Abstract
Objective:
To address calls for a resilience-informed approach to understanding the etiology and prevention of childhood obesity, the current study aims to investigate the independent and interactive associations between household chaos, maternal emotional responsiveness, and eating behavior in early childhood.
Method:
A sample of (n = 108) families of 18-24 month-olds completed self-report surveys and consented to home visits as part of the larger STRONG Kids 2 Study (N = 468). Videotapes of family mealtimes were collected during home visits, and coded for observed maternal emotional responsiveness. Mothers completed questionnaires assessing maternal emotional responsiveness, household chaos, and child eating behaviors. Moderation analyses assessed independent and interactive effects of chaos and emotional responsiveness on child appetite self-regulation.
Results:
In moderation analyses controlling for demographic covariates, higher levels of chaos were associated with more emotional overeating and with more food responsiveness, but only among children of mothers observed engaging in low levels of emotional responsiveness at mealtimes. There was no association between chaos and eating behavior among children of mothers observed engaging in high levels of emotional responsiveness at mealtimes. There was also no independent or interactive association between chaos and child eating behaviors characterized by food avoidance.
Conclusion:
Preliminary evidence suggests that maternal emotional responsiveness at mealtimes may attenuate the deleterious effects of chaos on child overeating and food responsiveness. Future research should prioritize using longitudinal designs, developing of observational assessments of early childhood eating behaviors, and understanding these processes among families exposed to greater socioeconomic adversity.
Introduction
Childhood overweight and obesity affect over 40% of preschoolers in the United States and are associated with increased risk for obesity in adolescence and adulthood, as well as the chronic diseases comorbid with higher weight in later life.1,2 Approach-related eating behaviors such as overeating, enjoyment of food, and food responsiveness (which involve a child being more oriented toward eating too much food) have been linked to higher weight outcomes.3,4 In contrast, avoidance-related eating behaviors such as satiety responsiveness, slowness in eating, and food fussiness (which involve a child being more oriented toward eating less, not eating, or avoiding eating) are associated with lower weight outcomes.4 Because of these patterns and evidence linking general (non-appetitive) self-regulation to obesity risk, these behaviors can be conceptualized as part of appetite self-regulation, or the process by which children attend and respond to internal cues of hunger and satiety.5,6 Approach-related eating behaviors may prompt children to eat beyond their internal cues of satiety, whereas avoidance-related eating behaviors may prevent children from eating in response to their cues of hunger.
Interventions have attempted to modify these eating behaviors in order to prevent excessive early weight gain, with modest success.7 Parents control young children’s access to and socialization around food. Therefore, these interventions tend to focus on the family context and include parent education focused on feeding, access and availability of healthy or unhealthy foods, and modeling or actively teaching healthy dietary and physical activity behaviors.8 However, effects vary within and across interventions, so it is critical to identify family factors that may account for these differential outcomes.
One such factor may include household chaos. Studies have linked household chaos—operationalized as high levels of confusion, noise, disorganization, and lack of routine—to general self-regulation in early childhood via direct and indirect pathways.9-12 Chaos may make it more difficult for children to learn effective coping mechanisms linked to self-regulation.11 For instance, household chaos has been positively linked with kindergarteners’ externalizing, and internalizing problems, and negatively with attentional control, as well as with less nurturing parenting.10 As a test of the hypothesis that chaos acts indirectly on children via parenting, a longitudinal study found that household chaos at 3-years-old was associated with children’s behavioral dysregulation at 5-years old, indirectly via reduced parent responsiveness and sensitivity.12 However, a cross-sectional study investigating associations between chaos and children’s problem behaviors (e.g., conduct problems, emotion dysregulation) found that effects were only significant for dyads with a highly negative parent-child relationship.9 Together, these studies demonstrate that both household chaos and parenting behaviors may be important to consider in relation to general child self-regulation, but that questions persist about the specific pathways and conditions of effect. Furthermore, findings about general self-regulation may not be generalizable to effects on eating behaviors or weight, but they inform potential hypotheses. To the best of our knowledge, only one study has investigated associations between chaos and child eating behavior, finding that higher levels of chaos were associated with greater dietary fat intake.13
Regarding specific parenting factors, investigators focused on improving child eating behaviors have been especially interested in parent emotional sensitivity. Parent emotional sensitivity—or responsiveness—is operationalized as the degree to which a parent responds to a child’s negative emotions in a warm, contingent, and developmentally appropriate manner.14 Low levels of maternal emotional sensitivity or responsiveness have been linked to poorer general child self-regulation, maternal use of fewer positive feeding practices in infancy, and higher weight outcomes among toddlers.15,16 Based in bio-behavioral theories of attachment and regulation, these studies suggest that maternal emotional responsiveness may promote children’s secure base behaviors by first serving as an external regulatory mechanism in infancy, and then by modeling and scaffolding to help the child develop a repertoire of healthy self-regulation strategies for later life.5,17 Studies linking attachment to eating behavior underscore the importance of parent-child relationships and emotional responsiveness for health promotion and obesity prevention across the life-course.18 However, few studies have attended to the broader family context in understanding how maternal emotional responsiveness or sensitivity may affect children’s eating behaviors.
Several gaps in the literature prevent researchers from applying these findings to child eating behaviors in efforts to understand potential strategies for childhood obesity prevention. First, as mentioned previously, although a few studies have found that household chaos may influence children’s general self-regulation as a function of parenting, no studies have yet investigated these links for children’s regulation-related eating behaviors. Second, despite calls for a resiliency-focused approach to child obesity,19 few studies have evaluated whether parenting practices like maternal sensitivity may be able to buffer children from the deleterious effects of household chaos on health outcomes. Third, current studies investigating associations between sensitivity and eating behaviors are limited in that maternal sensitivity has primarily been assessed using only self-reports, or observed during non-food related contexts.16 Thus, it is unclear whether sensitivity generally, or sensitivity in food-related contexts specifically, are differentially associated with eating in early childhood.
To address these gaps, the current study aims to investigate the independent and interactive associations between household chaos, maternal sensitivity, and child eating behaviors in a sample of 18–24-month-old children. Based on a theoretical framework we developed by integrating attachment and family systems theories to understand the etiology of early appetite self-regulation,20 we developed two hypotheses tested in the current study. Household chaos and maternal sensitivity—or a warm maternal response to a child’s secure base behavior—have been linked independently to children’s general (non-food related) self-regulation behavior and weight.15,16 However, no studies have examined relative contributions of these factors to children’s appetite self-regulation behaviors, neglecting to consider tenants of family systems theory suggesting that individual and dyadic factors (e.g. maternal sensitivity, child self-regulation, attachment) should be considered in the context of family-level factors.20 Therefore, our first hypothesis was that household chaos and maternal sensitivity would be independently associated with child eating behaviors (Online Supplementary Figure 1). Specifically, we expected that higher levels of household chaos and lower levels of maternal sensitivity would both be associated with more eating behaviors characterized by food approach (e.g., overeating, enjoyment of food, and food responsiveness). Second, as an answer to calls for a resilience-focused approach to childhood obesity prevention,19 we hypothesized that high levels of maternal sensitivity at mealtimes would provide a stronger buffer from the negative effects of household chaos on child eating behaviors, compared to maternal sensitivity generally (Online Supplementary Figure 1). We would expect that maternal sensitivity generally would have a weaker effect, as this construct is more distal to the food environment and eating behavior.
