Abstract
Background
The expansion of Medicaid as part of the Affordable Care Act opened new opportunities to provide health coverage to low-income adults who may be involved in other public sectors.
Objective
The main objective of this study was to describe cross-sector utilization patterns among urban Medicaid expansion enrollees.
Research Design
We merged data from 4 public sectors (health care, human services, housing, and criminal justice) for 98,282 Medicaid expansion enrollees in Hennepin County, MN. We fit a latent class model to indicators of cross-sector involvement.
Measures
Indicator variables described involvement levels within each sector from March 2011 through December 2014. Demographic and chronic condition indicators were included post hoc to characterize classes.
Results
We found 6 archetypes of cross-sector involvement: The “Low Contact” class (33.9%) had little involvement in any public sector; “Primary Care” (26.3%) had moderate, stable health care utilization; “Health and Human Services” (15.3%) had high rates of health care and cash assistance utilization; “Minimal Criminal History” (11.0%) had less serious criminal justice involvement; “Cross-sector” (7.8%) had elevated emergency department use, involvement in all 4 sectors, and the highest prevalence of behavioral health conditions; “Extensive Criminal History” (5.7%) had serious criminal justice involvement. The 3 most expensive classes (Health and Human Services, Cross-sector, and Extensive Criminal History) had the highest rates of behavioral health conditions. Together, they comprised 29% of enrollees and 70% of total public costs.
Conclusions
Medicaid expansion enrollees with behavioral health conditions deserve focus due to the high cost-reduction potential across public sectors. Cross-sector collaboration is a plausible path to reduce costs and improve outcomes.
Keywords: Medicaid expansion, social determinants of health, latent class analysis, cost, behavioral health, housing, criminal justice
The Affordable Care Act (ACA) allowed states to expand Medicaid to low-income, childless adults. These newly covered adults are disproportionately involved in health and non-health public sectors (ie, human services, housing, and criminal justice).1 In previous work, we found that urban Medicaid expansion enrollees in Hennepin County, MN visited the emergency department (ED) or were hospitalized 3 times more often than the national average and had extensive contact with housing [shelters and supportive housing (13% of enrollees)], criminal justice (34%), and human service sectors [food support, cash support and case management (68%).1 Human services is the term used in Minnesota and several Midwestern states and, for the purposes of this paper, is synonymous with the term “social services” used in other jurisdictions]. Cross-sector approaches may offer an effective and efficient mechanism to improve health care outcomes and control costs among nonelderly adults enrolled in Medicaid. Given limited public sector resources, such partnerships would ideally prioritize subpopulations with the greatest need and highest costs.
Within health care, a small subset of patients account for the majority of service use and costs.2 For this reason, research has focused on narrow population segments known to be high utilizers of health care, such as individuals with substance use disorders (SUDs),3,4 homelessness,5,6 mental illness (MI),7–9 or multimorbidity.10,11 High health care utilizers also incur higher costs in other sectors, suggesting that cost-drivers across public sectors may be similar.12 For this reason, connections between public sectors have received increased attention (eg, health care costs and supportive housing,13 health insurance and jail bookings,14 multiple sectors15). Although some organizations now utilize integrated cross-sector data for evaluation, these data have not been extensively leveraged to explore the comprehensive network of public sector interactions for the Medicaid expansion population.16,17 A more robust description and segmentation of service patterns among populations that consume a large portion of services across sectors, such as the Medicaid expansion population, would expand and improve on previous efforts to estimate cross-sector utilization. Specifically, it could provide further insight into the cross-sector involvement of health care high utilizers suggested in our previous work and help health care providers,12 social services and criminal justice agencies understand the total public sector experience of people under their care to improve service delivery and interventions.
The objective of this study was to identify distinct, cross-sector service use patterns among Medicaid expansion enrollees and compare costs across groups. In order to provide a more concise and nuanced examination of cross-sector patterns than is available through descriptive statistics, we used latent class analysis (LCA) to identify cross-sector involvement patterns across 4 public sectors: (1) health care; (2) human services; (3) criminal justice; and (4) housing. We then compared public sector investment across subpopulations using total cross-sector costs.
METHODS
Study Cohort
The study cohort included all persons in Hennepin County who enrolled in Medicaid through the ACA’s Medicaid expansion provisions any time from March 1, 2011 to December 31, 2014. Minnesota expanded Medicaid in 2011 to nondisabled adults aged 21–64 years with no dependent children and income up to 75% (138% since 2014) of the Federal Poverty Level (FPL).
Data Sources
We merged health care, human services, criminal justice, and housing (including supportive housing and shelter involvement) data from March 2011 to December 2014 using administrative records from state and county data systems in Minnesota (see Table 1, Supplemental Digital Content 1, http://links.lww.com/MLR/B646 for data sources). Health care, human services, and housing records were matched using unique identifiers maintained by the Minnesota Department of Human Services, whereas criminal justice data were matched on name and date of birth using probabilistic matching software (LinkPlus).18 We included all Medicaid expansion enrollees, regardless of Medicaid enrollment duration. Further, while health care claims describe only enrolled months, other data comprehensively describe service use during the study period regardless of Medicaid enrollment. This study was approved by the Minneapolis Medical Research Foundation Institutional Review Board.
