Abstract
Background:
Transcendental Meditation (TM) as a stress management technique may offer an adjunctive strategy to improve health and well-being in adults with cardiovascular disease (CVD).
Objectives:
To examine the efficacy of TM to improve aspects of cardiovascular health and psychological functioning in adults with CVD.
Method:
Studies (a) evaluating TM in adults with hypertension or CVD and (b) assessing a physiological or psychological outcome were retrieved and meta-analyzed. Weighted mean effect sizes were computed to assess between- and within-group changes.
Results:
Nine studies met inclusion criteria (N = 851; mean age = 60 ± 8 years; 47% women). Between-group analyses revealed no differences between TM and control groups. However, within-group (i.e., pre- to post-intervention) analyses revealed reductions in systolic (d+ = 0.31) and diastolic (d+ = 0.53) blood pressure (BP) for the TM group. There were no changes in depressive symptoms for TM or control participants.
Conclusions:
TM was associated with within-group (but not between-groups) improvements in BP. Continued research using randomized controlled trials with larger samples, and measuring psychophysiological outcomes at longer follow-up intervals is recommended.
1. INTRODUCTION
More than 28 million adults are diagnosed with cardiovascular disease (CVD) in the United States.1 High blood pressure (BP)2,3 and depression are associated with CVD onset and complications.4–6 Medical and surgical interventions are the first line treatments for CVD but non-pharmacological interventions can complement medical treatment(s) and assist in managing the risk factors associated with CVD.
Mantra meditation seeks to promote inner awareness through repetition of a sound, word, or phrase.7 Transcendental meditation (TM), one form of silent mantra meditation, involves repetition of a mantra to reach a state of effortless awareness8,9 – a state that is deeper than experienced during eyes-closed rest.10 In addition to increasing awareness, TM has been promoted for stress management.
Research suggests that TM can reduce BP among hypertensive patients11 with a meta-analysis revealing small improvements in individuals assigned to TM compared to controls.7 A recent summary concluded that TM reduces BP to levels achieved by other lifestyle interventions.12 Although encouraging, prior analyses either included a range of patients (not just those with hypertension) or focused on hypertensive exclusively. This pattern has yielded uncertainty about the benefits of TM for CVD patients. Given differences within the cardiovascular system associated with the disease processes and the influences of medical treatment for elevated BP, it is critical to understand whether TM can serve as an adjunctive treatment for individuals who are likely already receiving treatment or have more significant contributors to elevated BP compared to healthy samples.
As part of a 2013 American Heart Association (AHA) scientific statement on alternative strategies for BP reduction, TM was given a Class IIB, Level of Evidence B classification in the context of limited and somewhat mixed data.13 This designation implies that TM may be considered as treatment approach, though other interventions, such as aerobic exercise, have a stronger evidence to be considered as a BP reduction approach. A more recent AHA scientific statement suggested that meditation, including TM, may be a possible risk reduction technique for individuals with CVD based on evidence from a systematic review.14 However, definitive conclusions were limited by restricted data on follow-up and prognostic endpoints and no TM-specific recommendations.14 Others have cautioned against drawing firm conclusions regarding the efficacy of TM in lowering BP due to methodological limitations of prior research.12,15,16
Prior meta-analyses on TM have important limitations, namely, they have not focused on CVD populations exclusively, have primarily examined the impact of TM on BP, and have understudied depression, which may also benefit from TM.17,18 Because 15–20% of adults with CVD experience depression19,20 it is important to determine whether TM also allays depression among those living with CVD.
The purpose of the current research was to examine the efficacy of TM on cardiovascular and psychological health in adults with CVD. We hypothesized that TM would lead to greater improvements in psychological (e.g., depression) and physiological (e.g., BP) outcomes in adults with CVD relative to controls. We also describe intervention details and outcomes to identify gaps in our current understanding and guide future research.
2. METHOD
The Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) statement guided the current research (see Supplementary Materials 1).21
2.1. Eligibility criteria
Inclusion criteria were: (1) investigation of TM using a randomized controlled trial (RCT) or quasi-experimental design, (2) sampling only adults with hypertension or other form of CVD, (3) evaluation of a psychological (e.g., depression) and/or physiological (e.g., BP) outcome; and (4) provide information to calculate effect sizes. Studies that did not meet these criteria were excluded. Studies were not excluded based on language or geographic location.
2.2. Information Sources and Search Strategy
Potential studies were identified through (a) electronic databases (e.g., PubMed, PsycINFO, CINAHL, Cochrane Library, Web of Science: Science Citation Index), (b) reference sections of manuscripts, (c) tables of contents of journals, and (d) research databases (i.e., NIH RePORTer, ClinicalTrials.gov). Broad search terms included transcendental meditation, cardiovascular disease, and intervention. The specific search terms capture varied CVD conditions (e.g., “heart failure,” “myocardial infarction,” “coronary,” “hypertension”). The search strings used for each electronic bibliographic database is provided in Supplementary Materials 2. All searches were conducted through June 2019.
2.3. Study Selection
Identified papers were reviewed in several steps. First, duplicate bibliographic records were removed. Second, titles and abstracts were screened to identify studies that sampled adults with CVD and reported a TM intervention. Literature reviews and meta-analyses were excluded, though references were checked for primary studies. Finally, texts of the remaining records were reviewed by two authors. Studies were removed if they did not meet inclusion and exclusion criteria. Records that reported the same study and/or sample across multiple manuscripts were linked in the database to be represented as a single unit. The manuscript reporting the most complete data was selected as primary.
2.4. Data Collection Process, Data Items, and Reliability
Two trained independent coders extracted study information (e.g., dates of data collection), sample characteristics (e.g., age, gender, diagnosis), study design (e.g., comparison condition), intervention details (e.g., number sessions, format), and intervention components. The methodological quality (MQ) of each study was determined through 17 items adapted from validated measures.22–25 The possible MQ score was 25, with higher scores reflecting higher MQ. Standardized coding forms were used to maximize consistency of data extraction and coding. Regarding inter-rater reliability for characteristics reported as a categorical variable, coders agreed on 89% of the judgments (mean Cohen’s κ = 0.80). The average intra-class correlation coefficient (ρ) reflecting reliability of continuous variables was 0.87 across categories (median = 1.00). The two coders discussed discrepancies until consensus was reached; principal investigator (LAJSS) clarified any remaining unresolved discrepancies.
2.5. Study Outcomes
We focused on systolic BP and diastolic BP because TM is widely promoted as a BP reduction tool, which underscores the importance of evaluating TM as a BP reduction tool for this population. We also included depression as an outcome because depression is increasingly recognized as an indicator of CVD prognosis.
2.6. Summary Measures
Between group effect sizes assessed differences in outcomes in individuals who completed a TM intervention relative to individuals in a comparison group. For each study, effect sizes (d) were calculated as the mean difference in each outcome between the TM and comparison groups divided by the pre-test standard deviation.26,27 Positive effect sizes indicated that participants who received TM reported improvements on the outcome relative to controls. Within-group effects sizes were calculated as the mean change from pre- to post- intervention.26,27 Positive within group effects reflected improvement in the outcome at post-intervention relative to pre-intervention. All effect sizes were weighted by sample size to correct for sample size bias.28 Two independent coders calculated effect sizes. Discrepancies between coders were discussed and corrected following resolution.