Method
Participants and Recruitment
Participants in the current study were from a subsample of families in the larger STRONG Kids 2 Study (SK2; N = 468).21 Mothers in SK2 were recruited during their third trimester of pregnancy from healthcare facilities (e.g., obstetrics and gynecology) within 50 miles of the study site in East Central Illinois, between 2014 and 2017. Participants were excluded if children were born premature, unable to feed normally, or low birthweight (< 2.5 kg). Families completed validated questionnaires at intake and when children were 3, 12, 18, and 24 months of age. The current study utilizes survey data from baseline (to assess self-reported demographics), 18-month (to assess maternal reported emotional responsiveness), and 24-month (to assess maternal reported household chaos and child eating behavior) surveys.
A subsample of families in SK2 were recruited for additional home visits using flyers and phone calls. Targeted families were those with children in SK2 who were 18–24-months-old. Of 198 eligible families, 110 agreed to participate between October 2015 and July 2017. One family’s observational data were lost due to technological error and one family’s surveys demonstrated substantial response bias (straight-lining) and so the final sample included 108 families with survey data at 18 and 24 months and observational data from a home visit.
Mothers in the sample were mostly married, White, middle income, well-educated, and employed. About 85% (n = 94) of mothers were married, 8.1% (n = 9) were single, 2.7% (n = 3) were co-habiting, and 0.9% (n = 1) were divorced. Most mothers were White (n = 89, 80.9%), 7.3% (n = 8) were Black, 6.4% (n = 7) were Asian, 2.7% (n = 3) were Hispanic/Latino, 0.9% (n = 1) were American Indian/Alaska Native, and 4.5% (n = 5) were Biracial. About 29% (n = 30) of mothers reported income less than $3,000/month, 45% (n = 47) reported $3,000 - $6,000/month, and 20.7% (n = 23) reported more than $6,000/month. Most mothers had post-graduate degrees (40.9%, n = 45), 36.4% (n = 40) were college graduates, and 21.3% (n = 22) had some college/technical school or less. Most mothers were employed (71.8%, n = 79), 18.2% were stay-at-home parents (n = 20), 5.5% (n = 6) were unemployed, and 0.9% (n = 1) were students. Mothers were, on average, 30.9 years old (SD = 4.47, Range = 19.1 – 45.2). Children were, on average, 20.97 months old (SD = 2.73, Range = 17.8 – 34.9). One child was 34.9 months old at the home visit due to reporting error during recruitment. All analyses were run including and excluding this child, and no statistical or substantive differences were identified. Therefore, this child was included in all analyses. All other children were between 17.8 and 28.6 months old. There were no statistically significant differences between the subsample and the larger sample on the following demographic variables: maternal race/ethnicity, marital status, employment, income, maternal education, or maternal age (all p’s < 0.10). The SK2 sample is generally representative of the East Central Illinois region on key demographic variables.
Home Visit Procedures
Home visits were scheduled on weekday evenings. Two trained observers arrived at the home and attained written and informed consent from mothers while building rapport. Once the family was ready to eat, video cameras were set up to face the target child during the meal, and observers waited outside the home. After the family let observers know when the meal finished, parents were debriefed and provided remuneration ($75.00), and children were given a toy. This project’s human subjects research protocols were reviewed and approved by the University of Illinois at Urbana-Champaign’s Institutional Review Board.
Measures
Exposure: Household chaos.
Household chaos was measured using the 15-item Confusion, Hubbub, and Order Scale (CHAOS) when children were 24 months old (Table 1).22 For each item (e.g., “It’s a real zoo in our home,”), mothers indicated how much the statement described their home from 1 (Very much like your own home) to 4 (Not at all like your own home). Scores across the 15 items were averaged; higher scores indicate more chaotic or disorganized home characteristics. Reliability was excellent (α = .84), and comparable to other studies among families with toddlers.22
Table 1.
Descriptive statistics for model variables and sociodemographic characteristics of analytical sample (n = 108).
| Mean | SD | Range | N | % | ||
|---|---|---|---|---|---|---|
| Household chaos (24m survey) | 1.83 | 0.43 | 1.1 – 2.9 | Maternal race/ethnicity | ||
| Observed maternal emotional responsiveness at meal (18-24m observation) | White | 81 | 75.0% | |||
| Sensitivity to child negative emotions ratio | 0.66 | 0.27 | 0.0 – 0.9 | Black | 5 | 4.6% |
| Structuring responses to child negative emotions ratio | 0.52 | 0.25 | 0.0 – 0.9 | Asian | 7 | 6.5% |
| Attending responses to child negative emotions ratio | 0.18 | 0.18 | 0.0 – 0.7 | Hispanic/Latino | 3 | 2.8% |
| Self-reported maternal emotional responses (CCNES, 18m survey) | Other | 6 | 5.6% | |||
| Expressive encouragement responses | 5.38 | 1.09 | 1.0 – 7.0 | Monthly household income | ||
| Emotion-focused responses | 5.66 | 0.83 | 2.9 – 7.0 | <$3000/month | 30 | 27.8% |
| Problem-focused responses | 5.82 | 0.76 | 3.2 – 7.0 | $3000-$6000/month | 31 | 28.7% |
| Child eating behavior (CEBQ, 24m survey) | >$6000/month | 39 | 36.1% | |||
| Food responsiveness (4 items)* | 2.41 | 0.54 | 1.2 – 3.6 | Maternal education | ||
| Emotional overeating (4 items)* | 1.59 | 0.41 | 1.0 – 2.5 | Some college or less | 21 | 19.4% |
| Enjoyment of food (4 items) * | 3.67 | 0.59 | 1.3 – 5.0 | College graduate | 40 | 37.0% |
| Satiety responsiveness (4 items) | 3.09 | 0.55 | 1.6 – 4.4 | Post-graduate degree | 45 | 41.7% |
| Slowness in eating (4 items) | 2.99 | 0.55 | 1.5 – 5.0 | Maternal employment | ||
| Emotional undereating (3 items) | 3.15 | 0.78 | 1.3 – 5.0 | Employed | 79 | 73.1% |
| Food fussiness (5 items) | 2.72 | 0.69 | 1.0 – 4.8 | Stay-at-home parent | 20 | 18.5% |
| Maternal age at birth (years) | 30.9 | 4.47 | 19.1 – 45.2 | Unemployed | 6 | 5.6% |
| Child age at home visit (months) ǂ | 20.97 | 2.73 | 17.8 – 34.9 | Student | 1 | 0.9% |
| Mealtime length (minutes) | 17.07 | 3.94 | 6.0 – 20.0 | Marital status | ||
| Married | 94 | 87.0% | ||||
| Single | 9 | 8.3% | ||||
| Cohabiting | 3 | 2.8% | ||||
| Divorced | 1 | 0.9% | ||||
| Not reported | 1 | 0.9% | ||||
Note. m = month; SD = standard deviation; CCNES = Coping with Children’s Negative Emotions Scale; CEBQ = Child Eating Behavior Questionnaire. Percentages for socio-demographics may not add to 100% because of participant non-response.
Higher scores for these scales indicate higher levels of approach-related eating behavior dysfunction. Higher scores for all other CEBQ scales indicate higher levels of avoidance-related eating behavior dysfunction.