Indicator Variables
The indicator variables used in the LCA model reflected levels of involvement in each sector (Table 1). No demographic or diagnosis information was entered into the LCA model. We recoded continuous and count variables as ordinal and categorical variables to create clusters revelant to policymakers and practitioners.
TABLE 1.
Indicator Variables
| Indicators | Level | N (%) |
|---|---|---|
| Emergency department visits* | 0 | 52,217 (53) |
| 1 or 2 | 36,801 (37) | |
| 3+ | 9264 (9) | |
| Primary care visits* | 0 | 43,285 (44) |
| 1 to 3 | 19,929 (20) | |
| 4+ | 35,068 (36) | |
| Inpatient admissions* | 0 | 80,647 (82) |
| 1 | 14,397 (15) | |
| 2+ | 3238 (3) | |
| Food and cash support | Food support (SNAP) | 63,435 (65) |
| MFIP (TANF) | 6062 (6) | |
| General assistance | 25,108 (26) | |
| Social Security or Medicare dual eligible | 7458 (8) | |
| MHCP† insurance (any type) | 1–179 | 10,382 (11) |
| 180–364 | 17,766 (18) | |
| 365–729 | 27,021 (27) | |
| 730+ | 43,113 (44) | |
| Case management | Any Hennepin County case management | 4898 (5) |
| Supportive housing | 0 d | 88,535 (90) |
| < 365 d total | 4166 (4) | |
| ≥ 365 d total | 5581 (6) | |
| Emergency shelter | 0 d | 91,453 (93) |
| < 365 episode days | 4691 (5) | |
| ≥ 365 episode days | 2138 (2) | |
| Detention bookings | 0 | 72,826 (74) |
| 1 or 2 | 12,943 (13) | |
| 3+ | 12,513 (13) | |
| Criminal justice consequences | Any Hennepin supervision | 20,461 (21) |
| Any county incarceration | 7976 (8) | |
| Any state incarceration | 4713 (5) | |
| Court convictions | Gross misdemeanor or misdemeanor | 18,855 (19) |
| Felony | 8335 (8) | |
| Person crime | 7054 (7) |
Rate per 12 months of MHCP enrollment.
MHCP, including Medicaid.
MFIP indicates Minnesota Family Investment Program; MHCP, Minnesota Health Care Programs; SNAP, Supplemental Nutrition Assistance Program; TANF, Temporary Assistance for Needy Families.
We summarized health care utilization as rates of ED, primary care, and inpatient visits per 12 Minnesota Health Care Programs (MHCPs) enrollment months, each recoded as ordinal variables with 3 levels: ED (0, 1–2, or 3+ visits), hospitalization (0, 1, 2+), and primary care (0, 1–3, 4+). Cut points were chosen based on relevant literature2 and practice definitions for cases worthy of extra attention at Hennepin County Medical Center; high primary care use was further based on having visits at least quarterly.
We coded human services enrollment using binary variables for whether an individual had any enrollment during the study period in: (1) the Supplemental Nutrition Assistance Program; (2) the Minnesota Family Investment Program (MFIP) (ie, Minnesota’s administration of the federal Temporary Assistance for Needy Families cash assistance program); (3) General Assistance, a Minnesota cash assistance program for adults with disabilities not on Social Security; (4) Social Security or Medicare enrollment as determined by income, MHCP, and Medicaid waiver records; or (5) Hennepin County case management, that is, on a social worker’s case load for adult behavioral health, child welfare, or disability.
We categorized public health insurance enrollment according to total cumulative time of MHCP enrollment, coded ordinally to reflect cutoffs at 6 months, 1 year, and 2 years (0–179; 180–364; 365–729 d; 730+ d). Medicaid expansion eligibility made up the majority of all MHCP enrollment months, although counts also included enrollment in other types of Medicaid, as well as programs such as MinnesotaCare (public health insurance for people with incomes just above Medicaid thresholds) and Institutions for Mental Diseases.
Housing consisted of 2 variables measuring time spent in supportive housing and emergency shelters. We measured days in supportive housing ordinally based on Hennepin County’s focus on maintaining housing for at least 1 year (0, 1–365, or 365+ days). Following common practice in Hennepin County shelter analyses, we estimated shelter utilization from episodes of continuous or intermittent shelter stays, coded based on a 1-year equivalent (0, 1–365, or 365+ episode days).
We summarized criminal justice involvement based on 5 indicators summarizing pretrial detention, posttrial consequences, and convictions. We measured statewide detention bookings (ie, in county jails), coded ordinally (0, 1–2, 3+ bookings). For posttrial consequences, we created 3 nominal variables indicating consequences experienced during the study period: community supervision (including probation, parole, and community service); county incarceration (adult corrections facilities, typically for sentences <1 y); and state incarceration (prison, typically for sentences >1 y). For court convictions, we indicated whether someone was ever convicted during the study period of a felony or a gross misdemeanor/misdemeanor, and whether the offense was a crime against a person (eg, assault, robbery) or society (eg, forgery, drugs, theft) (see Glossary, Supplemental Digital Content 1, http://links.lww.com/MLR/B646 for definitions of terms used in this section).