2.7. Synthesis of Results
Weighted mean ES (d+) and 95% confidence intervals were calculated using random-effects assumptions (full information maximum likelihood).29 Box plots for each outcome identified outliers.30 The Q statistic was calculated to assess heterogeneity. The I2 index and 95% confidence intervals evaluated the consistency across effect sizes.31,32 All analyses were performed using Stata/SE 15.1 with published macros for examination of aggregated effect sizes and moderator analyses.33 Comprehensive Meta-Analysis was used to generate forest plots.34
3. RESULTS
3.1. Study Selection
A total of 893 records were identified from electronic database searches after removal of duplicates and 14 additional records were found through alternative sources, including five clinical trials records (, , , , ). Studies not meeting inclusion criteria were excluded following review of title and abstracts (529 records). Studies identified as reviews, editorials, or commentaries (345 records) or not relevant (184 records) were removed. Following full-text review, studies not sampling adults with CVD (140 records) were excluded. An additional 205 records were excluded because the studies did not meet inclusion criteria (see Figure 1 for details). Thus, the final sample included 9 studies with 24 supplemental texts. Table 1 provides details of study characteristics of the 9 studies reviewed in the meta-analysis. A complete list of the records reviewed is available upon request from the PI (LAJSS).
Figure 1.
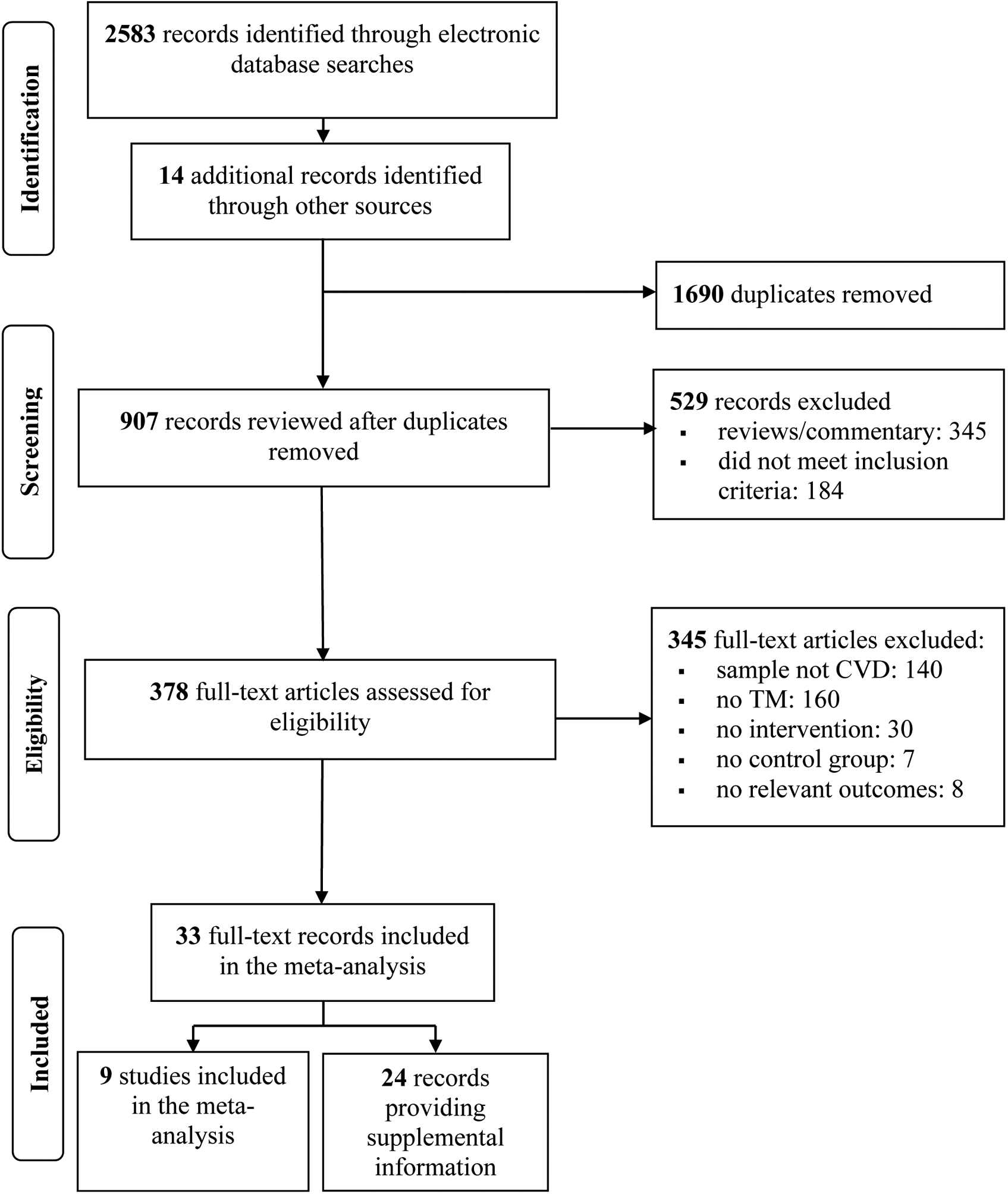
Screening and Selection Procedures
Table 1.
Study, Sample, and Intervention Characteristics of the 9 Studies Included in the Meta-Analysis
| Citation | Sample | Recruitment/Location | Condition | Current Tx | Randomized | Control | Intervention Type | Intervention | Home Practice | Checking Periodǂ | Outcomes & Last Assessment | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sessions | Dose | Sessions | Dose | Sessions | Dose | |||||||||
| Calderon (2000)35 Linked:55,56–58 |
N = 72(92%); 67% F; Mage = 54 | Self-selected volunteers, hospital, clinic; Los Angeles, CA, USA, Biobehavioral Research Center | HTN | Pharmacological | Yes | EDU | TM | 4 | 360 | 364 | 7280 | 10 | 600 | 25 wks: SBP; DBP |
| Duraimani et al. (2015)39 Linked:59–61 |
N = 48(75%); 54% F; Mage = 58 | Self-selected volunteers, hospital; Washington D.C., USA, Howard University Medical Center | HTN | Pharmacological | Yes | EDU+ | TM+HE classes | 12 | 900 | 224 | 4480 | 6 | 360 | SBP; DBP |
| Jayadevappa et al. (2007)37
Linked:62,63 |
N = 31(74%); 61% F; Mage = 64 | Clinical contact; Philadelphia, PA, USA, UPenn Health Care System | CHF | NR | Yes | EDU | TM | 4 | 360 | 365 | 6388 | 9 | 810 | Depression |
| Kondwani et al. (2005)40 Linked:64 |
N = 42(81%); 56% F; Mage = 51 | Self-selected volunteers, clinical contact; Oakland, CA, USA, West Oakland Health Center | Mild HTN | Pharmacological | Yes | EDU | TM | 4 | 360 | 728 | 14560 | 15 | 900 | SBP; DBP; Depression |
| Paul-Labrador et al. (2006)38 Linked:65–67 |
N = 103(82%); 18% F; Mage = 67 | Self-selected volunteers, clinical contact; Los Angeles, CA, USA, Cedars-Sinai Medical Center | CHD | Pharmacological | Yes | EDU | TM | 4 | 345 | NR | NR | 19 | 1710 | SBP; DBP; Depression |
| Schneider et al. (2005)41 Linked:68 |
N = 197(76%); 53% F; Mage = 49 | Health center, churches, senior center, department of aging programs; West Oakland, CA, USA | HTN | Pharmacological | Yes | EDU | TM | 4 | 345 | 104 | 2080 | 11 | 660 | SBP; DBP |
| Schneider et al. (2012)43 Linked:69 |
N = 201(73%); 42% F; Mage = 59 | Clinical contact; Milwaukee, Wisconsin, USA, Department of Medicine, Medical College of Wisconsin | CHD | Pharmacological | Yes | CVD EDU | TM | 4 | 420 | 3945 | 78894 | 74 | 4440 | SBP; DBP; Depression |
| Schneider et al. (1995)42 Linked:70,44,71,71–74*The PMR group is excluded. |
N = 127 [85](87%); 57% F; Mage = 67 | Clinical contact, senior citizens & other community organizations; Oakland, CA, USA, West Oakland Health Center | Mild history of HTN | Pharmacological | Yes | Lifestyle Modification EDU | TM | 4 | 360 | 182 | 3640 | 3 | 270 | SBP; DBP |
| Vivier (2004)36 | N = 30(93%); 14% F; Mage = 70 | Hospital, clinical contact; Iowa City, Iowa, USA, University of Iowa Heart Care Center | CVD | Pharmacological | No | TAU | TM+Maharishi Consciousness-based health care (TM + herbal supplements, exercise, & diet) | 12 | 900 | 546 | 10920 | 18 | 1230 | Depression; SBP; DBP |
N (%), number of participants who consented to participate in the study (retention); F, female; HTN, hypertension; CHD, coronary heart disease; CVD, cardiovascular disease; CAD, coronary artery disease; EC, education control; WLC, wait list control; UC, usual care; HE, health education; TM, transcendental meditation; PMR, progressive muscle relaxation; Wks, number of weeks post-intervention assessment occurred; SBP, systolic blood pressure; DBP, diastolic blood pressure.
