Abstract
Background
Millions of women worldwide undergo perineal suturing after childbirth and the type of repair may have an impact on pain and healing. For more than 70 years, researchers have been suggesting that continuous non‐locking suture techniques for repair of the vagina, perineal muscles and skin are associated with less perineal pain than traditional interrupted methods.
Objectives
To assess the effects of continuous versus interrupted absorbable sutures for repair of episiotomy and second‐degree perineal tears following childbirth.
Search methods
We searched the Cochrane Pregnancy and Childbirth Group's Trials Register (20 January 2012).
Selection criteria
Randomised trials examining continuous and interrupted suturing techniques for repair of episiotomy and second‐degree tears after vaginal delivery.
Data collection and analysis
Three review authors independently assessed trial quality. Two of the three authors independently extracted data and a third review author checked them. We contacted study authors for additional information.
Main results
Sixteen studies, involving 8184 women at point of entry, from eight countries, were included. The trials were heterogeneous in respect of operator skill and training. Meta‐analysis showed that continuous suture techniques compared with interrupted sutures for perineal closure (all layers or perineal skin only) are associated with less pain for up to 10 days' postpartum (risk ratio (RR) 0.76; 95% confidence interval (CI) 0.66 to 0.88, nine trials). There was an overall reduction in analgesia use associated with the continuous subcutaneous technique versus interrupted stitches for repair of perineal skin (RR 0.70; 95% CI 0.59 to 0.84). There was also a reduction in suture removal in the continuous suturing groups versus interrupted (RR 0.56; 95% CI 0.32 to 0.98), but no significant differences were seen in the need for re‐suturing of wounds or long‐term pain.
Authors' conclusions
The continuous suturing techniques for perineal closure, compared with interrupted methods, are associated with less short‐term pain, need for analgesia and suture removal. Furthermore, there is also some evidence that the continuous techniques used less suture material as compared with the interrupted methods (one packet compared to two or three packets, respectively).
Keywords: Female; Humans; Pregnancy; Episiotomy; Suture Techniques; Analgesics; Analgesics/administration & dosage; Delivery, Obstetric; Obstetric Labor Complications; Obstetric Labor Complications/surgery; Perineum; Perineum/injuries; Perineum/surgery; Randomized Controlled Trials as Topic
Plain language summary
Continuous and individual interrupted sutures for repair of episiotomy or second‐degree tears
Continuous stitching causes less pain than interrupted absorbable stitches when used for repairing the perineum after childbirth.
When women give birth, the perineum (the area between the vaginal opening and back passage) sometimes tears or it may be necessary for them to have an episiotomy (surgical cut) to increase the size of the vaginal outlet to facilitate the birth. Episiotomies and tears that involve the muscle layer (second degree) need to be stitched. Millions of women worldwide undergo perineal suturing after childbirth and the type of repair may have an impact on pain and discomfort, and healing. In the UK alone, approximately 1000 women per day will experience perineal stitches following vaginal birth and millions more worldwide. A midwife or doctor will stitch the episiotomy or second‐degree tear in three layers (vagina, perineal muscle and skin). Traditionally the vagina is stitched using a continuous locking stitch and the perineal muscles and skin are repaired using approximately three or four individual stitches, each needing to be knotted separately to prevent them from dislodging. Researchers have been suggesting for more than 70 years that the 'continuous non‐locking stitching method' is better than 'traditional interrupted methods'. This review looked at 'continuous stitching methods' compared with 'traditional interrupted stitching methods' and identified 16 randomised controlled trials involving 8184 women from eight different countries. Results from the trials showed that stitching just underneath the skin (subcutaneous) was associated with less pain with reduced need for analgesics after the birth, or for the sutures to be removed; however, when the 'continuous stitching method' was used for repair of all three layers, this may be associated with even less pain. The level of operator skill and training varied in the different trials. Other research is needed to assess perineal repair training programmes. In addition, research is needed to look at interventions that may reduce the incidence of perineal trauma during childbirth.
There is also some evidence that the continuous techniques use less suture material when compared with the interrupted methods (one packet compared to two or three packets, respectively).
Background
Prevalence and morbidity
Perineal trauma during childbirth affects millions of women throughout the world and can result in long‐term maternal morbidity. In the UK approximately 85% of women will sustain some degree of perineal trauma during vaginal birth and 60% to 70% of these will need suturing, which equates to approximately 1000 women per day (McCandlish 1998; Sleep 1984). However, rates of perineal trauma will vary considerably according to individual practices and policies of institutions and practitioners throughout the world. Perineal trauma may occur spontaneously during birth, or the midwife or obstetrician may need to make a surgical incision (episiotomy) to increase the diameter of the vaginal outlet to facilitate the baby's birth. Childbirth‐related perineal tears are classified according to the anatomical structures involved into; first degree (involving the perineal skin only), second degree (involving the perineal muscles and skin), third degree (injury to the anal sphincter complex ‐ 3a = less than 50% of the external anal sphincter torn; 3b = more than 50% of the external anal sphincter torn; 3c = internal anal sphincter also torn) and fourth degree (injury to the perineum involving the anal sphincter complex and anal epithelium) (Fernando 2006). The majority of women experience some short‐term discomfort or pain following perineal repair, and up to 20% will continue to have long‐term problems, such as superficial dyspareunia (painful intercourse) (Glazener 1995; Klein 1994; Sleep 1984). Short‐ and long‐term maternal morbidity associated with perineal repair can lead to major physical, psychological and social problems, affecting the woman's ability to care for her new baby and other members of the family (Sleep 1991). For those women who sustain perineal injury, it is important that skilled operators repair the trauma, and that they use the best suturing techniques and materials, in order to minimise any associated problems.
Techniques of perineal repair
Currently, midwives in the UK are responsible for suturing the majority of second‐degree tears and episiotomies sustained during spontaneous vaginal delivery. However, there are wide variations in both techniques and materials used for perineal repair between individual practitioners and maternity units. The rationale for the suturing technique chosen appears to evolve from the way the operator was first taught rather than robust clinical evidence. It could be hypothesised that even if the best suture techniques and materials are used to repair perineal trauma, the short‐ and long‐term outcome will be dependent on the skill of the operator.
Traditional interrupted technique
Perineal trauma is traditionally repaired in three stages: a continuous locking stitch is inserted to close the vaginal trauma, commencing at the apex of the wound and finishing at the level of the fourchette with a loop knot. The proposed rationale for using a locking stitch is to prevent shortening of the vagina; however, good‐quality evidence to support this theory is lacking. The perineal muscles are then re‐approximated with three or four interrupted sutures and finally, the perineal skin is closed by inserting continuous subcutaneous or interrupted transcutaneous stitches. Another variation of the interrupted suture technique involves placing inverted interrupted stitches to re‐approximate the muscle layer. The skin is then closed with inverted interrupted stitches placed in the subcutaneous tissue a few millimetres under the perineal skin edges (not transcutaneously). The rationale for this alternative technique is that the knots are 'hidden' in the depth of the perineal trauma and the interrupted skin suture knots are also buried to facilitate healing.
Two‐stage technique
This method is very similar to the traditional interrupted technique whereby the vaginal trauma is closed with a continuous locking stitch, followed by insertion of three or four interrupted stitches to re‐approximate the perineal muscles; however, the skin is left apposed but not sutured (skin edges no more than half a centimetre apart). The rationale behind this technique is that the insertion of skin sutures may contribute to some of the morbidity experienced by women following perineal repair. Women often complain of pain and tightness associated with transcutaneous skin sutures; moreover, if standard synthetic material is used there is an increased risk of the stitches having to be removed up to three months following birth (Kettle 2010).
Continuous non‐locking technique
This is a three‐stage technique: the repair begins with an anchoring stitch above the apex of the vaginal trauma and the deep tissues and mucosa are closed with a single continuous non‐locking stitch, in contrast to the locking stitch used for the traditional method. The perineal muscles are then re‐approximated using a similar continuous non‐locking technique and the repair is completed with a continuous suture inserted well below the skin surface in the subcutaneous fascia. The finished repair is secured with a knot placed in the vagina behind the hymenal remnants. A single length of absorbable suture material is used for the repair with no knots other than the anchoring and terminal knot. The rationale for using this suturing technique is that it is very easy to over tighten locked or interrupted stitches, which may restrict the distribution of tissue oedema and cause increased pain. With the continuous technique, the tension is transferred throughout the whole length of the single suture; also the skin sutures are inserted well below the skin surface, thus avoiding the nerve endings to reduce pain.
Aim of the review
The aim of this review is to examine the available research and to establish if there is any clear scientific evidence that the technique used for perineal repair, following childbirth, has any effect on the amount of pain and superficial dyspareunia experienced by women in the postpartum period.
This systematic review includes 16 randomised clinical trials and represents a substantial update of the previous Cochrane review.
Objectives
To assess the effects of continuous and interrupted suturing methods (using absorbable suture materials) on the incidence of short‐ and long‐term postpartum maternal morbidity experienced by women following repair of episiotomy or second‐degree perineal tears after vaginal birth. The evidence collated in this review will enable purchasers, providers and consumers of health care to choose the most appropriate technique of perineal repair in terms of both health gain and cost.
The main outcomes of interest are: short‐ and long‐term pain, amount of analgesia used, time of resumption of pain‐free intercourse, superficial dyspareunia, removal of suture material, re‐suturing of wound, time taken to perform the repair and number of suture packets used.
Methods
Criteria for considering studies for this review
Types of studies
We have included all identified, relevant randomised controlled trials and quasi‐randomised trials that compare different continuous and interrupted suturing techniques for perineal closure (all layers or skin only), using absorbable suture materials. We have assessed all of the trials included for risk of bias examining the method of treatment allocation, randomisation, blinding of outcome assessment and handling of exclusions.
We have included studies published as abstracts provided that there was sufficient information to allow us to assess eligibility and risk of bias; if there was not sufficient information in an abstract we planned to contact study authors.
Types of participants
All primiparous and multiparous women who have sustained an episiotomy or second‐degree perineal tear and required stitching following a spontaneous or instrumental vaginal delivery.
Types of interventions
All randomised controlled trials comparing different continuous and interrupted suturing techniques for perineal closure (all layers or skin only) following vaginal delivery using absorbable suture material. Trials that compared continuous suturing techniques using absorbable sutures versus interrupted transcutaneous techniques that used non‐absorbable sutures for perineal skin closure were excluded to avoid the confounding effect of suture material.
Types of outcome measures
The main focus was on outcome measures relating to short‐ and long‐term postpartum morbidity.
Primary outcomes
Short‐term pain (up to four days' postpartum).
Short term pain (up to 10 days' postpartum).
Use of analgesia (up to 10 days' postpartum).
Superficial dyspareunia.
Secondary outcomes
Removal of suture material.
Re‐suturing.
Long‐term pain (up to three months).
Wound dehiscence.
Failure to resume pain‐free intercourse (by three months).
In this updated version of the review we have also included outcomes relating to the number of suture packets used and the time taken to carry out repairs.
For the original version of this review, review authors sought consumer views regarding what outcomes they would expect from local focus groups, members of the National Childbirth Trust and other postnatal support groups.
The main outcomes of interest from the consumers' point of view were short‐ and long‐term pain, removal of suture material and the resumption of pain‐free intercourse.
Search methods for identification of studies
Electronic searches
We searched the Cochrane Pregnancy and Childbirth Group's Trials Register by contacting the Trials Search Co‐ordinator (20 January 2012).
The Cochrane Pregnancy and Childbirth Group's Trials Register is maintained by the Trials Search Co‐ordinator and contains trials identified from:
monthly searches of the Cochrane Central Register of Controlled Trials (CENTRAL);
weekly searches of MEDLINE;
weekly searches of EMBASE;
handsearches of 30 journals and the proceedings of major conferences;
weekly current awareness alerts for a further 44 journals plus monthly BioMed Central email alerts.
Details of the search strategies for CENTRAL, MEDLINE and EMBASE; the list of handsearched journals and conference proceedings; and the list of journals reviewed via the current awareness service can be found in the 'Specialized register' section within the editorial information about the Cochrane Pregnancy and Childbirth Group.
Trials identified through the searching activities described above are each assigned to a review topic (or topics). The Trials Search Co‐ordinator searches the register for each review using the topic list rather than keywords.
We did not apply any language restrictions.
Data collection and analysis
Selection of studies
At least two review authors independently assessed and selected the trials for inclusion in this review. It was not possible for us to assess the relevance of the trials blinded because we knew the authors' names, institution, journal of publication and results when we applied the inclusion criteria. We resolved all disagreements by discussion.
Data extraction and management
We designed a form to extract data. For eligible studies, two review authors extracted the data using the agreed form. We resolved discrepancies through discussion and, if required, we consulted the third review author. We entered data into Review Manager software (RevMan 2011) and checked for accuracy.
When information regarding any of the above was unclear, we attempted to contact authors of the original reports to provide further details.
Assessment of risk of bias in included studies
We assessed the risk of bias of each study using the criteria outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). Two review authors independently assessed the methodological quality of each trial and collected details of method of allocation and treatment concealment, attrition bias, performance bias and whether an intention‐to‐treat analysis was performed.
(1) Sequence generation (checking for possible selection bias)
We have described for each included study the method used to generate the allocation sequence to allow an assessment of whether it should produce comparable groups.
We assessed the method as:
adequate (any truly random process, e.g. random number table; computer random number generator);
inadequate (any non‐random process, e.g. odd or even date of birth; hospital or clinic record number);
unclear.
(2) Allocation concealment (checking for possible selection bias)
We have described for each included study the method used to conceal the allocation sequence and determined whether intervention allocation could have been foreseen in advance of, or during recruitment, or changed after assignment.
We assessed the methods as:
adequate (e.g. telephone or central randomisation; consecutively numbered sealed opaque envelopes);
inadequate (open random allocation; unsealed or non‐opaque envelopes, alternation; date of birth);
unclear.
(3) Blinding (checking for possible performance bias)
We have described for each included study the methods used, if any, to blind study participants and personnel from knowledge of which intervention a participant received. We are aware that achieving blinding for this intervention is not likely to have occurred as the suture technique will be apparent to clinical staff carrying out the repair or assessing the healing of the perineum, and may be apparent to women. It is possible though, that for some outcomes those carrying out outcome assessment may be blind to group allocation. We considered that studies were at low risk of bias if they were blinded, or if we judged that the lack of blinding could not have affected the results. We assessed blinding separately for different outcomes or classes of outcomes.
We assessed the methods as:
adequate, inadequate or unclear for participants;
adequate, inadequate or unclear for personnel;
adequate, inadequate or unclear for outcome assessors.
(4) Incomplete outcome data (checking for possible attrition bias through withdrawals, drop‐outs, protocol deviations)
We have described for each included study, and for each outcome or class of outcomes, the completeness of data including attrition and exclusions from the analysis. We have noted whether attrition and exclusions were reported, the numbers included in the analysis at each stage (compared with the total randomised participants), reasons for attrition or exclusion where reported, and whether missing data were balanced across groups or were related to outcomes. Where sufficient information was reported, or supplied by the trial authors, we re‐included missing data in the analyses. We assessed methods as:
adequate;
inadequate;
unclear.
For outcomes assessed in the early postpartum period loss to follow‐up had to be less that 10% for us to judge a study as adequate. For longer‐term outcomes (e.g. dyspareunia at three months' postpartum) we expected less than 20% attrition.
(5) Selective reporting bias
We have described for each included study how we investigated the possibility of selective outcome reporting bias and what we found.