Analysis
We conducted LCA using Latent Gold 5.1.19 We determined the number of classes using Bayesian Information Criterion from out-of-sample testing on 10 random samples of 2000 enrollees with replacement. The large size of the study population would have resulted in high dimensionality and, as a result, far more classes than would be analytically interpretable. Among the 10 samples, 6 suggested a 6-class solution, with other solutions ranging from 5 to 8 classes (see Table 2, Supplemental Digital Content 1, http://links.lww.com/MLR/B646 for Bayesian Information Criterion loglikelihood results for 10 random samples with replacement). We applied the 6-class model to the entire data set to arrive at the final latent class results.
Descriptive Analysis
We used demographic and diagnosis variables to characterize each latent class in a descriptive analysis following the LCA. Demographic data came exclusively from MHCP administrative records and included sex, age, race/ethnicity, preferred language, and marital status. Physical chronic health, SUD, and MI diagnoses were categorized from International Classification of Diseases, Ninth Revision codes using Chronic Condition Indicator (CCI) categories from the Healthcare Cost and Utilization Project (HCUP).20 Enrollees were classified as having an MI or SUD diagnosis if they had ≥ 1 diagnoses in their inpatient, outpatient, professional or skilled nursing facility claims during the study period.
Cost Estimation
We estimated public health care costs using available Minnesota Medicaid fee schedules, Centers for Medicare and Medicaid Services drug cost averages,21,22 and HCUP State Inpatient Database Diagnosis-Related Group per diem averages for hospital stays.23 Public health care cost estimates were not adjusted for MHCP enrollment. Emergency shelter, community supervision, jail, and county and state incarceration costs were calculated using per diem estimates from Minnesota state and local government agencies.24 Human services costs, including food and cash support, as well as supportive housing costs, were calculated from observed payments. Case management costs were calculated from per minute averages for time Hennepin County staff spent on human services cases and observed service authorization amounts. Administrative costs for human services were calculated from Hennepin County and Minnesota state averages.25 All costs represent 2014 dollar values (see Table 1, Supplemental Digital Content 1, http://links.lww.com/MLR/B646 for detailed cost estimation methods)
Missing Data
Missing data were limited. Race, preferred language, and marital status were missing in 8.9%, 3.2%, and 1.0% of cases, respectively, and reported as “unknown.” Detention bookings and case management events with missing end dates were imputed using the median length of stay and represented <1% of cases. Group Residential Housing data lacked end dates in 23% of cases, therefore we imputed missing end dates from monthly Group Residential Housing financial records. Costs for inpatient, outpatient, and professional claims without an available cost value were omitted from cost estimates and represented <10% of claims. We omitted these claim amounts rather than impute them because claim-level cost estimates were highly skewed, risking cost overestimation; we preferred more conservate cost estimates. Criminal justice facilities and case management events without corresponding per diem estimates were assigned average values for the facility or case type (<1% of cases).
RESULTS
Demographics
During the first 46 months of the Medicaid expansion, 98,282 Hennepin County residents enrolled in Medicaid via expansion eligibility, ~13% of the total nonelderly adult population in Hennepin County. Expansion enrollees were predominantly men, white or Black/African-American, English-speaking, and unmarried, with a median age of 37 (Table 2). MI and SUD diagnoses were common.
TABLE 2.
Demographics of Hennepin Medicaid Expansion Enrollees
| Hennepin Medicaid Expansion (N = 98,282) | |
|---|---|
| Sex (%) | |
| Women | 39.0 |
| Men | 61.0 |
| Race and ethnicity (%) | |
| White | 42.0 |
| Black/African-American | 36.5 |
| Asian/Pacific Islander | 4.6 |
| American Indian or Native American | 3.4 |
| Hispanic, any race | 2.7 |
| Multiracial | 1.9 |
| Unknown | 8.9 |
| Preferred spoken language (%) | |
| English | 88.9 |
| Other languages | 7.9 |
| Unknown | 3.2 |
| Marital status (%) | |
| Not married | 90.1 |
| Married | 8.9 |
| Unknown | 1.0 |
| Median age | 37 |
| Substance use disorder/mental illness diagnosis (%) | |
| Only MI diagnosis | 20.8 |
| Only SUD diagnosis | 5.9 |
| Both MI and SUD diagnoses | 20.6 |
| Average number of body systems affected by a chronic physical condition | 3.2 |
MI indicates mental illness; SUD, substance use disorder.
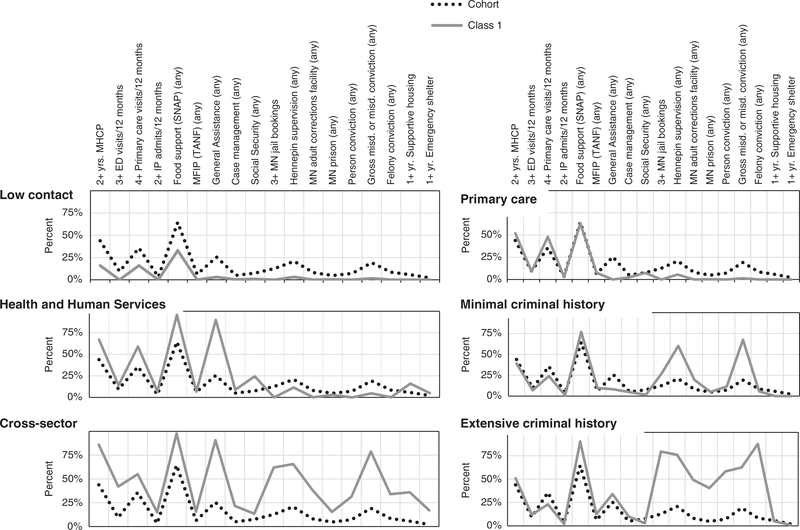
LCA
The LCA class solution produced 6 latent classes describing varying patterns of involvement across public sectors (Fig. 1). For ease of readability, we labelled each class with a name that typifies its cross-sector involvement pattern. The largest class, “Low Contact” (33,287 enrollees, 33.9% of the study cohort), had minimal involvement with any sector, although about one-third used food support (compared with almost two-thirds of all expansion enrollees). Another large class, “Primary Care” (25,837 enrollees, 26.3%) used primary care and some human services, but little else.