The checking period involves recommended follow-up sessions to check the correctness of the TM technique. Number listed reflects number of possible technique checks based on study length of follow-up.
3.2. Study Characteristics
Publication (or dissertation completion) dates ranged from 1995 to 2015 with most (75%) studies published on or before 2007. Seven studies were published in journals (79%). Two were unpublished dissertations.35,36 All studies were written in English and conducted in the United States. Six studies (67%) recruited participants through multiple methods (e.g., clinics, churches, senior centers, and media advertisements). Three studies (33%) recruited participants solely through clinical contacts.
3.3. Sample Characteristics
The initial samples included 851 adults who provided informed consent, with 658 included in final analyses (mean percentage [M%] = 80% ± 10% retention rate). Samples were comprised of mostly men (53%) with a mean age of 60 and standard deviation (SD) of 8 (range = 49 – 70 years). Of the studies reporting race, all sampled only African American participants. Race was not reported by two studies. Five studies reported marital status; 43% (SD = 22) of the participants were married. Adults with varied CVD conditions were included. Studies sampled patients with hypertension (7 out of 9), coronary heart disease (3 out of 9), or history of myocardial infarction (2 of 9); one study involved heart failure patients (not mutually exclusive).37 Of the eight studies providing details on participants’ CVD-related treatment, all studies reported pharmacological therapy. Two studies sampled patients who were enrolled in or had graduated from cardiac rehabilitation36,38 and one study reported sampling a portion of participants with a history of revascularization.38
3.4. Intervention Characteristics
All authors reported providing TM instruction in the standard format which typically includes two introduction lectures, one brief personal interview, both individual and group instruction led by trained instructors. The instructional sessions typically lasted a median of 90 minutes (range = 75 to 105). All studies referenced using the standard home practice recommendation (i.e., 15–20 minutes, twice daily) and follow-up visit (i.e., returning following the initial 4-day training period to check the individual’s technique).
Two studies offered additional components beyond TM (TM+).36,39 In one study, TM was supplemented with eight basic health education classes.39 In the second, participants received Maharishi Consciousness-Based Health Care, which included TM, herbal supplements, exercises (i.e., Maharishi Yoga asanas and Pranayama), and recommended running or walking, and diet.36
3.5. Design Characteristics
All studies included a control group with pre- and post-test assessments (8 RCTs; 1 quasi-experimental study with participants matched on gender, age, and severity of disease). The control conditions included standard care (1 of 9 studies), or an active comparison group (e.g., health education; 8 of 9 studies). Six studies matched the TM and control groups for time and contact, though the timing of intervention delivery sometimes varied between groups.40 The median number of follow-up assessments was 1 (range = 1 to 11) but five studies reported outcomes summed across multiple time-points.36,40–43 The length of follow-ups ranged from an immediate post-test to nearly eight years later. (Mortality was the only outcome assessed at the eight-year follow-up.42,44) Because most studies (k = 5) included results for a single post-test ranging from immediate post-test to 25 weeks post-intervention (median = 15), our analyses focused on the last (or only) assessment following TM training. Therefore, for systolic and diastolic BP (k = 6), assessments occurred 12 to 281 weeks post-intervention (median = 20 weeks). One study assessed BP at multiple time points (3, 6, 9, and 12 months) but the change in BP over the course of the entire follow-up (e.g., 12 months) was included in the analyses.41 Assessments of depressive symptoms ranged from 15 to 281 weeks post-intervention (median = 38 weeks). One study assessed depression on two separate occasions (12 and 25 weeks post-intervention); the final assessment (25 weeks) was used in analyses.37
3.6. Synthesis of Results for Between-Groups Analyses
Depression
To assess depressive symptoms (k = 5), four studies used the Center for Epidemiological Scale for Depression,36–38,43,45 a 20-item self-report measure where individuals are rate the frequency of symptoms of depression over the past week.45 One study used the depression subscale of the Mental Health Inventory, a 38-item self-report measure with five subscales assessing anxiety, depression, positive affect, emotional ties, and behavioral/emotional control.40,46 Two studies reported improvements in the TM group relative to controls.37,40 Weighted mean effect sizes revealed that depressive symptoms were not reduced in the TM-only group relative to controls (d+ = 0.27, 95% confidence interval [CI] = −0.14, 0.67; k = 4). The magnitude and direction of the weighted mean effect size did not change when we included the single TM+ study that measured depression (d+ = 0.24, 95% CI = −0.12, 0.61; k = 5).
Systolic and Diastolic Blood Pressure
All studies that assessed BP averaged multiple readings; the number of readings ranged from an average of 2 of 3 readings during a single visit39,42 up to measuring BP over 5 visits, 1–2 weeks apart and averaging the final two visits.40 There were no differences between TM and control groups on systolic (d+ = 0.27, 95% CI = −0.04, 0.57; k = 6) or diastolic (d+ = 0.28, 95% CI = −0.02, 0.59; k = 6) BP (see Table 2). The hypothesis of homogeneity was not supported for systolic (Q [5] = 16.29, p =.006; I2 = 69, 95% uncertainty limits = 28, 87) or diastolic (Q [5] = 10.92, p =.053; I2 = 54, 95% uncertainty limits = 0, 82) BP, and the uncertainty limits for the I2 exceeded the 50% threshold. The magnitude and direction of the weighted mean effect size did not change when we included the TM+ studies (systolic BP: d+ = 0.16, 95% CI = −0.11, 0.42; k = 8; Q[7] = 22.90, p =.002; I2 = 69, 95% uncertainty limits = 36, 85; diastolic BP: d+ = 0.15, 95% CI = −0.11, 0.42; k = 8; Q[7] = 19.66, p =.006; I2 = 64, 95% uncertainty limits = 24, 83).