We assessed the methods as:
adequate (where it is clear that all of the study's pre‐specified outcomes and all expected outcomes of interest to the review have been reported);
inadequate (where not all the study's pre‐specified outcomes were reported; one or more reported primary outcomes were not pre‐specified; outcomes of interest were reported incompletely and so could not be used; study failed to include results of a key outcome that would have been expected to have been reported);
unclear.
(6) Other sources of bias
We have described for each included study any important concerns we had about other possible sources of bias such as baseline imbalance.
We have assessed whether each study was free of other problems that could put it at risk of bias:
yes;
no;
unclear.
(7) Overall risk of bias
We have made explicit judgements about whether studies were at high risk of bias, according to the criteria given in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). With reference to (1) to (6) above, we have assessed the likely magnitude and direction of the bias and whether we considered it was likely to impact on the findings. We have explored the impact of the level of bias through undertaking sensitivity analyses ‐ see Sensitivity analysis.
Measures of treatment effect
We undertook statistical analysis using the Review Manager software (RevMan 2011) for calculation of the treatment effect. We performed fixed‐effect (assumption free) meta‐analysis for combining data in the absence of significant heterogeneity.
Dichotomous data
For dichotomous data, we have presented the results as summary risk ratio (RR) with 95% confidence intervals (CI).
Continuous data
For continuous data, we have used the mean difference if outcomes were measured in the same way between trials. We have used the standardised mean difference (SMD) to combine trials that measured the same outcome, but using different methods.
Unit of analysis issues
In this version of the review we did not identify any cluster randomised trials eligible for inclusion. In future updates, if any such trials are identified, we plan to include them in the analyses along with individually randomised trials. We will adjust standard errors, using the methods described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011) (using an estimate of the intra‐cluster correlation co‐efficient (ICC) derived from the trial (if possible), from a similar trial or from a study of a similar population. If we use ICCs from other sources, we will report this and conduct sensitivity analyses to investigate the effect of variation in the ICC. If we identify both cluster‐randomised trials and individually randomised trials, we plan to synthesise the relevant information. We will consider it reasonable to combine the results from both if there is little heterogeneity between the study designs and interaction between the effect of intervention and the choice of randomisation unit is considered to be unlikely.
We will also acknowledge heterogeneity in the randomisation unit and perform a sensitivity analysis to investigate the effects of the randomisation unit.
Dealing with missing data
For included studies, we have noted levels of attrition. We have explored the impact of including studies with high levels of missing data in the overall assessment of treatment effect by using sensitivity analysis.
For all outcomes, we have carried out analyses, as far as possible, on an intention‐to‐treat basis, that is we have attempted to include all participants randomised to each group in the analyses, with all participants analysed in the group to which they were allocated, regardless of whether or not they received the allocated intervention.
Assessment of heterogeneity
We have assessed statistical heterogeneity in each meta‐analysis using the T2, I2 and Chi2 statistics. We have regarded heterogeneity as substantial if I2 is greater than 30% and either T2 is greater than zero, or there is a low P value (less than 0.10) in the Chi2 test for heterogeneity.
Assessment of reporting biases
In this version of the review we were not able to explore possible publication bias using funnel plots as too few studies contributed data to the meta‐analyses.
We did not have access to the study protocols for most of the included studies, so most of the included studies have been assessed as unclear for reporting bias as we were not clear whether all pre‐specified outcomes were reported in published papers. Where we suspected possible bias (e.g. where only statistically significant results were reported) we have noted this.
Data synthesis
We have carried out statistical analysis using Review Manager software (RevMan 2011). We have used fixed‐effect meta‐analysis for combining data where it seemed reasonable to assume that studies were estimating the same underlying treatment effect: that is where trials are examining the same intervention, and the trials' populations and methods were judged to be sufficiently similar. If we suspected clinical heterogeneity sufficient to expect that the underlying treatment effects differed between trials, or if substantial statistical heterogeneity was detected, we have used random‐effects meta‐analysis to produce an overall summary, provided that an average treatment effect across trials was considered clinically meaningful. The random‐effects summary gives an indication of the average range of possible treatment effects, and we have discussed the clinical implications of treatment effects differing between trials. If we did not think the average treatment effect was clinically meaningful we have not combined trials.
Where we have used random‐effects analyses, the results have been presented as the average treatment effect with its 95% CI, and the estimates of T2 and I2, along with the 95% prediction interval.
Subgroup analysis and investigation of heterogeneity
For primary outcomes we undertook the following subgroup analyses:
whether the continuous group used continuous suture techniques for all layers or perineal skin only.
We have assessed differences between subgroups by inspection of the subgroups' CIs; non‐overlapping CIs suggesting a difference in treatment effect between the subgroups, we have also carried out subgroup interaction tests.
Sensitivity analysis
For primary outcomes we carried out sensitivity analysis, temporarily excluding those studies with poor methodological quality from the analyses (i.e. with poor allocation concealment or high levels of attrition, or both) to explore whether the inclusion of such studies has any impact on the results. We have not included separate tables with sensitivity analysis in the review, but have noted the results of these analyses in the text of the review.
Results
Description of studies
Results of the search
The search strategy identified 23 studies for possible inclusion in the review. The date of the most recent search was January 2012.
In this updated version of the review, we have included nine new studies in addition to the seven included in previous versions. We have excluded five studies and one study is awaiting assessment pending further investigation (Uslu 1992) and a further study is awaiting translation (Graczyk 1998).
Included studies
In this updated review we have included 16 studies, involving 8184 women at point of entry.
Included trials: Almeida 2008; Banninger 1978; Croce 1997; Detlefsen 1980; Gordon 1998; Isager‐Sally 1986; Kettle 2002; Kindberg 2008; Kokanali 2011; Mahomed 1989; Morano 2006; Oboro 2003; Perveen 2009; Stark 2009; Valenzuela 2009; Zafar 2008.
The studies were carried out in a range of countries: the UK (Gordon 1998; Kettle 2002; Mahomed 1989), Denmark (Detlefsen 1980; Isager‐Sally 1986; Kindberg 2008), Italy (Croce 1997; Morano 2006), Brazil (Almeida 2008), Switzerland (Banninger 1978), Nigeria (Oboro 2003), Spain (Valenzuela 2009), Turkey (Kokanali 2011) and Pakistan (Perveen 2009; Zafar 2008) (the setting of the study by Stark 2009 was not clear). The studies were published between 1978 and 2011. We requested unpublished data from authors of trial reports for some outcomes, and have indicated in the Characteristics of included studies tables and in the reference list when we have used unpublished data in the analyses.
Twelve trials in this review compared continuous suture techniques with interrupted methods for perineal closure (all layers or skin only). Within the 'interrupted suture' comparison groups, the perineal muscle and skin were closed with interrupted stitches; whereas, in the 'continuous suture' groups, two of the included trials used interrupted sutures to repair the perineal muscles prior to continuous subcutaneous closure of the perineal skin (continuous for perineal skin only) (Banninger 1978; Mahomed 1989). The other 12 trials used a continuous suturing technique throughout to close the vagina and perineal muscles prior to subcutaneous skin closure in the 'continuous suture' groups (continuous for all layers) (Almeida 2008; Croce 1997; Detlefsen 1980; Isager‐Sally 1986; Kettle 2002; Kindberg 2008; Kokanali 2011; Morano 2006; Perveen 2009; Stark 2009; Valenzuela 2009); in the trial by Almeida 2008 a separate suture was used to close the perineal skin intradermally following continuous closure of the vagina and perineal muscles in the 'continuous' group.
Two trials in the review compared a two‐stage technique of perineal repair to the more traditional three‐stage approach (the suture techniques were not clearly described) (Gordon 1998; Oboro 2003). In the two‐stage technique the vagina and perineal muscles were sutured and the skin was left apposed but not sutured (skin edges no more than half a centimetre apart). In comparison, in the three‐stage method, the vagina and perineal muscles were sutured and the skin was re‐approximated with interrupted or continuous subcutaneous sutures (see Characteristics of included studies for details).
Two trials examined other comparisons. In the trial by Zafar 2008 in the 'continuous suture' group the vaginal mucosa was closed with a running stitch and the same suture was used to re‐approximate the perineal muscle in two layers, followed by subcuticular sutures to close the skin (finishing at the lower end of the incision). In the 'interrupted' comparison group the vaginal mucosa was closed with a continuous running stitch, followed by interrupted sutures inserted in two layers to re‐approximate the perineal muscles and the skin was closed using continuous (subcuticular) sutures. One trial used interrupted inverted sutures in the 'interrupted' comparison group to close the perineal muscles, followed by interrupted inverted stiches to re‐approximate the skin (sutures were inserted a few millimetres under the skin edges and not transcutaneously) (Kindberg 2008).
Three of the trials included in the review used polyglycolic acid (Dexon) suture material throughout for repair of the vagina, perineal muscles and skin in each comparison group (Banninger 1978; Detlefsen 1980; Isager‐Sally 1986). The Almeida 2008, Morano 2006 and Valenzuela 2009 trial used the more rapidly absorbing Polyglactin 910 (Vicryl Rapide) suture material for perineal repair in both comparison groups, whereas the Croce 1997 trial used catgut suture material in both groups. The trial conducted by Kindberg 2008 used a more rapidly absorbing Polyglactin 910 (Vicryl Rapide) and Polyglactin 910 (Standard Vicryl) suture material (suture material was changed after 50% of the sample had been recruited). The Oboro 2003 trial used chromic catgut or polyglycolic acid suture material in each comparison group; however, it was not clear how it was allocated. The Stark 2009 and Zafar 2008 trial used polyglactin 910 (Standard Vicryl) suture material for both comparison groups, although in the Zafar 2008 trial 16 participants had chromic catgut sutures. A further five trials used a factorial 2 x 2 design whereby they compared suture techniques and materials (Gordon 1998; Kettle 2002; Kokanali 2011; Mahomed 1989; Perveen 2009). Participants in the Gordon 1998 trial were repaired with chromic catgut (approximately 50%) and polyglactin 910 (Standard Vicryl) suture material (approximately 50%); participants in the Mahomed 1989 trial were repaired with chromic catgut (approximately 50%) and polyglycolic acid (Dexon) suture material (approximately 50%); participants in the Kettle 2002 trial were repaired with the more rapidly absorbing Polyglactin 910 (Vicryl Rapide) or Polyglactin 910 (Standard Vicryl) suture material (50%) in each comparison group; participants in the Kokanali 2011 trial were repaired with monofilament or multifilament suture material (50%) in each group and the participants in the Perveen 2009 trial used chromic catgut or Polyglactin 910 (Standard Vicryl) suture material (50%) in each comparison group.
All 16 trials used absorbable suture material; however, there were some variations among type of material, gauge and needle size used. In addition, there was some clinical heterogeneity between trials in respect of skill and training of the operator (see Characteristics of included studies for details).
Excluded studies
We excluded five studies (Bendsen 1980; Buchan 1980; Doyle 1993; Hansen 1975; Roberts 1993); in all cases the reason for exclusion was that in addition to comparing suture techniques, different types of suture materials (non‐absorbable versus absorbable) were used in the different arms of trials. The use of different materials is likely to have a confounding effect and results were difficult to interpret.
For details of the excluded studies, see Characteristics of excluded studies.
Risk of bias in included studies
The methodological quality of the trials included review was inconsistent.
Allocation
Sequence generation
Methods used to generate the randomisation sequence were rated as adequate for most of these trials. Authors of five trials described using computer‐generated allocation sequences (Almeida 2008; Morano 2006; Oboro 2003; Valenzuela 2009; Zafar 2008). Kindberg 2008 reported using a computerised voice response system and Kettle 2002 used a remote clinical trials unit to generate the randomisation sequence. Random number tables were used in the Mahomed 1989 study. Gordon 1998 used a variable block design, although it was not clear how the order of allocation was decided. Methods were not clearly described in the studies by Detlefsen 1980, Croce 1997, Kokanali 2011, Isager‐Sally 1986 and Stark 2009, and the method was rated as inadequate for the Banninger 1978 and Perveen 2009 trials where an alternating sequence or sequential method was used.
Allocation concealment
Treatment allocation was concealed at the point of randomisation by the use of sealed, opaque, numbered envelopes in seven trials (Gordon 1998; Isager‐Sally 1986; Kettle 2002, Mahomed 1989; Morano 2006; Oboro 2003; Valenzuela 2009), and Kindberg 2008 described using a remote system. In the remaining eight trials the method was either unclear (Almeida 2008; Croce 1997; Detlefsen 1980; Kokanali 2011; Stark 2009; Zafar 2008), or inadequate: the Banninger 1978 trial used a quasi‐random method of treatment allocation by 'alternating sequence' and in the Perveen 2009 trial women were allocated sequentially to four arms; these methods carry a serious risk of introducing selection bias as those carrying out randomisation are able to anticipate sequence order in advance.
Blinding
Blinding the staff carrying out repairs would not be feasible with an intervention of this type. Staff frequently required additional training to be able to participate in trials, and frequently the same staff carried out both types of repair. In some of the trial reports information on protocol deviations was provided, and this indicates that staff may have had a preferred method of repair, and greater skill and confidence using a particular technique.
In most of the studies blinding women was not generally attempted, although authors sometimes claimed that women were blind to group allocation (women were simply not told which group they were in). Kindberg 2008 reported that the two methods "appeared similar", and Morano 2006 referred to a "double‐blind" study technique. Blinding women may not have been convincing as women would have been able to feel the repair, could possibly have seen it, discussed it with staff and others, and may well have had access to case notes. Moreover, women would probably have been aware of the type of repair if they had required suture removal, or had particular problems.
Blinding outcome assessors was also unlikely to have been convincing. Gordon 1998 and Valenzuela 2009 reported that interview data were collected by "blind" midwives, and Kindberg 2008 reported that the two techniques would "appear similar" to staff. Most of these studies collected outcome data that would necessitate examination of the perineum, and the type of repair may have been apparent to experienced clinicians.
The difficulties associated with blinding women, clinical staff and researchers to treatment allocation in these studies is potentially a serious source of bias particularly as several key outcomes (pain) involved women reporting to staff who would be aware of treatment allocation, and may even have carried out the repairs themselves.
Incomplete outcome data
Loss to follow‐up and missing data were problems in many of these studies and this means that results for some outcomes may be at high risk of bias; this particularly applies to long‐term outcomes.
There were missing outcome data in all studies although Kettle 2002, Kindberg 2008, Kokanali 2011 and Gordon 1998 had high response rates and few missing data at all data collection points (less than 10% attrition even for long‐term outcomes). Other studies had greater losses, even for outcomes measured in the first few days after delivery.
In the study by Almeida 2008 randomisation occurred at the point of delivery; 95 women were approached and 34 were excluded and replaced. It was not clear whether this exclusion and replacement took place after randomisation. If so, this represents a very high level of attrition (more than 30%) and means the study is at high risk of bias.
Morano 2006 reported approximately 10% loss to follow‐up by day 10, Zafar 2008 reported 29% attrition by day seven. Mahomed 1989 had high response rates at day two (97%) but by 10 days this had dropped to 86% and to 87% at three months.
The Isager‐Sally 1986 trial randomised 600 women to the two groups that were included in the meta‐analysis; however, approximately 11% (70 women) were excluded from the study soon after entry. The authors reported that it was not possible to provide follow‐up for these women, as most of them were transferred with their babies to a paediatric department in another unit, or they chose to leave hospital before the fifth day after delivery. These women were also excluded from the three‐month follow‐up; 86% of those participants who were initially randomised to the trial responded to the three‐month questionnaire.