FIGURE 1.
Probability plot. ED indicates emergency department; MFIP, Minnesota Family Investment Program; MHCP, Minnesota Health Care Program; SNAP, Supplemental Nutrition Assistance Program; TANF, Temporary Assistance for Needy Families.
“Health and Human Services” and “Cross-sector,” shared high rates of overall health care utilization, but had differing rates of ED, housing, and criminal justice involvement. Health and Human Services (15,046 enrollees, 15.3%) had high rates of primary care utilization, were enrolled in public health care programs continually, and usually received cash assistance and food support. Health and Human Services had a moderate level of housing involvement, but criminal justice involvement was uncommon. Cross-sector (7685 enrollees, 7.8%) had higher levels of ED use and more extensive involvement with housing and criminal justice, including the largest share of housing-involved enrollees and the highest convicted gross misdemeanor/misdemeanor rate of any class.
The remaining 2 classes were primarily characterized by their criminal justice involvement. The “Minimal Criminal History” class (10,840 enrollees, 11.0%) had less serious criminal justice involvement (misdemeanors, community supervision, etc.), while the “Extensive Criminal History” class (5,587 enrollees, 5.7%) had more serious criminal justice involvement, with the highest rates of incarceration and felony conviction of any class. Neither class had high health care or housing involvement, though health and human services involvement were generally higher than Low Contact.
Descriptive Analysis
Demographic analyses following the LCA procedure revealed stark differences in demographics and health conditions between the classes (Table 3). Low Contact was disproportionately young (median age, 35 y), white (50.2%), and less medically complex (2.0% with SUD and MI diagnoses, 2.0 average body systems with a physical chronic condition diagnosis). Primary Care was more racially diverse (40.7%. white) and had more medical complexity than Low Contact (13.4% with SUD and MI diagnoses, average 3.2 body systems with a physical chronic condition) and was the only class with a majority women (51.2%). Low Contact and Primary Care classes also had the lowest percentages of enrollees who chose English as their preferred language (85.5% and 85.7%, respectively), suggesting that immigrants were disproportionately represented in these low cross-sector use patterns. Health and Human Services was the oldest class (median age, 50 y), and more racially diverse than Low Contact or Primary Care. Health and Human Services had high average physical morbidity (4.3 body systems with a physical chronic condition) and high rates of MI diagnosis (71.4%), though SUD rates were not as high as the Cross-sector and Extensive Criminal History classes (46.6% vs. 86.1% and 54.5%, respectively).
TABLE 3.
Demographic and Diagnosis Characteristics by Class
| Hennepin Medicaid Expansion (N = 98,282) | Low Contact (N = 33,287) | Primary Care (N = 25,837) | Health and Human Services (N = 15,046) | Minimal Criminal History (N = 10,840) | Cross-sector (N = 7685) | Extensive Criminal History (N = 5,587) | |
|---|---|---|---|---|---|---|---|
| Sex (%) | |||||||
| Women | 39.0 | 42.4 | 51.2 | 41.9 | 20.4 | 25.4 | 8.8 |
| Race and ethnicity (%) | |||||||
| White | 42.0 | 50.2 | 40.7 | 39.7 | 35.0 | 35.0 | 27.7 |
| Black/African-American | 36.5 | 25.2 | 37.5 | 44.1 | 45.1 | 43.0 | 53.0 |
| Asian/Pacific Islander | 4.6 | 7.1 | 4.9 | 3.1 | 2.7 | 0.7 | 1.8 |
| American Indian or Native American | 3.4 | 1.1 | 2.3 | 4.9 | 3.7 | 11.4 | 5.4 |
| Hispanic | 2.7 | 2.7 | 2.9 | 2.5 | 3.1 | 2.7 | 2.2 |
| Multiracial | 1.9 | 1.8 | 2.0 | 1.1 | 2.6 | 2.3 | 3.0 |
| Unknown | 8.9 | 11.8 | 9.7 | 4.6 | 7.8 | 4.9 | 6.9 |
| Preferred spoken language (%) | |||||||
| English | 88.9 | 85.5 | 85.7 | 89.9 | 94.7 | 98.3 | 97.3 |
| Other languages | 7.9 | 8.8 | 11.1 | 9.6 | 3.2 | 1.4 | 1.5 |
| Unknown | 3.2 | 5.8 | 3.1 | 0.5 | 2.1 | 0.4 | 1.3 |
| Marital status (%) | |||||||
| Not married | 90.1 | 86.1 | 86.9 | 94.6 | 95.5 | 97.4 | 96.9 |
| Married | 8.9 | 12.4 | 12.3 | 4.6 | 3.9 | 2.0 | 2.8 |
| Unknown | 1.0 | 1.5 | 0.8 | 0.8 | 0.6 | 0.6 | 0.3 |
| Median age | 37 | 35 | 36 | 50 | 32 | 38 | 32 |
| Substance use disorder/mental illness diagnosis (%) | |||||||
| Only MI diagnosis | 20.8 | 14.0 | 31.3 | 31.2 | 15.2 | 9.1 | 12.4 |
| Only SUD diagnosis | 5.9 | 1.4 | 4.8 | 6.4 | 12.4 | 8.2 | 20.5 |
| Both MI and SUD diagnoses | 20.6 | 2.0 | 13.4 | 40.2 | 20.5 | 77.9 | 34.0 |
| Average body systems affected by chronic physical conditions | 3.2 | 2.0 | 3.2 | 4.3 | 2.3 | 4.0 | 2.2 |
MI indicates mental illness; SUD, substance use disorder.