Table 2.
The Overall Weighted Mean Effects Comparing TM® versus Controls on Systolic and Diastolic Blood Pressure.
| Study Citation | Outcome | N | Weeks | d+ | SE | Variance | 95% CI | d+ (95% CI) | |
|---|---|---|---|---|---|---|---|---|---|
| Lower | Upper | ||||||||
| Calderon (2000) | SBP | 71 | 25 | −0.2542 | 0.2419 | 0.0585 | −0.7283 | 0.2199 | 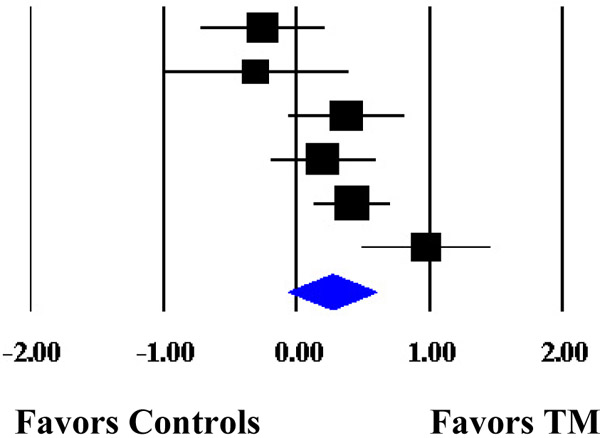 |
| Kondwani et al. (2005) | SBP | 34 | 51 | −0.3122 | 0.3591 | 0.1290 | −1.0162 | 0.3918 | |
| Paul-Labrador et al. (2006) | SBP | 84 | 15 | 0.3741 | 0.2235 | 0.0500 | −0.0642 | 0.8124 | |
| Schneider et al. (2005) | SBP | 98 | 52 | 0.1974 | 0.2058 | 0.0423 | −0.2057 | 0.6005 | |
| Schneider et al. (2012) | SBP | 183 | 281 | 0.4136 | 0.1505 | 0.0227 | 0.1183 | 0.7089 | |
| Schneider et al. (1995) | SBP | 74 | 12 | 0.9716 | 0.2501 | 0.0626 | 0.4812 | 1.4620 | |
| MM | 0.2636 | 0.1668 | 0.0278 | −0.0633 | 0.5905 | ||||
| ML | 0.2673 | 0.1547 | 0.0239 | −0.0358 | 0.5704 | ||||
| Calderon (2000) | DBP | 71 | 25 | −0.1990 | 0.2415 | 0.0583 | −0.6722 | 0.2742 | 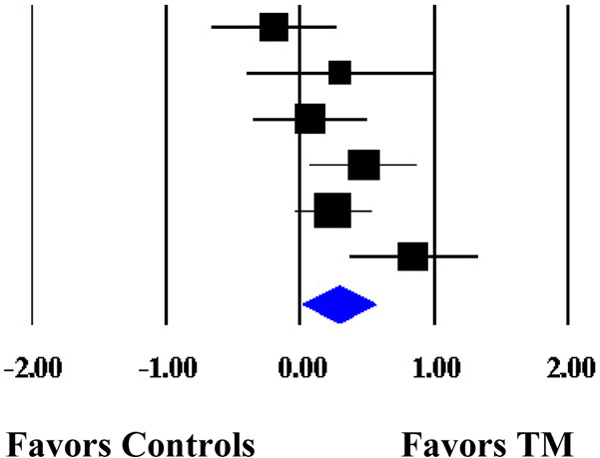 |
| Kondwani et al. (2005) | DBP | 34 | 51 | 0.2977 | 0.3589 | 0.1288 | −0.4057 | 1.0011 | |
| Paul-Labrador et al. (2006) | DBP | 84 | 15 | 0.0725 | 0.2216 | 0.0491 | −0.3618 | 0.5068 | |
| Schneider et al. (2005) | DBP | 98 | 52 | 0.4709 | 0.2081 | 0.0433 | 0.0631 | 0.8787 | |
| Schneider et al. (2012) | DBP | 183 | 281 | 0.2431 | 0.1493 | 0.0223 | −0.0496 | 0.5358 | |
| Schneider et al. (1995) | DBP | 74 | 12 | 0.8427 | 0.2467 | 0.0608 | 0.3594 | 1.3260 | |
| MM | 0.2837 | 0.1361 | 0.0185 | 0.0170 | 0.5504 | ||||
| ML | 0.2848 | 0.1571 | 0.0247 | −0.0231 | 0.5926 | ||||
Note. The overall weighted mean effect sizes are calculated using random-effects models with methods of moments (MM) and full information maximum likelihood (ML) methods to estimate the between-study variance. Weighted mean effect sizes (d+) are positive for differences that favor the transcendental meditation (TM) group relative to controls. Weeks refers to the number of weeks between the last intervention session and the assessment. d+, weighted mean effect size; SE, standard error; CI, confidence interval; SBP, systolic blood pressure; DBP, diastolic blood pressure.
Cumulative Meta-Analysis
A cumulative meta-analysis was performed using the initial date of data collection for each study (Table 3). Although TM-only interventions did not differ statistically from controls, results showed the benefits of TM-only on systolic and diastolic BP improved over time with the CIs surrounding the effect size estimates narrowing as the data accumulated. The cumulative meta-analysis also shows that TM-only interventions for patients with CVD were last reported in the mid-2000s with data collection commencing an average of 9 years (SD = 4) earlier. Results from TM+ studies (not included in the cumulative forest plot) were last published in 2015 with data collection commencing an average of 7 years (SD = 1) earlier.
Table 3.
Forest Plot of the Cumulative Weighted Mean Effects for Blood Pressure Based on Start Date of Data Collection.
