Abstract
Background:
Surgical treatment of both-column acetabular fractures is challenging because of the complex acetabular fracture patterns and the curved surface of the acetabulum. Seldom study has compared the application of three-dimensional (3D) printing technology and traditional methods of contouring plates intra-operatively for the surgical treatment of both-column acetabular fractures. We presented the use of both 3D printing technology and a virtual simulation in pre-operative planning for both-column acetabular fractures. We hypothesized that 3D printing technology will assist orthopedic surgeons in shortening the surgical time and improving the clinical outcomes.
Methods:
Forty patients with both-column acetabular fractures were recruited in the randomized prospective case–control study from September 2013 to September 2017 for this prospective study (No. ChiCTR1900028230). We allocated the patients to two groups using block randomization (3D printing group, n = 20; conventional method group, n = 20). For the 3D printing group, 1:1 scaled pelvic models were created using 3D printing, and the plates were pre-contoured according to the pelvic models. The plates for the conventional method group were contoured during the operation without 3D printed pelvic models. The operation time, instrumentation time, time of intra-operative fluoroscopy, blood loss, number of times the approach was performed, blood transfusion, post-operative fracture reduction quality, hip joint function, and complications were recorded and compared between the two groups.
Results:
The operation and instrumentation times in the 3D printing group were significantly shorter (130.8 ± 29.2 min, t = −7.5, P < 0.001 and 32.1 ± 9.5 min, t = −6.5, P < 0.001, respectively) than those in the conventional method group. The amount of blood loss and blood transfusion in the 3D printing group were significantly lower (500 [400, 800] mL, Mann-Whitney U = 74.5, P < 0.001 and 0 [0,400] mL, Mann-Whitney U = 59.5, P < 0.001, respectively) than those in the conventional method group. The number of the approach performed in the 3D printing group was significantly smaller than that in the conventional method group (pararectus + Kocher-Langenbeck [K-L] approach rate: 35% vs. 85%; χ2 = 10.4, P < 0.05). The time of intra-operative fluoroscopy in the 3D printing group was significantly shorter than that in the conventional method group (4.2 ± 1.8 vs. 7.7 ± 2.6 s; t = −5.0, P < 0.001). The post-operative fracture reduction quality in the 3D printing group was significantly better than that in the conventional method group (good reduction rate: 80% vs. 30%; χ2 = 10.1, P < 0.05). The hip joint function (based on the Harris score 1 year after the operation) in the 3D printing group was significantly better than that in the conventional method group (excellent/good rate: 75% vs. 30%; χ2 = 8.1, P < 0.05). The complication was similar in both groups (5.0% vs. 25%; χ2 = 3.1, P = 0.182).
Conclusions:
The use of a pre-operative virtual simulation and 3D printing technology is a more effective method for treating both-column acetabular fractures. This method can shorten the operation and instrumentation times, reduce blood loss, blood transfusion and the time of intra-operative fluoroscopy, and improve the post-operative fracture reduction quality.
Clinical trail registration:
No.ChiCTR1900028230; http://www.chictr.org.cn
Keywords: Both-column, Acetabulum fractures, Computer simulation, Three-dimensional printing, Internal fracture fixation
Introduction
Both-column acetabular fractures are the most serious and the second most common type of acetabular fractures. Approximately 21% of all acetabular fractures involving both columns of the acetabulum require good reduction and stable internal fixation to prevent post-traumatic arthritis and obtain excellent clinical outcomes.[1] Surgical treatment of both-column acetabular fractures is challenging because of the complex acetabular fracture patterns and curved surface of the acetabulum. In a traditional operation for acetabular fractures, the limited number of anterior approaches available (ilioinguinal or modified Stoppa) and contouring of the plates during the surgery result in an increase in the operation time and blood loss. Moreover, intra-operative contouring may reduce the quality of the reduction.
Three-dimensional (3D) printing technology is developing rapidly and is broadly used in clinical applications because it is easily accessible in terms of the equipment and cost.[2–5] Pre-operative virtual simulations can help a surgeon understand the shape of the fracture fragments and simulate the reduction of the fracture, especially in complex acetabular fractures.[6–12] The 3D printed, 1:1 scaled pelvic models can be used in the pre-contouring of the plates.[13–15] In addition, the pre-contoured plates can be used to achieve anatomical reduction of acetabular fractures.
