Abstract
Background
Lumbar supports are used in the treatment of low‐back pain patients, to prevent the onset of low‐back pain (primary prevention) or to prevent recurrences of a low‐back pain episode (secondary prevention).
Objectives
To assess the effects of lumbar supports for prevention and treatment of non‐specific low‐back pain.
Search methods
We updated the search in the Cochrane Central Register of Controlled Trials, PubMed, EMBASE, and CINAHL to December 2006. We also screened references given in relevant reviews and identified trials, and contacted experts to identify additional RCTs.
Selection criteria
Randomized controlled trials that reported on any type of lumbar supports as preventive or therapeutic intervention for non‐specific low‐back pain.
Data collection and analysis
One review author generated the electronic search. Two review authors independently identified trials that met the inclusion criteria. One review author extracted data on the study population, interventions, and final results. The methodological quality and the clinical relevance were independently assessed by two review authors.
Because it was not possible to perform a quantitative analysis, we performed a qualitative analysis in which the strength of evidence on the effectiveness of lumbar supports was classified as strong, moderate, limited, conflicting, or no evidence.
Main results
Seven preventive studies (14,437 people) and eight treatment studies (1361 people) were included in this updated review. Overall, the methodological quality of the studies was rather low. Only five of the fifteen studies met 50% or more of the internal validity items.
There was moderate evidence that lumbar supports are not more effective than no intervention or training in preventing low‐back pain, and conflicting evidence whether lumbar supports are effective supplements to other preventive interventions. It is still unclear if lumbar supports are more effective than no or other interventions for the treatment of low‐back pain.
Authors' conclusions
There is moderate evidence that lumbar supports are not more effective than no intervention or training in preventing low‐back pain, and conflicting evidence whether they are effective supplements to other preventive interventions. It remains unclear whether lumbar supports are more effective than no or other interventions for treating low‐back pain.
There is still a need for high quality randomised trials on the effectiveness of lumbar supports. One of the most essential issues to tackle in these future trials seems to be the realization of an adequate compliance. Special attention should be paid to different outcome measures, types of patients and types of lumbar support.
Plain language summary
Lumbar supports for the prevention and treatment of low‐back pain
Lumbar supports (also called braces or corsets) are used in the prevention and treatment of low‐back pain. This review is important because low‐back pain is very common. Prevention and treatment are important both to people with back pain and to society, which bears the expense of back pain treatment and sick leave due to back pain.
We included seven studies on prevention (14,437 people) and eight studies on treatment (1361 people) in this review.
Prevention: There was little or no difference between individuals with low‐back pain who used back supports and those who received no treatment (five studies, 13,995 people), or education on lifting techniques (two studies, 954 people) in back pain prevention or reduction of sick leave.
In one study (82 people), back supports added to back school (patient education about recovering from back pain) were helpful in reducing the number of days of sick leave but not in preventing back pain. Back supports plus usual medical care reduced the number of days of low‐back pain and improved function, but did not reduce sick leave (one study, 360 people).
Treatment: In four studies (1170 people), there was little or no difference between patients with acute or chronic back pain who used back supports and those who received no treatment in short‐term pain reduction or overall improvement.
There is conflicting evidence (two studies, 550 people) about whether back supports are better than nothing in helping low‐back pain patients return to work faster, however in three studies (410 patients), they were better than nothing in helping individuals with subacute and chronic low‐back pain recover function in the short term.
In three studies (954 people), there was little or no difference in short‐term pain reduction, overall improvement and return‐to‐work between those who used back supports and those who received manipulation, physiotherapy, or electrical stimulation. One study (164 people) reported mixed results on whether back supports improved function more than massage and in another study (19 people), use of a lumbar corset with back support was more effective in reducing pain in the short‐term than a corset alone.
Conclusions from this review should be viewed with caution due to the low quality of many of the studies. In the future, researchers should report side effects from wearing back supports and measure how many hours per day the supports are actually worn.
Background
Low‐back pain (LBP) is a major health problem in western industrialized countries. Seventy to 85% of the population has low‐back pain at some time in their life. The annual prevalence of low‐back pain ranges from 15% to 45%, with an average point prevalence of 30% (Asche 2007; Krismer 2007; Maniadakis 2000). The prevalence increases with age up to 65 years (Andersson 1999). Most patients recover quickly and without residual functional loss: 60% to 70% recover within six weeks and 80% to 90% recover within three months (Krismer 2007). Unfortunately, for individuals who do not recover within three months, the recovery process is slow and makes a large and costly demand on the health‐care system. This group of individuals is also a major contributor to disability and absence from work (Andersson 1999, Krismer 2007). In the USA, low‐back pain is the most common cause of activity limitation among people younger than 45 years and the second most frequent reason for visits to a physician (Andersson 1999). In 2002, low‐back pain accounted for approximately 2.3% of all physician visits (Deyo 2006).
The costs of back pain exceed the costs of many other conditions and diseases (Maniadakis 2000). A cost‐of‐illness study of low‐back pain in the United Kingdom estimated that the 1998 direct medical costs were £1.6 billion and that the indirect costs (total cost of absenteeism and disability payments) varied between £5.0 billion and £10.6 billion, depending on the costing method used (Maniadakis 2000). It has been estimated that in the United States, back pain has associated direct costs of US$20 billion and indirect costs of between US$75 and 100 billion. In the Netherlands in 1991, the total direct medicals costs were estimated at US$368 million and the total cost of absenteeism and disability payments (indirect costs) at US$3.1 and US$1.5 billion, respectively (Maniadakis 2000, van Tulder 1995).
Lumbar supports are used in the management of low‐back pain and are also commonly used in the workplace to prevent low‐back pain injuries in employees (Wassell 2000). Lumbar supports are provided as treatment to people suffering from LBP with the aim to decrease impairment and disability. They are also used as an intervention to prevent the onset of LBP (primary prevention) or to prevent recurrent LBP episodes (secondary prevention). There is a wide variety of lumbar supports, both flexible and rigid. They can be worn under or over clothing, with or without shoulder straps, during the whole day or part of the day, only at the workplace or during any activity. Nachemson reported different desired functions of lumbar supports: 1) to correct deformity; 2) to limit spinal motion; 3) to stabilize part of the spine; 4) to reduce mechanical uploading; 5) miscellaneous effects (massage, heat, placebo) (Nachemson 1987). However, at present, the putative mechanisms of action of a lumbar support remain a matter of debate (Dillingham 1998). The systematic review by Van Poppel and colleagues did not support the hypothesis that lumbar supports decrease back muscle force by decreasing the electromyogram of back muscles or by increasing intra‐abdominal pressure (Van Poppel 2000). Neither did Van Poppel's review support the hypothesis that workers would be inclined to lift heavier weights when wearing a lumbar support. The only hypothesis that could be confirmed was that lumbar supports affect trunk motion.
Potential adverse effects of wearing a lumbar support that have been reported are skin lesions, gastro‐intestinal disorders, muscle wasting, higher blood pressure and higher heart rates (Calmels 1996; McGill 1993).
The popularity of lumbar supports has led to several studies investigating their preventive and therapeutic effects. These studies have already been summarized in several reviews on the effectiveness of lumbar supports for prevention (Ammendolia 2005; Dillingham 1998; Linton 2001; van Poppel 1997; van Poppel 2004) and treatment (Koes 1994) of non‐specific low‐back pain. Van Tulder and colleagues published the original Cochrane review (Jellema 2001; Van Tulder 2000). In the earlier Cochrane review, the authors were unable to draw definite conclusions on the effectiveness of lumbar supports due to low methodological quality, heterogeneity and inconsistent results of the included studies. In this update, the results of studies published between 1998 and 2006 are added to the evidence reported in the original Cochrane review.
Objectives
The objectives of this systematic review were to determine whether lumbar supports are effective for prevention and treatment of non‐specific LBP. Comparisons that were investigated are: 1.1 Lumbar support as intervention for prevention of LBP versus no intervention. 1.2 Lumbar support as intervention for prevention of LBP versus other types of prevention. 1.3 Lumbar support as supplement to another type of prevention of LBP versus that other type of prevention alone.
2.1 Lumbar support as intervention for treatment of LBP versus no intervention. 2.2 Lumbar support as intervention for treatment of LBP versus other types of treatment. 2.3 Lumbar support as supplement to another type of treatment of LBP versus that other type of treatment alone. 2.4 Various types of lumbar support.
The control interventions were labelled as 'no intervention' when there was no intervention or when the control interventions were sham/placebo interventions.
Methods
Criteria for considering studies for this review
Types of studies
Only randomised controlled trials (RCTs) were included, with no language restriction. Non‐randomized trials that were included in the previous review are excluded from this update.
Types of participants
For preventive trials, the study population had to consist of workers aged 18 to 65 years. For therapeutic trials, the study population had to consist of subjects aged 18 to 65 years with non‐specific low‐back pain. RCTs that included subjects with low‐back pain caused by specific pathological entities such as infection, neoplasm, metastasis, osteoporosis, rheumatoid arthritis, or fractures were excluded.
Patients with acute (less than six weeks), subacute (six to 12 weeks) or chronic (12 weeks or more) low‐back pain were included.
Types of interventions
Trials studying any type of lumbar support, flexible or rigid, used for the prevention or treatment of non‐specific LBP were included. Special types of lumbar supports for severe scoliosis and kyphosis were excluded, as were special lumbar supports used after back surgery.
Types of outcome measures
Only preventive studies that used at least one of the following outcome measures were included: incidence of low‐back pain, duration of low‐back pain, absenteeism (% of the studied population, number of days) and back pain‐specific functional status (Roland‐Morris Disability Questionnaire (RMDQ), Oswestry scale). For therapeutic studies, only RCTs that used at least one of the following outcome measures were included: pain (Visual Analogical Scale (VAS), Numerical Rating Scale (NRS)), overall improvement (% improvement, NRS), return to work (% of the population, number of days of absenteeism) and back‐specific functional status (RMDQ, Oswestry scale).
Measurements of outcomes conducted less than three months after randomisation are described as short‐term follow‐up, between three and six months as intermediate follow‐up, and six months or more as long‐term follow‐up.