| Cumulative Statistics | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Study Citation | Outcome | N | Date | Point | SE | Variance | 95% CI | Cumulative d+ (95% CI) | |
| Lower | Upper | ||||||||
| Schneider et al. (1995) | SBP | 74 | 1989 | 0.9716 | 0.2501 | 0.0626 | 0.4814 | 1.4618 | 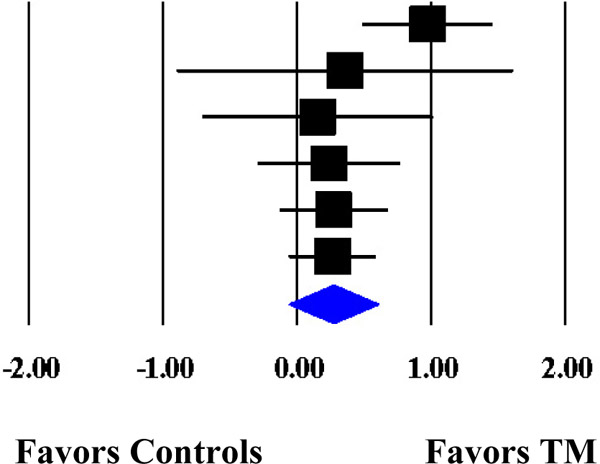 |
| Kondwani et al. (2005) | SBP | 34 | 1992 | 0.3556 | 0.6414 | 0.4114 | −0.9015 | 1.6126 | |
| Calderon (2000) | SBP | 71 | 1995 | 0.1503 | 0.4417 | 0.1951 | −0.7155 | 1.0160 | |
| Schneider et al. (2012) | SBP | 183 | 1998 | 0.2349 | 0.2733 | 0.0747 | −0.3008 | 0.7705 | |
| Paul-Labrador et al. (2006) | SBP | 84 | 1999 | 0.2715 | 0.2075 | 0.0430 | −0.1351 | 0.6781 | |
| Schneider et al. (2005) | SBP | 98 | 1999† | 0.2636 | 0.1668 | 0.0278 | −0.0633 | 0.5905 | |
| MM | 0.2636 | 0.1668 | 0.0278 | −0.0633 | 0.5905 | ||||
| ML | 0.2673 | 0.1547 | 0.0239 | −0.0358 | 0.5704 | ||||
| Schneider et al. (1995) | DBP | 74 | 1989 | 0.8427 | 0.2466 | 0.0608 | 0.3594 | 1.3260 | 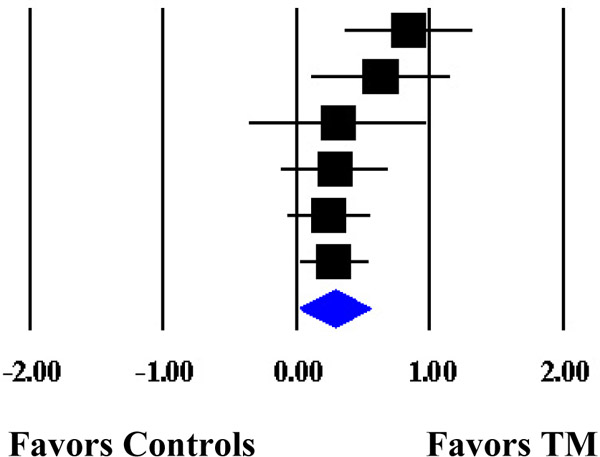 |
| Kondwani et al. (2005) | DBP | 34 | 1992 | 0.6326 | 0.2653 | 0.0704 | 0.1127 | 1.1525 | |
| Calderon (2000) | DBP | 71 | 1995 | 0.3134 | 0.3419 | 0.1169 | −0.3567 | 0.9835 | |
| Schneider et al. (2012) | DBP | 183 | 1998 | 0.2904 | 0.2071 | 0.0429 | −0.1154 | 0.6962 | |
| Paul-Labrador et al. (2006) | DBP | 84 | 1999 | 0.2429 | 0.1622 | 0.0263 | −0.0751 | 0.5609 | |
| Schneider et al. (2005) | DBP | 98 | 1999† | 0.2837 | 0.1361 | 0.0185 | 0.0170 | 0.5504 | |
| MM | 0.2837 | 0.1361 | 0.0185 | 0.0170 | 0.5504 | ||||
| ML | 0.2848 | 0.1571 | 0.0247 | −0.0231 | 0.5926 | ||||
Note. The cumulative weighted mean effect sizes are calculated using random-effects models with methods of moments (MM) or full information maximum likelihood (ML) to estimate the between-study variance. Weighted mean effect sizes (d+) are positive for differences that favor the transcendental meditation (TM) group relative to controls. Date refers to the year data collection commenced. d+, weighted mean effect size; SE, standard error; CI, confidence interval; SBP, systolic blood pressure; DBP, diastolic blood pressure.
The start and end dates for the study trial were not provided and therefore we used the start date of the study funding period.
3.7. Synthesis of Results for Exploratory Within-Groups Analyses
Pre- to post- changes were assessed for TM and controls. Results indicated that individuals with CVD who received a TM intervention demonstrated improvements in systolic (d+ = 0.31, 95% CI = 0.03, 0.59, k = 6) and diastolic (d+ = 0.53, 95% CI = 0.14, 0.92, k = 6) BP at post-test. Heterogeneity for systolic BP (Q [5] = 22.99, p <.001; I2 = 78, 95% uncertainty limits = 52, 90) and diastolic BP (Q [5] = 16.63, p <.01; I2 = 70, 95% uncertainty limits = 30, 87) was evident, and the uncertainty limits for the I2 exceeded the 50% (diastolic BP) and 75% (systolic BP) threshold. Systolic (d+ = 0.06, 95% CI = −0.20, 0.31, k = 6) and diastolic BP was not reduced (d+ = 0.24, 95% CI = −0.02, 0.50, k = 6) in the control groups. The hypothesis of homogeneity was not supported for systolic (Q [5] = 29.21, p <.001; I2 = 83, 95% uncertainty limits = 64, 92) or diastolic (Q [5] = 10.41, p =.064; I2 = 52, 95% uncertainty limits = 0, 81) BP. The magnitude and direction of the changes did not differ when including studies using a TM+ approach for TM (systolic: d+ = 0.35, 95% CI = 0.08, 0.61; k = 8; diastolic: d+ = 0.53, 95% CI = 0.19, 0.88) or controls (systolic: d+ = 0.20, 95% CI = −0.04, 0.43; k = 8) with one exception: diastolic BP was improved in the control group (diastolic: d+ = 0.37, 95% CI = 0.10, 0.64).
Although three studies reported improvements in depression in the TM group37,40,43 and two studies reported improvements in the control group,37,38 depressive symptoms did not improve within the TM-only (d+ = 0.21, 95% CI = −0.12, 0.54; k = 4) or control (d+ = −0.10, 95% CI = −0.51, 0.31; k = 4) groups. The magnitude and direction of the weighted mean effect size did not change when we included the single TM+ study that measured depression (TM: d+ = 0.14, 95% CI = −0.16, 0.43; k = 5; controls: d+ = −0.12, 95% CI = −0.50, 0.26; k = 5).
3.8. Moderators of Between-Group Differences in Systolic and Diastolic BP
Moderator tests focused on between-group changes in systolic BP, diastolic BP, and depressive symptoms. Moderator tests assessed whether (1) age, (2) gender (proportion women), and (3) TM delivered as a stand-alone intervention (TM-only) versus alongside additional components (e.g., health education; TM+) explained the variability in the overall weighted mean effect sizes for systolic BP, diastolic BP, or depressive symptoms.
Sample Characteristics
Mean age of the sample was not a moderator of the effect of systolic BP, diastolic BP, or depression (ps ≥.316). The proportion of women in the sample was also not a significant moderator of BP or depressive symptoms (ps ≥ .091).
TM with Additional Components
Examination of the delivery of TM-only versus TM plus additional components (TM+) revealed no differences in the overall weighted mean effect sizes for systolic BP between the TM and the TM+ groups (QB [1] = 3.52, p = .060). Compared to TM+, TM-only was more effective in reducing diastolic BP relative to controls (QB [1] = 6.36, p = .012). Differences between TM and TM+ could not be assessed as only a single TM+ study measured depression.
3.9. Methodological Quality and Risk of Publication Bias
The mean MQ rating was 19 (SD = 1.5; range = 16–21). Studies met an average of 76% of the MQ criteria. MQ did not predict systolic BP, diastolic BP, or depression (ps ≥.091). See Supplementary Materials 3 complete details on the MQ assessment. The risk of publication bias was not assessed using visual and statistical methods in line with recommendations cautioning against evaluating the risk of bias when outcomes with fewer than 10 effect sizes are available.47
4. DISCUSSION
The use of meditation, including TM, is increasingly popular among U.S. adults, including patients living with CVD.48,49 Understanding the benefits and risks of TM is critical for improving patient-care. This meta-analysis extended prior meta-analytic reviews on TM by exclusively evaluating samples with CVD, examining the effects of TM on depression, and providing a cumulative meta-analysis of the research conducted to date. Nine studies comparing TM to a control group were included; seven studies examined TM as a stand-alone intervention and were analyzed separately from two studies evaluating TM plus other intervention components. Between-group analyses indicated no difference between TM and controls on any outcome. Cumulative meta-analysis revealed that the differences in BP between TM and control groups have improved over time. Exploratory within-group analyses demonstrated small to moderate improvements in systolic and diastolic BP among patients who received a TM intervention but no improvements in controls.
