Abstract
Background
In the past women have been advised that lowering their salt intake might reduce their risk of pre‐eclampsia. Although this practice has largely ceased, it remains important to assess the evidence about possible effects of advice to alter dietary salt intake during pregnancy.
Objectives
The objective of this review was to assess the effects of dietary advice to alter salt intake compared to continuing a normal diet, on the risk of pre‐eclampsia and its consequences.
Search methods
We searched the register of trials maintained and updated by the Cochrane Pregnancy and Childbirth Group, and the Cochrane Controlled Trials Register Disc Issue 4, 1998.
Selection criteria
Studies were included if they were randomised trials of advice to either reduce or to increase dietary salt during pregnancy.
Data collection and analysis
All data were extracted independently by both reviewers.
Main results
Two trials were included, with 603 women. They compared advice about a low salt diet with no dietary advice. The confidence intervals for all of the outcomes reported were wide, and cross the no effect line. This includes pre‐eclampsia (relative risk 1.11, 95% confidence interval 0.46 to 2.66). Even when taken together, these trials are insufficient to provide reliable information about the effects of advice on salt restriction during normal pregnancy.
None of the trials included women with pre‐eclampsia, so this review provides no reliable information about changes in salt intake for treatment of pre‐eclampsia.
Authors' conclusions
Salt consumption during pregnancy should remain a matter of personal preference.
Plain language summary
Reduced salt intake compared to normal dietary salt, or high intake, in pregnancy
To be prepared.
Background
In the early part of this century a low salt diet was often recommended as treatment for oedema, in both pregnant and non‐pregnant people. At that time oedema was included in the definition of pre‐eclampsia, although it is now recognised to be part of normal pregnancy, occurring in 80% of pregnant women. This led to the idea that restricting salt intake would treat, and also prevent, pre‐eclampsia (Green 1989). By the 1940s a low salt diet was standard during pregnancy, particularly for women with pre‐eclampsia. In the late 1950s and early 1960s this practice began to be questioned, and it was even suggested that high salt intake might prevent or treat pre‐eclampsia (UK 1958, UK 1961). Subsequently, interest in salt consumption during pregnancy has largely faded away.
In most parts of the world women are no longer advised by clinicians to alter their salt intake during pregnancy. A notable exception is in the Netherlands where this practice has, until recently, remained widespread. Nevertheless, some lay literature aimed at pregnant women continues to advocate salt restriction during pregnancy.
Salt is a widely used flavour enhancer. Those who are used to salt in their diet may find a low salt diet unpalatable. This may be particularly relevant during the first half of pregnancy when nausea and vomiting is common, and taste can also be altered. Low salt foods can also be less convenient and more expensive than salted alternatives. Women should not be advised to alter their dietary salt during pregnancy unless there is reasonable evidence of benefit.
This review aims to summarise the evidence about the effects of advice to alter dietary salt intake during pregnancy.
Objectives
To assess the effects of advice to have either a low or a high salt intake, compared to normal dietary salt, during pregnancy on prevention and treatment of pre‐eclampsia and its complications.
Methods
Criteria for considering studies for this review
Types of studies
All randomised controlled trials of advice to alter salt intake during pregnancy. Quasi randomised trials were excluded, as inadequate concealment of the allocation may have introduced bias. For an intervention such as dietary advice where foreknowledge of the allocation may influence recruitment, adequate concealment of the allocation is of particular importance in avoiding bias.
Types of participants
Normal pregnant women, regardless of their risk of pre‐eclampsia, and women with pre‐eclampsia.
Types of interventions
Any study evaluating dietary advice to alter salt intake during pregnancy.
Types of outcome measures
For the woman: pregnancy‐induced hypertension, pre‐eclampsia (hypertension with proteinuria), placental abruption, caesarean section, serious maternal morbidity, admission to hospital and use of other hospital resources. For the baby: death, prematurity, birthweight, intrauterine growth restriction, admission to special care nursery, ventilation, measures of long term growth and development.
Search methods for identification of studies
Electronic searches
The register of trials maintained by the Pregnancy and Childbirth Group was searched for relevant trials. The Cochrane Controlled Trial Register, Disc Issue 4 1998, was also searched.
Data collection and analysis
Trials were checked for inclusion criteria and data were extracted independently by both reviewers. Discrepancies were resolved by discussion. There was no blinding of authorship or results. A quality score for concealment of allocation was assigned to each trial, using the following criteria:
(A) adequate concealment of allocation (B) unclear whether adequate concealment of allocation (C) inadequate concealment of allocation, quasi‐randomisation.
Studies were excluded if either it was not possible to enter data based on intention to treat, or >20% of participants were excluded from that outcome.
