Abstract
Background
Autoresuscitation describes the return of spontaneous circulation after termination of resuscitation (TOR) following cardiac arrest (CA). We aimed to identify phenomena that may lead to autoresuscitation and to provide guidance to reduce the likelihood of it occurring.
Materials and methods
We conducted a literature search (Google Scholar, MEDLINE, PubMed) and a scoping review according to PRISMA-ScR guidelines of autoresuscitation cases where patients undergoing CPR recovered circulation spontaneously after TOR with the following criteria: 1) CA from any cause; 2) CPR for any length of time; 3) A point was reached when it was felt that the patient had died; 4) Staff declared the patient dead and stood back. No further interventions took place; 5) Later, vital signs were observed. 6) Vital signs were sustained for more than a few seconds, such that staff had to resume active care.
Results
Sixty-five patients with ROSC after TOR were identified in 53 articles (1982–2018), 18 (28%) made a full recovery.
Conclusions
Almost a third made a full recovery after autoresuscitation. The following reasons for and recommendations to avoid autoresuscitation can be proposed: 1) In asystole with no reversible causes, resuscitation efforts should be continued for at least 20 min; 2) CPR should not be abandoned immediately after unsuccessful defibrillation, as transient asystole can occur after defibrillation; 3) Excessive ventilation during CPR may cause hyperinflation and should be avoided; 4) In refractory CA, resuscitation should not be terminated in the presence of any potentially-treatable cardiac rhythm; 5) After TOR, the casualty should be observed continuously and ECG monitored for at least 10 min.
Keywords: Autoresuscitation, Cardiopulmonary resuscitation, Emergency medicine, Hyperventilation, Lazarus phenomenon, Resuscitation, Resuscitation orders
Introduction
Autoresuscitation describes the return of spontaneous circulation (ROSC) after termination of resuscitation (TOR) following cardiac arrest (CA), when resuscitation has been attempted but has been deemed unsuccessful and abandoned [1]. It was first described in 1982 [2] and has been seen in out-of-hospital and in-hospital situations. It is sometimes called the “Lazarus Phenomenon” or “Lazarus Syndrome” after Lazarus, who was raised from the dead after 4 days by Jesus. The actual incidence of autoresuscitation is unknown but it is not rare, as surveys have shown that 37–50% of intensive care or prehospital emergency physicians have encountered it in clinical practice [3–6]. This means that there may be many unreported cases, since there are ≈1900 Intensive Care consultants in the UK alone. It is believed that the condition is grossly under-reported, partly because of fear of legal repercussions [7–9]. The implications of even a few reports of autoresuscitation are significant, not only because it can cause dismay and distress to healthcare professionals, bystanders and family, but also because delayed ROSC could lead to questions being asked about whether resuscitation had been conducted properly and whether it was stopped prematurely [10–13]. Personnel delivering resuscitation should know about the existence of autoresuscitation before being confronted with it [4, 14]. It was therefore decided to review the reported cases of autoresuscitation in patients undergoing CPR, to identify any factors that may contribute to it, and highlight changes in practice that could potentially reduce the likelihood of it occurring. This article maps the evidence about autoresuscitation, identifies the main theories and knowledge gaps, and proposes guidance on issues during resuscitation, and when confirming death, that could have a bearing on whether autoresuscitation will occur.
Methods
Cases of autoresuscitation were identified and selected through a scoping literature review. This method was chosen as it was felt to be most appropriate for identifying and mapping the available evidence on a very specific topic with a low-evidence base, when it is still unclear what other, more specific questions regarding its aetiology should be posed, and where evidence is still emerging [15]. We complied as much as possible with the Prisma-ScR scoping review checklist and guidelines [16]. We did not establish nor publish a priori a protocol for this study, and to our knowledge, there is not one currently in existence. For the purposes of this review, case reports conformed to all of the following criteria: 1) CA occurred from any cause; 2) Resuscitation attempts were performed (Basic Life Support or Advanced Life Support) for any length of time; 3) A point was reached when it was felt that either the patient had actually died (typically, persistent asystole) or a refractory arrhythmia occurred e.g. PEA, VF, that was not felt to be amenable to treatment; 4) Staff then declared the patient to be dead and stood back. No further interventions took place; 5) Later, signs of life were observed e.g. respiratory movements, electrocardiogram (ECG). Importantly, cases with transient ECG resumption compatible with cardiac output but no pulse were excluded. 6) The signs of life were sustained for more than a few seconds, such that staff had to resume active patient care. Patients who were expected to die, and therefore did not receive full Basic or Advanced Life Support, have not been included in this review. In addition, spontaneous reversion of VF to sinus rhythm with brief or no resuscitation attempts has been well documented for > 60 years [17–20] and is also not included.
We searched the literature up to 20th August 2019 with Google Scholar, MEDLINE and PubMed using the following terms alone and in combination: “Lazarus Phenomenon”; “Lazarus Syndrome”; “Autoresuscitation” or “Auto-resuscitation”. The composite search string used was (“lazarus phenomenon” OR “lazarus syndrome” OR “autoresuscitation” OR “auto-resuscitation”) for Google Scholar and ((“lazarus phenomenon”[All Fields] OR “lazarus syndrome”[All Fields]) OR “autoresuscitation”[All Fields]) OR “auto-resuscitation”[All Fields] for MEDLINE and PubMed. Articles of any type were included in this review, e.g. case reports and series; cohort and prospective studies and other systematic reviews, provided that they had been published in peer-reviewed journals. To expand the number of relevant retrieved articles, we then used two further search procedures. By placing the title of each article retrieved into the search field, we used the options to seek “Related articles” in Google Scholar and “Similar articles” in MEDLINE and PubMed. Articles in English, French, German, Russian, Spanish and Turkish were included. Finally, we searched the bibliography of the retrieved articles for additional articles that had not been picked up by the original searches.
The following data were collected for every case: age, sex, duration of resuscitation, rhythm when resuscitation was abandoned (e.g. asystole, pulseless electric activity (PEA), ventricular fibrillation (VF)), and the time when ROSC was first noticed. Outcome parameters included the cause of death or survival to hospital discharge (as appropriate) [21] and the neurological outcome (Cerebral Performance Category (CPC)) [22].
One author (LG) performed the literature search and built the database. In cases of doubt regarding the inclusion of a given case, the case was independently assessed for eligibility by the co-authors. All reports that clearly described a case of autoresuscitation were included, no matter how much detail was included. Descriptive statistics included frequencies, means and standard deviations, or median and interquartile range (IQR) to help better understand the scope of the problem. Groups were compared using Pearson’s Chi-square or Fischer’s exact tests, Student’s t-test, or the Wilcoxon rank-sum test as appropriate. The data retrieved from the database were exported to Stata version 14 (Stata Corporation, College Station, TX). A bilateral p-value < 0.05 was considered to indicate a significant difference.