The Minimal Criminal History and Extensive Criminal History classes contained high proportions of young people (median age of 32 y for both), men (79.6% and 91.2%, respectively), and people of color (60.1% and 65.4%, respectively), especially African Americans (45.1% and 53.0%, respectively). Rates of MI diagnoses for these 2 justice-involved classes were lower than Health and Human Services and Cross-sector, but SUD diagnosis rates were above average. Most members of Cross-sector had a MI or SUD diagnosis (87.0% and 86.1%, respectively) and over 3 quarters had both (77.9%).
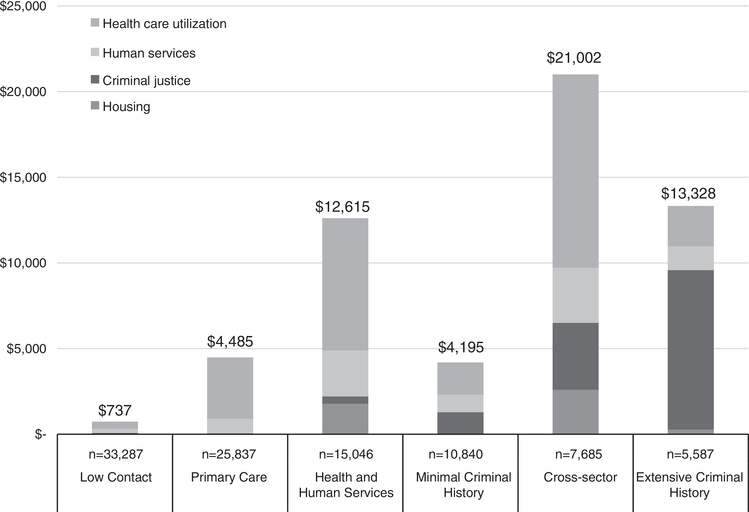
Cost Estimates
On a per person basis, Cross-sector incurred the highest public costs (Fig. 2). These enrollees had the highest per person medical, human services, and housing costs, as well as the second highest per person criminal justice costs. Among Cross-sector enrollees, public health insurance made up over half of all costs (53.7%), followed by criminal justice (18.6%), human services (15.3%), and housing (12.4%). Health and Human Services and Extensive Criminal History also incurred high total per person public costs, but in different ways. Health and Human Services incurred most costs through health care (61.3%), with the largest share going to housing of any class (14.1%). Although housing was not the main cost driver for Health and Human Services or Cross-sector, together these 2 classes accounted for almost all housing costs among Medicaid expansion enrollees (95.5%). Extensive Criminal History incurred most costs through criminal justice involvement (69.9%). Despite being the second smallest class, Cross-sector accumulated the largest total amount of annual non–health care costs ($74.7 million) and only trailed Health and Human Services in overall total annual public costs ($161.4 million vs. $189.8 million). Overall, Health and Human Services made up 31.0% of all public costs, followed by Cross-sector (26.4%), Primary Care (18.9%), Extensive Criminal History (12.2%), Minimal Criminal History (7.4%) and Low Contact (4.0%). Together, Health and Human Services, Cross-sector, and Extensive Criminal History represented 28.8% of enrollees and 69.6% of all public costs among Hennepin County Medicaid expansion enrollees.
FIGURE 2.
Annualized per person costs by class.
DISCUSSION
In this cross-sector analysis of Medicaid expansion enrollees in Hennepin County, we identified 6 patterns of service involvement (classes) across 4 sectors known to generate high public costs—health care, human services, criminal justice, and housing. This LCA result builds on previous research examining latent classes using only clinical and health care data26 by specifying groups’ sector-specific and total costs rather than high health care utilizers alone.12
Substantial research on health care high utilizers has focused on populations that might fit into the Health and Human Services class—older enrollees with chronic conditions often complicated by housing and/or behavioral health issues.10,27 However, our findings suggest that, within the Medicaid expansion, the situation is more complicated. The Health and Human Services, Primary Care, and Cross-sector classes all accounted for high overall health care costs themselves, but typified distinct patterns across sectors. In addition, classes could carry high total costs due to high per capita costs across sectors (eg, Class 5—Cross-sector), or high costs in 1 or 2 sectors (eg, Class 2—Primary Care).