Prior studies have revealed that the application of 3D printing technology in the surgical treatment of acetabular fractures can significantly reduce the operation time and blood loss but cannot obtain a fracture reduction of significantly better quality.[2,16–18] Many factors, such as the type of the acetabular fracture and the operation level of the orthopedic surgeon, may affect the clinical outcomes reported in these studies. Shon et al[19] reported five cases of both-column acetabular fractures treated with the use of 3D-printed models, and all of them achieved good-to-excellent reduction and good medium-term functional outcomes. Chen et al[20] reported 52 cases of bicolumnar acetabular fractures (including “T” shaped fractures, anterior column + posterior hemi-transverse fractures and both-column fractures) treated with and without 3D printing technology, and they achieved similar clinical outcomes as those reported in previous studies. However, few studies have focused on the types of acetabular fractures. Seldom study has compared the application of 3D printing technology and traditional methods of contouring plates intra-operatively for the surgical treatment of both-column acetabular fractures. We hypothesized that 3D printing technology will assist orthopedic surgeons in shortening the operation time and improving the clinical outcomes, such as the post-operative fracture reduction quality, hip joint function, and complication rate.
Methods
Ethical approval
Ethical approval was obtained from the Ethics Review Board of The Third Affiliated Hospital of Southern Medical University (No. 201304002). Informed consent forms were duly signed by each patient included in the study.
Patients
A total of 40 patients diagnosed with both-column acetabular fractures were included in the randomized prospective case–control study from September 2013 to September 2017. Twenty patients were allocated to the 3D-printing group, and the other 20 patients were allocated to the conventional method group using block randomization.
The inclusion criteria were (1) an age of 18 to 70 years, (2) the presence of a both-column acetabular fracture according to the Letournel-Judet classification, and (3) a lapse of fewer than 3 weeks from the injury. The exclusion criteria were (1) an age of <18 years, (2) another type of acetabular fracture according to the Letournel-Judet classification,[21] (3) an open fracture of the acetabulum, and (4) a lapse of more than 3 weeks from the injury.
Virtual simulation and 3D printing
The computed tomography images of each patient's pelvis were saved as DICOM (Digital Imaging and Communication in Medicine) files and imported into the 3D image processing software (MIMICS, version 15; Materialise, Leuven, Belgium). The masks of the fracture fragments were selected using the Edit in 3D function. The 3D models of the fracture fragments were calculated using the Calculate 3D from Mask function [Figure 1A]. The fracture fragments were reduced anatomically using the reposition function [Figure 1B]. The anatomically reduced 3D model of the fractured hemi-pelvis was exported as a binary stereolithography (STL) file, which was imported into Magics 21.0 software (Materialise) for fixing and support generation [Figure 1C and 1D]. The reduced hemi-pelvis model that was exported as an STL file was sent to the 3D printer (Prismlab Rapid400; Prismlab, Shanghai, China) for 3D printing. The plates were pre-contoured, and the length of the screws was measured using the 3D printed reduced hemi-pelvis model. After the surgical simulation, the pre-contoured anatomic plates and screws were disinfected. All the software and 3D printing procedures were performed by a single experienced 3D-printing engineer.
Figure 1.