Results
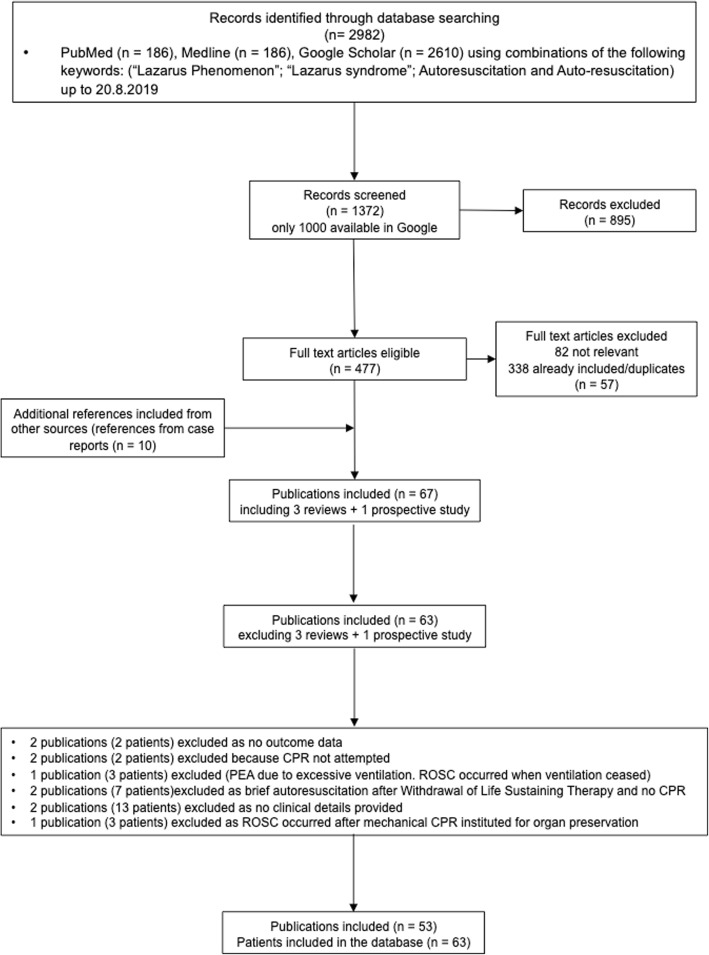
The literature search generated 1372 publications, 53 references with 63 patients for which outcome was available were included (Fig. 1). All the references were retrospective case reports of which five [2, 13, 23–25] described two patients, and one [26] described a series of five patients (Additional file 1: Table S1). Brief clinical details of the cases included in this review are reported in Additional file 2. We also included three published reviews and a prospective study (Additional file 3) in the qualitative synthesis.
Fig. 1.
Flowchart of patient selection
We included 34 out-of-hospital and 29 in-hospital CAs. The mean age of the patients was of 61 ± 24 (range 9 months – 97 years), the majority (68%) occurred in patients > 60 years old. The rhythm when CPR was first abandoned was asystole in 38 (70%) of the 54 patients for which this information was available (12 survivors; 26 non-survivors), PEA in 12/54 (22%) (3 survivors; 9 non-survivors), and VF in 4/54 (7%) (survivors only). Median duration of resuscitation was 30 min (IQR 18–40; range 0–90 min). Resuscitation attempts were performed for < 20 min (the time often recommended before abandoning resuscitation) [27–32] in 14 of 63 cases (22%). Signs of life were first noticed within 5 min in 30/63 cases (47%) cases and at 6–10 min in 14/63 cases (22%) (median of 5 min (IQR 3–10; range 0–220 min)) after resuscitation had been stopped. In the remaining cases, signs of life were not noticed until later or not recorded. In some cases, signs of life were only observed several hours after “death” was supposed to have occurred. Out of the 63 patients, 22 (35%) survived to hospital discharge, most (18; 82%) with good neurological outcome (Table 1). Forty-one patients died, the majority whilst still in hospital (Table 2) due to severe hypoxic brain damage or cardiac problems in most cases (28/41; 68%), while 4/41 (10%) initially fully recovered from arrest (CPC 1 or 2) but died due to other causes. Data on outcome was missing for two additional patients (Table 3). There was no difference between survivors and non-survivors regarding age (p = 0.18), duration of resuscitation (p = 0.47), and signs of life first noticed (p = 0.80). The rhythm when resuscitation was abandoned was associated with survival, as all four patients with VF survived, compared with 12/38 (32%) and 3/12 (35%) of those with asystole and PEA, respectively (p = 0.017).
Table 1.
Patients who survived autoresuscitation to hospital discharge (n = 22)
| Case | Reference | Age (y) | In-hospital (I) 14 Prehospital (P) 8 | Rhythm when resuscitation abandoned | Duration of resuscitation (min) | Signs of life first noticed (min) | Delay before death (s,h,d,m) | CPC |
|---|---|---|---|---|---|---|---|---|
| 56 ± 24 (range 0.9–84) | Asystole 12 (55%); VF 4 (18%); PEA 3 (14%); Not stated 3 (14%) | 30 (IQR 25–47.5; range 5–75) | 5.5 (IQR 3.5–10; range 1–20) | CPC 1–2 | ||||
| 1) | [2] | 68 | I | VF | 75 | 20 | – | 1 |
| 2) | [34] | 67 | I | “Abnormal” | 30 | 4 | – | 1 |
| 3) | [35] | 81 | I | Asystole | 5 | 2 | f | 1 |
| 4) | [36] | 50 | I | Asystole | 30 | 2 | 8 m | 1 |
| 5) | [59] | 36 | I | PEA | 25 | 3 | – | 1 |
| 6) | [60] | 84 | P | VF | 15 | 5 | – | 1 |
| 7) | [61] | 27 | P | Asystole | > 25a | 1 | – | 1 |
| 8) | [62] | 21 | I | Asystole | 30 | 10 | – | 1 |
| 9) | [63] | 80 | I | Asystole | 20 | 5 | – | 1 |
| 10) | [64] | 66 | I | Asystole | 18 | 10 | – | 1 |
| 11) | [65] | 66 | P | PEA | 45 | 5 | – | 1 |
| 12) | [66] | 83 | I | NS | 60 | 7 | – | 1 |
| 13) | [67] | 70 | I | Asystole | 34 | 8 | – | 1 |
| 14) | [23] | 66 | P | VF | > 30a | NSb | – | 2 (right sided hemiparesis) |
| 15) | [23] | 71 | I | Asystole | 35 | NSb | – | 1 |
| 16) | [68] | 63 | P | Asystole | 70 | NS d | – | 1 |
| 17) | [69] | 51 | I | Asystole | 61 | 3.5 | – | 2 (R arm weakness and partial amnesia) |
| 18) | [70] | 54 | P | PEA | 50 | NSd | – | 1 |
| 19) | [71] | 69 | I | Asystole | 25 | 10 | e | 3/Hypoxic brain damage |
| 20) | [8] | 47 | P | VF | 26 | 15 | 3 m | 3/Hypoxic brain damage |
| 21) | [72] | 0.92 | I | Asystole | NSc | 15 | 6 weeks | 3/Died progressive cardiomyopathy |
| 22) | [73] | 1.5 | P | NS | NSa | 6 | – | 3/Severe disability at 1y |
ALS denotes advanced life support, BLS basic life support, CPC cerebral performance category, ED emergency department, IQR interquartile range, PEA pulseless electrical activity, NS not stated, VF ventricular fibrillation; aBLS on scene + ALS in ambulance + ED; duration was considered =25 min and = 30 min for the analysis; b “moments”; c Intermittent over hours; d < 10 min; e = Alive at end of case report; f “few days
Table 2.