One child was 34.9 months at the home visit due to reporting error during recruitment. All analyses were run including and excluding this child, identifying no statistical or substantive differences. All other children were between 17.8 and 28.6 months.
Outcome: Child eating behavior.
Seven subscales from the Children’s Eating Behavior Questionnaire was used to assess child eating behavior at 24 months old (CEBQ; Table 1). The CEBQ is a parent-report survey of 35 items that comprise 8 subscales, and has been used previously with parents of children under two years old.23,24 Only subscales focused on eating behavior—not drinking—were included (food responsiveness, emotional overeating, enjoyment of food, satiety responsiveness, slowness in eating, emotional undereating, and food fussiness; Table 1). Internal reliability was > 0.70 for all subscales except for the food responsiveness (α = 0.65), satiety responsiveness (α = 0.65), and slowness in eating (α = 0.64) subscales. Higher scores on food responsiveness (orientation toward food-seeking behavior and overeating), emotional overeating (eating when experiencing a negative emotion or boredom), and enjoyment of food (expressing positive affect or interest in regards to food and meals) indicated higher levels of approach-related eating behavior dysfunction. Higher scores on satiety responsiveness (orientation toward eating less when full or not being interested in food when not hungry), slowness in eating (eating slowly or taking a long time to finish a meal), emotional undereating (avoiding food when experiencing a negative emotion), and food fussiness (food refusal, picky eating, food neophobia) indicated higher levels of avoidance-related eating behavior dysfunction.
Moderator: Maternal emotional responsiveness/sensitivity.
Emotional responsiveness is operationalized as the degree to which parents attend and respond to children’s cues of distress,14 and was assessed observationally during family mealtimes when children were between 18 and 24 months, and using a self-report measure when children were about 18 months old. The current study focuses on emotional responsiveness and sensitivity (positive behavior), rather than emotional non-responsiveness or non-sensitivity (negative behavior), to test the hypothesis that positive emotional responses may ameliorate the effects of household chaos on child outcomes.
Observed emotional responsiveness.
Observed maternal emotional responsiveness during mealtimes was assessed using a hierarchical coding structure to account for the fact that the behavior is contingent on children’s expressions of negative emotions. Research assistants coded observed emotional responsiveness during family mealtimes in several steps. First, a graduate-level lead coder applied the coding scheme to videos collected from a previous study for training purposes. Second, the lead coder trained two undergraduates using Mangold’s INTERACT, a software that facilitates implementation of hierarchical observational coding systems.25 Coders attained acceptable inter-rater reliability (intra-class correlation coefficient [ICC] ≥ .70) between each pair on training videos from another study before coding videos from the current study. Each undergraduate coded half (n = 55) of the videos. Lead coders double-coded about 20% (n = 22) of the videos, overlapping equally with each undergraduate, who were blinded to which videos would be double-coded. Differences were resolved by consensus at weekly meetings, which also prevented rater drift. Inter-rater reliability was adequate across all observational coding schemes in the current study (all ICC’s ≥ .70).
Each coder watched each video twice: once to code child emotion and a second time to code maternal emotional responses. First, child emotions were coded as either positive or negative using the event-based D.O.T.S Coding System.26 Child negative emotions (M [SD] = 7.59 [5.17], Range = 0 – 19, ICC = .99) were indicated by behavioral, facial, or vocal expressions (e.g., thrashing, crying, pouting). Second, mothers’ responses to children’s negative emotions and the sensitivity of those responses were assessed using a coding scheme developed based on attachment theory’s conceptualization of sensitivity as a mechanism for bio-behavioral self-regulation development.15 For each child negative emotion event, coders indicated whether mothers utilized one of six responses (structuring/limit setting, distracting, positive emotions, negative emotions, attending, and no response/ignoring), and then determined whether the response was sensitive (warm, responsive, contingent) or non-sensitive to the child’s needs, developmental status, and the situation. Distracting (M[SD] = .11 [.34], Range = 0 – 2, ICC = .92) and positive emotional responses (M[SD] = .12 [.38], Range = 0 – 2, ICC = .92) had small range and low incidence, and there were no negative emotional responses, so were not included in analyses.
Structuring/limit setting responses involve providing information, problem solving, modifying the physical environment, or giving the child directives to ameliorate negative emotion (M [SD] = 4.35 [3.25], Range = 0 – 12, ICC = .98). A sensitive structuring/limit setting response example might involve the child being upset about not being able to play with a toy, and the parent telling them: “It will be there for you later, but right now we’re not going to play with that.” A non-sensitive response might involve the parent getting the toy, putting it on the table, and saying: “there, are you happy now?” Attending responses involve noticing or briefly glancing at the child after an instance of negative emotion, but not interfering (M [SD] = 1.63 [1.93], Range = 0 – 13, ICC = .87). A sensitive attending response might involve the parent hearing the child whimper or shriek, responding by looking up briefly to assess the situation, and saying nothing or making a brief kind statement (e.g., “oops, it’s ok!”). A non-sensitive attending response might involve the parent looking up, rolling their eyes, and either saying nothing or saying a brief insensitive statement (e.g., “oh, please.”). No response/ignoring responses were indicated when the mother was not in the room or otherwise unable to respond to the child (M [SD] = 1.24, [1.80], Range = 0 – 8, ICC = .96). Analyzing data using frequency scores may misrepresent emotional responsiveness for mothers of less expressive children. Therefore, we constructed ratio variables by dividing the frequency of each type of response (e.g., the number of structuring/limit setting responses) by the number of negative emotions that a child expressed in a given meal (Table 1). No response/Ignoring responses involved an absence of behavior, so coders did not apply a sensitive or non-sensitive code to these responses. Thus, when constructing the ratio variable for Sensitive responses, we divided the total number of sensitive responses across all types of responses (M [SD] = 5.53 [3.86], Range = 0 – 15, ICC = .98), by the number of negative emotion incidents that mothers gave an emotional response to (e.g., the sum of all responses, minus No response/ Ignoring responses). Descriptive statistics are reported in Table 1.
Self-reported emotional responsiveness.
Three subscales from the Coping with Children’s Negative Emotions Scale27 were used to assess mothers’ self-reported emotional responsiveness at 18 months (Table 1). For the CCNES, parents read 12 vignettes that described scenarios in which children tend to express negative emotion. For each vignette, parents responded to 6 items (72 items total); each item asked parents to rate how likely they are to respond to the scenario using a given response, on a Likert scale from 1 (Very Unlikely) to 7 (Very Likely). Each response corresponds to one of six emotional response subscales: problem-focused, emotion-focused, expressive encouragement, distress, minimizing, and punitive responses to children’s negative emotions. Responses to items corresponding to the subscales are averaged across the 12 vignettes to calculate subscale scores. The current study focuses on the role of positive and sensitive responses to children’s negative emotions, so the latter three subscales were excluded. Problem-focused responses involve helping the child think about solutions (α = .89). Emotion-focused responses involve comforting or soothing the child (α = .88). Expressive encouragement involves talking to children about negative emotions (α = .87).
Covariates.
Maternal report of income, marital status, age, race/ethnicity, employment, and education were evaluated as potential covariates using demographic self-report items (Table 1). Mealtime length (minutes) was indicated by calculating the duration of time from the start of the meal (defined as the point at which food was placed on the table or in front of the target child) to the end of the meal (20 minutes after the start of the meal, or as the point at which food was removed from the table or from the target child). Parents were not instructed to stop the meal; mealtime duration was calculated after data were collected and were in the process of being coded.