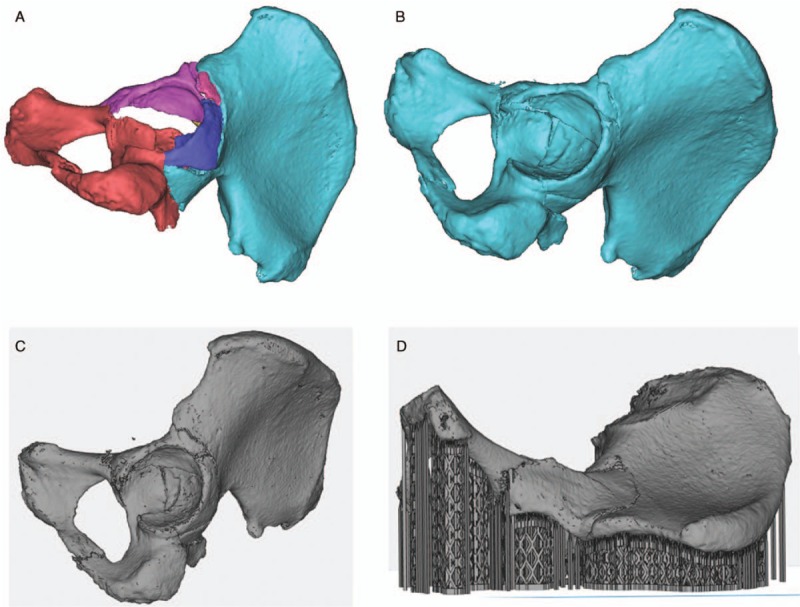
The 3D models of the fracture fragments were calculated using the calculate 3D from Mask function (A). The fracture fragments were reduced anatomically using the reposition function (B). The anatomically reduced 3D models of the fractured hemi-pelvis were exported as binary STL format files, which were imported into Magics 21.0 software (Materialise, Belgium) for fixing and support generation (C and D). 3D: Three-dimensional; STL: Stereolithography.
Surgical technique
The combination of the pararectus approach and Kocher-Langenbeck (K-L) approach or the pararectus approach alone was used for the patients included in this study [Figure 2A and 2B].
Figure 2.
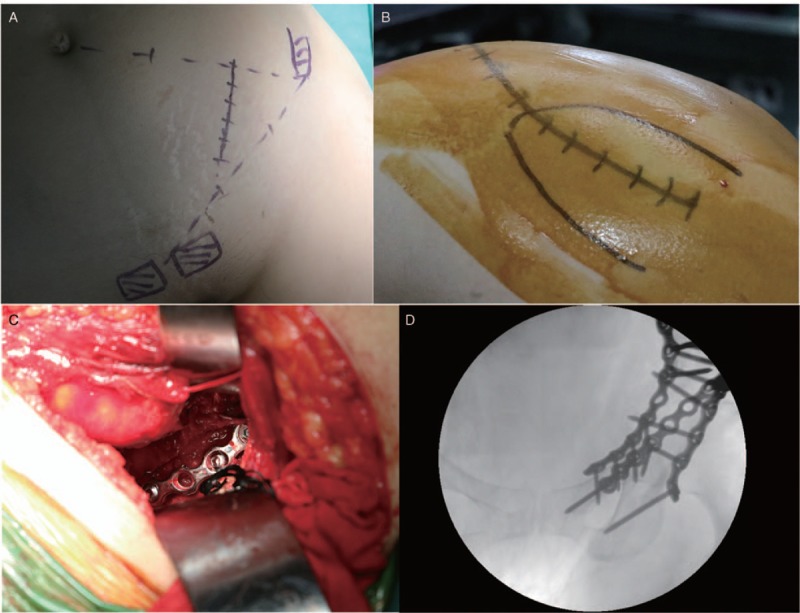
The Kocher-Langenbeck (K-L) approach (A). The pararectus approach (B). The disinfected pre-contoured anatomic plates and screws were placed in the position designated pre-operatively after the fracture reduction (C). The fluoroscopy was performed before closure to confirm the adequacy of the procedure (D).
In the 3D printing group, the disinfected pre-contoured anatomic plates and screws were set in the position designated pre-operatively after the fracture reduction [Figure 2C]. In the conventional method group, the plates were contoured, and the lengths of the screws were measured after the fracture reduction. Fluoroscopy was performed before closure to confirm the adequacy of the procedure [Figure 2D].
The rehabilitation protocol was initiated the first day after surgery, and it included active range of motion of the injured hip and isometric quadriceps strengthening. Non-weight bearing activities were allowed 4 weeks after the operation, partial weight bearing was allowed at 6 weeks according to the follow-up radiographs, and full weight bearing was allowed at 3 months.