Patients who did not survive autoresuscitation (n = 41)
| Case | Reference | Age | In-hospital (I) 15Prehospital (P) 26 | Rhythm when resuscitation abandoned | Duration of resuscitation (min) | Signs of life first noticed (min) | Delay before death (s,h,d,m) | CPC (if available)/Outcome or Cause of death |
|---|---|---|---|---|---|---|---|---|
| 64 ± 24 (range 0.75–97) | Asystole 26 (63%); PEA 9 (22%); VF 0 (0%); Not stated 6 (15%) | 30 (IQR 17–40; range 0–90) | 5 (IQR 2.5–10; range 0–220) | |||||
| 1) | [2] | 84 | P | Asystole | 17 | d | 6d | 3/Hypoxic brain damage |
| 2) | [2] | 67 | P | Asystole | 20 | c | 15d | 3/Hypoxic brain damage |
| 3) | [7] | 80 | I | Asystole | 30 | 5 | 2d | 3/Hypoxic brain damage |
| 4) | [10] | 65 | P | Asystole | 35 | 20 | 5d | 4/Hypoxic brain damage |
| 5) | [11] | 81 | P | Asystole | 13 | NSc | 20 h | 3/Cardiogenic shock |
| 6) | [13] | 65 | P | NS | 35 | 20 | 4d | 4/Myocardial infarction |
| 7) | [13] | 83 | P | Asystole | 23 | 33 | 6.5 h | 4/Myocardial infarction |
| 8) | [26] | 97 | P | Asystole | 16 | 3 | 2 m | Died without regaining consciousness |
| 9) | [26] | 30 | P | PEA | 31 | 6 | 88 m | Died without regaining consciousness |
| 10) | [26] | 63 | P | PEA | 12 | 3 | 26 h | Died without regaining consciousness |
| 11) | [26] | 91 | P | PEA | 16 | 3 | 15 m | Died without regaining consciousness |
| 12) | [26] | 61 | P | PEA | 18 | 8 | 3 m | Died without regaining consciousness |
| 13) | [37] | 53 | I | Asystole | 46 | 2 | 34d | 4/Died (multi-organ failure) |
| 14) | [74] | 89 | I | Asystole | 18 | 5 | 7 h | Died. Another cardiac event. |
| 15) | [24] | 0.75 | P | Asystole | NSd | 0.5 | Several days. | Died (WLST). |
| 16) | [24] | 3 | I | Asystole | 25 | 1 | 40 m | Died (WLST) |
| 17) | [75] | 64 | I | NS | 20 | 15 | 1 h | Died. Refractory hypotension. |
| 18) | [76] | 76 | I | Asystole | 30 | 5 | 24 h | 3/Died. Hypoxic brain damage. |
| 19) | [77] | 44 | P | PEA | 80 | 5 | NSe | 3/Palliative care only |
| 20) | [78] | 87 | I | Wide complexesg | 15 | Immediately | 12d | 4/Died |
| 21) | [79] | 63 | I | Asystole | 12 | 3 | 12d | Died. Sepsis. |
| 22) | [80] | 59 | I | NSb | 15 | 2 | 30 m | Died. |
| 23) | [81] | 67 | P | PEA | 55 | 2 | 22 h | 1/Died from severe comorbidity. |
| 24) | [82] | 10 | P | PEA | > 40f | 2 | Short time after | 5 (WLST) |
| 25) | [83] | 94 | I | PEA | 40 | 2.5 | 18d | 1/Died multi-organ failure |
| 26) | [84] | 65 | P | Asystole | 55 | 40 | 13d | Died without regaining consciousness |
| 27) | [85] | 35 | P | NS | 88 | NSc | 50 m | Died. Another cardiac event. |
| 28) | [86] | 83 | P | Asystole | 90 | 10 | 12d | Died. Pneumonia. |
| 29) | [87] | 85 | P | Asystole | 34 | 2 | 25 m | Died. Another cardiac event. |
| 30) | [88] | 62 | I | Idioventricular | 40 | 5 | 34 m | Died without regaining consciousness |
| 31) | [89] | 55 | P | Asystole | 30 | 7 | 3d | 5/Died. Hypoxic brain damage. |
| 32) | [25] | 63 | P | Asystole | 40 | 10 | 10 m | Died without regaining consciousness |
| 33) | [25] | 78 | P | Asystole | 41 | 2 | 20 m | Died without regaining consciousness |
| 34) | [90] | 78 | P | Asystole | 31 | 220 | 19 h | Died without regaining consciousness |
| 35) | [91] | 85 | P | Asystole | 0 | 6 | 48 h | 4/Died (WLST) |
| 36) | [92] | 69 | P | Asystole | 40 | 180 | 10d | Died without regaining consciousness |
| 37) | [93] | 46 | P | Asystole | 30 | 60 | NS (hours) | 2/Died from cardiogenic shock |
| 38) | [94] | 83 | I | Asystole | 15 | 10 | 2 h | Died without regaining consciousness |
| 39) | [95] | 25 | I | NS | 40 | 5–7 | 4 h | Died without regaining consciousness |
| 40) | [96] | 67 | I | Asystole | 49 | 5 | 9d | 1/Died of massive pulmonary embolism |
| 41) | [97] | 75 | I | Asystole | 23 | 5 | Several days | Died without regaining consciousness |
CPC cerebral performance category, d days, ED emergency department, h hours, IQR interquartile range, PEA pulseless electrical activity, m months, NS not stated, s seconds, VF ventricular fibrillation; WLST Withdrawal of Life Sustaining Therapy; a age in 40’s; b possible/probable PEA, interpreted as PEA in the analysis; c Exact time when signs of life were first noted is not stated but the authors stated that it was “several” or “a few minutes”; d Return of signs of life not stated but > 10 min (considered as =10 min for the analysis); e = Alive at end of case report; f considered = 40 for the analysis; g no more information, considered as a missing data for the analysis
Table 3.
Unknown final outcome of autoresuscitation (n = 2)
| Case | Ref | Age | Rhythm when resuscitation abandoned | Duration of resuscitation (min) | Signs of life first noticed (min) | Delay before death | CPC (if available)/Outcome or cause of death |
|---|---|---|---|---|---|---|---|
| 1) | [98] | 93 | NS | 6 | 5 | NS | Outcome not stated |
| 2) | [99] | 40 | Asystole | 45 | 30 | NS | Outcome not stated |
CPC denotes cerebral performance category, NS not stated
The definitions of autoresuscitation in published case reports vary but all contain the same two elements: 1) attempted and abandoned resuscitation attempts following CA, 2) subsequent ROSC without medical intervention (Additional file 4).
Discussion
The most important finding is that about 30% of patients made a good recovery after death had been diagnosed, so autoresuscitation is of major significance and puts a focus on resuscitation practice, the decision to terminate resuscitation and diagnosis of death. Although the biblical Lazarus rose from the dead without resuscitation attempts, there are no case reports of it occurring in someone who has died without CPR performed beforehand [9, 33]. Almost all cases of autoresuscitation occurred after CPR following non-traumatic CA; there is only one report following traumatic CA [34] and four others associated with major haemorrhage [26, 35–37]. Therefore, it has been suggested that autoresuscitation is due to the medical interventions that were performed during resuscitation, but their effectiveness was delayed for some reason [38]. Cases occurring in patients who have undergone withdrawal of life-sustaining treatment were short-lived [39], apart from the subgroup of intended organ donors in which death was thought to have occurred and the circulation was subsequently maintained by artificial means [40, 41]. It is essential to consider possible mechanisms of autoresuscitation because this has potential implications for the way resuscitation is performed. A clear mechanism for autoresuscitation has been identified in only a few cases. The pathophysiologic factors (possibly in combination) that are thought to contribute to autoresuscitation are listed in Table 4 and derived from the conclusions of the authors of the published case reports and studies. Autoresuscitation has been reported more frequently in adults than children [3, 33].
Table 4.