Analysis Plan
All analyses were conducted in Statistical Package for Social Sciences (SPSS) version 25.0.28 A forced-response format was not used, so some subscales had more missing data than others. Between 0 and 17.3% of data were missing, with greatest amount of data missing for measures of chaos at 24 months. We could not reject the null hypothesis of Little’s Missing Completely at Random test (MCAR; X2[df] = 4960.66 [56188], p = 1.00). Given that all variables were approximately normally distributed, likely missing in a random pattern, and had missingness < 20%, data were multiply imputed with a fully conditional Markov Chain Monte Carlo (MCMC) specification method. This method can only be used when data are not missing systematically, and is an iterative two-step numerical simulation method. In the first step, random samples of the missing data and random samples of parameters from the observed data are drawn. In the second step, a random sample of parameter estimates is drawn from the combination of random samples from step one. After the iterations, MCMC converged forming 10 imputed datasets, which were aggregated by generating mean scores across datasets. Demographic variables were not imputed and used only as imputation predictors. There were no differences in means, standard deviations, or ranges for raw and imputed datasets. Imputed descriptive statistics for the analytical sample (n = 108) are presented in Table 1.
Descriptive summary statistics were calculated for all model variables. Histograms indicated that household chaos and child eating behavior variables from the CEBQ were all normally distributed, but that emotional responsiveness variables were positively skewed. Therefore, non-parametric pairwise Spearman’s correlations were calculated to assess bivariate associations among model variables and continuous demographic characteristics. Tests of mean differences were conducted to assess associations between the outcome variables (CEBQ subscales) and categorical (e.g., child gender, maternal education, maternal race/ethnicity, household income, maternal employment status, and marital status) demographic variables, to assess the need to include these as covariates. Statistical significance was set at less than or equal to α (p ≤ .05). For Aim 1, independent effects were identified when either household chaos or maternal emotion responses were statistically significantly associated with the outcome of interest in bivariate correlation analyses. Demographic characteristics that were statistically significantly (p ≤ .05) associated with model variables were included as covariates in Aim 2 analyses. The PROCESS macro was used to examine interactive (moderation) effects;29 PROCESS is used to examine moderation and mediation, with benefits including the program’s ability to generate bootstrapped confidence intervals for model coefficients and interaction effects. After estimates were derived from PROCESS, we conducted simple slopes analysis by inputting coefficients, variances, and covariances from the regression equations, plotting values for the effect of chaos on child eating behaviors, and calculating slopes and slope standard errors at different levels of maternal emotion responsiveness.29 For Aim 2, interactive effects were identified when the interaction term was statistically significantly associated with the outcome of interest. Statistical significance was set at p < 0.05 for all analyses.
Results
Parent age was associated with emotional overeating (r = −.24, p = .03) and problem-focused responses to children’s negative emotions (r = .24, p = .04). Household income was associated with observed maternal sensitivity (r = .23, p = .04), and with household chaos (r = −.22, p = .05). Meal length was not significantly associated with any child eating behavior outcomes: food responsiveness (r = −.11, p = .26), emotional overeating (r = −.18, p = .07), emotional undereating (r = −.13, p = .19), food fussiness (r = −.09, p = .38), satiety responsiveness (r = −.04, p = .67), slowness in eating (r = −.03, p = .78), food enjoyment (r = .03, p = .80). Meal length was also not associated with maternal emotion responses (self-report and observed) or household chaos. Child age in months at the time of the home visit was not associated with any model variables.
Marital status, parent race, and employment status were all dichotomized into two groups (married vs. unmarried, White vs. non-White, Employed vs. Unemployed) because cell sizes were too small to examine mean differences using analysis of variance (ANOVA). Thus, associations between these and model variables were assessed using Mann Whitney U tests for unequal groups. Married mothers had children who were higher on emotional undereating (z = −2.33, p = .03), but there were no other differences by marital status or parent race. Education was associated with higher household chaos, with post-hoc Tukey tests indicating that mothers with postgraduate degrees reported significantly lower chaos compared to mothers with some college/technical school or less (F [df] = 4.31 [105], p = .016). There were no associations between child gender (Independent Samples t-test) or maternal employment and model variables.
Aim 1: Bivariate Analyses
Using Spearman’s correlations, household chaos was significantly associated with food responsiveness (r = .25, p = .009) and emotional overeating (r = .34, p < .001), but not with emotional undereating (r = .13, p = .21), food fussiness (r = .07, p = .46), satiety responsiveness (r = .07, p = .46), slowness in eating (r = −.14, p = .16), or food enjoyment (r = −.05, p = .64).
Observed maternal sensitivity (r’s = −.13 to .11, p’s = .23 to .86), structuring (r’s = −.13 to .09, p’s = .19 to .77), and attending responses (r’s = −.10 to .16, p’s = .12 to .90), were not associated with any child eating behaviors.
Similarly, mothers’ self-reports of expressive encouragement (r’s = −.13 to .11, p’s = .21 to .92), emotion focused (r’s = −.08 to 19, p’s = .06 to .77), and problem focused responses (r’s = −.16 to .08, p’s = .10 to .89) were also not significantly associated with child eating behaviors. Self-reported maternal emotion-focused responses was marginally (r = −.19, p = .06) but not significantly associated with child satiety responsiveness.
Aim 2: Moderation Analyses
We hypothesized that the association between household chaos and children’s eating behaviors would be attenuated by higher levels of maternal emotional responsiveness and exacerbated by lower levels of responsiveness. Although moderation does not require that both the exposure (household chaos) and the moderator (emotional responsiveness) are associated with the outcome,29 we only examined moderation effects for child eating behavior variables that were significantly associated with household chaos in bivariate analyses (food responsiveness and emotional overeating) in order to reduce the likelihood of Type I error. To be consistent across analyses, we included all demographic variables that were significantly associated with household chaos, maternal emotional responsiveness, or child eating behaviors as covariates in moderation analyses. Additionally, we included mealtime length as a covariate in all analyses because it has the theoretical potential to confound associations between behaviors observed at the mealtime and child eating behaviors. Thus, parent age, household income, mealtime length in minutes, marital status, and maternal educational attainment were included as covariates.
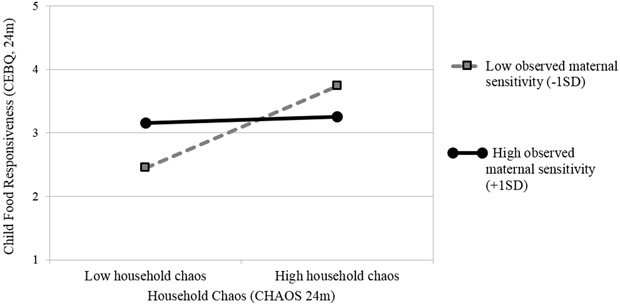
Food responsiveness.