Results
Description of studies
The two included trials, involving 603 women, were conducted in the Netherlands. The women in the studies were all healthy and nulliparous. Neither study included women with pre‐eclampsia, although one (Netherlands 1998) included women with mild hypertension. Both compared low dietary salt (20 or 50mmol/day) with an unchanged diet. Compliance was assessed by checking urinary sodium excretion. Although this was higher than the target level for the low sodium group, sodium excretion was still lower than for the normal diet group.
There was no blinding of the intervention and, although it is not mentioned in the reports, blinding of outcome assessment is unlikely.
Risk of bias in included studies
For both trials allocation was adequately concealed. One (Netherlands 1997) was conducted in two centres, and subsets of data from both hospitals have been published in a wide variety of formats. Ten per cent of women in this study were excluded from the analyses, and the proportion was higher in the low salt group as 17 women did not want to use the recommended diet. The other study (Netherlands 1998) involved eight centres and there was complete follow‐up for all women.
Effects of interventions
Two trials were included, with data reported for 603 women. Both compared advice to restrict dietary salt with advice to continue a normal diet. Confidence intervals for all the outcomes reported in this review are wide, and cross the no effect line. For example, the relative risk for pre‐eclampsia is 1.11, 95% confidence interval 0.44‐2.78. This means that the true effect could be anything from over a halving in the risk of pre‐eclampsia associated with salt restriction to a more than doubling.
No included trials evaluated a high salt diet, and none included women with established pre‐eclampsia.
Discussion
The aim of this review was to evaluate the effect of advice about dietary salt during pregnancy. Both trials evaluated advice on a low salt diet, and in both the low salt group did have lower urinary excretion than the normal diet group.
The trials in this review were not large and, even when taken together, they are insufficient to provide reliable information about the effects of advice to restrict salt intake during normal pregnancy. None of the trials enrolled women with pre‐eclampsia, so this review provides no information about the effects of advice to restrict salt intake for treatment of pre‐eclampsia.
Women's preferences were not reported. However, in one study (Netherlands 1997) 13% of women in the salt restriction arm were excluded as they did not want to follow the diet. In the other study only 24% of women successfully reduced their urinary sodium excretion to below the target level. This was presumed to be because a low salt diet is not very palatable and is therefore difficult to follow.
Although no included trials evaluated a high salt diet, three excluded studies did. In one study this was to evaluate prevention of pre‐eclampsia (UK 1958), and in the other two salt was used for treatment of pre‐eclampsia (UK 1961, USA 1961). All were excluded because the use of a quasi randomised design introduced substantial potential for bias. In the largest trial (2077 women) the relative risk for pre‐eclampsia was 0.45, 95% confidence interval (0.26‐0.75), a reduction that appeared to be reflected in fewer complications (UK 1958). The excluded trials of salt for treatment of pre‐eclampsia involved nearly 1000 women, and neither detected any effect on the course of pre‐eclampsia. In view of the methodological limitations of these studies it is difficult to draw firm conclusions, beyond saying that it seems unlikely that a high salt diet will increase the risk of pre‐eclampsia.
Authors' conclusions
Implications for practice.
A low salt diet is often unpalatable. In the absence of evidence that advice to reduce salt intake during pregnancy has any beneficial effect in prevention or treatment of pre‐eclampsia, or of any other outcome, salt consumption during pregnancy should remain a matter of personal preference.
Implications for research.
Salt restriction during pregnancy does not seem promising for the prevention of pre‐eclampsia. Very large numbers of women would need to be randomised to detect a moderate‐small effect. Such trials might be justified in the context of a setting where this form of dietary advice was already widespread practice, but they would be difficult to justify elsewhere. Unless new and plausible hypotheses emerge, further trials of salt intake are unlikely to be a priority.
What's new
| Date | Event | Description |
|---|---|---|
| 20 September 2008 | Amended | Converted to new review format. |
Notes
This review is being updated by the publication of two reviews: one review will evaluate salt intake for preventing pre‐eclampsia (see 'Reduced salt intake compared to normal dietary salt, or high intake, in pregnancy') and the other will evaluate salt intake for treating pre‐eclampsia. The latter is currently being prepared. Once it has been published, this review will be withdrawn.
Acknowledgements
None.