Search methods for identification of studies
The following search strategies were used for this updated review: 1. Cochrane Central Register of Controlled Trials (CENTRAL) 2006, issue 4; 2. PubMed up to December 2006; 3. EMBASE (Ovid) up to December 2006; 4. CINAHL (EBSCO host) up to December 2006; 5. Current Contents up to September 1999; 6. References in relevant reviews and identified trials; 7. Personal communication with experts in the fields.
The databases were searched using the algorithm recommended in the Updated Method Guidelines (van Tulder 2003). An experienced information expert helped with the literature search. We did not update the search for Current contents since it yielded no unique studies in the original search.
Data collection and analysis
One of the authors of this review is also first author of one of the included trials (van Poppel 1998). She was not involved in any decision regarding selection, quality assessment, data extraction or analysis of this trial. Two of the authors (van Poppel, van Tulder) are authors of another included trial (Roelofs 2007). Neither was involved in any decision regarding selection, quality assessment, data extraction or analysis of this trial.
Study selection
Two review authors selected the studies. Authors, title, subject‐headings, publication type and abstract of the identified studies were downloaded into Reference Manager version 10. Two review authors independently reviewed the information to identify trials that met the inclusion criteria. A consensus method was used to resolve disagreements concerning the final inclusion of RCTs. A third review author was consulted if disagreements were not resolved.
Methodological quality
The methodological quality was independently assessed by two review authors. The articles were not blinded for author, institution or journal, because one of the quality assessors was familiar with the literature. A consensus method was used to resolve disagreements concerning the assessment of the methodological quality of the RCTs included in the review. A third review author was consulted if disagreement persisted. If the article did not contain sufficient information on one or more of the criteria, the authors were contacted for additional information. If the authors could not be contacted or if the information was no longer available, the criteria were scored as 'unclear'.
The methodological quality of the studies was assessed using the criteria recommended in the Updated Method Guidelines (van Tulder 2003, Table 1). The item regarding the blinding of care providers was not included in our quality assessment, because blinding of care providers for lumbar support use seems impossible. Each criterion was scored as either 'positive', 'negative' or 'unclear' according to definitions of the criteria (Table 1). A validity item was scored as 'positive' when the available information regarding that item did not reveal any bias, 'negative' when no information at all was provided regarding that item or when the available information did reveal bias. A validity item was scored as 'unclear' when the available information regarding that item was too scarce to make a conclusion regarding potential bias.
1. Criteria for the Risk of Bias Assessment.
| Criteria for a judgment of yes for the sources of risk of bias |
Prevention: In order to score a 'yes', groups have to be similar at baseline with regarding to at least three of the following important prognostic characteristics: 1) age, 2) incidence and/or duration of a previous episode of low back pain, 3) incidence and/or duration of a present episode of low back pain, 4) type of work, 5) value of main outcome measures. Treatment: In order to score 'positive', groups have to be similar at baseline with regarding to at least three of the following important prognostic characteristics: 1) age, 2) duration of complaints, 3) percentage of patients with radiating pain and 4) value of main outcome measure(s). Moreover, for each group the mean and SD values of these characteristics have to be presented (for example in a table). When they aren't presented, the score is 'unclear'.
|
Clinical Relevance
The two review authors who assessed the methodological quality of the RCTs also judged the clinical relevance of each trial using the five questions recommended by the Updated Method Guidelines (van Tulder 2003, Table 2). Each criterion was scored as either 'positive', 'negative' or 'unclear' according to definitions of the criteria.
2. Questions for assessing clinical relevance.
| questions |
| Each criterion was scored as 'positive', 'negative' or 'unclear'. 1) Are the patients described in detail so that you can decide whether they are comparable to those that you see in your practice? In order to score 'positive' there should be enough information about the subject (age, type of work) and low back pain (type, duration) 2) Are the interventions and treatment settings described well enough so that you can provide the same for your patients? In order to score 'positive' there should be enough information about the type of lumbar support 3) Were all clinically relevant outcomes measured and reported? In order to score 'positive' at least the outcomes of pain and functional status should be reported 4) Is the size of the effect clinically important? In order to score 'positive' the outcome of pain has improved for at least 20%, and the outcome of functional status for at least 10%. This is not defined for work. 5) Are the likely treatment benefits worth the potential harms? In order to score 'positive' there should be benefits. |
Data extraction
Using a standardized form, one review author extracted data on the characteristics of the study population (age, gender), type of work performed by the study population (in prevention trials), type of LBP (with or without radiation, in treatment trials), duration of LBP ((sub)acute or chronic, in treatment trials), type of study (RCT), duration of intervention period, timing of follow‐up measurements (short term, intermediate or long term), characteristics of the studied intervention (type of lumbar support, the number of hours per day prescribed for the subjects to wear the lumbar support, duration of intervention period), characteristics of the control intervention (type, intensity, duration of intervention period), adverse effects due to the interventions, compliance, and the final results for each outcome measure on the effectiveness of lumbar supports. One review author (IvD) compared these findings to data extracted on the same characteristics of the same studies published in other reviews (van Poppel 2004). The articles were not blinded for author, institution or journal.
Data analysis
Many studies did not report results in a way that permitted statistical pooling (for example means with standard deviations for continuous data). Furthermore, studies were heterogeneous with regard to study populations, interventions and outcomes. Therefore, we decided not to perform a meta‐analysis but to qualitatively summarize the results. A rating system was used, consisting of five levels of scientific evidence based on the design, the quality, and the outcome of the studies (van Tulder 2003): 1) Strong evidence ‐ provided by generally consistent findings in multiple high quality RCTs. 2) Moderate evidence ‐ provided by generally consistent findings in one high quality RCT and one or more low quality RCTs or by generally consistent findings in multiple low quality RCTs. 3) Limited evidence ‐ only one RCT (either high or low quality). 4) Conflicting evidence ‐ inconsistent findings in multiple RCTs. 5) No evidence ‐ no RCTs.
High quality RCTs were defined as RCTs that fulfilled 50% or more of the validity criteria. Findings were considered to be 'generally consistent' when at least 75% of the studies showed similar results.
We had planned to conduct, if possible, subgroup analyses for prevention for: 1) primary versus secondary prevention, 2) short‐term follow‐up (less than three months after randomisation) versus long‐term follow‐up (more than six months after randomisation). We had also planned to conduct, if possible, subgroup analyses for treatment for: 1) acute versus chronic LBP, 2) short‐term follow‐up (less than three months after randomisation) versus long‐term follow‐up (more than six months after randomisation). Due to lack of data, planned subgroup analyses were not performed.
A sensitivity analysis was conducted to evaluate the influence of different thresholds for high quality on the overall conclusions. Also, a sensitivity analysis was done in which all 'unclear' scores on internal validity items were considered 'positive'.
Results
Description of studies
Results of literature search and study selection
The search strategy in the five databases resulted in the identification of 926 articles; 189 articles from CENTRAL, 472 articles from PubMed, 188 articles from EMBASE, 66 articles from CINAHL, and 11 from Current Contents. Because 106 articles were found in two or more databases, a total of 820 articles were found to be potentially eligible. The papers of Hsieh and Pope, two papers of Dalichau and two of van Poppel appeared to be reports of the same study. Based on titles, subject headings, abstracts and journal types, eight articles were included (Dalichau 2000; Doran 1975; Gibson 2002; Hsieh 1992; Million 1981; Valle‐Jones 1992; van Poppel 1998; Walsh 1990). Screening references of articles and reviews resulted in four additional studies (Alexander 1995; Coxhead 1981; Kraus 2002; Reddell 1992). Three additional studies (Gaber 1999; Penrose 1991; Roelofs 2007) were identified by contacting experts. Nineteen articles were excluded after reading the full paper, because they did not meet the inclusion criteria. Reasons for exclusion of these studies are explained in the Characteristics excluded studies table.
In summary, seven preventive studies (Alexander 1995; Gaber 1999; Kraus 2002; Reddell 1992; Roelofs 2007; van Poppel 1998; Walsh 1990) and eight treatment studies (Coxhead 1981; Dalichau 2000; Doran 1975; Gibson 2002; Hsieh 1992; Million 1981; Penrose 1991; Valle‐Jones 1992) were included. Since the last review, two new studies on prevention (Kraus 2002; Roelofs 2007) and two new studies on treatment (Dalichau 2000; Gibson 2002) were found.
Study characteristics are summarized in the Characteristics of included studies table.
Funding sources were stated in some papers. In six studies the lumbar supports were provided by a company (Alexander 1995; Gibson 2002; Kraus 2002; Million 1981; Valle‐Jones 1992; van Poppel 1998). Seven studies did not report any funding sources (Coxhead 1981; Dalichau 2000; Doran 1975; Gaber 1999; Penrose 1991; Reddell 1992; Walsh 1990) and two clearly reported that there was no financial conflict of interest (Hsieh 1992; Roelofs 2007).
Prevention
Seven studies were identified, six published in English and one in German (Gaber 1999). None of the preventive studies included solely patients with no of history of LBP. Consequently, they all studied a combination of primary and secondary prevention of low‐back pain. Five studies reported that workers with a history of LBP were included (Gaber 1999; Kraus 2002; Reddell 1992; Roelofs 2007; van Poppel 1998); five studies reported that workers with current LBP were included (Alexander 1995; Gaber 1999; Kraus 2002; Roelofs 2007; van Poppel 1998). In one study (Alexander 1995), no information was given about the history of LBP, and in one study (Reddell 1992), no information was given about current LBP. One study did not give information about the history or current status of LBP (Walsh 1990).
The type of lumbar support and control intervention used in the preventive studies varied considerably. In five studies the participants had to wear a specific lumbar support (Gaber 1999; Kraus 2002; Reddell 1992; van Poppel 1998; Walsh 1990), and in one study (Alexander 1995) no information was given about the type of lumbar support. The participants in the study by Roelofs (Roelofs 2007) could choose one of four types of lumbar support. In all studies the subjects were prescribed to wear the lumbar support at work. Only four studies presented data on compliance (Kraus 2002; Reddell 1992; Roelofs 2007; van Poppel 1998). The compliance rate varied from 43% of the subjects who wore the belt at least half of the time (van Poppel 1998) to 97% of the subjects who wore the belt at work (Kraus 2002).