Loss to follow‐up was a particular problem for longer‐term outcomes. A total of 90% of participants returned for follow‐up examination at two months in the Detlefsen 1980 trial; 85% of participants responded at three months in the Mahomed 1989 trial. In the Oboro 2003 study there were approximately 20% missing data for longer‐term outcomes, and in the Banninger 1978 trial two‐thirds of the sample were lost by three months (we have not included data for long‐term outcomes from this trial in the analyses in the review).
Twenty‐two randomisation envelopes were unaccounted for in the Mahomed 1989 trial and one in the Kettle 2002 trial.
Other potential sources of bias
There was little evidence of baseline imbalance between groups in these studies. However, there was some evidence of greater protocol deviations for women in particular arms of trials. For example, in the Mahomed 1989 trial 18% of those women allocated to the continuous suture group actually had interrupted sutures, while only 2% of those randomised to the interrupted group had continuous sutures. Furthermore, in the Mahomed 1989 trial midwives sometimes asked doctors to carry out the repairs (rather than carrying out the repair themselves) if the allocation was to continuous technique. Kettle 2002 reported some protocol deviations and suggested that less‐experienced staff were more likely to use interrupted techniques for women in the comparison group of this trial. In both of these trials data were analysed according to randomisation group. However, such protocol deviations may mean that the treatment effect has been underestimated.
Effects of interventions
We have included 16 studies, involving 8184 women at point of entry.
Continuous versus interrupted sutures (Comparisons 1 and 2), 12 studies, 4777 women
Primary outcomes
Short‐term pain ‐ up to day 10 postpartum
Nine trials presented data in a suitable format for inclusion in this analysis (Almeida 2008; Banninger 1978; Croce 1997; Isager‐Sally 1986; Kettle 2002; Mahomed 1989; Morano 2006; Perveen 2009; Valenzuela 2009). The trials used a variety of categorical scales to measure the pain experienced by women, and data from these were combined and included in the meta‐analysis as dichotomous outcomes (pain or no pain). Pooled results indicated that the risk of experiencing short‐term pain is less when continuous suture techniques are used for perineal closure versus interrupted sutures (average RR 0.76; 95% CI 0.66 to 0.88; 95% prediction interval 0.49 to 1.19, nine trials, 4231 women) (Analysis 1.1). However, results from individual studies varied considerably, and there was high heterogeneity for this outcome and so a random‐effects model was used to provide an average treatment effect (heterogeneity: I2 = 67%, T2 = 0.03, Chi2 test for heterogeneity P = 0.002). In three of the nine studies (Isager‐Sally 1986; Kettle 2002; Morano 2006) there was a statistically significant difference between the two groups (RR 0.73; 95% CI 0.65 to 0.81; RR 0.60; 95% CI 0.52 to 0.69; and RR 0.54; 95% CI 0.39 to 0.74, respectively), in other trials the treatment effect was less pronounced or CIs were wide, or both. It is possible that some of the heterogeneity may have been because of differences in the ways women were asked about their pain in different studies. Subgroup analysis suggested that there may have been a reduction in pain associated with continuous suturing for all layers (Almeida 2008; Croce 1997; Isager‐Sally 1986; Kettle 2002; Morano 2006; Perveen 2009; Valenzuela 2009) (RR 0.74; 95% CI 0.62 to 0.87) versus continuous subcutaneous for closure of perineal skin only (Banninger 1978; Mahomed 1989) (RR 0.89; 95% CI 0.73 to 1.07); however, there was high heterogeneity in the "all layers" subgroup, there was considerable overlap in the CIs for the two subgroups, and the test for subgroup differences was not statistically significant (Analysis 2.1).
1.1. Analysis.
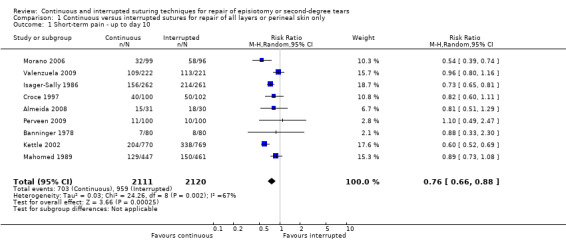
Comparison 1 Continuous versus interrupted sutures for repair of all layers or perineal skin only, Outcome 1 Short‐term pain ‐ up to day 10.
2.1. Analysis.
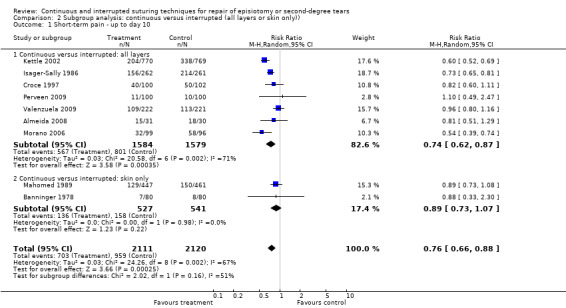
Comparison 2 Subgroup analysis: continuous versus interrupted (all layers or skin only)), Outcome 1 Short‐term pain ‐ up to day 10.
Analgesia use ‐ up to day 10 postpartum
Six of the included trials with data for 2971 women (Almeida 2008; Banninger 1978; Kettle 2002; Mahomed 1989; Morano 2006; Stark 2009) presented data regarding analgesia use in the immediate postpartum period that showed an overall reduction in analgesia use associated with the continuous techniques versus interrupted stitches (all layers or skin only) (RR 0.70; 95% CI 0.59 to 0.84) (Analysis 1.2 ). There was no significant heterogeneity between the results of the different trials, or when results were stratified by suturing method (subgroup analysis) (Analysis 2.2).
1.2. Analysis.
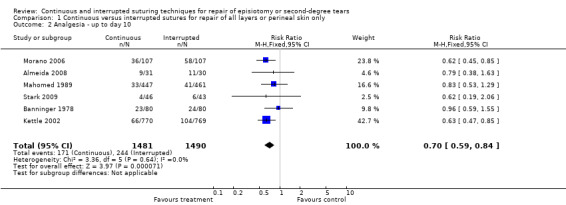
Comparison 1 Continuous versus interrupted sutures for repair of all layers or perineal skin only, Outcome 2 Analgesia ‐ up to day 10.
2.2. Analysis.
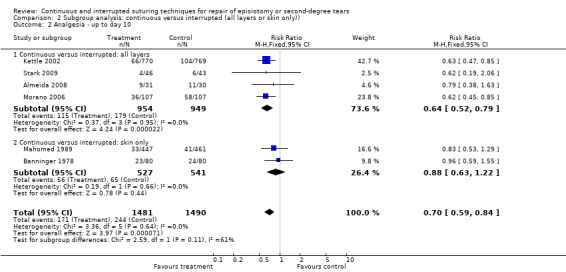
Comparison 2 Subgroup analysis: continuous versus interrupted (all layers or skin only)), Outcome 2 Analgesia ‐ up to day 10.
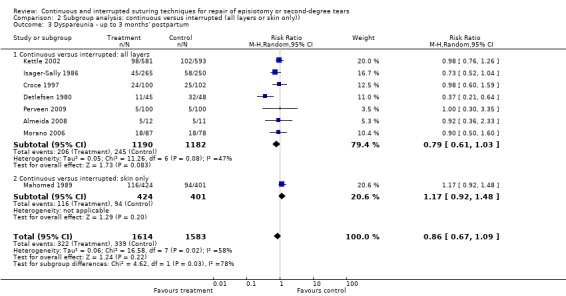
Dyspareunia ‐ reported up to three months after delivery
Nine trials with 3619 women provided data for inclusion in this analysis (Almeida 2008; Croce 1997; Detlefsen 1980; Isager‐Sally 1986; Kettle 2002; Mahomed 1989; Morano 2006; Perveen 2009; Valenzuela 2009). Although several trials reported a positive treatment effect associated with continuous suturing, overall, the meta‐analysis did not demonstrate any strong evidence of reduction in dyspareunia experienced by participants in the continuous technique groups (all layers or skin only), (average RR 0.86; 95% CI 0.70 to 1.06; 95% prediction interval 0.50 to 1.47). The presence of significant heterogeneity between trials makes any form of summary measure difficult to interpret although much of the heterogeneity was because of the more pronounced treatment effect in one of the trials (Detlefsen 1980) (heterogeneity: I2 53%, T2 0.04, Chi2 test for heterogeneity P = 0.03) (Analysis 1.3).
1.3. Analysis.
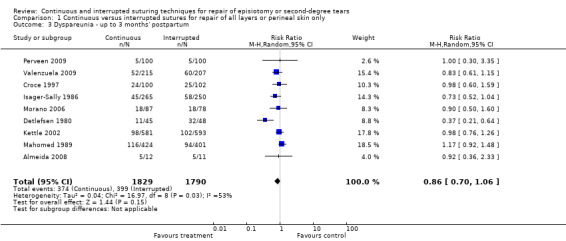
Comparison 1 Continuous versus interrupted sutures for repair of all layers or perineal skin only, Outcome 3 Dyspareunia ‐ up to 3 months' postpartum.
Secondary outcomes
Re‐suturing of wound ‐ reported up to three months after delivery
Data regarding the incidence of re‐suturing in the two intervention groups were provided by five trials with 3255 women. The Mahomed 1989 trial reported three cases requiring re‐suturing in each comparison group; the Banninger 1978 and Morano 2006 trials reported none in either group, the Kettle 2002 trial reported three cases in the treatment group and one case in the control group and the Valenzuela 2009 study there were no women requiring wound re‐suturing in the continuous group compared with two in the interrupted sutures group. Meta‐analysis showed that there was no difference in risk of re‐suturing between groups; however, with only 12 cases reported (six in each group) the numbers were too small to draw reliable conclusions (Analysis 1.4).
1.4. Analysis.
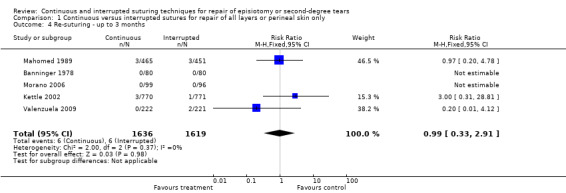
Comparison 1 Continuous versus interrupted sutures for repair of all layers or perineal skin only, Outcome 4 Re‐suturing ‐ up to 3 months.
Long‐term pain ‐ reported up to three months after delivery
Four trials (2891 women) presented data in a suitable format for inclusion in this analysis (Almeida 2008; Kettle 2002; Mahomed 1989; Valenzuela 2009). Overall the meta‐analysis showed that there was no significant difference in long‐term pain between the continuous and interrupted groups (average RR 0.88; 95% CI 0.64 to 1.20) (Analysis 1.5). There was some variability in these trials in the proportions of women reporting long‐term pain, with the number of women reporting pain being considerably lower in the Almeida 2008 and Valenzuela 2009 trials compared with the number reporting pain in the trials by Kettle 2002 and Mahomed 1989. A random‐effects method was used for this meta‐analysis.
1.5. Analysis.
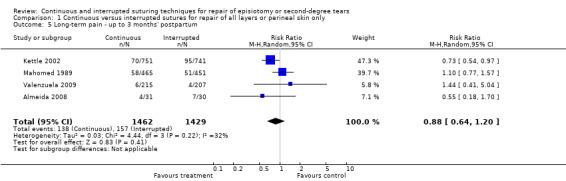
Comparison 1 Continuous versus interrupted sutures for repair of all layers or perineal skin only, Outcome 5 Long‐term pain ‐ up to 3 months' postpartum.
Failure to resume pain‐free intercourse ‐ up to three months after delivery
Two trials (2305 women) presented data for inclusion in this analysis (Kettle 2002; Mahomed 1989). Overall, there was no significant difference in failure to resume pain‐free intercourse between the two groups, with no evidence of heterogeneity of treatment effect (RR 1.07; 95% CI 0.93 to 1.24) (Analysis 1.6).
1.6. Analysis.
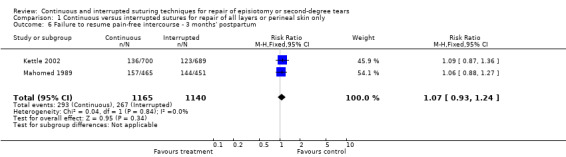
Comparison 1 Continuous versus interrupted sutures for repair of all layers or perineal skin only, Outcome 6 Failure to resume pain‐free intercourse ‐ 3 months' postpartum.
Removal of suture material ‐ up to three months after delivery
Six trials (3453 women) provided data for inclusion in the analysis (Kettle 2002; Mahomed 1989; Morano 2006; Perveen 2009; Stark 2009; Valenzuela 2009). The Morano 2006 trial reported no events of suture removal in either group, and there was no significant evidence of any difference between groups in the Valenzuela 2009 study, whereas the Kettle 2002, Mahomed 1989 and Perveen 2009 trials reported the removal of suture material to be less frequent in the continuous perineal closure groups. Overall pooled results suggest a marginally statistically significant difference between groups (favouring the continuous suture group) for this outcome but high levels of heterogeneity (I2 = 82%) in results mean that results should be interpreted with caution (average RR 0.56; 95% CI 0.32 to 0.98; 95% prediction interval 0.11 to 2.97) (Analysis 1.7).
1.7. Analysis.
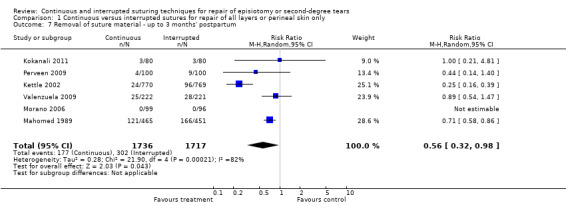
Comparison 1 Continuous versus interrupted sutures for repair of all layers or perineal skin only, Outcome 7 Removal of suture material ‐ up to 3 months' postpartum.
Non pre‐specified outcomes: resource use
In the trials by Valenzuela 2009 and Kettle 2002 the amount of suture material used was examined, and although the results of the two trials were very different, both showed that operators were much more likely to use more suture material (two or more packets) when the repair was done using the interrupted technique (RR 0.26; 95% CI 0.22 to 0.30) (Analysis 1.8); Kokanali 2011 also reported a significant reduction in the amount of suture material in the continuous repair group although the difference between groups was reported in centimetres rather than the use of sterile packets of suture material and the cost implications of the difference between groups was not clear (data not shown). Four studies (Almeida 2008; Kettle 2002; Kokanali 2011; Valenzuela 2009) looked at the time taken by operators to carry out the repairs; pooled results suggested there was no statistically significant difference between groups, although suturing time varied considerably between these studies and results were not consistent among the trials. Findings for this outcome are difficult to interpret as operators may have been more used to performing a particular technique and may have completed repairs using the technique with which they were more familiar in less time (mean difference ‐0.73 minutes; 95% CI ‐2.24 to 0.78 minutes) (Analysis 1.9). (We noted that for the Kokanali 2011 study the standard deviations were much lower than in any of the other studies; temporarily removing this study from the analysis resulted in a mean difference of ‐0.64 minutes; 95% CI ‐3.46 to 2.18 minutes; data not shown.)
1.8. Analysis.
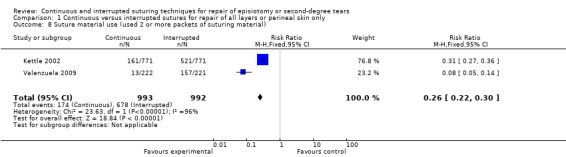
Comparison 1 Continuous versus interrupted sutures for repair of all layers or perineal skin only, Outcome 8 Suture material use (used 2 or more packets of suturing material).