Data and analyses
Comparison 1. Low vs normal salt intake in pregnancy.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Hypertension | 1 | 242 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.49, 1.94] |
| 2 Pre‐eclampsia | 2 | 603 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.11 [0.46, 2.66] |
| 3 Referral to hospital, no admission | 1 | 361 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.05 [0.48, 2.32] |
| 4 Admission to hospital | 1 | 361 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.82 [0.56, 1.22] |
| 5 Placental abruption | 1 | 361 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.19 [0.01, 3.98] |
| 6 Caesarean section | 1 | 361 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.75 [0.44, 1.27] |
| 7 Perinatal mortality | 2 | 409 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.92 [0.18, 21.03] |
| 8 Birthweight <10th centile | 1 | 242 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.5 [0.73, 3.07] |
| 9 Birthweight <2500g | 1 | 361 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.84 [0.42, 1.67] |
| 10 Preterm delivery | 1 | 242 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.08 [0.46, 2.56] |
| 11 Apgar at 5 min <7 | 1 | 361 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.37 [0.53, 3.53] |
| 12 Paediatric admission | 1 | 361 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.69, 1.40] |
1.1. Analysis.
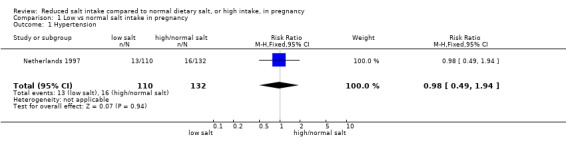
Comparison 1 Low vs normal salt intake in pregnancy, Outcome 1 Hypertension.
1.2. Analysis.
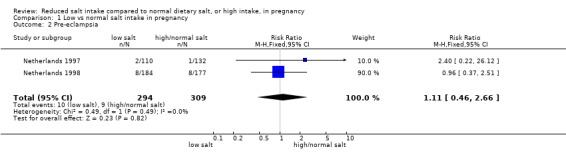
Comparison 1 Low vs normal salt intake in pregnancy, Outcome 2 Pre‐eclampsia.
1.3. Analysis.
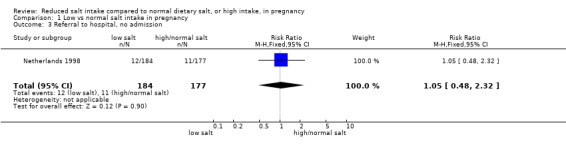
Comparison 1 Low vs normal salt intake in pregnancy, Outcome 3 Referral to hospital, no admission.
1.4. Analysis.
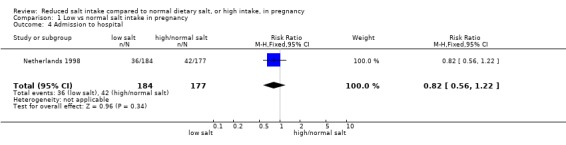
Comparison 1 Low vs normal salt intake in pregnancy, Outcome 4 Admission to hospital.
1.5. Analysis.
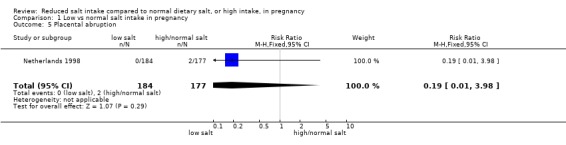
Comparison 1 Low vs normal salt intake in pregnancy, Outcome 5 Placental abruption.
1.6. Analysis.
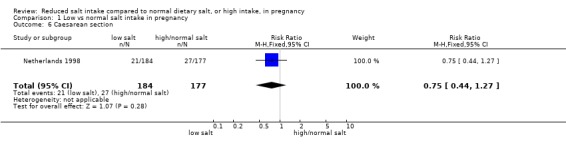
Comparison 1 Low vs normal salt intake in pregnancy, Outcome 6 Caesarean section.
1.7. Analysis.
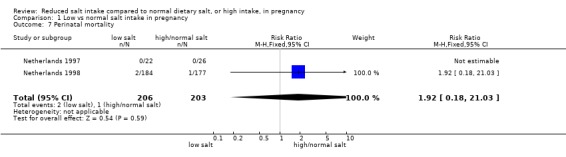
Comparison 1 Low vs normal salt intake in pregnancy, Outcome 7 Perinatal mortality.
1.8. Analysis.
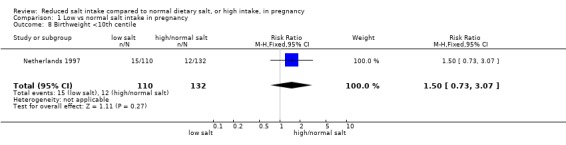
Comparison 1 Low vs normal salt intake in pregnancy, Outcome 8 Birthweight <10th centile.
1.9. Analysis.
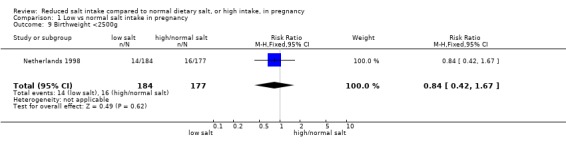
Comparison 1 Low vs normal salt intake in pregnancy, Outcome 9 Birthweight <2500g.