Treatment
Eight trials were identified, seven published in English and one in German (Dalichau 2000). Three studies included solely patients with chronic LBP (Dalichau 2000; Gibson 2002; Million 1981). Four studies included a mix of patients with acute, subacute and chronic LBP (Coxhead 1981; Doran 1975; Hsieh 1992; Valle‐Jones 1992). One study did not give any information about the duration of the LBP complaints of the patients (Penrose 1991). The type of lumbar supports and control interventions used in the studies varied considerably. One study reported that 'any type' of lumbar support was used (Coxhead 1981). The other studies used specific but different lumbar supports. In two studies, two types of lumbar support were compared (Gibson 2002; Million 1981).
Only four studies reported the number of hours a day the lumbar support should be worn (Hsieh 1992; Million 1981; Penrose 1991; Valle‐Jones 1992). Compliance was reported in only one study: Hsieh reported that 65% of the subjects wore the lumbar support during working hours (Hsieh 1992).
Risk of bias in included studies
The two quality assessors disagreed about 70 of the 170 validity items (42%). After one consensus meeting, all disagreements, due to reading and interpretation errors, were resolved.
The authors of the studies were informed about the methodological quality assessment. The addresses of two authors could not be traced (Doran 1975; Valle‐Jones 1992). We asked the authors if they agreed with the scores and if they could provide more information on the items that were scored as 'unclear'. The authors of five studies responded to this request (Coxhead 1981; Hsieh 1992; Million 1981; Roelofs 2007; van Poppel 1998). Seven scores were changed by this information; four unclear scores and three negative scores were changed into positive.
Overall, the methodological quality of the studies was low. Only five of the fifteen studies met our preset level for high quality of more than 50% positive criteria (Hsieh 1992; Million 1981; Roelofs 2007; van Poppel 1998; Walsh 1990). Prevalent methodological flaws were: no concealment of treatment allocation (item 2), no assessment of co‐interventions (item 4) and compliance (item 5), and no blinding of patients (item 6) and outcome assessors (item 7). See Figure 1 for details.
1.
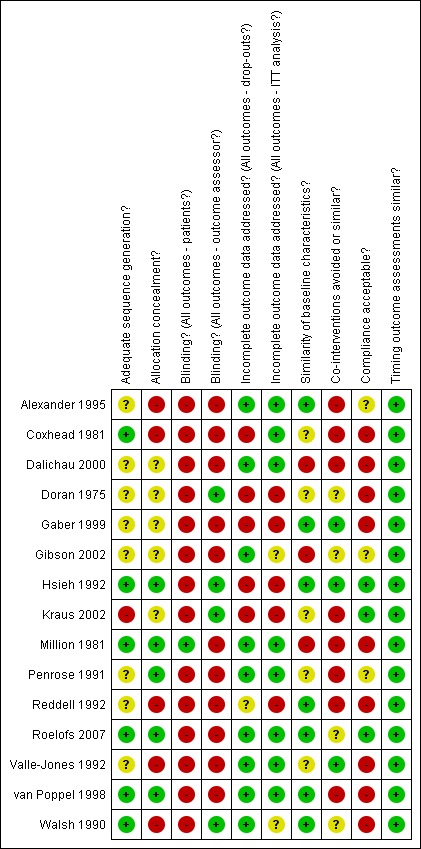
Summary of risks of bias
Effects of interventions
Clinical Relevance
Assessment of clinical relevance found that many of the trial publications supplied inadequate information. The study population was described by 67% of the publications and 80% adequately described the type of lumbar support. Clinically relevant outcomes were described as 'positive' when at least pain and functional status were reported. Just 26% of the publications reported both pain and functional status.
The size of effect for pain was considered 'clinically relevant' when pain was decreased by more than 20% at the end of the intervention period. The size of effect for functional status was considered 'clinically relevant' when functioning was improved more than 10%. The size of effect for absence of work was not pre‐defined. Only a small number of studies (13%) reported clinically relevant effects.
There was inadequate reporting of treatment benefits worth the potential harms in 80% of the studies. A small number of studies reported on the presence or absence of adverse events. Studies reported mild negative reactions to lumbar supports, such as restricted freedom of movement, too warm and uncomfortable. One study reported adverse effects: all patients with stenosis had more disabilities after wearing lumbar supports (Gibson 2002). See Table 3; Table 4 for details.
3. Clinical relevance of preventive trials.
| Studies | 1 | 2 | 3 | 4 | 5 |
| Alexander 1995 | + | + | ‐ | ‐ | ‐ |
| Gaber 1999 | ‐ | + | ‐ | ‐ | ‐ |
| Kraus 2002 | + | ? | ‐ | ‐ | ‐ |
| Reddell 1992 | + | + | ‐ | ‐ | ‐ |
| Roelofs 2007 | + | + | + | + | + |
| Van Poppel 1998 | + | + | ‐ | ‐ | ‐ |
| Walsh 1980 | ‐ | + | ‐ | ‐ | ? |
4. Clinical relevance of therapeutic trials.
| Studies | 1 | 2 | 3 | 4 | 5 |
| Coxhead 1981 | + | ‐ | ‐ | ‐ | ? |
| Dalichau 2000 | + | + | + | ‐ | ‐ |
| Doran 1975 | + | ‐ | ‐ | ‐ | ‐ |
| Gibson 2002 | ‐ | + | + | ‐ | ‐ |
| Hsieh 1992 | + | + | ‐ | ‐ | ‐ |
| Million 1981 | ‐ | + | ‐ | ? | ? |
| Penrose 1991 | ‐ | + | ‐ | ‐ | + |
| Valle‐Jones 1992 | + | + | + | + | + |
1. Effects of lumbar supports in prevention of low‐back pain
1.1 Lumbar supports versus no intervention
Five RCTs included a 'no intervention' group (Alexander 1995; Gaber 1999; Kraus 2002; Reddell 1992; van Poppel 1998). One RCT was considered to be a high quality RCT (van Poppel 1998) while the other four studies were considered to be low quality RCTs.
One RCT reported no significant differences in short‐term incidence of LBP (Alexander 1995, 60 people). Three RCTs, including the high quality study, reported no significant differences in long‐term back pain injury or incidence of LBP (Gaber 1999, 209 people; Reddell 1992, 642 people; van Poppel 1998, 312 people). One study used two control groups: one group had a safety meeting with information about low‐back health and the other group was passively followed and not informed about the study (Kraus 2002, 12,772 people). The study reported a difference in long‐term back pain injury between those who wore lumbar supports and the control group and no significant differences between those who wore lumbar support and the advice group.
One study did not find any significant difference in short‐term sick leave (Alexander 1995, 60 people). Three RCTs, including the high quality study, did not find any significant difference in long‐term sick leave (Gaber 1999, 209 people; Reddell 1992, 642 people; van Poppel 1998, 312 people) between those who wore lumbar supports and those who had no intervention.
There is moderate evidence that lumbar supports do not prevent short‐ and long‐term incidence of LBP or sick leave between those who wore lumbar supports and those who had no intervention (5 studies, 13,995 people).
1.2 Lumbar support versus other types of prevention
Two studies were identified, one high quality (van Poppel 1998, 312 people) and one low quality study (Reddell 1992, 642 people). Both RCTs used long‐term incidence of LBP and sick leave due to LBP as outcomes and compared lumbar supports with training of lifting techniques. Both trials failed to show significant differences between the intervention and control groups. There is moderate evidence that lumbar supports are not more effective than training of lifting techniques in preventing long‐term LBP and sick leave (two studies, 954 people).
1.3 Lumbar support as supplement to another type of prevention versus that other type of prevention
One high quality study compared lumbar support plus back school with a back school program alone (Walsh 1990, 82 people). The study found significant differences in the long‐term number of days lost from work because of back injury but no significant differences in the incidence of low‐back pain. There is limited evidence that lumbar supports plus back school reduce the number of days lost from work due to back injury in the long‐term more than back school alone but not the incidence of LBP (one study, 82 people).
Another, high quality study compared lumbar support plus usual care (only if an episode of LBP occurred) with usual care alone to prevent low‐back pain (Roelofs 2007, 360 people). The study found significant differences in the number of days with LBP and functional status in the long‐term, but no significant differences in long‐term sick leave. There is limited evidence that lumbar supports plus usual care reduce the number of days with LBP and improve functional status in the long‐term better than usual care alone, but are not better at reducing long‐term sick leave (one study, 360 people).
2. Effects of lumbar supports in treatment of low‐back pain
2.1 Lumbar support versus no intervention
Seven RCTs included a 'no intervention' group (Coxhead 1981; Doran 1975; Gibson 2002; Hsieh 1992; Penrose 1991; Valle‐Jones 1992). One RCT (Hsieh 1992) was considered to be a high quality RCT, while the other five were considered to be low quality RCTs. One of these studies included solely patients with chronic LBP (Gibson 2002) and five studies included a mix of patients with acute, subacute and chronic LBP (Coxhead 1981; Doran 1975; Hsieh 1992; Penrose 1991; Valle‐Jones 1992).
Chronic LBP One low quality study (Gibson 2002, 79 people) measured pain and functional status as main outcomes. The study reported no significant differences between groups. There is limited evidence that lumbar supports are not more effective than no intervention for short‐term pain reduction and improved functional status for patients with chronic LBP (one study, 79 people). Mix of acute, subacute and chronic LBP Four RCTs measured pain as a main outcome (Coxhead 1981; Doran 1975; Hsieh 1992; Valle‐Jones 1992). Only one low quality RCT (Valle‐Jones 1992, 216 people) reported a significant difference in short‐term pain in favour of the lumbar support group. The other three studies, including the high quality RCT, reported no significant differences (Coxhead 1981, 334 people; Doran 1975, 456 people; Hsieh 1992,164 people). There is moderate evidence that lumbar supports are not more effective than no intervention for short‐term pain reduction for patients with a mix of (sub)acute and chronic LBP (four studies, 1170 people).
Two low quality studies (Coxhead 1981, 334 people; Doran 1975, 456 people) measured overall improvement as the main outcome. Both studies reported no significant short‐term differences between groups. There is moderate evidence that lumbar supports are not more effective for short‐term overall improvement than no intervention for patients with a mix of (sub)acute and chronic LBP (two studies, 790 people).
Return‐to‐work was measured as a main outcome in two low quality studies (Coxhead 1981; Valle‐Jones 1992). One study (Coxhead 1981, 334 people) reported no significant difference in the short term between the groups, while the other (Valle‐Jones 1992, 216 people) found a significant difference in favour of the lumbar support group. There is conflicting evidence whether patients with a mix of (sub)acute and chronic LBP who use a lumbar support as treatment return to work faster than those who received no intervention (two studies, 550 people).