1.9. Analysis.
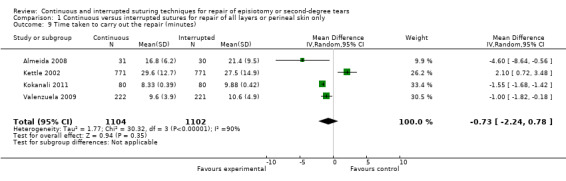
Comparison 1 Continuous versus interrupted sutures for repair of all layers or perineal skin only, Outcome 9 Time taken to carry out the repair (minutes).
Three‐stage versus two‐stage approaches (Comparison 3), two studies, 2857 women
Two studies compared a two‐stage repair technique (where the skin was opposed but remained unsutured) with a more traditional three‐stage approach (Gordon 1998; Oboro 2003).
Primary outcomes
Short‐term pain ‐ up to day 10 postpartum
Pooled results suggested that two‐stage repair techniques were associated with fewer women experiencing pain at up to two days and at up to 14 days (average RR 0.92; 95% CI 0.84 to 1.02 and RR 0.86; 95% CI 0.76 to 0.98, respectively) although the difference between groups did not reach statistical significance at two days (Analysis 3.1; Analysis 3.2).
3.1. Analysis.
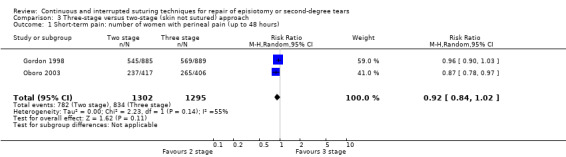
Comparison 3 Three ‐stage versus two‐ stage (skin not sutured) approach, Outcome 1 Short‐term pain: number of women with perineal pain (up to 48 hours).
3.2. Analysis.
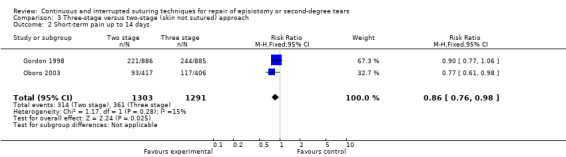
Comparison 3 Three ‐stage versus two‐ stage (skin not sutured) approach, Outcome 2 Short‐term pain up to 14 days.
Analgesia use ‐ up to day 10 postpartum
There was no statistically significant evidence of any difference between groups for use of analgesia up to 10 days, although there was high heterogeneity between these two studies and result should be interpreted with caution (Analysis 3.3).
3.3. Analysis.
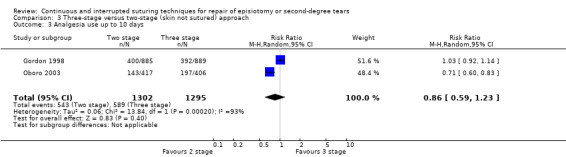
Comparison 3 Three ‐stage versus two‐ stage (skin not sutured) approach, Outcome 3 Analgesia use up to 10 days.
Dyspareunia ‐ reported up to three months after delivery
Women undergoing two‐stage repairs were less likely to report dyspareunia compared with those having three‐stage repairs, although there was evidence of moderate heterogeneity for this outcome (average RR 0.72; 95% CI 0.56 to 0.94) (heterogeneity I2 = 41%, T2 = 0.02, Chi2 test for heterogeneity 0.19) (Analysis 3.4).
3.4. Analysis.
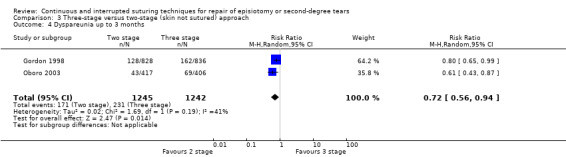
Comparison 3 Three ‐stage versus two‐ stage (skin not sutured) approach, Outcome 4 Dyspareunia up to 3 months.
Secondary outcomes
Long‐term pain ‐ reported up to three months after delivery
There was no clear evidence of any difference between groups for long‐term pain (Analysis 3.5).
3.5. Analysis.
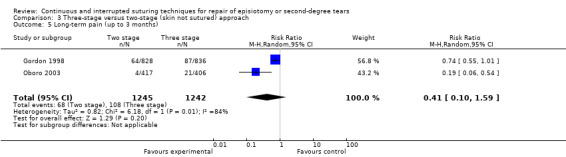
Comparison 3 Three ‐stage versus two‐ stage (skin not sutured) approach, Outcome 5 Long‐term pain (up to 3 months).
Resumption of pain‐free intercourse
Gordon 1998 and Oboro 2003 both reported failure to resume pain‐free intercourse, and again results favoured women having two‐stage repairs (RR 0.86; 95% CI 0.80 to 0.92) (Analysis 3.6).
3.6. Analysis.
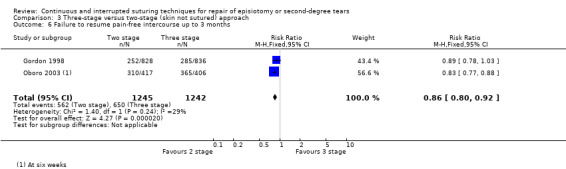
Comparison 3 Three ‐stage versus two‐ stage (skin not sutured) approach, Outcome 6 Failure to resume pain‐free intercourse up to 3 months.
Wound 'gaping' ‐ reported up to three months after delivery
It was more likely for women who had two‐stage repairs to have wounds that appeared to be 'gaping' (more than 0.5 cm) in the first week to 10 days after repair, although there was considerable heterogeneity between the findings from the two studies contributing data (Analysis 3.7).
3.7. Analysis.
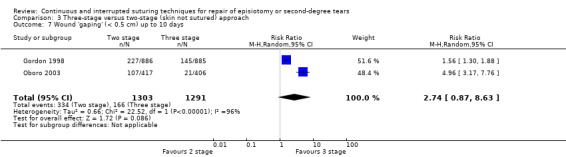
Comparison 3 Three ‐stage versus two‐ stage (skin not sutured) approach, Outcome 7 Wound 'gaping' (< 0.5 cm) up to 10 days.
Re‐suturing of wound ‐ reported up to three months after delivery
Women having two‐stage repairs seemed less likely to require their wounds to be re‐sutured (average RR 0.56; 95% CI 0.31 to 1.00) (Analysis 3.8).
3.8. Analysis.
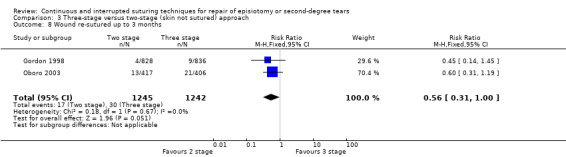
Comparison 3 Three ‐stage versus two‐ stage (skin not sutured) approach, Outcome 8 Wound re‐sutured up to 3 months.
Removal of suture material ‐ up to three months after delivery
Three‐stage repairs were associated with more women requiring the removal of suture material at up to three months after delivery (RR 0.60; 95% CI 0.46 to 0.77) (Analysis 3.9).
3.9. Analysis.
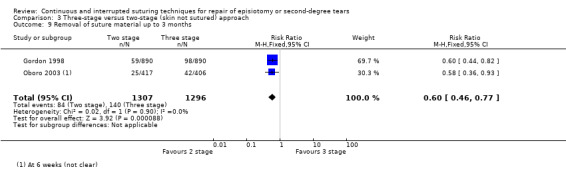
Comparison 3 Three ‐stage versus two‐ stage (skin not sutured) approach, Outcome 9 Removal of suture material up to 3 months.
Non pre‐specified outcomes: resource use
Oboro 2003 examined the time taken to carry out two‐ and three‐stage repairs, two‐stage repairs took, on average, four minutes less to complete (21 versus 25 minutes) (Analysis 3.10).
3.10. Analysis.
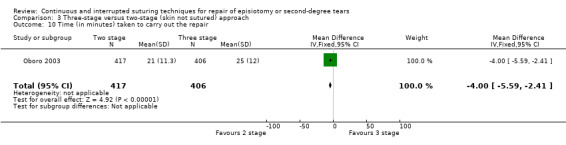
Comparison 3 Three ‐stage versus two‐ stage (skin not sutured) approach, Outcome 10 Time (in minutes) taken to carry out the repair.
Other techniques (Comparison 4), two trials, with 550 women
Two studies described findings for other suturing techniques. Kindberg 2008 compared two groups of women; in the 'continuous suture' group the vagina and perineal muscles were closed with a continuous suturing technique followed by subcutaneous skin closure (continuous for all layers); in the comparison group the vagina was closed with a continuous non‐locking suture, followed by interrupted 'inverted' sutures to close the perineal muscles, and interrupted inverted stiches to re‐approximate the skin (sutures were inserted a few millimetres under the skin edges and not transcutaneously). Zafar 2008 compared the 'continuous' technique whereby the vaginal mucosa was closed with a running stitch and the same suture was used to re‐approximate the perineal muscle in two layers, followed by subcuticular sutures to close the skin (finishing at the lower end of the incision). In the 'interrupted' comparison group the vaginal mucosa was closed with a continuous running stitch, followed by interrupted sutures inserted in two layers to re‐approximate the perineal muscles and the skin was closed using continuous (subcuticular) suture. In view of the differences in the techniques used in these two trials we have not pooled results from studies in meta‐analysis, rather we have provided subgroup totals only.
Primary outcomes
Short‐term pain and analgesia use ‐ up to day 10 postpartum
Kindberg 2008 examined pain at 10 days after delivery and found no significant differences between groups (Analysis 4.1).
4.1. Analysis.
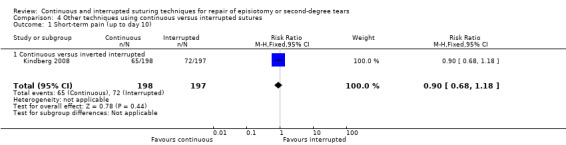
Comparison 4 Other techniques using continuous versus interrupted sutures, Outcome 1 Short‐term pain (up to day 10).
In the Zafar 2008 trial, data on short‐term pain was collected at 12 hours after delivery and, at this early stage, the single knot approach appeared to be associated with lower pain scores compared with the more traditional technique (Analysis 4.2).
4.2. Analysis.
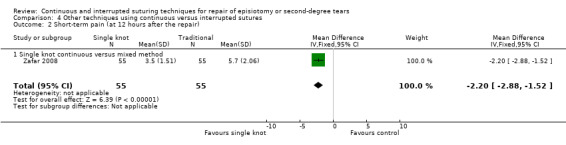
Comparison 4 Other techniques using continuous versus interrupted sutures, Outcome 2 Short‐term pain (at 12 hours after the repair).
Both studies collected information on the use of analgesics; neither study reported statistically significant differences between groups (Analysis 4.3).
4.3. Analysis.
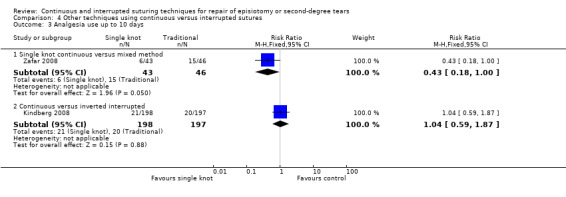
Comparison 4 Other techniques using continuous versus interrupted sutures, Outcome 3 Analgesia use up to 10 days.
Dyspareunia ‐ reported up to three months after delivery
Kindberg 2008 collected information on dyspareunia and found no statistically significant differences between groups (Analysis 4.4).
4.4. Analysis.
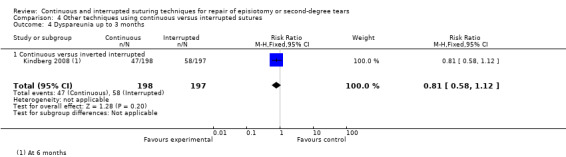
Comparison 4 Other techniques using continuous versus interrupted sutures, Outcome 4 Dyspareunia up to 3 months.
Secondary outcomes
Wound breakdown at up to three months
Zafar 2008 examined superficial wound gaping and found no significant differences between groups. Kindberg 2008 found no evidence of differences between groups for wound re‐suturing at up to three months (Analysis 4.5; Analysis 4.6).
4.5. Analysis.
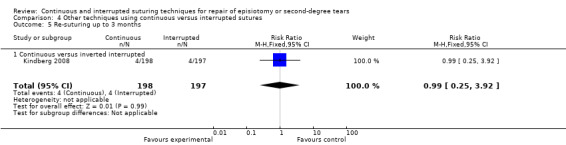
Comparison 4 Other techniques using continuous versus interrupted sutures, Outcome 5 Re‐suturing up to 3 months.
4.6. Analysis.
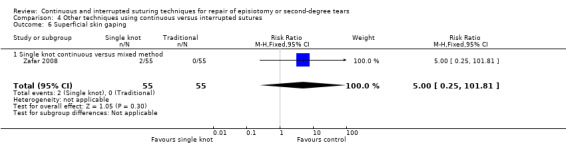
Comparison 4 Other techniques using continuous versus interrupted sutures, Outcome 6 Superficial skin gaping.
Removal of suture material up to three months
Kindberg 2008 reported findings for the number of women requiring the removal of suture material. There was no clear evidence of a difference between treatment groups for this outcome (Analysis 4.7).
4.7. Analysis.
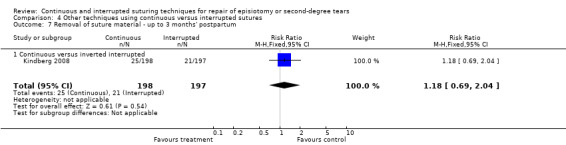
Comparison 4 Other techniques using continuous versus interrupted sutures, Outcome 7 Removal of suture material ‐ up to 3 months' postpartum.
Non pre‐specified outcomes: resource use and satisfaction with repair
Zafar 2008 reported that the single knot (continuous repair) took less time than the traditional technique (all repairs were carried out by the same person and in both arms of this trial repairs were completed much more speedily than in other studies examining different types of repairs) (Analysis 4.8).
4.8. Analysis.
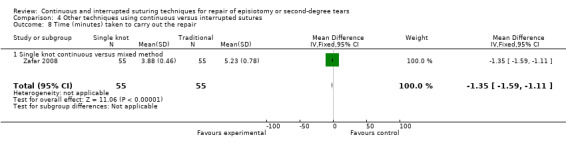
Comparison 4 Other techniques using continuous versus interrupted sutures, Outcome 8 Time (minutes) taken to carry out the repair.
Kindberg 2008 reported that repairs using the continuous technique required one packet of suture material, whereas the inverted interrupted method required two and that the continuous technique was quicker to perform compared with the inverted interrupted technique (15 minutes versus 17 minutes; standard deviations not reported).
Kindberg 2008 reported that similar numbers of women in both arms of this trial were satisfied with their perineal repairs (Analysis 4.9).
4.9. Analysis.
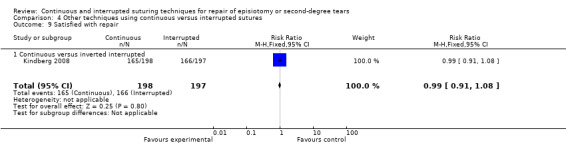
Comparison 4 Other techniques using continuous versus interrupted sutures, Outcome 9 Satisfied with repair.
Discussion
Summary of main results
The meta‐analysis of data provides evidence that continuous techniques for perineal closure (all layers or skin only) cause less pain in the immediate postpartum period, less need for analgesia and less need for suture removal compared with interrupted stitching methods. However, there is a significant degree of heterogeneity between trials for several outcomes that may be a result of clinical heterogeneity in terms of input in perineal repair training, different suturing techniques and materials used (see Characteristics of included studies tables for details).