The 6 classes identified in our LCAs raised different opportunities for cross-sector collaboration. For example, the Cross-sector class stood out due to the high prevalence of co-occurring behavioral health conditions. From previous literature, we expected Medicaid expansion enrollees to have higher rates of MI and SUD than other Medicaid populations, but it was surprising how closely behavioral health cooccurred with cross-sector utilization patterns.28 This co-occurrence suggests that behavioral health and high cost cross-sector patterns are closely related. Locally and nationally, health care,29,30 human services,31,32 housing,33 and criminal justice34,35 sectors are struggling to respond to the needs of people with MI and SUD. This means that health care interventions targeted to people in this class may have downstream effects on other sectors that would not occur for other classes. This dynamic would also work in reverse, where criminal justice policy changes around behavioral health could affect health care utilization for Cross-sector (and likely Extensive Criminal History). For these reasons, the Cross-sector class’s behavioral health and housing needs may require integrated community interventions that would be less relevant for other health or justice-involved enrollees.
Our finding of high costs in non–health care sectors underscores the importance of the role of social determinants of health. We reinforce previous observations about the high use of public services by homeless and unstably housed populations. Importantly, our findings also show that the criminal justice system was another important point of contact, aligning with other published literature underscoring the need to more deeply examine the health of those involved with the US criminal justice sector.36,37 This finding is especially important since criminal justice involvement is much more common in the United States than in other developed nations—US prisons and jails house the largest inmate population in the world, with millions more under community supervision.38 Additional research on the relationships between Medicaid expansion, criminal justice involvement, and access to other public sector resources (eg, housing, substance use treatment) are vital to ongoing debates related to Medicaid and social determinants of health.
Methodologically, LCA successfully added estimates of prevalence and intensity of service involvement across multiple public sectors to segment a large health care–enrolled population. This produced more nuanced classifications than are available through descriptive statistics and is thus more useful for identifying high cost subpopulations for adaptations to existing practice or the design of new research.
Limitations
We acknowledge multiple limitations. First, our analysis is cross-sectional and does not account for sequencing of cross-sector involvement over time. Second, some data were incomplete. For example, shelter data covered 75% of Hennepin County shelter beds, and supportive housing data did not cover all available units. Likewise, Medicare or private insurance data and health claims from care administered in another state or correctional facilities were unavailable. Third, probabilistic matching on name and date of birth for criminal justice records, which lacked any other common identifiers, meant that ~10% of criminal justice records went unmatched and unobserved. Fourth, health care costs were not adjusted for MHCP enrollment and thus may underestimate costs for enrollees with limited enrollment histories. Fifth, negotiated prices for health care claims were unavailable, requiring the use of fee schedules. Sources used for claims estimates are in line with similar, regional health care cost analyses. Sixth, for incarcerated persons, low health care use from claims did not necessarily indicate a lack of utilization—prisons and jails were the main source of health care during confinement, and these interactions were largely unobserved. Finally, while the underlying dynamics that govern our results are likely to exist in other urban areas in the United States, varying state and local policies may produce different results in other contexts.
Implications
Low-income adults enrolled in Medicaid have diverse patterns of involvement not only in health care, but across public sectors. Although high costs can arise from single sectors, the highest-cost class used multiple public sectors and had diagnoses of both SUD and MI. Overall, our findings suggest that siloed responses driven by single sectors are unlikely to meet the complex needs of the most costly low-income adults in Medicaid expansion. Health care delivery systems should partner with criminal justice, human service, and housing agencies to design integrated systems to support these complex patients.39 Some of this work is happening in our area, for example, in specialized courts such as Mental Health and Veteran’s Court, where clinical social workers act as court liaisons to help participants navigate health, human services, housing and criminal justice bureaucracies.40,41 Improved health outcomes may depend on such shared approaches. With recent interest in social determinants of health, cost-containment, and population health improvement, targeted cross-sector collaboration offers a plausible path to improved health outcomes and reduced costs.
Supplementary Material
ACKNOWLEDGMENTS
The authors thank Melissa Adkins, Tamra Boyce, Rob Kreiger, Center for Health Care Strategies for their contribution to this work.
Funded and supported from the Center for Health Care Strategies and the Rethinking Care Program: Innovations in Complex Care grant (#20141670) from the Kaiser Permanente Foundation.
Footnotes
The authors declare no conflict of interest.
Supplemental Digital Content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s website, www.lww-medicalcare.com.