Three studies, one high (Hsieh 1992, 164 people) and two low quality RCTs (Penrose 1991, 30 people; Valle‐Jones 1992, 216 people), measured functional status as a main outcome. The studies reported significant differences in short‐term functional status between the groups. There is moderate evidence that lumbar supports are more effective at improving short‐term functional status than no intervention for patients with a mix of (sub)acute and chronic LBP (three studies, 410 people).
2.2 Lumbar support versus other types of treatment
Three trials compared lumbar supports with some type of treatment for LBP and included a mix of patients with acute, subacute and chronic LBP (Coxhead 1981; Doran 1975; Hsieh 1992). One study compared corset with traction, manipulation and exercises (Coxhead 1981,334 people), one study compared corset with physiotherapy and manipulation (Doran 1975, 456 people), and another study compared corsets with transcutaneous muscle stimulation (TMS) and manipulation (Hsieh 1992, 164 people). Only one trial was considered a high quality RCT (Hsieh 1992).
The three studies reported no significant differences in short‐term pain between any of the groups. There is moderate evidence that for patients with a mix of (sub)acute and chronic LBP, lumbar supports are not more effective for short‐term pain reduction than other types of treatment (three studies, 954 people).
Two low quality studies (Coxhead 1981, 334 people; Doran 1975, 456 people) reported no significant differences in short‐term and intermediate‐term overall improvement. There is moderate evidence that for patients with a mix of (sub)acute and chronic LBP, lumbar supports are not more effective for short‐term and intermediate‐term overall improvement than other types of treatment (two studies, 790 people).
One low quality RCT (Coxhead 1981, 334 people) reported no significant differences in short‐term return‐to‐work between the groups. There is limited evidence that for patients with a mix of (sub)acute and chronic LBP, lumbar supports are not more effective for short‐term return‐to‐work than corsets and traction, manipulation, or exercises (one study, 334 people).
One high quality study (Hsieh 1992, 164 people) used two different instruments for measuring back pain‐specific functional status. The Roland‐Morris Disability Questionnaire showed a significant difference between the lumbar support and the soft tissue massage group. However, the revised Oswestry Scale showed no significant difference between the groups. The study authors concluded that differences had shown up between the two measurement tools because the Roland‐Morris is more sensitive to change than the Oswestry. Therefore, there is conflicting evidence about whether lumbar supports improve back pain‐specific functional status more than soft tissue massage for patients with a mix of (sub)acute and chronic LBP (one study, 164 people).
2.3 Lumbar support as supplement to another type of treatment versus that other type of treatment
One low quality RCT (Dalichau 2000, 63 people) compared a muscle strengthening program and elastic lumbar support with an elastic lumbar support for patients with chronic LBP. The study reported no significant differences in short‐term and long‐term pain and back‐specific functional status. There is limited evidence that lumbar supports as a supplement to a muscle strengthening program are not more effective for short‐ and long‐term pain reduction and improved back pain‐specific functional status than a muscle training program alone for patients with chronic LBP (one study, 63 people).
2.4 Comparison of different types of lumbar supports
One low quality RCT compared two different types of lumbar support, a flexible corset and a semi‐rigid corset, for patients with chronic LBP (Gibson 2002, 79 people). The study reported no significant differences in short‐term pain and functional status. There is limited evidence that a flexible corset is not more effective than a semi‐rigid corset for short‐term pain reduction and improved functional status for patients with chronic LBP (one study, 79 people).
Another low quality RCT also compared two different types of lumbar support, with and without spinal support, for patients with chronic LBP (Million 1981, 19 people). The study reported significant differences in short‐term pain and functional status in favour of the lumbar corset with back support. There is limited evidence that a lumbar corset with back support is more effective for short‐term pain reduction and improved back‐specific functional status than a lumbar support alone for patients with chronic LBP (one study, 19 people).
Sensitivity Analyses
A sensitivity analysis was conducted to evaluate the influence of different thresholds for high quality on the overall conclusions. A sensitivity analysis was also done in which all 'unclear' scores on internal validity items were considered 'positive'.
1. Different thresholds for high quality
When using a threshold of 40% for studies on prevention, one more RCT was considered high quality (Alexander 1995), resulting in a total of four high quality RCTs (Alexander 1995; Roelofs 2007; van Poppel 1998; Walsh 1990). Consequently, the conclusion on the comparison of lumbar supports versus 'no intervention' changed from 'moderate evidence to 'strong evidence that lumbar supports do not prevent the incidence of LBP or reduce the length of sick leave.
When using a threshold of 40% for studies on treatment, two more RCTs were also considered high quality (Penrose 1991; Valle‐Jones 1992). For the comparisons of lumbar supports to 'no intervention', the conclusions on pain reduction, overall improvement and return‐to‐work were still the same. The conclusion on improved functional status changed from 'moderate evidence' to 'strong evidence' that lumbar supports are effective for improving functional status in the short term.
When using a threshold of 60% for studies on prevention, one study (Walsh 1990) changed from a high quality to a low quality RCT, but the results and conclusions did not change. Using a threshold of 60% for studies on treatment, results and conclusions did not change.
2. All 'unclear' scores 'positive'
When all 'unclear' scores were assumed to be 'positive', five studies on prevention (Alexander 1995; Gaber 1999; Roelofs 2007; van Poppel 1998; Walsh 1990) and seven studies on treatment (Dalichau 2000; Doran 1975; Gibson 2002; Hsieh 1992; Million 1981; Penrose 1991; Valle‐Jones 1992) were considered high quality RCTs at the 50% cut‐off.
The conclusion for the comparison 'lumbar support versus no intervention' changed from 'moderate evidence' to 'strong evidence' that lumbar supports do not prevent the incidence of LBP or the length of sick leave. The conclusions for the comparison 'lumbar support versus no intervention' on overall improvement and return‐to‐work did not change. The conclusion for functional status changed from 'moderate evidence' to 'strong evidence' that lumbar supports are effective for short‐term improvement of functional status.
Discussion
Selection bias
Despite the extensive search strategy used to identify all relevant studies on the effectiveness of lumbar supports, some studies may have been missed. The keywords used in the missing studies may not have been in accordance with those used in the search strategy of the present review, or the journals may have been indexed in other databases. However, the risk of selection bias is probably low. It is unlikely that we missed any study, because we supplemented the search strategy with checking references and contacting experts.
Methodological quality
The two review authors who assessed the methodological quality were not blinded for authors, journal or institution. The potential bias caused by the non‐blinded quality assessment was expected to be low. First, neither review authors had a conflict of interest. This means that the review authors did not have any (financial or other) interest in positive or negative results. Second, one review author was an expert in the field of LBP and very familiar with the literature. Blinding this review author did not seem feasible. The other review author was not familiar with the literature and blinding this review author did not seem necessary, because this review author was new to the field. Furthermore, we presented the methodological criteria list, the operationalization of criteria, and the final results of the assessment, so readers can determine whether they agree with the conclusions.
The methodological quality was defined by the internal validity criteria, which refer to characteristics of the study that might be related to bias. The methodological quality of the studies included in our review was rather low. Only five of the fifteen studies met our pre‐set level for high quality of more than 50% positive scores. Compared to the previous review, the methodological quality improved very little. The quality changed somewhat because non‐randomised trials that were included in the first review were deleted from this update, but there was no clear improvement in methodological quality. Prevalent methodological flaws were: no concealment of treatment allocation, no assessment of co‐interventions, compliance, no blinding of patients or outcome assessors.
Although the authors of fifteen studies claimed that their study design was a randomised controlled trial, an appropriate method of randomisation and concealment of treatment allocation was described in only three papers. Most studies did not report data on co‐interventions or compliance. Two studies reported low (Reddell 1992; van Poppel 1998) and three reported high compliance (Hsieh 1992, Kraus 2002, Roelofs 2007). Compliance is a confounding factor when studying the effectiveness of lumbar supports. Because compliance with wearing lumbar supports is generally low and a matter of self‐selection, it is difficult to be certain of their real effectiveness.
Blinding of subjects is difficult in trials on the effectiveness of lumbar supports. Only one study succeeded in blinding the patients (Million 1981). Even more important should be blinding of the outcome assessor. However, only three of the thirteen studies reported the use of a blinded outcome assessor.
The validity, reliability and responsiveness of outcome measures were often not reported. Therefore, it is unclear whether the instruments actually measured what they were supposed to measure, whether they measured with consistency, and whether they were able to measure change over time.
Levels of evidence
In this review, we refrained from statistical pooling because of the heterogeneity of study populations, control interventions and outcome measures. The conclusions on the effectiveness of lumbar supports were based on a qualitative analysis of the strength of scientific evidence (van Tulder 2003). We had pre‐defined the levels of evidence; consistency was defined as 75% or more of the trials showing effects in the same direction. High quality was defined as meeting five or more of the 10 quality items. The classification of the comparisons to a level of evidence was sometimes arbitrary. When results of several studies regarding a comparison did not entirely agree with each other, it was difficult to decide whether these results should be entitled as 'generally consistent findings' or as 'inconsistent findings'. For example, if all trials were positive, it is obvious that the findings are consistent, but are findings also consistent if five out of seven trials are positive or if four out of seven are positive? We have presented extensive tables, so readers can determine for themselves if they agree with the classification of evidence in this review.
Effectiveness of lumbar supports in prevention of low‐back pain
Seven preventive RCTs (14,435 people) were included in this systematic review. The results showed that there is moderate evidence that lumbar supports do not prevent short‐ or long‐term LBP or sick leave more effectively than no intervention; and that there is moderate evidence that lumbar supports are not more effective than training in lifting techniques in preventing long‐term LBP and sick leave. Addition of two recent RCTs (Kraus 2002; Roelofs 2007) and removal of CCTs did not change the results of the previous systematic review (Jellema 2001; Van Tulder 2000) and this updated review still supports the original conclusions. The results of this systematic review are also in line with the European guidelines for prevention of low‐back pain (Burton 2005). Based on various reviews (Ammendolia 2005; Linton 2001; van Poppel 2004), these guidelines recommend that the general population and workers do not wear lumbar supports to prevent LBP.