The small to moderate improvements noted within groups receiving TM alone converges with prior meta-analyses identifying BP reductions following TM.50,51 Mean changes in systolic (3.46 mmHg) and diastolic BP (3.75 mmHg) in the TM group were observed compared to controls (1.26 mmHg and 2.43 mmHg, respectively). The findings support the Class IIB level of evidence recommended within the AHA statement on integrative methods to reduce BP.13
TM may lead to reduced BP through several pathways. First, TM may improve autonomic balance. Chronic or recurrent acute stressors contribute to sympathetic arousal including elevated BP.52 Conversely, practices such as TM, which can lead to the “relaxation response,” can dampen the effects of chronic sympathetic arousal for individuals with stress-related conditions or elevated BP.52,53 Second, TM may reduce perceived stress, which may contribute to high BP through behaviors such as poor medication adherence54 or dietary control. Participants in the TM groups may have experienced less distress and improved medication adherence but we could not test this hypothesis given that most studies did not report stress or medication adherence. Only two studies assessed changes in diet but these studies did not measure BP.
However, because between-group changes were not significant, the current results must be interpreted with caution. Most studies reported equivalent proportions of medication use across groups at baseline and, thus, differences in baseline medication use are unlikely to explain the absence of between-group differences. In contrast, prior reviews and meta-analyses evaluating TM in broader populations have reported between-group differences.11,50,51 This difference may be explained by methodological differences. For example, we included studies not evaluated in prior meta-analyses.36,39,40 Prior meta-analyses also examined a broader range of ages (e.g., adult and non-adult samples) and conditions (i.e., CVD and non-CVD),50,51 which allowed prior investigators to include a larger number of studies with additional power to detect small effects. In contrast, we restricted the present analyses to adults with CVD to address a more specific research question. Furthermore, our cumulative meta-analysis suggests that studies appear to be trending towards a reduction in systolic and diastolic BP over time but new studies are needed to determine whether the treatment benefits of TM outweigh standard care. Thus, additional RCTs with larger samples and increased power may be needed to reveal a between-groups effect in populations with existing CVD.
Between- and exploratory within-group results also revealed no significant changes in depressive symptoms. However, no studies reported details on depression treatment and the small number of studies reporting depression symptoms may have limited power to test for effects. The current meta-analysis did not evaluate other psychological outcomes (e.g., anxiety, stress) given the paucity of studies reporting on such outcomes. Due to the importance of psychological factors for cardiovascular health, as well as increased popularity of mind-body practices to alleviate distress, studies measuring depressive symptoms and other measures of psychological health are needed.
Moderator analyses indicated a difference between TM and TM+ interventions with respect to diastolic BP; that is, greater diastolic BP reductions were observed when TM was delivered as a stand-alone intervention. This finding should be with interpreted with caution given the small number of studies involved. No other sample characteristics (i.e., age, gender) emerged as moderators. The length of time between TM training and the post-intervention assessment varied widely and subgroup analysis based on timing of assessments was limited by the number of studies. Only two studies reported assessments that occurred less than six months following TM training. Medication changes and adherence to TM practice were not reported consistently to allow for evaluation of the impact on results.
Overall, these results should be interpreted carefully due to several limitations. First, the number of outcomes we could examine was limited because few studies reported outcomes other than BP. For example, only one study reported on heart rate variability38 and two studies reported on mortality.42–44 Additional measures of cardiovascular health will allow for a more comprehensive evaluation of the efficacy of TM. Also, only a single study reported including biomarkers of stress (e.g., cortisol).37 It is important that future studies measure stress to ensure that individuals with elevated stress, who would be expected to benefit from stress management interventions, show improvements. Second, we were unable to perform several planned moderator analyses because studies were limited by study and sample characteristics (e.g., we were unable to examined race as a moderator given that all studies reporting on race/ethnicity sampled African Americans exclusively). Third, our analyses were restricted to a single observation from each study. If future studies with longer follow-up are conducted, the duration of the effects can be evaluated. Fourth, within-group changes were assessed to determine if the TM group improved over time but the findings from the within-group analyses should be interpreted cautiously considering known threats to internal validity (e.g., history or testing effects). Finally, many studies had small samples, which contributes to less precise effect estimates.
5. CONCLUSION
Overall, our meta-analysis revealed limited evidence to support the use of TM in adults with existing CVD. Modest improvements in systolic and diastolic BP were observed within-, but not between-, groups. Thus, consistent with the AHA statement, we conclude that TM possibly represents an adjunctive BP reduction strategy for patients with CVD. However, TM should clearly be complementary and not a stand-alone intervention. Given the recent surge of interest in mindfulness-based interventions, it was surprising that there has been a dearth of research on TM for samples with CVD in the past decade. Additional research is needed to establish efficacy of TM to lower BP compared to other active interventions, to understand the mechanisms of change, and to determine whether TM can lead to enduring improvements in cardiovascular health. Such studies should sample a wider range of adults with CVD (e.g., non-Hispanic Whites and Blacks from a range of domestic settings) with multi-institutional research teams, measuring a range of psychological, physiological, and CVD-specific outcomes, with multiple follow-up assessments to fully understand the effects of TM in U.S. adults living with CVD.
Supplementary Material
Funding Acknowledgements:
The research reported in this paper was supported by the National Center for Complementary and Integrative Health of the National Institutes of Health under award number 5R01AT008815 to Lori A. J. Scott-Sheldon, PhD and Michael P. Carey, PhD (Multiple PIs). Emily C. Gathright, PhD was supported by the Cardiovascular Behavioral Medicine Training Grant (5T32HL076134; Rena R. Wing, PI) from the National Heart, Lung, and Blood Institute. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
REFERENCES
- 1.Centers for Disease Control and Prevention NCfHS. Heart Disease. https://www.cdc.gov/nchs/fastats/heart-disease.htm. Accessed November 14, 2018.