Proposed autoresuscitation mechanisms and recommendations based on case reports to reduce the likelihood of it occurring
| factor | Proposed Mechanism | Actions that might reduce the Likelihood of Autoresuscitation occurring |
|---|---|---|
| Poor controlled ventilation techniques | ||
| 1) Air trapping in the lungs causing hyperinflation | Caused by high tidal volume or rapid ventilation rates with insufficient time for exhalation. Releasing the positive intra-thoracic pressure will enable venous return to resume and restore the circulation [24, 38, 59, 64, 65, 74–79, 86, 98, 100–102]. Effect more pronounced in hypovolaemia [37, 64] and pre-existing obstructive airways disease, especially if not managed correctly [9, 59, 103]. |
Avoid excessive ventilation (rate, tidal volume, or both) Exclude hyperinflation as a reversible cause of Pulseless Electrical Activity (PEA) by stopping ventilation and disconnecting the bag |
| 2) High intrathoracic pressure | Delays injected CPR drugs from reaching the heart and allows drugs to accumulate peripherally. Stopping positive airway pressure allows drugs to reach the heart resulting in beneficial effects [65, 80, 86]. | |
| 3) Hyperventilation | Deleterious effects on coronary perfusion pressure (CPP) [104]. | |
| Delayed drug effects | In profound acidosis or impaired drugs delivery via peripheral or intraosseous lines [77–79]. | |
| CPP as low as 15 mmHg can produce Return of Spontaneous Circulation after asystole | Intrinsic vasomotor function of capacitance and resistance blood vessels may maintain CPP so that even when resuscitation has ceased, CPP may be high enough to restart the heart [105]. | Careful consideration before terminating resuscitation if vasopressor infusions and/or mechanical ventilation are used |
| Return of myocardial function following Termination of Resuscitation (TOR) | Myocardial reperfusion due to spontaneous dislodging of endovascular plaque from a coronary artery [7, 10, 38]. Might also possibly allow spontaneous defibrillation in refractory VF [8, 23, 60]. | |
| Premature TOR | Failure to appreciate that transient asystole can occur immediately after defibrillation [23]. | Resuscitation should never be abandoned immediately after defibrillation. |
| Resuscitation terminated prematurely before therapeutic measures could have adequate effect. | Careful consideration before terminating resuscitation especially if vasopressor infusions and/or mechanical ventilation are used. | |
| Untreated reversible causes e.g. acid-base balance; electrolyte imbalance; hypothermia [68]. | Check for and correct all reversible causes of CA before considering TOR. | |
| TOR in the presence of a potentially treatable cardiac rhythm (refractory VF, PEA, broad complexes, bradycardia) and not asystole. | Caution about which cardiac rhythms are acceptable for terminating resuscitation as in 30% of autoresuscitation cases, TOR had occurred in the presence of some cardiac electrical activity (i.e. not asystole) | |
| TOR too soon after resuscitation started | Careful consideration of how long CPR has been employed before TOR | |
| Procedural |
Unobserved minimal vital signs (e.g. pseudo-PEA) due to clinician oversight [38, 81]. Misdiagnosis of death, perhaps due to failure to fully examine patient prior to declaring death. |
A 10 min observation period with ECG is generally more appropriate than 5 min following TOR [2, 7–11, 14, 26, 60–64, 66, 76, 79, 81, 94, 95, 106, 107]. After the decision has been made to terminate resuscitation, chest compressions should not be restarted The possibility of autoresuscitation should not affect the decision about when to terminate resuscitation |
| Resuscitation may exacerbate acute internal bleeding leading to hypovolaemic arrest | When resuscitation is stopped, the cardiovascular system stabilises [36]. | Observe the patient after TOR for 10 min. |
Death may be defined as the irreversible cessation of vital functions, including absence of circulation, spontaneous breathing, and whole-brain death when no confounding factors are present [27, 42, 43]. Doctors therefore diagnose death based on the absence of functions that are fundamental for life. The Academy of UK Medical Royal Colleges guidelines specify that there should be an absence of heart sounds, a central pulse on palpation, pupillary responses to light, corneal reflexes, and any motor response to supra-orbital pressure before confirming death [42]. In an advanced care setting, these findings can be supplemented with: asystole on a continuous ECG, absence of pulsatile flow with intra-arterial monitoring or the absence of contractile activity using echocardiography [42]. Although patients exhibiting the above clinical findings are assumed to have passed the “point of no return” and become unsalvageable, in fact death is not an instantaneous event but takes place over time. Sporadic ECG activity in the absence of a circulation can occur for many minutes after death is diagnosed [1, 33, 39, 44], and this can confound the Academy’s use of asystole as an indicator of death. Thus, an essential requirement when defining autoresuscitation is the presence of a circulation, because death determination depends on the cessation of circulation, not just of cardiac electrical activity [45]. In addition, a recent animal study indicated that sporadic cortical neuronal activity may be present for 2 hours following cardiac arrest [46]. If ECG activity resumes, it is important to establish if it is in isolation or whether ROSC has occurred [45]. Importantly, arterial pulselessness and asystole for a short period, e.g. immediately after defibrillation [23, 47], cannot reliably establish that irreversible cessation of cardiac and neurological function has occurred [48]. Finally, several autoresuscitation case-reports have occurred in the presence of a discernible cardiac rhythm (refractory VF or PEA, wide QRS complexes, extreme bradycardia) i.e. not asystole. Therefore, caution is advised before abandoning resuscitation in the presence of an ECG that is potentially treatable or compatible with life [26].
The Academy also advises that the person responsible for confirming death should observe the patient for “a minimum of five minutes to establish that irreversible cardiorespiratory arrest has occurred” [42]. The observation period after TOR is crucial and could leave carers open to the criticism that resuscitation was terminated prematurely [10] if an adequate period of observation after TOR is not employed. Importantly, the 5 min observation period [42] will potentially miss almost half of the autoresuscitation cases identified in this review. Although a care provider will potentially always be open to the charge that the resuscitation efforts were ended prematurely, regardless of the period of observation following termination of efforts, it is unreasonable to recommend that a patient is observed for a prolonged period of time after TOR solely in case autoresuscitation occurs. There has to be a balance between stopping the observation period prematurely at one extreme and waiting for a protracted period of time at the other. Our analysis of the case reports suggests that increasing from 5 to 10 min will increase the number of cases of autoresuscitation that will be picked up from 47% in ≤5 min to 69% within 10 min, and this increase is advocated by many of the authors of the case reports.
Recommendations
It has been calculated that a study with 95% confidence interval and 80% statistical power would need to document zero cases of autoresuscitation among 10,516 patients just to “rule out” even a rather high autoresuscitation rate of one in 1000 deaths [49]. Therefore, it is unlikely that a formal study that includes sufficient numbers of patients will ever be conducted. Consequently, it is necessary to review the factors that have been identified in actual cases and propose measures that can be taken to reduce the likelihood of autoresuscitation occurring. A summary of these, the rationale underpinning them and the relevant references are detailed in Table 4. These have been derived from the conclusions of the authors of each individual case report. There are five principal points to consider:
Resuscitation attempts should be continued for at least 20 min. Although this is now standard practice, in 22% of autoresuscitation cases, resuscitation was performed for less than this.
Attempt to avoid high intrathoracic pressure and hyperinflation during ventilation, as these are believed to be the underlying mechanism in many of the autoresuscitation case reports. In practice, this means gentle manual ventilation at no more than 12 breaths/minute. In patients with a history of chronic lung disease, it may be helpful to periodically disconnect the breathing circuit to ensure that the lungs are fully deflated before recommencing ventilation to avoid hyperinflation of the chest and thus diminished venous return to the heart.
As transient asystole can occur after defibrillation, careful consideration should be given before abandoning resuscitation immediately after an unsuccessful defibrillation attempt.
In refractory cardiac arrest, it might be unwise to terminate resuscitation in the presence of any potentially treatable cardiac rhythm, as this can become a perfusing rhythm. If an ECG monitor is not available and the cardiac rhythm is unknown (e.g. as in some Search and Rescue teams staffed by lay people), attempts should be made to get healthcare professional advice before terminating resuscitation.
After termination of resuscitation, consider extending the patient observation period from five to 10 min with ECG monitoring. No rules are going to exclude all cases of autoresuscitation but extending the observation period from five to 10 min will increase the safety margin from 47 to 69%. It is important to remember that the quoted times to recognition that the patient was still alive recorded in the case reports are generally not the times that autoresuscitation actually occurred. As explained above, this is because in most cases, patient monitoring was stopped when death was declared, and it was only when something changed e.g. the patient was noticed to be breathing, that it was clear that they were not dead.
Limitations
This is a scoping review and not a systematic review. More databases could have been accessed. Also, there may be more reports because some older papers published in print are now unavailable. The quality of reporting was generally low (case reports or letters to the editor), and often contained too few data to be included in this review [50]. In most reports, continuous monitoring was switched off once resuscitation had been abandoned, so the time when signs of life were detected is not an accurate guide to when ROSC occurred. This explains at least some of the cases where the time interval from TOR to signs of life detected was prolonged. Given the scarcity of data with autoresuscitation it may be necessary to make recommendations, which are mainly based on case reports and series. Nevertheless, we are not aware of any better method than this scoping review to assess autoresuscitation. Autoresuscitation may be a concern in potential organ donors. This specialist area is covered elsewhere, so it was felt inappropriate to draw it into this discussion [3, 45, 51–58].
We have attempted to overcome some of the limitations imposed by language restrictions. Another potential limitation is that the search strategy focussed on papers in which the title indicated that the theme of the paper was about autoresuscitation, Lazarus, etc. This was to avoid identifying the many papers in which autoresuscitation is mentioned but only as part of a wider discussion about resuscitation. The recommendations have been based on a small sample size.