Effectiveness of lumbar supports in treatment of low‐back pain
Eight therapeutic RCTs (1361 people) were included in this systematic review. The results showed that there is limited evidence that lumbar supports are not more effective than no intervention for short‐term pain reduction and improved functional status for patients with chronic LBP. The results are still in line with the previous systematic review (Jellema 2001; Van Tulder 2000). Addition of two recent RCTs and removal of CCTs did not change the conclusions. The results of this systematic review are also in line with the European guidelines for the management of chronic low‐back pain that do not recommend using lumbar supports (Airaksinen 2006).
No trial specifically evaluated lumbar supports for acute LBP. There was conflicting evidence on the effectiveness of lumbar supports as treatment compared to no intervention or other interventions for a mixed population with acute, subacute and chronic LBP.
Authors' conclusions
Implications for practice.
There was moderate evidence that lumbar supports are not more effective than no intervention or training in preventing low‐back pain, and conflicting evidence whether lumbar supports are effective as supplement to another preventive intervention. It is still unclear if lumbar supports are more effective than no or other interventions for treatment of low‐back pain.
Implications for research.
Future trials should be of high quality and special attention should be paid to adequate compliance. Future trials should attempt to quantify effects in patient subgroups, particularly acute, subacute, and chronic. Also, they should focus on primary and secondary prevention separately. Outcomes are likely to be different for each of these groups. Outcomes may also be different for different types of supports and may be dose‐related.
What's new
| Date | Event | Description |
|---|---|---|
| 19 January 2011 | Amended | Contact details updated. |
History
Protocol first published: Issue 4, 1999 Review first published: Issue 3, 2000
| Date | Event | Description |
|---|---|---|
| 23 November 2009 | Amended | Contact details updated. |
| 3 June 2008 | Amended | Converted to new review format. |
| 19 February 2008 | New citation required but conclusions have not changed | Conclusions: There was moderate evidence that lumbar supports are not more effective than no intervention or training in prevention of low‐back pain, and conflicting evidence whether lumbar supports are effective as supplement to another preventive intervention. It is still unclear if lumbar supports are more effective than no or other interventions for treatment of low‐back pain. |
| 30 December 2006 | New search has been performed | There are some differences between the previous systematic review (Van Tulder 2000; Jellema 2001) and this update: Changes in this updated review include: ‐ Only RCTs are included; non‐randomized trials that were included in the previous review were excluded from this update (Anderson 1993; Thompson 1994). ‐ Two new studies on prevention (Kraus 2002; Roelofs 2007) and two new studies on treatment (Dalichau 2000; Gibson 2002) were found. ‐ Assessment of clinical relevance is new. ‐ A new comparison was added: lumbar support as supplement to another type of treatment versus that other type of treatment. |
Acknowledgements
We wish to thank Lex Bouter and acknowledge the contributions made by him and the late Alf Nachemson as members of the review team for the original review (Jellema 2001; Van Tulder 2000).
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Alexander 1995.
| Methods | RCT | |
| Participants | Subjects: 60 health care workers; 48 women and 12 men. Mean age 37 years. Exclusion criteria: subjects who have had back surgery, current workers' compensation claims, cardiovascular problems or were pregnant. Authors did not report whether workers with LBP or a past history of LBP were included in the study. | |
| Interventions | Preventive intervention:
1) Back belt group (n=30). Belt use at work for 3 months. Control intervention: 2) No intervention (n=30) |
|
| Outcomes | Perception of physical pain and work related back injuries. No significant differences after 3 months. | |
| Notes | The most common complaints: belt rode up, changed position and increased perspiration. No data available regarding compliance. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Unclear from text |
| Allocation concealment? | High risk | C ‐ Inadequate |
| Blinding? All outcomes ‐ patients? | High risk | |
| Blinding? All outcomes ‐ outcome assessor? | High risk | |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs? | Low risk | |
| Incomplete outcome data addressed? All outcomes ‐ ITT analysis? | Low risk | |
| Similarity of baseline characteristics? | Low risk | |
| Co‐interventions avoided or similar? | High risk | |
| Compliance acceptable? | Unclear risk | No data available regarding compliance. |
| Timing outcome assessments similar? | Low risk | |
Coxhead 1981.
| Methods | RCT; factorial design | |
| Participants | Subjects: 334 patients with pain of sciatic distribution with or without LBP; 185 men and 149 women. Mean age 41.9, mean duration of symptoms 14.3 weeks. Exclusion criteria: specific LBP, patients undergone trunk, lower‐limb or spinal surgery within the previous three months and pregnant & postpartum women. | |
| Interventions | Treatment intervention:
1) Fabric made lumbar support, 4 weeks (n=124). No data on number of hours / day. Control interventions: 2) No lumbar support (n=168). |
|
| Outcomes | Pain, overall improvement and turn to work / normal activities. No differences after 4 weeks, 4 months and 16 months. | |
| Notes | 334 patients entered the study, 12 were later found ineligible. Of these 322 patients, 292 were assessed at 4 weeks. At 4 months 250 patients and at 16 months 258 patients were assessed. No data available regarding compliance. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | |
| Allocation concealment? | High risk | C ‐ Inadequate |
| Blinding? All outcomes ‐ patients? | High risk | |
| Blinding? All outcomes ‐ outcome assessor? | High risk | |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs? | High risk | |
| Incomplete outcome data addressed? All outcomes ‐ ITT analysis? | Low risk | |
| Similarity of baseline characteristics? | Unclear risk | Unclear from text |
| Co‐interventions avoided or similar? | High risk | |
| Compliance acceptable? | High risk | |
| Timing outcome assessments similar? | Low risk | |
Dalichau 2000.
| Methods | RCT | |
| Participants | Subjects: 63 male with LBP, mean age 38.4 and 34 male without LBP. Inclusion criteria: LBP for more than 2 years and degenerative changes in lumbar region. No exclusion criteria. | |
| Interventions | Treatment intervention:
1) training and lumbar support (n = 21)
Use of lumbar support 8 weeks. Control intervention: 2) Training (n = 21) 3) No intervention (n = 21) 8 weeks. |
|
| Outcomes | Pain, back specific functional status, muscle flexibility, coordination flexion. Differences after 8 weeks and 6 months between training groups and control group. No differences between training plus lumbar support and training. | |
| Notes | No data available regarding compliance. No statistical test of effect between groups for pain and functional status. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Unclear from text |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Blinding? All outcomes ‐ patients? | High risk | |
| Blinding? All outcomes ‐ outcome assessor? | High risk | |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs? | Low risk | |
| Incomplete outcome data addressed? All outcomes ‐ ITT analysis? | Low risk | |
| Similarity of baseline characteristics? | High risk | |
| Co‐interventions avoided or similar? | High risk | |
| Compliance acceptable? | High risk | No data available regarding compliance. |
| Timing outcome assessments similar? | Low risk | |
Doran 1975.
| Methods | RCT | |
| Participants | Subjects: 456 patients with non‐specific LBP; 211 women, 245 men. Age 20‐50, duration of symptoms: less than a week to more than 6 months. Inclusion criteria: 1) age 20‐50 years, 2) painful limitation of movement in the lumbar spine and 3) suitable for any treatment. | |
| Interventions | Treatment interventions:
1) Corset (= 109), any type, 3 weeks. No data on number of hours/day. Control interventions: 2) Manipulation (n= 116), 2 treatments/ wk 3) Physiotherapy (n= 114), any treatment except manipulation, 2 treatments/wk 4) Analgesic tablets (n=113) 2 paracetamol / 4 hours. |
|
| Outcomes | Pain, overall assessment by the doctor. No significant differences after 3 and 6 weeks, and 3 and 12 months. | |
| Notes | 456 patients entered the trial. At baseline 452 patients were assessed. After 3 weeks 395 patients were assessed, after 6 weeks 340, after 3 month 335 and after 12 month 262 patients were assessed. No data available regarding compliance. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Unclear from text |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Blinding? All outcomes ‐ patients? | High risk | |
| Blinding? All outcomes ‐ outcome assessor? | Low risk | |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs? | High risk | |
| Incomplete outcome data addressed? All outcomes ‐ ITT analysis? | High risk | |
| Similarity of baseline characteristics? | Unclear risk | Unclear from text |
| Co‐interventions avoided or similar? | Unclear risk | Unclear from text |
| Compliance acceptable? | High risk | |
| Timing outcome assessments similar? | Low risk | |
Gaber 1999.
| Methods | RCT | |
| Participants | Subjects: 209 male workers whose jobs included manual material handling at an airport. The majority of the workers (77%) had no or only mild LBP at the start of the study. | |
| Interventions | Preventive intervention:
1) Synthetic lumbar support (n=118), lumbar support use at work for 12 months. Control intervention: 2) No intervention (n=91) |
|
| Outcomes | Pain score, sick leave due to LBP and medicine intake due to LBP. No differences in pain and sick leave; less medication intake in lumbar support group. | |
| Notes | Of the 267 workers included at the start of the study only 209 have finished the study. Only data of these subjects is presented in the study. No data on compliance. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Unclear from text |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Blinding? All outcomes ‐ patients? | High risk | |
| Blinding? All outcomes ‐ outcome assessor? | High risk | |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs? | High risk | |
| Incomplete outcome data addressed? All outcomes ‐ ITT analysis? | High risk | |
| Similarity of baseline characteristics? | Low risk | |
| Co‐interventions avoided or similar? | Low risk | |
| Compliance acceptable? | High risk | |
| Timing outcome assessments similar? | Low risk | |
Gibson 2002.
| Methods | RCT | |
| Participants | Subject: 79 patients with chronic LBP; 27 male, 52 female. Mean age men: 58.8, female: 63.9. Exclusion criteria: surgery in preceding 12 months, treatment in hospital, over 120 kg., younger than 30 years and history of malignancy. | |
| Interventions | Treatment intervention:
1) Flexible corset (n = not reported)
2) Semi‐rigid corset (n = not reported) Control intervention: 3) lingerie (n = not reported, only female) Treatment use two months. No data on numbers of hours a day. |
|
| Outcomes | Pain, back specific functional status, satisfaction, radiographs. After 2 months there are no differences between the corsets. Women rated the lingerie significant better on comfort than the other corsets. | |
| Notes | No data available regarding compliance. 79 were recruited. Comparative data were obtained from 64 patients. No data regarding duration of LBP. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Unclear from text |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Blinding? All outcomes ‐ patients? | High risk | |
| Blinding? All outcomes ‐ outcome assessor? | High risk | |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs? | Low risk | |
| Incomplete outcome data addressed? All outcomes ‐ ITT analysis? | Unclear risk | Unclear from text |
| Similarity of baseline characteristics? | High risk | |
| Co‐interventions avoided or similar? | Unclear risk | Unclear from text |
| Compliance acceptable? | Unclear risk | No data available regarding compliance. |
| Timing outcome assessments similar? | Low risk | |
Hsieh 1992.