- 2.Murray CJ, Abraham J, Ali MK, et al. The state of US health, 1990–2010: Burden of diseases, injuries, and risk factors. JAMA. 2013;310(6):591–606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yang Q, Cogswell ME, Flanders WD, et al. Trends in cardiovascular health metrics and associations with all-cause and CVD mortality among US adults. JAMA. 2012;307(12):1273–1283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rozanski A, Blumenthal JA, Davidson KW, Saab PG, Kubzansky L. The epidemiology, pathophysiology, and management of psychosocial risk factors in cardiac practice: the emerging field of behavioral cardiology. J Am Coll Cardiol. 2005;45(5):637–651. [DOI] [PubMed] [Google Scholar]
- 5.Tawakol A, Ishai A, Takx RA, et al. Relation between resting amygdalar activity and cardiovascular events: a longitudinal and cohort study. Lancet. 2017;389(10071):834–845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hamer M, Molloy GJ, Stamatakis E. Psychological distress as a risk factor for cardiovascular events: pathophysiological and behavioral mechanisms. J Am Coll Cardiol. 2008;52(25):2156–2162. [DOI] [PubMed] [Google Scholar]
- 7.Ospina MB, Bond K, Karkhaneh M, et al. Meditation Practices for Health: State of the Research Evidence report/technology assessment. No. 155. (Prepared by the University of Alberta Evidence-based Practice Center under Contract No. 290-02-0023.). Vol AHRQ Publication No. 07-E010. Rockville, MD: Agency for Healthcare Research and Quality; 2007:1–263. [PMC free article] [PubMed] [Google Scholar]
- 8.Mahesh Yogi M The science of being and art of living. London: International SRM publications; 1966. [Google Scholar]
- 9.Travis F, Shear J. Focused attention, open monitoring and automatic self-transcending: Categories to organize meditations from Vedic, Buddhist and Chinese traditions. Conscious Cogn. 2010;19(4):1110–1118. [DOI] [PubMed] [Google Scholar]
- 10.Dillbeck MC, Orme-Johnson DW. Physiological differences between transcendental meditation and rest. Am Psychol. 1987;42(9):879–881. [Google Scholar]
- 11.Rainforth MV, Schneider RH, Nidich SI, Gaylord-King C, Salerno JW, Anderson JW. Stress reduction programs in patients with elevated blood pressure: a systematic review and meta-analysis. Curr Hypertens Rep. 2007;9(6):520–528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ooi SL, Giovino M, Pak SC. Transcendental meditation for lowering blood pressure: An overview of systematic reviews and meta-analyses. Complement Ther Med. 2017;34:26–34. [DOI] [PubMed] [Google Scholar]
- 13.Brook RD, Appel LJ, Rubenfire M, et al. Beyond Medications and Diet: Alternative Approaches to Lowering Blood Pressure A Scientific Statement From the American Heart Association. Hypertension. 2013;61(6):1360–1383. [DOI] [PubMed] [Google Scholar]
- 14.Levine GN, Lange RA, Bairey-Merz CN, et al. Meditation and cardiovascular risk reduction a scientific statement from the American Heart Association. J Am Heart Assoc. 2017;6(10):e002218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Canter PH. The therapeutic effects of meditation: The conditions treated are stress related, and the evidence is weak. BMJ. 2003;326(7398):1049–1050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Parati G, Steptoe A. Stress reduction and blood pressure control in hypertension: a role for transcendental meditation? J Hypertens. 2004;22(11):2057–2060. [DOI] [PubMed] [Google Scholar]
- 17.Nidich SI, Fields JZ, Rainforth MV, et al. A randomized controlled trial of the effects of transcendental meditation on quality of life in older breast cancer patients. Integr Cancer Ther. 2009;8(3):228–234. [DOI] [PubMed] [Google Scholar]
- 18.Chhatre S, Metzger DS, Frank I, et al. Effects of behavioral stress reduction Transcendental Meditation intervention in persons with HIV. AIDS Care. 2013;25(10):1291–1297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fan AZ, Strine TW, Jiles R, Mokdad AH. Depression and anxiety associated with cardiovascular disease among persons aged 45 years and older in 38 states of the United States, 2006. Prev Med. 2008;46(5):445–450. [DOI] [PubMed] [Google Scholar]
- 20.Thombs BD, Bass EB, Ford DE, et al. Prevalence of depression in survivors of acute myocardial infarction. J Gen Intern Med. 2006;21(1):30–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264–269. [DOI] [PubMed] [Google Scholar]
- 22.Miller W, Brown J, Simpson T. What works? A methodological analysis of the alcohol treatment outcome literature Handbook of Alcoholism Treatment Approaches. Boston, MA: Alynn & Bacon; 1995. [Google Scholar]
- 23.Jadad AR, Moore RA, Carroll D, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17(1):1–12. [DOI] [PubMed] [Google Scholar]
- 24.Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. Journal of Epidemiology & Community Health. 1998;52(6):377–384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fowkes F, Fulton P. Critical appraisal of published research: introductory guidelines. BMJ. 1991;302(6785):1136–1140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Morris SB, DeShon RP. Combining effect size estimates in meta-analysis with repeated measures and independent-groups designs. Psychol Methods. 2002;7(1):105–125. [DOI] [PubMed] [Google Scholar]
- 27.Becker BJ. Synthesizing standardized mean‐change measures. Br J Math Stat Psychol. 1988;41(2):257–278. [Google Scholar]
- 28.Hedges LV. Distribution theory for Glass’s estimator of effect size and related estimators. Journal of Educational Statistics. 1981;6(2):107–128. [Google Scholar]
- 29.Lipsey MW, Wilson DB. Practical meta-analysis. Thousand Oaks, CA: Sage Publications, Inc; 2001. [Google Scholar]
- 30.Emerson JD, Strenio J. Boxplots and batch comparison In: Hoaglin D, Mosteller F, Tukey J, eds. Understanding robust and exploratory data analysis. New York: John Wiley & Sons; 1983:58–96. [Google Scholar]
- 31.Higgins JP, Thompson SG. Quantifying heterogeneity in a meta‐analysis. Stat Med. 2002;21(11):1539–1558. [DOI] [PubMed] [Google Scholar]
- 32.Huedo-Medina TB, Sánchez-Meca J, Marín-Martínez F, Botella J. Assessing heterogeneity in meta-analysis: Q statistic or I2 index? Psychol Methods. 2006;11(2):193–206. [DOI] [PubMed] [Google Scholar]
- 33.StataCorpLP. Stata Statistical Software; 15.1 for Windows ed. College Station, TX: 2017. [Google Scholar]
- 34.Comprehensive Meta-Analysis [computer program]. Version 3. New Jersey: Biostat; 2013. [Google Scholar]
- 35.Calderon R Jr. Effects of nonpharmacological approaches on cholesterol levels in mild hypertensive African Americans: A pilot study of the Transcendental Meditation program and a health education program [Ph.D.]. Ann Arbor, Maharishi University of Management; 2000. [Google Scholar]
- 36.Vivier EH. Effects of a multimodal approach of Maharishi consciousness-based health care on carotid atherosclerosis: A study of coronary artery disease patients [Ph.D.]. Ann Arbor, Maharishi University of Management; 2004. [Google Scholar]
- 37.Jayadevappa R, Johnson JC, Bloom BS, et al. Effectiveness of transcendental meditation on functional capacity and quality of life of African Americans with congestive heart failure: A randomized control study. Ethn Dis. 2007;16(1):72–77. [PMC free article] [PubMed] [Google Scholar]
- 38.Paul-Labrador M, Polk D, Dwyer JH, et al. Effects of a randomized controlled trial of transcendental meditation on components of the metabolic syndrome in subjects with coronary heart disease. Arch Intern Med. 2006;166(11):1218–1224. [DOI] [PubMed] [Google Scholar]