Across all models, household chaos was significantly independently associated with child food responsiveness, and maternal emotional responsiveness was not independently associated with the outcome (Table 2). However, observed sensitivity significantly moderated the association the between household chaos and child food responsiveness. In simple slopes analysis, higher levels of household chaos were associated with higher levels of child food responsiveness only among children of mothers observed engaging in lower levels of sensitivity at mealtimes (Figure 1). There was not a significant association between household chaos and child food responsiveness among children of mothers observed engaging in higher levels of observed sensitivity. More specifically, among children exposed to lower levels of observed maternal sensitivity, there is a 1.29 unit increase in food responsiveness from a mean predicted value of 2.45 for low levels of household chaos to 3.74 for higher levels of household chaos. These scores correspond to mothers’ responding—on average—that children “Rarely” or “Sometimes” are food responsive in conditions of low chaos and low sensitivity, and “Sometimes” or “Often” are food responsive in conditions of high chaos and low sensitivity.
Table 2.
Independent and interactive effects of household chaos (IV) and maternal emotional responsiveness or sensitivity (moderator) on child food responsiveness. ǂ
| ER Moderator (Self-report) → | Model 1: Expressive encouragement response |
Model 2: Emotion-focused responses |
Model 3: Problem-focused responses |
||||||
|---|---|---|---|---|---|---|---|---|---|
| B | SE | 95%CI | B | SE | 95%CI | B | SE | 95%CI | |
| Maternal age | −.03 | .02 | −.06, .00 | −.03 | .02 | −.06, .00 | −.04* | .02 | −.07, −.01 |
| Household income | −.01 | .02 | −.06, .04 | −.01 | .02 | −.05, .05 | .00 | .02 | −.05, .04 |
| Mealtime length (minutes) | −.03 | .02 | −.06, .01 | −.02 | .02 | −.05, .01 | −.02 | .06 | −.05, .01 |
| Marital status | .33 | .22 | −.11, .76 | .32 | .22 | −.11, .76 | .30 | .23 | −.15, .76 |
| Maternal educational attainment | .16 | .10 | −.03, .36 | .14 | .09 | −.05, .32 | .14 | .10 | −.05, .33 |
| Chaos (IV) | .40* | .14 | .12, .69 | .39* | .14 | .11, .67 | .38* | .15 | .08, .67 |
| ERS Moderator | −.05 | .05 | −.16, .06 | .08 | .09 | −.07, .23 | .05 | .10 | −.14, .24 |
| Chaos × ERS interaction term | −.18 | .13 | −.44, .07 | −.37 | .19 | −.75, .01 | −.34 | .21 | −.75, .07 |
| R2, p-value | R2 = .23*, p = .02 | R2 = .25*, p = .01 | R2 = .23*, p = .02 | ||||||
| ΔR2 with interaction term, p-value | ΔR2 = .03, p = .15 | ΔR2 = .04, p = .06 | ΔR2 = .03, p = .10 | ||||||
| ER Moderator (Observed) → | Model 4: Sensitive responses | Model 5: Attending responses |
Model 6: Structuring/ limiting responses |
||||||
| B | SE | 95% CI | B | SE | 95% CI | B | SE | 95% CI | |
| Maternal age | −.04* | .01 | −.06, −.01 | −.03 | .01 | −.06, .00 | −.04* | .01 | −.06, −.01 |
| Household income | −.01 | .02 | −.06, .03 | −.01 | .02 | −.05, .04 | −.01 | .02 | −.05, .04 |
| Mealtime length (minutes) | −.03 | .01 | −.05, .01 | −.02 | .02 | −.05, .01 | −.02 | .02 | −.05, .01 |
| Marital status (married, unmarried) | .40 | .21 | −.03, .82 | .25 | .22 | −.18, .68 | .34 | .22 | −.09, .78 |
| Maternal educational attainment | .14 | .09 | −.04, .32 | .15 | .09 | −.04, .33 | .16 | .09 | −.03, .35 |
| Chaos (IV) | .32* | .14 | .05, .60 | .37* | .15 | .08, .66 | .38* | .14 | .10, .66 |
| ER Moderator | .36 | .21 | −.06, .77 | −.04 | .34 | −.72, .63 | .07 | .23 | −.38, .53 |
| Chaos × ER interaction term | −1.01* | .40 | −1.81, −.22 | −.86 | .88 | −.72, .63 | −.81 | .50 | −1.79, .18 |
| R2, p-value | R2 = .27*, p < .01 | R2 = .21*, p = .02 | R2 = .26*, p = .02 | ||||||
| ΔR2 with interaction term, p-value | ΔR2 = .06*, p = .01 | ΔR2 =.01, p = .33 | ΔR2 =.03, p = .11 | ||||||
Note. Separate moderation analyses were run using the same IV (chaos) and outcome variable (child food responsiveness), but varying the variable used to describe maternal emotional responsiveness. Moderators in the top row (Models 1 – 3) are all derived from a self-report measure, and moderators in the bottom row (Models 4 – 6) are derived from observations of family mealtimes.
IV = independent variable; ER = Emotional Responsiveness.
p < .05
Higher scores for food responsiveness indicates higher levels of approach-related eating behavior dysfunction.
Figure 1.
Household chaos is associated with higher levels of child food responsiveness only among mothers observed engaging in lower levels of sensitive emotional responses at mealtimes.
Note. CHAOS = Confusion, Hubbub, and Order Scale; CEBQ = Children’s Eating Behavior Questionnaire.
Slope for association between household chaos and child food responsiveness was significant at low levels (−1SD) of observed maternal sensitivity (R2 [SE] = .68 [.28], p = .02). Slope at high levels of observed maternal sensitivity (+1SD) was not statistically significant (R2 [SE] = .05 [.51], p = .92).
Emotional overeating.
Results for emotional overeating mirrored those for food responsiveness. Across all models, household chaos was significantly associated with child emotional overeating, and maternal emotional responsiveness was not (Table 3). Observed sensitivity at mealtimes significantly moderated the association between household chaos and food responsiveness, and the pattern was identical to the one reported previously. That is, simple slopes analysis revealed that higher levels of household chaos were associated with higher levels of child emotional overeating only among children of mothers observed engaging in lower levels of sensitivity at mealtimes. There was no association between household chaos and child emotional overeating among children of mothers observed engaging in higher levels of observed sensitivity. More specifically, among children exposed to lower levels of observed maternal sensitivity, there is a 0.95 unit increase in overeating from a mean predicted value of 1.82 for low levels of household chaos to 2.77 for higher levels of household chaos. These scores correspond to mothers’ responding—on average—that children “Never” or “Rarely” overeat in conditions of low chaos and low sensitivity, and “Rarely” or “Sometimes” overeat in conditions of high chaos and low sensitivity. This figure is provided in Online Supplementary Figure 2 because the pattern of association is similar to that reported in Figure 1.
Table 3.