| Methods | RCT | |
| Participants | Subjects: 164 patients, 62 women and 102 men with non‐specific LBP and no sciatica. Median age 32 and mean duration of complaints between 3 weeks and 6 months. Inclusion criteria: 1) age 18‐55 years, 2) LBP between 3 weeks and 6 months duration, 3) good health. | |
| Interventions | Treatment intervention:
1) Corset (n=29),
lumbosacral canvas corset with metal stays in the back. Corset use during waking hours, 3 weeks. Control interventions: 2) Spinal manipulation (n=70), 3 times / week. 3) Soft tissue massage (n=37), 3 times / week. 4) TMS (n=28), unit should be worn for 8 hours / day. |
|
| Outcomes | Pain, functional status. No differences in pain. Functional status only after 4 weeks better compared to massage, not to manipulation and TMS. | |
| Notes | 88% of the original patients completed the assessments at baseline and at 4 weeks. Data of RDQ and revised Oswestry are reported by Hsieh (1992) for a subgroup of 83 patients from the study population of Pope. Compliance: 65% wore the belt more than 7 hours a day during the intervention period. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | |
| Allocation concealment? | Low risk | A ‐ Adequate |
| Blinding? All outcomes ‐ patients? | High risk | |
| Blinding? All outcomes ‐ outcome assessor? | Low risk | |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs? | High risk | |
| Incomplete outcome data addressed? All outcomes ‐ ITT analysis? | High risk | |
| Similarity of baseline characteristics? | Low risk | |
| Co‐interventions avoided or similar? | Low risk | |
| Compliance acceptable? | Low risk | Compliance: 65% wore the belt more than 7 hours a day during the intervention period. |
| Timing outcome assessments similar? | Low risk | |
Kraus 2002.
| Methods | RCT | |
| Participants | Subjects: 12772 home attendants, 12408 female and 364 male. No more information about inclusion and exclusion criteria. | |
| Interventions | Preventive intervention:
1) lumbar support (n=3837), 28 months. Control interventions: 2) 1 safety meeting with information about low back health (n=4300) 3) no intervention (n=4635) |
|
| Outcomes | Back injury rates. The lumbar support group had less back injuries than the information group (not significant) and no intervention group (significant). | |
| Notes | A cluster‐randomised trial design was chosen: 9 agencies were chosen a priori and randomised. Few data available regarding baseline and differences between groups. Compliance per month: 80 ‐ 97%. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | High risk | |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Blinding? All outcomes ‐ patients? | High risk | |
| Blinding? All outcomes ‐ outcome assessor? | Low risk | |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs? | High risk | |
| Incomplete outcome data addressed? All outcomes ‐ ITT analysis? | High risk | |
| Similarity of baseline characteristics? | Unclear risk | Few data available regarding baseline and differences between groups. |
| Co‐interventions avoided or similar? | High risk | |
| Compliance acceptable? | Low risk | Compliance per month: 80 ‐ 97%. |
| Timing outcome assessments similar? | Low risk | |
Million 1981.
| Methods | RCT | |
| Participants | Subjects: 19 patients, 13 women and 6 men. Mean age 47.1. Inclusion criteria: 1) over 18 years of age, 2) suffering from chronic non‐specific LBP > 6 months, 3) not responding to any form of treatment. | |
| Interventions | Treatment intervention:
1) Corset and lumbar support (n=9). Support is of rigid material. Corset use during the day, 8 weeks. Control intervention: 2) Corset (n=10), lumbosacral corset use during the day, 8 weeks. |
|
| Outcomes | Subjective and objective index. Rigid support better subjective index after 4 and 8 weeks. | |
| Notes | The subjective index is an overall measurement of the severity of symptoms and of the interference of these symptoms with normal activities. The objective index is an overall measurement of the straight leg raising and of spinal movements. No data on compliance. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | |
| Allocation concealment? | Low risk | A ‐ Adequate |
| Blinding? All outcomes ‐ patients? | Low risk | |
| Blinding? All outcomes ‐ outcome assessor? | High risk | |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs? | Low risk | |
| Incomplete outcome data addressed? All outcomes ‐ ITT analysis? | Low risk | |
| Similarity of baseline characteristics? | High risk | |
| Co‐interventions avoided or similar? | High risk | |
| Compliance acceptable? | High risk | No data on compliance. |
| Timing outcome assessments similar? | Low risk | |
Penrose 1991.
| Methods | RCT | |
| Participants | Subjects: 30 patients, 8 women and 22 men. Mean age 34 years (range 19 ‐ 61 years). Patients were diagnosed as having muscular strain/sprain of the lower back by an orthopedic‐neurologic examination. No information available on mean duration of complaints. | |
| Interventions | Treatment intervention:
1) Pneumatic lumbar support (n=15). Lumbar support use during 6 hours / day, 5 days / week, 6 weeks. Control intervention: 2) No intervention. |
|
| Outcomes | Pain index; lumbar supports better after 1 hour, 3 weeks and 6 weeks. | |
| Notes | No data on compliance. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Unclear from text |
| Allocation concealment? | Low risk | A ‐ Adequate |
| Blinding? All outcomes ‐ patients? | High risk | |
| Blinding? All outcomes ‐ outcome assessor? | High risk | |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs? | Low risk | |
| Incomplete outcome data addressed? All outcomes ‐ ITT analysis? | Low risk | |
| Similarity of baseline characteristics? | Unclear risk | Unclear from text |
| Co‐interventions avoided or similar? | High risk | |
| Compliance acceptable? | Unclear risk | No data on compliance. |
| Timing outcome assessments similar? | Low risk | |
Reddell 1992.
| Methods | RCT | |
| Participants | Subjects: 642 fleet service clerks; 70 women, 572 men. Age range: 19‐67 years. 26% of 642 subjects had suffered a previous back injury and 56% a previous back pain. No data available regarding subjects with current LBP. | |
| Interventions | Preventive intervention:
1) Weightlifting belt (n=145), belt use at work, 8 months.
2) Belt plus training class (n=127), belt use at work and 1 hour training class on spine anatomy and body mechanics. Control intervention: 3) Training class (n=122), 1 hour training class. 4) No intervention (n=248). |
|
| Outcomes | Lumbar injuries, lost work days case lumbar injury, restricted work days, case lumbar injury, compensation cost. No significant differences after 8 months. | |
| Notes | Of the 896 clerks selected to participate in this study 642 were located and interviewed at the end of 8 months. Only data of these subjects is presented in the article. Compliance: 58% stopped using it before the end of 8 months. Complaints: heat production around the waist, the belt rides up and pinches ribs. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Unclear from text |
| Allocation concealment? | High risk | C ‐ Inadequate |
| Blinding? All outcomes ‐ patients? | High risk | |
| Blinding? All outcomes ‐ outcome assessor? | High risk | |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs? | Unclear risk | Unclear from text |
| Incomplete outcome data addressed? All outcomes ‐ ITT analysis? | High risk | |
| Similarity of baseline characteristics? | Low risk | |
| Co‐interventions avoided or similar? | High risk | |
| Compliance acceptable? | High risk | Compliance: 58% stopped using it before the end of 8 months. |
| Timing outcome assessments similar? | Low risk | |
Roelofs 2007.
| Methods | RCT | |
| Participants | Subjects: 360 home workers with non‐specific LBP or two or more episodes of LBP in past 12 moths; 352 female, 8 male. Mean age 41.7 years. | |
| Interventions | Preventive intervention:
1) lumbar support and usual care (n=183), lumbar support use on those working days they expected LBP, for 12 months. Control intervention: 2) usual care |
|
| Outcomes | Severity of LBP, Number of days LBP, functional status, sick leave rates after one year. The intervention group had less of LBP, better functional status and significant less number days of LBP. No differences in sick‐leave. | |
| Notes | 78% wore the lumbar support at least on third of the total days LBP | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | |
| Allocation concealment? | Low risk | A ‐ Adequate |
| Blinding? All outcomes ‐ patients? | High risk | |
| Blinding? All outcomes ‐ outcome assessor? | High risk | |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs? | Low risk | |
| Incomplete outcome data addressed? All outcomes ‐ ITT analysis? | Low risk | |
| Similarity of baseline characteristics? | Low risk | |
| Co‐interventions avoided or similar? | Unclear risk | Unclear from text |
| Compliance acceptable? | Low risk | 78% wore the lumbar support at least on third of the total days LBP |
| Timing outcome assessments similar? | Low risk | |
Valle‐Jones 1992.
| Methods | RCT | |
| Participants | Subjects: 216 patients with non‐specific LBP; 97 women, 113 men and 6 'unknown'. Mean age 43, median duration of symptoms 11 days. Inclusion criteria: 1) first episode of non‐specific LBP, 2) chronic non‐specific LBP, 3) acute exacerbation of a longer‐standing problem. | |
| Interventions | Treatment intervention:
1) Back support (n=111), elasticised with an attached silicone rubber pad of special shape, 3 weeks. Control intervention: 2) Standard therapy: advice on rest and lifestyle (n=105). |
|
| Outcomes | Pain, limitation of activity, overall improvement, ability to work and use of analgesics; all significantly better in lumbar support group after 3 weeks. | |
| Notes | No data on compliance. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Unclear from text |
| Allocation concealment? | High risk | C ‐ Inadequate |
| Blinding? All outcomes ‐ patients? | High risk | |
| Blinding? All outcomes ‐ outcome assessor? | High risk | |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs? | Low risk | |
| Incomplete outcome data addressed? All outcomes ‐ ITT analysis? | Low risk | |
| Similarity of baseline characteristics? | Unclear risk | Unclear from text |
| Co‐interventions avoided or similar? | Low risk | |
| Compliance acceptable? | High risk | No data on compliance |
| Timing outcome assessments similar? | Low risk | |
van Poppel 1998.
| Methods | RCT | |
| Participants | Subjects: 312 workers whose jobs included manual material handling. Workers who had a permanent partial work disability were excluded. Mean age 35.1. 172 subjects with previous LBP, 49 subjects with LBP at baseline. | |
| Interventions | Preventive interventions:
1) Lumbar support (n=83), 6 months.
