranes and cervical dilation >6 cm, and the active phase stopped for 4 or 6 hours and was diagnosed as arrested labor if contractions were normal or poor.12 Zhang et al.13 believed that arrested labor should not be diagnosed when there is no obvious cervical dilation for more than 4 hours.
The current study showed that progress of labor in the trial of labor and non-trial of labor groups was similar when cervical dilation was <6 cm. However, when cervical dilation was >6 cm, the trial of labor group had a shorter duration of labor (Table 3 and Figure 2). This finding suggests that, when observing TOLAC, the duration of labor should be differentially treated according to the indications of previous cesarean section. For parturients with VBAC who underwent a trial of labor or non-trial of labor during the previous cesarean section, the 95th percentiles of the cumulative duration of labor from 6–7, 7–8, 8–9, and 9–10 cm of cervical dilation was 2 vs 3 hours, 1 vs 2 hours, 0.5 vs 1.5 hours, and 0.5 vs 1.5 hours, respectively. Therefore, for parturients with TOLAC, if cervical dilation is >6 cm, and the duration required for each 1-cm expansion exceeds the above-mentioned results, a senior obstetrician is required for further evaluation.
Duration of the second stage of labor
Treatments in the second stage of labor are closely related to outcomes of mothers and newborns. Along with prolongation in the second stage of labor, the incidence of postpartum hemorrhage and cesarean section is increased.14 When the second stage of labor lasts for longer than 3 hours, the incidence of blood transfusion treatment, neonatal asphyxia, neonatal intrapartum acidosis, and newborn hospitalization is significantly increased.15 Zhang et al.2 suggested that the 95th percentiles of the second stage of labor in nulliparas with and without epidural analgesia were 3.6 and 2.8 hours.
In 2012, the National Institute of Child Health and Human Development, Society for Maternal-Fetal Medicine, and American College of Obstetricians and Gynecologists jointly recommended the following standards for the second stage of labor: the duration of the second stage of labor for primiparas with and without epidural anesthesia should be 4 and 3 hours, and that for multiparas with and without epidural anesthesia should be 4 and 3 hours, respectively.16–18 Zhang et al.’s study2 included low-risk parturients in resource-rich medical institutions. Zhao and Fan19 studied labor of high-risk parturients, and they believed that different standards for the second stage of labor should be used for different populations.
In our study, the 95th percentile of the duration of the second stage of labor in all women was 1.18 hours, with good outcomes of mothers and newborns. The duration of labor in the previous trial of labor group was shorter than that in the non-trial of labor group (1.06 vs 1.2 hours), but this difference was not significant. Our findings on women with VBAC and non-epidural anesthesia suggest that when the duration of the second stage of labor reaches 1.0 hour, whether vaginal delivery should be performed can be decided. If the fetus has not been delivered yet, waiting should be avoided and a senior obstetrician is required to evaluate whether to continue the vaginal trial to reduce poor outcomes of mothers and newborns.
Strength and limitations
We investigated the patterns of labor in Chinese women in Fuzhou who attempted VBAC from different perspectives. The data and the research methods in this study are reliable and credible, and they provide a relevant theoretical basis for follow-up studies. However, subsequent studies may need to perform specific analysis methods to solve specific issues. This study was performed in a single-center, which is a limitation of this retrospective study. Therefore, multicenter, large-sample studies on VBAC are required in the future.
Conclusions
Management of labor in parturients with TOLAC whose cervical dilation is >6 cm should be treated differently according to previous cesarean section with or without a trial of labor. If there is a trial of labor in a previous delivery, the duration of labor should be shortened.
Declaration of conflicting interest
The authors declare that there is no conflict of interest.
Funding
This study was approved by the Fujian Science and Technology Project (2018Y0005), the Fujian Medical Innovation Subject (2017-CX-11), the Key Clinical Specialty Discipline Construction of Fujian, P.R.C. ([2015] no. 593) and the Fujian Provincial Health and Family Planning Commission Youth Research Project (2017-2-11).