REFERENCES
- 1.Bodurtha P, Van Siclen R, Erickson E, et al. Cross-Sector Service Use and Costs Among Medicaid Expansion Enrollees in Minnesota’s Hennepin County. Hamilton, NJ: Center for Health Care Strategies Inc; 2017. Available at: www.chcs.org/media/Hennepin-Research-Brief_103017.pdf Accessed November 2, 2017. [Google Scholar]
- 2.Johnson TL, Rinehart DJ, Durfee J, et al. For many patients who use large amounts of health care services, the need is intense yet temporary. Health Aff (Millwood). 2015;34:1312–1319. [DOI] [PubMed] [Google Scholar]
- 3.Gryczynski J, Schwartz RP, O’Grady KE, et al. Understanding patterns of high-cost health care use across different substance user groups. Health Aff (Millwood). 2016;35:12–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Whitesell NR, Beals J, Mitchel CM, et al. Latent class analysis of substance use: comparison of two american indian reservation populations and a national sample. J Stud Alcohol. 2006;67:32–43. [DOI] [PubMed] [Google Scholar]
- 5.Fazel S, Geddes JR, Kushel M. The health of homeless people in high-income countries: descriptive epidemiology, health consequences, and clinical and policy recommendations. Lancet. 2014;384:1529–1540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hwang SW, Burns T. Health interventions for people who are homeless. Lancet. 2014;384:1541–1547. [DOI] [PubMed] [Google Scholar]
- 7.Ahn J, McCombs JS, Jung C, et al. Classifying patients by antipsychotic adherence patterns using latent class analysis: characteristics of nonadherent groups in the California Medicaid (Medi-Cal) Program. Value Health. 2008;11:48–56. [DOI] [PubMed] [Google Scholar]
- 8.Young AS, Chinman MJ, Cradock-O’Leary JA, et al. The relationship between mental disorders and medical service utilization in a representative community sample. Community Ment Health J. 2005;41:159–168.15974496 [Google Scholar]
- 9.Gilmer TP, Stefancic A, Ettner SL, et al. Effect of full-service partnerships on homelessness, use and costs of mental health services, and quality of life among adults with serious mental illness. Arch Gen Psychiatry. 2010;67:645–652. [DOI] [PubMed] [Google Scholar]
- 10.Lehnert T, Heider D, Leicht H, et al. Review: health care utilization and costs of elderly persons with multiple chronic conditions. Med Care Res Rev. 2011;68:387–420. [DOI] [PubMed] [Google Scholar]
- 11.Elixhauser A, Steiner C, Harris RD, et al. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27. [DOI] [PubMed] [Google Scholar]
- 12.Vickery KD, Bodurtha P, Winkelman TNA, et al. Cross-sector service use among high health care utilizers in minnesota after medicaid expansion. Health Aff (Millwood). 2018;37:62–69. [DOI] [PubMed] [Google Scholar]
- 13.Wright BJ, Vartanian KB, Li H-F, et al. Formerly homeless people had lower overall health care expenditures after moving into supportive housing. Health Aff (Millwood). 2016;35:20–27. [DOI] [PubMed] [Google Scholar]
- 14.Regenstein M, Rosenbaum S. What the affordable care act means for people with jail stays. Health Aff (Millwood). 2014;33:448–454. [DOI] [PubMed] [Google Scholar]
- 15.DiPietro B, Klingenmaier L. Achieving public health goals through medicaid expansion: opportunities in criminal justice, homelessness, and behavioral health with the patient protection and Affordable Care Act. Am J Public Health. 2013;103 (S2):e25–e29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fan J, Lucenko B, Esteee S, et al. Improving Employment Outcomes for People With Mental Health Disorders in Washington State. Olympia, WA: Washington State Department of Social & Health Services; 2016. Available at: www.dshs.wa.gov/sesa/rda/research-reports/improving-employment-outcomes-people-mental-health-disorders-washington-state. Accessed July 7, 2018. [Google Scholar]
- 17.Ford Shah M, Liu Q, Eddy M, et al. Predicting Homelessness Among Emerging Adults Aging Out of Foster Care. Olympia, WA: Washington State Department of Social & Health Services; 2016. Available at:www.dshs.wa.gov/sesa/rda/research-reports/predicting-homelessness-among-emerging-adultsaging-out-foster-care. Accessed July 7, 2018. [Google Scholar]
- 18.Registry Plus Link Plus. Division of Cancer Prevention and Control, Centers for Disease Control and Prevention. 2015. Available at: www.cdc.gov/cancer/npcr/tools/registryplus/lp.htm.
- 19.Latent GOLD 5.1. Statistical Innovations. 2016. Available at: www.statisticalinnovations.com/latent-gold-5-1/.
- 20.HCUP Databases. Healthcare Cost and Utilization Project (HCUP). Agency for Healthcare Research and Quality; 2017. Available at: www.hcup-us.ahrq.gov/sidoverview.jsp. [PubMed] [Google Scholar]
- 21.Centers for Medicare and Medicaid Services. NADAC (National Average Drug Acquisition Cost) (Data.Medicaid.gov). 2014. Available at: data.medicaid.gov/Drug-Pricing-and-Payment/NADAC-National-Average-Drug-Acquisition-Cost-/a4y5-998d Accessed February 7, 2018.
- 22.Centers for Medicare and Medicaid Services. State Drug Utilization Data (medicaid.gov). 2014. Available at: www.medicaid.gov/medicaid/prescription-drugs/state-drug-utilization-data/index.html. Accessed February 7, 2018.