There is also some evidence that the continuous technique uses less suture material when compared with the interrupted methods (one packet compared to two or three packets, respectively). This is important information, as the introduction of a continuous suturing policy would reduce the overall suture material expenditure for maternity units worldwide.
To investigate the heterogeneity of results between the different trials, in line with the philosophy of Greenland 1987, we considered the possible sources of heterogeneity. In particular, we looked at the heterogeneity of treatment effects stratified by continuous suturing for all layers versus continuous subcutaneous for closure of perineal skin only. Six of the included trials (Croce 1997; Detlefsen 1980; Isager‐Sally 1986; Kettle 2002; Morano 2006, Perveen 2009) used a non‐locking continuous suturing technique to repair the vagina and perineal muscles with a continuous subcutaneous stitch inserted to close the skin in the experimental group; four trials (Croce 1997; Detlefsen 1980; Isager‐Sally 1986; Kettle 2002) used a locking suture for the vagina, and interrupted sutures to repair perineal muscle and skin in the control group and the Morano 2006 trial used a non‐locking suture for repair of the vaginal mucosa, three or four interrupted stitches to repair the deep and superficial perineal muscles, and interrupted transcutaneous stitches inserted to close the skin. The other two trials by Mahomed 1989 and Banninger 1978 used a locking continuous stitch and interrupted stitches to repair the vagina, respectively; interrupted stitches for the muscle layer and continuous subcutaneous stitches versus interrupted for skin closure.
The rationale for performing continuous suturing indicates that any benefit would be larger in those trials that use continuous suturing throughout for all layers, therefore this was investigated by performing stratified subgroup analysis. However, there remained considerable heterogeneity within the continuous 'all layers' group.
The Mahomed 1989 trial reported that the subcutaneous method of perineal skin closure was less practiced and unpopular with some operators and there was some cross‐over of treatment allocation (96 women in the subcutaneous group had interrupted transcutaneous stitches inserted). In the Almeida 2008 trial, there was also evidence of treatment cross‐over for women allocated to the interrupted suture group. Deviation from protocol and variation in technique within trial arms mean that results were more difficult to interpret. In the Kettle 2002 trial, adherence to treatment allocation was very high. Perhaps the better results produced by the Isager‐Sally 1986 trial were because of the continuous technique being introduced several months prior to the trial starting, thus ensuring that all members of staff were familiar with the new technique of perineal repair. In the Kettle 2002 trial, midwives received standardised training in both techniques (interrupted and continuous) prior to the study commencing. However, owing to rotation of midwives from the delivery suite and delay in starting the study, many of the participating midwives were not familiar with the continuous technique and were trained during the early part of the recruitment phase. During the first phase of the Kettle 2002 trial, senior midwives were more likely to undertake the continuous suturing. This imbalance was considered in a subsequent association analysis; however, there was no evidence of significant heterogeneity between groups.
Meta‐analysis also showed that continuous techniques were associated with a reduction in the need for suture removal up to three months following childbirth. It could be argued that this finding may be because continuous subcutaneous stitches are less accessible than interrupted transcutaneous stitches. Nevertheless, this finding is important, as most women find the experience of having sutures removed from perineal wounds very distressing.
Quality of the evidence
Overall, the quality of the evidence on which conclusions of the review are based was mixed. For methods of randomisation approximately half of the studies used methods of sequence generation and allocation concealment that we assessed as low risk of bias, while in other trials' methods were either not described, not clear or were at high risk of bias. Blinding operatives for this type of intervention may not be feasible and attempts to blind outcome assessors may not be convincing. It is difficult to assess whether lack of blinding of staff carrying out repairs affected other aspects of care, and for us to judge the overall impact of lack of blinding on outcomes. As we discussed above, some staff may have been more familiar with (and possibly preferred) one technique and this may have affected the quality of their repair and the way they assessed outcomes. An additional problem in some studies was the loss to follow‐up; even relatively small losses to follow‐up may be important for outcomes such as removal of suture material and the need for re‐suturing where event rates are relatively low.
Potential biases in the review process
We are aware that there is a risk of introducing bias at all stages in the review process. Assessing risk of bias, for example, involves individual judgements. We took a number of steps to reduce bias such as having two review authors assess each paper independently. One review author was an investigator in one of the included trials (Kettle 2002) and this author was therefore not involved in the assessment of evidence for this trial.
Authors' conclusions
Implications for practice.
The evidence produced by this review shows that continuous suturing techniques for perineal closure is associated with less short‐term pain. There is also some evidence that if the continuous technique is used for all layers (vagina, perineal muscles and skin), the benefit in terms of reducing pain may be even greater.
The continuous technique is easily performed by the novice or inexperienced operator. In addition, it has economical advantages in that the continuous technique requires one packet of suture material per perineal repair compared to two or more packets for the interrupted method (Kettle 2002). Therefore, the non‐locking continuous suturing technique is recommended for repair of vagina and perineal muscles with a continuous subcutaneous stitch to close the perineal skin.
Implications for research.
The review has highlighted the following areas that are worthy of further evaluation.
Future trials relating to perineal trauma need to address outcomes that are important to women, including sexual problems and pelvic floor muscle dysfunction in the immediate‐ and long‐term period following childbirth.
Research into the impact of standardised training programmes for the identification, management and repair of perineal trauma on short‐ and long‐term maternal morbidity.
Clinical trials to investigate techniques for the prevention of perineal trauma.
What's new
| Date | Event | Description |
|---|---|---|
| 12 March 2012 | New search has been performed | The most recent search was in January 2012. In this updated version of the review, we have included nine new studies in addition to the seven included in previous versions. |
| 12 March 2012 | New citation required but conclusions have not changed | The main conclusions of the review have not changed but we have added new comparisons and analysis. |
History
Protocol first published: Issue 1, 1997 Review first published: Issue 1, 1998
| Date | Event | Description |
|---|---|---|
| 1 September 2008 | Amended | Converted to new review format. |
| 12 July 2007 | New citation required and conclusions have changed | Meta‐analysis indicates that the subcutaneous suturing technique for perineal skin closure is associated with less short‐term pain, however a subgroup analysis showed that if the continuous technique is used for all layers (vagina, perineal muscles and skin) the reduction in pain is more significant. |
| 30 June 2007 | New search has been performed | Search updated. Three new studies were added to the included studies and four were added to the excluded studies. Changes to the text have been made to reflect new data. |
Acknowledgements
The Pregnancy and Childbirth Group (Liverpool) for their assistance and support during the preparation of this systematic review.
Data and analyses
Comparison 1. Continuous versus interrupted sutures for repair of all layers or perineal skin only.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Short‐term pain ‐ up to day 10 | 9 | 4231 | Risk Ratio (M‐H, Random, 95% CI) | 0.76 [0.66, 0.88] |
| 2 Analgesia ‐ up to day 10 | 6 | 2971 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.70 [0.59, 0.84] |
| 3 Dyspareunia ‐ up to 3 months' postpartum | 9 | 3619 | Risk Ratio (M‐H, Random, 95% CI) | 0.86 [0.70, 1.06] |
| 4 Re‐suturing ‐ up to 3 months | 5 | 3255 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.99 [0.33, 2.91] |
| 5 Long‐term pain ‐ up to 3 months' postpartum | 4 | 2891 | Risk Ratio (M‐H, Random, 95% CI) | 0.88 [0.64, 1.20] |
| 6 Failure to resume pain‐free intercourse ‐ 3 months' postpartum | 2 | 2305 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.07 [0.93, 1.24] |
| 7 Removal of suture material ‐ up to 3 months' postpartum | 6 | 3453 | Risk Ratio (M‐H, Random, 95% CI) | 0.56 [0.32, 0.98] |
| 8 Suture material use (used 2 or more packets of suturing material) | 2 | 1985 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.26 [0.22, 0.30] |
| 9 Time taken to carry out the repair (minutes) | 4 | 2206 | Mean Difference (IV, Random, 95% CI) | ‐0.73 [‐2.24, 0.78] |
Comparison 2. Subgroup analysis: continuous versus interrupted (all layers or skin only)).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Short‐term pain ‐ up to day 10 | 9 | 4231 | Risk Ratio (M‐H, Random, 95% CI) | 0.76 [0.66, 0.88] |
| 1.1 Continuous versus interrupted: all layers | 7 | 3163 | Risk Ratio (M‐H, Random, 95% CI) | 0.74 [0.62, 0.87] |
| 1.2 Continuous versus interrupted: skin only | 2 | 1068 | Risk Ratio (M‐H, Random, 95% CI) | 0.89 [0.73, 1.07] |
| 2 Analgesia ‐ up to day 10 | 6 | 2971 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.70 [0.59, 0.84] |
| 2.1 Continuous versus interrupted: all layers | 4 | 1903 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.64 [0.52, 0.79] |
| 2.2 Continuous versus interrupted: skin only | 2 | 1068 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.63, 1.22] |
| 3 Dyspareunia ‐ up to 3 months' postpartum | 8 | 3197 | Risk Ratio (M‐H, Random, 95% CI) | 0.86 [0.67, 1.09] |
| 3.1 Continuous versus interrupted: all layers | 7 | 2372 | Risk Ratio (M‐H, Random, 95% CI) | 0.79 [0.61, 1.03] |
| 3.2 Continuous versus interrupted: skin only | 1 | 825 | Risk Ratio (M‐H, Random, 95% CI) | 1.17 [0.92, 1.48] |
2.3. Analysis.
Comparison 2 Subgroup analysis: continuous versus interrupted (all layers or skin only)), Outcome 3 Dyspareunia ‐ up to 3 months' postpartum.
Comparison 3. Three ‐stage versus two‐ stage (skin not sutured) approach.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Short‐term pain: number of women with perineal pain (up to 48 hours) | 2 | 2597 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.84, 1.02] |
| 2 Short‐term pain up to 14 days | 2 | 2594 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.86 [0.76, 0.98] |
| 3 Analgesia use up to 10 days | 2 | 2597 | Risk Ratio (M‐H, Random, 95% CI) | 0.86 [0.59, 1.23] |
| 4 Dyspareunia up to 3 months | 2 | 2487 | Risk Ratio (M‐H, Random, 95% CI) | 0.72 [0.56, 0.94] |
| 5 Long‐term pain (up to 3 months) | 2 | 2487 | Risk Ratio (M‐H, Random, 95% CI) | 0.41 [0.10, 1.59] |
| 6 Failure to resume pain‐free intercourse up to 3 months | 2 | 2487 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.86 [0.80, 0.92] |
| 7 Wound 'gaping' (< 0.5 cm) up to 10 days | 2 | 2594 | Risk Ratio (M‐H, Random, 95% CI) | 2.74 [0.87, 8.63] |
| 8 Wound re‐sutured up to 3 months | 2 | 2487 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.56 [0.31, 1.00] |
| 9 Removal of suture material up to 3 months | 2 | 2603 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.60 [0.46, 0.77] |
| 10 Time (in minutes) taken to carry out the repair | 1 | 823 | Mean Difference (IV, Fixed, 95% CI) | ‐4.0 [‐5.59, ‐2.41] |
Comparison 4. Other techniques using continuous versus interrupted sutures.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Short‐term pain (up to day 10) | 1 | 395 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.68, 1.18] |
| 1.1 Continuous versus inverted interrupted | 1 | 395 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.68, 1.18] |
| 2 Short‐term pain (at 12 hours after the repair) | 1 | 110 | Mean Difference (IV, Fixed, 95% CI) | ‐2.2 [‐2.88, ‐1.52] |
| 2.1 Single knot continuous versus mixed method | 1 | 110 | Mean Difference (IV, Fixed, 95% CI) | ‐2.2 [‐2.88, ‐1.52] |
| 3 Analgesia use up to 10 days | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.1 Single knot continuous versus mixed method | 1 | 89 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.43 [0.18, 1.00] |
| 3.2 Continuous versus inverted interrupted | 1 | 395 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.04 [0.59, 1.87] |
| 4 Dyspareunia up to 3 months | 1 | 395 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.81 [0.58, 1.12] |
| 4.1 Continuous versus inverted interrupted | 1 | 395 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.81 [0.58, 1.12] |
| 5 Re‐suturing up to 3 months | 1 | 395 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.99 [0.25, 3.92] |
| 5.1 Continuous versus inverted interrupted | 1 | 395 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.99 [0.25, 3.92] |
| 6 Superficial skin gaping | 1 | 110 | Risk Ratio (M‐H, Fixed, 95% CI) | 5.0 [0.25, 101.81] |
| 6.1 Single knot continuous versus mixed method | 1 | 110 | Risk Ratio (M‐H, Fixed, 95% CI) | 5.0 [0.25, 101.81] |
| 7 Removal of suture material ‐ up to 3 months' postpartum | 1 | 395 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.18 [0.69, 2.04] |
| 7.1 Continuous versus inverted interrupted | 1 | 395 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.18 [0.69, 2.04] |
| 8 Time (minutes) taken to carry out the repair | 1 | 110 | Mean Difference (IV, Fixed, 95% CI) | ‐1.35 [‐1.59, ‐1.11] |
| 8.1 Single knot continuous versus mixed method | 1 | 110 | Mean Difference (IV, Fixed, 95% CI) | ‐1.35 [‐1.59, ‐1.11] |
| 9 Satisfied with repair | 1 | 395 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.99 [0.91, 1.08] |
| 9.1 Continuous versus inverted interrupted | 1 | 395 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.99 [0.91, 1.08] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Almeida 2008.
| Methods | RCT (individual randomisation). | |
| Participants | Setting: birth centre in a general hospital in Brazil. Dates of recruitment: July 2001 to April 2002. 61 women requiring perineal repair after episiotomy or second‐degree tear. Parity: primigravid and multigravid women included (16/31 in group 1 and 15/30 in group 2 had had a previous vaginal delivery). Mean age: group 1 = 24.2 years; group 2 = 24.2 years. Operator: 1 of 10 trained nurse/midwives. |
|
| Interventions | Method of repair: described as below. Women divided into 2 groups. Group 1 (N = 31),vaginal trauma and perineal muscle re‐approximated with the continuous non‐locking suture technique using polyglactin 910 (Vicryl Rapide) on a 1/2 circle, taper point needle (4 or 5 cm). The skin was approximated separately with a continuous intradermal suture using a 3/8 circle, reverse cutting needle. Group 2 (N = 30), vaginal trauma continuous locking and perineal muscle sutured using the interrupted technique with polyglactin 910 (Vicryl Rapide) using a 1/2 circle needle, taper point of 4 or 5 cm The skin was approximated separately with a 3/8 circle reverse cut needle of 3 cm using interrupted sutures. | |
| Outcomes | Included in analysis:
|
|
| Notes | Women in both groups had antisepsis of the vulva and perineum. Data collection from women by interview by researcher or midwife. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Described as by "electronic table". |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) Clinical staff | High risk | Different techniques used. |
| Blinding (performance bias and detection bias) Women | High risk | Different techniques. |
| Blinding (performance bias and detection bias) Outcome assessors | High risk | Method used would be recorded in notes. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Randomisation was "applied at the moment of delivery to 95 women. A total of 34 women were excluded from the study and replaced by others according to the randomization table". It was not clear whether women were excluded after randomisation. |
| Selective reporting (reporting bias) | Unclear risk | Not apparent. |
| Other bias | Unclear risk | Data collection from women by interview by researcher or midwife. There was some baseline imbalance. |
Banninger 1978.