ORCID iD
Jianying Yan https://orcid.org/0000-0003-2363-3065
References
- 1.Friedman EA. Primigravid labor: a graphicostatistical analysis. Obstet Gynecol 1955; 6: 567–589. [DOI] [PubMed] [Google Scholar]
- 2.Zhang J, Landy HJ, Ware BD, et al. Contemporary patterns of spontaneous labor with normal neonatal outcomes. Obstet Gynecol 2010; 116: 1281–1287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shi Q, Tan XQ, Liu XR, et al. Labor patterns in Chinese women in Chongqing. BJOG 2016; 123: 57–63. [DOI] [PubMed] [Google Scholar]
- 4.Zhu L, Zhang XY. 2013-2014 Analysis of cesarean rate and indications of cesarean in Beijing Haidian District Maternity and Child Care Centers. Chin J Clin Obstet Gynecol 2015; 3: 248–249. [Google Scholar]
- 5.Jie QG, Yang ZY, Xin YX. Analysis of indications of 5706 cesarean before and after the opening of two-child policy. J Tongji Univ 2017; 38: 90–93. [Google Scholar]
- 6.Curtin SC, Gregory KD, Korst LM, et al. Maternal morbidity for vaginal and cesarean deliveries, according to previous cesarean history: new data from the birth certificate, 2013. Nati Vital Stat Rep 2015; 64: 1–13. [PubMed] [Google Scholar]
- 7.Rossi AC, D'Addario V. Maternal morbidity following a trial of labor after cesarean section vs elective repeat cesarean delivery: a systematic review with meta-analysis. Am J Obstet Gynecol 2008; 199: 224–231. [DOI] [PubMed] [Google Scholar]
- 8.Silver RM, Landon MB, Rouse DJ, et al. Maternal morbidity associated with multiple repeat cesarean deliveries. Obstet Gynecol 2006; 107: 1226–1232. [DOI] [PubMed] [Google Scholar]
- 9.Nisenblat V, Barak S, Ohel G, et al. Maternal complications associated with multiple cesarean deliveries. Obstet Gynecol 2006; 108: 21–26. [DOI] [PubMed] [Google Scholar]
- 10.Incerti M, Locatelli A, Ghidini A, et al. Variability in rate of cervical dilatation in nulliparous women at term. Birth 2011; 38: 30–35. [DOI] [PubMed] [Google Scholar]
- 11.Suzuki R, Horiuchi S, Ohtsu H. Evaluation of the labor curve in nulliparous Japanese women. Am J Obstet Gynecol 2010; 203: 226.e1–226e6. [DOI] [PubMed] [Google Scholar]
- 12.The Obstetric Group of Obstetrics and Gynecology Branch of Chinese Medical Association. Specialist consensus on new labor standards and treatment. Chin J Obstet Gynecol 2014; 49: 486. [Google Scholar]
- 13.Zhang J, Yang ZJ, Huo XN. Progress in the study of partogragh. Chinese Journal of Perinatology Medicine 2014; 17: 145–147. [Google Scholar]
- 14.Li WH, Zhang HY, Ling Y, et al. Effect of prolonged second stage of labor on maternal and neonatal outcomes. Asian Pac J Trop Med 2011; 5: 409–411. [DOI] [PubMed] [Google Scholar]
- 15.Bleich AT, Alexander JM, McIntire DD, et al. An analysis of second-stage labor beyond 3 hours in nulliparous women. Am J Perinatol 2012; 29: 717–722. [DOI] [PubMed] [Google Scholar]
- 16.Safe prevention of the primary cesarean delivery. Obstetric Care Consensus No. 1. American College of Obstetricians and Gynecologists. Obstet Gynecol 2014; 123: 693–711. [DOI] [PubMed] [Google Scholar]
- 17.Spong CY, Berghella V, Wentrom KD, et al. Preventing the first cesarean delivery: summary of a joint Eunice Kennedy Shriver National Institute of Child Health and Human Development, Society for Maternal-Fetal Medicine, and American College of Obstetricians and Gynecologists Workshop. Obstet Gynecol 2012; 120: 1181–1193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Levneo KJ, Nelson DB, McIntire DD. Second-stage labor: how long is too long? Am J Obstet Gynecol 2016; 214: 484–489. [DOI] [PubMed] [Google Scholar]
- 19.Zhao RF, Fan L. Duration of second stage of labor and outcomes of mothers and infants of different high-risk parturients in new model of labor. Chinese Journal of Perinatology Medicine 2016; 19: 836–841. [Google Scholar]