Conclusions
Almost a third of the patients made a full recovery after autoresuscitation. This emphasises resuscitation should be terminated with caution. The following reasons for and recommendations to avoid autoresuscitation can be given: 1) In asystole with no reversible causes, resuscitation efforts should be continued for at least 20 min; 2) Resuscitation should not be abandoned immediately after unsuccessful defibrillation, as transient asystole can occur after defibrillation; 3) Excessive ventilation during resuscitation may cause hyperinflation and should be avoided; 4) In refractory cardiac arrest, resuscitation should not be terminated in the presence of any potentially-treatable cardiac rhythm; 5) After TOR, the casualty should be observed continuously and ECG monitored for at least 10 min.
Supplementary information
Additional file 1. Table S1. Year of publication, number of autoresuscitation cases and references reported in this review
Additional file 2. Published autoresuscitation case reports with brief clinical details
Additional file 3. Published reviews and prospective studies
Additional file 4. Published definitions of autoresuscitation
Acknowledgements
This manuscript has been funded with departmental sources only. The authors thank the Department of Innovation, Research and University of the Autonomous Province of Bozen/Bolzano for covering the Open Access publication costs.
Authors’ contributions
LG provided the idea to this study, performed the literature search and wrote the first draft of the manuscript. LG, MP, HB and PP discussed the findings. MP statistically analyzed the data. MP, HB and PP edited the manuscript. All authors finally agreed on the final version of this manuscript.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary information accompanies this paper at 10.1186/s13049-019-0685-4.
References
- 1.Wijdicks EF, Diringer MN. Electrocardiographic activity after terminal cardiac arrest in neurocatastrophes. Neurology. 2004;62(4):673–674. doi: 10.1212/WNL.62.4.673. [DOI] [PubMed] [Google Scholar]
- 2.Linko K, Honkavaara P, Salmenpera M. Recovery after discontinued cardiopulmonary resuscitation. Lancet. 1982;1(8263):106–107. doi: 10.1016/S0140-6736(82)90242-2. [DOI] [PubMed] [Google Scholar]
- 3.Dhanani S, Ward R, Hornby L, Barrowman NJ, Hornby K, Shemie SD, et al. Survey of determination of death after cardiac arrest by intensive care physicians. Crit Care Med. 2012;40(5):1449–1455. doi: 10.1097/CCM.0b013e31823e9898. [DOI] [PubMed] [Google Scholar]
- 4.Gerard D, Vaux J, Boche T, Chollet-Xemard C, Marty J. Lazarus phenomenon: knowledge, attitude and practice. Resuscitation. 2013;84(12):e153. doi: 10.1016/j.resuscitation.2013.07.030. [DOI] [PubMed] [Google Scholar]
- 5.Wind J, van Mook WN, Dhanani S, van Heurn EW. Determination of death after circulatory arrest by intensive care physicians: A survey of current practice in the Netherlands. J Crit Care. 2016;31(1):2–6. doi: 10.1016/j.jcrc.2015.09.006. [DOI] [PubMed] [Google Scholar]
- 6.El Dorado County EMS A. Five good reasons for better EMS documentation. Article 2. Proof of Life: Why we must make every possible effort, even when patients 'look' dead [Available from: https://www.edcgov.us/government/ems/pdf/documents/RequiredReading.pdf.
- 7.Maleck WH, Piper SN, Triem J, Boldt J, Zittel FU. Unexpected return of spontaneous circulation after cessation of resuscitation (Lazarus phenomenon) Resuscitation. 1998;39(1-2):125–128. doi: 10.1016/S0300-9572(98)00119-1. [DOI] [PubMed] [Google Scholar]
- 8.Kamarainen A, Virkkunen I, Holopainen L, Erkkila EP, Yli-Hankala A, Tenhunen J. Spontaneous defibrillation after cessation of resuscitation in out-of-hospital cardiac arrest: a case of Lazarus phenomenon. Resuscitation. 2007;75(3):543–546. doi: 10.1016/j.resuscitation.2007.05.021. [DOI] [PubMed] [Google Scholar]
- 9.Adhiyaman V, Adhiyaman S, Sundaram R. The Lazarus phenomenon. J R Soc Med. 2007;100(12):552–557. doi: 10.1177/0141076807100012013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Maeda H, Fujita MQ, Zhu BL, Yukioka H, Shindo M, Quan L, et al. Death following spontaneous recovery from cardiopulmonary arrest in a hospital mortuary: 'Lazarus phenomenon' in a case of alleged medical negligence. Forensic Sci Int. 2002;127(1-2):82–87. doi: 10.1016/S0379-0738(02)00107-X. [DOI] [PubMed] [Google Scholar]
- 11.De Salvia A, Guardo A, Orrico M, De Leo D. A new case of Lazarus phenomenon? Forensic Sci Int. 2004;146(Suppl):S13–S15. doi: 10.1016/j.forsciint.2004.09.022. [DOI] [PubMed] [Google Scholar]
- 12.Klein A, Lach H, Püschel K. Ein weiterer Fall von “Scheintod” – Diskussion über Richtlinien zur Todesfeststellung im Rettungswesen. Notfall Hausarztmedizin. 2007;33:330–335. doi: 10.1055/s-2007-985277. [DOI] [Google Scholar]
- 13.Puschel K, Lach H, Wirtz S, Moecke HP. Ein weiterer Fall von “Lazarus-Phänomen”? Notfall Rettungsmedizin. 2005;8:528–532. doi: 10.1007/s10049-004-0688-0. [DOI] [Google Scholar]
- 14.Hornby L, Dhanani S, Shemie SD. Update of a Systematic Review of Autoresuscitation After Cardiac Arrest. Crit Care Med. 2018;46(3):e268–ee72. doi: 10.1097/CCM.0000000000002920. [DOI] [PubMed] [Google Scholar]
- 15.Munn Z, Peters MDJ, Stern C, Tufanaru C, McArthur A, Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018;18(1):143. doi: 10.1186/s12874-018-0611-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann Intern Med. 2018;169(7):467–473. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- 17.Choquette G, Wasserman F, Lisker S, Bellet S. Spontaneous reversion of ventricular fibrillation to normal sinus rhythm in a case of acute myocardial infarction. Am Heart J. 1956;51(3):455–459. doi: 10.1016/0002-8703(56)90070-9. [DOI] [PubMed] [Google Scholar]