- 23.Agency for Healthcare Research and Quality. HCUP State Inpatient Dataset, Minnesota (Healthcare Cost and Utilization Project, HCUP) 2014. Available at: www.hcup-us.ahrq.gov/sidoverview.jsp. Accessed February 7, 2018. [Google Scholar]
- 24.Minnesota Department of Corrections. Minnesota Department of Corrections Performance Report, 2014. St. Paul, MN: 2014. Available at: mn.gov/doc/assets/DOC_2014_Performance_Report_tcm1089-276177.pdf. Accessed February 7, 2018. [Google Scholar]
- 25.Minnesota Department of Human Services. Minnesota County Human Service Cost Report for Calendar Year 2014. St. Paul, MN: 2014. Available at: mn.gov/dhs/assets/minnesota-county-human-service-cost-report_tcm1053-165117.pdf. Accessed February 7, 2018. [Google Scholar]
- 26.Rinehart DJ, Oronce C, Durfee MJ, et al. Identifying subgroups of adult superutilizers in an urban safety-net system using latent class analysis: implications for clinical practice. Med Care. 2018;56:e1–e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Burt M, Wilkins C, Locke G. Medicaid and Permanent supportive housing for chronically homeless individuals: emerging practices from the field. US Department of Health And Human Services, Office of Disability, Aging and Long-Term Care Policy; 2014. Available at: aspe.hhs.gov/system/files/pdf/77116/EmergPrac.pdf. Accessed February 7, 2018. [Google Scholar]
- 28.Mark TL, Wier LM, Malone K, et al. National estimates of behavioural health conditions and their treatment among adults newly insured under the ACA. Psychiatr Serv. 2015;66:426–429. [DOI] [PubMed] [Google Scholar]
- 29.Kronick R, Bella M, Gilmer T. The faces of Medicaid III: refining the portrait of people with multiple chronic conditions. Center for Health Care Strategies (CHCS) 2009. Available at: www.chcs.org/media/Faces_of_Medicaid_III.pdf. Accessed July 7, 2018. [Google Scholar]
- 30.US Department of Health and Human Services, Office of the Surgeon General. Chapter 6: Health care systems and substance use disorder Facing Addiction in America: The Surgeon General’s Report on Alcohol, Drugs, and Health. Washington, DC: US Department of Health and Human Services, Office of the Surgeon General; 2016:61–6.71. Available at: https://addiction.surgeongeneral.gov/chapter-6-health-care-systems.pdf. Accessed July 7, 2018. [PubMed] [Google Scholar]
- 31.McAlpine DD, Boudreaux M, Call K, et al. Minnesota Department of Human Services. Estimating the need for treatment for substance abuse among adults in minnesota: results of the 2010 Minnesota Survey on Adult Substance Use. 2011. Available at: https://edocs.dhs.state.mn.us/lfserver/Public/DHS-6423A-ENG. Accessed July 7, 2018. [Google Scholar]
- 32.US Department of Health and Human Services. Leading Change 20: Advancing the Behavioral Health of the Nation, 2015–2018. Rockville, MD: US Department of Health and Human Services, Substance Abuse and Mental Health Services Administration; 2014. Available at: https://store.samhsa.gov/shin/content//PEP14-LEADCHANGE2/PEP14-LEADCHANGE2.pdf. Accessed July 7, 2018. [Google Scholar]
- 33.Pearson CL, Locke G, Montgomery AE, et al. The Applicability of Housing First Models to Homeless Persons with Serious Mental Illness. Washington, DC: US Department of Housing and Urban Development, Office of Policy Development and Research; 2007. Available at: www.huduser.gov/portal/publications/hsgfirst.pdf Accessed July 7, 2018. [Google Scholar]
- 34.Minnesota Judicial Branch Fourth Judicial District and Hennepin County Department of Community Corrections and Rehabilitation. Hennepin County Chemical Dependency Task Force: Final Recommendations for Adult Drug and DWI Offenses. Minneapolis, MN: Minnesota Judicial Branch Fourth Judicial District and Hennepin County Department of Community Corrections and Rehabilitation; 2006. Available at: www.mncourts.gov/mncourtsgov/media/scao_library/Drug%20Courts/4th%20District/DWI%20Court/HC_CD_Task_Force_Report_Adult.pdf. Accessed February 7, 2018. [Google Scholar]
- 35.Skeem JL, Manchak S, Peterson JK. Correctional policy for offenders with mental illness: Creating a new paradigm for recidivism reduction. Law Hum Behav. 2011;35:110–126. [DOI] [PubMed] [Google Scholar]
- 36.Wildeman C, Wang E. Mass incarceration, public health, and widening inequality in the USA. Lancet. 2017;389:1464–1474. [DOI] [PubMed] [Google Scholar]
- 37.Miller J Contemporary modes of probation officer supervision: the triumph of the “synthetic” officer? Justice Q. 2015;32:314–336. [Google Scholar]
- 38.Walmsley R World Prison Population List, Eleventh Edition. Institute for Criminal Policy Research; 2016. Available at: www.prisonstudies.org/sites/default/files/resources/downloads/world_prison_population_list_11th_edition_0.pdf. Accessed February 7, 2018. [Google Scholar]
- 39.Towe VL, Levton L, Chandra A, et al. Cross-sector collaborations and partnerships: essential ingredients to help shape health and well-being. Health Aff. 2016;35:1946–1969. [DOI] [PubMed] [Google Scholar]
- 40.Steadman HJ, Redlich A, Callahan L, et al. Effect of mental health courts on arrests and jail days: a multisite study. Arch Gen Psychiatry. 2011;68: 167–172. [DOI] [PubMed] [Google Scholar]
- 41.Johson M Hennepin County Veterans Court Evaluation Minneapolis. Minnesota: Judicial Branch—Fourth District; 2016. Available at: www.mncourts.gov/mncourtsgov/media/fourth_district/documents/Research/Veterans-Court-Evaluation-FINAL.pdf Accessed September 27, 2018. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.