| Methods | Quasi‐RCT. | |
| Participants | Setting: Switzerland. 160 women having an episiotomy without complications. This was a subgroup of the main trial. Method of delivery: spontaneous vaginal with cephalic presentation. Parity: primigravidae. Mean age: group 1 = 25.2 years; group 2 = 24.8 years. Operator: doctors. |
|
| Interventions | Method of repair: described as below. Women divided into 2 groups. Group 1: (N = 80), vagina, perineal muscle and skin sutured using the interrupted technique with Dexon 2/0 on a 60‐mm round bodied needle. Group 2: (N = 80), vagina and perineal muscle sutured using the interrupted technique with polyglycolic acid (Dexon) 2/0 on a 60‐mm round bodied needle. Perineal skin closed using a continuous intracutaneous (subcutaneous) technique with Dexon 3/0 on a 16‐mm 3/8 circle atraumatic cutting needle. | |
| Outcomes | Included in analysis:
|
|
| Notes | Method of repair: described. Training period: not described. Exclusion criteria: described. Participant inclusion criteria described. Does not state if trial had Research Ethics Committee approval. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Alternate sequence. |
| Allocation concealment (selection bias) | High risk | Allocated by 'alternating sequence' ‐ quasi (non)‐randomised. |
| Blinding (performance bias and detection bias) Clinical staff | High risk | Different suturing techniques. |
| Blinding (performance bias and detection bias) Women | High risk | Not stated but women may have been aware of suturing technique. |
| Blinding (performance bias and detection bias) Outcome assessors | High risk | Different suturing techniques. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | All participants entered into the trial were included in the analysis. No information available on whether analysis was by 'intention to treat'. Only one‐third of participants followed up at 3 months. Observation of cosmetic results at 3 months: no data available. |
| Selective reporting (reporting bias) | Unclear risk | Not apparent. |
Croce 1997.
| Methods | RCT. | |
| Participants | Setting: single centre (Codogno Civic Hospital, Italy). 202 women with selective episiotomy. Mean age: group A = 29.5 years; group B = 27.7 years. Operator: not stated. |
|
| Interventions | Method of repair: as described below. Women divided into 2 groups. Group 1 (N = 100), vaginal trauma sutured with a continuous (Guilmen‐Pontonnier technique) with catgut. Group 2 (N = 102), interrupted (Blair‐Donatti technique) with catgut. | |
| Outcomes | Included in analysis:
|
|
| Notes | Method of repair: described. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Allocated by 'randomisation' but matched for age, socioeconomic status and parity. |
| Allocation concealment (selection bias) | Unclear risk | No information available regarding concealment of treatment allocation. |
| Blinding (performance bias and detection bias) Clinical staff | High risk | Different suture techniques. |
| Blinding (performance bias and detection bias) Women | High risk | Not stated but women may have been aware of suturing technique. |
| Blinding (performance bias and detection bias) Outcome assessors | High risk | Not stated but assessment was likely to have included perineal examination. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Analyses apparently ITT (202 women included in the analyses) but it was not clear how many women were originally randomised. |
| Selective reporting (reporting bias) | Unclear risk | Not apparent. |
Detlefsen 1980.
| Methods | RCT. | |
| Participants | Setting: Denmark. 117 women with a medio‐lateral episiotomy. This was a subgroup of the main trial. Method of delivery: spontaneous vaginal with cephalic presentation. Parity: primigravida and multigravida included. Mean age: not specified between groups. Operator: doctors and midwives. |
|
| Interventions | Method of repair: as described below. Women divided into 2 groups. Group 1 (N = 65), vaginal trauma sutured with a continuous locking stitch, perineal muscle and skin sutured using the interrupted technique with Dexon 1/0 on a T‐125 needle. Group 2 (N = 52), vaginal trauma sutured with a continuous locking stitch, perineal muscle closed with a continuous non‐locking (running) stitch and perineal skin closed using an intracutaneous (subcuticular) technique with Dexon 1/0 on a T‐125 needle. | |
| Outcomes | Included in analysis:
|
|
| Notes | Method of repair: described. Training period: midwives and doctors underwent training for 1 month in the new suturing technique used in group 2. All women delivered between 1 April 1978 and 31 July 1978 with an episiotomy were randomised into the trial. Long‐term follow‐up: 2 and 6 months' postpartum. Does not state if trial had Research Ethics Committee approval. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Allocated by 'randomisation': method not described. |
| Allocation concealment (selection bias) | Unclear risk | Allocated by 'randomisation'. No information available regarding concealment of treatment allocation. |
| Blinding (performance bias and detection bias) Clinical staff | High risk | Different suture techniques. |
| Blinding (performance bias and detection bias) Women | High risk | Not stated but women may have been aware of suturing technique. |
| Blinding (performance bias and detection bias) Outcome assessors | High risk | |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not clear and not clear whether analysis was by 'intention to treat'. |
| Selective reporting (reporting bias) | Unclear risk | Not apparent. |
Gordon 1998.
| Methods | RCT, factorial 2 x 2 design. | |
| Participants | Setting: Ipswich hospital, UK. Data collection from 1992 to 1994. 1780 women requiring perineal repair after spontaneous or simple instrumental delivery. First‐ and second‐degree tears included. Mean age: 2‐stage repair 28.5 years; 3‐stage repair 28.2 years. Both primiparous and multiparous women included. 40% in the 2‐stage and 38% in the 3‐stage repair groups had had a previous vaginal delivery. |
|
| Interventions | 2‐stage versus 3‐stage technique. Group 1: 2‐stage repair (skin opposed but unsutured) with chromic catgut. Group 2: 3‐stage repair (skin sutured) with chromic catgut. Group 3: 2‐stage repair with polyglactin 910. Group 4: 3‐stage repair with polyglactin 910. In the analyses in this review we have combined groups 1 and 3 (2‐stage repairs) versus combined results from groups 2 and 4 (3‐stage repairs). 75% of the repairs were carried out by midwives. For 3‐stage repairs operators were encouraged to use a continuous subcuticular techniqu.e for skin closure; however, 72% had interrupted sutures inserted and 26% subcuticular |
|
| Outcomes | Included in analysis:
|
|
| Notes | Suture techniques not clearly described. There was a change in recruitment criteria during the trial. Initially only women with spontaneous deliveries were included, during the second year of the trial deliveries by non‐rotational forceps or vacuum extraction were also included. There were some protocol deviations but analyses was according to randomisation group. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation at completion of the third stage of labour. Balanced block design (variable block size) stratified by type of delivery. |
| Allocation concealment (selection bias) | Low risk | Serially numbered, sealed opaque envelopes containing suture material prepared in advance by independent researcher. |
| Blinding (performance bias and detection bias) Clinical staff | High risk | Materials and technique obviously different. |
| Blinding (performance bias and detection bias) Women | Unclear risk | Not clear, women would be aware that skin had not been sutured. |
| Blinding (performance bias and detection bias) Outcome assessors | High risk | It was stated that data collection was by a "research midwife blinded to the allocation". The outcome assessment included face‐to‐face interviews and examination of the perineum so it is very unlikely that the assessor would be blinded to the type of repair for short‐term outcome assessment. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | It was stated that primary analysis was by ITT. 1780 women were recruited, 99% followed up at 48 hours and 93% at 3 months. |
| Selective reporting (reporting bias) | Unclear risk | Not apparent. |
| Other bias | Low risk | No baseline imbalance apparent. All randomisation envelopes accounted for. Double data entry. Some protocol deviation with 12% of those allocated to the 2‐stage repair technique having skin sutured but ITT analysis. |
Isager‐Sally 1986.
| Methods | RCT. | |
| Participants | Setting: Herlev Hospital, Denmark. 530 women with medio‐lateral episiotomy were analysed. This was a subgroup of the main trial Method of delivery: spontaneous or instrumental vaginal deliveries. Parity: primigravidae and multiparae. Mean age: group 1 = 27.5 years; group 2 = 27.1 years. Operators: midwives and experienced obstetricians. |
|
| Interventions | Method of repair: described as below. Women divided into 2 groups. Group 1 (N = 263), vaginal trauma sutured with a continuous locking stitch, perineal muscle and skin sutured using the interrupted technique with polyglycolic acid (Dexon) suture material gauge 0. Needle size not specified. Group 2 (N = 267), vaginal trauma sutured with a continuous locking stitch, perineal muscle closed with a continuous non‐locking (running) stitch and perineal skin closed using an intracutaneous (subcuticular) technique with polyglycolic acid (Dexon) suture material gauge 0. Needle size not specified. | |
| Outcomes | Included in analysis:
|
|
| Notes | Method of repair: method described. Training period: introductory period of several months to make sure all members of staff were familiar with the new suturing technique used in group 2. Does not state if trial had Research Ethics Committee approval. Response rate at 3 months: group 1 = 95%; group 2 = 99% (of those who responded at 5 days ‐ numbers randomised per arm not given). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomised immediately after delivery. Method not described. |
| Allocation concealment (selection bias) | Low risk | "Closed envelopes containing the number of the method to be used for the repair". |
| Blinding (performance bias and detection bias) Clinical staff | High risk | Not blinded owing to obvious differences in suturing techniques. |
| Blinding (performance bias and detection bias) Women | High risk | Not stated but women may have been aware of suturing technique. |
| Blinding (performance bias and detection bias) Outcome assessors | Unclear risk | Differences in suturing techniques apparent. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Analysis for only those participants still in the hospital at 5th day (not 'intention to treat' ‐ missing data possibly outcome dependent). Of 900 women randomised, 98 were not followed up at day 5. 781 women responded to the questionnaire at 3 months. |
| Selective reporting (reporting bias) | Unclear risk | Not apparent. |
| Other bias | Unclear risk | No baseline imbalance apparent. |
Kettle 2002.
| Methods | RCT. Factorial ‐ 2 x 2 design. | |
| Participants | Setting: UK district general hospital. 1542 women needing perineal repair following delivery (second‐degree tears and episiotomies included). Method of delivery: spontaneous vaginal deliveries. Parity: primiparous and multiparous. Mean age: continuous (group A) 27.2 years; interrupted (group B) 27.2 years. Operators: midwives (N = 150), 29 women sutured by doctor. |
|
| Interventions | Method of repair: described as below. Women divided into 2 groups. Group A (N = 771) vaginal trauma, perineal muscle and skin repaired with a continuous non‐locking suture technique. 50% were repaired with undyed Vicryl Rapide 2/0 on a 35‐mm tapercut needle and 50% were repaired with undyed standard Vicryl on a 35‐mm tapercut needle. Group B (N = 771) vaginal trauma repaired with a locking continuous stitch; perineal muscle and skin sutured using the interrupted method. 50% were repaired with undyed Vicryl Rapide 2/0 on a 35‐mm tapercut needle and 50% were repaired with undyed standard Vicryl on a 35‐mm tapercut needle. | |
| Outcomes | Included in analysis:
|
|
| Notes | Method of repair: described. Training period: described Concealed interim analysis after 400 women entered the trial. Ethics Committee Approval. 1 envelope unaccounted for. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Allocated randomly by remote clinical trials unit. Random permuted block design. |
| Allocation concealment (selection bias) | Low risk | Concealed treatment allocation ‐ serially numbered, sealed opaque envelopes, (envelopes contained 2 packets of masked suture material and instructions for method of repair on different coloured cards). |
| Blinding (performance bias and detection bias) Clinical staff | High risk | Differences in suture techniques. |
| Blinding (performance bias and detection bias) Women | High risk | Women may have been aware of suturing technique. |
| Blinding (performance bias and detection bias) Outcome assessors | High risk | Fully blind assessment was not possible owing to obvious differences in suture techniques. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 1542 women randomised and primary analysis was by ITT. High response rate at day 10 and at 3 and 12 months' follow‐up (96.7% response rate at 3 months and 90% at 12 months). |
| Selective reporting (reporting bias) | Unclear risk | Not apparent. |
| Other bias | Unclear risk | No baseline imbalance apparent. There were some protocol deviations (less experienced staff were more likely to use interrupted sutures). |
Kindberg 2008.
| Methods | RCT (individual randomisation), 2‐arm trial. | |
| Participants | Setting: Arrhus hospital, Denmark. Recruitment 2004 to 2005. 400 healthy low‐risk women > 36 weeks' gestation, requiring perineal repair following spontaneous or instrumental (silastic cup ventouse) vaginal delivery with second‐degree laceration or episiotomy. Exclusions: unable to speak English or Danish, metal cup ventouse or forceps delivery, third‐degree tears, PPH, previous perineal surgery, diabetes or severe mental illness. Parity: primiparous women only. Mean age: continuous 28.2 years; interrupted 28.2 years. Operators: midwives trained in suturing techniques. |
|
| Interventions | Method of repair: described below. Both groups were sutured using rapidly absorbing polyglactin 910 (Vicryl Rapide) gauge 2/0, 90‐cm long on 1/2c, 36‐mm needle. (There was a change in the protocol to standard polyglactin 910 using the same gauge and needle, this was after approximately half of the sample had been recruited). Group 1: (continuous) loose, continuous non‐locking suture to close vaginal mucosa and muscular layer of perineum. The perineal skin was approximated with the same continuous suture in the subcutaneous tissue, a few millimetres under the perineal skin, finishing with a terminal knot in front of the hymenal ring. Group 2: (inverted interrupted) loose continuous non‐locking suture to the vaginal mucosa, 2 to 4 inverted interrupted stitches to the muscular layer of the perineum. Perineal skin approximated with inverted, interrupted sutured to the subcutaneous tissue a few millimetres under the skin edges (not transcutaneously). |
|
| Outcomes | Included in analysis:
|
|
| Notes | Change in suture material part way through the trial; authors stated that this did not affect the results when a logistic regression analysis was carried out. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐assisted voice response system, using stratified block randomisation (variable block size). Stratification by episiotomy/laceration. |
| Allocation concealment (selection bias) | Low risk | Remote telephone randomisation. |
| Blinding (performance bias and detection bias) Clinical staff | Unclear risk | Different techniques; while the trial authors claim that the 2 techniques appeared similar this may not have been convincing in practice. |
| Blinding (performance bias and detection bias) Women | Unclear risk | Women were not told about the method of repair. |
| Blinding (performance bias and detection bias) Outcome assessors | Unclear risk | Research midwife carrying out assessments described as blind to the 2 techniques. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 400 women randomised, 395 followed up. "All statistical analyses were undertaken on an intention‐to‐treat basis". |
| Other bias | Unclear risk | Considerable amount of non‐compliance (23% in the continuous group and 20% in the interrupted group were not treated according to randomisation group although ITT analyses were carried out). |
Kokanali 2011.