1.10. Analysis.
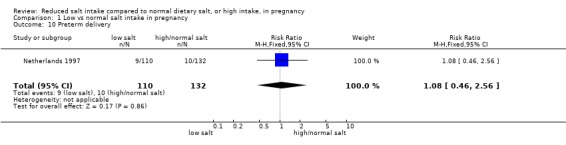
Comparison 1 Low vs normal salt intake in pregnancy, Outcome 10 Preterm delivery.
1.11. Analysis.
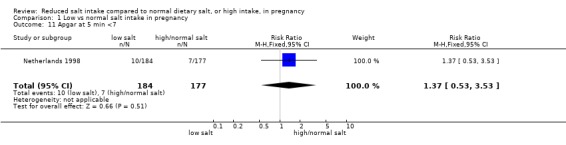
Comparison 1 Low vs normal salt intake in pregnancy, Outcome 11 Apgar at 5 min <7.
1.12. Analysis.
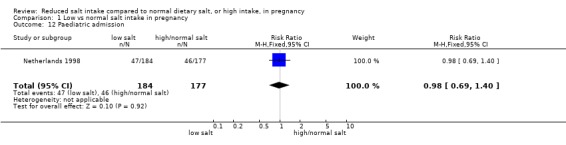
Comparison 1 Low vs normal salt intake in pregnancy, Outcome 12 Paediatric admission.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Netherlands 1997.
| Methods | "Closed envelope system", no further information. 28 women (10%) women excluded. Low salt 23 excluded: 17 refused diet, 3 social reasons, 2 medical reasons, 1 fetal trisomy. Normal salt 5 excluded: 2 social reasons, 3 medical reasons. | |
| Participants | 270 nulliparous women with a singleton pregnancy after 12 weeks, by dates and ultrasound. Excluded if pre‐existing HT, diabetes, renal disease, cardiovascular disease. | |
| Interventions | Low: diet with about 20mmol sodium per day. Oral and written instruction by dietician, no added salt and ready made foods only if no salt in preparation. Normal: no dietary restriction. | |
| Outcomes | Woman: PIH, PE, severe HT, small for gestational age, preterm delivery Baby: death. | |
| Notes | Mean urinary sodium after randomisation was around 70mmol/day in the low sodium group and 135mmol/day in the normal diet group. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Netherlands 1998.
| Methods | Sealed numbered opaque envelopes. Blocks of 10 stratified by centre. | |
| Participants | 361 women booked for midwifery care, nulliparous, DBP <90mmHg at booking visit before 20 weeks. Randomised if DBP >85 x2 in subsequent visit, or weight gain >1kg/week for 3 consecutive weeks, or excess oedema. Excluded if planning to leave the city or risk factors for PIH. | |
| Interventions | Low: sodium restricted diet, aimed at less than 50mmol/day. Written dietary instructions given by midwife. Normal: asked not to change eating habits. | |
| Outcomes | Woman: highest DBP, pre‐eclampsia, eclampsia, referrals and admissions for hypertension, time to delivery, abruption, mode of delivery. Baby: gestation at delivery (mean), birthweight, Apgar at 5 minutes, paediatric admission, death. | |
| Notes | Multicentre study involving 8 midwifery practices. Mean urinary sodium after randomisation 84mmol/day in low sodium group, 124mmol/day for normal diet. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
DBP=diastolic blood pressure, PIH=pregnancy induced hypertension, PE=pre‐eclampsia, HT=hypertension
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Australia 1986a | No clinical outcomes reported. Participants: 58 primigravid women. Intervention: one week of either high salt or low salt diet. Study design: 'assigned randomly'. |
| Australia 1986b | No clinical outcomes reported. Participants: 40 primigravid women. Intervention: one week of either high salt or low salt diet. Study design: 'assigned randomly'. |
| UK 1958 | Not a randomised trial. Quasi random, using alternate allocation of women attending clinic. Participants: 2077 women at booking clinic, 58 excluded. Intervention: high salt diet with advice to add salt to diet and eat salty food versus low salt with advice to avoid adding salt to food and not to eat salty food. |
| UK 1961 | Not a randomised trial. Allocation by ward and by consultant. Participants: 739 women with high blood pressure, oedema and proteinuria. Excluded if <24 hours from admission to delivery. Interventions: 2g salt versus 10g versus 25g. |
| USA 1961 | Not a randomised trial. Quasi random using alternate allocation. Participants: 48 women with pre‐eclampsia. Interventions: 1‐2g salt versus 10‐12g. |
Contributions of authors
Data were extracted and checked by both reviewers. The text was drafted by Lelia Duley, with comments from David Henderson‐Smart.