Evaluation
The operation time was considered the time from the skin incision to closure. The instrumentation time was considered the time from the plate configuration adjustments to implantation of the last screw. The number of the approach was recorded, and the pararectus + K-L approach rate was calculated and compared between the two groups. The time of intra-operative fluoroscopy was defined as the total duration of fluoroscopy before skin closure. Blood loss was recorded by calculating the amount of blood in the suction bottle and in the used gauze. Blood transfusion and time of bone union in both groups were also compared. The post-operative plain radiographs were evaluated by two experienced orthopedic surgeons. The evaluation criteria of the quality of reduction were as follows: a displacement of <2 mm was considered good, and a displacement of ≥2 mm was considered fair. The function of the hip joint was assessed according to the Harris score 1 year after the operation.[22] The function of the hip joint was considered excellent/good (Harris score of ≥80 points) or fair/poor (Harris score of <80 points). The complications included heterotopic ossification, an inflammatory response, iatrogenic neurological symptoms, and traumatic arthritis. Images of one patient in the 3D printing group are shown in Figure 3.
Figure 3.
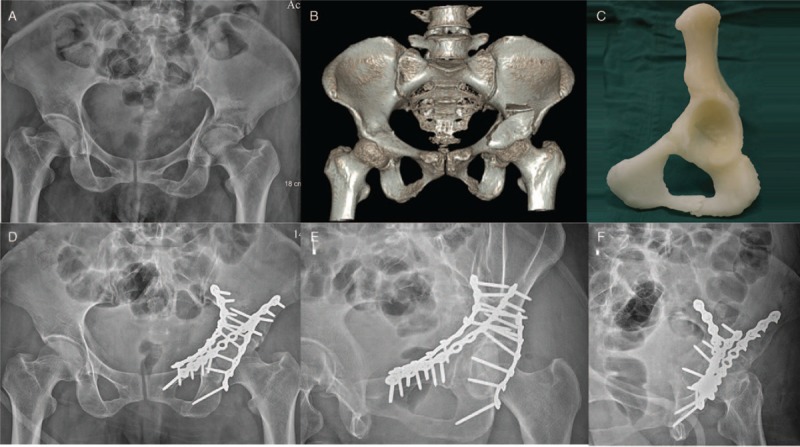
Images of one case in the 3D printing group. (A) Pre-operative radiograph (anteroposterior view). (B) The 3D reconstructed computed tomography images. (C) The 3D printed model used for pre-operative evaluation. (D–F) Post-operative follow-up radiograms at 1 year (pelvic anteroposterior and Judet views). 3D: Three-dimensional.
Statistical analysis
SPSS statistical software (version 20.0; SPSS, Inc., Chicago, IL, USA) was used for all the statistical analyses. Continuous variables were analyzed using an independent-samples t test. Variables with non-normal distributions were analyzed using the Mann-Whitney test. Categorical variables with expected values of greater than 5 were evaluated using the Chi-squared test, while categorical variables with expected values of less than 5 were evaluated using Fisher's exact test. A P < 0.05 was considered the significance level for all of the statistical tests.
Results
Demographic and clinical data
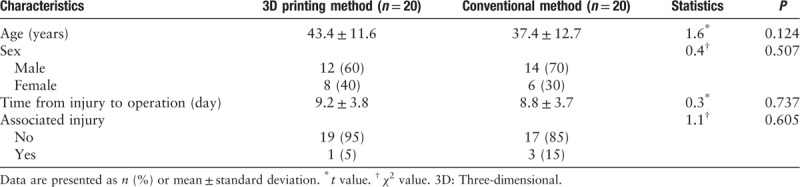
The demographics were comparable between the groups (age: t = 1.6, P > 0.05; sex: χ2 = 0.4, P > 0.05). There was no significant difference in associated injuries between the groups (χ2 = 1.1, P > 0.05). The mean times from injury to operation were 9.2 ± 3.8 and 8.8 ± 3.7 days in the 3D printing and conventional method groups, respectively (t = 0.3, P > 0.05). The average follow-up durations were 40.0 ± 14.5 and 45.2 ± 15.2 months in the 3D printing and conventional method groups, respectively (t = −1.1, P > 0.05) [Table 1].
Table 1.
Demographic data of patients with both-column acetabular fractures.