- 18.Goble AJ. Paroxysmal Ventricular Fibrillation with Spontaneous Reversion to Sinus Rhythm. Br Heart J. 1965;27:62–68. doi: 10.1136/hrt.27.1.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.van Hemel NM, Kingma JH. A patient in whom self-terminating ventricular fibrillation was a manifestation of myocardial reperfusion. Br Heart J. 1993;69(6):568–571. doi: 10.1136/hrt.69.6.568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mustafa MU, Baker CS, Stephens JD. Spontaneously terminating ventricular fibrillation and asystole induced by silent ischaemia causing recurrent syncope. Heart. 1998;80(1):86–88. doi: 10.1136/hrt.80.1.86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cummins RO, Chamberlain DA, Abramson NS, Allen M, Baskett PJ, Becker L, et al. Recommended guidelines for uniform reporting of data from out-of-hospital cardiac arrest: the Utstein Style. A statement for health professionals from a task force of the American Heart Association, the European Resuscitation Council, the Heart and Stroke Foundation of Canada, and the Australian Resuscitation Council. Circulation. 1991;84(2):960–975. doi: 10.1161/01.CIR.84.2.960. [DOI] [PubMed] [Google Scholar]
- 22.Safar P. Resuscitation after brain ischemia. In: Grenvik A, Safar P, editors. Brain Failure and Resuscitation. New York: Churchill Livingstone; 1981. pp. 155–184. [Google Scholar]
- 23.Gomes Emestina, Araújo Rui, Abrunhosa Rosário, Rodrigues Goretti. P-75 Two successful cases of spontaneous recovery after cessation of CPR. Resuscitation. 1996;31(3):S40. doi: 10.1016/0300-9572(96)83936-0. [DOI] [Google Scholar]
- 24.Duff JP, Joffe AR, Sevcik W. deCaen A. Autoresuscitation after pediatric cardiac arrest: is hyperventilation a cause? Pediatr Emerg Care. 2011;27(3):208–209. doi: 10.1097/PEC.0b013e31820d8e1e. [DOI] [PubMed] [Google Scholar]
- 25.Vaux J, Reveaux F, Hauter A, Chollet-Xemard C, Marty J. Le phénomène de Lazare (French) Ann Fr Med Urgence. 2013;3:182–183. doi: 10.1007/s13341-013-0284-3. [DOI] [Google Scholar]
- 26.Kuisma M, Salo A, Puolakka J, Nurmi J, Kirves H, Vayrynen T, et al. Delayed return of spontaneous circulation (the Lazarus phenomenon) after cessation of out-of-hospital cardiopulmonary resuscitation. Resuscitation. 2017;118:107–111. doi: 10.1016/j.resuscitation.2017.07.022. [DOI] [PubMed] [Google Scholar]
- 27.Paal P, Milani M, Brown D, Boyd J, Ellerton J. Termination of cardiopulmonary resuscitation in mountain rescue. High Alt Med Biol. 2012;13(3):200–208. doi: 10.1089/ham.2011.1096. [DOI] [PubMed] [Google Scholar]
- 28.Bossaert LL, Perkins GD, Askitopoulou H, Raffay VI, Greif R, Haywood KL, et al. European Resuscitation Council Guidelines for Resuscitation 2015: Section 11. The ethics of resuscitation and end-of-life decisions. Resuscitation. 2015;95:302–311. doi: 10.1016/j.resuscitation.2015.07.033. [DOI] [PubMed] [Google Scholar]
- 29.Drennan IR, Case E, Verbeek PR, Reynolds JC, Goldberger ZD, Jasti J, et al. A comparison of the universal TOR Guideline to the absence of prehospital ROSC and duration of resuscitation in predicting futility from out-of-hospital cardiac arrest. Resuscitation. 2017;111:96–102. doi: 10.1016/j.resuscitation.2016.11.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Morrison LJ, Eby D, Veigas PV, Zhan C, Kiss A, Arcieri V, et al. Implementation trial of the basic life support termination of resuscitation rule: reducing the transport of futile out-of-hospital cardiac arrests. Resuscitation. 2014;85(4):486–491. doi: 10.1016/j.resuscitation.2013.12.013. [DOI] [PubMed] [Google Scholar]
- 31.Verhaert DV, Bonnes JL, Nas J, Keuper W, van Grunsven PM, Smeets JL, et al. Termination of resuscitation in the prehospital setting: A comparison of decisions in clinical practice vs. recommendations of a termination rule. Resuscitation. 2016;100:60–65. doi: 10.1016/j.resuscitation.2015.12.014. [DOI] [PubMed] [Google Scholar]
- 32.Soar J, Nolan JP, Bottiger BW, Perkins GD, Lott C, Carli P, et al. European Resuscitation Council Guidelines for Resuscitation 2015: Section 3. Adult advanced life support. Resuscitation. 2015;95:100–147. doi: 10.1016/j.resuscitation.2015.07.016. [DOI] [PubMed] [Google Scholar]
- 33.Hornby K, Hornby L, Shemie SD. A systematic review of autoresuscitation after cardiac arrest. Crit Care Med. 2010;38(5):1246–1253. doi: 10.1097/CCM.0b013e3181d8caaa. [DOI] [PubMed] [Google Scholar]
- 34.Backer H, Kyburz A, Bosshard A, Babst R, Beeres FJP. Dead or dying? Pulseless electrical activity during trauma resuscitation. Br J Anaesth. 2017;118(5):809. doi: 10.1093/bja/aex105. [DOI] [PubMed] [Google Scholar]
- 35.Duck MH, Paul M, Wixforth J, Kammerer H. The Lazarus phenomenon. Spontaneous return of circulation after unsuccessful intraoperative resuscitation in a patient with a pacemaker. Anaesthesist. 2003;52(5):413–8.36. doi: 10.1007/s00101-003-0472-4. [DOI] [PubMed] [Google Scholar]
- 36.Wilseck Z, Cho K. Spontaneous circulation return after termination of resuscitation efforts for cardiac arrest following embolization of a ruptured common hepatic artery pseudoaneurysm. Gastrointes Interv. 2015;4:55–57. doi: 10.1016/j.gii.2015.01.002. [DOI] [Google Scholar]
- 37.Ekmektzoglou KA, Koudouna E, Bassiakou E, Stroumpoulis K, Clouva-Molyvdas P, Troupis G, et al. An intraoperative case of spontaneous restoration of circulation from asystole: a case of lazarus phenomenon. Case Rep Emerg Med. 2012;2012:380905.38. doi: 10.1155/2012/380905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sahni V. The Lazarus phenomenon. JRSM Open. 2016;7(8):2054270416653523. doi: 10.1177/2054270416653523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yong SA, D'Souza S, Philpot S, Pilcher DV. The Alfred Hospital experience of resumption of cardiac activity after withdrawal of life-sustaining therapy. Anaesth Intensive Care. 2016;44(5):605–606. doi: 10.1177/0310057X1604400508. [DOI] [PubMed] [Google Scholar]
- 40.Ali A, White P, Dhital K, Ryan M, Tsui S, Large S. Cardiac recovery in a human non-heart-beating donor after extracorporeal perfusion: source for human heart donation? J Heart Lung Transplant. 2009;28(3):290–293. doi: 10.1016/j.healun.2008.12.014. [DOI] [PubMed] [Google Scholar]
- 41.Mateos-Rodríguez A, Pardillos-Ferrer L, Navalpotro-Pascual JM. Kidney transplant function using organs from non-heart-beating donors maintained by mechanical chest compressions. Resuscitation. 2010;81:904–907. doi: 10.1016/j.resuscitation.2010.04.024. [DOI] [PubMed] [Google Scholar]
- 42.Academy of Medical Royal C. A Code of Practice for the Diagnosis and Confirmation of Death 2008 [Available from: http://aomrc.org.uk/wp-content/uploads/2016/04/Code_Practice_Confirmation_Diagnosis_Death_1008-4.pdf.