Independent and interactive effects of household chaos (IV) and maternal emotional responsiveness or sensitivity (moderator) on child emotional overeating. ǂ
| ER Moderator (Self report)→ | Model 7: Expressive encouragement response |
Model 8: Emotion-focused responses |
Model 9: Problem- focused responses |
||||||
|---|---|---|---|---|---|---|---|---|---|
| B | SE | 95%CI | B | SE | 95%CI | B | SE | 95%CI | |
| Maternal age | −.03* | .01 | −.05, −.01 | −.04* | .01 | −.06, −.01 | −.04* | .01 | −.06, −.01 |
| Household income | −.04 | .09 | −.22, .15 | .02 | .02 | −.02, .05 | .01 | .02 | −.02, .05 |
| Mealtime length (minutes) | −.02 | .01 | −.05, .00 | −.02 | .01 | −.04, .00 | −.02 | .01 | −.04, .00 |
| Marital status | .13 | .16 | −.18, .44 | .08 | .16 | −.23, .39 | .11 | .50 | −.22, .44 |
| Maternal educational attainment | .13 | .07 | −.01, .27 | .14* | .07 | .01, .27 | .13 | .07 | −.01, .27 |
| Chaos (IV) | .38* | .10 | .17, .58 | .40* | .10 | .20, .60 | .38* | .11 | .17, .59 |
| ER Moderator | −.02 | .04 | −.10, .05 | .10 | .05 | −.01, .21 | .03 | .07 | −.10, .17 |
| Chaos × ERS interaction term | −.04 | .09 | −.22, .15 | −.03 | .14 | −.30, .24 | −.09 | .15 | −.38, .21 |
| R2, p-value | R2 = .28*, p = .002 | R2 = .31*, p < .001 | R2 = .28*, p = .002 | ||||||
| ΔR2 with interaction term, p-value | ΔR2 = .002, p = .70 | ΔR2 = .001, p = .81 | ΔR2 = .003, p = .56 | ||||||
| ER Moderator (Observed) → | Model 10: Sensitive Responses |
Model 11: Attending Responses |
Model 12: Structuring/ Limiting Responses |
||||||
| B | SE | 95%CI | B | SE | 95%CI | B | SE | 95%CI | |
| Maternal age | −.04* | .01 | −.06, −.02 | −.03* | .01 | −.05, −.01 | −.04* | .01 | −.06, −.02 |
| Household income | .01 | .02 | −.03, .04 | .01 | .02 | −.02, .04 | .01 | .02 | −.02, .04 |
| Mealtime length (minutes) | −.02 | .01 | −.05, .00 | −.02 | .01 | −.04, .00 | −.02 | .01 | −.05, .00 |
| Marital status (married, unmarried) | .19 | .15 | −.12, .49 | .11 | .15 | −.20, .42 | .17 | .16 | −.14, .47 |
| Maternal educational attainment | .13 | .06 | .00, .26 | .13 | .07 | .00, .26 | .14* | .07 | .01, .27 |
| Chaos (IV) | .33* | .10 | .13, .53 | .37* | .10 | .16, .57 | .36* | .10 | .16, .56 |
| ER Moderator | .16 | .15 | −.13, .46 | −.04 | .24 | −.52, .44 | .09 | .16 | −.24, .41 |
| Chaos × ERS interaction term | .33* | .10 | .13, .53 | −.22 | .62 | −1.46, 1.02 | −.46 | .35 | −1.16, .24 |
| R2, p-value | R2 = .32*, p < .001 | R2 = .28*, p = .002 | R2 = .30*, p < .001 | ||||||
| ΔR2 with interaction term, p-value | ΔR2 = .04*, p = .05 | ΔR2 = .001, p = .72 | ΔR2 = .02, p = .19 | ||||||
Note. Separate moderation analyses were run using the same IV (chaos) and outcome variable (child food responsiveness), but varying the variable used to describe maternal emotional responsiveness. Moderators in the top row (Models 7 – 9) are all derived from a self-report measure, and moderators in the bottom row (Models 10 – 12) are derived from observations of family mealtimes.
IV = independent variable; SR = self-reported; ER = Emotional Responsiveness or Sensitivity; Obs = Observed.
p < .05
Higher scores for overeating indicates higher levels of approach-related eating behavior dysfunction.
The magnitude of the association between household chaos and child emotional eating was smaller than magnitude of the association between household chaos and child food responsiveness, as evidenced by a smaller ΔR2 (ΔR2 = .04 vs. .06) and a lower slope at low levels of observed maternal sensitivity (Slope = .51 vs. .69) for models with child emotional overeating. This in addition to the fact that moderation effects were only significant at p = 0.05 (confidence intervals not at risk of overlapping with zero), necessitates caution when interpreting findings for emotional overeating. Nevertheless, findings suggest that household chaos is associated with certain child eating behaviors, and that maternal emotional sensitivity at mealtimes may be a buffer for the association between household chaos and child food responsiveness and emotional overeating.
Discussion
In partial support of the first hypothesis, we found that higher levels of household chaos were associated with more eating behaviors characterized by food approach in bivariate analyses, although expected associations between sensitivity and child eating behaviors were not present. In support of the second hypothesis however, those independent effects were statistically significant only for children exposed to low levels of observed maternal emotional sensitivity at mealtimes. That is, household chaos was not associated with overeating or food responsiveness behaviors among children exposed to high levels of observed maternal emotional sensitivity at mealtimes. Additionally, it was only maternal emotional sensitivity at mealtimes—but not sensitivity generally—that buffered the effects of chaos on eating behavior. Findings, limitations, and recommendations are discussed below.
To the best of our knowledge, the current study is the first to show (1) associations between household chaos and child eating behaviors and (2) that maternal sensitivity during mealtimes may attenuate the effect of household chaos on children’s eating behaviors. Consistent with prior studies showing a link between household chaos and poorer dietary intake,13 we found that chaos was associated with overeating and food responsiveness eating behaviors in 18–24 month old children. However, this association was only significant among children of mothers observed engaging in lower levels of sensitivity at family meals. Mothers engaging in high levels of emotional sensitivity may protect their children from the negative effects of household chaos (unpredictable or unstable environment) by providing a predictable, organized response to their child’s emotions. In contrast, mothers engaging in low levels of sensitivity may be exacerbating the unpredictable effects of household chaos on children’s eating behaviors.
Interaction effects were only significant when maternal emotional sensitivity observed at mealtimes, but not general maternal emotional sensitivity, was modeled as the moderator. Measures of emotional sensitivity varied on two dimensions: contextual effects (mealtime vs. general emotional sensitivity) and measurement method (observed vs. self-report). Although it could be argued that measurement error was responsible for this lack of association, it would be more likely that self-report measures of parenting would correlate with self-report measures of child eating. Given that we found that neither measure of maternal emotional responsiveness was associated with child eating behavior in bivariate correlation analyses, we suggest that maternal emotional responsiveness and sensitivity may only have contextually specific (e.g., during mealtimes, when considering household chaos) effects on child eating behaviors. However, it is possible that an objective assessment of general maternal emotional sensitivity would serve as a moderator for this association, and future studies should consider evaluating these effects.
Household chaos was not associated with enjoyment of food or food avoidance behaviors (slow eating, satiety responsiveness, emotional undereating, food fussiness). From a methodological standpoint, the slightly lower internal reliability for some of these scales may reflect the practical difficulty in determining when a very young child is no longer hungry. From a conceptual standpoint, household chaos may act on eating by creating a more unpredictable environment, which in turn might push children toward food approach behaviors as a self-soothing strategy, or to ensure they are fed if food becomes scarce. It is possible that a more food avoidant child could contribute to a more chaotic household by demanding different meals or contributing to a combative mealtime emotional climate, but in this study, we did not see such an effect. Nevertheless, it is important to consider these potential bidirectional associations between eating and environment, highlighting the need for longitudinal studies with repeated measures.