Intra-operative clinical outcomes
The operation time in the 3D printing group was significantly shorter than that in the conventional method group (130.8 ± 29.2 vs. 206.3 ± 34.6 min; t = −7.5, P < 0.001). The instrumentation time in the 3D printing group was significantly shorter than that in the conventional method group (32.1 ± 9.5 vs. 57.9 ± 15.1 min; t = −6.5, P < 0.001). The amounts of blood loss and blood transfusion in the 3D printing group were significantly lower (500 [400, 800] mL, Mann-Whitney U = 74.5, P < 0.001 and 0 (0, 400) mL, Mann-Whitney U = 59.5, P < 0.001, respectively) than those in the conventional method group. The number of the approach in the 3D printing group was significantly smaller than that in the conventional method group (pararectus + K-L approach rate: 35% vs. 85%; χ2 = 10.4, P < 0.05). The time of intra-operative fluoroscopy in the 3D printing group was significantly shorter than that in the conventional method group (4.2 ± 1.8 vs. 7.7 ± 2.6 s; t = −5.0, P < 0.001) [Table 2].
Table 2.
Clinical characteristics and outcomes of patients with both-column acetabular fractures.
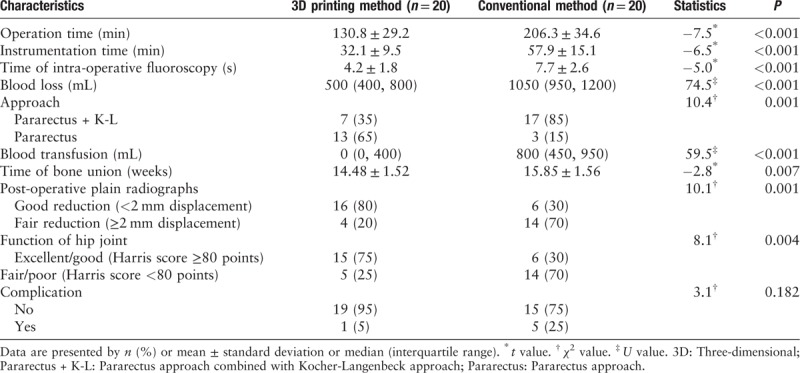
Post-operative evaluation
The post-operative fracture reduction quality in the 3D printing group was significantly better than that in the conventional method group (good reduction rate: 80% vs. 30%; χ2 = 10.1, P < 0.05). The hip joint function in the 3D printing group was significantly better than that in the conventional method group (excellent/good rate: 75% vs. 30%; χ2 = 8.1, P < 0.05) [Table 2].
Complications
In the 3D printing group, one patient suffered heterotopic ossification 2 months after the operation. In the conventional method group, two patients suffered an inflammatory response, one patient had heterotopic ossification 1 month after the operation, one patient had iatrogenic neurological symptoms that resolved 5 months after the operation, and one patient had post-traumatic arthritis. The complication rate was similar in both groups (5% vs. 25%; χ2 = 3.1, P = 0.182) [Table 2].
Discussion
Prior studies have documented the effectiveness of pre-operative virtual simulations and 3D printing techniques in the surgical treatment of acetabular fractures in reducing the operation time and blood loss.[2,16–18,20] Maini et al[17] reported a randomized prospective case–control study that included 21 patients with acetabular fractures and concluded that the pre-contoured plates made using patient-specific 3D printed pelvic models were better than the plates contoured intra-operatively. Zeng et al[15] reported that a combination of 3D printing and computer-assisted virtual surgical procedures can significantly improve the clinical outcomes of patients with acetabular fractures. Merema et al[6] showed that 3D printed patient-specific plates and drilling templates are feasible, effective, and safe for the surgical treatment of acetabular fractures. Hsu et al[2] demonstrated the effectiveness of pre-operative virtual simulations and 3D printing techniques for the surgical treatment of 29 patients with acetabular fractures in shortening the surgical duration and reducing the blood loss. Li et al[16] reported a retrospective study that included 16 patients diagnosed with traumatic dislocation of the hip joint combined with acetabular fractures and demonstrated that the combination of 3D printing techniques and computer-assisted simulations using pre-contoured plates is effective for the surgical treatment of acetabular fractures. Chen et al.[20] reported a retrospective study that included 52 cases of bicolumnar acetabular fractures and found that computer-assisted virtual simulations and 3D printing techniques are clinically relevant in the surgical treatment of complicated acetabular fractures. Shon et al[19] reported five cases of both-column acetabular fractures treated with the use of 3D-printed models, and all of them achieved good-to-excellent reduction and good medium-term functional outcomes. Wan et al[18] reported a retrospective study that included 96 patients with acetabular fractures and revealed that the combination of 3D printing techniques and computer-assisted simulations can remarkably improve the accuracy and safety of the clinical operation.