| Methods | RCT factorial design, 4‐arm trial. | |
| Participants | Setting: Dr Zekai Tahir Burak Women's Health Education and Research Hospital, Ankara, Turkey. Study period: March to August 2009. Inclusion criteria: women with live, singleton birth at 37 to 42 weeks' gestation; spontaneous vaginal delivery with right mediolateral episiotomy. Exclusion criteria: assisted vaginal delivery, perineal‐cervical tears, episiotomy involving the anal sphincter or rectum, viable baby with congenital abnormalities and extensive varicose veins of external genitalia. |
|
| Interventions | Experimental intervention (2 groups). Group 1: continuous technique with monofilament suture material (40 women). Group 2: continuous technique with multi‐filament suture material (40 women). Continuous technique: "Vaginal wall sutured with a continuous locking stitch. The same suture is continued in the muscles which are sutured continuously reaching the end of the incision. The same stitch is then carried in the skin and the perineal skin is approximated with the same continuous suture in the subcutaneous tissue a few millimetres under the perineal skin edges finishing with a terminal knot in the vaginal mucosa in front of the hymeneal ring". Control/comparison intervention (2 groups). Group 1: interrupted technique with monofilament suture material (40 women). Group 2: interrupted technique with multifilament suture material (40 women). Interrupted technique: "three‐layer technique, in which the vaginal mucosa was sutured with a continuous locking stitch. Two to four interrupted stitches were applied to the muscular layers and skin separately". Suture material (experimental and control groups): monofilament suture was polyglycolide‐co‐caprolactone material – gauge 0, 75‐cm long on a 1/2c 40‐mm needle. The multi‐filament suture was polyglactin 910‐Rapide material, gauge 0, 90‐cm long on a 1/2c 40‐mm needle. |
|
| Outcomes | Included in analysis:
Complications (wound infection, haematoma, healing, removal of suture material) up to 6 weeks. |
|
| Notes | The 4 study groups have been combined to form 2 groups so that we could carry out pair‐wise comparisons by suture technique (continuous versus interrupted). For dichotomous outcomes event rates and totals were added and for continuous outcomes means and standard deviations were combined using the methods set out in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | It was stated that women were allocated "using a computer for random selection" but the methods were not clear; "the treatment allocations were written on papers (40 of each) and placed in numbered, sealed, opaque envelopes" that were kept on the delivery ward concealing the assignment of treatment. |
| Allocation concealment (selection bias) | Unclear risk | It was stated that women were allocated "using a computer for random selection" but the methods were not clear; "the treatment allocations were written on papers (40 of each) and placed in numbered, sealed, opaque envelopes" that were kept on the delivery ward concealing the assignment of treatment. |
| Blinding (performance bias and detection bias) Clinical staff | Unclear risk | It was not clear whether or not women were told about which group they were allocated to. |
| Blinding (performance bias and detection bias) Women | High risk | All repairs were carried out by the same operator (unable to blind operator to technique of repair or materials used). |
| Blinding (performance bias and detection bias) Outcome assessors | Low risk | It was stated that outcomes were assessed by a blinded investigator. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 160 women were randomised and it was stated that no women were lost to follow‐up. It was not clear whether there were any protocol violations. |
| Selective reporting (reporting bias) | Unclear risk | Assessed from published study report. |
| Other bias | Unclear risk | Methods section was not clear regarding the method of randomisation. Unclear if all eligible women were approached as the repairs were carried out by the same operator (unable to be available 24 hours a day). |
Mahomed 1989.
| Methods | RCT. Modified factorial ‐ 2 x 3 x 2 design. | |
| Participants | Setting: Southmead Hospital, Bristol. 1057 women needing perineal repair following delivery (all tears and episiotomies included). This was a subgroup of the main trial. Method of delivery: spontaneous or instrumental vaginal deliveries. Parity: primigravidae and multiparae. Mean age: group 1 = 26.0 years; group 2 = 25.9 years. Operators: midwives, senior house officers, registrars, consultants, medical students. |
|
| Interventions | Method of repair: described as below. Women divided into 2 groups. Group 1 (N = 524) vaginal trauma repaired with a continuous stitch, perineal muscle and skin sutured using the interrupted technique. 50% were repaired with Dexon (plus) 2/0 on a multipurpose needle and 50% were repaired with chromic catgut on a 35‐mm tapercut needle. Group 2 (N = 533) vaginal trauma repaired with a continuous stitch, perineal muscle apposed with interrupted stitches and skin sutured using the continuous subcuticular technique. 50% were repaired with Dexon (plus) 2/0 on a multipurpose needle and 50% were repaired with chromic catgut on a 35‐mm tapercut needle. | |
| Outcomes | Included in analysis:
|
|
| Notes | Method of repair: method described. Subcuticular technique was unpopular with some operators. Training period: not described. No interim analysis. Ethics Committee Approval. Pre‐set trial size had 80% chance of detecting significant clinical differences. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not clear. |
| Allocation concealment (selection bias) | Low risk | Serially numbered, sealed opaque envelopes (envelopes contained suture material and instructions for method of repair). 22 envelopes were unaccounted for. |
| Blinding (performance bias and detection bias) Clinical staff | High risk | Differences in suture materials and techniques. |
| Blinding (performance bias and detection bias) Women | High risk | Women may have been aware of suturing technique. |
| Blinding (performance bias and detection bias) Outcome assessors | High risk | Fully blind assessment was not possible owing to obvious differences in suture materials and techniques. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 1574 women randomised. 97% response rate at day 2, 86% at day 10 and 87% at 3 months (1366 women). |
| Other bias | Unclear risk | There were some protocol deviations; of those allocated to continuous sutures 18% had interrupted, only 2% of those allocated to interrupted had continuous sutures. "some midwives preferred the interrupted technique... sometimes a midwife called a senior house officer if the allocation was to subcuticular suturing". |
Morano 2006.
| Methods | RCT. | |
| Participants | Setting: single centre (University Hospital, Italy). 214 women with a second‐degree tear or episiotomy. Method of delivery: spontaneous vaginal deliveries after 37 weeks' gestation. Parity: primiparous. Mean age: continuous (group A) = 28 years; interrupted (group B) = 27 years. Operators: young medical doctors with supervision provided by an experienced doctor. |
|
| Interventions | Method of repair: as described below. Women divided into 2 groups. Group A (N = 107), vaginal trauma, perineal muscles and skin repaired with loose, continuous non‐locking technique. Suture material rapidly absorbed polyglactin 910 (Vicryl Rapide) ‐ gauge 0 for vagina, perineal muscles and skin. Needle size not specified. Group B (N = 107) vaginal trauma repaired with a continuous non‐locking stitch; perineal muscle and skin sutured with interrupted method. Suture material: rapidly absorbed polyglactin 910 (Vicryl Rapide) ‐ gauge 0 for vagina, 1 for perineal muscles and 2/0 for skin. Needle size not specified. | |
| Outcomes | Included in analysis:
|
|
| Notes | Method of repair: method described. Training period: doctors had opportunity to practice 2 methods prior to commencement of study. Local research ethics committee approval obtained. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Computer‐generated list of random numbers. |
| Allocation concealment (selection bias) | Low risk | Sealed and consecutively numbered opaque envelopes (instructions for method of repair written on cards within envelopes). |
| Blinding (performance bias and detection bias) Clinical staff | High risk | Different suture techniques. |
| Blinding (performance bias and detection bias) Women | Unclear risk | Stated that trial was double blind, but women may have been aware of sutures. |
| Blinding (performance bias and detection bias) Outcome assessors | High risk | It would be difficult to blind the assessment of wound healing due to obvious differences in suturing techniques. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 214 women randomised, 19 lost to follow‐up by day 10. |
| Other bias | Unclear risk | No baseline imbalance apparent. |
Oboro 2003.
| Methods | RCT (individual randomisation) 2‐arm trial. | |
| Participants | Setting: 4 district government hospitals in Nigeria. Data collection 2000 to 2001. 1077 women requiring perineal repair after episiotomy or second‐degree tears (women with first‐ or third‐degree tears were excluded). Operators: over 75% repairs by midwives. Parity: both primi‐ and multiparous women included. Mean age: group 1 (2‐layer technique) = 26.3 years; group 2 (3‐layer technique) = 26.2 years. | |
| Interventions | Group 1: 2‐stage approach (not clear) but with the skin left unsutured using number 00 chromic catgut or polyglycolic sutures. Group 2: 3‐stage approach (not clear) with skin closure with interrupted or subcuticular continuous sutures (the subcuticular technique was encouraged) using number 00 chromic catgut or polyglycolic sutures. |
|
| Outcomes | Included in analysis:
|
|
| Notes | Suture techniques not clearly described. Not clear what materials were used and whether there were any differences in materials in different arms of the trial | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation when women completed the third stage of labour. Envelopes were prepared by "a statistician using computer generated block randomisation with varying block sizes". |
| Allocation concealment (selection bias) | Low risk | Sequentially numbered opaque sealed envelopes. |
| Blinding (performance bias and detection bias) Clinical staff | High risk | Different techniques. |
| Blinding (performance bias and detection bias) Women | High risk | Noy clear, although women would be aware from the appearance of the wound whether or not the skin had been sutured. |
| Blinding (performance bias and detection bias) Outcome assessors | High risk | Technique used would be apparent to assessors who carried out an examination of the perineum to assess gaping and bruising. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 1077 randomised, 823 completed both the 2 and 6 weeks questionnaires (approximately 20% attrition for longer‐term outcomes), loss to follow‐up balanced across groups. The level of missing data was not clear in the results tables. |
| Other bias | Unclear risk | No baseline imbalance apparent. |
Perveen 2009.
| Methods | RCT, factorial design (4 arms). Quasi‐randomised, alternating sequence. |
|
| Participants | Setting: Darul‐Sehat Hospital (private teaching tertiary care hospital) Karachi, Pakistan. Inclusion criteria: 200 primiparous and multiparous women who sustained an episiotomy or second‐degree tear after spontaneous vaginal delivery. Exclusion criteria: women under 18 years of age, requiring instrumental delivery, with severe anaemia (Hb < 6 g/dL), pre‐existing vaginal discharge or coagulation disorder. |
|
| Interventions | 4 arms (50 women in each group). Experimental intervention: (owing to resource constraints chromic catgut is still used in the study setting). Group 1: continuous repair with chromic catgut No 0 and 00 (chromic surgical gut – Ethicon). Group 2: continuous repair with polyglactin 910 No 0 and 00 (Vicryl‐Ethicon). Continuous technique: first suture inserted above apex of vaginal mucosa; mucosa and muscles sutured with continuous non‐locking stitches and subcuticular stitches used to close skin. Control/comparison intervention: Group 3: interrupted repair with chromic catgut No 0 and 00 (chromic surgical gut – Ethicon). Group 4: interrupted repair with polyglactin 910 No 0 and 00 (Vicryl‐Ethicon). Interrupted technique: first suture inserted above apex of vaginal mucosa; vaginal mucosa approximated with continuous sutures and muscles and skin with interrupted sutures. All repairs were carried out by 1 of 2 operators with similar experience. All women received diclofenac 50 mg every 8 hours for 5 days and cephalosporin 500 mg every 8 hours for 5 days as part of routine postnatal care. |
|
| Outcomes | Included in analysis:
|
|
| Notes | The 4 study groups have been combined to form 2 groups so that we could carry out pair‐wise comparisons by suture technique (continuous versus interrupted). For dichotomous outcomes event rates and totals were added and for continuous outcomes means and standard deviations were combined using the methods set out in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Women allocated in sequence (quasi‐randomised). |
| Allocation concealment (selection bias) | High risk | Women allocated in sequence (quasi‐randomised). |
| Blinding (performance bias and detection bias) Clinical staff | High risk | Women were informed about the suture material and repair. |
| Blinding (performance bias and detection bias) Women | High risk | Staff carrying out repair could not be blinded to technique. |
| Blinding (performance bias and detection bias) Outcome assessors | High risk | Staff including outcome assessors were not stated to be blinded to allocated intervention. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 200 women randomised. There was no information about loss to follow‐up and denominators were not provided in the results tables although it was stated that any women lost to follow‐up at 6 weeks were excluded from the analysis. |
| Selective reporting (reporting bias) | Unclear risk | Assessment from published study report. |
| Other bias | Unclear risk | Women were described as similar at baseline. |
Stark 2009.
| Methods | Described as randomised prospective pilot study. Method of randomisation not described (2 arms). |
|
| Participants | Setting: not described. Inclusion criteria: 89 primiparous women with an episiotomy (no details on type of episiotomy, e.g. midline or right or left medio lateral). Exclusion criteria: not described. |
|
| Interventions | Experimental intervention: (46 women) 2 layer closure. Described as modified closure (continuous suturing of the deep layers starting high as possible, 1 suture at the lower point and using the rest of the suture material to close the skin continuously all the way up back to the introitus where the final knot is done). It was also documented that "bleedings from the vaginal wall in women who were sutured with the 2 layers were handled with punctual stitching of the bleeding points". Suture material: polyglactin (Vicryl) (not clear if it was standard vicryl or vicryl rapide, suture material gauge and type of needle not described). Control/comparison intervention: (43 women) described as traditional 3‐layer closure (vaginal wall continuously, deep layer and skin with interrupted sutures). Suture material: polyglactin (Vicryl) (not clear if it was standard vicryl or vicryl rapide, suture material gauge and type of needle not described). |
|
| Outcomes | Included in analysis:
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) Clinical staff | Unclear risk | Not mentioned. |
| Blinding (performance bias and detection bias) Women | High risk | The person carrying out the repair would not be blinded. |
| Blinding (performance bias and detection bias) Outcome assessors | Unclear risk | Not mentioned. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 89 women randomised, 54 available for follow‐up at 6 to 8 weeks. |
| Selective reporting (reporting bias) | Unclear risk | Assessment from published study report. Inconsistencies in data tables. |
| Other bias | Unclear risk | Very little information on methods. Not clear if there was any baseline imbalance between groups (group characteristics not described). |
Valenzuela 2009.
| Methods | RCT. Individual randomisation. | |
| Participants | Setting: The Hospital Universitario Principe de Asturias (state hospital), Madrid. Recruitment period: September 2005 to July 2007. Ethics committee approval obtained. 445 women with an episiotomy or second‐degree tear. Method of delivery: ? spontaneous vaginal birth. Parity: ? primigravidae and multigravidae. Mean age: group 1 = 30.2 years; group 2 = 30.1 years. Operator: ? 4 midwives with more than 5 years' experience of attending deliveries and trained in both suturing techniques. Inclusion criteria: vaginal childbirth; viable foetus at least 37 weeks' gestation; delivered by 1 of the 4 matrons participating in the research; episiotomy or second‐degree tear affecting the skin and muscle. Exclusion criteria: instrumental delivery; episiotomy or perineal tear involving the anal sphincter or rectum; baby born with serious congenital malformations. |
|
| Interventions | Method of repair: described as below.