- 43.Zamperetti N, Bellomo R, Ronco C. Defining death in non-heart beating organ donors. J Med Ethics. 2003;29(3):182–185. doi: 10.1136/jme.29.3.182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Dhanani S, Hornby L, Ward R, Baker A, Dodek P, Chamber-Evans J, et al. Vital signs after cardiac arrest following withdrawal of life-sustaining therapy: a multicenter prospective observational study. Crit Care Med. 2014;42(11):2358–2369. doi: 10.1097/CCM.0000000000000417. [DOI] [PubMed] [Google Scholar]
- 45.Bernat JL. How autoresuscitation impacts death determination in organ donation. Crit Care Med. 2010;38:1377–1378. doi: 10.1097/CCM.0b013e3181d8bd76. [DOI] [PubMed] [Google Scholar]
- 46.Pani P, Giarrocco F, Giamundo M, Brunamonti E, Mattia M, Ferraina S. Persistence of cortical neuronal activity in the dying brain. Resuscitation. 2018;130:e5–e7. doi: 10.1016/j.resuscitation.2018.07.001. [DOI] [PubMed] [Google Scholar]
- 47.Niemann JT, Stratton SJ, Cruz B, Lewis RJ. Outcome of out-of-hospital postcountershock asystole and pulseless electrical activity versus primary asystole and pulseless electrical activity. Crit Care Med. 2001;29(12):2366–2370. doi: 10.1097/00003246-200112000-00020. [DOI] [PubMed] [Google Scholar]
- 48.Rady MY, Verheijde JL. No-touch time in donors after cardiac death (nonheart-beating organ donation) Curr Opin Organ Transplant. 2013;18(2):140–147. doi: 10.1097/MOT.0b013e32835e29a8. [DOI] [PubMed] [Google Scholar]
- 49.Halpern SD, Truog RD. Organ donors after circulatory determination of death: not necessarily dead, and it does not necessarily matter. Crit Care Med. 2010;38(3):1011–1012. doi: 10.1097/CCM.0b013e3181cc1228. [DOI] [PubMed] [Google Scholar]
- 50.Braun P, Herff H, Paal P. The Lazarus phenomenon-false positive death certifications and auto-resuscitation cases covered in lay press. Resuscitation. 2011;82(10):1363–1364. doi: 10.1016/j.resuscitation.2011.06.021. [DOI] [PubMed] [Google Scholar]
- 51.Rady MY, Verheijde JL. Lazarus phenomenon, autoresuscitation, and nonheart-beating organ donation. Crit Care Med. 2010;38(8):1757–1758. doi: 10.1097/CCM.0b013e3181defd10. [DOI] [PubMed] [Google Scholar]
- 52.Kompanje EJ, de Groot YJ. Autoresuscitation is not a determinant to lower the observation time in declaring death for organ donation. Crit Care Med. 2012;40(2):708. doi: 10.1097/CCM.0b013e31823b8b1e. [DOI] [PubMed] [Google Scholar]
- 53.Rady MY, Verheijde JL. Autoresuscitation and determining circulatory-respiratory death in clinical practice for organ donation. Crit Care Med. 2012;40(5):1655–1656. doi: 10.1097/CCM.0b013e318241e0fa. [DOI] [PubMed] [Google Scholar]
- 54.Woodside KJ. Autoresuscitation and organ donation: when is it safe to declare someone dead? Crit Care Med. 2012;40(1):329–330. doi: 10.1097/CCM.0b013e3182326634. [DOI] [PubMed] [Google Scholar]
- 55.Rady MY, Verheijde JL. Lazarus phenomenon and clinical practice guidelines for death diagnosis: regaining public trust in medical practice. Resuscitation. 2014;85(4):e63. doi: 10.1016/j.resuscitation.2013.09.027. [DOI] [PubMed] [Google Scholar]
- 56.Sheth KN, Nutter T, Stein DM, Scalea TM, Bernat JL. Autoresuscitation after asystole in patients being considered for organ donation. Crit Care Med. 2012;40(1):158–161. doi: 10.1097/CCM.0b013e31822f0b2a. [DOI] [PubMed] [Google Scholar]
- 57.Veatch RM. Are Organ Donors Really Dead: The Near-Irrelevance of Autoresuscitation. Am J Bioeth. 2018;18(8):1–2. doi: 10.1080/15265161.2018.1489652. [DOI] [PubMed] [Google Scholar]
- 58.Weiss MJ, Sherry W, Hornby L. Pediatric donation after circulatory determination of death (pDCD): A narrative review. Paediatr Respir Rev. 2019;29:3–8. doi: 10.1016/j.prrv.2018.03.006. [DOI] [PubMed] [Google Scholar]
- 59.Rosengarten PL, Tuxen DV, Dziukas L, Scheinkestel C, Merrett K, Bowes G. Circulatory arrest induced by intermittent positive pressure ventilation in a patient with severe asthma. Anaesth Intensive Care. 1991;19(1):118–121. doi: 10.1177/0310057X9101900126. [DOI] [PubMed] [Google Scholar]
- 60.Krarup NH, Kaltoft A, Lenler-Petersen P. Risen from the dead: a case of the Lazarus phenomenon-with considerations on the termination of treatment following cardiac arrest in a prehospital setting. Resuscitation. 2010;81(11):1598–1599. doi: 10.1016/j.resuscitation.2010.06.010. [DOI] [PubMed] [Google Scholar]
- 61.Walker A, McClelland H, Brenchley J. The Lazarus phenomenon following recreational drug use. Emerg Med J. 2001;18(1):74–75. doi: 10.1136/emj.18.1.74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Adanali M, Güvenç TS, Kale MY. Lazarus phenomenon in a patient with Duchenne muscular dystrophy and dilated cardiomyopathy. J Acute Med. 2014;4:99–102. doi: 10.1016/j.jacme.2014.03.003. [DOI] [Google Scholar]
- 63.Letellier N, Coulomb F, Lebec C, Brunet JM. Recovery after discontinued cardiopulmonary resuscitation. Lancet. 1982;1(8279):1019. doi: 10.1016/S0140-6736(82)92017-7. [DOI] [PubMed] [Google Scholar]
- 64.Ben-David B, Stonebraker VC, Hershman R, Frost CL, Williams HK. Survival after failed intraoperative resuscitation: a case of "Lazarus syndrome". Anesth Analg. 2001;92(3):690–692. doi: 10.1213/00000539-200103000-00027. [DOI] [PubMed] [Google Scholar]
- 65.Spowage-Delaney B, Edmunds CT, Cooper JG. The Lazarus phenomenon: spontaneous cardioversion after termination of resuscitation in a Scottish hospital. BMJ Case Rep. 2017;2017. [DOI] [PMC free article] [PubMed]
- 66.Torbado A, Pellejero S, Uriz J, Pavon A, Salvador M. No neurological impairment after a case of Lazarus phenomenon. Eur J Anaesthesiol. 2006;23:214. doi: 10.1097/00003643-200606001-00769. [DOI] [Google Scholar]
- 67.Quick G, Bastani B. Prolonged asystolic hyperkalemic cardiac arrest with no neurologic sequelae. Ann Emerg Med. 1994;24(2):305–311. doi: 10.1016/S0196-0644(94)70144-X. [DOI] [PubMed] [Google Scholar]
- 68.Pasquier M, de Riedmatten M, Paal P. Autoresuscitation in Accidental Hypothermia. Am J Med. 2018;131(9):e367–e3e8. doi: 10.1016/j.amjmed.2018.04.026. [DOI] [PubMed] [Google Scholar]
- 69.Vorotyntsev SI, Goldovsky BM, Potalov SA, Serikov KV, Serbin VG, Nikolayenko AM, et al. The Phenomenon of Lazarus – Autoresuscitation after cardiac arrest (Russian) 2011. [Google Scholar]
- 70.Fumeaux T, Borgeat A, Cuenoud PF, Erard A, de Werra P. Survival after cardiac arrest and severe acidosis (pH = 6.54) Intensive Care Med. 1997;23(5):594. [PubMed] [Google Scholar]
- 71.Meeker JW, Kelkar AH, Loc BL, Lynch TJ. A Case Report of Delayed Return of Spontaneous Circulation: Lazarus Phenomenon. Am J Med. 2016;129(12):e343–e3e4. doi: 10.1016/j.amjmed.2016.07.009. [DOI] [PubMed] [Google Scholar]
- 72.Tretter JT, Radunsky GS, Rogers DJ, Daugherty LE. A pediatric case of autoresuscitation. Pediatr Emerg Care. 2015;31(2):138–139. doi: 10.1097/PEC.0000000000000355. [DOI] [PubMed] [Google Scholar]
- 73.Mullen S, Roberts Z, Tuthill D, Owens L, Te Water Naude J, Maguire S. Lazarus Syndrome - Challenges Created by Pediatric Autoresuscitation. Pediatr Emerg Care. 2018. [DOI] [PubMed]