However, these studies had either a small sample size or did not compare the same types of acetabular fractures. Most of the previous studies used 3D models of the pelvis mirrored from the healthy side to contour the plates pre-operatively, which could not simulate the actual shape of the fracture fractured fragments.[2,16] The K-L approach was used for posterior column acetabular fractures, and the ilioinguinal approach[23] or Stoppa approach[24] was used for anterior column acetabular fractures in most of the previous studies.[25] In our opinion, the ilioinguinal or Stoppa approach will lead to damage to the surrounding soft tissues and blood loss. There were no significant differences between the groups in the clinical outcomes reported in the previous studies.
This study with a large sample size compared the use of 3D printing technology with conventional method of contouring the plates in the surgical treatment of patients with both-column acetabular fractures. In addition, we used 3D printed reduced hemi-pelvis models to pre-contour the plates.
We found that the post-operative fracture reduction quality and the hip joint function in the 3D printing group were significantly better than those in the conventional method group. The pre-contoured plates contributed the most to this difference because the type of acetabular fractures and the surgeon were the same in both groups. The 3D printed reduced hemi-pelvis models may help in anatomically pre-contouring the plates to obtain good fracture reduction quality and hip joint function and reduce the risk of traumatic arthritis. In addition, the 3D printed reduced hemi-pelvis models may contribute to a reduction in the number of times the approach is performed and the amount of damage caused by the surgery. The operation time, the instrumentation time, and the time of intra-operative fluoroscopy were significantly shorter, and the blood loss and blood transfusion were significantly less in the 3D printing group than in the conventional method group. The complication rate was similar in both groups. One patient in the conventional method group had post-traumatic arthritis that was treated with total-hip replacement. These results extended those reported by Maini et al,[17] illustrating that fracture reduction quality and hip joint function in the 3D printing group were significantly better than those in the conventional method group. In addition, these findings confirmed that the operation time was significantly shorter and reveal that the time of intra-operative fluoroscopy was significantly shorter in the 3D printing group. This study indicated that a pre-operative virtual simulation with 3D printing technology was a more effective method for treating both-column acetabular fractures. This study reported significantly better clinical outcomes with the 3D method because the type of acetabular fractures and the surgeon were the same in both groups and the sample size was large. The results of this study provided compelling evidence for the surgical treatment of acetabular fractures and suggest that 3D printing technology appears to be effective for the surgical treatment of acetabular fractures.
However, some limitations should be noted in this study. First, although the types of fractures were classified by three experienced orthopedic doctors according to the Letournel-Judet classification, the results may be inaccurate because a few types of acetabular fractures cannot be classified according to the Letournel-Judet classification. Second, although our 3D printer (Prismlab Rapid400; Prismlab) can significantly shorten the time of 3D printing, the high cost of the 3D models printed by our 3D printer may limit the applicability of this method. Third, although the results in this study support our hypothesis statistically, the sample size may not be sufficiently large because both-column acetabular fractures are very rare. Future studies with a sufficiently large sample size are necessary to confirm the effectiveness of the application of pre-operative virtual simulations and 3D printing techniques in the surgical treatment of both-column acetabular fractures.
In conclusion, a pre-operative virtual simulation with 3D printing technology is a more effective method than the conventional method to treat both-column acetabular fractures. This method can shorten the operation and instrumentation time, reduce blood loss, blood transfusion, and the time of intra-operative fluoroscopy, and improve the post-operative fracture reduction quality.