- 39.Duraimani S, Schneider RH, Randall OS, et al. Effects of Lifestyle Modification on Telomerase Gene Expression in Hypertensive Patients: A Pilot Trial of Stress Reduction and Health Education Programs in African Americans. PLoS One. 2015;10(11):e0142689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kondwani KA, Schneider RH, Alexander CN, et al. Left Ventricular Mass Regression with the Transcendental Meditation Technique and a Health Education Program in Hypertensive African Americans. Journal of Social Behavior and Personality. 2005;17(1):181–200. [Google Scholar]
- 41.Schneider RH, Alexander CN, Staggers F, et al. A randomized controlled trial of stress reduction in African Americans treated for hypertension for over one year. Am J Hypertens. 2005;18(1):88–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Schneider RH, Staggers F, Alexander CN, et al. A Randomized Controlled Trial of Stress Reduction for Hypertension in Older African-Americans. Hypertension. 1995;26(5):820–827. [DOI] [PubMed] [Google Scholar]
- 43.Schneider RH, Grim CE, Rainforth MV, et al. Stress Reduction in the Secondary Prevention of Cardiovascular Disease Randomized, Controlled Trial of Transcendental Meditation and Health Education in Blacks. Circ Cardiovasc Qual Outcomes. 2012;5(6):750–758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Barnes VA, Schneider RH, Alexander CN, et al. Impact of the Transcendental Meditation Program on Mortality in Older African Americans with Hypertension -- Eight-Year Follow-Up. Journal of Social Behavior & Personality. 2005;17(1):201–216. [Google Scholar]
- 45.Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1(3):385–401. [Google Scholar]
- 46.Veit CT, Ware JE. The structure of psychological distress and well-being in general populations. J Consult Clin Psychol. 1983;51(5):730–742. [DOI] [PubMed] [Google Scholar]
- 47.Lau J, Ioannidis JP, Terrin N, Schmid CH, Olkin I. The case of the misleading funnel plot. BMJ. 2006;333(7568):597–600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sirois FM, Jiang L, Upchurch DM. Use and Disclosure of Complementary Health Approaches in US Adults With Cardiovascular Disease. Am J Cardiol. 2018;122(1):170–174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Clarke TC, Barnes P, Black L, Stussman B, Nahin R. Use of Yoga, Meditation, and Chiropractors Among US Adults Aged 18 and Over. NCHS data brief. 2018(325):1–8. [PubMed] [Google Scholar]
- 50.Anderson JW, Liu C, Kryscio RJ. Blood pressure response to transcendental meditation: a meta-analysis. Am J Hypertens. 2008;21(3):310–316. [DOI] [PubMed] [Google Scholar]
- 51.Bai Z, Chang J, Chen C, Li P, Yang K, Chi I. Investigating the effect of transcendental meditation on blood pressure: a systematic review and meta-analysis. J Hum Hypertens. 2015;29(11):653–662. [DOI] [PubMed] [Google Scholar]
- 52.Benson H The relaxation response: History, physiological basis and clinical usefulness. Acta Med Scand. 1982;212(Suppl. 660):231–237. [DOI] [PubMed] [Google Scholar]
- 53.Benson H, Klipper MZ. The relaxation response. Harper Collins, New York; 1992. [Google Scholar]
- 54.Holt EW, Muntner P, Joyce C, Morisky DE, Webber LS, Krousel-Wood M. Life events, coping, and antihypertensive medication adherence among older adults: the cohort study of medication adherence among older adults. Am J Epidemiol. 2012;176(suppl_7):S64–S71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Castillo-Richmond A, Schneider RH, Alexander CN, et al. Effects of stress reduction on carotid atherosclerosis in hypertensive African Americans. Stroke. 2000;31(3):568–573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Schneider RH, Castillo-Richmond A, Alexander CN, et al. Behavioral treatment of hypertensive heart disease in African Americans: Rationale and design of a randomized controlled trial. Behavioral Medicine. 2001;27(2):83–95. [DOI] [PubMed] [Google Scholar]
- 57.Schneider R, Alexander C, Myers H, et al. Lifestyle modification in the prevention of left ventricular hypertrophy: A randomized controlled trial of stress reduction and health education in hypertensive African Americans. J Hypertens. 2006;24(Suppl. 6):90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Schneider R Stress Reduction and Atherosclerotic CVD in Blacks. https://clinicaltrials.gov/ct2/show/NCT00000546. Accessed April 16, 2018.
- 59.Randall O Evaluating Mechanisms of Blood Pressure Reduction Using Meditation in Hypertensive African Americans (HMEC). https://clinicaltrials.gov/ct2/show/NCT00681200. Accessed April 16, 2018. [Google Scholar]
- 60.Duraimani Lakshmi. Lifestyle Modifications and Healthy Biological Aging: Effects of Telomerase Activity and Telomere Length [Ph.D.]. Ann Arbor, Maharishi University of Management; 2012. [Google Scholar]
- 61.Mattik L Effect of the Transcendental Meditation Program and Health Education on Allostatic Load: Promoting Normal Aging [Ph.D.]. Ann Arbor, Maharishi University of Management; 2011. [Google Scholar]
- 62.Jayadevappa R, Canter PH. Is transcendental meditation effective in congestive heart failure? Focus on Alternative & Complementary Therapies. 2007;12(3):199–201. [Google Scholar]
- 63.Jayadevappa R, Johnson JC, Bloom BS, et al. Erratum: Effectiveness of transcendental meditation on functional capacity and quality of life of African Americans with congestive heart failure: A randomized control study. Ethn Dis. 2007;17(3):595. [PMC free article] [PubMed] [Google Scholar]
- 64.Kondwani KA. Nonpharmacologic treatment of hypertensive heart disease in African-Americans: A trial of the Transcendental Meditation program and a health education program [Ph.D.]. Ann Arbor, Maharishi University of Management; 1998. [Google Scholar]
- 65.Paul-Labrador MJ, Merz CNB, Dwyer JH, et al. Transcendental meditation improves insulin resistance in coronary artery disease subjects: A randomized controlled trial Paper presented at: Circulation; Oct, 2003. [Google Scholar]
- 66.Merz CNB. Effects of Meditation on Mechanism of Coronary Heart Disease. https://clinicaltrials.gov/ct2/show/NCT00010738. Accessed April 16, 2018.
- 67.Paul-Labrador M, Merz CNB. In reply. Arch Intern Med. 2006;166(22):2554‐.17159026 [Google Scholar]
- 68.Schneider R, Alexander C, Staggers F, et al. Effects of stress reductionon hypertension in African Americans: A randomized controlled trial over one year Paper presented at: Circulation2003. [Google Scholar]
- 69.Schneider R A Randomized Controlled Trial of Stress Reduction on Cardiovascular Morbidity and Mortality in African Americans. https://clinicaltrials.gov/ct2/show/NCT01299935. Accessed April 16, 2018.
- 70.Alexander CN, Schneider RH, Staggers F, et al. Trial of stress reduction for hypertension in older African Americans. II. Sex and risk subgroup analysis. Hypertension. 1996;28(2):228–237. [DOI] [PubMed] [Google Scholar]
- 71.Barnes VA. Reduced cardiovascular and all-cause mortality in older African Americans practicing the Transcendental Meditation. US, ProQuest Information & Learning; 1997. [Google Scholar]
- 72.Clayborne BM. Effects of Stress Reduction on Anger and Cardiovascular Reactivity in Hypertensive African Americans: A Randomized Controlled Trial of Transcendental Meditation and Progressive Relaxation. Abstract presented at International Interdisciplinary Conference on Hypertension and Related Cardiovascular Risk Factors in Ethnic Populations; 1997, 1997. [Google Scholar]
- 73.Schneider RH, Alexander CN, Staggers F, et al. Long-term effects of stress reduction on mortality in persons > or = 55 years of age with systemic hypertension. The American journal of cardiology. 2005;95(9):1060–1064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Schneider RH, Alexander CN, Rainforth M, et al. A Controlled Trial of Transcendental Meditation and Progressive Relaxation- For Treatent of Hypertension in Elderly African-Americans. Psychosom Med. 1994;56(2):175–175. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