2) Lumbar support use at work plus education (n=70), 6 months. Control intervention: 3) Education: 5 hrs lifting instructions (n=82) 4) No intervention (n=77) |
|
| Outcomes | LBP incidence, sick leave due to back pain; no differences after 6 months. | |
| Notes | A total of 312 workers were randomised of whom 282 were available for the 6‐month follow‐up. Compliance with wearing the lumbar support at least half of the time was 43%. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | |
| Allocation concealment? | Low risk | A ‐ Adequate |
| Blinding? All outcomes ‐ patients? | High risk | |
| Blinding? All outcomes ‐ outcome assessor? | High risk | |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs? | Low risk | |
| Incomplete outcome data addressed? All outcomes ‐ ITT analysis? | Low risk | |
| Similarity of baseline characteristics? | Low risk | |
| Co‐interventions avoided or similar? | High risk | |
| Compliance acceptable? | High risk | Compliance with wearing the lumbar support at least half of the time was 43%. |
| Timing outcome assessments similar? | Low risk | |
Walsh 1990.
| Methods | RCT | |
| Participants | Subjects: 90 male warehouse workers. Individuals currently being treated for back pain or back injury were excluded, although those with a prior history of back injury were not excluded. Mean age 29 years. | |
| Interventions | Preventive intervention:
1) A lumbosacral orthosis at work plus back school: a 1‐hr training session on back pain prevention and body mechanics, 6 months (n=30). Control intervention: 2) Back school (n=30), 1‐hr training session. 3) No intervention (n=30). |
|
| Outcomes | Work injury incidence, productivity, use of health care services, days lost from work by back injury. Days lost from work significantly better in lumbar support group. | |
| Notes | A total of 90 workers were randomly assigned. Follow‐up was obtained at 6 months from 82 workers. Only the data of these 82 workers is presented in the article. No data on compliance. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | |
| Allocation concealment? | High risk | C ‐ Inadequate |
| Blinding? All outcomes ‐ patients? | High risk | |
| Blinding? All outcomes ‐ outcome assessor? | Low risk | |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs? | Low risk | |
| Incomplete outcome data addressed? All outcomes ‐ ITT analysis? | Unclear risk | Unclear from text |
| Similarity of baseline characteristics? | Low risk | |
| Co‐interventions avoided or similar? | Unclear risk | Unclear from text |
| Compliance acceptable? | High risk | No data on compliance. |
| Timing outcome assessments similar? | Low risk | |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Amudsen 1982 | Not RCT |
| Anderson 1993 | No randomisation. |
| Carr 2003 | Patients were pregnant. |
| Celestini 2005 | No contrast for lumbar supports. |
| Garg 1992 | Not RCT |
| Hamonet 1993 | Not RCT |
| Iwamoto 2004 | No contrast for lumbar supports. |
| Jellema 2002 | No contrast for lumbar supports. |
| Jonai 1997 | Not RCT |
| Langford 2005 | Magnet, no lumbar support |
| Larsson 1980 | No contrast for lumbar supports. |
| Marty 1998 | No contrast for lumbar support. |
| Monticone 2004 | No contrast for lumbar supports. |
| Spratt 1993 | No contrast for lumbar support. |
| Thompson 1994 | Not RCT |
| Toda 2002 | No randomisation |
| Wassell 2000 | No randomisation. |
Contributions of authors
Petra Jellema and Maurits van Tulder identified and selected studies in the original review. Ingrid van Duijvenbode and Maurits van Tulder identified and selected additional studies for this update.
Petra Jellema and Maurits van Tulder assessed the methodological quality of studies in the original review. Ingrid van Duijvenbode and Maurits van Tulder assessed the methodologic quality and clinical relevance of additional studies for this update.
Petra Jellema performed the data extraction of studies in the original review, Ingrid van Duijvenbode for the update.
Petra Jellema, Mireille van Poppel and Maurits van Tulder conducted the data analyses in the original review; Ingrid van Duijvenbode and Maurits van Tulder for the update.
All authors were involved in writing of the protocol and final review.
Declarations of interest
One author (Mireille van Poppel) has published a randomised trial on prevention of back pain that was included in this review (van Poppel 1998). She was not involved in any decision regarding selection, quality assessment, data extraction or analysis of this trial. Two authors (Maurits van Tulder, Mireille van Poppel) are authors of another included trial (Roelofs 2007). Neither was involved in any decision regarding selection, quality assessment, data extraction or analysis of this trial.
One author (Maurits van Tulder) is co‐editor of the Cochrane Back Review Group. Editors are required to conduct at least one Cochrane review. This requirement ensures that editors are aware of the processes and commitment needed to conduct reviews. None of the editors are first authors. This involvement does not seem to be a source of conflict of interest in the Back Review Group. Any editor who is a review author is excluded from editorial decisions on the review in which they are contributors.
Edited (no change to conclusions)
References
References to studies included in this review
Alexander 1995 {published data only}
- Alexander A, Woolley SM, Bisesi M, Schaub E. The effectiveness of back belts on occupational back injuries and worker perception. Professional Safety 1995;September:22‐7. [Google Scholar]
Coxhead 1981 {published data only}
- Coxhead CE, Inskip H, Meade TW, North WRS, Troup JDG. Multicentre trial of physiotherapy in the management of sciatic symptoms. Lancet 1981;i:1065‐8. [DOI] [PubMed] [Google Scholar]
Dalichau 2000 {published data only}
- Dalichau S, Scheele K. [Auswirkungen elastischer lumbalstutzgurte auf den effect eines muskeltrainingsprogrammes fur patienten mit chronischen ruckenschmerzen]. Z Orthop 2000;138:8‐16. [DOI] [PubMed] [Google Scholar]
- Dalichau S, Scheele K. The effectiveness of a muscle training program for chronic back pain, using a functional orthosis [Wirksamkeit eines muskeltrainingsprogramms in der therapie chronischer ruckenschmerzen bei verwendung funktioneller orthesen]. Krankengymnastik: Zeitschrift fur physiotherpeuten 2004;56:414. [Google Scholar]
Doran 1975 {published data only}
- Doran DML, Newell DJ. Manipulation in treatment of low back pain: a multicentre study. Br Med J 1975;2:161‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gaber 1999 {published data only}
- Gaber W, Drozd A, Frauenrath‐Volkers C, Schüle A, Schwarz N, Pressel G. Lifting and carrying with lumbar supports; end report of a project at the airfreight department of Frankfurt / Main airport [Heben und Tragen mit Rückenstützbandagen; abschlussbericht zum Modellprojekt in der Luftfracht und der Flugzeugabfertigung, Flughafen Frankfurt / Main]. Airfreight department, Frankfurt/ Main airport 1999.
Gibson 2002 {published data only}
- Gibson JNA, Ahmed M. The effectiveness of flexible and rigid supports in patients with lumbar backache. The Journal of Orthopaedic Medicine 2002;24:86‐9. [Google Scholar]
Hsieh 1992 {published data only}
- Hsieh CJ, Phillips RB, Adams AH, Pope MH. Functional outcomes of low back pain: comparison of four treatment groups in a randomized controlled trial. J Manipulative Physiol Ther 1992;15:4‐9. [PubMed] [Google Scholar]
- Pope MH, Phillips RB, Haugh LD, Hsieh CJ, MacDonald L, Haldeman S. A prospective randomized three week trial of spinal manipulation, TMS, massage and corset in the treatment of subacute low back pain. Spine 1994;19:2571‐7. [DOI] [PubMed] [Google Scholar]
Kraus 2002 {published data only}
- Kraus JF, Schaffer KB, Rice T, Maroosis J, Harper J. A filed trial of back belts to reduce the incidence of acute low back injuries in New York city home attendants. Int J Occup Environ Health 2002;8:97‐104. [DOI] [PubMed] [Google Scholar]
Million 1981 {published data only}
- Million R, Nilsen KH, Jayson MIV, Baker RD. Evaluation of low back pain and assessment of lumbar corsets with and without back supports. Ann Rheum Dis 1981;40:449‐54. [DOI] [PMC free article] [PubMed] [Google Scholar]
Penrose 1991 {published data only}
- Penrose KW, Chook K, Stump JL. Acute and chronic effects of pneumatic lumbar support on muscular strength, flexibility, and functional impairment index. Sports Training Med Rehab 1991;2:121‐9. [Google Scholar]
Reddell 1992 {published data only}
- Reddell CR, Congleton JJ, Huchingson RD, Montgomery JF. An evaluation of a weightlifting belt and back injury prevention training class for airline baggage handlers. Applied Ergonomics 1992;23:319‐29. [DOI] [PubMed] [Google Scholar]
Roelofs 2007 {published data only}
- Roelofs PD, Bierma‐Zeinstra SM, Poppel MN, Jellema P, Willemsen SP, Tulder MW, et al. Lumbar supports to prevent recurrent low back pain among home care workers: a randomized trial. Ann Intern Med 2007;147:685‐92. [DOI] [PubMed] [Google Scholar]
Valle‐Jones 1992 {published data only}
- Valle‐Jones JC, Walsh H, O'Hara J, O'Hara H, Davey NB, Hopkin‐Richards H. Controlled trial of a back support in patients with non‐specific low back pain. Curr Med Res Opin 1992;12:604‐13. [DOI] [PubMed] [Google Scholar]
van Poppel 1998 {published data only}
- Poppel MNM, Koes BW, Ploeg GE, Smid T, Bouter LM. [Geen meetbaar effect van tilgordel en tilinstructies ter preventie van lage rugklachten op de werkplek: een gerandomiseerde, gecontroleerde trial]. Ned. Tijdschr. Geneeskd 1999;143(38):914‐8. [PubMed] [Google Scholar]