There are several limitations that bear noting. First, the current study was conducted among a non-diverse, relatively small sample of families at low risk for chaos, limiting the study’s generalizability and our ability to detect statistically significant differences, as was demonstrated in the relatively small effect detected in analyses on child overeating. Families in the current study reported less chaos in comparison to previously published reports using the same measure.9 Nevertheless, because household chaos was normally distributed with no outliers, it is possible that findings are more conservative than those in a higher-risk group with higher levels of household chaos. Future research should investigate associations between chaos and child eating in higher risk populations with more diverse and larger samples.10 Second, we measured only mothers’ behaviors in the current study, although fathers and other family members may also have influenced child eating behaviors. Other studies have examined fathers’ influence on mothers’ feeding behaviors,30 but the current study is limited in that it did not measure or examine whether paternal sensitivity or the behaviors of other family members were associated with child outcomes. Third, we can make no assertions about directionality because of the cross-sectional design, limiting our ability to make recommendations for practitioners. Longitudinal studies using naturalistic observations of family mealtimes are needed. Fourth, use of self-report surveys, the presence of a camera in the family home, and stopping coding after 20 minutes may have introduced bias. Although using an observational assessment of feeding and eating behavior in addition to surveys would be ideal and could reduce social desirability bias, there are currently no validated observational assessments of eating behaviors for children under 3-years old that can be applied in home environments. However, the measure used to assess eating behavior is one of the most commonly used measures in early childhood, allowing findings to be compared across studies with similarly aged samples. The CEBQ is also the only parent-report assessment of eating behavior patterns that has been used previously with children in the phase of life after weaning from a primarily milk-based diet.24 Future studies should prioritize developing observational assessments of children’s eating behaviors that can be implemented with high levels of ecological validity in naturalistic home environments, particularly given our findings showing the association between the home environment and child eating behaviors. Regarding mealtime length, coding stopped at 20 minutes because average mealtime length has been consistently reported to be about 20 minutes in studies including clinical and non-clinical samples.31 However, this may have introduced bias for families who normally have longer mealtimes because of children’s eating-related issues. Finally, it is possible that specific aspects of household chaos—such as mealtime routines or rituals—may have had a stronger effect on parent and child mealtime behaviors than other components like excessive noise. Indeed, in a recent study, we found that higher levels of distractions at mealtimes were associated with lower levels of maternal feeding responsiveness, suggesting that these proximal facets of household chaos may make good targets for parent-focused interventions.31 Future studies should address this by examining the relative contributions of different components of household chaos to variance in children’s appetite self-regulation behaviors and weight outcomes.
Conclusions
The current study found that higher levels of household chaos are associated with more emotional overeating and food responsiveness behaviors only among 18–24 month old children of mothers observed engaging in relatively lower sensitivity at mealtime. Findings suggest that higher maternal sensitivity may attenuate the negative effects of household chaos on unhealthy child eating behaviors. Responding sensitively to children’s negative emotions at mealtimes may create a predictable environment, thus promoting resilience to the deleterious effects of household chaos on eating behaviors. Future studies should prioritize longitudinal designs with observational assessments of parenting behaviors at mealtimes, untangling parenting in food-related and non-food related contexts and replicating these findings in samples families at higher risk for household chaos. Although methodological limitations for the current study prevent strong recommendations for action among practitioners and policymakers, pediatricians working with overweight or obese children and their parents may consider discussing ways to increase sensitivity and decrease chaos around family mealtimes.
Supplementary Material
Online Supplementary Figure 1. Conceptual model for hypothesized independent (a) and interactive (b) associations between household chaos, maternal sensitivity, and child appetite dysregulation.
Online Supplementary Figure 2. Household chaos is associated with higher levels of child emotional overeating only among mothers observed engaging in lower levels of sensitive emotional responsiveness at mealtimes. Note. CHAOS = Confusion, Hubbub, and Order Scale; CEBQ = Children’s Eating Behavior Questionnaire. Slope for association between household chaos and child emotional overeating was significant at low levels (−1SD) of observed maternal sensitivity (R2 [SE] = .51 [.12], p < .01). Slope at high levels of observed maternal sensitivity (+1SD) was not statistically significant (R2 [SE] = .18 [.14], p = .20).
Acknowledgements
The authors would like to thank Dr. Janet Liechty for providing feedback on previous versions of this manuscript, and to acknowledge Dr. Natasha Chong Cole, Dr. Maria Pineros-Leano, Dr. Steve Tran, Alyssa Parsons, Samantha Iwinski, Marisa Cullnan, Jocelyne Lopez, Valerie Sherman, and McKenzie Martin for their substantial contributions to data collection and coding.
Funding
This material is based upon work that is supported by the National Institute of Food and Agriculture, U. S. Department of Agriculture, under award number 2011–67001-30101. This research was supported in part by grants from the National Dairy Council to Sharon Donovan and Barbara H. Fiese (CoPI’s), the Gerber Foundation to Sharon Donovan, the Christopher Family Foundation to Sharon Donovan and Kelly K. Bost, Hatch ILLU 793–330 from the U.S. Department of Agriculture to Barbara H. Fiese, Kelly K. Bost and Margarita Teran-Garcia, the National Institutes of Health DK107561 to Sharon Donovan, the Illinois Association for Infant Mental Health to Jaclyn A. Saltzman, and an Illinois Transdisciplinary Obesity Prevention Program Seed Grant to Jaclyn A. Saltzman. The STRONG Kids 2 Team includes Kelly Bost, Sharon Donovan, Soo-Yeun Lee, Brent McBride, Margarita Teran-Garcia and Barbara H. Fiese. The authors of this publication have no other conflicts of interest to report.
Contributor Information
Jaclyn A. Saltzman, Department of Social and Behavioral Sciences, Harvard T. H. Chan School of Public Health, Boston, MA; Academic Pediatrics, Massachusetts General Hospital for Children, Boston, MA.
Kelly K. Bost, Department of Human Development and Family Studies, University of Illinois at Urbana-Champaign, Urbana, IL.
Brent A. McBride, Child Development Laboratory, Department of Human Development and Family Studies, University of Illinois at Urbana-Champaign, Urbana, IL.
Barbara H. Fiese, Family Resiliency Center, Department of Human Development and Family Studies, University of Illinois at Urbana-Champaign, Urbana, IL.