Funding
This work was supported by the grants from the High Level University Development Foundation of Southern Medical University (No. LC2016PY045), the Science and Technology Projects of Tianhe District in Guangdong Province (No. 2018YZ011), and the Science and Technology Projects in Guangdong Province (No. 2016B090917001).
Conflicts of interest
None.
Footnotes
How to cite this article: Huang JH, Liao H, Tan XY, Xing WR, Zhou Q, Zheng YS, Cao HY, Zeng CJ. Surgical treatment for both-column acetabular fractures using pre-operative virtual simulation and three-dimensional printing techniques. Chin Med J 2020;133:395–401. doi: 10.1097/CM9.0000000000000649
References
- 1.Mauffrey C, Hao J, Cuellar DO, 3rd, Herbert B, Chen X, Liu B, et al. The epidemiology and injury patterns of acetabular fractures: are the USA and China comparable? Clin Orthop Relat Res 2014; 472:3332–3337. doi: 10.1007/s11999-014-3462-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hsu CL, Chou YC, Li YT, Chen JE, Hung CC, Wu CC, et al. Pre-operative virtual simulation and three-dimensional printing techniques for the surgical management of acetabular fractures. Int Orthop 2019; 43:1969–1976. doi: 10.1007/s00264-018-4111-8. [DOI] [PubMed] [Google Scholar]
- 3.Wang H, Guo YT, Jiao Y, He DL, Wu B, Yuan LJ, et al. A minimally invasive alternative for the treatment of nutcracker syndrome using individualized three-dimensional printed extravascular titanium stents. Chin Med J 2019; 132:1454–1460. doi: 10.1097/CM9.0000000000000255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Li M, Li ZR, Li JT, Lei MX, Su XY, Wang GQ, et al. Three-dimensional mapping of intertrochanteric fracture lines. Chin Med J 2019; 132:2524–2533. doi: 10.1097/CM9.0000000000000446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tian H, Zhao MW, Geng X, Zhou QY, Li Y. Patient-specific instruments based on knee joint computed tomography and full-length lower extremity radiography in total knee replacement. Chin Med J 2018; 131:583–587. doi: 10.4103/0366-6999.226062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Merema BJ, Kraeima J, Ten Duis K, Wendt KW, Warta R, Vos E, et al. The design, production and clinical application of 3D patient-specific implants with drilling guides for acetabular surgery. Injury 2017; 48:2540–2547. doi: 10.1016/j.injury.2017.08.059. [DOI] [PubMed] [Google Scholar]
- 7.Duncan JM, Nahas S, Akhtar K, Daurka J. The use of a 3D printer in pre-operative planning for a patient requiring acetabular reconstructive surgery. J Orthop Case Rep 2015; 5:23–25. doi: 10.13107/jocr.2250-0685.247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Upex P, Jouffroy P, Riouallon G. Application of 3D printing for treating fractures of both columns of the acetabulum: benefit of pre-contouring plates on the mirrored healthy pelvis. Orthop Traumatol Surg Res 2017; 103:331–334. doi: 10.1016/j.otsr.2016.11.021. [DOI] [PubMed] [Google Scholar]
- 9.Chana-Rodriguez F, Mananes RP, Rojo-Manaute J, Gil P, Martinez-Gomiz JM, Vaquero-Martin J. 3D surgical printing and pre contoured plates for acetabular fractures. Injury 2016; 47:2507–2511. doi: 10.1016/j.injury.2016.08.027. [DOI] [PubMed] [Google Scholar]
- 10.Boudissa M, Courvoisier A, Chabanas M, Tonetti J. Computer assisted surgery in preoperative planning of acetabular fracture surgery: state of the art. Expert Rev Med Devices 2018; 15:81–89. doi: 10.1080/17434440.2017.1413347. [DOI] [PubMed] [Google Scholar]
- 11.Huang Z, Song W, Zhang Y, Zhang Q, Zhou D, Zhou X, et al. Three-dimensional printing model improves morphological understanding in acetabular fracture learning: a multicenter, randomized, controlled study. PLoS One 2018; 13:e0191328.doi: 10.1371/journal.pone.0191328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kim JW, Lee Y, Seo J, Park JH, Seo YM, Kim SS, et al. Clinical experience with three-dimensional printing techniques in orthopedic trauma. J Orthop Sci 2018; 23:383–388. doi: 10.1016/j.jos.2017.12.010. [DOI] [PubMed] [Google Scholar]