Women divided into 2 groups. Group 1 (N = 222) continuous non‐locking sutures in the vagina, perineum and subcutaneous tissue using Polyglactin 910 (Vicryl Rapide) on a 36‐mm needle, calibre/gauge 0. Group 2 (N = 223) vaginal trauma repaired with a continuous locking suture; interrupted sutures in the perineal muscle and interrupted transcutaneous sutures to close the skin using Polyglactin 910 (Vicryl Rapide) on a 36‐mm needle, calibre/gauge 0. |
|
| Outcomes | Included in analysis:
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer generated. |
| Allocation concealment (selection bias) | Low risk | Numbered opaque envelopes. |
| Blinding (performance bias and detection bias) Clinical staff | High risk | Different techniques used. |
| Blinding (performance bias and detection bias) Women | High risk | |
| Blinding (performance bias and detection bias) Outcome assessors | Low risk | "The midwife who conducted the questioning did not know the technique that had been used and was also blinded to other patient data". |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 445 women randomised and primary analysis was by ITT. High response rate at 2 and 10 days and at 3 months (3.6% in the continuous group and 6.7% in the interrupted group were lost to follow‐up at 3 months' postpartum). |
| Other bias | Unclear risk | All women received intervention as allocated. No baseline imbalance apparent. |
Zafar 2008.
| Methods | RCT, 2‐arm trial (individual randomisation). | |
| Participants | Setting: hospital in Islamabad, Pakistan (the hospital was described as having a high episiotomy rate). Data collection 2002 to 2006. 150 women requiring perineal repair following a mediolateral episiotomy after a spontaneous vaginal delivery. Women who had assisted deliveries or perineal tears were excluded. Parity: both primi‐ and multiparous women included. Mean age: group 1 = 27.2 years; group 2 = 27.2 years. All repairs were carried out by the same surgeon. |
|
| Interventions | Group 1: continuous (all layers and skin) with single knot at the apex of the vaginal mucosa. Continuous running stitch to vaginal wall, and muscles sutured in 2 layers, subcuticular sutures to skin, the repair is finished with the needle passing through the muscles lateral to the episiotomy and 4 to 5 cm of suture material is left to hang without a knot. Group 2: 3‐layer technique with continuous stitch to vaginal mucosa, interrupted sutures in 2 layers and continuous (subcuticular) sutures to the skin. Both groups: the repairs were mainly carried out with polyglactin 910 2/0 although 16 had chromic catgut 2/0 sutures (9 versus 7 cases in the 2 groups). |
|
| Outcomes | Included in analysis:
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated numbers. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) Clinical staff | High risk | Same operator for both study groups. |
| Blinding (performance bias and detection bias) Women | Unclear risk | Not discussed. |
| Blinding (performance bias and detection bias) Outcome assessors | High risk | Outcome assessors would be aware of the type of repair. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 150 women were randomised (it was not clear how many in each group). Full data for only 1 outcome (time taken to carry out the repair) with 29% attrition by day 7 (110/150 available at follow‐up). |
| Selective reporting (reporting bias) | Unclear risk | Not apparent. |
| Other bias | Unclear risk | High attrition and not clear how many randomised to each group. |
ITT: intention to treat PPH: postpartum haemorrhage RCT: randomised controlled trial VAS: visual analogue scale
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Bendsen 1980 | This study was excluded from the meta‐analysis owing to non‐absorbable and absorbable material being compared that may have had a confounding effect on the results. |
| Buchan 1980 | This study was excluded from the meta‐analysis owing to non‐absorbable and absorbable material being compared that may have had a confounding effect on the results. |
| Doyle 1993 | This study was excluded from the meta‐analysis owing to non‐absorbable and absorbable material being compared that may have had a confounding effect on the results. |
| Hansen 1975 | This study was excluded from the meta‐analysis owing to non‐absorbable and absorbable material being compared that may have had a confounding effect on the results. |
| Roberts 1993 | This study was excluded from the meta‐analysis owing to non‐absorbable and absorbable material being compared that may have had a confounding effect on the results. |
Characteristics of studies awaiting assessment [ordered by study ID]
Graczyk 1998.
| Methods | This paper is in Polish. We are awaiting a translation before we are able to assess whether the study is eligible for inclusion. It is not clear that this was a randomised trial. |
| Participants | 117 women after episiotomy (44 lost to follow‐up). |
| Interventions | Interrupted versus subcuticular suture. |
| Outcomes | Wound healing and pain. |
| Notes |
Uslu 1992.
| Methods | This paper is very similar to another study already included in the review (Isager‐Sally 1986). The study is awaiting assessment pending further investigation. |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes |
Differences between protocol and review
The methods section of the review has been updated. We have changed the title ‐ see Kettle 2007 for the title of the previous version of this review.
Contributions of authors
This update was based on the previous Cochrane review 'Continuous versus interrupted sutures for perineal repair' by Christine Kettle (CK) and Richard B Johanson (Kettle 1998).
CK co‐ordinated the update. All three review authors critically appraised all papers for quality and eligibility independently. CK and Therese Dowswell (TD) independently extracted the data and TD entered them onto the Review Manager software. CK checked all entered data for accuracy. CK and TD drafted the updated review and Khaled Ismail commented on drafts and checked the final document for accuracy, including data interpretation prior to submission.
Sources of support
Internal sources
The University of Liverpool, UK.
External sources
-
National Institute for Health Research (NIHR), UK.
TD is supported by the NIHR NHS Cochrane Collaboration Programme grant scheme award for NHS‐prioritised centrally‐managed, pregnancy and childbirth systematic reviews: CPGS02.
Declarations of interest
Christine Kettle (CK) was the recipient of a fellowship from the Iolanthe Midwifery Research Trust 1996, which provided funding to enable her to carry out a randomised controlled trial of perineal repair following childbirth (Kettle 2002). The Iolanthe Midwifery Research Trust and Ethicon Ltd, UK (manufacturers of suture material) provided funding for employment of a part‐time data management clerk for that trial.
CK and Khaled Ismail run perineal repair workshops both nationally and internationally and have developed an episiotomy and second‐degree tear training model with Limbs & Things, UK.
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
Almeida 2008 {published data only}
- Almeida SF, Riesco ML. Randomized controlled clinical trial on two perineal trauma suture techniques in normal delivery. Revista Latino‐Americana de Enfermagem 2008;16(2):272‐9. [DOI] [PubMed] [Google Scholar]
Banninger 1978 {published data only}
- Banninger U, Buhrig H, Schreiner WE. A comparison between chromic catgut and polyglycolic acid sutures in episiotomy repair. Geburtshilfe und Frauenheilkunde 1978;38:30‐3. [PubMed] [Google Scholar]
Croce 1997 {published data only}
- Croce P, Signorelli P, Dede A, Galli D. Selective episiotomy. Comparison of two suture techniques. Minerva Ginecologica 1997;49:449‐53. [PubMed] [Google Scholar]
Detlefsen 1980 {published data only}
- Detlefsen GU, Vinther S, Larsen P, Schroeder E. Intradermal suturing of episiotomy wounds compared with interrupted sutures. Ugeskrift for Laeger 1980;142:3117‐20. [PubMed] [Google Scholar]
Gordon 1998 {published data only}
- D'Souza D. The Ipswich Childbirth Study: 1 A randomised evaluation of two stage postpartum perineal repair leaving the skin unsutured [letter; comment]. British Journal of Obstetrics and Gynaecology 1999;106(1):89‐90. [DOI] [PubMed] [Google Scholar]
- Gordon B, Mackrodt C, Fern E, Truesdale A, Ayers S, Grant A. The Ipswich Childbirth Study: 1. A randomised evaluation of two stage postpartum perineal repair leaving the skin unsutured. British Journal of Obstetrics and Gynaecology 1998;105:435‐40. [DOI] [PubMed] [Google Scholar]
- Grant A, Gordon B, Mackrodt C, Fern E, Truesdale A, Ayers S. The Ipswich Childbirth Study: one year follow up of alternative methods used in perineal repair. BJOG: an International Journal of Obstetrics and Gynaecology 2001;108(1):34‐40. [DOI] [PubMed] [Google Scholar]
- Mackrodt C, Fern E, Gordon B. Ipswich Childbirth Study ‐ perineal suturing study. Proceedings of Research in Midwifery Conference; 1993 Sept 14; Birmingham, UK. 1993.
Isager‐Sally 1986 {published data only}
- Isager‐Sally I, Legarth J, Jacobsen B, Bostofte E. Episiotomy repair ‐ immediate and long‐term sequelae. A prospective randomized study of three different methods of repair. British Journal of Obstetrics and Gynaecology 1986;93:420‐5. [PubMed] [Google Scholar]
Kettle 2002 {published data only}
- Kettle C, Hills R, Jones P, Darby L, Gray R, Johanson R. Continuous versus interrupted perineal repair with standard or rapidly absorbed sutures after spontaneous vaginal birth: a randomised controlled trial. Lancet 2002;359:2217‐23. [DOI] [PubMed] [Google Scholar]
Kindberg 2008 {published data only}
- Kindberg S, Stehouwer M, Hvidman L, Henriksen TB. Postpartum perineal repair performed by midwives: a randomised trial comparing two suture techniques leaving the skin unsutured. BJOG: an International Journal of Obstetrics and Gynaecology 2008;115(4):472‐9. [DOI] [PubMed] [Google Scholar]
Kokanali 2011 {published data only}
- Kokanali D, Ugur M, Kuntay M, Karayalcin R, Tonguc E. Continuous versus interrupted episiotomy repair with monofilament or multifilament absorbed suture materials: a randomised controlled trial. Archives of Gynecology and Obstetrics 2011;284(2):275‐80. [DOI] [PubMed] [Google Scholar]
Mahomed 1989 {published data only}
- Mahomed K, Grant AM, Ashurst H, James D. The Southmead perineal suture study. A randomized comparison of suture materials and suturing techniques for repair of perineal trauma. British Journal of Obstetrics and Gynaecology 1989;96:1272‐80. [DOI] [PubMed] [Google Scholar]
Morano 2006 {published data only}
- Morano S, Mistrangelo E, Pastorino D, Lijoi D, Costantini S, Ragni N. A randomized comparison of suturing techniques for episiotomy and laceration repair after spontaneous vaginal birth. Journal of Minimally Invasive Gynecology 2006;13(5):457‐62. [DOI] [PubMed] [Google Scholar]
Oboro 2003 {published data only}
- Oboro VO, Tabowei TO, Bosah JO. A multicentre evaluation of the two‐layered repair of postpartum perineal trauma. Journal of Obstetrics and Gynaecology 2003;23(1):5‐8. [DOI] [PubMed] [Google Scholar]
Perveen 2009 {published data only}
- Perveen F, Shabbir T. Perineal repair: comparison of suture materials and suturing techniques. Journal of Surgery Pakistan 2009;14(1):23‐8. [Google Scholar]
Stark 2009 {published data only}
- Stark M. Episiotomy ‐ the destructive tradition. Gineco.ro 2009;5(3):142‐5. [Google Scholar]
Valenzuela 2009 {published data only}
- Valenzuela P, Saiz Puente MS, Valero JL, Azorin R, Ortega R, Guijarro R. Continuous versus interrupted sutures for repair of episiotomy or second‐degree perineal tears: a randomised controlled trial. BJOG: an International Journal of Obstetrics and Gynaecology 2009;116(3):436‐41. [DOI] [PubMed] [Google Scholar]
Zafar 2008 {published data only}
- Zafar S. Comparison of a single‐knot versus three layered technique of perineal repair after vaginal delivery in women requiring episiotomy: a double blind randomized controlled trial. Journal of the Turkish‐German Gynecology Association 2008;9(3):129‐33. [Google Scholar]
References to studies excluded from this review
Bendsen 1980 {published data only}
- Bendsen J, Madsen H. Intracutaneous suturing of episiotomy wounds. Comparison between polyglycolic acid (Dexon) intracutaneously and silk sutures in the skin. Ugeskrift for Laeger 1980;142:3120‐2. [PubMed] [Google Scholar]
Buchan 1980 {published data only}
- Buchan PC, Nicholls JAJ. Pain after episiotomy ‐ a comparison of two methods of repair. Journal of the Royal College of General Practitioners 1980;30:297‐300. [PMC free article] [PubMed] [Google Scholar]
Doyle 1993 {published data only}
- Doyle PM, Johanson R, Geetha T, Wilkinson P. A prospective randomised controlled trial of perineal repair after childbirth, comparing interrupted chromic catgut to subcuticular prolene for skin closure. British Journal of Obstetrics and Gynaecology 1993;100:93‐4. [DOI] [PubMed] [Google Scholar]
Hansen 1975 {published data only}
- Hansen MK, Selnes A, Simonsen E, Sorensen KM, Pedersen GT. Polyglycolic acid (Dexon) used as suture material for the repair of episiotomies. Ugeskrift for Laeger 1975;137:617‐20. [PubMed] [Google Scholar]
Roberts 1993 {published data only}
- Roberts M, Richardson L, Johnson D, Coleman S, Michael EM. A randomised trial of perineal repair following childbirth: a comparison of subcuticular polyglactin 910 (Vicryl) and interrupted black silk for perineal skin closure. Online Journal of Current Clinical Trials 1993;2:Doc 90. [Google Scholar]
References to studies awaiting assessment
Graczyk 1998 {published data only}
- Graczyk S, Limanowski M, Wyduba M. Interrupted vs. subcuticular technique of episiotomy wound repair in clinical and cosmetic aspects. Ginekologia Polska 1998;69(1):6‐11. [PubMed] [Google Scholar]
Uslu 1992 {published data only}
- Uslu MA, Ozekici U, Simsek M, Berkman S. A prospective randomized study of three different methods of episiotomy repair. Istanbul Tip Fakultesi Mecumasi 1992;55:237‐42. [Google Scholar]
Additional references
Fernando 2006
- Fernando R, Sultan AH, Kettle C, Thakar R, Radley S. Methods of repair for obstetric anal sphincter injury. Cochrane Database of Systematic Reviews 2006, Issue 3. [DOI: 10.1002/14651858.CD002866.pub2] [DOI] [PubMed] [Google Scholar]
Glazener 1995
- Glazener CMA, Abdalla M, Stroud P, Naji S, Templeton A, Russell IT. Postnatal maternal morbidity: extent, causes, prevention and treatment. British Journal of Obstetrics and Gynaecology 1995;102:286‐7. [DOI] [PubMed] [Google Scholar]
Greenland 1987
- Greenland S. Quantitative methods in the review of epidemiologic literature. Epidemiologic Reviews 1987;9:1‐30. [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Kettle 2010
- Kettle C, Dowswell T, Ismail KMK. Absorbable suture materials for primary repair of episiotomy and second degree tears. Cochrane Database of Systematic Reviews 2010, Issue 6. [DOI: 10.1002/14651858.CD000006.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Klein 1994
- Klein MC, Gauthier RJ, Robbins JM, Kaczorowski J, Jorgensen SH, Franco ED, et al. Relationship of episiotomy to perineal trauma and morbidity, sexual dysfunction, and pelvic floor relaxation. American Journal of Obstetrics and Gynecology 1994;171:591‐8. [DOI] [PubMed] [Google Scholar]
McCandlish 1998
- McCandlish R, Bowler U, Asten H, Berridge G, Winter C, Sames L, et al. A randomised controlled trial of care of the perineum during second stage of normal labour. British Journal of Obstetrics and Gynaecology 1998;105(12):1262‐72. [DOI] [PubMed] [Google Scholar]
RevMan 2011 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 5.1. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2011.
Sleep 1984
- Sleep J, Grant A, Garcia J, Elbourne D, Spencer J, Chalmers I. West Berkshire perineal management trial. British Medical Journal 1984;289:587‐90. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sleep 1991
- Sleep J. Perineal care: a series of five randomised controlled trials. In: Robinson S, Thompson A editor(s). Midwives, Research and Childbirth. Vol. 2, London: Chapman and Hall, 1991. [Google Scholar]
References to other published versions of this review
Johanson 1995
- Johanson RB. Continuous vs interrupted sutures for perineal repair [revised 10th March 1994]. In: Enkin MW, Keirse MJNC, Renfrew MJ, Neilson JP, Crowther C (eds.) Pregnancy and Childbirth Module. In: The Cochrane Pregnancy and Childbirth Database [database on disk and CDROM]. The Cochrane Collaboration; Issue 2, Oxford: Update Software. 1995.
Kettle 1998
- Kettle C, Johanson RB. Continuous versus interrupted sutures for perineal repair. Cochrane Database of Systematic Reviews 1998, Issue 1. [DOI: 10.1002/14651858.CD000947] [DOI] [PubMed] [Google Scholar]
Kettle 2007
- Kettle C, Hills RK, Ismail KMK. Continuous versus interrupted sutures for repair of episiotomy or second degree tears. Cochrane Database of Systematic Reviews 2007, Issue 4. [DOI: 10.1002/14651858.CD000947.pub2] [DOI] [PubMed] [Google Scholar]