References
- 1.Dietz WH. Health Consequences of Obesity in Youth: Childhood Predictors of Adult Disease. Pediatrics. 1998;101(Supplement 2):518–525. [PubMed] [Google Scholar]
- 2.Freedman DS, Khan LK, Dietz WH, et al. Relationship of Childhood Obesity to Coronary Heart Disease Risk Factors in Adulthood: The Bogalusa Heart Study. Pediatrics. 2001;108(3):712–718. doi: 10.1542/peds.108.3.712 [DOI] [PubMed] [Google Scholar]
- 3.Llewellyn C, Wardle J. Behavioral susceptibility to obesity: Gene–environment interplay in the development of weight. Physiol Behav. 2015;152:494–501. doi: 10.1016/j.physbeh.2015.07.006 [DOI] [PubMed] [Google Scholar]
- 4.Webber L, Hill C, Saxton J, et al. Eating behaviour and weight in children. Int J Obes. 2009;33(1):21–28. doi: 10.1038/ijo.2008.219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Frankel LA, Hughes SO, O’Connor TM, et al. Parental Influences on Children’s Self-Regulation of Energy Intake: Insights from Developmental Literature on Emotion Regulation. J Obes. 2012;2012:1–12. doi: 10.1155/2012/327259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Graziano PA, Calkins SD, Keane SP. Toddler self-regulation skills predict risk for pediatric obesity. Int J Obes. 2010;34(4):633–641. doi: 10.1038/ijo.2009.288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Daniels LA, Mallan KM, Battistutta D, et al. Child eating behavior outcomes of an early feeding intervention to reduce risk indicators for child obesity: The NOURISH RCT. Obesity. 2014;22(5):E104–E111. doi: 10.1002/oby.20693 [DOI] [PubMed] [Google Scholar]
- 8.Blake-Lamb TL, Locks LM, Perkins ME, et al. Interventions for Childhood Obesity in the First 1,000 Days A Systematic Review. Am J Prev Med. 2016;50(6):780–789. doi: 10.1016/j.amepre.2015.11.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Coldwell J, Pike A, Dunn J. Household chaos – links with parenting and child behaviour. J Child Psychol Psychiatry. 2006;47(11):1116–1122. doi: 10.1111/j.1469-7610.2006.01655.x [DOI] [PubMed] [Google Scholar]
- 10.Dumas JE, Nissley J, Nordstrom A, et al. Home Chaos: Sociodemographic, Parenting, Interactional, and Child Correlates. J Clin Child Adolesc Psychol. 2005;34(1):93–104. doi: 10.1207/s15374424jccp3401_9 [DOI] [PubMed] [Google Scholar]
- 11.Martin A, Razza RA, Brooks-Gunn J. Specifying the links between household chaos and preschool children’s development. Early Child Dev Care. 2012;182(10):1247–1263. doi: 10.1080/03004430.2011.605522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vernon-Feagans L, Willoughby M, Garrett-Peters P, et al. Predictors of behavioral regulation in kindergarten: Household chaos, parenting, and early executive functions. Dev Psychol. 2016;52(3):430–441. doi: 10.1037/dev0000087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Martin‐Biggers J, Quick V, Zhang M, et al. Relationships of family conflict, cohesion, and chaos in the home environment on maternal and child food-related behaviours. Matern Child Nutr. 2018;14(2):e12540. doi: 10.1111/mcn.12540 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Davidov M, Grusec JE. Untangling the Links of Parental Responsiveness to Distress and Warmth to Child Outcomes. Child Dev. 2006;77(1):44–58. doi: 10.1111/j.1467-8624.2006.00855.x [DOI] [PubMed] [Google Scholar]
- 15.Spanglar G, Schieche M, Ilg U, et al. Maternal sensitivity as an external organizer for biobehavioral regulation in infancy. Dev Psychobiol. 1994;27(7):425–437. doi: 10.1002/dev.420270702 [DOI] [PubMed] [Google Scholar]
- 16.Wendland BE, Atkinson L, Steiner M, et al. Low maternal sensitivity at 6 months of age predicts higher BMI in 48 month old girls but not boys. Appetite. 2014;82:97–102. doi: 10.1016/j.appet.2014.07.012 [DOI] [PubMed] [Google Scholar]
- 17.Cassidy J Emotion Regulation: Influences of Attachment Relationships. Monogr Soc Res Child Dev. 1994;59(2–3):228–249. doi: 10.1111/j.1540-5834.1994.tb01287.x [DOI] [PubMed] [Google Scholar]
- 18.Faber A, Dubé L, Knäuper B. Attachment and eating: A meta-analytic review of the relevance of attachment for unhealthy and healthy eating behaviors in the general population. Appetite. 2018;123:410–438. doi: 10.1016/j.appet.2017.10.043 [DOI] [PubMed] [Google Scholar]
- 19.Sigman-Grant M, Hayes J, VanBrackle A, et al. Family Resiliency: A Neglected Perspective in Addressing Obesity in Young Children. Child Obes. 2015;11(6):664–673. doi: 10.1089/chi.2014.0107 [DOI] [PubMed] [Google Scholar]
- 20.Saltzman JA, Fiese BH, Bost KK, et al. Development of appetite self-regulation: Integrating perspectives from attachment and family systems theory. Child Dev Perspect. 2017;12(1):1–7. doi: 10.1111/cdep.12254 [DOI] [Google Scholar]
- 21.Fiese BH, Musaad S, Bost KK, et al. STRONG Kids2 Birth Cohort Study: A Cell-to-Society Approach to Dietary Habits and Weight Trajectories Across the First Five Years of Life. Curr Dev Nutr. In press; nzz007. doi: 10.1093/cdn/nzz007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Matheny AP, Wachs TD, Ludwig JL, et al. Bringing order out of chaos: Psychometric characteristics of the confusion, hubbub, and order scale. J Appl Dev Psychol. 1995;16(3):429–444. doi: 10.1016/0193-3973(95)90028-4 [DOI] [Google Scholar]
- 23.Carnell S, Wardle J. Measuring behavioural susceptibility to obesity: Validation of the child eating behaviour questionnaire. Appetite. 2007;48(1):104–113. doi: 10.1016/j.appet.2006.07.075 [DOI] [PubMed] [Google Scholar]
- 24.Brown A, Lee M. Breastfeeding during the first year promotes satiety responsiveness in children aged 18–24 months. Pediatr Obes. 2012;7(5):382–390. doi: 10.1111/j.2047-6310.2012.00071.x [DOI] [PubMed] [Google Scholar]
- 25.Mangold International. INTERACT.; 2016. [Google Scholar]
- 26.Cole PM, Wiggins CN, Radzioch AM, et al. D.O.T.S. Emotion Coding System.; 2007. [Google Scholar]
- 27.Fabes RA, Poulin RE, Eisenberg N, et al. The Coping with Children’s Negative Emotions Scale (CCNES): Psychometric properties and relations with children’s emotional competence. Marriage Fam Rev. 2002;34(3–4):285–310. doi: 10.1300/J002v34n03_05 [DOI] [Google Scholar]
- 28.IBM Analytics. Statistical Package for the Social Sciences, Version 24.0.; 2016. http://www.ibm.com/analytics/us/en/technology/spss/. Accessed April 18, 2016.
- 29.Hayes AF. Introduction to Mediation, Moderation, and Conditional Process Analysis, Second Edition: A Regression-Based Approach. Guilford Publications; 2017. [Google Scholar]
- 30.Saltzman JA, Musaad S, Bost KK, et al. Associations between father availability, mealtime distractions and routines, and maternal feeding responsiveness: An observational study J Fam Psychol. Advance online publication. doi: 10.1037/fam0000519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fiese BH, Winter MA, Botti JC. The ABCs of Family Mealtimes: Observational Lessons for Promoting Healthy Outcomes for Children with Persistent Asthma. Child Dev. 2011;82(1):133–145. doi: 10.1111/j.1467-8624.2010.01545.x [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Online Supplementary Figure 1. Conceptual model for hypothesized independent (a) and interactive (b) associations between household chaos, maternal sensitivity, and child appetite dysregulation.
Online Supplementary Figure 2. Household chaos is associated with higher levels of child emotional overeating only among mothers observed engaging in lower levels of sensitive emotional responsiveness at mealtimes. Note. CHAOS = Confusion, Hubbub, and Order Scale; CEBQ = Children’s Eating Behavior Questionnaire. Slope for association between household chaos and child emotional overeating was significant at low levels (−1SD) of observed maternal sensitivity (R2 [SE] = .51 [.12], p < .01). Slope at high levels of observed maternal sensitivity (+1SD) was not statistically significant (R2 [SE] = .18 [.14], p = .20).