- 13.Maini L, Mishra A, Agarwal G, Verma T, Sharma A, Tyagi A. 3D printing in designing of anatomical posterior column plate. J Clin Orthop Trauma 2018; 9:236–240. doi: 10.1016/j.jcot.2018.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Maini L, Verma T, Sharma A, Sharma A, Mishra A, Jha S. Evaluation of accuracy of virtual surgical planning for patient-specific pre-contoured plate in acetabular fracture fixation. Arch Orthop Trauma Surg 2018; 138:495–504. doi: 10.1007/s00402-018-2868-2. [DOI] [PubMed] [Google Scholar]
- 15.Zeng C, Xing W, Wu Z, Huang H, Huang W. A combination of three-dimensional printing and computer-assisted virtual surgical procedure for preoperative planning of acetabular fracture reduction. Injury 2016; 47:2223–2227. doi: 10.1016/j.injury.2016.03.015. [DOI] [PubMed] [Google Scholar]
- 16.Li YT, Hung CC, Chou YC, Chen JE, Wu CC, Shen HC, et al. Surgical treatment for posterior dislocation of hip combined with acetabular fractures using preoperative virtual simulation and three-dimensional printing model-assisted precontoured plate fixation techniques. Biomed Res Int 2019; 2019:3971571.doi: 10.1155/2019/3971571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Maini L, Sharma A, Jha S, Sharma A, Tiwari A. Three-dimensional printing and patient-specific pre-contoured plate: future of acetabulum fracture fixation? Eur J Trauma Emerg Surg 2018; 44:215–224. doi: 10.1007/s00068-016-0738-6. [DOI] [PubMed] [Google Scholar]
- 18.Wan L, Zhang X, Zhang S, Li K, Cao P, Li J, et al. Clinical feasibility and application value of computer virtual reduction combined with 3D printing technique in complex acetabular fractures. Exp Ther Med 2019; 17:3630–3636. doi: 10.3892/etm.2019.7344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shon HC, Choi S, Yang JY. Three-dimensional printing-assisted surgical technique with limited operative exposure for both-column acetabular fractures. Ulus Travma Acil Cerrahi Derg 2018; 24:369–375. doi: 10.5505/tjtes.2018.47690. [DOI] [PubMed] [Google Scholar]
- 20.Chen K, Yang F, Yao S, Xiong Z, Sun T, Zhu F, et al. Application of computer-assisted virtual surgical procedures and three-dimensional printing of patient-specific pre-contoured plates in bicolumnar acetabular fracture fixation. Orthop Traumatol Surg Res 2019; 2019:877–884. doi: 10.1016/j.otsr.2019.05.011. [DOI] [PubMed] [Google Scholar]
- 21.Judet R, Judet J, Letournel E. Fractures of the acetabulum: classification and surgical approaches for open reduction. Preliminary report. J Bone Joint Surg Am 1964; 46:1615–1646. doi: 10.2106/00004623-196446080-00001. [PubMed] [Google Scholar]
- 22.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am 1969; 51:737–755. doi: 10.2106/00004623-196951040-00012. [PubMed] [Google Scholar]
- 23.Letournel E. The treatment of acetabular fractures through the ilioinguinal approach. Clin Orthop Relat Res 1993; (292):62–76. doi: 10.1097/00003086-199307000-00009. [PubMed] [Google Scholar]
- 24.Stoppa RE. The treatment of complicated groin and incisional hernias. World J Surg 1989; 13:545–554. doi: 10.1007/BF01658869. [DOI] [PubMed] [Google Scholar]
- 25.Wang XJ, Lu L, Zhang ZH, Su YX, Guo XS, Wei XC, et al. Ilioinguinal approach versus Stoppa approach for open reduction and internal fixation in the treatment of displaced acetabular fractures: a systematic review and meta-analysis. Chin J Traumatol 2017; 20:229–234. doi: 10.1016/j.cjtee.2017.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]