- van Poppel, Koes BW, Ploeg T, Smid T, Bouter LM. Lumbar supports and education for the prevention of low back pain in industry: a randomized controlled trial. JAMA 1998;279:1789‐94. [DOI] [PubMed] [Google Scholar]
Walsh 1990 {published data only}
- Walsh NE, Schwartz RK. Effects of the use of lumbosacral corsets in the workplace (Letter to the editor). Am J Phys Med Rehab 1991;70:111‐2. [PubMed] [Google Scholar]
- Walsh NE, Schwartz RK. The influence of prophylactic orthoses on abdominal strength and low back injury in the workplace. Am J Phys Med Rehab 1990;69:245‐50. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Amudsen 1982 {published data only}
- Amundsen T, Weber H. Braces in the treatment of chronic back pain. Tidsskrift for Den Norske Laegefrening 1982;102:1649‐51. [PubMed] [Google Scholar]
Anderson 1993 {published data only}
- Anderson CK, Morris TL, Vechio DC. The effectiveness of using a lumbar support belt. Dallas, Texas: Advanced Ergonomics Inc, 1993. [Google Scholar]
Carr 2003 {published data only}
- Carr CA. Use of a maternity support binder for relief of pregnancy‐related back pain. J Obstet Gynecol Neonatal Nurs 2003;32:495‐502. [DOI] [PubMed] [Google Scholar]
Celestini 2005 {published data only}
- Celestini M, Marchese A, Serenelli A. A randomized controlled trial on the efficacy of physical exercise in patients braced for instability of the lumbar spine. Europa Medicophysica 2005;41:223‐31. [PubMed] [Google Scholar]
Garg 1992 {published data only}
- Garg A, Owen B. Reducing back stress to nursing personnel: an ergonomic intervention in a nursing home. Ergonomics 1992;35:1353‐75. [DOI] [PubMed] [Google Scholar]
Hamonet 1993 {published data only}
- Hamonet C, Meziere C. Comparative study of the activity level of the abdominal muscles with and without a flexible lumbar belt in back pain. Rhumatologie 1993;45:165‐70. [Google Scholar]
Iwamoto 2004 {published data only}
- Iwamoto J, Takeda T, Wakano K. Returning athletes with severe low back pain and spondylolysis to original sporting activities with conservative treatment. Scand J Med Sci Sports 2004;14:346‐51. [DOI] [PubMed] [Google Scholar]
Jellema 2002 {published data only}
- Jellema P, Bierma‐Zeinstra SM, Poppel MN, Bernsen RM, Koes BW. Feasability of lumbar supports for home care workers with low back pain. Occup Med (Lond) Sept 2002;52(6):317‐23. [DOI] [PubMed] [Google Scholar]
Jonai 1997 {published data only}
- Jonai H, Villanueva MBG, Sotoyama M, Hisanaga H, Saito S. The effect of a back belt on torso motion: survey in an express package delivery company. Ind Health 1997 Apr;35(2):235‐42. [DOI] [PubMed] [Google Scholar]
Langford 2005 {published data only}
- Langford J, McCarthy PW. Randomised controlled clinical trial of magnet use in chronic low back pain: a pilot study. Clinical Chiropractic 2005;8:13‐9. [Google Scholar]
Larsson 1980 {published data only}
- Larsson U, Choler U, Lidström A, Lind G, Nachemson A, Nilsson B, et al. Auto‐traction for treatment of lumbago‐sciatica. A multicentre controlled investigation. Acta Orthop Scand 1980;51:791‐8. [DOI] [PubMed] [Google Scholar]
Marty 1998 {published data only}
- Marty M, Blotman F, Avouac B, Rozenberg S, Valat JP. Validation of the French version of the Dallas Pain Questionnaire in chronic low back pain patients. Rev Rhum 1998;65:126‐34. [PubMed] [Google Scholar]
Monticone 2004 {published data only}
- Monticone M, Barbarino A, Testi C, Arzano S, Moschi A, Negrini S. Symptomatic efficacy of stabilizing treatment versus laser therapy for sub‐acute low back pian with positive tests for sacroiliac dysfunction: a randomised clinical controlled trial with 1 year follow‐up. Europa Medicophysica 2004 Dec;40(4):263‐8. [PubMed] [Google Scholar]
Spratt 1993 {published data only}
- Spratt KF, Weinstein JN, Lehmann TR, Woody J, Sayre H. Efficacy of flexion and extension treatments incorporating braces for low back pain patients with retrodisplacement, spondylolisthesis, or normal sagittal translation. Spine 1993;18:1839‐49. [DOI] [PubMed] [Google Scholar]
Thompson 1994 {published data only}
- Thompson L, Pati AB, Davidson H, Hirsch D. Attitudes and back belts in the workplace. Work 1994;4:22‐7. [DOI] [PubMed] [Google Scholar]
Toda 2002 {published data only}
- Toda Y. Impact of waist/hip ratio on the therapeutic efficacy of lumbosacral corsets for chronic muscular low back pain. J Orthop Sci 2002;7(6):644‐9. [DOI] [PubMed] [Google Scholar]
Wassell 2000 {published data only}
- Wassell JT, Gardner LI, Landsittel DP, Johnston JJ, Johnston JM. A prospective study of back belts for prevention of back pain and injury. JAMA 2000;284(21):1‐10. [DOI] [PubMed] [Google Scholar]
References to studies awaiting assessment
Oleske 2007 {published data only}
- Oleske DM, Lavender SA, Andersson GB, Kwasny MM. Are back supports plus education more effective than education alone in promoting recovery from low back pain?: results from a randomized clinical trial.. Spine 2007;32:2050‐7.. [DOI] [PubMed] [Google Scholar]
Additional references
Airaksinen 2006
- Airaksinen O, Brox JI, Cedraschi C, Hildebrandt J, Klaber‐Moffett J, Kovacs F, Mannion AF, Reis S, Staal JB, Ursin H, Zanoli G. European guidelines for the management of chronic nonspecific low back pain. Eur Spine J 2006;15 (Suppl 2):S192‐S300. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ammendolia 2005
- Ammendolia C, Kerr MS, Bambardier C. Back belt use for prevention of occupational low back pain: a systematic review. Journal of Manipulative and Physiological Therapeutics 2005;28(2):128‐134. [DOI] [PubMed] [Google Scholar]
Andersson 1999
- Andersson GBJ. Epidemiological features of chronic low‐back pain. Lancet 1999;354:581‐585. [DOI] [PubMed] [Google Scholar]
Asche 2007
- Asche CV, Krikness CS, McAdam‐Marx C, Fritz JM. The societal costs of low back pain: data published between 2001 and 2007.. J Pain Palliat Care Pharmacother. 2007;21:25‐33.. [PubMed] [Google Scholar]
Burton 2005
- Burton AK. How to prevent low back pain. Best Practice & Research Clinical Rheumatology 2005;19(4):541‐555. [DOI] [PubMed] [Google Scholar]
Calmels 1996
- Calmels P, Fayolle‐Minon I. An update on orthotic devices for the lumbar spine based on a review of the literature. Rev Rhum 1996;63(4):285‐291. [PubMed] [Google Scholar]
Deyo 2006
- Deyo RA, Mirza SK, Martin BI. Back pain prevalence and visit rates. Spine 2006;31(23):2724‐2727. [DOI] [PubMed] [Google Scholar]
Dillingham 1998
- Dillingham TR. Lumbar supports for prevention of low back pain in the workplace. JAMA 1998;279(22):1826‐1828. [DOI] [PubMed] [Google Scholar]
Koes 1994
- Koes BW, Hoogen HMM. Efficacy of bed rest and orthoses of low‐back pain. Eur J Phys Med Rehabil 1994;4(3):86‐93. [Google Scholar]
Krismer 2007
- Krismer M, Tulder M. The low back pain group of the bone and health strategies for Europe project. Strategies for prevention and management of musculoskeletal conditions. Low back pain (non‐specific).. Best Pract Res Clin Rheumatol 2007;21:77‐91. [DOI] [PubMed] [Google Scholar]
Linton 2001
- Linton SJ, Van Tulder, MW. Preventive interventions for back and neck pain problems: what is the evidence. Spine 2001;26(7):778‐787. [DOI] [PubMed] [Google Scholar]
Maniadakis 2000
- Maniadakis N, Gray A. The economic burden of back pain in the UK.. Pain 2000;84:95‐103. [DOI] [PubMed] [Google Scholar]
McGill 1993
- McGill SM. Abdominal belts in industry: a position paper on their assets, liabilities and use. American Industrial Hygiene Association 1993;54(12):752‐754. [DOI] [PubMed] [Google Scholar]
Nachemson 1987
- Nachemson AL. Orthotic treatment for injuries and diseases of the spinal column. Physical Medicine and Rehabilitation: state of the art reviews 1987;1(1):11‐24. [Google Scholar]
van Poppel 1997
- Poppel MNM, Koes BW, Smid T, Bouter LM. A systematic review of controlled clinical trials on the prevention of back pain in industry. Occupational and Environmental Medicine 1997;54:841‐847. [DOI] [PMC free article] [PubMed] [Google Scholar]
Van Poppel 2000
- Poppel MNM, Looze MP, Koes BW, Smid T, Bouter LM. Mechanisms of action of lumbar supports. Spine 2000;25(16):2103‐2113. [DOI] [PubMed] [Google Scholar]
van Poppel 2004
- Poppel MNM, Hooftman WE, Koes BW. An update of a systematic review of controlled clinical trials on the primary prevention of back pain at the workplace. Occupational Medicine 2004;54(5):345‐352. [DOI] [PubMed] [Google Scholar]
van Tulder 1995
- Tulder MW, Koes BW, Bouter LM. A cost‐of‐illness study of back pain in The Netherlands. Pain 1995;62:233‐240. [DOI] [PubMed] [Google Scholar]
van Tulder 2003
- Tulder M, Furlan A, Bombardier C, Bouter L, Editorial Board of the Cochrande Collaboration Back Review Group. Updated method guidelines for systematic reviews in the Cochrane Collaboration Back Review Group. Spine 2003;28(12):1290‐1299. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Jellema 2001
- Jellema P, Tulder MW, Poppel MNM, Nachemson AL, Bouter LM. Lumbar supports for prevention and treatment of low back pain: a systematic review within the framework of the Cochrane Back Review Group. spine 2001;26:377‐386. [DOI] [PubMed] [Google Scholar]
Van Tulder 2000
- Tulder MW, Jellema P, Nachemson AL, Poppel MNM, Bouter LM. Lumbar supports for prevention and treatment of low back pain (Cochrane Review). Cochrane Database of Systematic Reviews 2000, Issue 3. [DOI: 10.1002/14651858.CD001823] [DOI] [PubMed] [Google Scholar]