- 74.Huang Y, Kim S, Dharia A, Shalshin A, Dauer J. Delayed recovery of spontaneous circulation following cessation of cardiopulmonary resuscitation in an older patient: a case report. J Med Case Rep. 2013;7:65. doi: 10.1186/1752-1947-7-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Rogers PL, Schlichtig R, Miro A, Pinsky M. Auto-PEEP during CPR. An "occult" cause of electromechanical dissociation? Chest. 1991;99(2):492–493. doi: 10.1378/chest.99.2.492. [DOI] [PubMed] [Google Scholar]
- 76.MacGillivray RG. Spontaneous recovery after discontinuation of cardiopulmonary resuscitation. Anesthesiology. 1999;91(2):585–586. doi: 10.1097/00000542-199908000-00052. [DOI] [PubMed] [Google Scholar]
- 77.Hagmann H, Oelmann K, Stangl R, Michels G. Is increased positive end-expiratory pressure the culprit? Autoresuscitation in a 44-year-old man after prolonged cardiopulmonary resuscitation: a case report. J Med Case Rep. 2016;10(1):364. doi: 10.1186/s13256-016-1148-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Martens P, Vandekerckhove Y, Mullie A. Restoration of spontaneous circulation after cessation of cardiopulmonary resuscitation. Lancet. 1993;341(8848):841. doi: 10.1016/0140-6736(93)90627-S. [DOI] [PubMed] [Google Scholar]
- 79.Al-Ansari MA, Abouchaleh NM, Hijazi MH. Return of spontaneous circulation after cessation of cardiopulmonary resuscitation in a case of digoxin overdosage. Clin Intensive Care. 2005;16:179–181. doi: 10.1080/09563070500193092. [DOI] [Google Scholar]
- 80.Bradbury N. Lazarus phenomenon: another case? Resuscitation. 1999;41(1):87. doi: 10.1016/S0300-9572(99)00030-1. [DOI] [PubMed] [Google Scholar]
- 81.Hannig KE, Hauritz RW, Grove EL. Autoresuscitation: A Case and Discussion of the Lazarus Phenomenon. Case Rep Med. 2015;2015:724174. doi: 10.1155/2015/724174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Cummings BM, Noviski N. Autoresuscitation in a child: The young Lazarus. Resuscitation. 2011;82(1):134. doi: 10.1016/j.resuscitation.2010.09.015. [DOI] [PubMed] [Google Scholar]
- 83.Garcia JLC, Gonzalez-Latorre MV, Fernandez AN. El fenómeno de Lázaro: Reanimación espontánea (Spanish) Rev Esp Anestesiol Reanim. 2004;51:390–394. [PubMed] [Google Scholar]
- 84.Low DW, Looi I, Manocha AB, Ang HA, Nagalingam M, Ayop NA, et al. Rising from the dead! Med J Malaysia. 2012;67(5):538–539. [PubMed] [Google Scholar]
- 85.Mutzbauer TS, Stahl W, Lindner KH. Compression-decompression (ACD)-CPR. Prehosp Disaster Med. 1997;12:S21. doi: 10.1017/S1049023X00046562. [DOI] [Google Scholar]
- 86.Aguado OR, Portilla FJS, Ruiz JPN. Lazarus phenomenon in an out-of-hospital emergency attended by a home emergency service. Emergencias. 2011;23:43–46. [Google Scholar]
- 87.Tiesmeier J, Brandt O, Emmerich M. Unerwartete Lebenszeichen nach erfolgloser Reanimation (German) MMW Fortschr ed. 2010;152:33–36. [PubMed] [Google Scholar]
- 88.Thong SY, Ng SY. Case report – Lazarus syndrome after prolonged resuscitation: Herbert Publications Ltd; 2013. Available from: http://www.hoajonline.com/journals/pdf/2049-9752-2-14.pdf
- 89.Voelckel W, Kroesen G. Unexpected return of cardiac action after termination of cardiopulmonary resuscitation. Resuscitation. 1996;32(1):27–29. doi: 10.1016/0300-9572(96)00954-9. [DOI] [PubMed] [Google Scholar]
- 90.Monticelli F., Bauer N., Meyer H. J. Lazarus-Phänomen. Rechtsmedizin. 2006;16(2):57–63. doi: 10.1007/s00194-006-0366-2. [DOI] [Google Scholar]
- 91.Wiese CHR, Stojanovic T, Klockgether-Radke A, Bartels U, Schmitto JD, Quintel M, et al. Intraoperatives “Lazarus-Phänomen”? Spontane Kreislaufstabilisierung bei einem Patienten mit Herzschrittmacher (German) Anaesthesist. 2007;56:1231–1236. doi: 10.1007/s00101-007-1263-0. [DOI] [PubMed] [Google Scholar]
- 92.Güven AT, Petridis G, Özkal SS, Kalfoglu EA. Lazarus Phenomenon in Medicolegal Perspective: A case report (Turkish) Adli Tıp Bülteni. 2017;22(3):224–227. [Google Scholar]
- 93.Jasra S, Majumdar S, Rajagopalan B, Fernandez S. Lazarus syndrome. A rare case of auto-resuscitation: American College of Physicians Annual Scientific Meeting – poster competition. 2015. [Google Scholar]
- 94.Alves S, Campos M, Reis G. Lazarus syndrome in the emergency room: A case report. Resuscitation. 2010;84:e151. [Google Scholar]
- 95.Sukhyanti K, ShriKrishan C, Anu K, Ashish D. Lazarus phenomenon revisited: a case of delayed return of spontaneous circulation after carbon dioxide embolism under laparoscopic cholecystectomy. Anaes Pain Int Care. 2012.
- 96.Frolich MA. Spontaneous recovery after discontinuation of intraoperative cardiopulmonary resuscitation: case report. Anesthesiology. 1998;89(5):1252–1253. doi: 10.1097/00000542-199811000-00028. [DOI] [PubMed] [Google Scholar]
- 97.Bray JG., Jr The Lazarus phenomenon revisited. Anesthesiology. 1993;78(5):991. doi: 10.1097/00000542-199305000-00030. [DOI] [PubMed] [Google Scholar]
- 98.Abdullah RS. Restoration of circulation after cessation of positive pressure ventilation in a case of "Lazarus syndrome". Anesth Analg. 2001;93(1):241. doi: 10.1097/00000539-200107000-00050. [DOI] [PubMed] [Google Scholar]
- 99.Mustamam AHM, Jailani AFMAK, Z’aba N, Balakrishnan SL, Ali NM. Arise from the dead – case report. Malaysian J Emerg Med. 2016;1:49.
- 100.Wiener C. Ventilatory management of respiratory failure in asthma. JAMA. 1993;269(16):2128–2131. doi: 10.1001/jama.1993.03500160098040. [DOI] [PubMed] [Google Scholar]
- 101.Lapinsky SE, Leung RS. Auto-PEEP and electromechanical dissociation. N Engl J Med. 1996;335(9):674. doi: 10.1056/NEJM199608293350916. [DOI] [PubMed] [Google Scholar]
- 102.Manara AR, Thomas I. The use of circulatory criteria to diagnose death after unsuccessful cardiopulmonary resuscitation. Resuscitation. 2010;81(7):781–783. doi: 10.1016/j.resuscitation.2010.05.004. [DOI] [PubMed] [Google Scholar]
- 103.Connery LE, Deignan MJ, Gujer MW, Richardson MG. Cardiovascular collapse associated with extreme iatrogenic PEEPi in patients with obstructive airways disease. Br J Anaesth. 1999;83(3):493–495. doi: 10.1093/bja/83.3.493. [DOI] [PubMed] [Google Scholar]
- 104.Aufderheide TP, Lurie KG. Death by hyperventilation: a common and life-threatening problem during cardiopulmonary resuscitation. Crit Care Med. 2004;32(9 Suppl):S345–S351. doi: 10.1097/01.CCM.0000134335.46859.09. [DOI] [PubMed] [Google Scholar]
- 105.Paradis NA, Martin GB, Rivers EP, Goetting MG, Appleton TJ, Feingold M, et al. Coronary perfusion pressure and the return of spontaneous circulation in human cardiopulmonary resuscitation. JAMA. 1990;263(8):1106–1113. doi: 10.1001/jama.1990.03440080084029. [DOI] [PubMed] [Google Scholar]
- 106.Peña SB, Aedo IF, Palomino SL. Spontaneous return of circulation after termination of cardiopulmonary resuscitation maneuvers: a systematic review of cases of Lazarus phenomenon. Emergencias. 2014;26:307–316. [Google Scholar]
- 107.DeVita MA. The death watch: certifying death using cardiac criteria. Prog Transplant. 2001;11(1):58–66. doi: 10.1177/152692480101100109. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. Table S1. Year of publication, number of autoresuscitation cases and references reported in this review
Additional file 2. Published autoresuscitation case reports with brief clinical details
Additional file 3. Published reviews and prospective studies
Additional file 4. Published definitions of autoresuscitation