Sources of support
Internal sources
Centre for Perinatal Health Services Research, University of Sydney, Australia.
External sources
Department for Interenational Development, UK.
Medical Research Council, UK.
Declarations of interest
None known.
Edited (no change to conclusions)
References
References to studies included in this review
Netherlands 1997 {published data only}
- Steegers EAP, Lakwijk HPJM, Jongsma HW, Fast JH, Boo T, Eskes TKAB, et al. (Patho)physiological implications of chronic dietary sodium restriction during pregnancy; a longitudinal prospective randomized study. Br J Obstet Gynaecol 1991;98:980‐7. [DOI] [PubMed] [Google Scholar]
- Maten GD. Low sodium diet in pregnancy: effects on maternal nutritional status. Eur J Obstet Gynecol Reprod Biol 1995;61:63‐64. [DOI] [PubMed] [Google Scholar]
- Buul BJA, Steegers EAP, Jongsma HW, Rijpkema AL, Eskes TKAB, Thomas CMG, et al. Dietary sodium restriction in the prophylaxis of hypertensive disorders of pregnancy: effects on the intake of other nutrients. Am J Clin Nutr 1995;62:49‐57. [DOI] [PubMed] [Google Scholar]
- Buul BJA, Steegers EAP, Maten GD, Delemarre FMC, Jongsma HW, Oosterbaan HP, et al. Dietary sodium restriction does not prevent gestational hypertension: a Dutch two‐center randomized trial. Hyper Preg 1997;16:335‐346. [Google Scholar]
- Buul E, Rijpkema A, Steegers E, Jonggsma T, Eskes P. Chronic dietary sodium restriction in pregnancy reduces calcium intake. J Perinat Med 1992;20 Suppl 1:216. [Google Scholar]
- Buul EJA, Steegers EAP, Jongsma HW, Thomas CMG, Hein PR. Chronic dietary sodium restriction in pregnancy: effects on urinary prostaglandin excretion. Proceedings of 2nd European Congress on Prostaglandins in Reproduction. 1991:186.
- Post JA, Buul BJ, Hart AA, Heerikhuize JJ, Pesman G, Legros JJ, et al. Vasopressin and oxytocin levels during normal pregnancy: effects of chronic dietary sodium restriction. J Endocrinol 1997;152:345‐354. [DOI] [PubMed] [Google Scholar]
Netherlands 1998 {published data only}
- Knuist M, Bonsel GJ, Zondervan HA, Treffers PE. Low sodium diet and pregnancy‐induced hypertension: a multi‐centre randomised controlled trial. Br J Obstet Gynaecol 1998;105:430‐434. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Australia 1986a {published data only}
- Brown MA, Gallery EDM. Sodium excretion in human pregnancy: a role for arginine vasopressin. Am J Obstet Gynecol 1986;154:914‐919. [DOI] [PubMed] [Google Scholar]
Australia 1986b {published data only}
- Brown MA, Sinosich MJ, Saunders DM, Gallery EDM. Potassium regulation and progesterone‐aldosterone interrelationships in human pregnancy: a prospective study. Am J Obstet Gynecol 1986;155:349‐353. [DOI] [PubMed] [Google Scholar]
UK 1958 {published data only}
- Robinson M. Salt in pregnancy. Lancet 1958;1:178‐181. [DOI] [PubMed] [Google Scholar]
UK 1961 {published data only}
- Bower D. The influence of dietary salt intake on pre‐eclampsia. J Obstet Gynaecol Br Cmmwlth 1961;63:123‐126. [DOI] [PubMed] [Google Scholar]
USA 1961 {published data only}
- Mengert WF, Tacchi DA. Pregnancy toxemia and sodium chloride ‐ preliminary report. Am J Obstet Gynecol 1961;81:601‐605. [DOI] [PubMed] [Google Scholar]
Additional references
Green 1989
- Green J. Diet and the prevention of pre‐eclampsia. In: Chalmers I, Enkin MW, Keirse MJNC editor(s). Effective Care in Pregnancy and Childbirth. Oxford: Oxford University Press, 1989:281‐300. [Google Scholar]
References to other published versions of this review
Duley 1995
- Duley L. Low vs high salt intake in pregnancy.. Keirse MJNC, Renfrew MJ, Neilson JP, Crowther C (eds.) Pregnancy and Childbirth Module. In: The Cochrane Pregnancy and Childbirth Database. 1995, Issue 2. [Google Scholar]


